Abstract
Obtaining maximum antiretroviral therapy (ART) adherence is critical for maintaining a high CD4 count and strong immune function in PLWHA. Key factors for achieving optimum adherence include good medication self-efficacy, decreased medication-taking difficulties, and positive patient-healthcare provider (HCP) relationships. Limited studies have analyzed the correlation of these factors and ART adherence in Chinese population. In this paper, structural equation modeling was performed to assess the proposed model of relations between patient-HCP relationships and adherence. Audio Computer-Assisted Self-Interview (ACASI) software was used to collect data on ART adherence and patient variables among 227 PLWHA in Shanghai and Taipei. Participants completed a one-time 60-minute ACASI survey that consisted of standardized measures to assess demographics, recent CD4 counts, self-efficacy, patient-HCP relationship, adherence, and medication-taking difficulties. The data shown the relationship between patient-HCP relationships and adherence was significantly consistent with mediation by medication self-efficacy. However, patient-HCP interaction did not directly influence medication-taking difficulties, and medication-taking difficulties did not significantly affect CD4 counts. Furthermore, patient-HCP interactions did not directly impact CD4 counts; rather, the relation was consistent with mediation (by either better medication self-efficacy or better adherence) or by improved adherence alone. Future interventions should be designed to enhance self-management and provide better patient-HCP communication. This improved communication will enhance medication self-efficacy and decrease medication-taking difficulties. This in turn will improve medication adherence and immune function among PLWHA.
INTRODUCTION
Healthcare Providers (HCPs) play a critical role in supporting patients diagnosed with stigmatized diseases, such as people living with HIV/AIDS (PLWHA) (Chen, Wantland, et al., 2013). Also, HCPs have a greater impact on PLWHA living in collectivist cultures in particular, such as Chinese culture, because HIV stigma may severely deprive PLWHA of social support and resources (Huang et al., 2013). As a result, HCPs often become the only available sources of necessary support, both instrumental and emotional (Rao et al., 2012). Therefore, maintaining positive patient-HCP interactions, particularly in Chinese culture, is crucial for the well-being of PLWHA.
To date, the empirical findings remain far from conclusive regarding the relationships between patient-HCP interactions and patient well-being, particularly patient physical health. Although some empirical studies support the direct associations between positive patients-HCP interactions and improved patient physical outcomes, other studies did not reach similar conclusions (Mead, Bower, & Hann, 2002). In addition, one study on the effects of interventions targeting patient-HCP communication concluded that the interventions had only small, though significant, effect sizes (Kelly et al., 2015). In HIV care, there is limited evidence supporting that positive patient-HCP interactions are associated with increased likelihood of viral suppression, higher CD4 count, less severe symptom experiences, better quality of life (QOL), and long-term survival (Lee, Rand, Ellen, & Agwu, 2014).
One study has shown that strong patient-HCP relationships can enhance self-efficacy and then study participants presented with better ART adherence (Johnson et al., 2006). Another study found a significant association between patient-HCP relationships and improved physical health and functioning, as well as an improved engagement in care, especially in HIV-infected men who have sex with men (Bankoff, McCullough, & Pantalone, 2013). Other studies reported that patient-provider interaction has a direct and positive effect on patient satisfaction, medication adherence, and QOL (Oetzel et al., 2015).
In explaining this weak association between patient-HCP interactions and patient physical outcomes, Street and colleagues contend that mediators may exist linking patient-HCP interactions and patient outcomes, and they propose a multi-step model that inserts proximal and intermediate outcomes in the pathway (Street, Curtis, Sabin, Monteiro, & Johnson, 2009). In Street and colleagues’ definitions, proximal outcomes are psychological, and include factors such as self-efficacy and motivation for optimal care engagement, while intermediate outcomes are behavioral, and include skills and tasks necessary for treatment success, such as medical adherence and self-management (Street et al., 2009). However, there remains a shortage of empirical studies in HIV/AIDS care that seek to integrate multiple pathway factors and simultaneously test their effects in relation to patient-HCP interactions and patient outcomes.
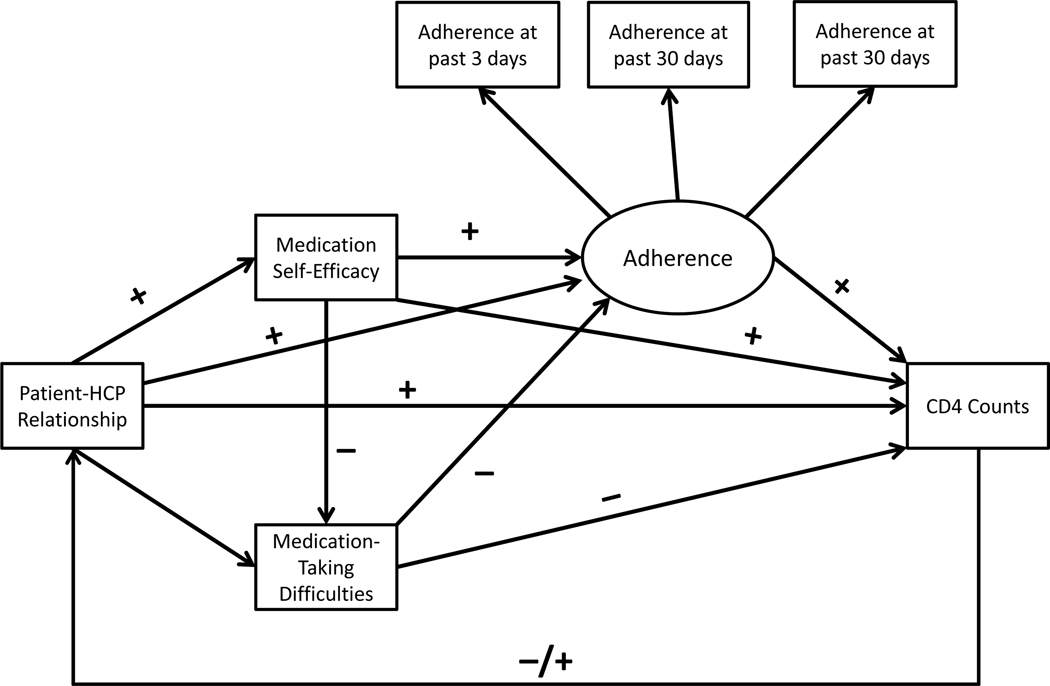
To fill the gap in the literature and to provide insights on potential mechanisms, this study aims to link the patient-HCP interactions to clinically meaningful outcomes through selected psychological and behavioral factors. Utilizing Street and colleagues’ framework, this paper proposes a four-step model as illustrated in Figure 1 (Street et al., 2009). In this model, patient-HCP interactions are associated with PLWHA’s CD4 counts through medication self-efficacy, subjective treatment difficulties, and medication adherence. Medication self-efficacy is defined as PLWHA being confident to follow treatment recommendations even when confronted with barriers, such as a busy work life, scheduling conflicts, and societal stigma. It has been shown that positive patient-HCP interactions are associated with heightened medication self-efficacy (Fuertes et al., 2007). Higher medication self-efficacy, may be associated with decreased perceived barriers to adherence and is proven to be associated with improved medical adherence (Langebeek et al., 2014). Finally, optimal adherence is associated with higher CD4 counts, which has consistently been substantiated in the literature (Lee et al., 2014).
Figure 1:
Hypothesized Model
Observed variables are shown within rectangles.
Note: Directional relationships are indicated with +/−.
Although the relationships among medication self-efficacy, adherence, and medication taking difficulties are well known, limited research describes the association of these variables with patient-HCP relationships. We used a Structural Equation Modeling (SEM) to test the hypothesis that these factors could explain the improved ART adherence and CD4 counts. And this study’s aim was to test these relationships.
METHODS
Sample, Settings, and Procedures
This study utilized a secondary data analysis approach and analyzed a pooled sample from two related, yet independent studies that focused primarily on self-management among local PLWHA. These projects stemmed from ongoing research partnerships among the same group of investigators across several universities, Taipei City Hospital-Kunming (TCH) and Shanghai Public Health Clinic Center (SPHCC). The survey component of the research involved Audio Computer-Assisted Self-Interview (ACASI) questionnaires given to 227 PLWHA who were receiving care at TCH and SPHCC.
The data were collected from April 2011 to November 2012 at TCH and November 2009 to March 2010 at SPHCC. TCH and SPHCC clinicians informed patients from outpatient clinics during their routine clinical visits about the studies and referred them to non-clinical research personnel who then explained the study, answered questions, and obtained signed written consent. The inclusion criteria included (a) diagnosed with HIV, (b) taking ART currently, and (c) at least 18 years old. Prospective participants who passed the inclusion criteria and agreed to voluntarily participate in the studies were then led to a separate room where they can anonymously answer the surveys on the ACASI system. All study procedures were reviewed and approved by the institutional review boards of the designated institutions.
Measures
In this study, several variables were chosen for statistical modeling, including demographics, recent CD4 counts, self-efficacy, patient-HCP relationship, adherence, and medication-taking difficulties. These instruments have been previously tested in Chinese populations and have shown strong reliability and validity (Holzemer et al., 2006; Shively, Smith, Bormann, & Gifford, 2002).
Demographics
Participants’ age, sex, education level, and residency were collected via self-report.
Patient- HCP Relationships
This is a 13-item scale designed to assess how individuals rate their interactions with their HCP (Bakken et al., 2000). Cronbach’s alpha reliability estimate was 0.96 in the U.S. based study (Bakken et al., 2000). A Chinese version of the scale has been tested and published (Chen et al., 2007). Each item is measured on a 4-point scale (1 = always true and 4 = never true). Lower scores indicate greater provider engagement. Cronbach’s alpha reliability estimate in this sample was 0.94.
HIV Self-efficacy (HIV-SE)
This scale is derived from the HIV-SE 34-item scale to measure self-efficacy for specific disease management behaviors in PLWHA. The adapted scale measures two conceptual domains: managing medication and managing symptoms. Each item describes a skill related to increasing degrees of confidence in management. A 9-point scale indicating how confident the respondent is of his/her ability to manage the disease is anchored by “not at all sure” at the low end and “totally sure” at the high end. Internal consistency reliabilities in previous studies ranged from 0.88 to 0.97 (Shively et al., 2002) and in this sample was 0.82 to 0.90.
Subjective Medication-taking Barriers
This nine-item survey measures reasons for missed medications. This came from the revised AIDS Clinical Trials Group that collected reasons for non-adherence to medications (Holzemer et al., 2006). Items are rated on a 4-point Likert scale from 0 = never to 3 = often (Holzemer et al., 2006). A higher score indicates a lower level of adherence to medication regimens. Cronbach’s alpha for these two subscales and the total scale ranged from 0.8 to 0.9 (Holzemer et al., 2006) and in this sample was 0.82 to 0.91.
Adherence
The participants were asked to do a 3-day and 30-day recall of any missed medication doses. These two visual analog scales were designed to collect data on 3-day and 30-day adherence of the study participants (Walsh, Mandalia, & Gazzard, 2002). The questions assess 3-day and 30-day ART adherence, reporting separately for each drug, along a continuum from “took all of my doses” to “missed all of my doses.” Results returned by this scale have been shown to correspond with those reported by other adherence measures such as electronic monitoring caps for measuring the number of times a pill bottle has been opened (Walsh et al., 2002).
CD4
The most recent CD4 counts to the data collected time were assessed by self-report. Because the distribution of the CD4 counts was positively skewed, Yeo-Johnson transformation was applied to transform the CD4 value to an approximately normal distribution.
Analysis
Descriptive and bivariate statistics were used to examine the distributions of selected factors and the relationships among patient-HCP relationship, self-efficacy, medication-taking difficulties, adherence, CD4, and background characteristics. For correlation analyses, we applied Pearson’s r and Point-Biserial correlations according to the nature of the distributions of the selected variables. Then we utilized SEM to test the proposed model. First, we built a measurement model to create a latent variable (adherence to medication schedule) with three observed adherence indicators. After we built the measurement model, we further tested the structural relationships among patient-HCP relationship, self-efficacy, medication-taking difficulties, adherence, and CD4 count. In both models, we applied several model-fit criteria to judge the overall fit of the model to the data. These criteria included Root Mean Square Error of Approximation (RMSEA) < .07, the 90% Confidence Interval of RMSEA, Comparative Fit Index (CFI) > .90, and Tucker-Lewis Index (TLI) > .90. To achieve a more parsimonious model, we further removed parameters that did not significantly differ from zero. These adjustments were made with assistance of formal testing (chi-square test) and modification indices in order to maintain the excellent fit between the model and data. We also adjusted the estimates by controlling key demographic backgrounds, including site, age, gender, and educational attainment. Then, we calculated the direct and indirect effects of these factors to investigate the relationships between patient-HCP relationship and CD4 through different pathways. Because this study drew upon samples from two different sites, we applied a cluster-robust Huber-White estimator to calculate the standard error for statistical inferences. All tests were conducted using Stata 13 statistical packages.
RESULTS
Descriptive and Bivariate Analysis
Demographic characteristics are presented in Table 1 with site comparison. Among the total sample of 227 PLWHA, 91% were male (n =207), with a mean age of 37 years (SD = 9.22; range = 18–72). Detail demographic data were and QOL subscale scores are all presented in Table 1.
Table 1:
Demographics
| Total Sample N = 227 M(SD) or N(%) | Taipei N = 120 M(SD) or N(%) | Shanghai N = 107 M(SD) or N(%) | |
|---|---|---|---|
| Age | 37.19 (9.22) | 36.85 (8.82) | 37.57 (9.69) |
| Gender** | |||
| Men | 207(91.15) | 117(97.48) | 90(84.11) |
| Education | |||
| >= HS | 183(80.53) | 100(83.20) | 83(77.57) |
| Income | |||
| Adequate | 151(66.37) | 84(69.75) | 67(62.62) |
| Patient-HCP relationships * | 3.11 (0.75) | 3.22 (0.72) | 2.98 (0.76) |
| Medication Self-Efficacy | 8.18 (1.53) | 8.29 (1.51) | 8.06 (1.56) |
| Medication Difficulties* | 1.87 (0.57) | 1.83 (0.55) | 1.93 (0.59) |
| Adherence 3 Day | 91.34 (14.92) | 91.97 (13.85) | 89.26 (17.88) |
| Adherence 30 Days | 90.33 (13.59) | 90.99 (16.89) | 88.17 (12.40) |
| CD4 Count** | 400 (270) | 559 (245) | 232 (181) |
Notes:
= p < 0.05;
= p < 0.01
M(SD)- Mean (Standard Deviation)
HS- High School
HCP- Healthcare Provider
Results of bivariate analyses are summarized in Table 2. The results suggest that research sites as well as selected demographic backgrounds are significantly correlated with patient-HCP relationships, medication self-efficacy, medication-taking difficulties, adherence indicators, and CD4. Being a male participant was correlated with younger age, marginally higher CD4 counts, greater patient-HCP relationships, and lower medication-taking difficulties. The detail correlations are presented in Table 2.
Table 2:
Bivariate Correlation among Variables
| SH§ | Men§ | Age | Edu | CD4 | P-HCPR | Med SE | Ad3d | Ad30d | RAd30d | |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Men | −.24** | |||||||||
| Age | .02 | −.17* | ||||||||
| Edu | −.18** | .05 | −.13† | |||||||
| CD4 | −.59** | .12† | −.04 | .22** | ||||||
| P-HCP R | −.13† | .21** | −.10 | −.01 | −.01 | |||||
| Med SE | −.07 | .03 | −.06 | .19** | .10 | .15* | ||||
| Ad3d | .03 | .09 | −.14* | .09 | .12† | .20** | .43** | |||
| Ad30d | .03 | .05 | −.15* | .06 | .13† | .20** | .46** | .81** | ||
| RAd30d | −.06 | .05 | .03 | .12† | .08 | .07 | .31** | .43** | .54** | |
| Diff | .68** | −.25** | .11 | −.13† | −.41** | −.20** | −.27** | −.19** | −.20** | −.22** |
Note: SH = Shanghai; Edu = Education levels; P-HCP R = Patient-Healthcare Provider Relationship; Med Self-Efficacy = Medical Self-Efficacy; Ad3d = Adherence in previous 3 days; Ad30d = Adherence in previous 30 days; RAd30d = Self-rated adherence levels in previous 30 days; and Diff = Subjective med-taking difficulties.
Pearson correlation was used except for SH and Men. Point-Biserial correlation was used for SH and Men.
= p < 0.1;
= p < 0.05;
= p < 0.01.
Structural Equation Modeling
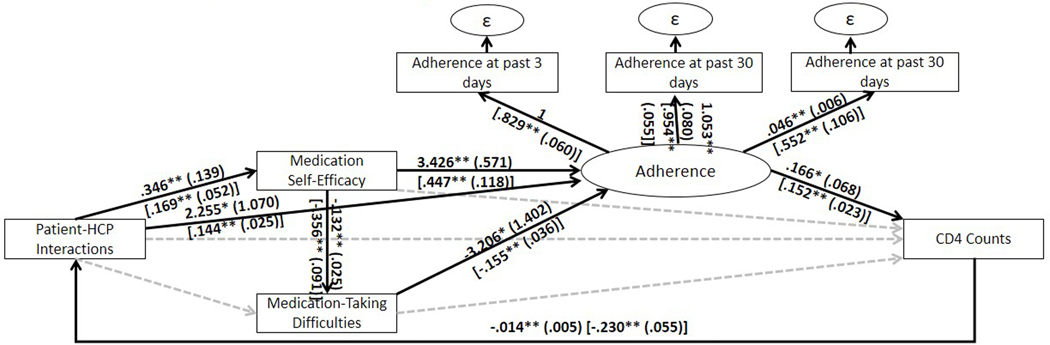
As measurement model only included three indicators, without additional constraints it was a saturated model and fit indices and Chi-Square test were not applicable. However, since all the standardized loadings were close to or greater than 0.6 and statistically significant, it was suggested that the underlying latent construct, adherence to medication, can largely explain the observed variables (Brown, 2015). It is acceptable to include a latent construct that is just-identified if the overall structural model is over-identified (Mora, Gelman, Steenkamp, & Raisinghani, 2012). Also, as shown by the fit indices that for the proposed model , RMSEA = 0.017 (90% CI: 0.001 – 0.063, P-Close = 0.852), CFI = 0.997 & TLI = 0.997, suggesting the proposed structural model fit well to the data. However, because the relationship between HCP-patient relationships and medication-taking difficulties was insignificant, we further suppressed this relationship to zero, which yielded slightly better AIC (proposed: 9021.571 vs. reduced: 9020.639) and BIC (proposed: 9175.495 vs. reduced: 9171.142) values while the likelihood ratio test showed insignificant result (). This suggested that the reduced model fit as well as the proposed model. The model fit indices for the reduced model were , RMSEA = 0.017 (90% CI: 0.001 – 0.062, P-Close = 0.860), CFI = 0.997 & TLI = 0.993. To achieve a more parsimonious model, therefore, we selected the reduced model to be our final model, as presented in Figure 2. Finally, the stability index equaled 0.259, suggesting that all the eigenvalues laid within the unit circle and the proposed model reached stable equilibrium.
Figure 2:
Final standardized parameter estimates model after modifications
Note: Error variance terms for measured variables are shown as ε. * p<0.5; ** p<0.01
A unit increase in HCP-patient relationship was associated with 0.346 unit increase in medication self-efficacy (SE = 0.108, p = 0.001), and 2.255 unit increase in medical adherence (SE = 0.185, p < 0.001). A unit increase in medical self-efficacy was associated with a 0.132 unit decrease in medication taking difficulties (SE = 0.031, p < 0.001) but a 3.246 unit increase in medical adherence (SE = 0.650, p < 0.001). A unit increase in medication taking difficulty was associated with 3.206 unit decrease in medical adherence (SE = 0.609, p < 0.001). A unit increase in medical adherence was associated with a 0.152 unit increase in transformed CD4 count (SE = 0.023, p < 0.001). Finally, a unit increase in transformed CD4 count was associated with 0.230 unit decrease in patient-HCP relationships (SE = 0.055, p < 0.001). The total effects considering different pathways in this non-recursive system were also significant at 0.05 level. Specifically, 1 unit increase in patient-HCP relationship was associated with 0.344 unit increase in medication self-efficacy (SE = 0.108, p = 0.001), 0.045 unit decrease in medication taking difficulty (SE = 0.014, p = 0.001), 1.30 unit increase in medical adherence (SE = 0.412, p = 0.002), and 0.590 unit increase in transformed CD4 count (SE = 0.099, p < 0.001).
The results of SEM model fitting were presented in Figure 2, in which standardized coefficients were reported in the brackets. In Figure 2, most of the hypothesized direct relationships were significant and supported by the data.
DISCUSSION
Our data and models are consistent with an explanation that patients’ positive relationships with HCP enhance medication self-efficacy, leading to better ART adherence and achievement of elevated CD4 counts. Given the self-efficacy and medication-taking difficulties for PLWHA, a focus on improving healthy patient-HCP relationships is warranted as a potential mechanism to better ART adherence and consequently, enhanced CD4 counts and stronger immune function (Johnson et al., 2006).
Our results echo previous studies that indicate a significant difference in patient engagement with HCPs, and specifically, studies showing that those who experience less engagement with their providers have lower medication self-efficacy (Tyer-Viola et al., 2014). Other studies have supported that better physician-patient collaboration is positively associated with better medication adherence (Arbuthnott & Sharpe, 2009). Also, more patient engagement with HCPs has been found to be important for retention in care (Schnall, Wantland, Velez, Cato, & Jia, 2014). Positive patient-HCP interactions can foster greater medication self-efficacy, which is associated with fewer medication-taking difficulties and better ART adherence (Kibicho & Owczarzak, 2011).
Interestingly, patient-HCP interaction did not directly influence medication-taking difficulties, and medication-taking difficulties did not significantly affect CD4 counts. Furthermore, patient-HCP interactions did not directly impact CD4 counts; rather, the relation was consistent with mediation (by either better medication self-efficacy or better adherence) or by improved adherence alone. This unanticipated finding demonstrates that medication-taking difficulties might not be the only mediating factor in CD4 count fluctuation. Rather, the influencing factor may be patient-HCP relationships (Tsuyuki & Surratt, 2015). Indeed, one study has described the need to enhance engagement in HIV care for HIV-infected populations by strengthening patient-HCP relationships to improve retention in HIV care and ART adherence for PLWHA (Tsuyuki & Surratt, 2015).
PLWHA face myriad difficulties, such as stigma, family pressure, potential for inadvertent disclosure to the public, and other challenges that could be addressed by cultivating closer patient-HCP relationships (Chen, Lee, et al., 2013). Studies on reasons for non-adherence have reported that some HIV-infected participants slept through dose times, could not follow medication instructions, and/or had inconsistent daily routines that negatively impacted ART adherence (Murphy, Roberts, Martin, Marelich, & Hoffman, 2000). These might be impacted by strengthening patient-HCP relationships so that providers can stress the importance of taking ART on time and can recommend strategies to remind patients to take their medication. Other studies have shown that patients and providers both feel that the patient’s responsibility and autonomy (self-efficacy) over their own healthcare is an important factor in ART adherence (Baranoski et al., 2014). Therefore, the question of how to reinforce the patient-HCP should be the key factor to achieving optimal ART adherence (Baranoski et al., 2014).
In our analysis, negative feedback has shown that PLWHA who have lower CD4 counts will need to strengthen their patient-HCP interaction. This might be because PLWHA who present with high CD4 counts already have good adherence and high self-efficacy, with fewer medication-taking difficulties, and are therefore less dependent on their HCP. One study reported a similar result, showing that good patient-HCP relationships led to better QOL, less severe and burdensome symptom experience, higher CD4 counts, and better ART adherence (Clucas et al., 2011).
Behavioral researchers can devise strategies to plan interventions that will enhance ART adherence. Our study suggests that a culturally sensitive, individually tailored self-management intervention with cognitive behavioral component can be an effective method to enhance patient-HCP relationships. Self-management intervention usually includes positive coping skills, relaxation, problem-solving, psycho-education and mental distress management, and cognitive-behavioral management skills (Grey, Knafl, & McCorkle, 2006). With family support, PLWHA can achieve higher adherence when family members remind them to take their pills on time, every day.
There are a number of important implications from this analysis. First, medication self-efficacy mediates the patient-HCP relationship and medication-taking difficulties. Also, medication-taking difficulties are consistent with mediation by medication self-efficacy and adherence. Second, decreasing medication-taking difficulties can enhance ART adherence and elevate CD4 count later on. A self-management intervention increases PLWHA’s self-efficacy through a combination of improved self-management skills and ART adherence. The intervention should include helping patients gain HIV-related knowledge and communicating efficiently with their HCP, friends and family. With these basic skills, PLWHA can improve their ability to reduce psychosocial barriers, such as fear of speaking up to providers, potential disclosure their serostatus and decrease self-stigma (Tsuyuki & Surratt, 2015).
Finally, patient-HCP relationships, medication self-efficacy and medication-taking barriers are key factors to achieving good ART adherence. Intervention focused on adherence and decrease in medication-taking difficulties should be considered. This paper has shown that PLWHA can have better self-efficacy to take care of themselves with guided practice, modeling and feedback provided from their HCP. Therefore, a self-management intervention can be delivered with the goal of improved QOL, and health outcomes.
Limitation
There are several limitations in this study. First, this is a cross-sectional study. Therefore, any associations among variables should not be taken to imply causality. Future longitudinal studies should be conducted to further causally test these relationships. Second, we recruited study participants from two major East Asian metropolitans with distinct healthcare systems. PLWHA in other locations might not share the same experiences and the findings might not be generalizable to all culturally Chinese PLWHA. Third, our participants were referred by clinicians and those who were dissatisfied with their HCP might choose not to participate. Fourth, our selection of measurement was limited by the available data. The measurements for adherence, for instance, may not be sufficiently sensitive because of their varied timeframes but were available in both datasets. Fifth, although this study harmonized two datasets to increase the sample size, the additional Monte Carlo studies revealed that this sample size did not have sufficient power for two parameters in our proposed model. Our sample size also prevented us from including additional latent variables to further handle potential measurement errors. Last, in this model, we focus on the physical variables; therefore, many possible mental health variables were not discussed. For example, depressive symptoms and perceived stigma might be also play important role on ART adherence.
CONCLUSION
In this paper, we examined the association among patient-HCP relationships, medication self-efficacy, medication-taking difficulties, ART adherence, and CD4 counts in PLWHA. The analysis is consistent with our model that medication self-efficacy and medication-taking difficulties mediators of patients’ ability to achieve maximum adherence, and to maintain high CD4 counts over time. Future interventions should be designed to enhance self-management and provide better patient-HCP communication. This improved communication will enhance medication self-efficacy and decrease medication-taking difficulties. This will improve medication adherence and immune function among PLWHA.
Acknowledgements
We gratefully acknowledge all the study participants, without them, it is not possible to complete these projects. This publication resulted (in part) from research supported by NINR under Award Numbers [K23NR14107; PI: Chen, Wei-Ti]. In addition, this research reported in this publication was supported by the University of Washington Center for AIDS Research (CFAR), an NIH funded program [30 AI027757; PI: Holmes, King], which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NCCAM) through an international pilot grant awarded to Dr. Wei-Ti Chen and by the University of Washington’s (UW) School of Nursing Research & Intramural Funding Program (RIFP). In addition, the research project was supported by DOH101-DC-1004 from the Taiwan Centers for Disease Prevention and Control (PI: Chuang, Peing). The contents of this article are solely the views of the authors and do notrepresent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest Statement
No conflict of interest has been declared by the authors.
References
- Arbuthnott A, & Sharpe D.(2009). The effect of physician-patient collaboration on patient adherence in non-psychiatric medicine. Patient Educ Couns, 77(1), 60–67. doi: 10.1016/j.pec.2009.03.022 [DOI] [PubMed] [Google Scholar]
- Bakken S, Holzemer WL, Brown MA, Powell-Cope GM, Turner JG, Inouye J, . . . Corless IB (2000). Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS, 14(4), 189–197. [DOI] [PubMed] [Google Scholar]
- Bankoff SM, McCullough MB, & Pantalone DW (2013). Patient-provider relationship predicts mental and physical health indicators for HIV-positive men who have sex with men. J Health Psychol, 18(6), 762–772. doi: 10.1177/1359105313475896 [DOI] [PubMed] [Google Scholar]
- Baranoski AS, Meuser E, Hardy H, Closson EF, Mimiaga MJ, Safren SA, . . . Kumar VS (2014). Patient and provider perspectives on cellular phone-based technology to improve HIV treatment adherence. AIDS Care, 26(1), 26–32. doi: 10.1080/09540121.2013.802282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Timothy A. (2015). Confirmatory factor analysis for applied research. New York, London: The Guilford Press. [Google Scholar]
- Chen WT, Lee SY, Shiu CS, Simoni JM, Pan C, Bao M, & Lu H.(2013). Fatigue and sleep disturbance in HIV-positive women: a qualitative and biomedical approach. J Clin Nurs, 22(9–10), 1262–1269. doi: 10.1111/jocn.12012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Starks H, Shiu CS, Fredriksen-Goldsen K, Simoni J, Zhang F, . . . Zhao H.(2007). Chinese HIV-positive patients and their healthcare providers: contrasting Confucian versus Western notions of secrecy and support. ANS Adv Nurs Sci, 30(4), 329–342. doi: 10.1097/01.ANS.0000300182.48854.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Wantland D, Reid P, Corless IB, Eller LS, Iipinge S, . . . Webel AR (2013). Engagement with Health Care Providers Affects Self- Efficacy, Self-Esteem, Medication Adherence and Quality of Life in People Living with HIV. J AIDS Clin Res, 4(11), 256. doi: 10.4172/2155-6113.1000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clucas C, Harding R, Lampe FC, Anderson J, Date HL, Johnson M, . . . Sherr L.(2011). Doctor-patient concordance during HIV treatment switching decision-making. HIV Med, 12(2), 87–96. doi: 10.1111/j.1468-1293.2010.00851.x [DOI] [PubMed] [Google Scholar]
- Fuertes JN, Mislowack A, Bennett J, Paul L, Gilbert TC, Fontan G, & Boylan LS (2007). The physician-patient working alliance. Patient Educ Couns, 66(1), 29–36. [DOI] [PubMed] [Google Scholar]
- Grey M, Knafl K, & McCorkle R.(2006). A framework for the study of self- and family management of chronic conditions. Nurs Outlook, 54(5), 278–286. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Bakken S, Portillo CJ, Grimes R, Welch J, Wantland D, & Mullan JT (2006). Testing a nurse-tailored HIV medication adherence intervention. Nurs Res, 55(3), 189–197. [DOI] [PubMed] [Google Scholar]
- Huang L, Li L, Zhang Y, Li H, Li X, & Wang H.(2013). Self-efficacy, medication adherence, and quality of life among people living with HIV in Hunan Province of China: a questionnaire survey. J Assoc Nurses AIDS Care, 24(2), 145–153. doi: 10.1016/j.jana.2012.04.006 [DOI] [PubMed] [Google Scholar]
- Johnson MO, Chesney MA, Goldstein RB, Remien RH, Catz S, Gore-Felton C, . . . Team, Nimh Healthy Living Project. (2006). Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care STDS, 20(4), 258–268. doi: 10.1089/apc.2006.20.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D, Cook R, Cecchini D, Sued O, Bofill L, Weiss S, . . . Spence A.(2015). Examining Adherence Among Challenging Patients in Public and Private HIV Care in Argentina. AIDS Behav, 19(9), 1619–1629. doi: 10.1007/s10461-015-1037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly E, Ivers N, Zawi R, Barnieh L, Manns B, Lorenzetti DL, . . . McBrien KA (2015). Patient navigators for people with chronic disease: protocol for a systematic review and meta-analysis. Syst Rev, 4, 28. doi: 10.1186/s13643-015-0019-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibicho J, & Owczarzak J.(2011). Pharmacists’ strategies for promoting medication adherence among patients with HIV. J Am Pharm Assoc (2003), 51(6), 746–755. doi: 10.1331/JAPhA.2011.10190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdottir TB, Richter C, . . . Nieuwkerk PT (2014). Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med, 12, 142. doi: 10.1186/PREACCEPT-1453408941291432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee L, Rand CS, Ellen JM, & Agwu AL (2014). Factors Informing HIV Providers’ Decisions to Start Antiretroviral Therapy for Young People Living With Behaviorally Acquired HIV. J Adolesc Health, 55(3), 358–365. doi: 10.1016/j.jadohealth.2014.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead N, Bower P, & Hann M.(2002). The impact of general practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc Sci Med, 55(2), 283–299. [DOI] [PubMed] [Google Scholar]
- Mora Manuel, Gelman Ovsei, Steenkamp Annette L., & Raisinghani Mahesh. (2012). Research Methodologies, Innovations and Philosophies in Software Systems Engineering and Information Systems. Hershey, PA: IGI Global. [Google Scholar]
- Murphy DA, Roberts KJ, Martin DJ, Marelich W, & Hoffman D.(2000). Barriers to antiretroviral adherence among HIV-infected adults. AIDS Patient Care STDS, 14(1), 47–58. doi: 10.1089/108729100318127 [DOI] [PubMed] [Google Scholar]
- Oetzel J, Wilcox B, Avila M, Hill R, Archiopoli A, & Ginossar T.(2015). Patient-provider interaction, patient satisfaction, and health outcomes: testing explanatory models for people living with HIV/AIDS. AIDS Care, 27(8), 972–978. doi: 10.1080/09540121.2015.1015478 [DOI] [PubMed] [Google Scholar]
- Rao D, Chen WT, Pearson CR, Simoni JM, Fredriksen-Goldsen K, Nelson K, . . . Zhang F.(2012). Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS, 23(7), 481–484. doi: 10.1258/ijsa.2009.009428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall R, Wantland D, Velez O, Cato K, & Jia H.(2014). Feasibility testing of a web-based symptom self-management system for persons living with HIV. J Assoc Nurses AIDS Care, 25(4), 364–371. doi: 10.1016/j.jana.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shively MJ, Smith TLJE, & Gifford AL (2002). Evaluating self-efficacy for HIV disease menagement skills. AIDS Behav, 6(4), 371–379. [Google Scholar]
- Street E, Curtis H, Sabin CA, Monteiro EF, & Johnson MA (2009). British HIV Association (BHIVA) national cohort outcomes audit of patients commencing antiretrovirals from naive. HIV Med, 10(6), 337–342. doi:HIV692 [pii] 10.1111/j.1468-1293.2009.00692.x [DOI] [PubMed] [Google Scholar]
- Tsuyuki K, & Surratt HL (2015). Antiretroviral drug diversion links social vulnerability to poor medication adherence in substance abusing populations. AIDS Behav, 19(5), 869–881. doi: 10.1007/s10461-014-0969-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyer-Viola LA, Corless IB, Webel A, Reid P, Sullivan KM, Nichols P, & International Nursing Network for, H. I. V. Aids Research. (2014). Predictors of medication adherence among HIV-positive women in North America. J Obstet Gynecol Neonatal Nurs, 43(2), 168–178. doi: 10.1111/1552-6909.12288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh JC, Mandalia S, & Gazzard BG (2002). Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. Aids, 16(2), 269–277. [DOI] [PubMed] [Google Scholar]