Abstract
AIM
To evaluate the effectiveness of peripheral defocus spectacle lenses (PDLs) in myopia control.
METHODS
Literature retrieval on PubMed, Cochrane Library, Embase, and Web of Science databases, and the search time limit was from the establishment of each database to December 29, 2021 were conducted. Change of spherical equivalent refraction (SER) and axial change (AL) were extracted from the literatures that met the inclusion criteria, and RevMan5.3 software was used for Meta-analysis.
RESULTS
A total of 4 randomized controlled trials (RCTs) were included in this Meta-analysis, involving 770 myopic children. The results showed that PDLs could delay the progression of myopia in children with myopia compared with single vision spectacle lenses (SVLs; WMD=0.21 D, 95%CI: 0.01, 0.41, P=0.04). However, there was no significant difference in controlling the growth of axial length (AL) in myopic children (WMD=-0.10 mm, 95%CI: -0.21, 0.01, P=0.07). The results of the effectiveness of myopia control between the two spectacle lenses showed that PDLs were more effective in controlling the progression of myopia (OR=5.73, 95%CI: 2.58, 12.70, P<0.001) and delaying the growth of AL (OR=44.25, 95%CI: 8.84, 221.58, P<0.001) than SVLs, and the differences were statistically significant.
CONCLUSION
PDLs can control the progression of myopia compared with SVLs, but cannot delay the growth of AL, and the effectiveness of PDLs in myopia control better than SVLs.
Keywords: Meta-analysis, peripheral defocus spectacle lenses, hyperopia defocus, myopia defocus, myopia control
INTRODUCTION
Myopia is one of the common eye diseases, and it has become the sixth leading cause of global blindness. It is a pandemic that has not been controlled by the World Health Organization so far[1]–[2]. Globally, the prevalence of myopia (diopter ≤ -0.50D) and high myopia (diopter ≤ -5.00 D) are 28.3% and 4.0%, respectively. It is projected that by 2050, the prevalence of myopia and high myopia will increase to 50% (5 billion people) and 10% (1 billion people)[3]–[4]. Myopia mainly occurs in childhood, and myopia that occurs in childhood will progress rapidly, and it will not gradually slow down until adulthood. Early childhood myopia is closely related to high myopia in adulthood. Therefore, it is very important for children to detect myopia early and take measures to control the progression of myopia[5].
Animal experiments (primates, guinea pigs, mice, chickens, etc.) have shown that putting a negative lens in front of the eyes and applying retinal peripheral hyperopia defocus can induce experimental myopia[6]. Based on these animal studies, it has been shown that the retinal peripheral hyperopia defocus is closely correlated with the progression of myopia, and the progression of myopia can be delayed by inducing retinal peripheral myopia defocus[7]–[8]. Based on this principle, several optical treatment methods have emerged, such as orthokeratology, multifocal contact lenses, and peripheral defocus spectacle lenses (PDLs). These methods can induce retinal peripheral myopia defocus (or reduce retinal peripheral hyperopia defocus) to achieve the effect of myopia control[9].
Meta-analysis and systematic reviews have been conducted on the myopia control effectiveness of orthokeratology[10]–[14] and multifocal contact lenses[15]. However, Meta-analysis and systematic reviews of PDLs have not been reported. Therefore, we will perform a Meta-analysis and systematic review of the effectiveness of PDLs in myopia control.
MATERIALS AND METHODS
Retrieval Strategy
Literatures from PubMed, Cochrane Library, Embase, and Web of Science databases were retrieved until December 29, 2021. Retrieval terms included: ‘peripheral defocus’, ‘myopia defocus’, ‘hyperopia defocus’, ‘myopia’, ‘spectacles’ and their synonyms.
Inclusion and Exclusion Criteria
Inclusion criteria
PICOS rules: 1) Patient: children with myopia; 2) Intervention: using PDLs to control myopia; 3) Comparison: using single vision spectacle lenses (SVLs) to control myopia; 4) Outcome: changes of spherical equivalent refraction (SER) and axial length (AL); 5) Study design: randomized controlled trail (RCT).
Exclusion criteria
1) Reviews; 2) Animal researches; 3) Repeated inclusion.
Literatures Selection and Data Extraction
Two investigators independently screened the literatures according to the inclusion and exclusion criteria, and discussed or decided by the third investigator in case of disagreement. Information such as the first author, publication time, country, study type, patient age, follow-up time, type of spectacle lenses and other information were extracted.
Quality Assessment
The quality of literatures was evaluated by the Cochrane risk of bias tool. Selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases were evaluated.
Statistical Analysis
RevMan5.3 software was used for Meta-analysis. Effect model was selected according to the heterogeneity. I2<50% was regarded as low heterogeneity, and the fixed-effect model was adopted. On the contrary, I2>50% was high heterogeneity, the random-effect model was used. The effect size of continuous variables used weighted mean difference (WMD) and its 95% credibility interval (CI), and binary variables used odds ratio (OR) and its 95%CI. When the heterogeneity was large than 50%, sensitivity analysis and subgroup analysis were performed. Funnel plot and Egger test were used to check publication bias. The difference was considered statistically significant if P<0.05.
RESULTS
Literatures Selection
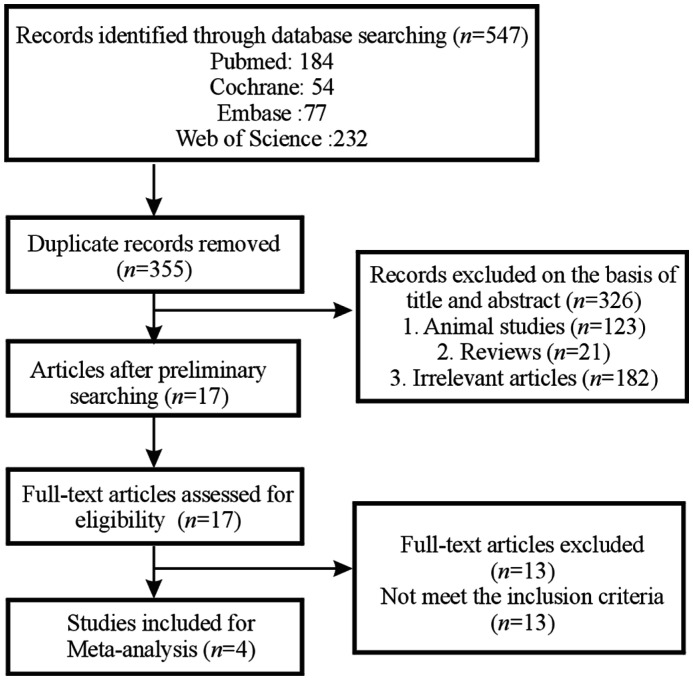
Figure 1 showed the literatures selection process of this study. A total of 547 articles were retrieved in the study. After excluding duplicate articles, the remaining 355 articles were selected on the basis of titles and abstracts, and 17 articles were evaluated in full-text. Finally, 4 articles were included in this Meta-analysis[16]–[19].
Figure 1. Flow chart of literatures selection.
Characteristics of Included Studies
Table 1 showed the basic characteristics of the 4 studies included in this Meta-analysis. All the 4 studies were RCT. A total of 770 children were included, with an average age of 6-16y, myopia -0.75 D to -5.00 D, and astigmatism ≤1.50 DC. Three of the studies were conducted in Hong Kong, China, Zhongshan, China, Wenzhou, China, and one study was conducted in Japan. All the experimental groups of these studies used PDLs to control myopia, and the control group used SVLs to control myopia. And all studies were followed up for more than 12mo.
Table 1. Characteristics of included studies.
| Study | Country | Published year | Study type | Follow-up (mo) | Completed/all sample size (%) | Age, y | Experimental group (n) | Control group (n) |
| Sankaridurg et al[16] | Zhongshan, China | 2010 | RCT | 12 | 201/210 (95.71) | 6-16 | MyoVision: Type I (50), Type II (60), Type III (50) | SVLs (50) |
| Kanda et al[17] | Japan | 2018 | RCT | 6, 12, 18, 24 | 203/207 (98.07) | 6-12 | MyoVision: Type III (102) | SVLs (105) |
| Bao et al[18] | Wenzhou, China | 2020 | RCT | 6, 12 | 161/170 (94.71) | 8-13 | HAL (58), SAL (57) | SVLs (55) |
| Lam et al[19] | Hong Kong, China | 2020 | RCT | 6, 12, 18, 24 | 160/183 (87.43) | 8-13 | DIMS (93) | SVLs (90) |
RCT: Randomized controlled trial; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; DIMS: Defocus incorporated multiple segments; SVLs: Single vision spectacle lenses.
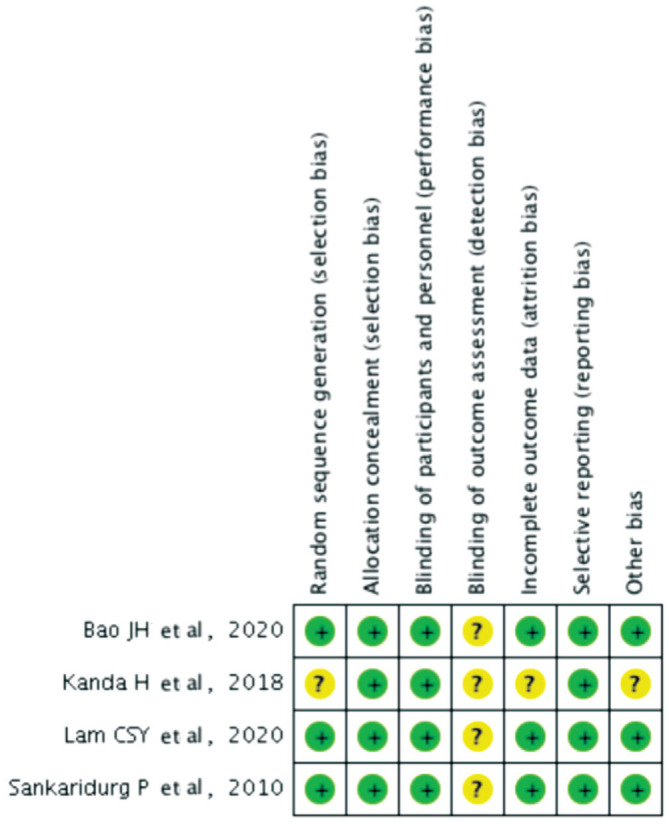
Risk of Bias Assessment
Figure 2 showed the results of the risk of bias assessment of the included studies. Three studies pointed out the specific method of randomization, while the other 1 study only mentioned randomization without mentioning the specific methods. All studies report on allocation concealment and blinding. Four studies clearly reported the number of people who were lost to follow-up or dropped out, but one study did not report the specific reasons for loss to follow-up or dropped out.
Figure 2. Risk of bias assessment.
Change in Spherical Equivalent Refraction
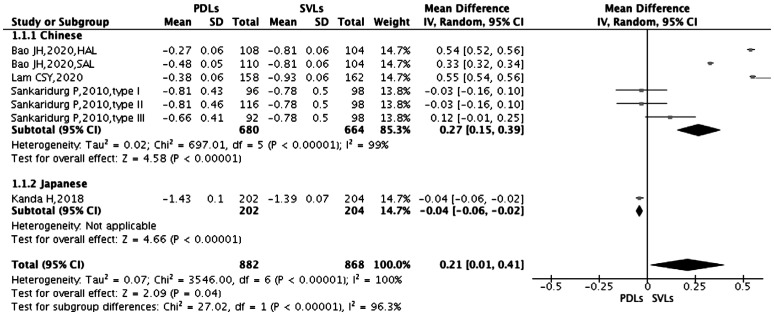
Bao et al[18] used two different types of PDLs in their study (HAL and SAL), and Sankaridurg et al[16] used three different types of PDLs in their study (type I, type II, type III), and the specific data of each subgroup were shown in the two studies. Therefore, they were regarded as independent studies for Meta-analysis. Heterogeneity test showed high heterogeneity (χ2=3546.00, P<0.001, I2=100%), so the random-effect model was used. Figure 3 showed that PDLs can delay the progression of myopia in myopic children compared with SVLs, and the difference was statistically significant (WMD=0.21 D, 95%CI: 0.01, 0.41, P=0.04). Due to the high heterogeneity, sensitivity analysis was performed by eliminating each study one by one, and the results showed that the results of this Meta-analysis were relatively stable (Table 2). In addition, a subgroup analysis according to study region showed that PDLs could delay the progression of myopia in Chinese myopic children compared with SVLs, and the difference was statistically significant (WMD=0.27 D, 95%CI: 0.15, 0.39, P<0.001). However, in Japanese myopic children, PDLs could not delay the progression of myopia compared with SVLs, and the difference was statistically significant (WMD=-0.04 D, 95%CI: -0.06, -0.02, P<0.001; Figure 3).
Figure 3. Forest plot of the change in SER.
PDLs: Peripheral defocus spectacle lenses; SVLs: Single vision spectacle lenses; SER: Spherical equivalent refraction; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; CI: Confidence interval.
Table 2. Sensitivity analysis of the change in SER.
| Eliminate research | I 2 | WMD | 95%CI | P |
| Bao et al, 2020 (HAL) | 100 | 0.15 | -0.08, 0.39 | 0.20 |
| Bao et al, 2020 (SAL) | 100 | 0.19 | -0.07, 0.45 | 0.16 |
| Kanda et al, 2018 | 100 | 0.27 | 0.15, 0.39 | <0.001 |
| Lam et al, 2020 | 100 | 0.15 | -0.08, 0.38 | 0.19 |
| Sankaridurg et al, 2010 (Type I) | 100 | 0.25 | 0.04, 0.46 | 0.02 |
| Sankaridurg et al, 2010 (Type II) | 100 | 0.25 | 0.04, 0.46 | 0.02 |
| Sankaridurg et al, 2010 (Type III) | 100 | 0.23 | 0.01, 0.44 | 0.04 |
| All studies | 100 | 0.21 | 0.01, 0.41 | 0.04 |
SER: Spherical equivalent refraction; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; WMD: Weighted mean difference; CI: Confidence interval.
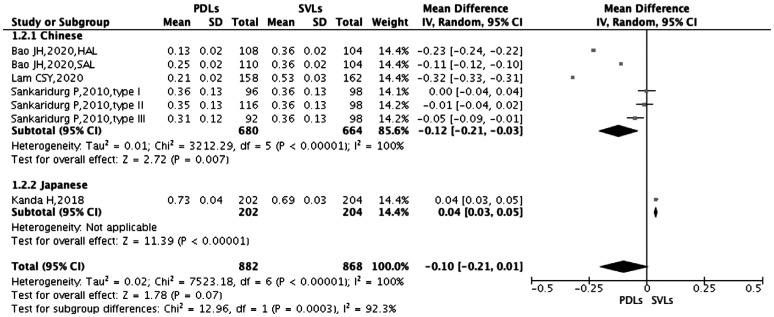
Change in Axial Length
The heterogeneity test showed high heterogeneity (χ2=7523.18, P<0.001, I2=100%), so the random-effect model was selected. Figure 4 shows that there was no significant difference between PDLs and SVLs in controlling the growth of AL in myopic children (WMD=-0.10 mm, 95%CI: -0.21, 0.01, P=0.07). Sensitivity analysis showed that the results of this Meta-analysis were relatively stable (Table 3). The results of subgroup analysis showed that PDLs could delay the growth of AL in Chinese myopic children compared with SVLs, and the difference was statistically significant (WMD=-0.12 mm, 95%CI: -0.21, -0.03, P=0.007); but in Japanese myopic children, PDLs could not slow down the growth of AL in myopic children compared with SVLs, the difference was statistically significant (WMD=0.04 mm, 95%CI: 0.03, 0.05, P<0.001).
Figure 4. Forest plot of the change in AL.
PDLs: Peripheral defocus spectacle lenses; SVLs: Single vision spectacle lenses; AL: Axial Length; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; CI: Confidence interval.
Table 3. Sensitivity analysis of the change in AL.
| Eliminate research | I 2 | WMD | 95%CI | P |
| Bao et al, 2020 (HAL) | 100 | -0.08 | -0.21, 0.06 | 0.28 |
| Bao et al, 2020 (SAL) | 100 | -0.10 | -0.23, 0.04 | 0.17 |
| Kanda et al, 2018 | 100 | -0.12 | -0.21, 0.03 | 0.007 |
| Lam et al, 2020 | 100 | -0.06 | -0.16, 0.04 | 0.24 |
| Sankaridurg et al, 2010 (Type I) | 100 | -0.11 | -0.23, 0.00 | 0.05 |
| Sankaridurg et al, 2010 (Type II) | 100 | -0.11 | -0.23, 0.00 | 0.06 |
| Sankaridurg et al, 2010 (Type III) | 100 | -0.11 | -0.22, 0.01 | 0.07 |
| All studies | 100 | -0.1 | -0.21, 0.01 | 0.07 |
AL: Axial Length; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; WMD: Weighted mean difference; CI: Confidence interval.
Subgroup Analysis
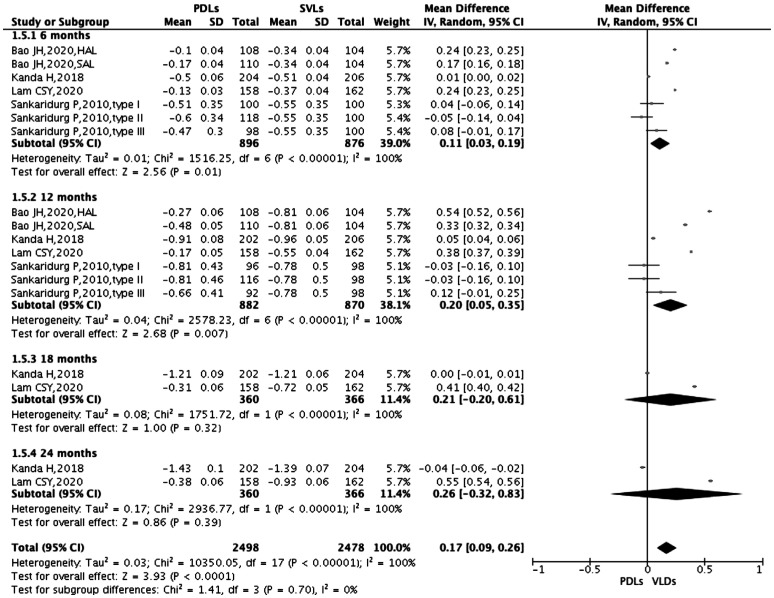
Subgroup analysis in spherical equivalent refraction
All studies reported changes of SER during different follow-up periods, so Meta-analysis was conducted according to follow-up periods. Figure 5 showed the results of subgroup analysis. The results showed that in the 6-month follow-up period, PDLs could delay the progression of myopia in myopic children compared with SVLs, and the difference was statistically significant (WMD=0.11 D, 95%CI: 0.03, 0.19, P=0.01); in the 12-month follow-up period, PDLs could delay the progression of myopia in myopic children compared with SVLs, and the difference was statistically significant (WMD=0.20 D, 95%CI: 0.05, 0.35, P=0.007); however, no difference was found between the two groups in delaying the progression of myopia in myopic children at 18-month and 24-month follow-up period (both P>0.05). At the same time, the overall data showed that PDLs could delay the progression of myopia in myopic children compared with SVLs, and the difference was statistically significant (WMD=0.17 D, 95%CI: 0.09, 0.26, P<0.001).
Figure 5. Forest plot for subgroup analysis of the change in SER.
PDLs: Peripheral defocus spectacle lenses; SVLs: Single vision spectacle lenses; SER: Spherical equivalent refraction; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; CI: Confidence interval.
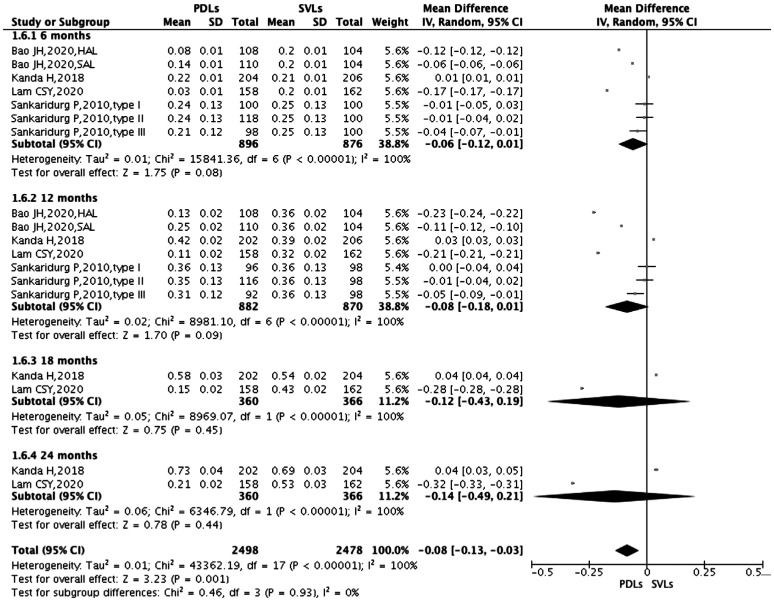
Subgroup analysis in axial length
Figure 6 showed a subgroup analysis of changes of AL at 6, 12, 18, and 24mo of follow-up. There was no significant difference between the two groups in controlling the growth of AL in myopic children (all P>0.05). However, the overall data showed that PDLs could control the growth of AL in myopic children compared with SVLs, and the difference was statistically significant (WMD=-0.08 mm, 95%CI: -0.13, -0.03, P=0.001).
Figure 6. Forest plot for subgroup analysis of the change in AL.
PDLs: Peripheral defocus spectacle lenses; SVLs: Single vision spectacle lenses; AL: Axial length; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; CI: Confidence interval.
Subgroup analysis of change in SER and AL in Chinese or all population
When performing sensitivity analysis, we found that the statistical results were reversed after excluding the study by Kanda et al[17]. Therefore, we further analyzed the differences of SER and AL between the Chinese and the Japanese. Table 4 showed that Chinese myopic children in the follow-up period of 6, 12, 18, and 24mo all P<0.05. The results showed that PDLs could delay the progression of myopia and the growth of AL in Chinese myopic children compared with SVLs.
Table 4. Subgroup analysis of change in SER and AL in Chinese or all population.
| Follow-up period | SER |
AL |
||||
| WMD | 95%CI | P | WMD | 95%CI | P | |
| 6mo | ||||||
| Chinese | 0.15 | 0.11, 0.20 | <0.001 | -0.07 | -0.12, -0.02 | 0.003 |
| All | 0.11 | 0.03, 0.19 | 0.01 | -0.06 | -0.12, 0.01 | 0.08 |
| 12mo | ||||||
| Chinese | 0.25 | 0.16, 0.34 | <0.001 | -0.10 | -0.16, -0.05 | <0.001 |
| All | 0.20 | 0.05, 0.35 | 0.007 | -0.08 | -0.18, 0.01 | 0.09 |
| 18mo | ||||||
| Chinese | 0.41 | 0.40, 0.42 | <0.001 | -0.28 | -0.28, -0.28 | <0.001 |
| All | 0.21 | -0.20, 0.61 | 0.32 | -0.12 | -0.43, 0.19 | 0.45 |
| 24mo | ||||||
| Chinese | 0.55 | 0.54, 0.56 | <0.001 | -0.32 | -0.33, -0.31 | <0.001 |
| All | 0.26 | -0.32, 0.83 | 0.39 | -0.14 | -0.49, 0.21 | 0.44 |
SER: Spherical equivalent refraction; AL: Axial length; WMD: Weighted mean difference; CI: Confidence interval.
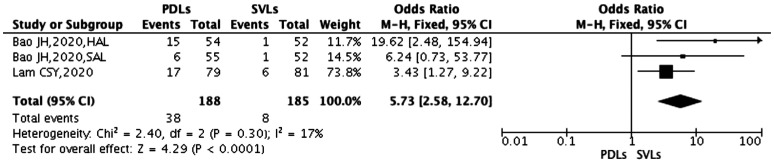
Effectiveness of Myopia Control
Effectiveness of myopia control of change in spherical equivalent refraction
There were 2 studies (3 subgroups) at the end of follow-up that counted the effectiveness of two spectacle lenses for myopia control (including non-progressive and decreased of myopia). The heterogeneity test showed low heterogeneity (χ2=2.40, P=0.30, I2=17%), so the fixed-effect model was selected. Figure 7 showed that compared with SVLs, effectiveness of myopia control of PDLs was better, and the difference was statistically significant (OR=5.73, 95%CI: 2.58, 12.70, P<0.001).
Figure 7. Effectiveness of myopia control of change in SER.
PDLs: Peripheral-defocus spectacle lenses; SVLs: Single-vision spectacle lenses; SER: Spherical equivalent refraction; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; OR: Odds ratio; CI: Confidence interval.
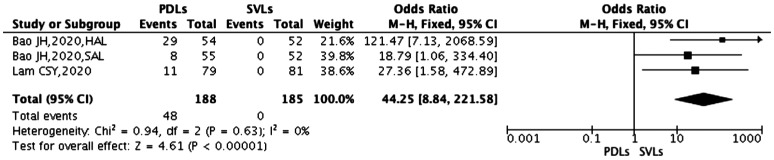
Effectiveness of myopia control of change in axial length
There were 2 studies (3 subgroups) at the end of follow-up that counted the effectiveness of two spectacle lenses for myopia control (including unexpanded and shortened of AL). The heterogeneity test showed low heterogeneity (χ2=0.94, P=0.63, I2=0), so the fixed-effect model was selected. Figure 8 showed that compared with SVLs, effectiveness of myopia control of PDLs was better, and the difference was statistically significant (OR=44.25, 95%CI: 8.84, 221.58, P<0.001).
Figure 8. Effectiveness of myopia control of change in AL.
PDLs: Peripheral-defocus spectacle lenses; SVLs: Single-vision spectacle lenses; AL: Axial length; HAL: Highly aspherical lenslets; SAL: Slightly aspherical lenslets; OR: Odds ratio; CI: Confidence interval.
Adverse Events
Study by Sankaridurg et al[16] reported two cases of children wearing type II spectacle lenses who fell due to running during the first week of wearing the spectacle lenses, and no adverse events were reported in the other three studies.
Publication Bias
Because only 4 studies were included, Funnel plot and Egger's test were not used to examine publication bias.
DISCUSSION
Myopia is the most common type of ametropia, and the prevalence of myopia is on an uptrend worldwide, and in some Asian regions the prevalence is up to 70%-80%. Some studies have shown that the prevalence of high myopia is growing faster than the overall prevalence of myopia. At the same time, the incidence of complications that irreversible blinding associated with high myopia is also on the rise[20]–[21]. Pathological changes, for instance, retinal detachment, choroidal neovascularization, macular atrophy appear in the fundus of high myopia, it is called “pathological myopia”. Pathological myopia results in visual impairment or blindness in 0.2%-1.5% of Asians. Pathological myopia is now among the main reasons of irreversible blindness in China and Japan in Asia[22]. Studies have shown that the incidence of retinal detachment and macular degeneration increases logarithmically when myopia is above -2.00 D. Researchers have shown that when myopia is between -3.00 D and -1.00 D, the incidence of macular degeneration will decrease by 4 times and the incidence of retinal detachment will decrease by 3 times[23].
Myopia is known to progress most rapidly in children ages 8 to 15 (Caucasian X=0.6 diopter/y, Asian X=0.7 diopter/y) and then starts to mitigation with age. Therefore, for children, early detection of myopia and take measures to control the progress of myopia is very important. At present, the goal of myopia control is to control the progression of myopia and delay the growth of AL, so as to decrease the prevalence of high myopia and pathological myopia[4],[23]–[24]. Accordingly, to control the development of myopia to high myopia, and then to pathological myopia, taking positively measures to prevent is significant.
Optical defocus is caused by the inconsistency between the image and the retinal horizon. Hyperopia defocus is induced when the image is located behind the retinal horizon, myopic defocus is induced when the image is located in front of the retinal horizon. Studies have suggested that hyperopia defocus is one of the potential causes for the occurrence and development of myopia[25]. Based on this theory, some researchers believe that specially designed lenses that can induce retinal peripheral myopia defocus (or reduce retinal peripheral hyperopia defocus) can be used to control myopia. The myopia control effect of orthokeratology has been confirmed. Orthokeratology reversibly reshapes the corneal shape and induces retinal peripheral myopia defocus, which is considered to be one of the mechanisms of orthokeratology to control the progression of myopia[24],[26]. Although orthokeratology has a certain control effect on myopia, it is difficult to use in young children, and improper operation and inadequate cleaning can cause corneal infection. In addition, the recovery of corneal shape during the daytime will affect children's vision[27]. Some studies[28]–[29] have also confirmed the effect of myopia control of contact lenses design to reduce peripheral hyperopia defocus, but inadequate cleaning of contact lenses may induce chronic inflammation and acute inflammation, thus affecting the normal physiological of the cornea[30].
SVLs are the most commonly used initial treatment for myopic children. Although SVLs can provide clear vision with almost no potential side effects, they cannot control the progression of myopia and the growth of AL[31]–[32]. Based on the theory of optical defocus, spectacle lenses that induce retinal peripheral myopia defocus (or reduce retinal peripheral hyperopia defocus) have developed, but different studies have come to different conclusions. Therefore, we performed a Meta-analysis and systematic review of the myopia control effectiveness of PDLs.
A total of 4 RCTs (7 subgroups) were included in this study. The results of Meta-analysis showed that the effectiveness of PDLs on myopia control was inconsistent between Chinese and Japanese subjects (both interaction P<0.001). In other words, PDLs can delay the progression of myopia and the growth of AL in Chinese myopic children compared with SVLs, but no effect was observed in Japanese myopic children. Because the 4 RCTs all reported changes of SER and AL at different follow-up periods, subgroup analysis was performed according to follow-up period, and the results showed: During the follow-up period of 6mo and 12mo, the PDLs could delay the progression of myopia in myopic children compared with SVLs (both P<0.05). However, during the follow-up period of 18 and 24mo, no difference was found between the two spectacle lenses in delaying the progression of myopia in myopic children (both P>0.05). During the follow-up period of 6, 12, 18, and 24mo, no difference was found between the spectacle lenses in controlling the growth of AL in myopic children (all P>0.05). Furthermore, we also performed a Meta-analysis on the effectiveness of myopia control, and the results showed that PDLs was better than SVLs in myopia control (P<0.001).
There were also some limitations in our study. In the first place, due to the limited number of studies, only 4 RCTs finally met the purpose of this study, and each study has a small number of subjects, which may affect the stability of the results. Second, the study population was small, only one of the 4 studies was conducted in Japan, the other three were conducted in China, and the population of the 4 studies were all Asians, in order to make the results more convincing, more large-scale, multicenter, randomized controlled trials are needed in the future. When we conducted literature retrieval, we found that multiple studies on PDLs for myopia control have been registered, and we believed that more data will be added in the next few years. Third, increasing outdoor activity time has been used as a preventive measure to control myopia[33], but none of the 4 researches included in this study considered the effect of outdoor activity time on myopia control, its influence on myopia control cannot be ruled out. Therefore, future research should exclude the effect of outdoor activity time on myopia control. Finally, 4 studies involving 6 different designs of frames, the studies by Bao et al[18] and Lam et al[19] had similar spectacle lenses designs, the central optical zone was used to correct distance vision, and the periphery of the central optical zone was a concentric circle formed by a plurality of continuous small-diameter lens lets, which were used to induce retinal peripheral myopia defocus. The studies by Sankaridurg et al[16] and Kanda et al[17] included three different designs of spectacles. Types I and II are similar in design, both were rotationally symmetrical designs, and the central optical zone was used to correct distance vision. A progressively sloping zone of progressively increasing positive power surrounded the central optic zone to reduce peripheral hyperopia defocus. Type III was an optimized asymmetric design that reduced astigmatism in the horizontal meridian, including the central optic zone and the peripheral positive additional peripheral power. Although there were some differences in spectacle lenses designs, the basic principle was to induce retinal peripheral myopia defocus (or reduce retinal peripheral hyperopia defocus). Differences in lenses design may affect results.
In conclusion, the results of this study showed that PDLs compared with SVLs can control the progression of myopia, but cannot delay the growth of AL. And the effectiveness of PDLs in myopia control better than SVLs.
Acknowledgments
Foundations: Supported by National Natural Science Foundation of China (No.81960177); Jiangxi Provincial Science and Technology Grant (No.20192BAB205049); A research grant from Jiangxi Provincial Health Commission (No.202210723); Postgraduate Innovation Special Fund Project of Jiangxi Province (No.YC2021-S077).
Conflicts of Interest: Ma JX, None; Tian SW, None; Liu QP, None.
REFERENCES
- 1.Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith EL, Zhou XT, Matsui KO, Wu PC, Sankaridurg P, Chia A, Rosman M, Lamoureux EL, Man R, He MG. Myopia. Nat Rev Dis Primers. 2020;6:99. doi: 10.1038/s41572-020-00231-4. [DOI] [PubMed] [Google Scholar]
- 2.Spillmann L. Stopping the rise of myopia in Asia. Graefes Arch Clin Exp Ophthalmol. 2020;258(5):943–959. doi: 10.1007/s00417-019-04555-0. [DOI] [PubMed] [Google Scholar]
- 3.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Saw SM, Matsumura S, Hoang QV. Prevention and management of myopia and myopic pathology. Invest Ophthalmol Vis Sci. 2019;60(2):488–499. doi: 10.1167/iovs.18-25221. [DOI] [PubMed] [Google Scholar]
- 5.Wu PC, Huang HM, Yu HJ, Fang PC, Chen CT. Epidemiology of myopia. Asia Pac J Ophthalmol (Phila) 2016;5(6):386–393. doi: 10.1097/APO.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 6.Summers JA, Schaeffel F, Marcos S, Wu H, Tkatchenko AV. Functional integration of eye tissues and refractive eye development: mechanisms and pathways. Exp Eye Res. 2021;209:108693. doi: 10.1016/j.exer.2021.108693. [DOI] [PubMed] [Google Scholar]
- 7.Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020;103(1):44–54. doi: 10.1111/cxo.12947. [DOI] [PubMed] [Google Scholar]
- 8.Zhang HY, Lam CSY, Tang WC, Leung M, To CH. Defocus incorporated multiple segments spectacle lenses changed the relative peripheral refraction: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2020;61(5):53. doi: 10.1167/iovs.61.5.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.García García M, Pusti D, Wahl S, Ohlendorf A. A global approach to describe retinal defocus patterns. PLoS One. 2019;14(4):e0213574. doi: 10.1371/journal.pone.0213574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan M, Zhao WJ, Geng Y, Zhang Y, Ma J, Chen ZH, Peng MQ, Li Y. Changes in axial length after orthokeratology lens treatment for myopia: a meta-analysis. Int Ophthalmol. 2020;40(1):255–265. doi: 10.1007/s10792-019-01167-9. [DOI] [PubMed] [Google Scholar]
- 11.Si JK, Tang K, Bi HS, Guo DD, Guo JG, Wang XR. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92(3):252–257. doi: 10.1097/OPX.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 12.Sun Y, Xu F, Zhang T, Liu ML, Wang DY, Chen YL, Liu Q. Orthokeratology to control myopia progression: a meta-analysis. PLoS One. 2015;10(4):e0124535. doi: 10.1371/journal.pone.0124535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang SZ, Wang J, Wang NL. Combined orthokeratology with atropine for children with myopia: a meta-analysis. Ophthalmic Res. 2021;64(5):723–731. doi: 10.1159/000510779. [DOI] [PubMed] [Google Scholar]
- 14.Yang N, Bai J, Liu L. Low concentration atropine combined with orthokeratology in the treatment of axial elongation in children with myopia: a meta-analysis. Eur J Ophthalmol. 2022;32(1):221–228. doi: 10.1177/1120672121998903. [DOI] [PubMed] [Google Scholar]
- 15.Li SM, Kang MT, Wu SS, Meng B, Sun YY, Wei SF, Liu LR, Peng XX, Chen Z, Zhang FJ, Wang NL. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic Physiol Opt. 2017;37(1):51–59. doi: 10.1111/opo.12332. [DOI] [PubMed] [Google Scholar]
- 16.Sankaridurg P, Donovan L, Varnas S, Ho A, Chen X, Martinez A, Fisher S, Lin Z, Smith EL, 3rd, Ge J, Holden B. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87(9):631–641. doi: 10.1097/OPX.0b013e3181ea19c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanda H, Oshika T, Hiraoka T, Hasebe S, Ohno-Matsui K, Ishiko S, Hieda O, Torii H, Varnas SR, Fujikado T. Effect of spectacle lenses designed to reduce relative peripheral hyperopia on myopia progression in Japanese children: a 2-year multicenter randomized controlled trial. Jpn J Ophthalmol. 2018;62(5):537–543. doi: 10.1007/s10384-018-0616-3. [DOI] [PubMed] [Google Scholar]
- 18.Bao JH, Yang A, Huang YY, Li X, Pan YG, Ding CL, Lim EW, Zheng JW, Spiegel DP, Drobe B, Lu F, Chen H. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br J Ophthalmol. 2021:bjophthalmol-2020. doi: 10.1136/bjophthalmol-2020-318367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lam CSY, Tang WC, Tse DYY, Lee RPK, Chun RKM, Hasegawa K, Qi H, Hatanaka T, To CH. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363–368. doi: 10.1136/bjophthalmol-2018-313739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moderiano D, Do M, Hobbs S, Lam V, Sarin S, Alonso-Caneiro D, Chakraborty R. Influence of the time of day on axial length and choroidal thickness changes to hyperopic and myopic defocus in human eyes. Exp Eye Res. 2019;182:125–136. doi: 10.1016/j.exer.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Sankaridurg P, Tahhan N, Kandel H, Naduvilath T, Zou HD, Frick KD, Marmamula S, Friedman DS, Lamoureux E, Keeffe J, Walline JJ, Fricke TR, Kovai V, Resnikoff S. IMI impact of myopia. Invest Ophthalmol Vis Sci. 2021;62(5):2. doi: 10.1167/iovs.62.5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohno-Matsui K, Wu PC, Yamashiro K, Vutipongsatorn K, Fang YX, Cheung CMG, Lai TYY, Ikuno Y, Cohen SY, Gaudric A, Jonas JB. IMI pathologic myopia. Invest Ophthalmol Vis Sci. 2021;62(5):5. doi: 10.1167/iovs.62.5.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper J, Tkatchenko AV. A review of current concepts of the etiology and treatment of myopia. Eye Contact Lens. 2018;44(4):231–247. doi: 10.1097/ICL.0000000000000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruiz-Pomeda A, Villa-Collar C. Slowing the progression of myopia in children with the MiSight contact lens: a narrative review of the evidence. Ophthalmol Ther. 2020;9(4):783–795. doi: 10.1007/s40123-020-00298-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2019;102(4):364–377. doi: 10.1111/cxo.12839. [DOI] [PubMed] [Google Scholar]
- 26.Lipson MJ, Brooks MM, Koffler BH. The role of orthokeratology in myopia control: a review. Eye Contact Lens. 2018;44(4):224–230. doi: 10.1097/ICL.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 27.Mak CY, Yam JC, Chen LJ, Lee SM, Young AL. Epidemiology of myopia and prevention of myopia progression in children in East Asia: a review. Hong Kong Med J. 2018;24(6):602–609. doi: 10.12809/hkmj187513. [DOI] [PubMed] [Google Scholar]
- 28.Lam CSY, Tang WC, Tse DYY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98(1):40–45. doi: 10.1136/bjophthalmol-2013-303914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sankaridurg P, Holden B, Smith E, 3rd, Naduvilath T, Chen X, de la Jara PL, Martinez A, Kwan J, Ho A, Frick K, Ge J. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52(13):9362–9367. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 30.Bullimore MA, Richdale K. Myopia Control 2020: where are we and where are we heading? Ophthalmic Physiol Opt. 2020;40(3):254–270. doi: 10.1111/opo.12686. [DOI] [PubMed] [Google Scholar]
- 31.Tone S, Niagu IA, Bogdănici ŞT, Bogdănici CM. Update in pediatric myopia treatment strategies. Rom J Ophthalmol. 2020;64(3):233–238. [PMC free article] [PubMed] [Google Scholar]
- 32.Walline JJ, Lindsley K, Vedula SS, Cotter SA, Mutti DO, Twelker JD. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2011(12):CD004916. doi: 10.1002/14651858.CD004916.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morgan IG, Wu PC, Ostrin LA, Tideman JWL, Yam JC, Lan WZ, Baraas RC, He XG, Sankaridurg P, Saw SM, French AN, Rose KA, Guggenheim JA. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3. doi: 10.1167/iovs.62.5.3. [DOI] [PMC free article] [PubMed] [Google Scholar]