Abstract
Introduction
Drysuits use flexible neck and wrist seals to maintain water-tight seals. However, if the seals exert too much pressure adverse physiological effects are possible, including dizziness, lightheadedness, syncope, and paresthesias in the hands. We aimed to quantify the seal pressures of neck and wrist seals in non-immersed divers.
Methods
We recruited 33 diving volunteers at two dive facilities in High Springs, Florida. After a history and physical exam, we measured vital signs as well as wrist and neck seal pressures using a manometer system.
Results
The mean (SD) seal pressure of the right wrist seals was found to be 38.8 (14.9) mmHg, while that of the left wrist seals was 37.6 (14.9) mmHg. The average neck seal pressure was 23.7 (9.4) mmHg. Subgroup analysis of seal material demonstrated higher mean sealing pressure with latex seals compared to silicone; however, this difference was not statistically significant.
Conclusions
Drysuit seal pressures are high enough to have vascular implications and even potentially cause peripheral nerve injury at the wrist. Divers should trim their seals appropriately and be vigilant regarding symptoms of excessive seal pressures. Further research may elucidate if seal material influences magnitude of seal pressure.
Keywords: Diving, Latex, Paresthesia, Silicone, Technical diving
Introduction
Proper exposure protection is vital for a variety of outdoor pursuits. Appropriate exposure protection not only provides comfort, but it also aids in preventing complications secondary to cold, such as decreased manual dexterity, altered mental status, and hypothermia. Cold environments have been historically associated with occupational exposures; however, more recently these are increasingly recreational in nature.[ 1]
For those participating in aquatic sports, exposure protection is even more important because water has a much greater conductive transfer of heat compared to that of air, which may lead to a rapid loss of body heat and increase the risk of hypothermia.[ 2] In addition to preventing hypothermia, individuals pursuing scuba diving seek thermal protection to maintain their manual dexterity, which is vital to safely retrieve equipment, perform underwater tasks, such as inflating a lift bag or adding breathing gas to a closed-circuit rebreather.
Furthermore, research has shown that thermal effects can influence the efficiency of decompression and that remaining warm during the decompression process significantly reduces the risk of decompression sickness (DCS).[3] It is postulated that vasoconstriction induced by cold body temperatures can increase the degree of gas bubble formation during a dive and increase the risk of the diver developing DCS.[ 4] Therefore, it is crucial that scuba divers don the proper exposure protection for the conditions in which they will be diving so they stay comfortable and warm as well as maintain manual dexterity and limit the risk of DCS.
For dives in temperate waters or short dives, wetsuits often provide adequate exposure protection. However, for longer dives and/or dives in cold water, drysuits are the preferred exposure protection. Drysuits are composed of durable, waterproof material with elastic seals at the wrist and neck that prevent water penetration into the suits. To facilitate a water-tight seal, drysuits apply pressure via these neck and wrist seals. The seals must be comfortable enough to dive and to use over long periods of time as well as durable enough to withstand abrasions and repeated use. Not surprisingly, if these seals exert too much pressure, they can have adverse physiological effects. For instance, neck seals that are too tight can induce dizziness, lightheadedness, and/or syncope due to pressure exerted on the carotid sinus. Similarly, divers with wrist seals that are too tight may experience paresthesias, weakness, or numbness in their hands (likely due to radial nerve involvement), which may lead to decreased manual dexterity and inability to complete underwater tasks. Furthermore, these symptoms persisting after a dive may complicate the differential diagnosis of DCS.
Although the consequences of excessively restrictive drysuit seals are commonly encountered by drysuit divers, especially novice drysuit divers, the seal pressures of drysuit neck and wrist seals have yet to be quantified. The purpose of this study was to quantify the seal pressures of neck and wrist seals in non-immersed divers. We hypothesised that these seals exert pressures consistent with impedance of venous blood flow as suggested by the potential side effects of these seals, such as craniofacial vascular engorgement, syncope, and upper extremity paresthesias.
Methods
Institutional Review Board (IRB 201602349) approval at the University of Florida was obtained.
The study was performed from 0800 to 1700 over three days at two dive facilities in High Springs, Florida, using subjects recruited at those locations. All subjects denied significant cardiopulmonary disease, as well as any significant medical history. All subjects were certified drysuit divers who had at least two months of drysuit diving experience and at least 10 dives in the drysuit they used in the study. Exclusion criteria included historical or physical examination findings consistent with cardiopulmonary disease.
In order to satisfy ethics approval requirements, a brief health survey, diving history, and measurements of non-invasive blood pressure, oxygen saturation, and heart rate before and after drysuit donning were performed. Per the ethics approval committee, these assessments were to ensure subject safety.
To determine the seal pressure of the drysuit seals, a manometer (HT-1890, HT Instruments, Faenza, Italy) was connected to a three-way stopcock via clear, plastic pressure tubing as well as a neonatal non-invasive blood pressure cuff (Welch Allyn, Neonate #1, M1866A, Skaneateles Falls, New York, USA) and an inflation bulb (Figure 1). The pressure was zeroed by partially inflating the non-invasive cuff with the bulb and turning the stop cock to allow the cuff to communicate with the manometer. With the subject’s arm supine, the non-invasive cuff was advanced under the seal on the medial volar surface of the wrist (Figure 2). The same procedure was followed for the contralateral wrist. After measurement of seal pressure on the wrists, the same cuff was placed underneath the drysuit neck seal in the right anterolateral and left anterolateral positions to obtain seal pressures. These two neck measurements were then averaged. The subject then doffed the drysuit and rested for 120 seconds before a final set of blood pressure, heart rate and oxygen saturation measurements were recorded as described above.
Figure 1.
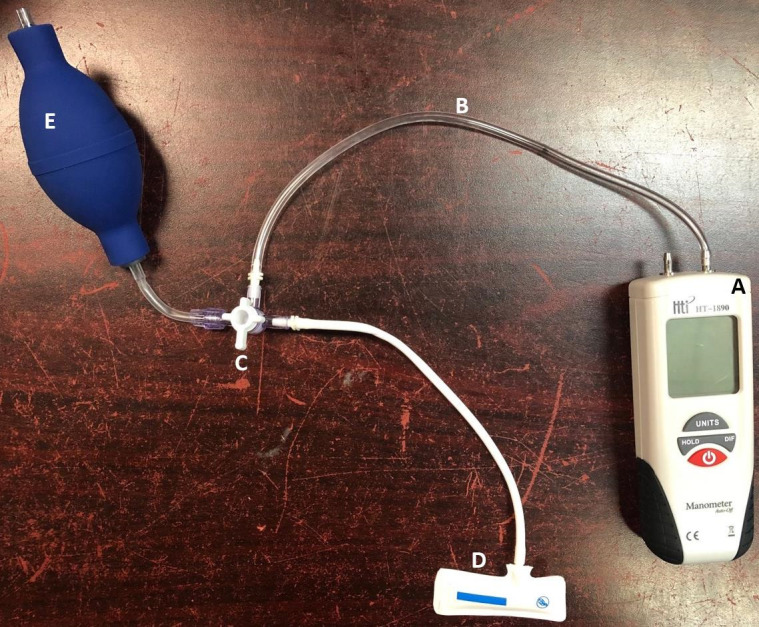
The device assembled to measure the drysuit seal pressures; A − manometer; B − plastic tubing; C − a three-way stop cock; D − disposable vinyl neonatal blood pressure cuff; E − bulb inflator
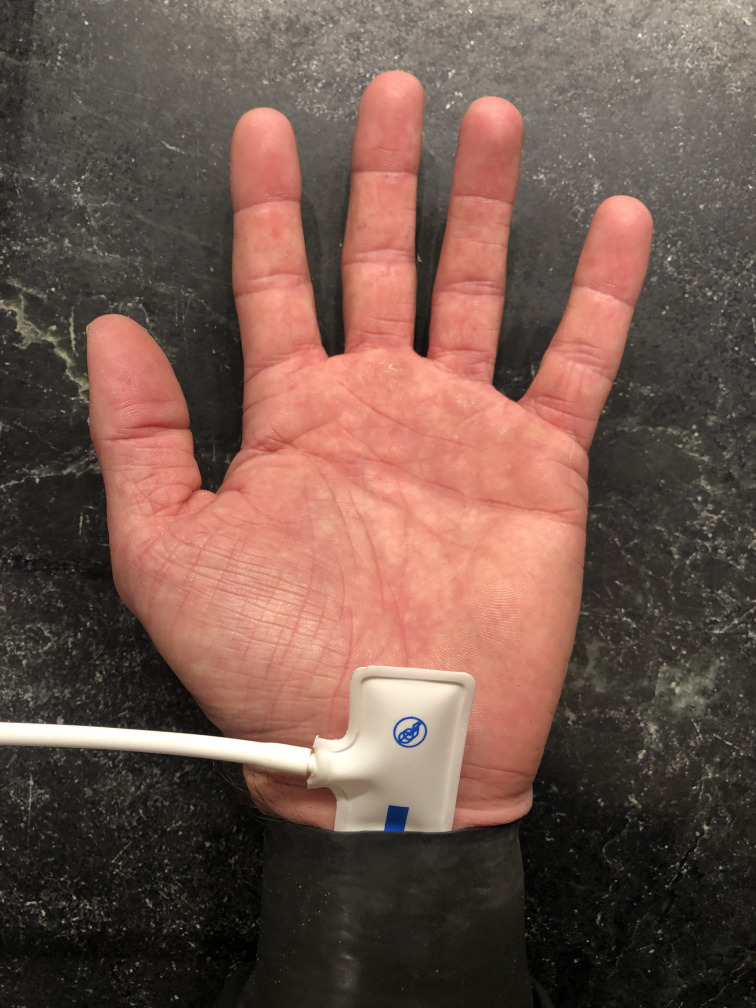
Figure 2.
The neonatal blood pressure cuff slightly inflated, zeroed, and advanced under the drysuit seal along the volar aspect of the wrist
All statistical analyses were performed using JMP® Software (JMP® v15, Cary NC, USA). Summary statistics were calculated for demographic data for study participants and seal pressures for each type of drysuit seal: latex, silicone, and neoprene. Two sample t-tests were used to compare seal pressure means between latex and silicone. Only one study participant used a neoprene drysuit; therefore, no comparisons were completed between neoprene drysuits and other types of drysuits. Statistical significance was set at P < 0.05 and pressure data are presented as mean (SD).
Results
This study involved 33 subjects comprising 24 males (73%) and 9 (27%) females. The mean age was 37.9 (SD 11.2) with a range from 19 to 69 years. The mean years of diving experience was 16.7 (9) with a range of 1 to 40 years. The mean total number of dives was 2,037 (1,854) with a range of 60 to 7,000 dives, while the mean time of diving in a drysuit was 10.45 (7) years with a range from 2 months to 27 years (Table 1).
Table 1. Subject demographics .
| Demographic | Mean (SD) | Median (range) |
| Age (years) | 37.9 (11.2) | 35 (19−69) |
| Height (cm) | 175.2 (9.2) | 178 (155−190) |
| Weight (kg) | 79.7 (15.6) | 77.3 (47.7−113.4) |
| Body mass index (kg·m-2) | 25.7 (3.7) | 26.1 (18.6−34.9) |
| Diving experience | 16.7 (9) | 18 (1−40) |
| Total dives | 2,037 (1,854) | 1,500 (60−7,000) |
| Drysuit experience (years) | 10.5 (7) | 10 (0.2−27) |
Wrist and neck seal pressures are reported in Table 2. Subgroup analysis showed that the wrist seals made of latex had higher mean seal pressures than those made of silicone. There was no significant measurable difference between right and left seals. No subjects used neoprene wrist seals. Subgroup analysis of the latex neck seals also yielded higher mean seal pressures compared to those made of silicone and neoprene. One subject had a neoprene neck seal, which had a seal pressure of 22.7 mmHg (Table 3).
Table 2. Drysuit seal pressures (mmHg) measured in 33 subjects .
| Seal | Mean (SD) | Median (range) |
| Right wrist | 38.8 (14.9) | 34.8 (15.3−66.3) |
| Left wrist | 37.6 (12.8) | 37.7 (9.2−62.2) |
| Neck | 23.7 (9.4) | 22.5 (6.8−44.5) |
Table 3. Drysuit seal pressures (mmHg) by seal material .
| Seal | Mean (SD) | Median (range) |
| Latex (n = 28) | ||
| Right wrist | 39.7 (14.7) | 36.0 (15.3−66.3) |
| Left wrist | 38.2 (12.8) | 37.8 (9.2−62.2) |
| Neck | 24.4 (10.8) | 22.9 (7.3−43.6) |
| Silicone (n = 5) | ||
| Right wrist | 34.1 (16.8) | 31.7 (17.7−57.5) |
| Left wrist | 34.2 (14.1) | 30.3 (18.9−56.7) |
| Neck n = 4 | 18.8 (10.7) | 18.8 (5.7−31.9) |
| Neoprene (n = 1) | ||
| Neck | 22.7 | 22.7 |
Although the latex seals exerted higher pressures compared to those made of silicone and neoprene, statistical analysis via unpaired t-tests did not support statistically significant differences in these pressures. The statistical analysis is presented in Table 4.
Table 4. Unpaired t-tests assessing differences in exerted pressure (mm Hg) of latex and silicone drysuit seals .
| Comparison | Absolute mean difference (95% CI) | P-value |
| Right wrist latex vs silicone | 5.6 (-9.2 to 20.4) | 0.45 |
| Left wrist latex vs silicone | 4 (-8.8 to 16.8) | 0.53 |
| Neck latex vs silicone | 7.43 (-2.64 to 17.5) | 0.22 |
Discussion
We found that the average sealing pressures of the wrist and neck seals were substantial and likely of enough magnitude to induce physiological changes, such as paresthesias and syncope. These findings help explain the commonly reported symptoms of hand paresthesias and occasional syncopal episodes in divers using drysuits.
Previous research investigating pressure and nerve injuries has shown that pressures of 30 mmHg can limit axonal transport and result in nerve dysfunction as well as endoneurial oedema.[ 5] The same study also found that pressures of 50.25 mmHg applied to the carpal tunnel for 120 seconds can alter the structure of the myelin sheaths, leading to permanent nerve damage.[ 5] Our findings show that the average pressures generated by the wrist seals of drysuits exceed the pressure required to limit axonal transport and epineural blood flow. Furthermore, a large percentage of the subjects demonstrated seal pressures greater than that required to damage the myelin sheath, which could lead to permanent nerve damage.
If only the latex seals are considered, the average seal pressures in this study were even higher. These high seal pressures and the fact that some subjects reported dive times exceeding 10 hours are concerning for nerve injury; however, there are no reports in the literature of upper extremity nerve injury due to drysuit wrist seals. It is possible that the seal pressures of the wrist seals may be lower during diving secondary to immersion physiology, which can be characterised by an increased shunting of blood to the central circulation, diuresis, and intravascular depletion.[ 6 , 7] It is also possible that these wrist seals induce subclinical neuronal damage.
Previous research investigating pressure and venous return found that initial venous narrowing of superficial and deep leg veins occurs between 30 and 40 mmHg when in a seated or standing position.[ 8] The same study found that complete occlusion of superficial and deep leg veins occurs at 20 to 25 mmHg when in the supine position and 50 to 60 mmHg when in the seated position.8 In the aforementioned study, cuff pressures were gradually increased over 30 seconds while occlusion was observed via ultrasound. Our findings suggest that the pressure exerted by the drysuit seals on the neck are sufficient to occlude venous return from the head and neck. It is possible that this restriction of venous outflow could lead to increasing venous pressure and intracranial pressure, which can result in decreased cerebral perfusion pressure (CPP).[ 9] It is worth noting the latex seals are narrower than the venous tourniquet, which may lead to differences in pressures exerted into deeper tissues.
A study on syncope, cerebral perfusion, and oxygenation found that presyncopal symptoms coincided with an excessive reduction in mean middle cerebral artery blood flow velocity.[ 10] In the same study, it was noted that progressive drops in mean arterial pressure and CPP were observed when vasovagal syncope was induced under laboratory conditions. As the pressures exerted by the neck seals were found to be higher than what would be expected within many of the veins in the superficial neck, it is likely these seals are inhibiting craniofacial drainage, which could increase intracranial pressure and subsequently reduce CPP. These findings in the above-mentioned study and those in the present study lead us to believe that a decrease in CPP may explain the syncopal episodes reported by some divers using drysuits.
We also found that the average seal pressure was lower in divers with silicone seals, although these differences were not statistically significant. Thus, our research suggests that divers who are sensitive to the effects of seal pressures should consider the use silicone seals instead of the more commonly used latex seals. However, it is important to note that variances in seal design and material property could also impact seal pressures as well. Considering only one subject had neoprene seals, we cannot make conclusions regarding this material’s seal pressure.
Limitations of this study include the relatively small number of subjects. In addition, this study included only five subjects with silicone wrist seals, four subjects with silicone neck seals, and one with a neoprene neck seal. All remaining seals were latex. In addition, as mentioned above, seal design and differences in material properties could also influence seal pressures. Furthermore, this study assessed only non-immersed divers. Thus, the described physiologic changes associated with drysuits when the diver is topside may not translate to the haemodynamic changes induced by diving and immersion. As immersion phenomena and activity underwater induce a variety of significant physiologic changes, such as increases in preload, decreases in heart rate, and others, it is likely that the blood flow through these seals would be different. Lastly, drysuit seals will stretch over time and with use. Thus, the seal pressures will likely decrease over time. Consequently, our results represent only a single point in time for each subject and for each seal.
Conclusions
Drysuit seals exert a significant amount of force to prevent water intrusion. Although the average seal pressure may vary slightly between divers and seal materials, the seal pressures are of a magnitude consistent with vascular implications and even possible neural injury, especially in the setting of latex wrist seals. Divers wishing to avoid the effects of these seals should be especially careful to trim their seals appropriately. Further work should focus upon the impact of seal material on seal pressure.
Footnotes
Conflict of interest and funding: nil
Contributor Information
Derek B Covington, Department of Anesthesiology, Center for Hyperbaric and Environmental Physiology, Duke University, Durham (NC), USA.
Matthew Spears, Department of Anesthesiology, University of Florida College of Medicine, Gainesville (FL), USA.
Richa Wardhan, Department of Anesthesiology, University of Florida College of Medicine, Gainesville (FL), USA.
Meghan Brennan, Department of Anesthesiology, University of Florida College of Medicine, Gainesville (FL), USA.
Yasmin Islam, Department of Ophthalmology, University of Florida College of Medicine, Gainesville (FL), USA.
Andrew D Pitkin, Department of Anesthesiology, University of Florida College of Medicine, Gainesville (FL), USA.
References
- Procter E, Brugger H, Burtscher M. Accidental hypothermia in recreational activities in mountains: a narrative review. Scand J Med Sci Sports. 2018;28:2464–72. doi: 10.1111/sms.13294. [DOI] [PubMed] [Google Scholar]
- Koop LK, Tadi P. Physiology, heat loss. Treasure Island (FL): StatPearls Publishing; 2022 Jan. [PubMed] [Google Scholar]
- Gerth WA. On diver thermal status and susceptibility to decompression sickness. Diving Hyperb Med. 2015; 45: 208 . [cited 2022 Feb 28]. Available from: https://www.dhmjournal.com/images/IndividArticles/45Sept/Gerth_dhm.45.3.208.pdf. [PubMed] [Google Scholar]
- Smertz R. The relationship of decongestant use and risk of decompression sickness; a case-control study of Hawaiian scuba divers. Hawaii J Med Public Health. 2014;73:61–5. [PMC free article] [PubMed] [Google Scholar]
- Rempel D, editor. Work-related musculoskeletal disorders: report, workshop, summary, and workshop papers. Washington (DC): National Academies Press (US); 1999. [PubMed] [Google Scholar]
- Arborelius M, Ballidin UI, Lilja B, Lundgren CE. Hemodynamic changes in man during immersion with head above water. Aerosp Med. 1972;43:592–8. [PubMed] [Google Scholar]
- Boussuges A, Gole Y, Mourot L, Jammes Y, Melin B, Regnard J, et al. Haemodynamic changes after prolonged water immersion. J Sports Sci. 2009;27:641–9. doi: 10.1080/02640410902717001. [DOI] [PubMed] [Google Scholar]
- Partsch B, Partsch H. Calf compression pressure required to achieve venous closure from supine to standing positions. J Vasc Surg. 2005;42:734–8. doi: 10.1016/j.jvs.2005.06.030. [DOI] [PubMed] [Google Scholar]
- Mayer SA, Randolph M, editors . On call neurology, 3rd ed. Elsevier Saunders; 2007. [Google Scholar]
- Van Lieshout JJ, Wieling W, Karemaker JM, Secher NH. Syncope, cerebral perfusion, and oxygenation. J Appl Physiol (1985). 2003;94:833–48. doi: 10.1152/japplphysiol.00260.2002. [DOI] [PubMed] [Google Scholar]