Abstract
Gerontological research suggests that social network characteristics are key elements of successful aging as they are related to a positive quality-of-life (QoL). Less is known about the social networks of persons aging with HIV. To describe social network characteristics and assess the effect of social network size on QoL, a sample of 146 OPWH (age ≥50) was recruited from an outpatient HIV clinic in Atlanta, GA. Social network size was assessed using Cohen’s social network index (SNI). Domains of QoL (physical, emotional, and social) were assessed using the RAND-36. Descriptive analyses were used to determine the frequency of contact within social networks and multivariable regression models were used to assess the relationship between SNI and three domains of QoL controlling for potential covariates. Participants were predominantly male (60%), heterosexual (63%), and African American (86%). Regular contact occurred most frequently with friends (82%) and relatives (77%). Multivariable modeling revealed that SNI explained 58% of the variance in emotional QoL (R2 = 0.58, F(8, 137)= 25.48, p < .001). Findings provide basis for potential interventions focused on the specific social network to improve emotional QoL of this vulnerable population.
Keywords: social network size, HIV, aging, depression, quality of life
INTRODUCTION
Social ties play an important role in promoting health across all life stages (Umberson, Crosnoe, & Reczek, 2010). Regardless of quantity, quality, or type, social relationships are consistently associated with well-being (Berkman, Kawachi, & Glymour, 2014; Huxhold, Fiori, & Windsor, 2013; Pinquart & Sörensen, 2000). The term social network generally refers to an objective feature of social engagement such as size or quantity of one’s social relationships with a preidentified set of roles such as family, friends, or group-based contacts (B. Cornwell, Schumm, Laumann, & Graber, 2009). While the concept of social network describes the more objective features of one’s social circle, social connectedness describes the subjective perceptions related to belonging, loneliness, and strength of social ties (Ashida & Heaney, 2008).
Among older adults, social networks– defined herein as the quantity and diversity of connections with others beyond marital status, including relatives, friends, and society– generate positive impacts on overall health, quality-of-life, psychological well-being, and mortality (Gerritsen, Steverink, Ooms, & Ribbe, 2004; Jansen & von Sadovszky, 2004; Kawachi & Berkman, 2001; Kiely & Flacker, 2003). Older adults tend to have smaller social network sizes compared to younger adults but report strong social ties and equivalent numbers of close friends (Bruine de Bruin, Parker, & Strough, 2020). de Bruin et al (Bruine de Bruin et al., 2020) found the number of close friends, not total network size, to be the main driver of well-being for both younger and older adults. Studies specifically among older people living with HIV (OPWH) have also described shrinking social network sizes with advancing age (Shippy & Karpiak, 2005). In addition to age-related changes to the social environment such as retirement and the death of loved ones, many OPWH are also part of the cohort of HIV long-term survivors. Long-term survivors came of an age in the early days of the HIV/AIDS epidemic, prior to the advent of life-saving antiretroviral therapy (ART), and when HIV was characterized by the swift and tragic loss of life. The loss of partners, friends, communities, and other important social relationships to AIDS in those decades created a ripple effect on support systems which persist in later life (Schrimshaw & Siegel, 2003).
Extant studies have examined the role of social networks in health outcomes specifically for OPWH (Brennan-Ing, Seidel, & Karpiak, 2017; Emlet, 2006; Poindexter & Shippy, 2008). Emlet (Emlet, 2006) found that although older adults have smaller social networks, having someone to confide in was associated with lower perceived HIV-related stigma. A qualitative study by Poindexter and Shippy (Poindexter & Shippy, 2008) illustrates the ways in which OPWH navigate their changing social networks. In their description, individual’s networks tend to be comprised of other people living HIV and these networks shrink when people die of HIV-related complications. However, these earlier studies occurred when mortality rates were higher among people living with HIV. HIV-associated mortality rates have fallen steadily since 2005 (Global Burden of Disease, 2019). More recently, Brennan-Ing et al (Brennan-Ing et al., 2017) developed a typology of social networks for OPWH and found those who were characterized as isolated experienced greater psychological distress and lower well-being. These studies support the importance of social networks and social relationships in promoting positive quality-of-life (QoL). However, few studies have focused on the social network size in relation to specific domains of QoL for OPWH using a quantitative approach. As defined by the World Health Organization (WHO), QoL is “a state of complete physical, mental, and social well-being not merely the absence of disease” (WHO, 1948). Given the important effects of social networks on well-being and QoL, the current study assessed the diversity and size of the social ties of OPWH with the following aims: 1) characterize the social networks of OPWH and 2) assess the association between social network size and the physical, social, and emotional domains of QoL while controlling for covariates (Figure 1).
Figure 1.
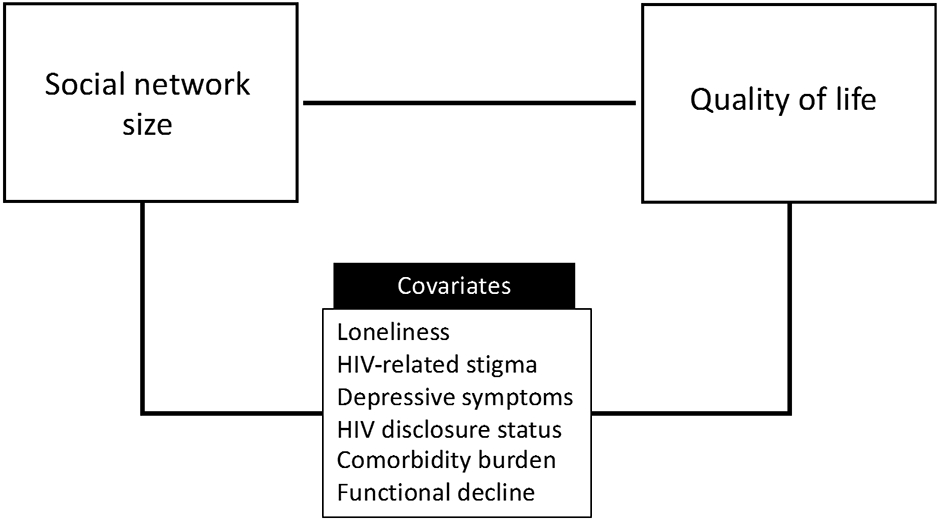
Conceptual framework of the study
METHODS
Data source & study sample
This study is a secondary analysis of data from an observational study of OPWH recruited from a comprehensive HIV clinic in Atlanta, GA from 2016 to 2017.(M. Yoo-Jeong, Haardörfer, Holstad, Hepburn, & Waldrop-Valverde, 2021; Moka Yoo-Jeong, Hepburn, Holstad, Haardörfer, & Waldrop-Valverde, 2020) Inclusion criteria included: 1) age ≥50, 2) HIV diagnosis confirmed from medical chart, and 3) enrollment in the recruiting clinic. Participants were recruited through flyers, word of mouth, and healthcare provider referrals. Study information was provided to 149 eligible individuals but three failed to provide consent, leaving a final sample of 146 participants. After obtaining informed consent, participants met with research staff to complete a one-time survey. Total time to complete the survey was approximately 45-60 minutes. Participants were compensated with $25 for their participation. All study procedures were reviewed and approved by the Institutional Review Boards (IRB) at Emory University and the recruiting clinic’s Research Oversight Committee.
Measures
Social network size was measured using the Social Network Index (SNI). The measure assessed frequency of interaction with 12 categories of social relationships, including: (1) spouse, (2) parents, (3) parents-in-law, (4) children, (5) close relatives, (6) neighbors, (7) close friends, (8) coworkers/colleagues, (9) classmates/teachers, (10) fellow volunteers, (11) members from organizations such as social clubs, professional organizations, etc., and (12) religious group members (such as church or temple). Having “regular contact” was defined as physically seeing or talking on the phone with someone at least once every two weeks (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997). Having regular contact with at least one person from a social contact category is assigned one point for a maximum SNI score of 12. A total SNI score of 12 denotes a strong social network. SNI score was treated as a dichotomous variable following established procedures from previous studies. Having a ‘diverse social network’ was defined as having a SNI score of 4 or greater and having a SNI score of 3 or less was defined as having a ‘limited social network’ (Aberaraw, Boka, Teshome, & Yeshambel, 2020; Aung et al., 2016; Musich, Wang, Slindee, Kraemer, & Yeh, 2019).
Quality-of-life was assessed using the RAND-36. The RAND-36 is a well-validated (test-retest reliability r = 0.94; internal consistency, Cronbach’s alpha 0.96) (VanderZee, Sanderman, Heyink, & de Haes, 1996) in the HIV population (Riley et al., 2003) and widely used health-related, quality-of-life measure. The full scale includes 36 items across 8 domains, but the current analyses focus on the three domains of physical, social, and emotional QoL to reflect the definition of QoL by the WHO. Items assess perceived health status during the last 4 weeks (Hays & Morales, 2001). Scores for each domain range from 0-100, with higher scores indicating better quality-of-life.
Covariates were chosen a priori based on their potential to covary with quality-of-life as suggested from the extant gerontological and HIV literature. We collected self-reported demographic data on age, sex assigned at birth, sexual orientation, time since HIV diagnosis, level of education, race/ethnicity, and homelessness/unstable housing in the previous 12 months. Additional covariates measures are described below.
Loneliness was measured with the Patient-Reported Outcomes Measurement Information System (PROMIS)-Social Isolation (SI) Short Form v2.0 8a. The PROMIS-SI measure uses a 5-point Likert scale (1=“Never” to 5=“Always”) on 8-items derived from social relationship scales and the UCLA-Loneliness Scale (Cyranowski et al., 2013). A total raw score ranging from 8 to 40 is calculated by summing the values of the response to each item. The total raw score was converted into a standardized T-score with a mean of 50 and a standard deviation (SD) of 10 (Cella et al., 2010), following the score conversion table in the scoring instructions. Cronbach’s alpha for our sample was 0.95.
HIV-related stigma was measured with the Internalized AIDS-Related Stigma Scale (Kalichman et al., 2009), which contains 6 items rated dichotomously (1=“agree”, 0=“disagree”), with scores ranging from 0 to 6. A higher score is indicative of greater HIV-related stigma. This scale shows good internal reliability (α= .73 to .76) and criterion validity. The Cronbach’s alpha for our sample was 0.83.
HIV-disclosure status was assessed using one-item that assessed whether participants disclosed their HIV status to at least one other person. Participants were dichotomized into two categories based on their response (0=“disclosure to no one”, 1=“disclosure to someone”).
Depressive symptoms were assessed using the 20-item Center for Epidemiologic Studies Depression Scale Revised (CESD-R)(Eaton, Smith, Ybarra, Muntaner, & Tien, 2004) that assesses nine symptoms of depression (dysphoria, anhedonia, appetite, sleep, concentration, worthlessness, fatigue, agitation, and suicidal ideation) in accordance with the Diagnostic and Statistical Manual (DSM-V) criteria for Major Depressive Disorder. Participants answered 0= “Not at all or less than one day” to 3= “Nearly every day for 2 weeks,” with possible scores ranging from 0 to 60. The Cronbach’s α was 0.93 in our sample.
Comorbidity burden was measured using the self-reported version of the Charlson Comorbidity Index (CCI) (Charlson, Pompei, Ales, & MacKenzie, 1987). Participants were asked to identify if they have a diagnosis (0= “No”, 1=“Yes”) of 19 listed conditions (myocardial infarction, congestive heart failure, peripheral vascular disease, etc.). Each condition was assigned a weight based on the adjusted 1-year mortality risk. AIDS diagnosis is included in the original CCI but was omitted in our study as its weight is outdated in the current era of combination ART (Zavascki & Fuchs, 2007) and age was not adjusted in this study as our sample consisted of only those who are age 50 and older.
Functional Status was measured using a modified version of Instrumental Activities of Daily Living Scale (IADL (Lawton & Brody, 1969), which consists of self-reported levels of functionality on eight daily tasks (e.g., using the telephone, shopping, preparing meals, doing housework, doing laundry, traveling methods, medication management, and managing finances) with possible scores ranging from 0 (low function, dependent) to 8 (high function, independent). The IADL has been used frequently in HIV research and shows good reliability (α= .85) and validity.
Analysis
Participant characteristics by dichotomized SNI scores were described using test for independence or independent t-test as appropriate. Three separate hierarchical multivariable regression models were used to assess the association between dichotomized SNI scores and quality-of-life domains, controlling for covariates found to have p-value <.10 from or t-tests. In multivariable regression models, p-values <.05 were considered statistically significant. All analyses were conducted using SPSS version 26.
RESULTS
A total of 146 OPWH completed the study. The sample characteristics by dichotomized SNI scores are presented in Table 1. The study sample was predominantly African American (85.6%), male (60.3%), heterosexual (63%), and had high school education or greater/or GED (78%). Seventeen people reported past homelessness/unstable housing and about 11% reported not disclosing their HIV status to anyone. The mean SNI score was 4.84 (SD = 2.1). In bivariate analysis, participants with limited social networks (SNI<4) were more likely to have higher scores for depressive symptoms, HIV-related stigma, and loneliness, and reduced emotional well-being than individuals with diverse social network (p<.05). As shown in Figure 2, the most frequent regular contacts for our sample were with close friends and relatives.
Table 1.
Characteristics of OPWH in categories of social network index (N=146)
| Characteristic | Total | Social network index | p-value | |
|---|---|---|---|---|
| Limited (SNI 0-3) |
Diverse (SNI ≥4) |
|||
| n (%) | ||||
| Race/ethnicity | .297 | |||
| African American/Black | 125 (85.6) | 34 | 91 | |
| White/Non-Hispanic | 12 (8.2) | 5 | 7 | |
| Other | 9 (6.2) | 1 | 8 | |
| Sex assigned at birth | .297 | |||
| Male | 88 (60.3) | 28 | 60 | |
| Female | 55 (37.7) | 11 | 44 | |
| Other, Not reported | 3(2.1) | 1 | 2 | |
| Sexual orientation | .442 | |||
| Homosexual, Gay, or Lesbian | 30 (20.5) | 11 | 19 | |
| Heterosexual or Straight | 92 (63.0) | 23 | 69 | |
| A Man Who Has Sex With Men, Bisexual, Other | 24 (16.5) | 6 | 18 | |
| Education | .812 | |||
| Some high school or less | 32 (22.0) | 10 | 22 | |
| High school graduate or equivalent (GED) | 54 (37.0) | 15 | 39 | |
| Some college or higher | 60 (41.0) | 15 | 45 | |
| Homelessness or unstable housing in the past 12 months | 17 (11.6) | 8 | 9 | .053 |
| HIV disclosure to no one | 17 (11.6) | 6 | 11 | .437 |
| mean ± SD | ||||
| Age, years | 56.53 (4.55) | 56.90 (5.12) | 56.39 (4.33) | .545 |
| Time since HIV diagnosis, years | 18.10 (8.36) | 16.75 (8.69) | 18.61 (8.21) | .231 |
| Comorbidity burden | 1.28 (1.54) | 1.68 (1.91) | 1.13 (1.36) | .106 |
| Functional status | 7.66 (0.78) | 7.65 (0.77) | 7.67 (0.79) | .892 |
| Depressive symptoms | 10.86 (10.31) | 13.63 (11.47) | 9.82 (9.69) | .046 |
| HIV-related stigma | 1.94 (1.94) | 2.5 (2.12) | 1.72 (1.84) | .032 |
| Loneliness | 47.19 (10.09) | 50.43 (11.95) | 45.97 (9.07) | .037 |
| Quality of life domains | ||||
| Physical functioning | 60.92 (27.90) | 59.38 (30.13) | 61.51 (27.13) | .682 |
| Emotional wellbeing | 74.38 (19.41) | 64.20 (23.38) | 78.23 (16.21) | .001 |
| Social functioning | 71.27 (25.91) | 64.75 (30.61) | 73.73 (23.61) | .099 |
Notes. OPWH=older persons living with HIV; SNI= social network index. SD=standard deviation.
Figure 2. Distribution of active social networks*.
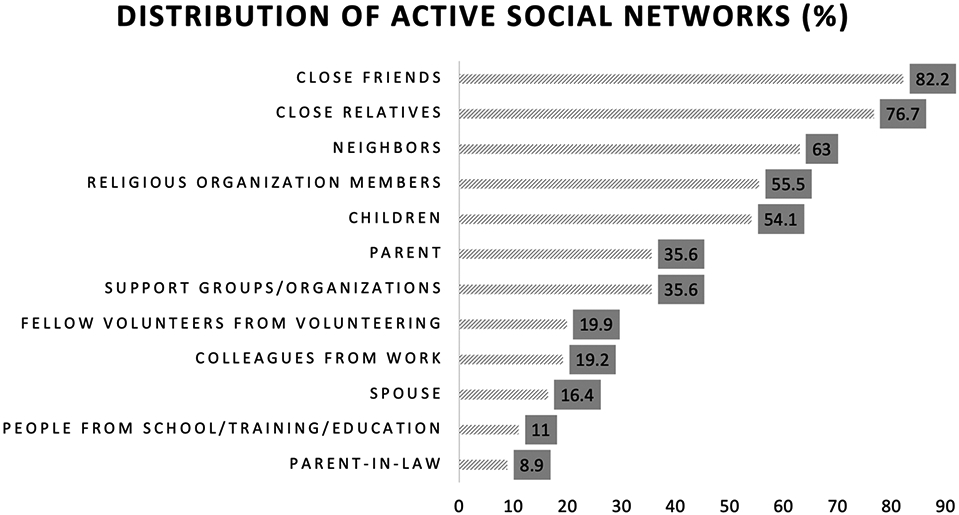
Notes. *Having regular contact with at least one person from each type of social contact is considered having an active social networks.
The multivariable regression used the dichotomized SNI score to assess the relationship to each domain of quality-of-life, controlling for significant covariates (Table 2). The results showed that social network index explained a significant amount of the variance in the QoL domain of emotional wellbeing, controlling for other covariates (R2 = 0.58, F(8, 137)= 25.48, p < .001). Although SNI significantly predicted emotional wellbeing (β=.168, t(145)=2.246, p=.026), it was not a significant predictor of the other QoL domains. Among all covariates considered, symptoms of depression remained a significant predictor for all three domains of QoL, controlling for other factors.
Table 2.
Estimated standardized coefficient (β) on domains of quality of life
| Variables | Physical functioning | Emotional wellbeing | Social functioning |
|---|---|---|---|
| Model 1 | R2=.167*** | R2=.143*** | R2=.136*** |
| Male | .259 ** | .004 | .147 |
| Past unstable housing | −.013 | −.255 ** | −.104 |
| Comorbidity burden | −.151 | −.246 ** | −.210 ** |
| Functional status | .280 *** | .076 | .232 ** |
| Model 2 | R2=.269*** | R2=.558*** | R2=.416*** |
| Male | .239** | −.024 | .109 |
| Past unstable housing | .081 | −.046 | .061 |
| Comorbidity burden | −.069 | −.070 | −.080 |
| Functional status | .260 ** | .006 | .202 ** |
| Depressive symptoms | −.296 ** | −.510 *** | −.534 *** |
| HIV stigma | .078 | −.077 | −.015 |
| Loneliness | −.117 | −.254 ** | −.062 |
| Model 3 | R2=.269*** | R2=.584*** | R2=.420*** |
| Male | .240** | −.006 | .116 |
| Past unstable housing | .081 | −.029 | .068 |
| Comorbidity burden | −.068 | −.052 | −.074 |
| Functional status | .260 ** | .012 | .204 ** |
| Depressive symptoms | −.296 ** | −.501 *** | −.531 *** |
| HIV stigma | .078 | −.061 | .009 |
| Loneliness | −.116 | −.242 ** | −.058 |
| Social network size | .005 | .168 ** | .066 |
Notes. Bolded items indicate statistical significance at
p<.05
p <.01
p<.001, two-taile
DISCUSSION
As persons living with HIV continue to benefit from potent antiretroviral therapy and move into older age, issues seen in HIV-negative older adult populations, such as loneliness and isolation, are now of critical importance to understand and address among OPWH. This study evaluated the association of social network size to three domains of QoL—defined as physical and social functioning and emotional well-being (WHO, 1948) – among HIV-positive individuals who are 50 years old and older. Adjusting for relevant covariates, study results indicate that greater social network size was associated with better emotional well-being. Social network size was unrelated to physical and social QoL in this sample.
Prior studies among HIV-positive individuals have partially supported our results. A study among a sample of mostly gay men in Ontario, Canada, found that perceived availability of social support was directly related to both mental and physical aspects of QoL (Bekele et al., 2013). Similarly, a study that operationalized social support through the concept of social capital (both individual/family and community/society social capital), found that mental QoL was associated with both individual/family and community/society social capital (Lin et al., 2020). Among older persons without HIV, research supports the notion that self-rated emotional health is related to social disconnectedness but that loneliness is a particularly strong indicator of emotional health (E. Y. Cornwell & Waite, 2009). One’s perceptions of loneliness and one’s tangible social network may impact QoL in different ways. Although each of these studies included samples and measures different from those used in the current study, the findings suggest that social support is associated with different aspects of QoL. Relationships between the social networks and aspects of QoL may vary by population but in general, findings from these studies and ours suggest a meaningful indicator of QoL among persons living with HIV (PWH) is social network support.
The make-up of social networks for participants in this study were comprised of mostly close friends and relatives. This aligns with other studies among older persons living in the community without HIV (Fiori, Smith, & Antonucci, 2007), suggesting that size of social networks often shrinks over time as one ages. Although our study sample was much younger than older persons living in the community without HIV, many of our participants were unemployed or receiving disability benefits. Like those older adults without HIV, the current sample were typically not working and therefore did not have work colleagues with whom to connect and socialize. Unemployment may further limit HIV-positive individuals’ social connections at a younger age than those older adults living without HIV. Given the likelihood of OPWH relying on close friends and relatives for support, future research and interventions in the population may benefit from a focus on these connections and steps to strengthen them. Additionally, more research is needed to identify specific needs for social networks in relation to QoL to inform the development of intervention. For example, whether OPWH prioritize targeted counseling to strengthen or rectify existing relationships over finding ways to increase social participation needs to be explored.
Research suggests that quality of life of older adults are positively affected by the quality of social networks (Bruine de Bruin et al., 2020). While the current study measured the size and diverse nature of social networks, it did not capture the quality of the networks. The effects of the quality of social networks on QoL may be different from the effects of quantity of networks in OPWH. Future study is needed to assess both the quality and the size of social networks to understand the mechanism by which social networks affect QoL among OPWH.
Depression was associated with all forms of QoL measured in this study. Rates of major depression and depressive symptoms are higher among persons with HIV than among the general population with prevalence estimated at around 39% of PWH (Uthman, Magidson, Safren, & Nachega, 2014). Symptoms of depression can affect social relationships, through symptoms of withdrawal, loss of interest, and lack of motivation to engage in social relationships. The resulting self-isolation can also worsen depression, creating a vicious cycle. Lack of social relationships can also exacerbate symptoms of depression, ultimately affecting the QoL. Although the relationship of depression to QoL was not the primary focus of this study, it is important to note its consistent relationship with all domains of QoL and that, social network size continued to be associated with emotional domain of QoL in addition to the effects of depression. These findings may help provide avenues for intervention (e.g., strengthening or growing one’s social network) that can improve emotional well-being and thus, depression. It is also possible that depressive symptoms work as a mechanistic pathway that explains the effect of social network size on emotional QoL, such that individuals with low social networks have higher depressive symptoms, resulting in reduced emotional QoL. Similarly, a study among a sample of mostly gay men in Canada tested the indirect effects of social support on mental and physical QoL through symptoms of depression and found that depressive symptoms mediated the effects of social support on QoL (Bekele et al., 2013). Future research is needed to understand whether depression explains the effect of size of networks on QoL among OPWH.
These findings should be considered within their limitations. The study sample was recruited from a US southern HIV clinic in a high resource setting and may not be generalized to other populations of persons living with HIV. This clinic provides multidisciplinary services including support groups and therefore may have affected participants’ social network size positively. Measures of the quality of social relationships were also not included. Such measures may provide more precision in our understanding of social networks’ influence on QoL. Moreover, the nature of social networks, depressive symptoms, and QoL are likely complex and multi-directional; the cross-sectional data from the present study were not suitable for more complex statistical analyses. Future studies should explore potentially moderating/mediating effects of important covariates such as depressive symptoms on the association between social networks and QoL in OPWH.
In conclusion, the present study found that social network size was associated with emotional well-being among older persons living with HIV in a southern US clinic. Findings support those among HIV-negative older adults and inform potential interventions focused on close friends and relatives to improve emotional well-being of this vulnerable population.
Acknowledgements
This work was supported in part by the National Institute of Nursing Research [F31NR015975] and the National Institute on Aging [K01AG064986].
Footnotes
Disclosure Statement
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
REFERENCES
- Aberaraw R, Boka A, Teshome R, & Yeshambel A (2020). Social networks and quality of life among female breast cancer patients at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia 2019. BMC women's health, 20(1), 50–50. doi: 10.1186/s12905-020-00908-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashida S, & Heaney CA (2008). Differential associations of social support and social connectedness with structural features of social networks and the health status of older adults. J Aging Health, 20(7), 872–893. doi: 10.1177/0898264308324626 [DOI] [PubMed] [Google Scholar]
- Aung MN, Moolphate S, Aung TNN, Katonyoo C, Khamchai S, & Wannakrairot P (2016). The social network index and its relation to later-life depression among the elderly aged ≥80 years in Northern Thailand. Clinical interventions in aging, 11, 1067–1074. doi: 10.2147/CIA.S108974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekele T, Rourke SB, Tucker R, Greene S, Sobota M, Koornstra J, … Guenter D (2013). Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care, 25(3), 337–346. doi: 10.1080/09540121.2012.701716 [DOI] [PubMed] [Google Scholar]
- Berkman LF, Kawachi I, & Glymour MM (2014). Social epidemiology: Oxford University Press. [Google Scholar]
- Brennan-Ing M, Seidel L, & Karpiak SE (2017). Social Support Systems and Social Network Characteristics of Older Adults with HIV. Interdiscip Top Gerontol Geriatr, 42, 159–172. doi: 10.1159/000448561 [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W, Parker AM, & Strough J (2020). Age differences in reported social networks and well-being. Psychol Aging, 35(2), 159–168. doi: 10.1037/pag0000415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, … Hays R (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol, 63(11), 1179–1194. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, & MacKenzie CR (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis, 40(5), 373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM Jr. (1997). Social ties and susceptibility to the common cold. Jama, 277(24), 1940–1944. [PubMed] [Google Scholar]
- Cornwell B, Schumm LP, Laumann EO, & Graber J (2009). Social Networks in the NSHAP Study: rationale, measurement, and preliminary findings. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 64(suppl_1), i47–i55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav, 50(1), 31–48. doi: 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Zill N, Bode R, Butt Z, Kelly MA, Pilkonis PA, … Cella D (2013). Assessing social support, companionship, and distress: National Institute of Health (NIH) Toolbox Adult Social Relationship Scales. Health Psychol, 32(3), 293–301. doi: 10.1037/a0028586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, & Tien A (2004). Center for Epidemiologic Studies Depression Scale: review and revision (CESD and CESD-R). In Maruish ME (Ed.), The Use of Psychological Testing for Treatment Planning and Outcomes Assessment (3rd ed., Vol. 3, pp. 363–377). Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- Emlet CA (2006). An examination of the social networks and social isolation in older and younger adults living with HIV/AIDS. Health Soc Work, 31(4), 299–308. doi: 10.1093/hsw/31.4.299 [DOI] [PubMed] [Google Scholar]
- Fiori KL, Smith J, & Antonucci TC (2007). Social Network Types Among Older Adults: A Multidimensional Approach. The Journals of Gerontology: Series B, 62(6), P322–P330. doi: 10.1093/geronb/62.6.P322 [DOI] [PubMed] [Google Scholar]
- Gerritsen DL, Steverink N, Ooms ME, & Ribbe MW (2004). Finding a useful conceptual basis for enhancing the quality of life of nursing home residents. Qual Life Res, 13(3), 611–624. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15130025 [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease 2017 HIV Collaborators. (2019). Global, regional, and national incidence, prevalence, and mortality of HIV, 1980-2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV, 6(12), e831–e859. doi: 10.1016/s2352-3018(19)30196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, & Morales LS (2001). The RAND-36 measure of health-related quality of life. Ann Med, 33(5), 350–357. doi: 10.3109/07853890109002089 [DOI] [PubMed] [Google Scholar]
- Huxhold O, Fiori KL, & Windsor TD (2013). The dynamic interplay of social network characteristics, subjective well-being, and health: The costs and benefits of socio-emotional selectivity. Psychology and aging, 28(1), 3. [DOI] [PubMed] [Google Scholar]
- Jansen DA, & von Sadovszky V (2004). Restorative activities of community-dwelling elders. West J Nurs Res, 26(4), 381–399; discussion 400-384. doi: 10.1177/0193945904263010 [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, & Ginindza T (2009). Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care, 21(1), 87–93. doi: 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- Kawachi I, & Berkman LF (2001). Social ties and mental health. J Urban Health, 78(3), 458–467. doi: 10.1093/jurban/78.3.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiely DK, & Flacker JM (2003). The protective effect of social engagement on 1-year mortality in a long-stay nursing home population. J Clin Epidemiol, 56(5), 472–478. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12812822 [DOI] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Lin P, Yu B, Han J, Wang Z, Jia P, & Yang S (2020). Social Capital in Old People Living with HIV Is Associated with Quality of Life: A Cross-Sectional Study in China. Biomed Res Int, 2020, 7294574. doi: 10.1155/2020/7294574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich S, Wang SS, Slindee L, Kraemer S, & Yeh CS (2019). Association of Resilience and Social Networks with Pain Outcomes Among Older Adults. Population health management, 22(6), 511–521. doi: 10.1089/pop.2018.0199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, & Sörensen S (2000). Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychology and aging, 15(2), 187. [DOI] [PubMed] [Google Scholar]
- Poindexter C, & Shippy RA (2008). Networks of older New Yorkers with HIV: fragility, resilience, and transformation. AIDS Patient Care STDS, 22(9), 723–733. doi: 10.1089/apc.2007.0260 [DOI] [PubMed] [Google Scholar]
- Riley ED, Bangsberg DR, Perry S, Clark RA, Moss AR, & Wu AW (2003). Reliability and validity of the SF-36 in HIV-infected homeless and marginally housed individuals. Qual Life Res, 12(8), 1051–1058. doi: 10.1023/a:1026166021386 [DOI] [PubMed] [Google Scholar]
- Schrimshaw EW, & Siegel K (2003). Perceived barriers to social support from family and friends among older adults with HIV/AIDS. J Health Psychol, 8(6), 738–752. doi: 10.1177/13591053030086007 [DOI] [PubMed] [Google Scholar]
- Shippy RA, & Karpiak SE (2005). The aging HIV/AIDS population: fragile social networks. Aging Ment Health, 9(3), 246–254. doi: 10.1080/13607860412331336850 [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, & Reczek C (2010). Social relationships and health behavior across the life course. Annual review of sociology, 36, 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uthman OA, Magidson JF, Safren SA, & Nachega JB (2014). Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep, 11(3), 291–307. doi: 10.1007/s11904-014-0220-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderZee KI, Sanderman R, Heyink JW, & de Haes H (1996). Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med, 3(2), 104–122. doi: 10.1207/s15327558ijbm0302_2 [DOI] [PubMed] [Google Scholar]
- Preamble to the Constitution of WHO as adopted by the International Health Conference (1948).
- Yoo-Jeong M, Haardörfer R, Holstad M, Hepburn K, & Waldrop-Valverde D (2021). Is Social Isolation Related to Emotion Dysregulation and Retention in Care Among Older Persons Living with HIV? AIDS Behav, 25(1), 171–181. doi: 10.1007/s10461-020-02957-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo-Jeong M, Hepburn K, Holstad M, Haardörfer R, & Waldrop-Valverde D (2020). Correlates of loneliness in older persons living with HIV. AIDS Care, 32(7), 869–876. doi: 10.1080/09540121.2019.1659919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavascki AP, & Fuchs SC (2007). The need for reappraisal of AIDS score weight of Charlson comorbidity index. J Clin Epidemiol, 60(9), 867–868. doi: 10.1016/j.jclinepi.2006.11.004 [DOI] [PubMed] [Google Scholar]


