Abstract
Quality discharge teaching prepares patients and families to transition safely from hospital to home. Technology can enhance and support quality discharge teaching by promoting patient family engagement during the transition. The purpose of this mixed method study was to explore clinical nurses’ experience with using engaging parents in education for discharge (ePED), an iPad application to guide quality discharge teaching. Twelve nurses at a large Midwestern Children’s Hospital participated in small focus groups after use of the ePED application and completed a questionnaire on their perception of the acceptability and feasibility of the app. Findings revealed three themes: 1) development and deployment issues focused on the importance of training and support by the study team during implementation; 2) workflow integration centered on the importance of incorporating use of the app into current workflows and to preserve effective communication strategies with parents in order to optimize use in the healthcare setting; and 3) nurses perceived value in the use of the ePED app for beneficial scripting, questions on discharge topics often forgotten, and guidance for complex patients. Results of this study offer insight into key components for consideration when implementing and integrating technology to aid nursing practice.
Keywords: Nursing, discharge teaching, technology
Pediatric health care providers and leaders are constantly faced with the challenges of improving children’s health, enhancing child and family experiences, providing for safe care and managing the costs of health care.1 According to the National Academy of Medicine (formerly the Institute of Medicine) 2 an important focus for improving the health of children is optimizing the discharge transition process, a major emphasis of nursing practice that impacts the overall quality of care.2–6 When parents of hospitalized children report feeling inadequately prepared to implement discharge instructions7 they may have difficulty making the transition from hospital to home and managing their child’s healthcare needs.4, 5, 8 Engaging parents during the discharge process promotes quality discharge teaching and the successful transition from hospital to home.
Health information communication and technology is increasingly used to facilitate nursing care by supporting the engagement of patients and families. Nurses are involved in the development and implementation of new innovations because they understand hospital workflow, as well as the opportunities and challenges present when providing care to patients and families.9 New applications that are accessible and evidence-based are being designed and tested by nurses to improve patient’s understanding and decision making about health care conditions, concerns and processes.
The Engaging Parents in Education for Discharge app (ePED; Lerret, 2020, Milwaukee, WI, US) is one such innovation that was developed and tested in a quasi-experimental study at a large academic Midwest free-standing pediatric hospital.10,11 The ePED app has scripted questions prompting families to think through issues they may encounter once they return home.10,11 Topics include signs and symptoms, medications, appointments, recovery and thinking ahead about family adjustments.10 Nurses received online education and limited in person support by way of a member of the research team rounding on the units to answer questions and trouble shoot technology. While the use of the ePED app enhanced the quality of discharge teaching for parents involved in the study,10,11 the nurse’s perception of the usefulness of the app was only gathered and reported on during the first six weeks of the implementation. 11 Thus, a comprehensive accounting of the experience and perception of the nurses who implemented the ePED app is lacking.
Literature Review
This literature review focuses on the collaborative efforts and previous research by this established team of pediatric nurse scientists that underpins this study. The work examined outcomes of the clinical nurse delivered family discharge preparation intervention (ePED app) 10–12 and the reach, adoption and implementation of the ePED app. 11 The key process components of the Individual and Family Self-Management Theory13 (knowledge and beliefs, self-regulation, and social facilitation) were translated, tested and refined into the current ePED app. Clinical nurses were engaged in each of the studies to provide feedback about the content, delivery and implementation of the different iterations of the application and the potential for integration into their daily workflow.
Research involving development and implementation of health information communication and technology provides insight into the critical nature and importance of collaborating with clinical nurses during design and implementation of applications. 14–16 Failing to engage practicing nurses early in the process of development can derail a project when important clinical workflows are not considered, potentially impacting quality and safety during care delivery and transitions. In a recent integrative review of 33 articles focused on nurses’ use of workarounds and the electronic health record (EHR), usability was a prominent concern and reason for use of workarounds.17 Nurses’ reactions to novel technology can capture both opportunities and barriers to successful development and implementation of applications with the intention to support their clinical processes and to capture their important contributions to patient outcomes.14 End-users’ early and continuous involvement in the development of health care technologies is critical to inform efficient and meaningful adaptations to applications that support documentation, integration, decision-making and clinical processes. 14–16, 18 Ultimately, incorporating the end-user throughout the process will improve the quality and safety of health care delivery.
Studying change management and sustainability of newly implemented processes or technologies is an important and complex challenge. Stakeholders are essential to engage and involve in any change process. A systematic review by Khong et al19 focused on theoretical and conceptual frameworks and the adoption of clinical decision-support systems (CDSS) by health care professionals. Perceived usefulness and ease of use were both critical factors for staff adoption of technology and CDSS.19–22 O’Rourke21 emphasizes the importance of understanding the complexities involved in healthcare system changes and that leaders must understand how activities will enhance stakeholder involvement in the change. Nurses who are implementing innovative technology to facilitate improved patient and family outcomes, should be engaged in both the development and implementation phases of projects.9
Currently, there is a gap in this type of research. A key strategy in the present study was to learn directly from nurses, a primary stakeholder, about their experiences of using the ePED app during their discharge teaching with patients and families. This study provides evidence that by interviewing and surveying staff about the acceptability and implementation of an innovative application, much can be learned to incorporate into future innovative solutions for clinical processes. The purpose of this mixed method study was to explore the experiences, challenges and gain feedback from the clinical nurses who implemented the ePED app.
Theoretical Framework
This project is framed by two conceptual frameworks and a teaching method: Tanner’s Reflective Practitioner Theory,23 the Individual and Family Self-Management Theory,24 and the “Teach-Back” approach to health literacy (Figure 1).25,26 Tanner’s theory emphasizes that reflective nurses notice problems, interpret child and family behavior, respond with individualized action, read the family’s response to nursing actions, and adjust their actions accordingly.23 The reflective nature of Tanner’s theory was the driving force for this study to access nurses experiences while using the application. Combining these conceptual frameworks with an effective teaching method informed the innovative intervention associated with quality discharge preparation of children and families. The refinement of the original version to the currently used ePED application maintains the integrity of the theoretical base of the discharge intervention. 11 The development of the theory-based discharge application is further detailed in a previously published article by Sawin and colleagues.13
Figure 1.
Framework.
Methods
In this mixed method QUAL:quant design study, nurses who participated in the ePED app implementation, participated in small focus groups that used a structured question guide (Figure 2), and completed a questionnaire on their perception of the acceptability and feasibility of the app. This study followed the ePED implementation study focused on the use of an iPad app used with parents of children who were approaching discharge to home after an inpatient hospital stay. 10,11 Study approval was granted by the pediatric hospital’s Institutional Review Board. The study was further supported by the nursing leadership team (Director, Clinical Nurse Specialist and Patient Care Supervisors) of the hospital unit, where the original study was conducted and the ePED app was employed. The unit’s nursing leadership team recommended times when staff, if interested in participating, could be available to take part in the focus groups.
Figure 2.
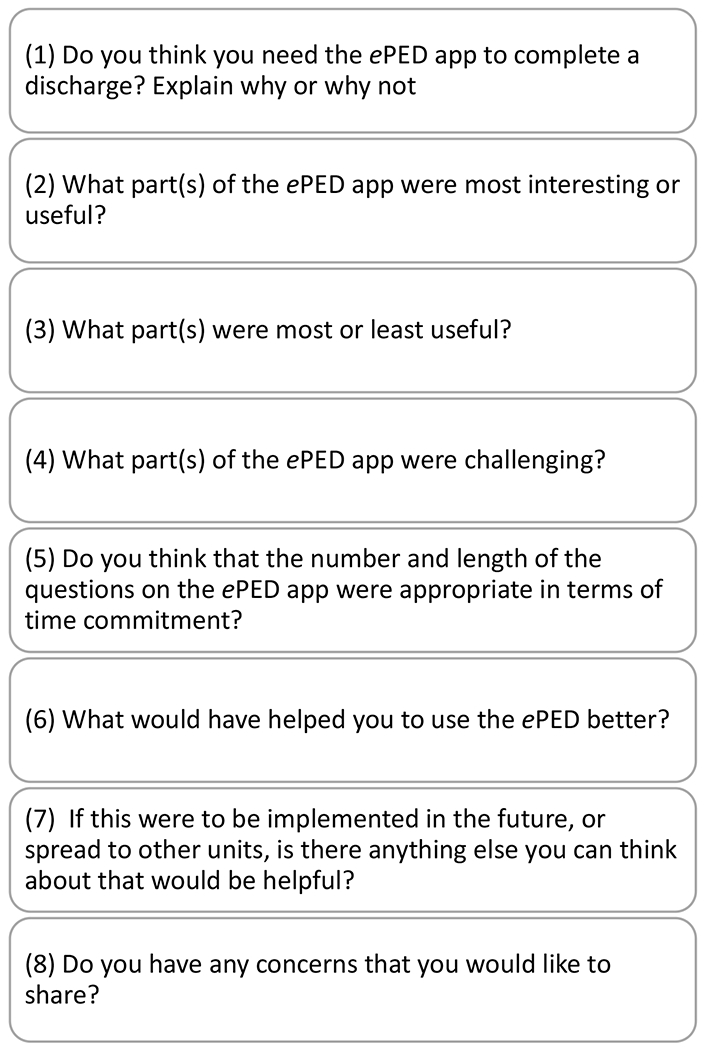
Interview questions.
Nurses on the implementation unit volunteered to be in the study following an email solicitation to discuss their experiences using the ePED app during the study. The interview questions used to explore the nurses’ experience of using the ePED app are presented in Figure 2. The unit Charge Nurse was instrumental in informing the staff nurses that the study team was available and encouraging them to share their experiences of the ePED discharge intervention. In addition to the question guide, demographic data about the nurses were collected to describe the sample.
A quantitative instrument called The Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM) was used to address the nurses’ approval and perception of the appeal of the app along with its suitability for implementation and ease of use.27 Strong psychometric properties were reported in a series of three studies including content validity, discriminant content validity, reliability, structural validity, structural invariance, known-groups validity, and responsiveness to change.27 This free, open-access, 12-item instrument was provided with paper and pencil to the nurses after the interviews were conducted. This measure was intended for use as a structured framework augmented by the details from the qualitative interviews.
The interview room was quiet, private and away from patient contact. Interviews were recorded for future transcription and analysis of themes. After questions were completed, staff were offered a healthy snack to thank them for their time.
Data from the demographic forms and the AIM, IAM and FIM were collated by hand. Descriptive statistics were computed by the study team. Content analysis was used to examine the interviews that were transcribed by an experienced transcriptionist. Two study team members(CK, CG) reviewed the transcripts independently several times for themes before meeting. To assure rigor, independent reviews were initially conducted, and an audit trail was maintained during each team meeting. The two study team members convened once to compare and label themes, discuss commonalities and differences in meaning. Quotes from the transcripts were identified by the two reviewers to illustrate the themes. A third study team member(SL) joined the team and reviewed the transcripts independently for common themes. The three-person study analysis team convened one final time to review and discuss the final themes and quotes to represent the meaning of the final themes. Any differences in opinion or theme assignment between reviewers was discussed until consensus reached.
Results
Demographics
Twelve of 45 staff nurses (27%) in the larger ePED app implementation study volunteered to participate in the nine focus group and individual interviews. The years of experience working as a Registered Nurse (RN) varied, with the majority of the nurses (n=7, 58%) having over 15 years of experience, while 25% (n=3) had up to 5 years’ experience, and followed by 17% (n=2) reported 5 to 15 years of experience. Most nurses were bachelor’s prepared (n=9, 75%), 17 %(n=2) having a master’s degree and 8 % (n=1) with an associate degree. All nurses (n=12, 100%) reported their work experience was in a pediatric health care setting. Ages were reported in groups of ten-year age spans with an even distribution between 26-35 years, 36-45 years and over 46 years old. One nurse was over 56 years of age.
Quantitative data on the nurse perception of the acceptability and feasibility of the ePED app included that a majority of nurses (67%) reported that the ePED app met their approval. The majority of nurses also agreed or completely agreed that the ePED app was possible (75%), applicable (67%) and doable (58%). Participants reported the ePED app seemed easy to use (42%) and implementable (50%). Full results of the acceptability and feasibility of the ePED app are in Table 1.
Table 1.
Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM)
| Questions N=12, No.(%) | Completely Disagree | Disagree | Neither | Agree | Completely Agree |
|---|---|---|---|---|---|
| 1. The ePED app meets my approval. | 0 | 1(8) | 3(25) | 6(50) | 2(17) |
| 2. The ePED app is appealing to me. | 0 | 1(8) | 5(42) | 5(42) | 1(8) |
| 3. I like the ePED app. | 0 | 1(8) | 5(42) | 4(33) | 2(17) |
| 4. I welcome the ePED app. | 0 | 1(8) | 3(25) | 6(50) | 1(8) |
| 5. The ePED app seems fitting. | 0 | 1(8) | 4(33) | 5(42) | 2(17) |
| 6. The ePED app seems suitable. | 0 | 1(8) | 3(25) | 7(58) | 1(8) |
| 7. The ePED app seems applicable. | 0 | 1(8) | 3(25) | 7(58) | 1(8) |
| 8. The ePED app seems like a good match. | 0 | 1(8) | 5(42) | 5(42) | 1(8) |
| 9. The ePED app seems implementable. | 0 | 1(8) | 5(42) | 5(42) | 1(8) |
| 10. The ePED app seems possible. | 0 | 1(8) | 2(17) | 8(67) | 1(8) |
| 11. The ePED app seems doable. | 0 | 1(8) | 4(33) | 6(50) | 1(8) |
| 12. The ePED app seems easy to use. | 0 | 3(25) | 4(33) | 2(17) | 3(25) |
Interview Themes
Three themes emerged: 1) Development and deployment issues focused on the importance of training and support by the study team during implementation 2) Workflow integration centered on the importance of incorporating use of the app into current workflows and to preserve effective communication strategies with parents in order to optimize use in the healthcare setting 3) Nurses found educational value in the use of the ePED app for useful scripting, questions on discharge topics often forgotten, and guidance for complex patients. Subthemes were further identified for each category.
Theme 1: Development and Deployment
The majority of the participants reported on additional factors regarding the implementation of technology into the healthcare setting that they thought were not considered in the use of the ePED in the larger study. These factors included training, implementation and sustainability efforts. Each of these subthemes will be expanded on below.
Training factors.
Nurses described the need to allow adequate time for training, including opportunities for hands-on practice and initial help with implementation that one nurse called “at the elbow support”. For example, one nurse stated, “even though I did the education, I still have to have someone walk me through the first time.” Some nurses working part-time or on weekend or evening shifts reported that they felt they did not have enough practice and never felt comfortable with the use of the ePed prior to the implementation study.
Ensuring nursing staff understood the flexibility of the app when using it with different patients and families was identified as a key learning need to stress in future staff training. Although this information was included in the online training for the nurses, some of the nurses in the focus group reported that they didn’t realize that the app served as a conversation guide and that they had the opportunity to use their own judgement as to whether they needed to ask each question and how to appropriately reflect this process in their documentation. In particular, one nurse noted that she was confused about the “ask/not asked” section of the ePED app, which was intended to capture the questions that the nurses decided to ask, based on their clinical judgement of the individual patient situations. She stated, “Was ‘asked’ mean that did we read each question but if we put ‘not asked’ does that mean we didn’t talk about it but they (the parents) talked about it because we didn’t ask them the question?” Furthermore, one nurse noted “People (the nurses) were afraid to put ‘not asked’ because then it looks like they weren’t doing their job correctly.”
Implementation factors.
Research components during evaluation of technology implementation were another challenge which need to be considered. Nurses stressed their perception that long evaluation surveys can place burden on patients and families. “I just wish it was a little bit shorter so it would be easier for families to participate and not so much demographics”. “I had a lot of parents grumble about the length of their part. I think one of my dad’s just stopped midway and said, ‘I don’t have time for this”. So that was a drawback…the length of the research part”. Select nurses suggested there were too many questions and too many screens for families to complete. “When families answer those other questions (the research portion), that wouldn’t be something that would be built in anymore…I think that was one thing that might have been a little barrier sometimes for a family.” Foreseeing and addressing potential technical issues would also help nurses be successful with new technology implementation. A few nurses shared connectivity issues impaired their ability to use the app on the iPad at times. Weak signals, lags, and poor internet connections left some nurses frustrated at times. One nurse stated, “Sometimes the app would just freeze. Stop working-right in the middle of it!”
Sustainability efforts.
Nurses appreciated the check-ins on the floor by the research team. This action was valued during weekends and evening shifts. “It was really helpful to see someone say “How’s it going? You guys are doing great!’ Just that type of encouragement because it was challenging. I won’t lie. It was challenging. That was helpful,” stressed one nurse. Having the research team actively check-in with the nursing unit provided the needed encouragement and support to continue. Visual posters displayed at the nurses’ station were helpful in showing progress toward completion of enrollment numbers. A nurse recognized these visuals as encouraging, stating, “We had a little chart and we were like, ‘Oh! We’re halfway there! We can do this!”
Theme 2: Workflow Integration
Participants shared the importance of incorporating use of the app into current workflows in order to optimize use in the healthcare setting. This included incorporating technology with pediatric patients and families, timing of delivery, and avoiding redundancies.
Incorporating technology with pediatric patients and families.
Nurses were cognizant of the fact that use of technology can feel impersonal when communicating with others. “Computers can be very impersonal type of communication”. “I would never stand by my computer to do a discharge because you need to sit…look straight at them-face to face”. However, nurses appreciated the use of an iPad for app delivery. “The iPad is nice because it’s something you can hold and be right next to the patient,” a nurse replied. Nurses preferred use of an iPad over a computer, as its portability facilitated more eye-to-eye contact and allowed for sitting with the patient and family, not in front of a computer screen. Another interesting finding related to the frequency of children using iPads for gaming purposes. One nurse reported, “The only problem I had using the iPad is that kids are so used to working with iPads now so the kids were yanking them out of the parent’s hands, trying to find the games on them”. Considering how often iPads are used in the pediatric setting as a distraction device for children needs to be considered when trying to incorporate this technology in a new way.
Timing.
Nurses felt use of the app at the actual time of discharge may not have been the most ideal. Nurses expressed concern families were often ready to go home and wouldn’t have enough time to devote to going through all the questions. At times, nurses didn’t ask families to participate since they perceived that it wasn’t the right time. One participant shared, “At the end of discharge, seems like too much is happening…people [families] are checked out” while another nurse recalled one had to “make sure you had enough time to do it because some families are like ‘I’m going now’. Those were the ones that declined or I made the executive decision and said ‘I’m not going to do this with them because it wasn’t the right time.”
Avoiding redundancies.
Nurses commented some questions were already asked and confirmed upon admission, which then felt redundant to ask again at discharge. Nurses’ current workflows involve using the After Visit Summary (AVS ) from the electronic health record to review discharge information with families prior to discharge. Interestingly, some nurses felt the AVS covered what was needed to be covered and the app questions didn’t line up very well, resulting in it “feeling clunky and didn’t really go with the workflow that we had”. “We’re supposed to go over it with the AVS as we go through, it was very redundant. Like, I went over this with you and then I’m going to ask ‘Tell me how you know your child is not doing well and what will you watch for?’ Well, we just talked about that. And they’d [family] be like ‘what do you want me to say? You just told me’ kind of thing,” a participant described. Others thought the app aligned with the AVS which made it easier to use. “It seemed to follow along with our AVS too, so you felt like you were hitting all the points and double checking yourself with the app,” replied one nurse. Building the questions into the electronic health record (EHR) was seen as another way to reduce duplication of work. Nurses suggested the value in being able to pull up and go through the questions and then document the teaching and interventions done, avoiding the need for duplicate charting. One nurse questioned, “Could it be part of the EHR from the iPad?...you’re charting it as you’re doing it. That would be great because you know you’ve covered everything.”
Theme 3: Perceived Value
Nurses found educational value in the use of the ePED app. The app provided useful scripting, questions on discharge topics often forgotten, and guidance for complex patients.
Scripting was useful.
The nurses in this study shared their appreciation, valuing the comprehensive questions the app guided them to use when delivering discharge education. The questions provided a new way of getting information from families. One nurse reported, “It’s different than just saying ‘What questions do you have?’ because they [parents] don’t think of the questions. But when you say ‘What are you worried about at home?’ it was just a different way [of asking].” The app provided prompts and lead in questions to help guide conversations. “I never thought about saying it this way or talking to the family about it this way,” another nurse explained. Nurses recommended the app as extremely valuable for new nurses with less discharge experience. The app provided guidance as to “this is what a good discharge looks like,” as reported by one participant.
Things I never thought of before.
The questions on the app served as a prompt for inquiring about different aspects of care at home. “There’s really not anything on the AVS [after visit summary] that would prompt me to ask something like this,” a nurse explained. Another stated, “I wouldn’t have thought to ask unless they were worded on here [app].” Nurses found particular value in questions related to follow-up, medications, and the home environment. Questions reminded them to ask more detailed questions to avoid making assumptions. “When you talked about who else will be taking care of the child, I don’t usually ask that, I just assume” said one nurse. Another nurse revealed “sometimes we just assume the parents know what [medication] is for.” The medication section of the app helped nurses keep track of different aspects of medication administration to ensure family understood those pieces. “Going over it so they really understood about dose, the frequency, how they were giving it, how often they could have it…even though it’s [medications] on our AVS, but it just says ‘We gave this and it’s due now. Next dose in…’”, revealed one nurse. Another appreciated the medication questions were “much more in detail and helped us remember” when asking about parent concerns about medications and how they kept track of their child’s medications. Overall, the questions aided in reminding nurses of the necessary topics which needed to be covered. “Some of these questions helped me to remember that I still need to think about…the prompts were helpful because everyone has a routine of questions they ask…this made us stretch out of the box a little more to make sure we are covering all the bases.” One nurse declared, “this is kind of cool that’s there as a prompt because it might not be covered”.
Helpful for complex patients.
Although some nurses viewed some of questions as too detailed for a simple discharge, nurses found use of the app most helpful for complex patients. The questions helped to ensure all necessary topics were covered. One nurse exclaimed, “It’s helpful on some of the complicated discharges that we have to really make sure that you’re covering all the bases.” Using the app provided guidance for review of discharge elements and interventions based on parental responses, such as reinforcement of teaching. Some nurses were also disappointed that the app couldn’t be used for non-English speaking families.
Discussion
The value of nurse feedback about innovative technology and implementation successes and challenges was evident throughout the study and aligns with previous studies.19–20 Important themes evolved about training, potential misunderstandings about the use of the app and how the app could best be fully integrated into the discharge workflow for consistency with more complex patients and support of new staff. Appreciation for research team visibility and support during implementation was clearly conveyed during the small group interviews and should be a take-home message. Discussion of each theme will provide more details for consideration when developing and implementing new technology with nurses in clinical settings.
Development and Deployment
During the interviews, important factors for development and deployment of this electronic discharge iPad application were identified by the nurses. Central was having an opportunity for initial use and on-going practice on the unit until they were comfortable using the application and integrating it in their workflow. This finding is consistent with previous literature identifying nurse perception of the usefulness and ease of use as an important factor in adoption and acceptance of new technology in practice.19–20
Nurses expressed their feedback and concern about using their judgement when learning and using the application in practice. Questions about not using different areas of the application continued to be a question during implementation. Perhaps this finding is related to their usual practice when documenting in the EHR and the need for complete documentation and resolving check boxes within the EHR. There were opportunities that were presented to enhance training and the app itself during the focus group interviews. Typical nursing care has involved a workflow of checking boxes as complete or not complete within the electronic health record for daily tasks. Using the ePED app that involves choice on the part of the nurse and is a new method of capturing nursing actions, so it would be beneficial to stress this innovation in the training so as to reduce confusion.
Important lessons when implementing a unit level project were presented as the nurses expressed how instrumental the support from the research team was during implementation of the application. The encouragement and checking in from members of the research team was helpful to keep the energy moving to use the application and to reach the goals for participants in the study. A consistent theme about the potential burden of the research on families especially during a time of stress and fatigue with hospitalization and the desire to just go home. They expressed how many families declined to complete the research forms and that the number of instruments and time involved should be an important consideration by the research team.
Workflow Integration
Integrating technology but allowing the nurses to maintain connections with families during such a critical time was addressed by many of the nurses. Nurses shared that they wanted to protect the time and intimacy they needed to have important conversations about what would create safety and comfort in asking important questions before this potentially vulnerable transition home. They wanted to be sure that the technology remained an adjunct instrument and not an intruder or barrier for effective communication.
The timing of the intervention continues to emerge as a question and potential adjustment in the intervention for the future. Opportunities to use the application before the final day of discharge were discussed by some of the nurses interviewed. Nurses were acutely aware of the vulnerability of parents’ attention and focus when approaching the time of discharge. Families expressed that they just needed to get home and that considering research at this time was simply too much to ask of them. This is a recurring theme from prior research and needs to be seriously considered with any further implementation.12 However, effective use of the ePED app is linked to better quality discharge teaching and better patient outcomes10 so it is imperative that training and implementation of the ePED is refined to promote its use.
Integrating the application with current EHR workflow and completion of discharge paperwork created some clumsiness and feelings of redundancy in certain areas such as medication knowledge and signs and symptoms to watch for at home. This recommendation is consistent with previous studies that have identified that engaging nurses early in the development and implementation of technology provides critical information about usability that can lead to future adoption of the application, fewer workarounds and integration into workflow.14–18 Nurses discussed the need to integrate use of the application with several other current systems in place so that it flows and doesn’t feel redundant. Resolving the prior issue of timing might facilitate the streamlining of processes.
Perceived Value
The perceived value was high among many of the nurses who pointed out the utility of the scripting for both new and experienced nurses. Nurses also reported value in being pro-active by asking parents to think forward about being at home with their child and family after discharge. They valued the comprehensive and holistic framework that provided a standardized approach for this important aspect of the discharge process. 12 Many nurses expressed that after getting comfortable with the application they were able to create a meaningful conversation with families who were approaching a challenging time during their child’s recovery. Nurses discussed there were questions they wouldn’t necessarily have asked without the scripting that they found to be very valuable and important, such as who was going to be caring for the child at home when the parent returned to work.
Another recurring theme from prior research was how the ePED application was highly useful for the more complex patients.8,12 Alternatively, several nurses reported the ePED application was too comprehensive for patients who were less complicated and had a brief hospitalization. This highlights the importance of nursing judgement to address certain questions or fields within the application based on each unique patient and family situation.
Limitations
This study involved a single inpatient unit resulting in a limited sample size. Despite the small sample size, we were able to reach saturation. Another potential limitation is that nurses were asked to recall experiences as opposed to being asked during study enrollment. However, feedback was detailed and thoughtful. While much of the feedback focused on challenges with the application, there were both positive aspects and challenges offered throughout the interviews.
Implications for practice
Integrating documentation completed by the nurse as part of the ePED app within the hospital electronic health record is critical for sustainability. Collaborating with the hospital’s Information Services electronic health record team will be an important next step to eliminate double documentation in the electronic health record for nurses. Continued sensitivity to the workflow of the staff nurse is imperative in any innovation intended for sustainability. A broader reach with this app will also be an important next step to utilize on different types of inpatient units and to also garner a larger sample to more thoroughly assess patient outcomes and utilization of healthcare resources. Further exploration before full implementation should include the parents and patient’s perspective on the contributions and challenges from using the application during this important time during hospitalization.
Conclusion
This study with nurses involved in technology development and implementation provides valuable insight into the important elements of technology integration within existing EHRs. Training and support are essential for nurses to have a full understanding of the intention, use of the application and how to manage potential issues with workflow integration. Providing feedback loops for adjustments in training and support during implementation are a critical component for any research team seeking full implementation of an intervention. The perceived value of the application to improve outcomes and enhance practice is an important indicator that there is merit and feasibility in moving this application for safe and quality discharge forward within pediatric hospitals.
Conflicts of Interest and Source of Funding
This work was supported by the CTSI Pilot Collaborative Clinical and Translational Research Grants Program National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), Award Number UL1TR001436. Additional funds were provided by the Pediatric Nursing Research Consortium, a joint project of Children’s Hospital of Wisconsin, University of Wisconsin Milwaukee College of Nursing and Marquette University College of Nursing.
Contributor Information
Carol G. Klingbeil, College of Nursing, University of Wisconsin-Milwaukee.
Cori Gibson, Children’s Wisconsin.
Norah L. Johnson, College of Nursing, Marquette University.
Michele Polfuss, College of Nursing, University of Wisconsin-Milwaukee and Children’s Wisconsin.
Karen Gralton, Children’s Wisconsin.
Stacee M Lerret, Medical College of Wisconsin.
References
- 1.Bowles JR, et al. The role of the nurse leader in advancing the Quadruple Aim. Nurse Leader. Aug. 2018; 16(4): 244–248. doi: 10.1016/j.mnl.2018.05.011. [DOI] [Google Scholar]
- 2.Institute of Medicine. The future of nursing: leading change, advancing health. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- 3.Lerret SM, Johnson NL, Haglund KA. Parents’ perspectives on caring for children after solid organ transplant. Journal for Specialists in Pediatric Nursing. Feb 2017; 22(3): 1–8. doi. 10.1111/jspn.12178 [DOI] [PubMed] [Google Scholar]
- 4.Lerret SM. Discharge readiness: an integrative review focusing on discharge following pediatric hospitalization. Journal for Specialists in Pediatric Nursing. Oct 2009;14(4):245–255. doi: 10.1111/j.1744-6155.2009.00205.x. [DOI] [PubMed] [Google Scholar]
- 5.Lerret SM, Weiss ME. How ready are they? Parents of pediatric solid organ transplant recipients and the transition from hospital to home following transplant. Pediatric Transplantation. 2011;15(6):606–616. doi: 10.1111/j.1399-3046.2011.01536.x. [DOI] [PubMed] [Google Scholar]
- 6.Toomey SL, Zaslavsky AM, Elliott MN, et al. The development of a pediatric inpatient experience of care measure: Child HCAHPS. Pediatrics. 2015;136(2):360–369. doi: 10.1542/peds.2015-0966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glick AF, Farkas JS, Nicholson J, et al. Parental management of discharge instructions: A systematic review. Pediatrics. 2017;140(2):e20164165. doi: 10.1542/peds.2-16-4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lerret SM, Weiss ME, Stendahl GL, et al. Pediatric solid organ transplant recipients: transition to home and chronic illness care. Pediatric Transplantation. 2015;19(1):118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roddy L, Polfuss M. Employing design thinking methods in nursing to improve patient outcomes. Nursing Forum. 2020;55(4):553–558. doi: 10.1111/nuf.12461. [DOI] [PubMed] [Google Scholar]
- 10.Lerret SM, Johnson NL, Polfuss M, et al. Using the engaging parents in education for discharge (ePED) iPad application to improve parent discharge experience. Journal of Pediatric Nursing. 2020;52:41–48. doi: 10.1016/j.pedn.2020.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson NL, Lerret S, Klingbeil CG, et al. , M. Engaging parents in education for discharge (ePED): evaluating the reach, adoption & implementation of an innovative discharge teaching method. Journal of Pediatric Nursing, 2020;54:42–49. doi: 10.1016/j.pedn.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiss ME, Sawin KJ, Gralton K, et al. Discharge teaching, readiness for discharge, and post-discharge outcomes in parents of hospitalized children. Journal of Pediatric Nursing. 2017;34:58–64. doi: 10.1016/j.pedn.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Sawin KJ, Weiss MA, Johnson N, et al. Development of a self-management theory guided discharge intervention for parents of hospitalized children. Journal of Nursing Scholarship. 2017;49(2):202–213. doi: 10.1111/jnu.12284. [DOI] [PubMed] [Google Scholar]
- 14.Kent B, Redley B, Wickramasinghe N, et al. Exploring nurses’ reactions to a novel technology to support acute health care delivery. Journal of Clinical Nursing. 2015;24(15-16): 2340–2340–2351. doi: 10.111/jocn.12881. [DOI] [PubMed] [Google Scholar]
- 15.Lee S, Jeon MY, & Kim EO .Implementation of structured documentation and standard nursing statements: Perceptions of nurses in acute care settings. CIN: Computers, Informatics, Nursing. 2019;37(5):266–275. doi:1097/CIN.0000000000000510 [DOI] [PubMed] [Google Scholar]
- 16.Müller-Staub M, de Graaf-Waar H, Paans W. (2016). An internationally consented standard for nursing process-clinical decision support systems in electronic health records. CIN: Computers, Informatics, Nursing. 2016;34(11):493–502. doi: 10.1097/CIN0000000000000277. [DOI] [PubMed] [Google Scholar]
- 17.Fraczkowski D, Matson J, & Lopez KD. Nurse workarounds in the electronic health record: An integrative review. Journal of the American Medical Informatics Association. 2020;27(7):1149–1165. doi: 10.1093/jamia/ocaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smailes PS, Zurmehly J, Schubert C, Loversidge JM, Sinnott LT. An electronic medical record training conversion for onboarding inpatient nurses. CIN: Computers, Informatics, Nursing. 2019;37(8):405–412. doi: 10.1097/CIN.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 19.Khong PCB, Holroyd E, Wang W. A critical review of the theoretical frameworks and the conceptual factors in the adoption of clinical decision support systems. CIN: Computers, Informatics, Nursing. 2015;33(12): 555–570. doi: 10.1097/CIN.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 20.Bagot K, Moloczij N, Arthurson L, et al. Nurses’ role in implementing and sustaining acute telemedicine: A mixed‐methods, pre‐post design using an extended technology acceptance model. Journal of Nursing Scholarship. 2020;52(1):34–46. doi: 10.1111/jnu.12509. [DOI] [PubMed] [Google Scholar]
- 21.O’Rourke T, Higuchi KS, Hogg W. Stakeholder participation in system change: A new conceptual model. Worldviews on Evidence Based Nursing. 2016;13(4),261–269. doi: 10.1111/wvn.12165. [DOI] [PubMed] [Google Scholar]
- 22.McKenzie L, Shaw L, Jordan JE, et al. Factors influencing the implementation of a hospital-wide intervention to promote professionalism and build a safety culture: a qualitative study. The Joint Commission Journal on Quality and Patient Safety. 2019;45(10):694–705. doi: 10.1016/j.jcjq.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Tanner CA. Thinking like a nurse: a research-based model of clinical judgment in nursing. Journal of Nursing Education. 2006;45(6):204–211. doi: 10.3928/01484834-20060601-04. [DOI] [PubMed] [Google Scholar]
- 24.Ryan P, Sawin KJ. The Individual and Family Self-Management Theory: background and perspectives on context, process, and outcomes. Nursing Outlook. 2009;57(4):217–225.e6. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peter D, Robinson P, Jordan M, Lawrence S, Casey K, Salas-Lopez D. Reducing readmissions using teach-back: enhancing patient and family education. Journal of Nursing Administration. 2015;45(1):35–42. doi: 10.1097/NNA.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 26.Yen PH, Leasure AR. Use and Effectiveness of the Teach-Back Method in Patient Education and Health Outcomes. Federal Practitioner. 2019;36(6):284–289. [PMC free article] [PubMed] [Google Scholar]
- 27.Weiner BJ, Lewis CCN, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implementation Science. 2017;12:108. 10.1186/s13012-017-06353. [DOI] [PMC free article] [PubMed] [Google Scholar]


