Abstract
Objectives
Transferred emergency general surgery (EGS) patients experience worse outcomes than directly admitted patients. Improving communication during transfers may improve patient care. We sought to understand the nature of and challenges to communication between referring (RP) and accepting (AP) providers transferring EGS patients from the transfer center nurse’s (TCN) perspective.
Methods
Guided by the Relational Coordination Framework, we interviewed 17 TCNs at an academic medical center regarding (in)efficient and (in)effective communication between RPs and APs. In-person interviews were recorded, transcribed, and managed in NVivo. Four researchers developed a codebook, co-coded transcripts, and met regularly to build consensus and discuss emergent themes. We used data matrices to perform constant comparisons and arrive at higher-level concepts.
Results
Challenges to ideal communication centered on the appropriateness and completeness of information, efficiency of the conversation, and degree of consensus. TCNs described that RPs provided incomplete information due to a lack of necessary infrastructure, personnel, or technical knowledge; competing clinical demands; or a fear of the transfer request being rejected. Inefficient communication resulted from RPs being unfamiliar with the information APs expected and the lack of a structured process to share information. Communication also failed when providers disagreed about the necessity of the transfer. APs diffused tension and facilitated communication by embracing the role of a “coach,” negotiating “wait-and-see” agreements, and providing explanations of why transfers were unnecessary.
Conclusions
TCNs described numerous challenges to provider communication. Opportunities for improvement include sharing appropriate and complete information, ensuring efficient communication, and reaching consensus about the course of action.
INTRODUCTION
Transferred emergency general surgery (EGS) patients are a vulnerable patient population who have worse outcomes than their directly admitted counterparts.1–3 Transferred EGS patients experience significantly increased in-hospital morbidity, mortality, lengths of stay, and cost, which persist after risk adjustment.1 Previous research examining contributing factors to these poor outcomes has focused on patients’ demographics (e.g., age, insurance status, income), clinical features (e.g., diagnoses, comorbidities), and hospital characteristics (e.g., bed size, geographic region).1–6 Qualitative aspects of the transfer that likely influence patient outcomes, such as communication between providers, have been less rigorously studied.
Poor outcomes among patients transferred within a single institution have been partly attributed to poor communication between providers.7,8 Improving communication during intrahospital transfers prevents medical errors, improves patient outcomes, and has been identified as a leading patient safety goal by The Joint Commission.7–11 Unlike communication during intrahospital transitions of care,12 there is a paucity of research on the communication that occurs during interhospital transfers and the potential impact of that communication on patient outcomes. There is preliminary evidence demonstrating that improved communication prior to interhospital transfers may prevent up to 70% of adverse events among transferred critically ill patients5 and may lead to better patient outcomes.13,14
Transfers of patients between acute care hospitals typically involve a series of conversations (Figure 1). At most hospitals, referring providers [RPs (typically physicians or advance practice practitioners)] call the transfer center of the accepting hospital and speak to the transfer center staff, often a nurse, who gathers initial information.15 Transfer center nurses (TCN) provide a brief summary to accepting providers (APs) and facilitate and participate in a conversation with the two providers.
Figure 1:
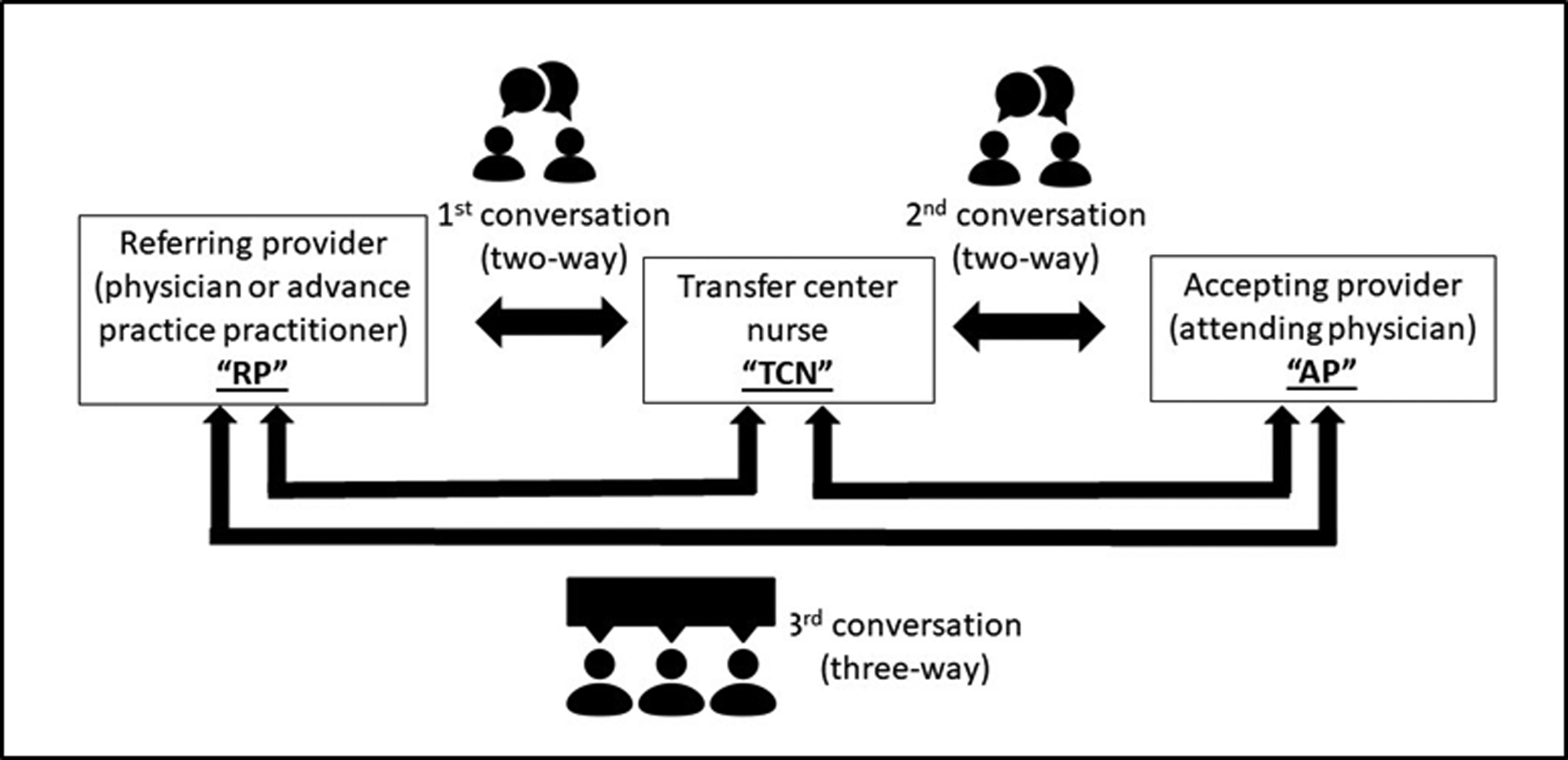
Conversations between Referring Providers, Accepting Providers, and Transfer Center Nurses during requests for interhospital transfer
We hypothesize that improving communication between providers during interhospital transfers of EGS patients may improve patient care. Our long-term goal is to gain a thorough understanding of the factors that facilitate or impede providers’ communication during transfer calls. Understanding the nature of these interactions and identifying challenges providers experience will inform strategies to improve this communication. Because TCNs coordinate calls between RPs and APs, they have a global view of providers’ conversations about interhospital transfers. Thus, we began this line of study by collecting TCNs’ insights regarding providers’ conversations discussing transfers of EGS patients. The data presented here is based on the TCNs’ perspective; future phases of this work will explore the perspectives of RPs and APs.
METHODS
Conceptual framework
Our data collection and analysis was guided by the Relational Coordination Framework (RCF) (Figure 2).16–18 The RCF examines how effective coordination is best carried out within and across interdependent institutions. The RCF is a theory widely applied to healthcare delivery including quality and continuity of care.19–21 The RCF builds on three relationship dimensions (shared goals, shared knowledge, and mutual respect) and four aspects of communication (frequency, timeliness, accuracy, and problem-solving). According to the RCF, the quality of relationships and communication among workers interacts through “mutually reinforcing dynamics” to impact effective coordination. The RCF posits that relationships are shaped by actors’ levels of shared knowledge about the work process (i.e., how each task/role is related) as well as the degree to which actors share goals and mutual respect. Grounded by the RCF, we sought to (1) understand the nature of provider communication by applying the dimensions of shared knowledge, shared goals, and mutual respect, and (2) examine how these elements influence one another as well as communication regarding transfers.
Figure 2:
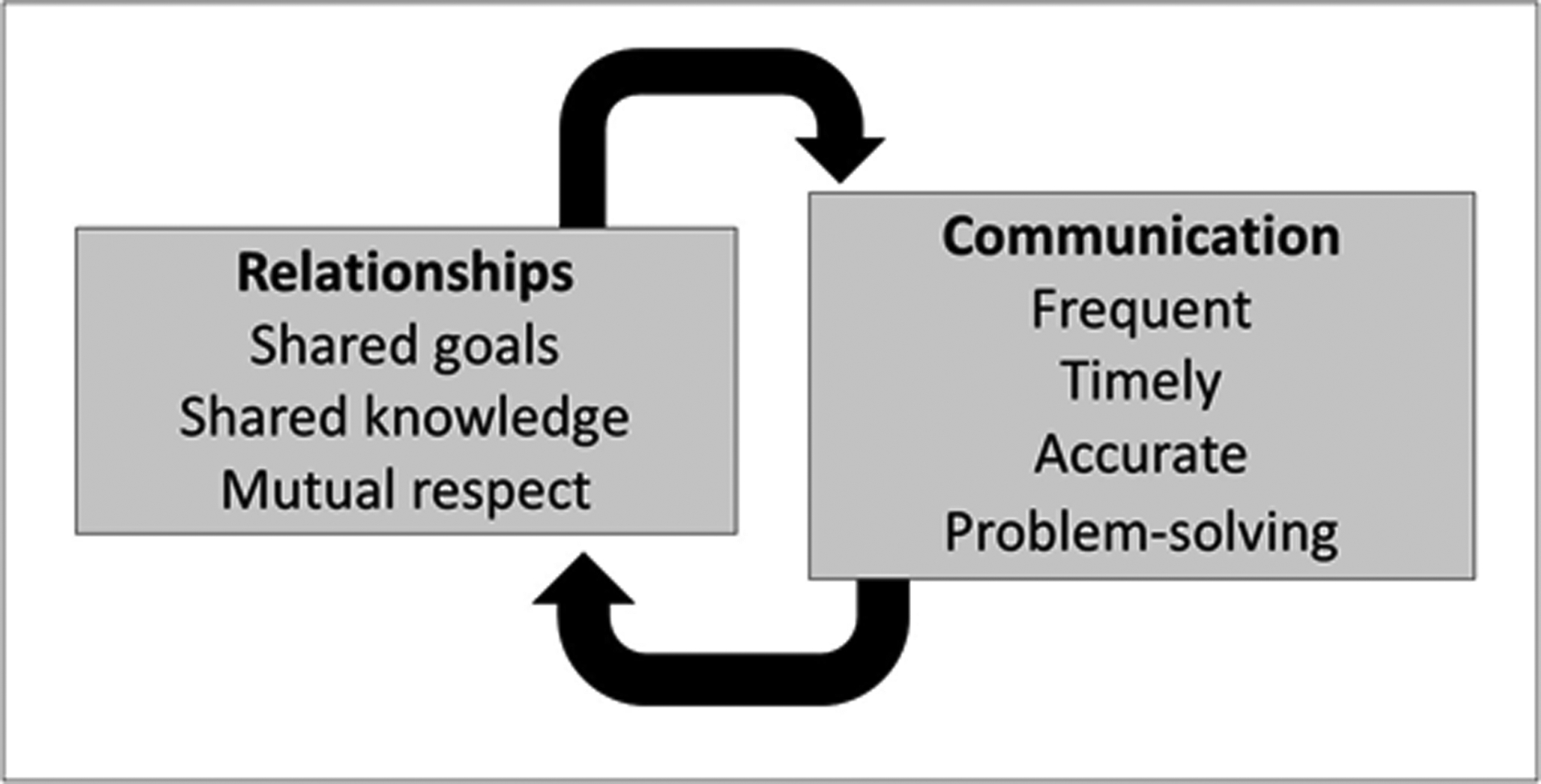
The Relational Coordination Framework
Data collection
This study occurred at a tertiary medical center from March to August, 2019. We invited all TCNs to participate by email and through in-person visits. We interviewed 17 of 24 current or previous TCNs. Guided by the RCF, we developed an interview script eliciting descriptions of (in)efficient and (in)effective communication between RPs and APs discussing interhospital transfers of EGS patients. Trained researchers conducted in-person interviews lasting approximately 60 minutes. TCNs filled out a demographic questionnaire. Participants were compensated $100. Interviews were audio recorded, transcribed verbatim, de-identified, and uploaded in NVivo for data management. This study was approved by the University of Wisconsin-Madison Institutional Review Board.
Data Analysis
Data were analyzed using directed content analysis.22 The analysis team consisted of a surgeon, health services researchers, and qualitative experts. We developed a codebook based on RCF elements as well as emergent themes. Emergent themes were characterized as any topics within the data that were not captured by the framework elements. We captured these emergent themes (e.g., “strategies for a successful communication,” “strategies to diffuse tension”) as new codes. At least three researchers coded each transcript individually. The team met regularly to review all codes, to achieve consensus and accuracy, and to discuss patterns and core meanings of themes. We took extensive notes and created memos to document themes. For this study, we examined all data associated with codes relating to the elements of RP and AP communication (20 main codes and 22 sub-codes). We used data matrices23 organized by study participant, code, argument, and representative quote to perform constant comparisons24 and arrive at higher-level concepts.
RESULTS
Participant Demographics
A total of 17 TCNs were interviewed. Approximately 75% and 50%, respectively, had experience working in inpatient care and emergency department settings. The range of experience with direct patient care was between 5 to 35 years; their experience working at the transfer center ranged between 4 months and 17 years. More than 70% of TCNs had a bachelor’s degree or higher.
Ideal Referring and Accepting Provider Conversations
To begin, we asked TCNs to describe their observations of an ideal conversation between RPs and APs to ground our analysis. TCNs consistently described “ideal” communication as RPs providing a clear, concise presentation that precisely described the patient’s condition (including previous treatments and procedures), encompassed a “complete work-up” with images and lab results, and explicitly stated the reason for transfer. Information TCNs frequently alluded to that should be included in RPs’ presentations is listed in Table 1. TCNs described APs as ideally being respectful and patient as well as letting RPs talk without interrupting. According to TCNs, because APs were unable to physically examine patients, APs relied on RPs’ presentations to make medical decisions.
“The biggest challenge, is just in as little time as possible, because everybody’s busy, understanding a clear clinical picture, so that an appropriate judgement is made about the patient’s coming or not.”
(TCN 11)
TABLE 1.
Information that transfer center nurses identified that referring providers should include in their presentations when requesting transfer of an emergency general surgery patient
| Two or more patient identifiers |
| Working diagnosis (if known) |
| Reason for transfer |
| History of present illness |
| Relevant past medical or surgical history |
| Hemodynamic stability or instability |
| Physical exam findings |
| Workup completed (e.g., labs, imaging [final reads and images if available]) |
| Interventions at referring hospital (e.g., antibiotics, nasogastric tube, resuscitation, procedures) |
| Location of patient at referring hospital (i.e., emergency room versus inpatient status [general, intermediate, or intensive care]) |
Although RP-AP conversations often flowed as described, situation-specific elements led to challenges in communication. TCNs’ descriptions of these challenges centered on: (1) appropriateness and completeness of the information provided, (2) efficiency of communication, and (3) degree of consensus between providers about the decision to transfer. Figure 3 summarizes these results.
Figure 3:
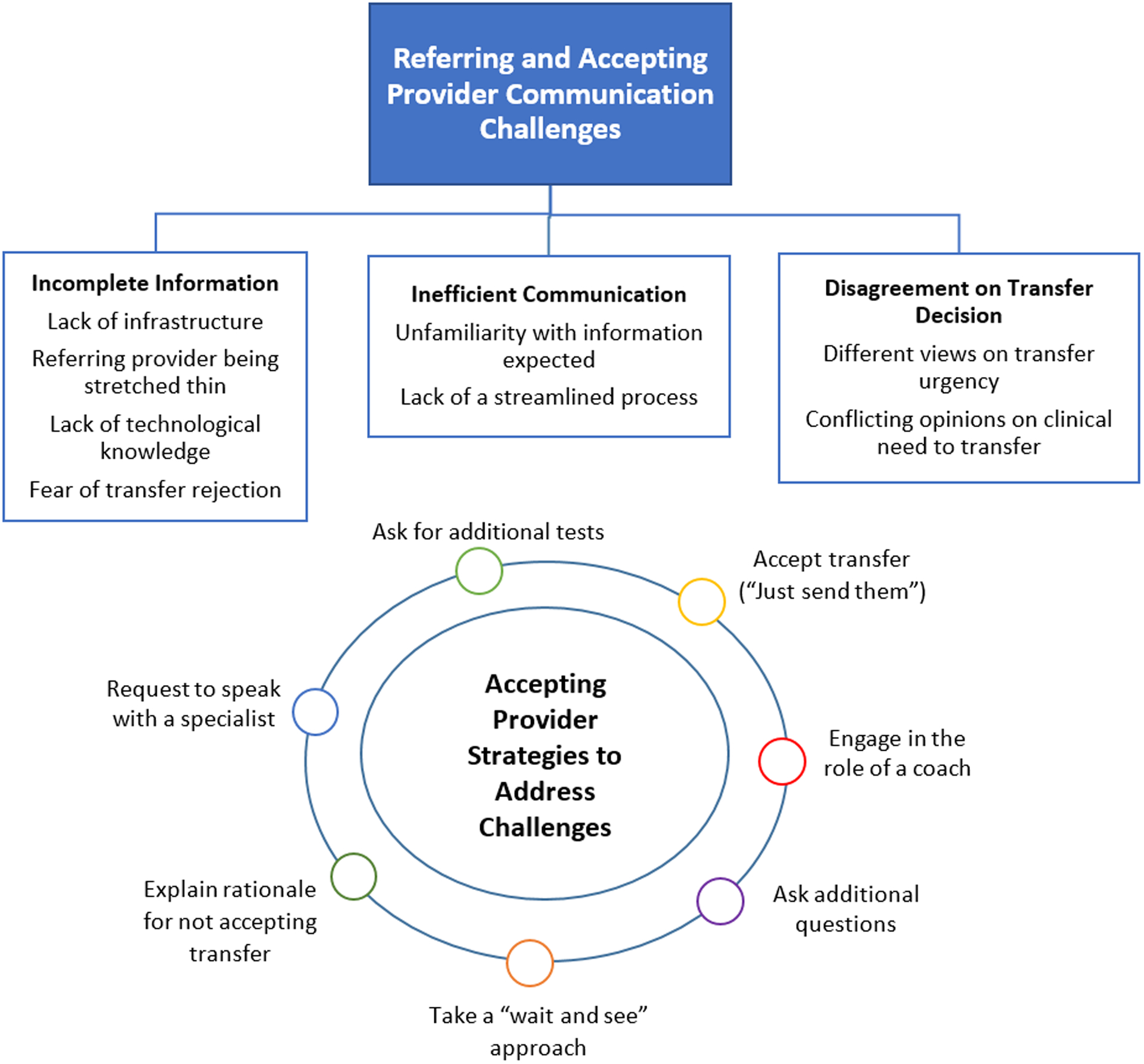
Visual representation of the results of this study
Appropriateness and completeness of the information
TCNs outlined several scenarios when RPs presented inappropriate or incomplete information. Several reasons for not having the necessary information were described by TCNs: (1) limited infrastructure and personnel to complete the work-up (e.g., imaging studies), (2) RPs being overextended (e.g., managing a crowded emergency room) and placing the call prior to personally examining the patient or gathering the information, (3) RPs lacking the familiarity or knowledge to send images electronically to the accepting hospital despite completing the workup, and (4) RPs not including certain details about patients’ conditions (e.g., a history of chemical dependence) out of fear that APs would reject the transfer based on this information.
“Part of it could be that they don’t want to give the information ‘cause they’re worried we won’t take the patient based on some piece of information.”
(TCN 22)
TCNs reported that not sharing enough information or leaving out necessary information resulted in a number of obstacles for all parties. TCNs relied on this information to connect RPs to the appropriate APs. When TCNs lacked information, they either asked RPs to call back (e.g., call back after images were pushed) or connected the providers without them having the necessary information. In the latter situation, APs spent considerable time asking questions to obtain a clear picture of the patient’s condition to decide whether the transfer was necessary. In both cases, conversations took longer to complete, which ultimately delayed care.
When RPs did not provide the necessary information, APs asked RPs to conduct additional tests (e.g., further labs or imaging) to gain a better picture of the patient’s condition. APs also asked to speak to the specialist or surgeon taking care of the patient to provide critical information. TCNs noted that because surgeons speak the “same language” (i.e., they recognized and were able to describe unique elements of the patient’s condition) having two specialists on the call could facilitate ideal communication.
When RPs did not provide essential information, APs also pushed back on the transfer and asked for more details about the patient or the referring facility’s resources to decide whether the transfer was out of necessity or a “dump.” TCN described “dumps” as cases where APs believed that the referring hospital should be able to care for the patient, but RPs sought a transfer for reasons other than patient request or “true” clinical need (e.g., no surgical coverage, no access to imaging). In some cases, TCNs recounted that APs asked RPs if they requested the transfer because caring for the patient was inconvenient.
“We have some EGS surgeons that will call them out on it. Like, ‘So, are you just trying to give us this patient ‘cause it’s Friday night right before a holiday? Or do you actually feel like you can’t manage this patient. ‘Cause we’re not gonna do anything for this patient over the weekend either.’”
(TCN 8)
In situations where the RP completed the workup to the extent they were able before calling for a transfer and was honest and forthright about the clinical status of the patient and the reason for transfer, it promoted trust between all parties and helped the process go more smoothly.
“…They have all the relative lab work back. They have the appropriate imaging. They are forthcoming with their reason for transfer, either it’s bowel perforation, they don’t have beds, they don’t have a surgeon. And I have all this information up front. I can call my provider, give them the short story.”
(TCN 6)
Efficiency of communication
Another element that contributed to the quality of communication according to TCNs was the efficiency of the conversation (i.e., how much and in what order the information was shared). TCN noted that efficient communication was a key factor in successful AP-RP communications.
“[Efficient] conversation is very directed. You know exactly what we need to know, nothing more, nothing less.”
(TCN 19)
Excessive amounts of information on the patient’s condition or details of previous treatments that did not pertain to the acute illness created a “word salad” during RPs’ presentation. When RPs provided unnecessary information, APs had difficulties sorting through and identifying critical information. APs missed information that had already been shared, causing RPs to repeat themselves. TCNs emphasized that a concise presentation minimized the high cognitive load carried by the providers during these conversations.
“…if it comes out as like a giant word salad, like I’m sitting there documenting on the call while they’re talking, and I’ll hear them say something and I’ve even typed it, and then I’ll hear our surgeon ask about something that was already shared, I think just ‘cause it was so much information all at once.”
(TCN 27)
TCNs posited several reasons why RPs shared excess information. TCNs described the absence of a streamlined process to concisely deliver information. Lacking an understanding of how APs utilized the information provided, RPs tended to include as much detail as possible assuming that APs would be well-informed. Additionally, because individual APs asked for different amounts of information, RPs were not be able to anticipate the information APs expected. This led to inconsistencies regarding the amount of detail RPs included in their presentation.
“Maybe the last time that Doctor A called and spoke to [AP], they just said, ‘Sure, send them along.’ And they didn’t need anything, they didn’t want anything. So maybe this follow-up interaction they’re having where someone’s asking for some objective evidence of condition is abnormal to them. So, maybe just a difference in providers.”
(TCN 28)
The order in which information was presented also affected the efficiency of the communication. TCNs stated that RPs were inclined to present the patient’s story chronologically. Although at times chronological details helped paint a clear picture, in situations where APs were overburdened and under time constraints (e.g., starting an emergency operation), it became more important to be brief. In these situations, RPs should focus on the critical points pertaining to the patient’s current condition, especially the reason for transfer, rather than giving a chronological history of the patient’s story.
“…it doesn’t seem like there’s really a template for how they share information or what information they share, so it does come out as a little bit like…narrative-y. So it’s sort of in chronological order, but they talk about some labs and then they talk about something else, and then they talk about other labs, and so I think pieces sort of get lost. Because it’s not organized in a super meaningful way to the surgeon who wants certain elements of information.”
(TCN 27)
Consensual decision making
Even when appropriate information was shared efficiently, TCNs noted that RP-AP communication suffered when they disagreed about the need for transfer. When RPs were certain that a transfer was necessary but received pushback from APs or were questioned about the reason(s) for transfer, they pressured APs to accept the transfer, got defensive, asked to talk to someone higher up, called a different hospital, or called back later to talk to a different AP.
TCNs described the various ways APs responded to reduce or avoid tension when initially refusing a transfer (Figure 3). As one approach, APs embraced the role of a “coach” and educated RPs about interventions that should be done if the patient stayed at the referring hospital. This occurred when APs were convinced that RPs had the infrastructure and resources necessary to care for patients.
“I think [APs] try to redirect in a sense and try to get them to do as much as they can in their own facility. And, look at things in a different way or try to do as much as they can.”
(TCN 17)
As a second approach, APs negotiated a “wait and see” agreement with RPs. Here, APs refused the transfer but promised to revisit the decision, especially if the patient’s condition worsened.
“Sometimes [AP]’ll say, ‘Wait ‘til tomorrow. Get the images that we need. And then call me back and we’ll see where we are from there.’ You know, ‘give the patient 24 hours to rebound, get more imaging, labs and things like that, and then we’ll reassess the situation tomorrow’…And a lot of times in those cases, the patients end up staying at the referring facility.”
(TCN 18)
A third approach by APs was to provide detailed explanations of their rationale for why the patient did not need to be transferred. TCNs described how APs explained why they were not concerned about the patient’s condition or why the situation was not urgent. APs reinforced that they would not do anything differently than what the RPs described, reassuring RPs and giving them peace of mind. In these situations, APs usually adopted a firm stance on their decision while at the same time keeping the conversation professional.
“Sometimes [RP] will say, ‘Fine. If you can’t take the patient, we’ll just send the patient somewhere else.’ And so, usually, then our doctors will say, ‘Well that’s not the case. It’s not that we don’t want to take your patient, but there’s nothing we’re gonna be doing for this patient right now…’cause it’s not an emergency.’”
(TCN 8)
A fourth approach by APs was to acquiesce to transfer requests that may not be considered medically urgent or necessary. In situations where RPs became “pushy” about the transfer or were not appeased by the aforementioned strategies, APs may accept the patient to avoid confrontation. In these conversations, APs told RPs to “just send the patient to ER” for an evaluation and assessment and took an approach of “we’ll figure it out when they get here.”
“If they have like a sketchy story, or the provider’s not giving them a good clinical picture of the patient, our providers will say, ‘Yes, send it to the ED so we can evaluate the patient and see what service is appropriate for the patient.’ That’s their go-to line for, ‘Okay, just forget it. Send them over, shut up.’ [Laughs]”
(TCN 18)
DISCUSSION
A conversation between RPs and APs is required before patients are transferred between hospitals at most transfer centers in the United States (84%).15 Despite the importance of these conversations to the care of this vulnerable patient population, little attention has been directed toward improving RP and AP communication. To begin to understand deficiencies in provider communication, we examined the perspectives of TCNs, the primary organizers of conversations regarding transfers. We focused on the elements that challenged or facilitated efficient and effective communication between providers. Our results identified several challenges to provider communication including factors related to appropriateness and completeness of information, inefficiencies in communication, and lack of consensus about the course of action. Understanding challenges and facilitators of this communication from the TCN vantage provides a starting point from which to explore the insights and perspectives of RPs and APs in future interviews.
Communication regarding transfers of care involves more than just sharing the patient’s history and workup. In addition to the content of the conversation, contextual factors at both the institutional level (e.g., image sharing capabilities) and provider level (e.g., providers juggling competing duties) must be considered to optimize communication. The RCF characterizes the micro-dynamics of coordination, particularly for scenarios, such as interhospital transfers, that are “highly interdependent, uncertain, and time-constrained.”16 Our results confirm that the micro-dynamics of coordination are substantial contributors to the challenges that occur during interhospital transfer communication. The RCF posits that friction can be mitigated when providers are connected through relationships grounded by shared knowledge, shared goals, and mutual respect.
Per TCNs, one important component missing from RP-AP communication was providers’ knowledge of the systems or processes at their counterpart’s hospital. For example, despite what was expected by the transfer center, RPs did not always provide a patient summary to TCNs. This was mainly due to unfamiliarity with the TCN’s role and how TCNs use this information to triage the call to the correct AP. Similarly, APs were not aware of the available infrastructure and staffing at referring hospitals, leading to mistaken expectations of the care referring hospitals could provide. Establishing a shared knowledge of resources and practices at the respective hospitals may enable providers to understand the overall work process and start the conversation on a common ground.
Another critical challenge to sharing accurate information efficiently was the absence of a structured communication process. Inconsistencies in the amount and detail of information expected by APs frustrated RPs. Without a structured process, RPs shared too much or too little information. In some cases, the lack of structure in the RP’s presentation made it harder for the AP to identify the information needed to make the transfer decision. A better understanding of how to help RPs tell a cohesive story tailored to the patient’s condition with the appropriate level of detail and in a manner that facilitates understanding by the AP is needed. This joint approach can be used to develop a partnership to reach consensus regarding the treatment plan and the shared goal of improved patient outcomes.
Provider expectations also influenced the communication between RPs and APs. Being the tertiary care center in the region and having expansive infrastructure and expertise, there can be pressure to “accept all patients.” Per the TCNs, some RPs assumed that all patients, even those that could safely be cared for at the referring hospital, would be accepted for transfer. However, TCNs noted that accepting all transfer requests could adversely impact overall patient health and safety due to capacity issues and delayed transfers of complex patients. RPs insisting on a transfer and/or requesting to speak to an administrator led to APs acquiescing to avoid conflict, even though transfer may not be the optimal course of action.
Our study has several limitations. First, our data comes from a single institution in the Midwest; thus, our results may not be generalizable. However, this is less likely given that most tertiary hospitals utilize some form of a transfer center.15 Second, recall bias may have impacted our results. However, most themes in our analysis were reported by multiple participants. Lastly, we only report the TCN perspective. RPs or APs may perceive barriers or facilitators to communication differently than TCNs and may have a more nuanced appreciation for the content and depth of information necessary to improve communication. Future work will investigate RPs’ and APs’ perspectives on barriers and facilitators to communication and elicit their thoughts on improving communication surrounding EGS transfers.
CONCLUSION
Achieving optimal patient outcomes requires timely, high-quality care provided by appropriate providers and staff. During interhospital transfers, APs rely on RPs’ clinical acumen, situational assessment, and communication skills as they have the “eyes on the patient.” For both RPs and APs, making decisions under time constraints and determining the best course of action can become a stressful task, particularly when transportation to a different facility is needed. The RCF suggests that these challenges can be overcome through shared goals, shared knowledge, and mutual respect.16 Opportunities for improving communication surrounding interhospital transfers include sharing appropriate and complete information through structured processes and tools. Such methods to enhance providers’ work may include checklists and/or scripts but could also include the integration of telemedicine into the assessment of EGS patients and the ultimate decision to transfer. These adjuncts could help to ensure that communication is efficient and solidified by mutual respect and trust, and promote consensus about the course of action, in part, by enhancing providers’ understanding about institution-level resources. TCNs have provided an initial understanding of the communication between RPs and APs, which will be verified and adapted through engaging RPs and APs so that evidence-based interventions can be developed to address gaps in provider communication and to hopefully result in quantifiable improvements in patient care and safety.
Acknowledgements
Graphics in Figure 1 were sourced from the Noun Project.
Funding
The project described was supported by the Agency for Healthcare Research and Quality (AHRQ) K08 144-AAD5359-539714-4 and the Clinical and Translational Science Award program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences grant ULTR002373. The content is solely the responsibility of the authors and does not represent the official views of the AHRQ or NIH.
Footnotes
Competing interests
The authors have no personal or financial conflicts of interest. Disclosure: Dr. Ingraham serves as a Clinical Consultant for the American College of Surgeons for work unrelated to this project.
Patient consent for publication
Not required.
Data availability statement
Data are available upon reasonable request.
REFERENCES
- 1.Philip JL, Yang D-Y, Wang X, et al. Effect of transfer status on outcomes of emergency general surgery patients. Surgery 2020;168(2):280–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sokol‐Hessner L, White AA, Davis KF, et al. Interhospital transfer patients discharged by academic hospitalists and general internists: Characteristics and outcomes. Journal of Hospital Medicine 2016;11(4):245–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mueller S, Zheng J, Orav EJ, et al. Inter-hospital transfer and patient outcomes: a retrospective cohort study. BMJ Quality & Safety 2019;28(11):e1–e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mueller SK, Fiskio J, Schnipper J. Interhospital Transfer: Transfer Processes and Patient Outcomes. Journal of Hospital Medicine 2019;14(8):486–91. doi: 10.12788/jhm.3192 [published Online First: 2019/04/16] [DOI] [PubMed] [Google Scholar]
- 5.Ligtenberg JJ, Arnold LG, Stienstra Y, et al. Quality of interhospital transport of critically ill patients: a prospective audit. Critical Care 2005;9(4):R446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mueller SK, Schnipper JL. Physician perspectives on interhospital transfers. Journal of Patient Safety 2019;15(2):86–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Payne CE, Stein JM, Leong T, et al. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Quality & Safety 2012;21(11):925–32. [DOI] [PubMed] [Google Scholar]
- 8.Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. New England Journal of Medicine 2014;371(19):1803–12. [DOI] [PubMed] [Google Scholar]
- 9.Nagpal K, Abboudi M, Fischler L, et al. Evaluation of postoperative handover using a tool to assess information transfer and teamwork. Annals of Surgery 2011;253(4):831–37. [DOI] [PubMed] [Google Scholar]
- 10.BMA Junior doctors Committee NMA, National Patient Safety Agency. Safe handover: safe patients. Guidance on Clinical Handover for Clinicians and Managers, 2005. [Google Scholar]
- 11.Safe practices for better healthcare–2010 update: a consensus report. Washington, DC, National Quality Forum; 2010. [Google Scholar]
- 12.Ong M-S, BiomedE M, Coiera E. A systematic review of failures in handoff communication during intrahospital transfers. The Joint Commission Journal on Quality and Patient Safety 2011;37(6):274–AP8. [DOI] [PubMed] [Google Scholar]
- 13.Theobald CN, Choma NN, Ehrenfeld JM, et al. Effect of a handover tool on efficiency of care and mortality for interhospital transfers. Journal of Hospital Medicine 2017;12(1):23–28. [DOI] [PubMed] [Google Scholar]
- 14.Malpass HC, Enfield KB, Keim-Malpass J, et al. The interhospital medical intensive care unit transfer instrument facilitates early implementation of critical therapies and is associated with fewer emergent procedures upon arrival. Journal of Intensive Care Medicine 2015;30(6):351–57. [DOI] [PubMed] [Google Scholar]
- 15.Herrigel DJ, Carroll M, Fanning C, et al. Interhospital transfer handoff practices among US tertiary care centers: A descriptive survey. Journal of Hospital Medicine 2016;11(6):413–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gittell JH. Relational coordination: Coordinating work through relationships of shared goals, shared knowledge and mutual respect. Relational perspectives in organizational studies: A research companion 2006:74–94. [Google Scholar]
- 17.Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Medical Care 2000:807–19. [DOI] [PubMed] [Google Scholar]
- 18.Gittell JH, Godfrey M, Thistlethwaite J. Interprofessional collaborative practice and relational coordination: improving healthcare through relationships. Journal of Interprofessional Care 2013;27(3):210–13. [DOI] [PubMed] [Google Scholar]
- 19.Gittell JH. Coordinating mechanisms in care provider groups: Relational coordination as a mediator and input uncertainty as a moderator of performance effects. Management Science 2002;48(11):1408–26. [Google Scholar]
- 20.Havens DS, Vasey J, Gittell JH, et al. Relational coordination among nurses and other providers: impact on the quality of patient care. Journal of Nursing Management 2010;18(8):926–37. [DOI] [PubMed] [Google Scholar]
- 21.Cramm JM, Nieboer AP. Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Healthcare Management Review 2012;37(4):301–09. [DOI] [PubMed] [Google Scholar]
- 22.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qualitative health research 2005;15(9):1277–88. [DOI] [PubMed] [Google Scholar]
- 23.Miles MB, Huberman AM. Qualitative data analysis: A sourcebook of new methods: Sage publications 1984.
- 24.Creswell JW, Miller DL. Determining Validity in Qualitative Inquiry. Theory Into Practice 2000;39(3):124–30. doi: 10.1207/s15430421tip3903_2 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.


