Abstract
Purpose
This review evaluated the knowledge, utilisation, prevention education, and policy response across the six geopolitical regions of Nigeria to inform national efforts for the prevention and control of cervical cancer.
Methods
A keyword-based systematic search was conducted in PubMed/MEDLINE (NCBI), Google Scholar, and AJOL electronic databases, including a manual scan of papers, journals and websites to identify relevant peer-reviewed studies. Articles were screened and assessed for eligibility.
Results
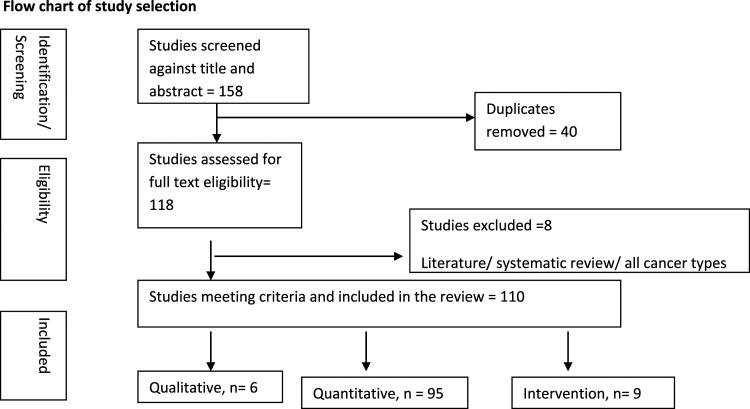
Many (158) articles were downloaded and after duplicates were removed, 110 articles were included in the final analysis. These were made up of qualitative, quantitative (cross-sectional), intervention and policy studies. Studies have generally reported poor knowledge and awareness of cervical cancer screening but those carried out in urban areas demonstrated a slightly higher level of awareness of Human Papilloma Virus (HPV) vaccine, HPV vaccination uptake and utilization of cervical cancer preventive services than the rural studies. The studies did not show strong government support or policies in relation to cervical cancer control.
Conclusion
Knowledge and uptake of cervical cancer preventive services across diverse groups in Nigeria remain poor. These could be linked to socio-cultural factors, the lack of an organised cervical cancer screening programme and low financial resource pool for cervical cancer prevention. Therefore, it is necessary to increase government, donor prioritisation and political support in order to ensure increased investment and commitment to cervical cancer elimination in Nigeria.
Keywords: prevention education, knowledge, screening, uptake, policy response
Background
Globally, cervical cancer (CC) is one of the leading gynaecologic malignancies of public health concern with approximately 570,000 new cases in 2018 and with 80% of these occurring in low- and middle-income countries. 1 Over 99% of cervical cancer cases have been linked to infection with the Human Papillomavirus (HPV). 2 According to recent projections, the number of new cases will increase to 700,000 by 2030 while annual deaths from the disease will rise from 311 000 to 400 000. 3 Higher incidences and mortality rates have also been documented in the SSA region compared to other regions of the world, with over 75,000 annual new cases and an estimated 50,000 deaths per year.4,5 In Africa, cervical cancer affects 27.6 per 100,000 women annually, and a significant proportion - 17.5 per 100,000 women results in death compared to its incidence of 6 new cases per 100,000 women among the African American population.6,7 The West African region has an age-standardized incidence rate of 31.5 per 100,000 women, mortality rate of 17.9 per 100,000 women and the prevalence of the Human Papilloma virus in the general population is 17.9%.8-10
Nigeria is Africa’s most populous country located in the West African region and data from the Cervical Cancer Global Crisis Card ranks her as the 5th leading nation with the highest death count from cervical cancer, after India, China, Brazil and Bangladesh. 11 Data from two population-based cancer registries in Nigeria showed that the age standardised incidence rate for cervical cancer is 34.5 per 100 000. 12 Nigeria is faced with similar challenges like other Low Health Development Index nations, with 44,699 deaths and 73,417 new cases of cervical cancer in women in 2020. Cervical cancer contributed 12,075 which is 9.7% of new cases and 7968 (10.1%) cancer deaths in Nigeria in 2020, making it the second most common cancer after breast cancer. 13 Most, over 70% of patients with cervical cancer present late at the invasive stage of the disease leading to poor outcome.14,15 All the six geopolitical zones in Nigeria (South-east, South-south, South-west, North-east, North-west and North- central) are faced with similar circumstances with regards to cervical cancer screening access and uptake. Nigeria is yet to fully implement a structured guideline for cervical cancer screening, thuss screening is more opportunistic and is not readily available in the primary level of care, 16 unlike in developed countries. 17
Prevention remains the major strategy to tackle the growing burden of cervical cancer in Nigeria. The World Health Organisation Global Strategy for the elimination of cervical cancer proposes ambitious targets aimed at ensuring girls are fully vaccinated with the HPV vaccine, women are screened, and those with precancerous lesions or cervical cancer are treated. 18 These approaches have contributed to the significant decrease in cervical cancer burden in developed countries.19,20
However, many sub-Saharan African countries have been unable to attain a reduction in the cervical cancer burden due to resource limitations and implementation challenges thus underscoring the global inequities.21-23 Most African countries like Nigeria have developed strategic plans for cervical cancer control, but these have not been well implemented using best practices except for South Africa. For example, “There is still no national policy or programme regarding cervical cancer screening in Ghana and that could be contributing to the persisting low patronage of cervical cancer screening in Ghana”. 24 It was documented that South Africa has a national policy document with a structured cervical cancer control programme, which is well implemented. 25 The policy has good algorithms that guide cervical cancer screening unlike most other African countries. This is compounded by the complex interplay of socio-cultural, biological and health systems factors. In Nigeria, routine population-based screening programmes are lacking, and this contributes to less availability of screening facilities and late detection of the disease. 26 Furthermore, HPV vaccination has not been fully integrated into the national vaccination schedule in Nigeria 27 and this is currently provided to female clients at an average cost of $13 per dose, which is beyond what most Nigerians can afford thus limiting its availability and affordability.
Several studies have been conducted in Nigeria to identify factors influencing the uptake of HPV vaccination and cervical cancer screening. However, these have been limited in scope and geographic coverage. Furthermore, there are no national or regional data on HPV vaccination uptake and cervical cancer screening in Nigeria.28,29 Given the public health burden of cervical cancer in Nigeria, it is imperative to examine individual-level behavioural factors within and across the geopolitical regions to provide a holistic overview and understanding of cervical cancer prevention and control in Nigeria and appropriate interventions. This article aims to comprehensively analyse knowledge, utilisation, prevention education and policy response across the six geopolitical regions of Nigeria, and to suggest actionable solutions to inform national efforts for the prevention and control of cervical cancer in Nigeria.
Methodology
This review was done with available original research studies. No ethical approval was required.
Description of the Study Setting
The review focused on studies conducted in Nigeria, Africa's most populous country. Healthcare delivery in Nigeria remains the responsibility of the three tiers of government: the local, state and federal government.30-32 The primary health care system is managed by the local government with support from the state ministries of health. 31 The secondary health care system is managed by the state ministries of health and patients are often referred from the primary health care or private facilities. This is the first level of specialty services and is available at different divisions of the state. The Federal government manages the tertiary facilities which provides the highest level of care. These include teaching hospitals and specialist hospitals.
Information Sources and Search Strategy
We searched PUBMED, Google Scholar and AJOL and sourced for original research articles that were published in the last 10 years. We included studies that reported awareness/knowledge/acceptability/willingness of cervical cancer screening and HPV vaccination in Nigeria.
Databases (PubMed/MEDLINE (NCBI), Google Scholar) and AJOL were searched for records in English. We divided the review topic into the following concepts: 1) cervical cancer, 2) HPV vaccine, 3) educational intervention and 4) prevention education. We adopted suitable MeSH terms and truncated keywords and employed Boolean operators AND/OR to link the concept and associated terms in the following way: (Cervical cancer) AND (Knowledge OR Awareness OR Acceptability OR Willingness) AND (Nigeria[Tiab]) (Figure 1 shows details of the search strategy). The authors further manually searched reference lists identified in relevant publications, journals and websites.
Figure 1.
Flow chart for study selection.
Eligibility Criteria
For a study to be eligible, it had to be a peer-reviewed research, written in English language, human studies, primary research in Nigeria and included female or other participants. Articles that reported in their aims, primary outcome (quantitative studies) or main theme (qualitative studies) on cervical cancer screening and HPV vaccine (knowledge, awareness, acceptability or willingness, educational intervention, prevention education, policy (ies) OR effect of intervention on knowledge and/or acceptability) were included. Of the one hundred and fifty-eight studies which were published between 2012 and until the final search date mid-2021, 110 met the criteria and were included.
Study Selection
Articles that were included were checked and double screened at two stages; title and abstract, and full-text review. The authors discussed to resolve the variance of opinions at each stage.
Scope of the Review
The team searched for studies that reported on cervical cancer screening and HPV vaccine awareness, knowledge, acceptability and willingness, HPV vaccine; educational intervention and policy. Interventional studies were also reported. Results regarding literature and systematic reviews, knowledge or awareness of cervical cancer alone, treatment of cervical cancer, risk factors for HPV infection and general screening for all cancer types were not included. In addition, the search strategy did not focus on studies related to prevalence and mortality of cervical cancer.
Data Extraction, Data Charting Process and Data Items
Each study was independently reviewed to assess its consistency with the review objectives. Four authors extracted data independently, and data plotting fields for data on awareness, knowledge, utilization, willingness and prevention education included; authors’ names; title of paper; publication year; journal; volume; issue; geopolitical region; state; LGA; study setting; type of study; primary aim of the paper; study population; sample size; sampling technique; results; statistical test; predictors/co-variates for cancer screening and uptake/non-uptake of HPV vaccination; conclusion; study limitation.
Study Characteristics
A total of 158 studies was downloaded after which each article was screened to avoid duplication and exclude studies not relevant to the search objective. At the end of this stage, we were left with a total of 118 articles covering all the six geopolitical zones of Nigeria. For HPV vaccination, the South-west returned (27 studies), followed by South-east (15 studies), North-central (8 studies) and South-south (6 studies). Two studies covered the North-east, while the North-east had the lowest coverage with just one study. Twenty four studies were conducted in an urban setting, hospital based with 14 studies, sub-urban (7 studies), 2 studies were carried out in rural settings while 6 studies were carried out in a mixed setting. All studies were carried out between one and three years.
For cervical cancer screening, 35 studies were retrieved for southwest, 19 for southeast, 13 for north central, 5 for north west and south south with just one study from north east. Most studies were conducted in urban setting (33), hospital based with 11 studies, sub-urban (9 studies), 7 studies were carried out in a rural settings and (8) studies were from mixed settings. All studies were carried out between one and three years.
Results
Study Designs of Included Research
Both observational (descriptive) and interventional studies (quasi-experimental intervention studies) were included in the review. A total of 110 studies were included, which consisted of: 6 qualitative, 95 quantitative (cross-sectional) and 9 intervention studies. Study research methods included: focus group discussions, in-depth interviews, surveys using questionnaires and intervention-control assessment intervention studies. The study designs limit the level of evidence available on the topic.
Population and Geographic Locations of Included Research
Overall data were reported from approximately 23,607 study participants. Study population included women aged 15 and older, women participating in mass cervical cancer screening in community, institutional and hospital settings, HIV positive women, female attendees of the antenatal and gynaecological clinics, female sex workers, female secondary school students, mothers of female adolescents (aged 10-19 years), health care professionals and medical students students, fathers and husbands.
Studies took place in all the six geo-political zones of Nigeria. The studies were done in urban, rural or a mixture of both settings.
Quality of Research Overall
A systematic quality assessment of the articles was not performed since this is not a required activity in a scoping review. The emphasis was a comprehensive coverage of available information rather than a synthesis for evidence-based healthcare.
Awareness and Knowledge of Cervical Cancer Screening and HPV Vaccine
Awareness and knowledge of cervical cancer screening
Several researchers assessed the awareness and knowledge of cervical cancer screening among various groups in Nigeria.33-73 Fourteen in the south east34,38,43,48,49,51,52,57-63, one in the north central 53 north east 55 and south south; 56 fourteen in the south east34,38,43,48,49,51,52,57-63, with thirteen in the southwest.37,39,42,44,45,53,54,61,64-66,68,69 The studies reviewed, generally showed poor awareness45,46,60,61,62,68,70-73 and knowledge of cervical cancer and screening34,35,43,45,46,48-52 across all the geopolitical zones of Nigeria.
In a cross-sectional study carried out among market women in a sub-urban area of Northwest, Nigeria, 43 it was reported that more than 68% of the respondents were aware of cervical cancer screening before the study, but 43.5% of those aware of the screening had good knowledge of it. In another study 44 in an urban setting in south east Nigeria, it was reported that only 19.0% of those who were aware of cervical cancer screening (55.2%) had ever taken the test. In another study in an urban area of south south, Nigeria, among in-school female adolescents, the authors reported that majority of the students had poor awareness (14.8%) and knowledge of risk factors (2.4%) and causes of cervical cancer, but fair knowledge of prevention and treatment of cervical cancer pre-training intervention. However awareness (97.8%) and knowledge (93.4%) of students was significantly increased after a training intervention. 45 Studies that have reported good knowledge and awareness (greater than or equal to 60%) were majorly carried out in urban areas of south east and south west Nigeria41,43,44,56,60,65 and one in a rural area in north central Nigeria. 36
Awareness and Knowledge of HPV Vaccine
Many researchers in a bid to investigate the reasons for low uptake of human papilloma virus (HPV) vaccine have assessed knowledge and awareness of the vaccine. A study that assessed the knowledge, practice and acceptability of HPV vaccine among parents of in-school adolescent girls in north central, Nigeria reported that only 35.1% were aware of HPV vaccine and many (58.7%) had never heard of the vaccine. 46 Other studies that assessed HPV vaccine awareness and vaccination history among women in an out-patient clinic in south west, and among women in south west and north central, Nigeria, reported awareness of (35% and 11.8% respectively) for HPV vaccine among the groups.47,48 Another population study in south west and south east, Nigeria, 49 reported that only 31.97% of respondents having ever heard of HPV, while only 9.91% knew the correct name for the vaccine. However, a hospital based survey that assessed the knowledge, belief and practice of cervical cancer screening and prevention among 1200 women in north east Nigeria 37 reported that 90.3% of women were aware that HPV infection could be prevented by HPV vaccination but majority were not vaccinated.
Also, a survey among a heterogeneous sample of health care providers, 50 revealed that less than half (44%) of the health care providers had knowledge of HPV vaccine. In another study that assessed the knowledge and perception of Obstetricians and Gynaecologists towards human papilloma virus vaccination in Nigeria (employing consultants, senior and junior residents), the majority (85%) of the physicians had knowledge that HPV vaccine could prevent cancer of the cervix and were willing to recommend the vaccine for their prospective clients. 51 However, less than half (44.5%) had adequate knowledge of the vaccination protocol.
Overall, knowledge of HPV vaccine was not high: only six of nineteen studies reported good knowledge among respondents. However, studies carried out among health care professionals reported good knowledge.51,52 In comparing the awareness and knowledge statistics of HPV vaccine, it could be implied that awareness did not translate to good knowledge.53,54 We recommend that emphasis should be placed on population level educational interventions for improved HPV vaccination awareness and knowledge.
Acceptability and Willingness of Cervical Cancer Screening and HPV Vaccine
Acceptability and willingness of cervical cancer screening
In this section, the context of willingness or acceptability of HPV screening were assumed as same term because literature uses both terms interchangeably. Many of the studies reviewed reported high acceptability and willingness for cervical cancer screening services.
Over 50% of the respondents in eight studies were willing to undergo a screening test.55-62 However, in some studies where respondents had high willingness to screen (88.9%), about seventy percent would require the consent of their spouses. 64 This was similarly noted in a study 65 where 81% reported the likelihood of going for screening but their decision could be influenced by husbands (58.1%), physicians (49.5%) and co-workers (48.3%). It was also reported that 64.1% women considered it important to discuss screening with their spouse. 66 In a pre-screening assessment, a high level of cervical cancer screening willingness and acceptability was reported at baseline in an intervention study 63 and although there was an increase following intervention, the changes were not significant.
Nonetheless, in other studies, women indicated unwillingness for cervical cancer screening using Pap smear test in the future. 67 The feeling of embarrassment (94%), high cost (45.2%) and lack of access to screening centres (35%) were some reasons for refusal. 68 However, it was reported that there was acceptability of cervical cancer screening when HPV DNA based tests were incorporated into routine antenatal care. 69 This suggests that employing implementation science research could enhance integrating this evidence into routine practice. Furthermore, high acceptability was reported in a study that employed self-sampling method. 70 However, a decline in willingness and acceptability of respondents was noted if a fee was attached. 44 Two studies however documented that respondents considered it important to pay for screening.66,71
The studies in the south west and north central geopolitical zones all had high willingness and acceptability to screen. Howbeit across all zones, only studies in the south east took into cognisance the cost of screening. Although many studies reported high willingness, this needs to translate into practice for a reduced morbidity and mortality rates. This could be achieved by addressing the mitigating factors influencing willingness, in addition to local advocacy campaigns to alter this disparity.
Acceptability and Willingness of HPV Vaccine
The HPV vaccine prevents pre-cancer lesions by preventing infections. The willingness and acceptability of the vaccine remains an important aspect that could translate to uptake. There was high willingness among parents to vaccinate their female children42,50-52,72-76 and to recommend the vaccine to others (91.0%). 72 In addition, at baseline in an experimental study in north-central Nigeria, 73.9% (experimental group) and 83.1% (control group) of the mothers were willing to accept HPV vaccination for their adolescent daughters. 77 However, in another study in north central Nigeria, 44.9% women were not willing to vaccinate their children with HPV vaccine. 46 Various women however, including health professionals, were willing to be vaccinated.49,61,78,79
The studies reviewed did not cut across all geopolitical zones and although many parents were willing to vaccinate their daughters, the cost, availability, accessibility, socio-cultural and religious factors and other limiting factors for HPV vaccination contributed an important role in eventual uptake. Therefore, there is the need for more studies in other parts of the country, including the northern and south south regions, to allow for regional comparison and for a more robust overview.
Cervical Cancer Screening and Human Papilloma Virus Vaccination Uptake
Uptake of cervical cancer screening and HPV vaccination are fundamental for any cervical cancer preventive packages. Structured programmes aimed at reducing cervical cancer are divided into four (4) stages of prevention; primary (vaccination against HPV), secondary (screening and treatment of pre- cancerous lesions), tertiary (diagnosis and treatment of invasive cervical cancer) and palliative care. 80 Even though cervical cancer screening is very critical in successful prevention of the disease, the services are not readily available in developing countries. Suboptimal coverage and constraints of accessibility to services offering screening and preventive treatment contributes to this challenging public health situation.81,82
Utilisation of various screening services makes early detection possible thereby making invasive cervical cancer preventable as well as effective reduction in mortality rate. 83 The level of progress and disparity in reduction of cervical cancer between developed and developing nations could be linked with the utilization of screening services,84,85 and the uptake of the screening services has not been quite encouraging in Nigeria. 78
Cervical Cancer Screening Uptake in Nigeria
Studies from across various regions in Nigeria have reported that the proportion of women who have ever used cervical screening services ranged between .6% to 19% with most studies reporting less than 10% which is quite dismal.56,62,71,86-91 In a study among women attending the gynaecological clinics of health facilities in south east Nigeria, it was reported that only 19.0% out of 3712 had utilised screening services. 44 Despite being hospital patients with gynaecological problems, yet most of them were not screened for cervical cancer. Similar study in the south east region reported a range of .6 to 12.2% screening among women.62,71,86 In south west Nigeria, the pattern of uptake was similar to other regions that had reported a range of 3% to 12.2% uptake of cervical cancer screening among the women.56,87,88
The situation was similar in Northern Nigeria; a study among market women in Niger state showed that only one respondent (1.1%) had ever done Pap smear before. 89 From a study among Federal Civil Servants in north central Nigeria, uptake of Pap smear test among the population was 10.2% 90 while it was reported that only 8.0% of the women studied had ever been screened for the disease. 91 They further reported that screening for cervical cancer was significantly higher among respondents who had positive attitude towards screening, who were aware of cervical cancer screening, as well as those who were aware of cancer of the cervix.
Human Papilloma Virus Vaccination Uptake in Nigeria
Vaccines prevent cervical cancers 92 but not much has been achieved in the area of uptake of HPV vaccines in Nigeria. Less progress has been achieved for uptake of HPV vaccination among parents/caregivers of female children in south-East, Nigeria. 42 Accessibility and affordability were the most common challenges among those aware of the vaccine. An improvement in HPV vaccination uptake from .9% to 33.2% was reported among girls aged 9-13 years after a quasi-experimental study in south east Nigeria. 86 Poor HPV vaccination uptake was reported in studies in south west Nigeria,52,72,78,93 south south, 94 north central, 46 north east 37 and the capital city-Abuja, Nigeria. 77
It can be deduced from these studies that HPV vaccination uptake and the utilisation of cervical cancer preventive services in Nigeria is generally poor. This has been shown to be due to some barriers, including lack of awareness, cost and accessibility. 95 Associations between perception and uptake of HPV vaccine and parental approval and readiness for HPV vaccine uptake has been documented in a study. 93
Prevention and Educational Interventions for Cervical Cancer and HPV Vaccination
Educational Interventions for HPV and cervical cancer screening
Behavioural interventions that employ educational delivery methods have a potential to influence positive outcomes, 96 however few studies that employ educational or communication methods for cervical cancer prevention, especially HPV vaccination, have been documented.96,97 Few studies in Nigeria have employed educational interventions to improve the uptake of both cervical cancer screening and HPV vaccination in the last 10 years. Most studies have focused on cross sectional surveys to highlight the level of awareness, knowledge, willingness, acceptability and uptake of both cervical cancer screening and HPV vaccination. These studies have shown a dearth of knowledge about cervical cancer, HPV and HPV vaccination among Nigerian adolescents, women, and in rural communities.
More of the educational intervention studies have focused on increased awareness and knowledge of cervical cancer risk factors, symptoms, treatment, causative agent/virus and preventive strategies.45,77,89,93,98,99 More of these educational intervention studies have targeted cervical screening knowledge and uptake, among women at community levels and health care workers (nurses). Fewer studies have targeted increased HPV vaccination.45,77,86 Educational intervention strategies that were employed included peer education,45,63 community health education 86 and educational intervention strategies and methods, including health education, training, 93 use of electronic and multimedia methods 98 and seminars. 99
Educational interventions for the creation of awareness and to increase knowledge of cervical cancer and prevention practices are very vital for its elimination in Nigeria. Educational interventions are important and have the potential to translate to practice but behaviour change is complex and many factors influence adaptation of positive behaviour. Health promotion strategies, which goes beyond health education to include reorientation of health services and advocacy, and employing peer education, community engagement/involvement and health education communication strategies, are important in reinforcing and sustaining optimal uptake of cervical cancer screening and HPV vaccination in different settings across Nigeria. Scale up of educational interventions in communities and settings to ensure validity and reliability of interventions is important. In addition, different factors, including age, level of education, marital status, parity, employment status influence awareness, knowledge and/or uptake of cervical cancer prevention. Interventions should take into consideration these various factors in targeting the appropriate intervention to particular target groups.
Also, the reorientation of services at the primary care level, provision of cervical cancer prevention services at the primary and secondary healthcare levels including subsidised Pap smear screening test are essential for the successful implementation of a national cervical cancer control and HPV vaccination programme. 86
Despite the strong global call for the elimination of cervical cancer by the WHO, 100 and the policy efforts by the Nigerian government to reduce the national prevalence of cervical cancer, there are still many gaps to cover in the process of eliminating cervical cancer in Nigeria. Implementation sciences studies that employ educational strategies and methods targeting both individual and community groups are needed to understand and highlight evidence-based interventions for reducing the burden of cervical cancer in Nigeria.
Government Policies and Interventions on CC Screening and HPV Vaccination in Nigeria
The Nigerian government articulated a National Cancer Control Policy (2018-2022) for the prevention and control of different types of malignancies. 101 The policy stipulates strategies for cervical cancer prevention and control, specifically outreaches to increase awareness about HPV vaccination and screening, the establishment of nationwide routine screening programmes and management of precancerous lesions at Primary Healthcare centres. The proposed actions align with the WHO Global Strategy for the elimination of cervical cancer.
To support this process, the Nigerian Federal Ministry of Health and the World Health Organisation developed a costed National Strategic Plan on Prevention and Control of Cervical Cancer: Nigeria, 2017—2021. 101 According to this costed 5-year national strategic plan, the government will require an estimate of US$ 1.017 billion to implement activities for the primary, secondary and tertiary prevention of cervical cancer. Of the total estimated sum, 2% will cover cost of vaccination, 90% for cervical cancer service delivery for screening and pre-cancer treatment, 6% will address cancer diagnosis, treatment and palliative care. 101
Although laudable, the feasibility for implementation and sustainability of this costed plan is currently unknown however this seems unlikely given the country’s current economic situation 102 and historical antecedence of poor political prioritisation, funding and implementation of health policies and programmes. For instance, an evaluation of the implementation of National Cancer Control Plans in Africa revealed that poor resource and partner mobilisation was a major challenge. Cancer control planners are inhibited by the suboptimal budget allocation with grave implication on the human, technical, education and infrastructure resources required for its implementation. 103
Conclusions
This review evaluated the knowledge, utilisation and, prevention education for cervical cancer prevention and HPV vaccination uptake across the six geopolitical regions of Nigeria. It also documented policy support to inform national efforts for the prevention and control of cervical cancer. It outlined regional differences and factors influencing uptake. Review highlighted that knowledge and uptake of cervical cancer preventive services across diverse groups in Nigeria remains poor. This could be linked to socio-cultural factors, the lack of an organized cervical cancer screening programme and low financial resource pool for cervical cancer prevention. Unlike the global HIV/AIDS response, there is less centralised financial resource pool for cancer prevention in Nigeria. Compounding this is the fragmentation of cancer control programmes within different departments of the ministry of health with no dedicated cancer-control officer or budget. In order to achieve the cancer-related goals, there is need for increased government and donor prioritisation and political buy-in to ensure increased investment and commitment to cervical cancer elimination in Nigeria.
Acknowledgments
We are grateful to Damilola Busari who helped with the search and extraction of information from the articles.
Footnotes
Authors’ Contribution: Authors (YOJA and MMO) conceptualized the review. All authors contributed to the development of the data charting process, data extraction and writing first draft of the manuscript. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Yetunde O. John-Akinola https://orcid.org/0000-0002-5291-765X
Chizoma M. Ndikom https://orcid.org/0000-0002-4036-156X
Mojisola M. Oluwasanu https://orcid.org/0000-0001-7186-1113
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Lowy D, Solomon D, Hildesheim A, Schiller JT, Schiffman M. Human papillomavirus infection and the primary and secondary prevention of cervical cancer. Cancer. 2008;113:S1980–S1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mailhot Vega RB, Balogun OD, Ishaq OF, Bray F, Ginsburg O, Formenti SC. Estimating child mortality associated with maternal mortality from breast and cervical cancer. Cancer. 2019;125(1):109-117. doi: 10.1002/cncr.31780. [DOI] [PubMed] [Google Scholar]
- 4.De Vuyst H, Alemany L, Lacey C, et al. The burden of human papillomavirus infections and related diseases in sub-Saharan Africa. Vaccine. 2013;31(suppl 5):F32-F46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893-2917. [DOI] [PubMed] [Google Scholar]
- 6.De Vuyst H, Alemany L, Lacey C, et al. The burden of human papillomavirus infections and related diseases in sub-Saharan Africa. Vaccine. 2013;31(suppl 5):F32-F46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-E386. [DOI] [PubMed] [Google Scholar]
- 8.Cancer Incidence and Mortality Worldwide: IARC Cancer Base GLOBOCAN 2012 v1.0. 2013. Available online: http://globocan.iarc.fr. Accessed on 1 June 2018.
- 9.Human Papillomavirus and Related Diseases Report. Available online: http://www.hpvcentre.net/statistics/reports/XFX.pdf. Accessed on 3 May 2018.
- 10.Black E, Richmond R. Prevention of cervical cancer in sub-Saharan Africa: The advantages and challenges of HPV vaccination. Vaccines. 2018;6(3):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cervical Cancer Free Coalition . Cervical cancer global crisis card. Accessed January 12, 2017.
- 12.Jedy-Agba E, Curado MP, Ogunbiyi O, Oga E, Fabowale T, Igbinoba F, et al. Cancer incidence in Nigeria: a report from population-based cancer registries. Cancer epidemiology. 2012;36(5):e271-e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Agency for Cancer Research/World Health Organization Nigeria Factsheet: Globocan 2020. 2021. https://gco.iarc.fr/today/data/factsheets/populations/566-nigeria-fact-sheets.pdf. Accessed September 11, 2022.
- 14.Awofeso O, Roberts AA, Salako O, Balogun L, Okediji P. Prevalence and pattern of late-stage presentation in women with breast and cervical cancers in Lagos University Teaching Hospital, Nigeria. Niger Med J. 2018;59:74-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okolie EA, Aluga D, Anjorin S, Ike FN, Ani EM, Nwadike BI. Addressing missed opportunities for cervical cancer screening in Nigeria: a nursing workforce approach. Ecancermedicalscience. 2022;16:1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekwunife OI, Lhachimi SK. Cost-effectiveness of human papilloma virus (HPV) vaccination in Nigeria: a decision analysis using pragmatic parameter estimates for cost and program coverage. BMC Health Serv Res. 2017;17(1):815. doi: 10.1186/s12913-017-2758-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anyasi HI, Foss AM. A comparative analysis of cervical cancer prevention between Nigeria and Nordic countries that have experienced a decline in cervical cancer incidence. Int health. 2021;13(4):307-317. doi: 10.1093/inthealth/ihaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization . Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 19.Safaeian M, Solomon D, Castle PE. Cervical cancer prevention—cervical screening: science in evolution. Obstet Gynecol Clin N Am. 2007;34(4):739-760. ix 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jemal A, Bray F, Forman D, et al. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118(18):4372-4384. [DOI] [PubMed] [Google Scholar]
- 21.Lim JN, Ojo AA. Barriers to utilisation of cervical cancer screening in sub Saharan Africa: a systematic review. Eur J Cancer Care. 2017;26(1):12444. doi: 10.1111/ecc.12444. [DOI] [PubMed] [Google Scholar]
- 22.McFarland DM, Gueldner SM, Mogobe KD. Integrated review of barriers to cervical cancer screening in sub-Saharan Africa. J Nurs Scholarsh. 2016;48(5):490-498. [DOI] [PubMed] [Google Scholar]
- 23.Randall TC, Ghebre R. Challenges in prevention and care delivery for women with cervical cancer in sub-Saharan Africa. Front Oncol. 2016;6:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calys-Tagoe BNL, Aheto JMK, Mensah G, et al. Cervical cancer screening practices among women in Ghana: evidence from wave 2 of the WHO study on global AGEing and adult health. BMC Wom Health. 2020;20:49. doi: 10.1186/s12905-020-00915-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Department of Health . Cervical Cancer Prevention and Control Policy; 2017, pp. 1-68. https://www.health.gov.za/wp-content/uploads/2021/07/cervical-cancer-policy.pdf [Google Scholar]
- 26.Sowemimo OO, Ojo OO, Fasubaa OB. Cervical cancer screening and practice in low resource countries: Nigeria as a case study. Trop J Obstet Gynaecol. 2017;34(3):170-176. [Google Scholar]
- 27.Bisi-Onyemaechi AI, Chikani UN, Nduagubam O. Reducing incidence of cervical cancer: knowledge and attitudes of caregivers in Nigerian city to human papilloma virus vaccination. Infect Agents Cancer. 2018;13(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.B-RL BL, AlberoG S, Mena M, GómezD MJ, Bosch FX, de Sanjosé S. ICO/IARC information Centre on HPV and Cancer (HPV information Centre). Human papillomavirus and related diseases in Nigeria. Summary Report. 2017. [Google Scholar]
- 29.Nkwonta CA, Hilfinger Messias DK, Felder T, Luchok K. Increasing Human Papillomavirus vaccination and cervical cancer screening in Nigeria: An assessment of community-based educational interventions. Int Q Community Health Educ. 2020;41(1):89-99. [DOI] [PubMed] [Google Scholar]
- 30.Adeyemo DO. Local government and health care delivery in Nigeria: A Case Study. J Hum Ecol. 2005;18:149-160. [Google Scholar]
- 31.Omoruan AI, Bamidele AP, Phillips OF. Social health insurance and sustainable healthcare reform in Nigeria. Ethno Med. 2009;3:105-110. [Google Scholar]
- 32.National Health Insurance Scheme Decree No 35 of 1999 . Laws of the Federation of Nigeria. Available from: http://www.nigeria-law.org/National%20Health%20Insurance%20Scheme%20Decree.htm. Accessed on 2010 November 6. [Google Scholar]
- 33.Onyenwenyi AO, Mchunu GG. Primary health care workers’ understanding and skills related to cervical cancer prevention in Sango PHC centre in south-western Nigeria: a qualitative study. Prim Health Care Res Dev. 2019;20:e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toye MA, Okunade KS, Roberts AA, Salako O, Oridota ES, Onajole AT. Knowledge, perceptions and practice of cervical cancer prevention among female public secondary school teachers in Mushin local government area of Lagos State, Nigeria. Pan African Medical Journal. 2017;28(1):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Awolude OA, Oyerinde SO, Akinyemi JO. Screen and triage by community extension workers to facilitate screen and treat: task-sharing strategy to achieve universal coverage for cervical cancer screening in Nigeria. J Glob Oncol. 2018;4:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ilesanmi RE, Kehinde DR. Pattern of utilization of cervical cancer screening services among female sex workers in some selected brothels in Abuja, Nigeria. Asia Pac J Oncol Nurs. 2018;5(4):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rimande-Joel R, Ekenedo GO. Knowledge, Belief and practice of cervical cancer screening and prevention among women of Taraba, North-East Nigeria. Asian Pac J Cancer Prev APJCP: Asian Pac J Cancer Prev APJCP. 2019;20(11):3291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ezeanochie M, Olasimbo P. Awareness and uptake of human papilloma virus vaccines among female secondary school students in Benin City, Nigeria. Afr Health Sci. 2020;20(1):45-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adibe MO, Aluh DO. Awareness, knowledge and attitudes towards cervical cancer amongst hiv-positive women receiving care in a Tertiary Hospital in Nigeria. J Cancer Educ. 2018;33(6):1189-1194. [DOI] [PubMed] [Google Scholar]
- 40.Ifediora CO, Azuike EC. Knowledge and attitudes about cervical cancer and its prevention among female secondary school students in Nigeria. Trop Med Int Health. 2018;23(7):714-723. [DOI] [PubMed] [Google Scholar]
- 41.Ifemelumma CC, Anikwe CC, Okorochukwu BC, et al. Cervical cancer screening: assessment of perception and utilization of services among health workers in low resource setting. Int J Reprod Med. 2019;2019:6505482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Azuogu BN, Umeokonkwo CD, Azuogu VC, Onwe OE, Okedo-Alex IN, Egbuji CC. Appraisal of willingness to vaccinate daughters with human papilloma virus vaccine and cervical cancer screening uptake among mothers of adolescent students in Abakaliki, Nigeria. Niger J Clin Pract. 2019;22(9):1286. [DOI] [PubMed] [Google Scholar]
- 43.Ahmed SA, Sabitu K, Idris SH, Ahmed R. Knowledge, attitude and practice of cervical cancer screening among market women in Zaria, Nigeria. Niger Med J. 2013;54(5):316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chigbu CO, Aniebue U. Why southeastern Nigerian women who are aware of cervical cancer screening do not go for cervical cancer screening. Int J Gynecol Cancer. 2011;21(7):1282–1286. [DOI] [PubMed] [Google Scholar]
- 45.Sadoh AE, Okonkwo C, Nwaneri DU, et al. Effect of peer education on knowledge of human papilloma virus and cervical cancer among female adolescent students in Benin City, Nigeria. Ann Glob Health. 2018;84(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adesina KT, Saka A, Isiaka-Lawal SA, et al. Knowledge, practice and acceptability of HPV vaccine by mothers of adolescent girls in Ilorin, Nigeria. Sudan J Med Sci. 2018;13(1):33-49. [Google Scholar]
- 47.Faneye AO, Adeiga AA, Awoderu OB, Fayemiwo AS. Human papilloma virus vaccine awareness and vaccination history in patients attending STI clinics in Lagos and Ibadan, Nigeria. Arch Basic Appl Med. 2018;6(1):95. [PMC free article] [PubMed] [Google Scholar]
- 48.Ajayi MP, Amoo EO, Olawande TI, Iruonagbe TC, Idowu AE, Adekeye OA. Awareness of Breast and Cervical Cancer among Women in the Informal Sector in Nigeria. Open Access Maced J Med Sci. 2019;7(14):2371-2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eni AO, Soluade MG, Efekemo OP, Igwe TT, Onile-Ere OA. Poor knowledge of human papilloma virus and vaccination among respondents from three Nigerian states. J Community Health. 2018;43(6):1201-1207. [DOI] [PubMed] [Google Scholar]
- 50.Audu BM, Bukar M, Ibrahim AI, Swende TZ. Awareness and perception of human papilloma virus vaccine among healthcare professionals in Nigeria. J Obstet Gynaecol. 2014;34(8):714-717. [DOI] [PubMed] [Google Scholar]
- 51.Morhason-Bello IO, Adesina OA, Adedokun BO, et al. Knowledge of the human papilloma virus vaccines, and opinions of gynaecologists on its implementation in Nigeria. Afr J Reprod Health. 2013;17(2):150-156. [PubMed] [Google Scholar]
- 52.Adejuyigbe FF, Balogun BR, Sekoni AO, Adegbola AA. Cervical cancer and human papilloma virus knowledge and acceptance of vaccination among medical students in Southwest Nigeria. Afr J Reprod Health. 2015;19(1):140-148. [PubMed] [Google Scholar]
- 53.Makwe CC, Anorlu RI, Odeyemi KA. Human papillomavirus (HPV) infection and vaccines: knowledge, attitude and perception among female students at the University of Lagos, Lagos, Nigeria. J Epidemiol Glob Health. 2012;2(4):199-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morhason-Bello IO. Household survey on Human Papilloma Virus vaccine awareness among women of reproductive age in Ibadan, Nigeria. Afr J Med Med Sci. 2015;44(1):61-69. [PubMed] [Google Scholar]
- 55.Balogun F, Omotade O. She must have been sleeping around”: Contextual interpretations of cervical cancer and views regarding HPV vaccination for adolescents in selected communities in Ibadan, Nigeria. PLoS One. 2018;13(9):e0203950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ezechi OC, Gab-Okafor CV, Ostergren PO, Pettersson KO. Willingness and acceptability of cervical cancer screening among HIV positive Nigerian women. BMC Publ Health. 2013;13(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adefuye PO, Dada OA, Adefuye BO, Shorunmu TO, Akinyemi BO, Idowu-Ajiboye BO. Feasibility, acceptability, and effectiveness of visual inspection of the cervix with acetic acid and cryotherapy for dysplasia in Nigeria. Int J Gynecol Obstet. 2015;129(1):62-66. [DOI] [PubMed] [Google Scholar]
- 58.Odafe S, Torpey K, Khamofu H, et al. Integrating cervical cancer screening with HIV care in a district hospital in Abuja, Nigeria. Niger Med J. 2013;54(3):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thomas JO, Ojemakinde KO, Ajayi IO, Omigbodun AO, Fawole OI, Oladepo O. Population-based prevalence of abnormal cervical cytology findings and local risk factors in Ibadan, Nigeria: implications for cervical cancer control programs and human papilloma virus immunization. Acta Cytol. 2012;56(3):251-258. [DOI] [PubMed] [Google Scholar]
- 60.Ugwu EO, Obi SN, Ezechukwu PC, Okafor II, Ugwu AO. Acceptability of human papilloma virus vaccine and cervical cancer screening among female health-care workers in Enugu, Southeast Nigeria. Niger J Clin Pract. 2013;16(2):249-252. [DOI] [PubMed] [Google Scholar]
- 61.Akanbi OA, Iyanda A, Osundare F, Opaleye OO. Perceptions of Nigerian women about human papilloma virus, cervical cancer, and HPV Vaccine. Scientifica. 2015;2015:285702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Eze JN, Umeora OU, Obuna JA, Egwuatu VE, Ejikeme BN. Cervical cancer awareness and cervical screening uptake at the Mater Misericordiae Hospital, Afikpo, Southeast Nigeria. Ann Afr Med. 2012;11(4):238. [DOI] [PubMed] [Google Scholar]
- 63.Mbachu C, Dim C, Ezeoke U. Effects of peer health education on perception and practice of screening for cervical cancer among urban residential women in south-east Nigeria: a before and after study. BMC Wom Health. 2017;17(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Olubodun T, Odukoya OO, Balogun MR. Knowledge, attitude and practice of cervical cancer prevention, among women residing in an urban slum in Lagos, South West, Nigeria. Pan Afr Med J. 2019;32:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arulogun OS, Maxwell OO. Perception and utilization of cervical cancer screening services among female nurses in University College Hospital, Ibadan, Nigeria. Pan Afr Med J. 2012;11(1):69. [PMC free article] [PubMed] [Google Scholar]
- 66.Okedo-Alex IN, Uneke CJ, Uro-Chukwu HC, Akamike IC, Chukwu OE. It is what I tell her that she will do”: a mixed methods study of married men’s knowledge and attitude towards supporting their wives’ cervical cancer screening in rural South-East Nigeria. Pan Afr Med J. 2020;36:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chigbu CO, Onyebuchi AK, Egbuji CC, Ezugwu EC. Experiences and unmet needs of women undergoing Pap smear cervical cancer screening: impact on uptake of cervical cancer screening in south eastern Nigeria. J Cancer Educ. 2015;30(1):81-85. [DOI] [PubMed] [Google Scholar]
- 68.Ogwunga CC, Anyadoh-Nwadike SO, Ahumibe NC, Nwakwasi EU. Knowledge and attitude of female students of tertiary institutions in Imo State, Nigeria towards cervical cancer and its screening. J Community Health. 2020;46:1-6. [DOI] [PubMed] [Google Scholar]
- 69.Filade TE, Dareng EO, Olawande T, Fagbohun TA, Adebayo AO, Adebamowo CA. Attitude to human papillomavirus deoxyribonucleic acid-based cervical cancer screening in antenatal care in Nigeria: a qualitative study. Front Public Health. 2017;5:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Desai KT, Ajenifuja KO, Banjo A, et al. Design and feasibility of a novel program of cervical screening in Nigeria: self-sampled HPV testing paired with visual triage. Infect Agents Cancer. 2020;15(1):1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dim CC, Onyedum CC, Dim NR, Chukwuka JC. Cervical cancer screening among HIV-positive women in Nigeria: an assessment of use and willingness to pay in the absence of donor support. J Int Assoc Provid AIDS Care. 2015;14(3):241-244. [DOI] [PubMed] [Google Scholar]
- 72.Ezenwa BN, Balogun MR, Okafor IP. Mothers’ human papilloma virus knowledge and willingness to vaccinate their adolescent daughters in Lagos, Nigeria. Int J Wom Health. 2013;5:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chigbu CO, Onyebuchi AK, Ajah LO, Onwudiwe EN. Motivations and preferences of rural Nigerian women undergoing cervical cancer screening via visual inspection with acetic acid. Int J Gynecol Obstet. 2013;120(3):262-265. [DOI] [PubMed] [Google Scholar]
- 74.Dairo MD, Adeleke MO, Salawu AT, Adewole AD. Parental support for human papilloma virus vaccination by adolescents in Ibadan North Local Government Area, Ibadan, Nigeria. Int J Adolesc Med Health. 2016;30(2):0034. [DOI] [PubMed] [Google Scholar]
- 75.Ambali RT, John-Akinola YO, Oluwasanu MM. Indepth interviews’ on acceptability and concerns for human papilloma virus vaccine uptake among mothers of adolescent girls in community settings in Ibadan, Nigeria. J Cancer Educ. 2020:37:1-7. [DOI] [PubMed] [Google Scholar]
- 76.Agida TE, Akaba GO, Isah AY, Ekele B. Knowledge and perception of human papilloma virus vaccine among the antenatal women in a Nigerian tertiary hospital. Niger Med J. 2015;56(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Odunyemi FT, Ndikom CM, Oluwatosin OA. Effect of nursing intervention on mothers’ knowledge of cervical cancer and acceptance of human papillomavirus vaccination for their adolescent daughters in Abuja–Nigeria. Asia Pac J Oncol Nurs. 2018;5(2):223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Oluwole EO, Idowu OM, Adejimi AA, Balogun MR, Osanyin GE. Knowledge, attitude and uptake of human papillomavirus vaccination among female undergraduates in Lagos State, Nigeria. J Fam Med Prim Care. 2019;8(11):3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Makwe CC, Anorlu RI. Knowledge of and attitude toward human papillomavirus infection and vaccines among female nurses at a tertiary hospital in Nigeria. Int J Wom Health. 2011;3:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.World health organization . Human Papillomavirus (HPV) and Cervical Cance; 2019. Retrieved from. http://www.who.int [Google Scholar]
- 81.Randall TC, Ghebre R. Challenges in Prevention and Care Delivery for Women with Cervical in Sub-Saharan Africa. Front Oncol. 2016;6:160. doi: 10.3389/fonc.2016.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.White HL, Meglioli A, Chowdhury R, Nuccio O. Integrating cervical cancer screening and preventive treatment with family planning and HIV-related services. Int J Gynaecol Obstet. 2017;138(suppl 1):41-46. doi: 10.1002/ijgo.12194. [DOI] [PubMed] [Google Scholar]
- 83.Akinpelu AO, Agboola OA, Umezurike ET. Factors affecting utilization of cervical cancer screening services among nurses in a teaching hospital in Ibadan, Nigeria. Int J Cancer Stud Res. 2018;7(1):131-136. [Google Scholar]
- 84.Li M, Nyabigambo A, Navvuga P, et al. Acceptability of cervical cancer screening using visual inspection among women attending a childhood immunization clinic in Uganda. Papillomavirus Res. 2017;4:17-21. doi: 10.1016/j.pvr.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sultana R, Hafeez M, Shafiq S. Awareness about cervical cancer in Pakistani Women. Pak Armed For Med J. 2019;69(1):21-25. [Google Scholar]
- 86.Chigbu CO, Onyebuchi AK, Onyeka TC, Odugu BU, Dim CC. The impact of community health educators on uptake of cervical and breast cancer prevention services in Nigeria. Int J Gynecol Obstet. 2017;137(3):319-324. [DOI] [PubMed] [Google Scholar]
- 87.Dareng EO, Jedy-Agba E, Bamisaye P, et al. Influence of spirituality and modesty on acceptance of self-sampling for cervical cancer screening. PLoS One. 2015;10(11):e0141679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Adepoju EG, Ilori T, Olowookere SA, Idowu A. Targeting women with free cervical cancer screening: challenges and lessons learnt from Osun state, southwest Nigeria. Pan Afr Med J. 2016;24:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gana GJ, Oche MO, Ango JT, Kaoje AU, Awosan KJ, Raji IA. Educational intervention on knowledge of cervical cancer and uptake of Pap smear test among market women in Niger State, Nigeria. J Publ Health Afr. 2017;8(2):575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hyacinth HI, Adekeye OA, Ibeh JN, Osoba T. Cervical cancer and pap smear awareness and utilization of pap smear test among Federal civil servants in North Central Nigeria. PLoS One. 2012;7(10):e46583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Idowu A, Olowookere SA, Fagbemi AT, Ogunlaja OA. Determinants of cervical cancer screening uptake among women in Ilorin, North Central Nigeria: a community-based study. J Cancer Epidemiol. 2016;2016:6469240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang H, Wu S. HPV vaccine knowledge and perceived risk of cervical cancer among female college students in Taiwan. Asian Pac J Cancer Prev APJCP. 2013;14(12):7371-7374. doi: 10.7314/APJCP.2013.14.12.7371. [DOI] [PubMed] [Google Scholar]
- 93.Ndikom CM, Oboh PI. Perception, acceptance and uptake of Human papillomavirus vaccine among female adolescents in selected secondary schools in Ibadan, Nigeria. Afr J Biomed Res. 2017;20(3):237-244. [Google Scholar]
- 94.Ezeanochie M, Olasimbo P. Awareness and uptake of human papilloma virus vaccines among female secondary school students in Benin City, Nigeria. Afr Health Sci. 2020;20(1):45-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nguyen NY, Okeke E, Anglemyer A, Brock T. Identifying perceived barriers to human papillomavirus vaccination as a preventative strategy for cervical cancer in Nigeria. Ann Glob Health. 2020;86(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901-1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Foss HS, Oldervoll A, Fretheim A, Glenton C, Lewin S. Communication around HPV vaccination for adolescents in low-and middle-income countries: a systematic scoping overview of systematic reviews. Syst Rev. 2019;8(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Abiodun OA, Olu-Abiodun OO, Sotunsa JO, Oluwole FA. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC Publ Health. 2014;14(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Adamu AN, Abiola AO, Ibrahim MT. The effect of health education on the knowledge, attitude, and uptake of free Pap smear among female teachers in Birnin-Kebbi, North-Western Nigeria. Niger J Clin Pract. 2012;15(3):326-332. [DOI] [PubMed] [Google Scholar]
- 100.World Health Organization (2020) . Costing the National Strategic Plan on Prevention and Control of Cervical Cancer: Nigeria, 2017—2021. Geneva, Switzerland: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 101.Federal Ministry of Health, Nigeria (2018) . National Cancer Control Plan 2018 – 2022; 2018. [Google Scholar]
- 102.Beddoe AM. Elimination of cervical cancer: challenges for developing countries. Ecancermedicalscience. 2019;13:975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Duncan K, Cira MK, Barango P, Trimble EL. Challenges and opportunities in the creation and implementation of cancer-control plans in Africa. Ecancermedicalscience. 2019;13:938. [DOI] [PMC free article] [PubMed] [Google Scholar]