Abstract
Prior research suggests that the implicit biases of physicians are negatively associated with quality of medical care (Green et al., 2007; Sabin & Greenwald, 2012, see Fitzgerald & Hurst, 2017 for review) and patient satisfaction among minority patients (Cooper et al., 2012; Hagiwara et al., 2013; Penner et al., 2010). However, relatively little is known about how physicians express these subtle forms of bias in patient interactions. This study examined the implicit and explicit anti-Hispanic biases of 53 resident physicians and the relationship between anti-Hispanic bias and language use during outpatient medical appointments with 291 Hispanic patients. Physician implicit bias was positively associated with use of interrogatives and work-related words and negatively associated with the use of prepositions and relativity-related words (e.g., words related to time and the future). These findings contribute to the growing body of evidence suggesting that, in addition to nonverbal and paraverbal behaviors, providers may communicate implicit bias to patients through the words they use during a clinical visit.
Keywords: patient care, implicit bias, language use
Previous studies indicate that healthcare providers hold negative stereotypes (beliefs) and prejudices (attitudes) toward a variety of underserved patient groups (Maina et al., 2018; Zestcott et al., 2016). One implication is that these biases operate implicitly, that is, they come to mind so quickly that providers do not realize they are using them in making lower quality medical decisions about a stigmatized patient (see Fitzgerald & Hurst, 2017 for review). They may also fail to recognize that they are communicating their biases in a way that lowers patient satisfaction (Cooper et al., 2012; Hagiwara et al., 2013; Penner et al., 2010). The automatic communication of bias in a clinical context may play an important role in reducing the quality of care for underserved patients and contribute to racial and ethnic disparities in health outcomes.
However, at present, the pathways by which providers communicate implicit bias to patients are not well understood. Studies suggest that implicit bias manifests through nonverbal mannerisms, such as eye contact, speech errors, and subtle avoidance behaviors that convey dislike or unease in the presence of stigmatized individuals (e.g., Dovidio et al., 2002; 2006; Trawalter et al., 2009). Bias can also seep into subtle forms of verbal behavior that extend beyond content. For example, Johnson et al. (2004) found that physicians displayed more verbal dominance, less positive affect, and less patient-centered communication with African-American (compared with White) patients. Among physicians who showed high implicit activation of the noncompliance stereotype about African-American patients, Cooper et al. (2012) found a slower rate of speech and lower patient centeredness during clinical encounters. Whereas these studies suggest that verbal, nonverbal and paraverbal cues contribute to the communication of implicit bias, few studies have examined the role that automatic aspects of language play in this process.
The present research examines the possibility that implicit bias leaks into interaction through non-semantic aspects of the words that providers use during a clinical encounter (Falkenstein et al., 2016; Hagiwara et al., 2017). We sought to document how the structure and form of the language that providers use (beyond content and semantics) reflects the biases they express to their patients. Documenting novel linguistic markers of implicit bias improves our growing understanding of, and ability to address, the full process by which providers unintentionally communicate bias during interaction with underserved patients.
Examining implicit verbal bias in patient care
Contemporary research suggests that language provides a unique insight into the automatic processes that govern social interaction. Beyond the content of the spoken word, many of the function words people use in speech, (e.g. pronouns, verbs, and prepositions) communicate how people are thinking and feeling, their focus of attention, recognition of status differences, the fluency of group processes, and other aspects of the social class and personality of the speaker (e.g., Chung & Pennebaker, 2007; Pennebaker, 2011). It is widely assumed that the use of function words occurs automatically or implicitly (Mehl et al., 2017; Tausczik & Pennebaker, 2010). Whereas people are capable of choosing their words carefully, in many conversations, function words are generated automatically as the bridges between semantic words that give syntax meaning (Mehl et al., 2017). Thus, the automatic use of function words suggests that it may be one avenue for communicating implicit bias.
In a clinical context, patterns of physician word use covary with health outcomes. In a recent study, Falkenstein and colleagues (2016) recorded 145 interactions between six surgeons and their patients and examined the use of words related to rapport (pronoun use and language style matching), the patient’s future (verb tense), emotional tone (positive and negative emotion words), and the sharing of information (cognitive process words). The results showed that physicians used more plural first person pronouns and future tense than patients, which according to the researchers, may reflect the physicians’ aim to create a partnership with the patient. Physicians also demonstrated a relatively high level of language style matching, with patients, which was mostly accounted for by high correspondence between the number of words used, verb tense, and the use of negative emotion words. Finally, physician word use predicted patient satisfaction and adherence to pre- and post-operative directives. This suggests that beyond their semantic meaning, physician word use with patients can have an impact on the quality of the interactions and care they provide. However, few studies to date have examined if implicit bias relates to the words that physicians use when interacting with underserved patient groups.
We propose that there is a relationship between intergroup biases and language that includes the automatic use of function words during intergroup interaction. Biases like negative stereotypes and emotions may relate to the use of function words because people associate parts of speech with other concepts stored in memory (von Hippel et al., 2008). When activated, people may automatically use certain pronouns, verbs, prepositions, and other function words while talking to an outgroup member, that they would not use when communicating with a member of their ingroup, or with other outgroup members to whom the stereotypes and prejudices do not apply. This expression of verbal implicit bias is consistent with previous theory and research on the relationship between prejudice, discrimination and language (e.g., Collins & Clement, 2012; Maass et al., 2014). For example, Ng (2007) observes that while sexist language may have an evolutionary neural substrate, people acquire and rehearse it through exposure to cultural and political discourse (e.g., the media), which can foster automatic encoding of sexist pronoun usage (e.g., masculine generics like “he” or “guys”) and word ordering (“men and women”, see Maass et al., 2014; see also MacArthur et al., 2020).
People also express implicit verbal bias through the use of abstraction. In work on the Linguistic Intergroup Bias, Maas and colleagues (1989) found that when referring to stereotype incongruent behavior of an outgroup member, people use relatively concrete descriptors, but when referring to stereotype congruent behaviors, people use abstract descriptors. Whereas the use of abstraction can be a conscious, deliberate process, researchers also maintain that these linguistic processes can reflect automatic associations between components of language like verbs and adjectives, and stereotypes that people hold about race (von Hippel et al., 1997) and gender (Siegling et al., 2014). For example, people who display greater Linguistic Intergroup Bias also tend to evaluate a Black person as more threatening than a White person (von Hippel et al., 1997). In health care, physicians use different levels of abstraction to describe the goals and behaviors of different patient groups (Gallois et al., 2015), and patients use different levels of abstraction to describe interactions with physicians (Watson & Gallois, 2002). These health-related linguistic patterns may also occur without conscious deliberation.
Research on interracial interaction suggests that implicit bias may cause physicians to engage in more negative nonverbal and paraverbal behaviors (Penner et al., 2010; Cooper et al., 2012; see Hagiwara et al., 2020) during interactions with stigmatized minorities. If these biased communication behaviors are also encoded with linguistic patterns, they could be expected to correspond with the linguistic categories investigated by Falkenstein and colleagues (2016). Specifically, when physicians interact with patients, their implicit bias may predict lower use of words that convey rapport (e.g., first person plural pronoun use; e.g., Karan et al., 2019), less focus on the patient’s future (verb tense; e.g., Brianza & Demiray, 2019), more negative than positive emotion (positive and negative emotion words; e.g., Krejtz et al., 2020), and less sharing of information (cognitive processing words; e.g., Burke & Dollinger, 2005). Hagiwara and colleagues (2017) reported some evidence consistent with our reasoning. In their study, 14 non-Black primary care physicians completed measures of implicit and explicit prejudice toward Blacks before recording interactions with 117 Black patients. Analyses showed that physicians with higher implicit prejudice used more first-person plural pronouns, and more anxiety-related words. The present study examines the relationship between implicit bias and language use when physicians interact with Hispanic patients during a clinical encounter.
Finally, several individual differences may relate to the words providers use when expressing implicit bias to patients. For example, physicians who are internally motivated to respond without prejudice toward a specific patient group may express lower implicit bias than physicians who are motivated to respond without prejudice because of external pressures (Plant & Devine, 1998; see Green et al., 2007). Physicians who tend to take the perspective of their patients may also show lower implicit bias (Blatt et al., 2010). The way that physicians think about their own biases, and how they attempt to manage them during an interaction with underserved patients, may determine their expression of implicit bias. For example, those with high implicit bias may endorse a color-blind ideology and the belief that prejudice is immutable, and they may be more likely to use escape or avoidance strategies to manage interracial interactions (Neel & Shapiro, 2012). In contrast, adopting mitigation strategies in difficult interracial interactions may reflect a lower level of automatic prejudice and stereotyping toward underserved patient groups.
The present study uses Linguistic Inquiry and Word Count (LIWC) software (Pennebaker et al., 2015) to examine the presence of linguistic markers of bias in the natural conversations between resident physicians and Hispanic patients during out-patient medical care. The primary research questions were: Are there linguistic markers of implicit and explicit bias in the language physicians use during interaction with Hispanic patients? And are there demographic, motivational, or emotional correlates of physician verbal implicit bias?
Method
Participants
Resident physicians in Internal Medicine and Family Medicine at the University of Arizona and their patients served as participants in this study1. Power analysis (Spybrook, et al., 2011) suggested that 50 residents (seeing 5 patients each) were needed to achieve our desired level of statistical power. To achieve this sample size, we recruited all willing residents between Spring 2015 and Summer 2016. In all, 59 residents were recruited. After exclusions (described below), the final sample consisted of 53 residents (29 female, 24 male, 49% White, 28% Asian or Asian American, 11% Hispanic2, all other races < 6%, Mage = 29.83, SDage = 3.61).
Three hundred forty-three adult Hispanic patients of the participant resident physicians consented to be part of the study. Patients were recruited at check-in for an outpatient medical appointment if their medical record listed their ethnicity or race as Hispanic, or if they requested that they conduct their appointment with the resident in Spanish. Twenty three patients were excluded because they did not self-identify as Hispanic. Additional exclusions were made due to recording errors (n = 17), being the sole patient associated with a particular resident (n = 6), being unable to reconsent the patient (n = 1), and due to very high wait times (n = 5). This left a final sample of 291 (183 female, 100 male, 8 unreported gender, 95% Hispanic, all other races < 5%, Mage = 46.36, SDage = 16.49) patient participants. Between 2 and 9 recordings were obtained from each resident physician (M = 5.62 patients, SD = 1.33).
Procedure
After consenting, residents completed online measures of implicit and explicit bias, their approach to intergroup interactions, demographics and medical training experiences. Approximately 2 to 4 weeks later we began recording outpatient visits.
Hispanic patients were recruited after arriving and being assigned to an exam room, prior to seeing a resident. After obtaining patient consent, an audio recording device (TASCAM DR-100MKiii audio recorder) was used to record the visit with the patient and resident. After the clinic visit, the resident and the patient completed survey measures of their perceptions of the clinic visit in different locations. In addition, the patients completed a demographic questionnaire that included questions about their age, gender, race, ethnicity, first language, years speaking English, SES, and parents’ country of origin.
Measures
Resident-level Measures.
Implicit Racial Bias.
Resident physicians first completed two Implicit Association Tests (IAT; Greenwald et al., 1998) to measure implicit prejudice (unpleasant versus pleasant associations to the group) and stereotyping (noncompliance associations to the group) of Hispanic patients. The IAT requires participants to simultaneously complete two sorting tasks. The first involves sorting White American vs. Hispanic American faces to the appropriate category using two keys on the keyboard. The second involves sorting words using the same two keys. For the prejudice IAT this involved sorting pleasant versus unpleasant words. For the stereotyping IAT the pleasant and unpleasant words were replaced with noncompliance and compliance words.
For half of all test blocks, each target group shares a response key with one of the conceptual categories (e.g. White American and pleasant share one response key while Hispanic American and unpleasant share a different response key). For the remaining test blocks, the pairings are switched (e.g. White American and unpleasant share a response key and Hispanic American and pleasant share a response key). To the extent that individuals associate a particular target category (e.g. Hispanic people) with a particular concept (e.g. unpleasant), this sorting should be easier when the target and concept share a response key.
For the IATs in this study, words and images of faces appeared on the screen one at a time. Participants categorized these images of faces and words as quickly and accurately as possible using the ‘E’ and ‘I’ keys on a computer keyboard. If a participant incorrectly categorized a face or word the program paused until the participant corrected their response. The amount of time to correct response was recorded and these response latencies were used to calculate IAT scores for each resident.
For both IATs, the images sorted were three White American males and three Hispanic American males ( see Bean et al., 2013). In the prejudice IAT, participants categorized these images while simultaneously sorting words related to the concepts pleasant versus unpleasant. For half of all test trials, the categories White American—pleasant and Hispanic American—unpleasant shared a response key. For the remaining trials, White American—unpleasant and Hispanic American—pleasant shared a response key. Trials in which White American—pleasant and Hispanic American—unpleasant shared a response key were considered compatible trials because they are compatible with the cultural biases that exist towards Hispanics in the U.S. Trials for which White American—unpleasant and Hispanic American—pleasant shared a response key were considered incompatible trials. For the stereotype IAT, participants categorized the same images but categorized them while also sorting words related to the categories reluctant versus compliant. Compatible trials were identified as White American—compliant and Hispanic American—reluctant response pairings, whereas incompatible trials were identified as White American—reluctant and Hispanic American—compliant response pairings.
Table 1 illustrates the order in which participants completed practice and test blocks and provides information on the number of trials completed in each block. After practicing each categorization task separately, the tasks are combined in blocks three and four. The order in which participants completed compatible and incompatible test blocks, as well as the order of the Prejudice IAT and Stereotype IAT, was counterbalanced.
Table 1.
Configuration of IATs
| Prejudice IAT | ||||
|---|---|---|---|---|
| Block # | “E” key response categories | “I” key response categories | Type of Block | # of Trials |
| 1 | pleasant words | unpleasant words | practice | 20 |
| 2 | White American faces | Hispanic American faces | practice | 20 |
| 3 | pleasant words White American faces |
unpleasant words Hispanic American faces |
test (compatible) | 20 |
| 4 | pleasant words White American faces |
unpleasant words Hispanic American faces |
test (compatible) | 40 |
| 5 | Hispanic American faces | White American faces | practice | 20 |
| 6 | pleasant words Hispanic American faces |
unpleasant words White American faces |
test (incompatible) | 20 |
| 7 | pleasant words Hispanic American faces |
unpleasant words White American faces |
test (incompatible) | 40 |
|
Stereotype IAT | ||||
| Block # | “E” key response categories | “I” key response categories | Type of Block | # of Trials |
| 1 | compliant words | reluctant words | practice | 20 |
| 2 | White American faces | Hispanic American faces | practice | 20 |
| 3 | compliant words White American faces |
unpleasant words Hispanic American faces |
test (compatible) | 20 |
| 4 | compliant words White American faces |
reluctant words Hispanic American faces |
test (compatible) | 40 |
| 5 | Hispanic American faces | White American faces | practice | 20 |
| 6 | compliant words Hispanic American faces |
reluctant words White American faces |
test (incompatible) | 20 |
| 7 | compliant words Hispanic American faces |
reluctant words White American faces |
test (incompatible) | 40 |
Note. Table presents a list of the blocks completed for each of the anti-Hispanic IATs used in this study. “E” key response categories lists the categories for which the participant was supposed to press the “e” key for a given block. “I” key response categories lists the categories for which the participant was supposed to press the “i” key for a given block. The order of test blocks (compatible and incompatible) was counterbalanced across participant as was the order in which participants completed the two IATs.
All response latencies for each participant were converted into a d-score (Greenwald et al., 2003). Higher d-scores indicated greater implicit prejudice towards Hispanics or Hispanic = reluctant stereotypic association.
Explicit Bias Measure (α=0.75).
The explicit bias measure was adapted from the Modern Racism Scale (McConahay, 1986). Participants were asked to self-report their agreement with 9 statements related to ant-Hispanic prejudice (e.g. “Discrimination against Hispanics is no longer a problem in the United States.”).
Approaches to Intergroup Interactions.
Participants completed several other scales to measure motivational and emotional aspects if residents’ approaches to interactions with members of other groups. First, they completed the Internal (IM) & External (EM) Motivation to Respond without Prejudice scale (Plant & Devine, 1998; αIM=0.70, αEM=0.75) to examine the extent to which they feel internal and external pressure to appear non-biased. Next, they completed the perspective taking subscale of the Perspective Taking and Empathic Concern Scale (Davis, 1983; α=0.83 Participants completed items assessing the extent to which they believe prejudice is immutable (Neel & Shapiro, 2012, α=0.88), a single item assessing receptiveness to feedback about racial bias, a measure of colorblind ideology (α=0.89 ) and self-reported how they would respond to difficult interracial interactions (see Neel & Shapiro, 2012). A complete list of these survey items can be found in online Appendix A (https://osf.io/px6c5/?view_only=b0965e271ba7494fb41aaf2f2aaca572).
Patient-Level Variables.
Language Data.
For each patient visit, the audio recording was professionally transcribed (by Datagain, a HIPAA-compliant transcription and translation service; http://datagainservices.com/). Any Spanish language on the recordings was transcribed in Spanish and then translated verbatim into English. Finally, a trained bilingual research assistant reviewed the transcript and translation for accuracy. Resident language was separated from the transcript and processed using the Linguistic Inquiry and Word Count software (LIWC, 2015, Pennebaker et al., 2015). LIWC is currently the best validated and most widely used computerized text analysis tool in the social sciences (Mehl, 2006). LIWC analyzes text by comparing each word in a text document to an internal dictionary. LIWC calculates the percentage of total words in a given text that match a set of pre-determined grammatical or semantic category of target words (e.g. articles, prepositions, or work-related words). Examples of words from each language category can be found in online Appendix B.3
Results
Resident Implicit Bias
Online Appendices C and D present demographic characteristics of the resident and patient samples. To examine whether resident physicians held implicit stereotypes and prejudice, on average, one-sample t-tests were conducted to compare average IAT scores to a neutral score 0. Figure 1 presents the distribution of IAT scores on the prejudice and stereotype measures. On average, residents demonstrated significant implicit anti-Hispanic prejudice, M = 0.37, SD = 0.42, t(52) = 6.41, p < .001, 95% CI (0.25, 0.48), Cohen’s d = 0.88, indicating that residents associated Hispanics with negatively-valenced words and Whites with positively-valenced words to a greater extent than the reverse. Similarly, residents displayed significant implicit Hispanic-noncompliance stereotypes, M = 0.26, SD = 0.40, t(52) = 4.73, p < .001, 95% CI (0.15, 0.37), Cohen’s d = 0.65.
Figure 1.
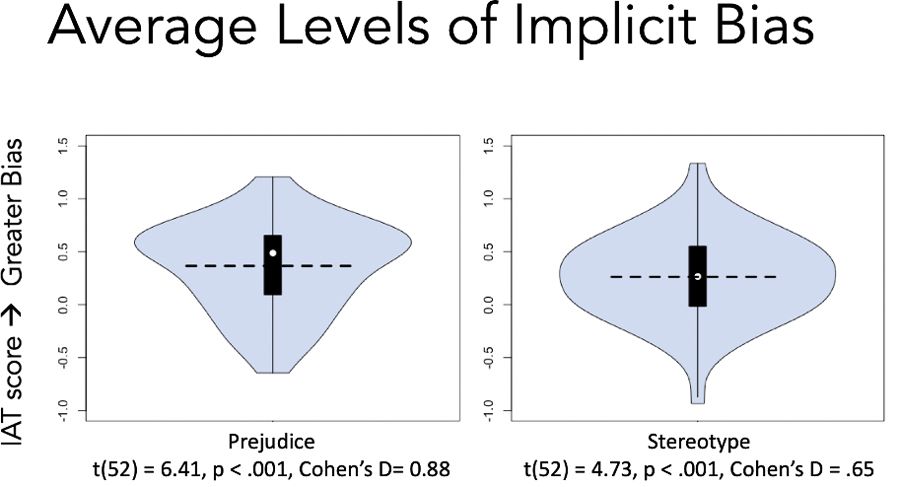
Violin plots of IAT scores for the anti-Hispanic prejudice (left) and stereotype (right) measures. Violin plots visualize a boxplot superimposed over the distribution of responses. The white dot represents the median IAT d-score. The horizontal line represents the mean IAT d-score.
The two measures of implicit bias were strongly correlated, r(51) = 0.64, p < .001, 95% CI (0.44, 0.77). Thus, they were averaged to create a single implicit bias score for each resident. The aggregate measure of implicit bias was also significantly different from 0, M = 0.31, SD = 0.37, t(52) = 6.10, p < .001, 95% CI (0.21, 0.42), Cohen’s d = 0.84. Resident implicit bias was moderately correlated with explicit bias, Mexplicit = 2.48, SD = 0.78, r(51) = 0.38, p = .01, 95% CI (0.12, 0.59).
Resident-Level Correlates of Resident Physician Bias
To understand what physician characteristics were associated with implicit and explicit bias, we examined bivariate relationships between the resident-level survey measures and implicit bias and explicit bias, separately. Tables 2 & 3 (found online at this link: https://osf.io/px6c5/?view_only=b0965e271ba7494fb41aaf2f2aaca572) present these correlations and mean differences.
On average, there were no differences in the level of implicit bias for resident age, gender, ethnicity (Hispanic vs. non-Hispanic), race, or first language, all ps > .05. However, residents in the internal medicine programs demonstrated higher levels of implicit anti-Hispanic bias than participants in the family medicine programs, t(51) = 2.47, p = 0.02, 95% CI = (0.05, 0.48), Cohen’s d = 0.72. Further, participants who demonstrated higher levels of implicit anti-Hispanic bias reported engaging in less perspective taking: r(51) = −0.37, p = 0.01, 95% CI (−0.58, −0.11, endorsed a colorblind racial ideology: r(51) = 0.33, p = 0.02, 95% CI (0.07, 0.55), and expressed higher external motivation to control prejudice: r(51) = 0.28, p = 0.05, 95% CI (0.01, 0.51).
On the measure of explicit prejudice toward Hispanics, residents in the internal medicine programs displayed higher average levels compared to residents in the family medicine programs, t(51) = 3.28, p = 0.002, 95% CI (0.28, 1.15), Cohen’s d = 0.92. Additionally, participants higher in explicit bias self-reported less perspective taking: r(51) = −0.41, p < 0.001, 95% CI (−0.67, −0.25), greater endorsement of a colorblind racial ideology: r(51) = 0.33, p = 0.01, 95% CI (0.07, 0.55), were less appreciative of feedback on how to appear less racially biased: r(51) = −0.37, p = 0.01, 95% CI (−0.58, −0.11), and were less likely to adopt direct or indirect strategies when engaging in a difficult interracial interaction, direct: r(51) = −0.27, p = 0.05, 95% CI (−0.51, −0.00), indirect: r(51) = −0.37, p = 0.01, 95% CI (−0.58, −0.11).
Language Correlates of Resident Physician Bias
To account for non-independence introduced by collecting multiple recordings from the same resident physician, linear mixed effects models were used to estimate the relationship between resident implicit bias language. Each language variable was regressed on resident implicit bias and the intercept was allowed to vary as a function of resident (models that allowed for random slopes were also estimated, but did not converge in all cases, so models with random intercepts are presented for consistency). The same process was repeated for the explicit attitude measure.
Figure 2 presents the 10 strongest relationships between residents’ implicit bias and their language use with their patients. Six language categories were significantly associated with resident implicit bias: interrogatives, work-related language, future-oriented language, relativity language (i.e. words related to space, time and motion), time-related words (a subcategory of relativity language), and prepositions (e.g., shorter phrases). There was a positive association between resident implicit bias and the use of interrogatives. More implicitly biased residents used more interrogatives talking to their patients. This relationship persisted after controlling for explicit bias, b* = 0.21, p = .03, 95% CI (0.02, 0.39). There was no overall relationship between explicit bias and resident use of interrogatives. A similar pattern emerged for work-related language (e.g. “work”, “career”, “test”)—more implicitly biased residents used more work-related language. This relationship remained significant after controlling for explicit bias, b* = 0.18, p = .02, 95% CI (0.03, 0.34), and explicit bias was unrelated to the use of work-related language.
Figure 2.
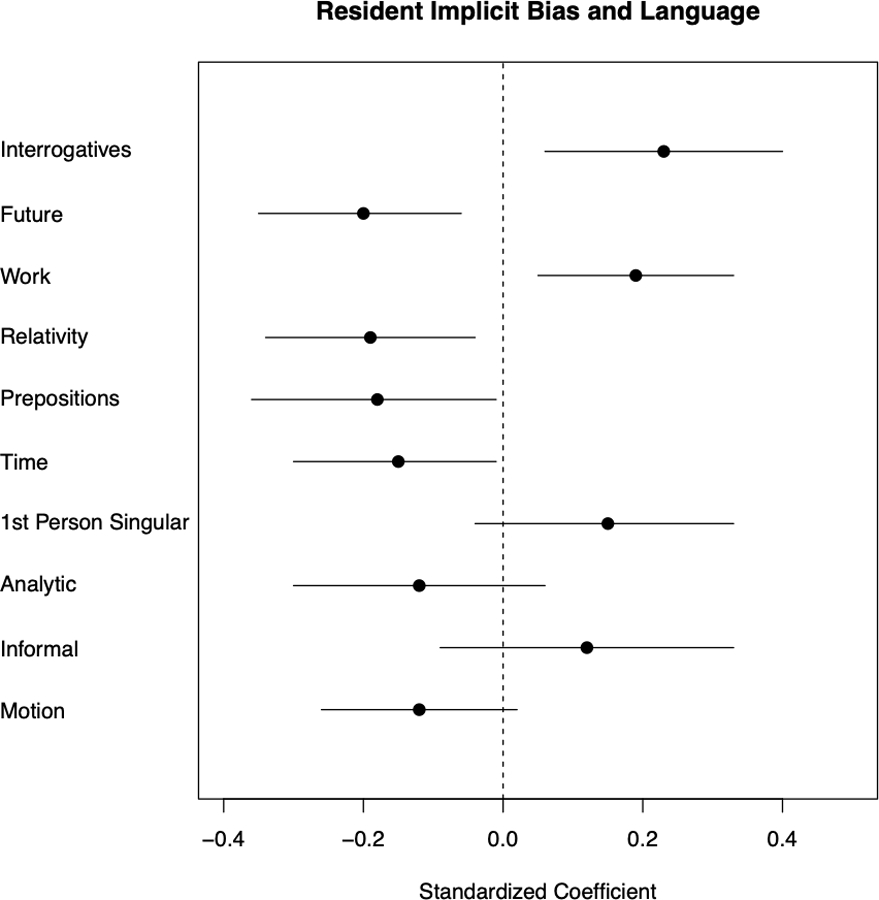
Standardized coefficients for the 10 largest relationships between implicit bias and LIWC language categories. Dots represent the value of the standardized coefficient for the relationship between implicit bias and the indicated language category. Bars represent the 95% confidence interval.
The remaining language variables were negatively associated with resident bias. Residents with higher implicit bias used less future-oriented language (e.g. “will”, “soon”, “then”), fewer relativity words, fewer time-related words (e.g. “hour”, “day”, “year”), and fewer prepositions (e.g. “in”, “on”, “through”. These relationships remained significant after controlling for explicit bias, future-oriented: b* = −0.17, p = .04, 95% CI (−0.33, −0.01); relativity: b* = −0.25, p = .004, 95% CI (−0.41, −0.09); time: b* = −0.18, p = .03, 95% CI (−0.34, −0.03); prepositions: b* = −0.20, p = .04, 95% CI (−0.39, −0.01).
Figure 3 presents the relationship between explicit bias and language correlates for the 10 strongest relationships. Resident explicit bias was related to two language variables. Participants with greater explicit anti-Hispanic bias used fewer insight-related (e.g. “think”, “know”) words and used fewer words related to sadness (e.g. “crying”, “grief”). The relationship between explicit bias and insight-related words remained statistically significant after controlling for implicit bias, b* = −0.20, p = .02, 95% CI (−0.36, −0.04). The relationship between explicit bias and sadness-related words was attenuated: b* = −0.13, p = .07, 95% CI (−0.27, 0.01).
Figure 3.
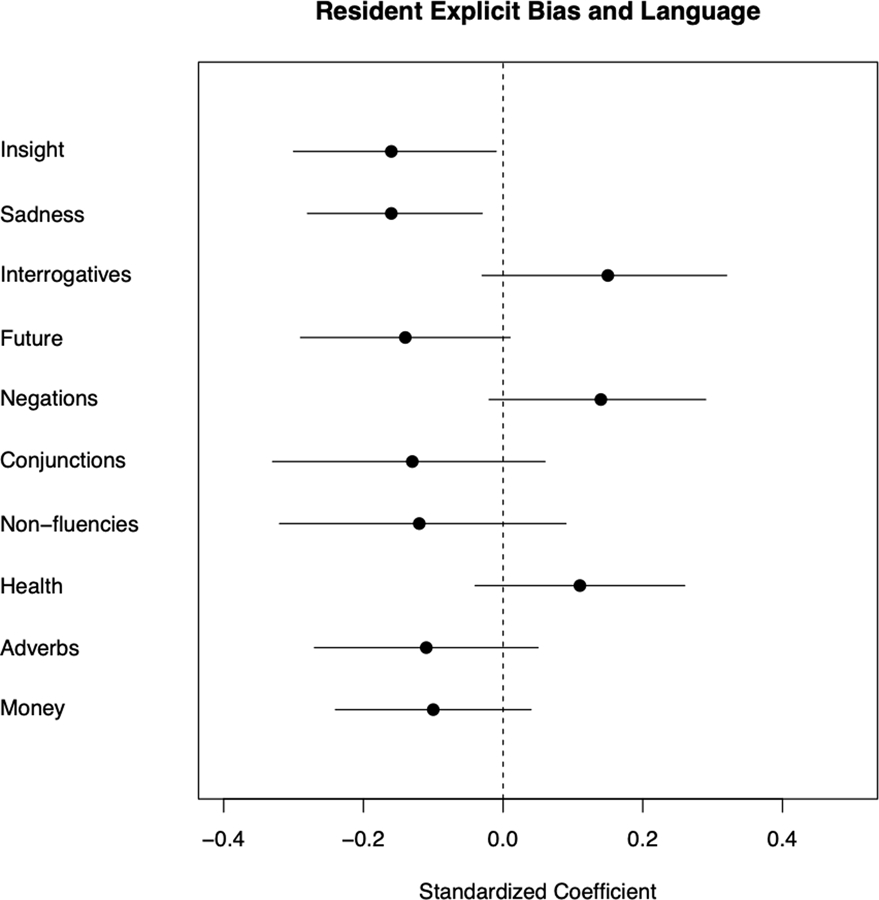
Standardized coefficients for the 10 largest relationships between explicit bias and LIWC language categories. Dots represent the value of the standardized coefficient for the relationship between explicit bias and the indicated language category. Bars represent the 95% confidence interval.
General Discussion
The results showed that implicit bias predicted linguistic patterns of communication by resident physicians when they were meeting with Hispanic patients in an out-patient clinic. Higher levels of implicit bias toward Hispanics predicted less use of relativity words, especially time and future-oriented words, and lower use of prepositions. Together, these linguistic patterns are consistent with the idea that the activation of negative emotions and stereotypes may correspond with less attention to future meetings and toward conveying less complex information to Hispanic patients (Pennebaker, 2011). The present study also found that higher levels of implicit bias predicted more use of interrogatives, suggesting that resident physicians with higher implicit bias were more likely to ask Hispanic patients questions during their meeting, and more words related to work, which are thought to reflect a focus on personal concerns (Pennebaker et al., 2015). Whereas asking more questions and talking about personal concerns may reflect higher concern about the patient’s welfare, these patterns may also reflect concerns associated with implicit stereotypes about medical non-adherence.
The relationship between implicit bias and language remained after controlling for the influence of explicit prejudice towards Hispanics, suggesting that language represents a unique pathway by which providers communicate implicit bias to patients during a clinical encounter. Explicit prejudice toward Hispanics also predicted specific linguistic patterns during the meetings with patients, although only one, less use of insight-related words (cognitive process), remained significant after controlling for implicit bias. These findings reinforce previous evidence that implicit and explicit forms of bias hold unique explanatory power in describing prejudice-related outcome measures (Greenwald et al., 2009).
The study did not find evidence for several linguistic patterns that theoretically should correspond with implicit bias. For example, higher levels of implicit bias did not predict more use of first person singular words as reported in other, smaller scale studies with more experienced physicians (Hagiwara et al., 2017). Implicit bias also did not relate to the use of negative and positive emotion words. One reason may be that according to Sun and colleagues (2019), LIWC’s method for analyzing positive and negative emotion words may not track positive and negative experiences as predicted. However, people may not convey implicit bias through positive and negative emotion words if in spoken language, positive and negative emotion words tend to be more consciously chosen (“happy”, “sad”).
The results also revealed novel correlates of the implicit bias resident physicians hold toward Hispanics. First, internal medicine residents expressed higher levels of implicit bias, and higher explicit prejudice towards Hispanics, than residents from family medicine. Other studies have reported differences across provider training and specialties (e.g., physicians versus nurses, Liang et al., 2019; Sabin et al., 2015) which may reflect differences in the background and training of students who self-select into various programs, differences in the programs themselves, or a combination of both influences. Also consistent with previous research, higher resident implicit bias related to less perspective taking and greater external motivation to control prejudice. Higher implicit bias and explicit prejudice toward Hispanics related to higher endorsement of adopting a color-blind ideology about race in the clinic. Additionally, higher explicit anti-Hispanic bias predicted being less appreciative of feedback on how to appear less racially biased and less desire to adopt direct or indirect approach strategies when engaging in a difficult interracial interaction. These findings suggest that for some providers, increasing awareness may be insufficient to mitigate verbal expressions of bias. Physicians with high implicit bias may also need to learn more about the value of multiculturalism and acquire more productive strategies for interacting with underrepresented patients.
Limitations and future directions
Whereas the present results are based on a larger sample size of physicians than previous studies, there are limitations to the findings. First, the high correlation between the measures of implicit prejudice and stereotyping necessitated combining them into one overall measure of “implicit bias.” While this helped guard against false positive findings, the specific patterns of words that the measure predicted may not fully replicate in studies that examine either implicit prejudice or stereotyping separately.
Another potential limitation is that the sample of physicians was restricted to medical residents in two specialties in one geographic region of the US. A broader range of physician experience in other regions of the US may produce different patterns of word use even when implicit bias is high (Hagiwara et al., 2017). The current study also focused exclusively on Hispanics living in the American Southwest as the target of the bias, and whereas the uniqueness of this sample is an important contribution to the literature on implicit bias in patient care, we acknowledge the possibility that the results are specific to this sample of minority group patients.
The analyses of word use in the current paper were restricted to word counts using LIWC, a closed-vocabulary, dictionary-based text analysis approach, which does not permit examination of other ways in which language may relate to the role that implicit bias plays in care for stigmatized patients (e.g., Linguistic Intergroup Bias; open-vocabulary approaches such as n-grams or topic models; Iliev, et al., 2015; Schwartz & Ungar, 2015). A full analysis of the way in which implicit bias influences patient care would examine the intersection between implicit verbal bias with other markers, such as nonverbal and paraverbal communication behaviors, with patient variables, such as the degree to which patients have experienced discrimination while seeking care in the past (Hagiwara et al., 2017), and the extent to which linguistic markers of bias are associated with different treatment outcomes.
Summary
The present study suggests that implicit verbal bias, defined as the linguistic patterns of words that physicians use when they interact with stigmatized patients, represents another pathway by which providers communicate their biases during a clinical encounter. Considering verbal implicit bias together with the evidence for nonverbal and paraverbal patterns of behavior that also correspond with implicit bias (Cooper et al., 2012; Penner et al., 2010) provides a more wholistic view of the processes by which implicit bias enters into patient care. More research is needed to complete our understanding of the degree to which these forms of biased communication influence patient outcomes, and if they do, the degree to which physicians can learn to change their communication patterns in ways that improve health outcomes for stigmatized patients.
Supplementary Material
Acknowledgments
This work was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Grant #5R01MD008940–05.
Footnotes
We have no conflicts of interest to report.
This research was submitted for ethics review and approved by the University of Arizona Institutional Review board, protocol number 1406364892A010.
Although the NIH term for this ethnic group is “Hispanic or Latino”, we choose to use the gender-neutral term Hispanic as it is seen as more inclusive.
Two other measures, measures of patient satisfaction and resident perceptions of the appointment, are discussed in another manuscript (Wolsiefer, et al., in prep) and are thus not reported here. We include this footnote for transparency.
References
- Bean MG, Stone J, Moskowitz GB, Badger TA, & Focella ES (2013). Evidence of nonconscious stereotyping of Hispanic patients by nursing and medical students. Nursing Research, 62(5), 362–367. 10.1097/NNR.0b013e31829e02ec [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blatt B, LeLacheur SF, Galinsky AD, Simmens SJ, & Breenberg L (2010). Does perspective-taking increase satisfaction in medical encounters? Academic Medicine, 85, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Brianza E, & Demiray B (2019). Future time perspective and real-life utterances about the future in young and older adults. GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry, 32, 161–173. 10.1024/1662-9647/a000216. [DOI] [Google Scholar]
- Burke PA, & Dollinger SJ (2005). “A picture’s worth a thousand words”: Language use in the autophotographic essay. Personality and Social Psychology Bulletin, 31(4), 536–548. [DOI] [PubMed] [Google Scholar]
- Chung C, & Pennebaker J (2007). The Psychological Functions of Function Words. In Fiedler K(Ed.), Social Communication (pp. 343–359). Psychology Press. [Google Scholar]
- Collins KA, & Clément R (2012). Language and prejudice: Direct and moderated effects. Journal of Language and Social Psychology, 31(4), 376–396. 10.1177/0261927X12446611 [DOI] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, & Inui TS (2012). The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health, 102(5), 979–987. 10.2105/AJPH.2011.300558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MH (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44(1), 113–126. [Google Scholar]
- Dovidio JF, Hebl M, Richeson JA, & Shelton JN (2006). Nonverbal communications, race, and intergroup interaction. In Manusov V & Patterson ML (Eds.), The Sage Handbook of Nonverbal Communication (pp. 481–500). Sage. [Google Scholar]
- Dovidio JF, Kawakami K, & Gaertner SL (2002). Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology 82, 62–68. [DOI] [PubMed] [Google Scholar]
- Falkenstein A, Tran B, Ludi D, Molkara A, Nguyen H, Tabuenca A, & Sweeny K (2016). Characteristics and correlates of word Use in physician-patient communication. Annals of Behavioral Medicine, 50 (5), 664–677, 10.1007/s12160-016-9792-x [DOI] [PubMed] [Google Scholar]
- Fitzgerald C, & Hurst S (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18(1), 1–18. 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallois C, Wilmott L, White B, Winch S, Parker M, Graves N, Shepherd N & Close E (2015). Futile treatment in hospital: Doctors’ intergroup language. Journal of Language and Social Psychology, 34(6), 657–671. 10.1177/0261927X15586430 [DOI] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, & Banaji R (2007). Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of General Internal Medicine, 22(9), 1231–1238. 10.1007/s11606-007-0258-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, & Schwartz JLK (1998). Measuring individual differences in implicit cognition: The Implicit Association Test. Journal of Personality and Social Psychology, 74(6), 1464–1480. 10.1037/0022-3514.74.6.1464 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, & Banaji MR (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85, 197–216. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann EL, & Banaji MR (2009). Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology, 97(1), 17–41. [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Eggly S, Dovidio JF, Gaertner SL, West T, & Albrecht TL (2013). Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Social Science & Medicine, 87, 123–131. 10.1016/j.socscimed.2013.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Slatcher RB, Eggly S, & Penner LA (2017). Physician racial bias and word use during racially discordant medical interactions. Health Communication, 32(4), 401–408. 10.1080/10410236.2016.1138389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Dovidio JF, Stone J, & Penner LA (2020). Applied racial/ethnic healthcare disparities research using implicit measures. Social Cognition, 38, s68–s97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliev R, Dehghani M, & Sagi E (2015). Automated text analysis in psychology: Methods, applications, and future developments. Language and Cognition, 7(2), 265–290. [Google Scholar]
- Johnson RL, Roter D, Powe NR, & Cooper LA (2004) Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health, 94(12), 2084–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karan A, Rosenthal R, & Robbins ML (2019). Meta-analytic evidence that we-talk predicts relationship and personal functioning in romantic couples. Journal of Social and Personal Relationships, 36(9), 2624–2651. [Google Scholar]
- Krejtz I, Rohnka N Holas P, Rusanowska M, & Nezlek JB (2020). Manifestations of clinical depression in daily life: A daily diary study of descriptions of naturally occurring events. Cognition and Emotion, 34(8), 1664–1675. [DOI] [PubMed] [Google Scholar]
- Liang J, Wolsiefer K, Zestcott CA, Chase D, & Stone J (2019). Implicit bias toward cervical cancer: Provider and training differences. Gynecologic Oncology, 153, 80–86. [DOI] [PubMed] [Google Scholar]
- Maass A, Salvi D, Arcuri L, & Semin GR (1989). Language use in intergroup contexts: The linguistic intergroup bias. Journal of Personality and Social Psychology, 57, 981–993. [DOI] [PubMed] [Google Scholar]
- Maass A, Arcuri L, & Suitner C (2014). Shaping intergroup relations through language. In Holtgraves TM (Ed.), The Oxford Handbook of Language and Social Psychology (pp. 157–176). Oxford University Press. 10.1093/oxfordhb/9780199838639.013.036. [DOI] [Google Scholar]
- MacArthur HJ, Cundiff JL, & Mehl MR (2020). Estimating the prevalence of gender-biased language in undergraduates’ everyday speech. Sex Roles, 82, 81–93. [Google Scholar]
- Maina IW, Belton TD, Ginzberg S, Singh A, & Johnson TJ (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the Implicit Association Test. Social Science & Medicine, 199, 219–229. [DOI] [PubMed] [Google Scholar]
- McConahay JB (1986). Modern racism, ambivalence, and the modern racism scale. In Dovidio JF & Gaertner SL (Eds.), Prejudice, discrimination and racism (pp. 91–125). Academic Press. [Google Scholar]
- Mehl M (2006). Quantitative text analysis. In Eid M & Diener E (Eds.), Handbook of Multimethod Measurement in Psychology (pp. 141–156). American Psychological Association. 10.1037/11383-011. [DOI] [Google Scholar]
- Mehl MR, Raison CL, Pace TWW, Arevalo JMG, & Cole SW (2017). Natural language indicators of differential gene regulation in the human immune system. Proceedings of the National Academy of Sciences, 114, 12554–12559. 10.1073/pnas.1707373114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neel R, & Shapiro JR (2012). Is racial bias malleable? Whites’ lay theories of racial bias predict divergent strategies for interracial interactions. Journal of Personality and Social Psychology, 103(1), 101–120. [DOI] [PubMed] [Google Scholar]
- Ng S (2007). Language-based discrimination: Blatant and subtle forms. Journal of Language and Social Psychology, 26(2), 106–122. 10.1177/0261927X07300074 [DOI] [Google Scholar]
- Pennebaker JW (2011). The Secret Life of Pronouns: What Our Words Say About Us Bloomsbury Press. [Google Scholar]
- Pennebaker JW, Booth RJ, Boyd RL, & Francis ME (2015). Linguistic Inquiry and Word Count: LIWC2015. Pennebaker Conglomerates www.LIWC.net.
- Penner LA, Dovidio JF, West TW, Gaertner SL, Albrecht TL, Dailey RK, & Markova T (2010). Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology, 46(2), 436–440. 10.1016/j.jesp.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant EA & Devine PG (1998). Internal and external motivation to respond without prejudice. Journal of Personality and Social Psychology, 75(3), 811–832. [DOI] [PubMed] [Google Scholar]
- Sabin JA, & Greenwald AG (2012). The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American Journal of Public Health, 102, 988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Riskind RG, & Nosek BA (2015). Health care providers’ implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health, 105, 1831–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz HA, & Ungar LH (2015). Data-driven content analysis of social media: a systematic overview of automated methods. The ANNALS of the American Academy of Political and Social Science, 659(1), 78–94. [Google Scholar]
- Siegling AB, Eskritt M & Delaney ME (2014). A Preliminary Investigation into Effects of Linguistic Abstraction on the Perception of Gender in Spoken Language. Current Psychology 33, 479–500. 10.1007/s12144-014-9224-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spybrook J, Bloom H, Congdon R, Hill C, Martinez A, & Raudenbush S (2011). Optimal design for longitudinal and multilevel research: Documentation for the optimal design software version 3.0. University of Michigan Retrieved from http://sitemaker.umich.edu/group-based/optimal_design_software.
- Sun J, Schwartz HA, Son Y, Kern ML, & Vazire S (2019). The language of well-being: Tracking fluctuations in emotion experience through everyday speech. Journal of Personality and Social Psychology, 118(2), 364–387. [DOI] [PubMed] [Google Scholar]
- Tausczik YR, & Pennebaker JW (2010). The psychological meaning of words: LIWC and computerized text analysis methods. Journal of Language and Social Psychology, 29(1), 24–54. [DOI] [Google Scholar]
- Trawalter S, Richeson J & Shelton J (2009). Predicting behavior during interracial interactions: A stress and coping approach. Personality and Social Psychology Review, 13, 243–268. 10.1177/1088868309345850. [DOI] [PubMed] [Google Scholar]
- von Hippel W, Sekaquaptewa D, & Vargas PT (1997). The Linguistic intergroup bias as an implicit indicator of prejudice. Journal of Experimental Social Psychology, 33, 490–509. 10.1006/jesp.1997.1332. [DOI] [Google Scholar]
- von Hippel W, Sekaquaptewa D, & Vargas PT (2008). Linguistic markers of implicit attitudes. In Petty RE, Fazio RH, & Briñol P (Eds.), Attitudes: Insights from the new implicit measures (pp. 429–458). Psychology Press. [Google Scholar]
- Watson B, & Gallios C (2002). Patients’ interactions with health providers: A linguistic category model approach. Journal of Language and Social Psychology,21(1), 32–52. [Google Scholar]
- Wolsiefer K, Stone J, Mehl M, Moskowitz GB, Cagno C, & Zestcott CA Examining the Association between anti-Hispanic implicit bias of Resident Physicians and Patient Satisfaction [Unpublished Manuscript]. Department of Psychology, University of Arizona
- Zestcott CA, Blair IV, & Stone J (2016). Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Processes & Intergroup Relations, 19, 528–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


