Abstract
Background:
The aim of this study was to evaluate the behavioral performance of a selection of currently available hearing aid apps in patients with mild hearing loss.
Methods:
We investigated 3 user-friendly hearing aid apps (EarMachine, Sound Amplifier, and Petralex) with real-ear measurement, warble-tone audiometry, word recognition testing in unaided and aided conditions, and hearing-in-noise tests in quiet and noise-front conditions in a group of users with mild hearing impairment (n = 7) as a pilot for a future long-term investigation. Results from the apps were compared with those of a conventional hearing aid.
Results:
Hearing aids showed greater gain at 1 and 3 kHz than hearing aid apps in real-ear insertion gain of real-ear measurements. Hearing aids tended to have greater gain than hearing aid apps at 2 and 3 kHz in the sound field audiometry test. The clinical performance of the listeners tended to be better when using a hearing aid and Petralex (13% and 6% improvement in word recognition score, respectively), while EarMachine and Sound Amplifier conferred limited user benefit. The hearing aid apps did not improve signal-to-noise ratio in comparison with the unaided condition in the hearing-in-noise test.
Conclusions:
Some hearing aid apps were beneficial for patients with mild hearing loss in terms of amplification, but participants using the apps showed no improvements in hearing-in-noise tests.
Keywords: Hearing aid apps, hearing loss, smartphone, hearing aids, hearing disability
Introduction
In 2018, the World Health Organization estimated that there were 466 million people worldwide with hearing loss and that this would be likely to increase up to 900 million by the end of 2050.1 Despite considerable evidence of the benefits of using conventional hearing aids,2 much of the hearing-impaired population has not undergone any hearing rehabilitation. Numerous barriers to hearing aid adoption still remain in different parts of the world, including cost,3 lack of availability of trained professionals,4 the acceptance of hearing loss stigmatization, and lack of internal or external motivations.5 It follows that many with hearing impairment wait a long time before seeking treatment (8.9 years on average).6 Despite the need for a better understanding, the literature has already highlighted relationships between hearing disabilities and the incidence of dementia and other later-life disorders.7,8 Therefore, early intervention may be crucial to reduce the influence of hearing impairment on these adverse events. Currently, numerous devices are available for people with mild-to-moderate hearing loss; however, this population is more likely to wait for their hearing to worsen before seeking interventions.
A number of diverse solutions are being developed to reach larger numbers of hearing-impaired people. Governments are aware that hearing impairment is an important public health concern, and some are participating in improving accessibility to hearing care, for example, by training specialists and by helping patients to finance these services. Nevertheless, these initiatives are mostly insufficient and a considerable proportion of people with hearing impairment remain underserved. As an intermediate step in the process of hearing care, there have been a number of advances in hearing loss prevention and awareness globally. For example, hearing test apps (e.g., HearWHO, HearZa, Ear scale, and Hearing Test) allow self-screening and provide information and advice to users. Studies have shown that such apps can be useful in settings where conventional pure-tone audiometry is not available9 or for large-scale hearing screening.10 Hearing-based apps are also considered to have the potential as gaming and exercise tools to improve cognitive performance, which can decline with age and other adverse events.11 Furthermore, there is a diversification of devices for hearing enhancement. Access without a medical prescription to low-cost hearing amplifiers, such as personal sound amplification products or over-the-counter hearing aids, is now widespread.
In hearing care or other fields, direct-to-consumer devices set aside the requirement of a specialist, to increase accessibility to health care. This raises the question of whether they can maintain a suitable degree of quality. The development of wearable health devices is increasing, and they show great potential to benefit the aging population despite numerous concerns about data privacy and management, controlled standards, and quality requirements.12 Therefore, there is a need to investigate the effectiveness of hearing aid apps as an intermediate solution for people without access to hearing care or people who wait a long time to seek help.13 However, these studies showed that there were many perceptible differences between the different apps, with some attempting to be as close as possible to what a hearing aid can provide, while others position themselves only as basic hearing amplifier apps.13-16 Moreover, few apps have been investigated, which makes the current overall conclusion about their benefits difficult to generalize.
This was a pilot study designed for a future evaluation of hearing aid apps under real-world conditions. The objective of the study was to evaluate their potential immediate benefits to users with mild hearing loss in a controlled environment.
Methods
Hearing Aid Apps, Devices, and Test Equipment
Three authors independently searched for hearing aid apps with the aim of providing information on the apps most likely to be found and used around the world. Therefore, as a first approach, we focused the search using the most commonly represented operating systems. The search was conducted in April through the App Store from Apple and Google Play using the keywords “hearing aid apps,” “sound amplifier,” and “hearing amplifier.” At the same time, we searched for apps on the search engines Google, Safari, and Naver with the addition of “smartphone” and “mobile” to the list of keywords. The search engines allowed us to determine which apps were the most cited and to identify those providing information about their developers and their structure. After the search using keywords, we identified the different apps that would match the criteria of the smartphone-based app. That is, apps that record sound from the environment using a microphone on the smartphone, process and amplify those sounds, and then transmit them through the earbuds to the user. Based on the apps that appeared most frequently at the top of the search results and the number of downloads when available, we selected 14 among a total of 27 apps initially identified. Seven were available on iOS and 7 were available on Android, with only 1 app (Petralex) available on both operating systems (Table 1).
Table 1.
Hearing Aid Apps, Listed by Mobile Operating System, Number of Installations, Provider, and In-App Purchase Information
| Apps | No. of Installations | Provider | Optional In-App Purchases | |
| iOS | ||||
| EarMachine | N/A | EarMachine LLC | Free | |
| Jacoti | Jacoti | Free | ||
| Mobile ears | Listen AS | Free | ||
| Hearing aid: sound enhancer | Emre Turgay | $1.99/week, $6.49/month | ||
| Fennex | Adam Palmquist | $4.99/month, $49.99/year | ||
| Listening device, hearing aids | Alexander Bredikhin | $9.99/week, $15.99/month $59.99/year | ||
| Petralex | IT4YOU | $5.99/month, $59.99/year | ||
| Android | ||||
| Sound amplifier | 10 000 000+ | Google LLC | Free | |
| DaMic | 1 000 000+ | SoomSoft | Free | |
| Petralex | 500 ,000+ | IT4YOU | $5.99/month, $59.99/year | |
| Super ear | 500 000+ | Liberation studio | Free | |
| EarShot | 50 000+ | Raja Muhammad Abdullah | Free | |
| Hearing aid master | 50 000+ | Sennikpro | Free | |
| Hearing aid maximizer | 10 000+ | SinCUR | Free | |
We selected Sound Amplifier, Petralex app for Android, which was most popular among android apps and is updated regularly, and EarMachine app for iOS. We used an iPhone 8 (Apple Inc., Cupertino, Calif, USA) for iOS apps, a Galaxy S8 (Samsung, Seoul, South Korea) for android apps, and 2 wired earbuds with built-in microphones provided with the smartphone by each manufacturer: Apple A1748 earpods with lightning connector and Samsung EO-IG955 earbuds tuned by AKG. We considered these devices to be among the most common types available to users because they were bundled with the mobile device. In addition, the earbuds were initially calibrated according to the corresponding smartphone, thereby accurately transmitting the sound level delivered by the device and controlling the output. We placed the earbuds into the participant’s ear canals toward to eardrum and it would represent an everyday listening setting. For the hearing aid, we tested the Siya 1 miniRITE coupled with two 85 dB receivers and single closed-ear tips (Oticon, Smorum, Denmark) with advanced features turned off, and the microphone directivity was omni microphone setting. All measurement materials were calibrated before the tests.
Recruitment
Eight fluent Korean speakers (2 males, 6 females; mean age 65.6 years, range 23-79 years) were selected from among patients who visited the Department of Otolaryngology of Seoul National University Hospital. Ethical committee approval was received from the Ethics Committee of Seoul National University Hospital (approval no: 2003-028-1109). All participants provided written informed consent for the present study. The inclusion criteria were acquired symmetrical, sensorineural, mild-to-moderate hearing loss, and currently using a smartphone. They did not have any previous experience with hearing amplification. We excluded those with external and middle-ear disease or anomalies and other communication problems. One of them did not complete the study due to withdrawal of consent. Due to technical problems, word recognition score (WRS) data from another patient were excluded from the data analyses. The pure tone average (PTAs) of each ear were calculated at 0.5, 1, 2, and 4 kHz. We considered mild hearing loss as a PTA range of 26-40 dB HL (WHO, ASHA). Otoscopy, pure-tone audiometry by air and bone conduction, and tympanometry were performed to confirm sensorineural hearing loss. The study was approved by the Institutional Review Board of Seoul National University Hospital (No. 2003-028-1109), Seoul, South Korea.
Real-Ear Measurement
Real-ear measurement was performed using Affinity 2.0 software (version 2.6.0; Interacoustics). We manually adjusted the gain control and parameters of the apps to match the targets. For hearing aids, this measurement is used to set the output based on the amplification target determined by the audiometric thresholds of the patient. All devices were set according to the NAL-NL2 targets prescribed for input levels of 65 dB SPL using the real-ear measurement to represent conversation sound level.17,18
Warble-Tone Audiometry Thresholds and Word Recognition Scores in Unaided and Aided Conditions
Before warble-tone audiometry threshold could be tested, Interacoustics AC 40(Interacoustics, Middelfar, Denmark) were calibrated. Sound-field audiometry was administered to the listener in both unaided and aided conditions (i.e., with the hearing aid apps and hearing aid) to measure the improvement in warble-tone audiometry at 0.5, 1, 2, 3, 4, and 6 kHz. We used a warble-tone to avoid standing waves. We calculated the WRS (percentage of words correctly repeated) using Korean standard monosyllabic word lists19 as a quiet speech test, which was composed of lists of monosyllabic words unknown to the subject. Twenty-five monosyllabic words per condition were presented at 50 dB HL under unaided and aided conditions as fixed output levels to find out the effectiveness of hearing aid and smartphone-based hearing aid apps. We then calculated the mean and standard deviation for the WRS under both conditions.
Hearing-in-Noise Test
The listener was played a list of 20 hearing-in-noise tests (HINTs) sentences per condition alongside stationary noise.20 The speech and noise were initially presented at 65 dB SPL (0 dB SNR) via a loudspeaker located in front of the participant. Using the transformed up-down methods described by Levitt in 1971 which is estimated percentile points other than 50% as stimulus level is increased or decreased after specific sequences of stimuli and responses.21 The level of the subsequent sentence was adjusted based on the response of the listener, while the noise levels remained constant. For the HINT, the subject was positioned 1 m in front of the speaker, and the speech reception threshold (SRT; sound level for the listener to achieve correct answers 50% of the time) in quiet and noise front conditions. The signal-to-noise ratio (SNR) needed for listeners to achieve correct answers 50% of the time was determined at a fixed level for the stimuli and by adjusting the sound level of the noise. Both measurements were conducted under unaided and aided conditions.
Results
Real-Ear Measurement
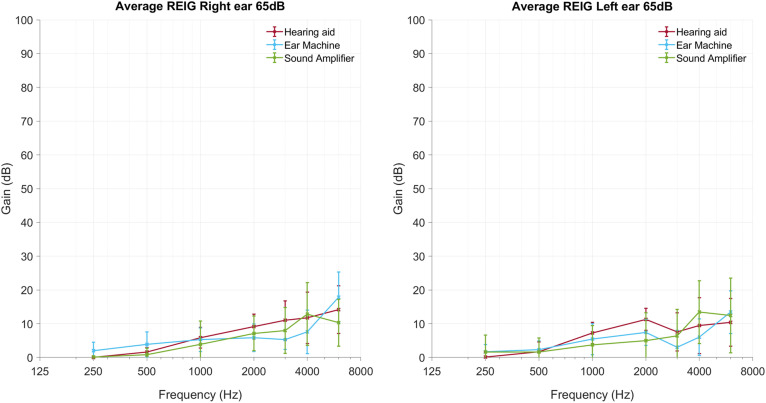
In real-ear insertion gain, hearing aids without advanced features showed greater gain at 1000 and 2000 Hz than hearing aids apps. EarMachine and Sound Amplifier apps showed greater gain at the 250 and 500 Hz than hearing aids, respectively (Figure 1).
Figure 1.
Real-ear insertion gain measured in subjects. REIG, real-ear insertion gains.
Warble-Tone Audiometry Thresholds and Word Recognition Scores in Unaided and Aided Conditions
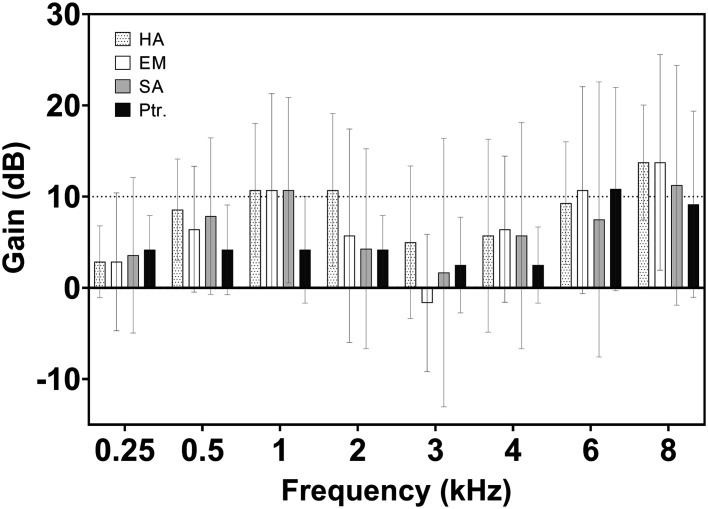
EarMachine and Sound Amplifier apps tested here tended to have lower gain than the hearing aid at 2 and 3 kHz, respectively (Figure 2). Petralex showed a slightly inferior gain from 1 to 3 kHz. The 3 apps also had lower WRS than the hearing aid, although the difference was not significant (Figure 3). We observed average speech intelligibility of 90% and 76% with the hearing aid and the EarMachine app, respectively, with the latter being only a slight improvement over the unaided condition. Petralex showed a better improvement of 6% over the unaided condition. The Sound Amplifier app showed no improvement compared with the unaided condition.
Figure 2.
Average sound-field warble-tone thresholds under unaided and aided conditions via a hearing aid or one of 3 apps (Petralex, EarMachine, and Sound Amplifier).
Figure 3.
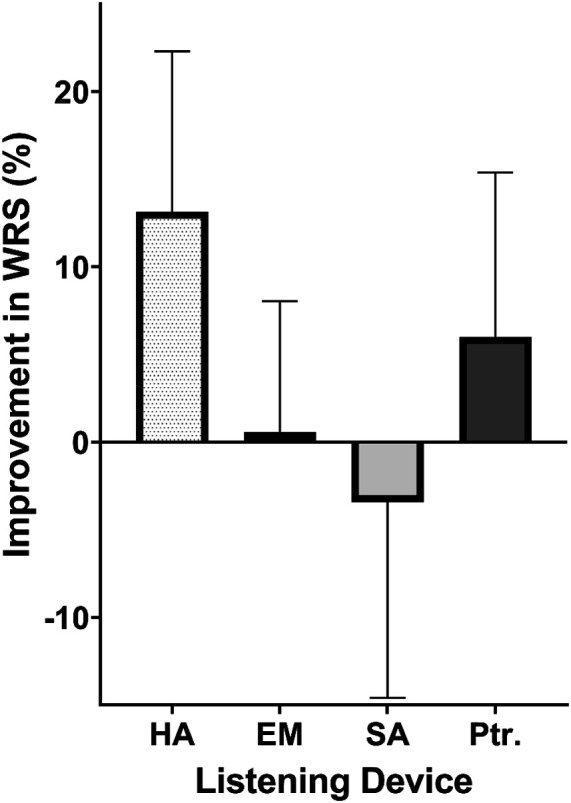
Improvement in word recognition scores compared to the unaided condition via a hearing aid or one of 3 apps (EarMachine, Sound Amplifier, and Petralex). Error bars indicate standard deviation. HA, hearing aid; EM, EarMachine; SA, Sound Amplifier; Ptr, Petralex.
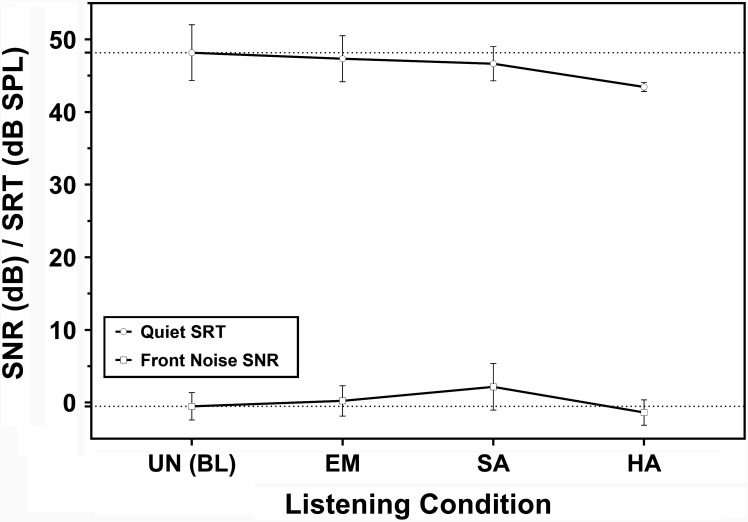
Hearing-in-Noise Test
Participants using the hearing aid showed consistent improvements in SNR in both quiet and noisy conditions (Figure 4). However, participants using the hearing aid apps showed no improvements in SNR compared with the unaided condition.
Figure 4.
HINT results in quiet (dotted line) and noisy (full line) conditions when participants were either unaided (UN) or aided (via a hearing aid or the EarMachine or Sound Amplifier apps). Error bars indicate standard deviation. EM, EarMachine; HA, hearing aid; HINT, hearing-in-noise test; SA, Sound Amplifier; SRT, speech reception threshold; SNR, signal-to-noise ratio.
Discussion
Our results showed that the hearing aid generally improved the listening conditions of subjects more than the EarMachine and Sound Amplifier apps. Additional data showed that Petralex had a higher WRS and, therefore, it could improve the intelligibility of speech.
Unexpectedly, none of the tested apps consistently improved speech recognition by users, although there was a slight shift in tests with EarMachine. Hearing-impaired users with the apps showed worse performance than those with the hearing aids on warble-tone audiometry because of lower gain at mid and high frequencies, which are important for speech understanding, but higher gain at a low frequency, which may worsen the speech understanding because of the upward spread of masking.22 When using the apps, no differences were observed compared to the unaided condition except with Petralex when calculating the WRS. These results indicate that the tested low-end apps may be unsuitable, and the single high-end app tested in this study might be more appreciated for the middle hearing loss patients. This study did not compare the advanced signal processing techniques such as noise canceling, speech enhancement, or microphone directionality. These techniques would improve the sound quality of devices. The sound quality of hearing aid apps would be another important consideration in real-world conditions.15,16
Apps are a fairly recent development, and their use is not currently widespread. Few studies have examined their sound quality or investigated their benefits to users over behavioral evaluations. Diverse electroacoustic data were collected and analyzed for some apps, while speech-in-noise was mostly used for behavioral evaluation. The general conclusion in the current literature is that hearing aid apps may be a viable intermediary before rehabilitation with a hearing aid.
To benefit the user, direct-to-consumer hearing devices first need to fulfill the requirements of usability and sound quality. Examinations of the usability parameter must answer the question: “Does it work?” De Sousa15 investigated the processing delay and other functional parameters of hearing aid apps. They reported that some apps performed poorly in terms of processing delay. Indeed, hearing devices need to be able to process the sound in a time short enough to improve speech perception. Intelligibility may be altered even if the quality of amplification itself is suitable.23-25 Numerous methods and parameters are available to evaluate the sound quality of a hearing device. The commonly used standards described by the American National Standards Institute (ANSI)26,27 and the International Electrotechnical Commission (IEC)28 are used to check the specifications of hearing aids as described by their manufacturers. These references have already been used for the electroacoustic analysis of direct-to-consumer hearing devices,29 including some hearing aid apps.13 Sound quality parameters related to the hardware or to certain features of apps were also investigated. Medwetsky16 studied the influence of the earbuds used with a smartphone and De Sousa15 analyzed the SNR improvement achieved with the NR feature. These devices do not need to pass safety tests within the scope of medical standards. However, these apps are made for hearing loss users. Therefore, we compared the behavioral performance on the basis of the commonly used methods for an aided hearing evaluation.
Compared with similar studies,13,15,16,30 this pilot study had too few subjects to provide general conclusions regarding the improvement of speech intelligibility. Further investigations with a larger sample size will allow us to compare more apps to hearing aids in terms of benefits under real-world conditions. We focused on low-end apps that were easy to use, which we considered a significant advantage for first-time users. We aimed to choose the earbuds bundle that would be most highly represented. The earbuds bundle may not provide enough high frequencies. Recently, the earbuds bundle shows better performance than the previous one in the high frequencies. In addition, high-end earphones and earbuds would provide the higher frequency gain and improve the final output.16
The accessibility and convenience of using apps are clearly advantageous, but may not offer enough benefits to use them when hearing impairment becomes significant. A number of apps have been introduced as hearing amplifiers, while others are marketed as hearing aids. Generalizing access to hearing care through smartphone-based apps also means increasing diversity without fixed standards. As in other fields of science, generalization and greater access to previously unavailable tools result in lower or missing quality control. Hearing aid apps are a response to a need for hearing care, but there is also a need for reliability. To generalize health care, a balance between the development of new tools and defined quality requirements is necessary. Apps that are regularly updated and the growing development of direct-to-consumer devices may allow hearing aid apps to play a more important role in hearing rehabilitation and awareness of the population in the future. We also expect major international companies to explore and invest in the development of access to health care, for example, Google has produced the app “Sound Amplifier,” and Apple Computer is also developing a hearing amplifier or hearing aid tool that will be accessible through their operating system.
Footnotes
Ethics Committee Approval: Ethical committee approval was received from the Ethics Committee of Seoul National University Hospital (approval no: 2003-028-1109).
Informed Consent: Written informed consent was obtained from all participants who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Conceptualization: W.N., M.K., J.H.L., S.H.O., M.K.P. Data collection and visualization: W.N., M.K. Writing – original draft: W.N., M.K. Writing—review and editing: W.N., M.K., M.K.P.
Acknowledgments: The author would like to thank Ms. Ye Jin Byeon for her help in collecting data.
Declaration of Interests: The authors declare that they have no conflict of interest.
Funding: This research was supported by a grant from Patient-Centered Clinical Research Coordinating Center funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0481, HC19C0128).
References
- 1. Deafness and hearing loss https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss . Geneva: World Health Organization; 2021. . Available at: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss. [Google Scholar]
- 2. Ferguson MA, Kitterick PT, Chong LY, Edmondson-Jones M, Barker F, Hoare DJ. Hearing aids for mild to moderate hearing loss in adults. Cochrane Database Syst Rev. 2017;9(9):CD012023. 10.1002/14651858.CD012023.pub2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Valente M, Amlani AM. Cost as a barrier for hearing aid adoption. JAMA Otolaryngol Head Neck Surg. 2017;143(7):647 648. 10.1001/jamaoto.2017.0245) [DOI] [PubMed] [Google Scholar]
- 4. Mulwafu W, Ensink R, Kuper H, Fagan J. Survey of ENT services in sub-Saharan Africa: little progress between 2009 and 2015. Glob Health Action. 2017;10(1):1289736. 10.1080/16549716.2017.1289736) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ritter CR, Barker BA, Scharp KM. Using attribution theory to explore the reasons adults with hearing loss do not use their hearing aids. PLoS ONE. 2020;15(9):e0238468. 10.1371/journal.pone.0238468) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Simpson AN, Matthews LJ, Cassarly C, Dubno JR. Time From hearing aid candidacy to hearing aid adoption: a longitudinal cohort study. Ear Hear. 2019;40(3):468 476. 10.1097/AUD.0000000000000641) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thomson RS, Auduong P, Miller AT, Gurgel RK. Hearing loss as a risk factor for dementia: A systematic review. Laryngoscope Investig Otolaryngol. 2017;2(2):69 79. 10.1002/lio2.65) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lin FR, Metter EJ, O'Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68(2):214 220. 10.1001/archneurol.2010.362) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin HH, Chu YC, Lai YH.et al. A smartphone-based approach to screening for sudden sensorineural hearing loss: cross-sectional validity study. JMIR MHealth UHealth. 2020;8(11):e23047. 10.2196/23047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Masalski M, Morawski K. Worldwide prevalence of hearing loss among smartphone users: cross-sectional study using a mobile-based app. J Med Internet Res. 2020;22(7):e17238. 10.2196/17238) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Frost E, Porat T, Malhotra P, Picinali L. A novel auditory-cognitive training app for delaying or preventing the onset of dementia: participatory design With stakeholders. JMIR Hum Factors. 2020;7(3):e19880. 10.2196/19880) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu L, Zhang J, Xie Y.et al. Wearable health devices in health care: narrative systematic review. JMIR MHealth UHealth. 2020;8(11):e18907. 10.2196/18907) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amlani AM, Taylor B, Levy C, Robbins R. Utility of smartphone-based hearing aid applications as a substitute to traditional hearing aids. The Hear Rev. 2013;20(13):16 18. [Google Scholar]
- 14. De Sousa KC, Moore DR, Motlagh-Zadeh L, Myburgh HC, Swanepoel DW. Do smartphone hearing aid apps work?. Hearing Journal. 2019;72(11):34. 10.1097/01.HJ.0000612588.11985.6a) [DOI] [Google Scholar]
- 15. De Sousa K, Moore D, Motlagh Zadeh L, Myburgh H, Swanepoel D. Do smartphone hearing aid apps work? Hear J. 2019;72:34. [Google Scholar]
- 16. Medwetsky L, Kelly K, Bakke M. Earphone models for iPhones: Surprising results when used with a hearing app; Hearing Review. 2020;27(1):22 25. [Google Scholar]
- 17. Verification of hearing devices using probe microphone measurements [internet]; 2021.. Available at: https://www.thebsa.org.uk/resources/guidance-on-the-verification-of-hearing-devices-using-probe-microphone-measurements/. Accessed 5 Oct 2021. [Google Scholar]
- 18. Ko Y, Lee JH. Clinical importance of sound-field speech recognition test for measurement of hearing aid benefit. Korean J Otorhinolaryngol-head Neck Surg. 2021;64(5):310 320. [Google Scholar]
- 19. Kim J-S, Lim DH, Hong H-N.et al. Development of Korean standard monosyllabic word lists for adults (KS-MWL-A). Audiol Speech Res. 2008;4(2):126 140. 10.21848/audiol.2008.4.2.126) [DOI] [Google Scholar]
- 20. Moon SK, Mun HA, Jung HK, Soli SD, Lee JH, Park K. Development of sentences for Korean Hearing in Noise Test (KHINT). Korean J Otorhinolaryngol-head Neck Surg . 2005;48(6):724 728. [Google Scholar]
- 21. Levitt H. Transformed up-down methods in psychoacoustics. J Acoust Soc Am. 1971;49(2):467. 10.1121/1.1912375) [DOI] [PubMed] [Google Scholar]
- 22. Klein AJ, Mills JH, Adkins WY. Upward spread of masking, hearing loss, and speech recognition in young and elderly listeners. J Acoust Soc Am. 1990;87(3):1266 1271. 10.1121/1.398802) [DOI] [PubMed] [Google Scholar]
- 23. Stone MA, Moore BC. Tolerable hearing aid delays. I. Estimation of limits imposed by the auditory path alone using simulated hearing losses. Ear Hear. 1999;20(3):182 192. 10.1097/00003446-199906000-00002) [DOI] [PubMed] [Google Scholar]
- 24. Stone MA, Moore BC. Tolerable hearing aid delays. II. Estimation of limits imposed during speech production. Ear Hear. 2002;23(4):325 338. 10.1097/00003446-200208000-00008) [DOI] [PubMed] [Google Scholar]
- 25. Stone MA, Moore BC, Meisenbacher K, Derleth RP. Tolerable hearing aid delays. V. Estimation of limits for open canal fittings. Ear Hear. 2008;29(4):601 617. 10.1097/AUD.0b013e3181734ef2) [DOI] [PubMed] [Google Scholar]
- 26. American National Standards Institute . Specification of hearing aid characteristics (ANSI S3.22-1987). New York: Acoustical Society of America; 1987. [Google Scholar]
- 27. American National Standards Institute. Specification of hearing aid characteristics (ANSI S3.22-2003). New York: Acoustical Society of America; 2003. [Google Scholar]
- 28. IEC. Measurement of the Performance Characteristics of Hearing Aids for Production, Supply and Delivery Quality Assurance Purposes. Geneva, Switzerland: Electroacoustics-Hearing Aids; 2005. [Google Scholar]
- 29. Callaway SL, Punch JL. An electroacoustic analysis of over-the-counter hearing aids. Am J Audiol. 2008;17(1):14 24. 10.1044/1059-0889(2008/003)) [DOI] [PubMed] [Google Scholar]
- 30. Martinez-Beneyto P, Franchella S, Alonso Rodriguez F.et al. Are smartphone applications (App) useful to improve hearing? Acta Otorhinolaryngol Ital. 2020;40(4):304 310. 10.14639/0392-100X-N0318) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a