Abstract
Coronavirus disease 2019 (Covid-19) is caused by severe acute respiratory syndrome type 2 (SARS-CoV-2). Covid-19 is characterized by hyperinflammation, oxidative stress, and multi-organ injury (MOI) such as acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Covid-19 is mainly presented with respiratory manifestations; however, extra-pulmonary manifestations may also occur. Extra-pulmonary manifestations of Covid-19 are numerous including: neurological, cardiovascular, renal, endocrine, and hematological complications. Notably, a cluster of differentiation 26 (CD26) or dipeptidyl peptidase-4 (DPP-4) emerged as a new receptor for entry of SARS-CoV-2. Therefore, DPP-4 inhibitors like sitagliptin could be effective in treating Covid-19. Hence, we aimed in the present critical review to assess the potential role of sitagliptin in Covid-19. DPP-4 inhibitors are effective against the increased severity of SARS-CoV-2 infections. Moreover, DPP-4 inhibitors inhibit the interaction between DPP-4 and scaffolding proteins which are essential for endosome formation and replication of SARS-CoV-2. Therefore, sitagliptin through attenuation of the inflammatory signaling pathway and augmentation of stromal-derived factor-1 (SDF-1) may decrease the pathogenesis of SARS-CoV-2 infection and could be a possible therapeutic modality in treating Covid-19 patients. In conclusion, the DPP-4 receptor is regarded as a potential receptor for the binding and entry of SARS-CoV-2. Inhibition of these receptors by the DPP-4 inhibitor, sitagliptin, can reduce the pathogenesis of the infection caused by SARS-CoV-2 and their associated activation of the inflammatory signaling pathways.
Keywords: Coronavirus disease 2019, Dipeptidyl peptidase-4, Sitagliptin, Inflammatory signaling pathways
Introduction
Coronavirus disease 2019 (Covid-19) is principally triggered by various variants of severe acute respiratory syndrome type 2 (SARS-CoV-2) including α, β, and omicron variants (Al-Kuraishy et al. 2021a; Schmidt et al. 2022). Covid-19 is characterized by hyperinflammation, oxidative stress, and multi-organ injury (MOI) such as acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (Al-Kuraishy et al. 2021b; Elekhnawy and Negm 2022). Covid-19 patients are frequently asymptomatic in most of the cases (nearly up to 85%). Nevertheless, 15% of Covid-19 patients may present with moderate to severe form due to the advancement of SARS-CoV-2 infection with the propagation of ALI. In addition, 5% of Covid-19 patients may develop a serious form due to the development of ARDS that requires ventilator support and mechanical ventilation (Al-kuraishy et al. 2022c; Attallah et al. 2021). Covid-19 is particularly presented with respiratory manifestations; however, extra-pulmonary manifestations may propagate a critical form of Covid-19. Extra-pulmonary manifestations of Covid-19 are numerous including: neurological, cardiovascular, renal, endocrine, and hematological complications (Onohuean et al. 2021; Al-Kuraishy et al. 2021c). Of interest, SARS-CoV-2 uses angiotensin-converting enzyme 2 (ACE2) as a receptor and entry-point in the host cells (Al-Kuraishy et al. 2021c). Down-regulation of ACE2 by SARS-CoV-2 induces dysregulation of the renin–angiotensin system with augmentation of vasoconstrictor angiotensin II (AngII) and reduction of vasodilator of Ang1-7 (Schmidt et al. 2022). These changes together with the oxidative and inflammatory disorders can cause endothelial dysfunction, coagulation disorders, and the development of critical ALI/ARDS (Al-Kuraishy et al. 2021b).
Notably, the cluster of differentiation 26 (CD26) or dipeptidyl peptidase-4 (DPP-4) emerged as a new receptor for entry of SARS-CoV-2 (Al-Kuraishy et al. 2021e). Therefore, DPP-4 inhibitors like sitagliptin could be effective in treating Covid-19. Thus, the main aim of the present critical review was to assess the potential role of sitagliptin in Covid-19.
DPP-4 inhibitors and viral infections
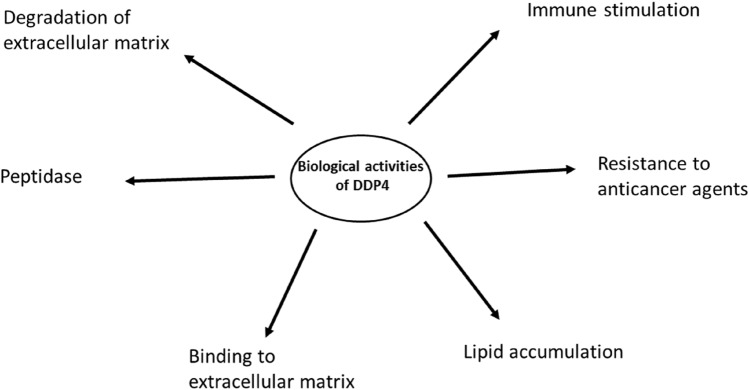
DPP-4 is highly expressed in different immune cells and they are involved mainly in the regulation of blood glucose and inflammation. DPP-4 induces cleavage of glucagon-like peptide (GLP-1) and other incretins (Al-Kuraishy et al. 2020). DPP-4 inhibitors are widely used and tolerated in the management of type 2 diabetes mellitus (T2DM) with minimal or no hypoglycemia as an adverse effect (Al-Kuraishy et al. 2020). DPP-4 receptors are also involved in the regulation of other biological processes like immune response during viral infections owing to their expression on T cells, B cells, natural killer (NK) cells (Elekhnawy et al. 2021a), and macrophages (Amori et al. 2007) as shown in Fig. 1.
Fig. 1.
Various biological activities of DPP-4
Previous meta-analyses illustrated that using of DPP-4 inhibitors was linked with a higher risk of respiratory viral infections (Amori et al. 2007). Similarly, a controlled study depended on the database of the World Health Organization (WHO) also implicates the use of DPP-4 inhibitors in increasing the risk of different viral infections (Yang et al. 2016). However, a recent meta-analysis by Yang et al. (2016) illustrated that uses of DPP-4 inhibitors were not related to increased risk of viral infections as compared with placebo. In addition, there is an updated meta-analysis which showed that that using DPP-4 inhibitors was not linked with a higher risk of respiratory viral infections (Grenet et al. 2021).
The immunological effects of DPP-4 inhibitors are related to the decrease of T cell activity and release of co-stimulatory chemokines and cytokines with upregulation of immunosuppressive cytokines (Yang et al. 2016; Grenet et al. 2021). Though these effects were not confirmed in experimental and preclinical studies.
These observations suggested that the uses of DPP-4 inhibitors in T2DM patients are safe and do not increase the risk of viral infections. In addition, immunomodulatory effects of DPP-4 inhibitors may reduce exaggeration of the immune response in viral infections; thereby decreasing the risk of immune-mediated tissue injury as in Covid-19 (Al-Kuraishy et al. 2021e).
DPP-4 inhibitors and Covid-19
Many recent studies reported that DPP-4 inhibitors are effective in decreasing the severity of SARS-CoV-2 infections (Al-Kuraishy et al. 2021e; Noh et al. 2021). Of note, DPP-4 receptors are highly expressed in the case of obesity and T2DM (Grenet et al. 2021). Upregulation of DPP-4 receptors in the respiratory tract in obese and T2DM patients increase the risk for SARS-CoV-2 infection (Noh et al. 2021). Thus, overexpression of the membrane-bound DPP-4 increases the entry of SARS-CoV-2 into the host cells and is associated with augmentation of Covid-19 severity (Krejner-Bienias et al. 2021). However, soluble DPP-4 (sDPP-4) which are mainly released from the activated T lymphocytes may have a protective activity by neutralizing SARS-CoV-2 spike protein and preventing the binding with the bounded DPP-4 (Krejner-Bienias et al. 2021). It has been shown that sDPP-4 is decreased in SARS-CoV-2 infection and is correlated with lymphopenia in patients suffering from severe Covid-19 (Krejner-Bienias et al. 2021).
Moreover, DPP-4 inhibitors inhibit the interaction between DPP-4 and scaffolding proteins which are essential for endosome formation and replication of SARS-CoV-2 (Bardaweel et al. 2021). Furthermore, DPP-4 inhibitors have potent anti-inflammatory effects by reducing interleukin (IL-6) serum levels in Covid-19 patients. This property may diminish the risk of the progress of the cytokine storm (Bardaweel et al. 2021). Remarkably, an Italian prospective study comprising 338 Covid-19 patients revealed that the use of sitagliptin was correlated with a significant reduction in hospitalization time, severity, and mortality (Solerte et al. 2020). A narrative review and meta-analysis demonstrated inconsistent findings on the association between the use of DPP-4 inhibitors and clinical outcomes of Covid-19 patients (Bonora et al. 2021).
In this state, most of after mentioned studies did not discuss the possible beneficial mechanistic pathways of DPP-4 inhibitors in the amelioration of inflammatory signaling pathways in SARS-CoV-2 infection.
Mechanisms of DPP-4 inhibitors in Covid-19
Several inflammatory signaling pathways are involved in the pathogenesis of the infections caused by SARS-CoV-2. The nod-like receptor pyrin 3 receptor (NLRP3) inflammasome is concerned with the activation of natural killer cells and the nuclear factor kappa β (NF-κβ) signaling pathway with the release of interferon gamma (INF-γ) (Al-Kuraishy et al. 2022a; Elekhnawy et al. 2021b). Suppression of NLRP3 inflammasome may decrease exaggerated immune response-induced organ injury (Al-Kuraishy et al. 2022a). As well, toll-like receptor (TLR4) is also activated in severe Covid-19 (Mostafa-Hedeab et al. 2022). Of interest, sitagliptin blocks activation of TLR4/NF-κβ/NLRP3 inflammasome axis in acute liver injury (El-Kashef and Serrya 2019).
Undoubtedly, p38 mitogen-activated protein kinase (p38MAPK) is a pro-inflammatory pathway connected with the progress of ALI and acute cardiac injury in Covid-19 (Al-Kuraishy et al. 2022b). Overactivation of p38MAPK in Covid-19 might be due to down-regulation of ACE2 and upsurge of AngII level. In addition, SARS-CoV-2 can in a straight line activate the p38MAPK signaling pathway causing endothelial dysfunction, vasoconstriction, and thrombosis (Gaohong et al. 2019). Gaohong et al. (2019) confirmed that sitagliptin inhibits p38MAPK signaling pathway-induced renal tubules epithelial cell injury in the experimental animals.
Likewise, the mechanistic target of the rapamycin (mTOR) pathway which is the intimate regulator of cell growth, proliferation, metabolism, and survival is found to be activated during SARS-CoV-2 infection. Moreover, it has a role in the transcription and mRNA translation of SARS-CoV-2 particles (Elekhnawy et al. 2022). Notably, sitagliptin attenuates cadmium-induced testicular injury by inhibiting the activation of the mTOR pathway in rats (Arab et al. 2021).
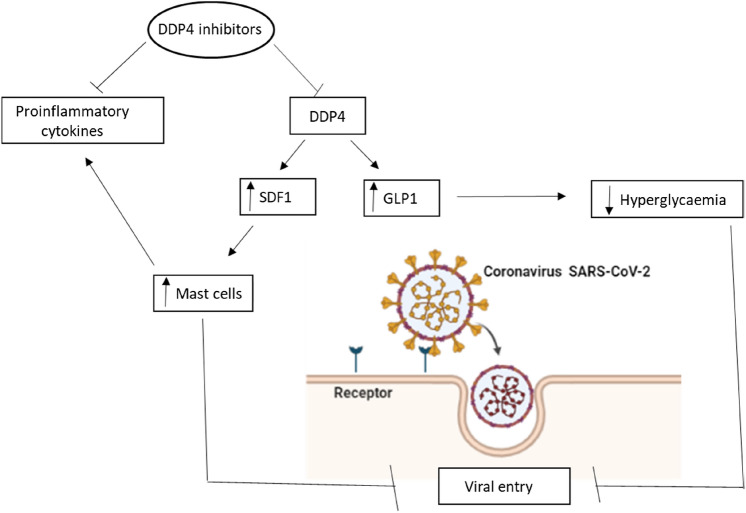
Further, stromal-derived factor-1 (SDF-1) which regulates immune response and migration of neutrophils is cleaved by DPP-4 (Mirabelli et al. 2020). Augmentation of SDF-1 by DPP-4 inhibitors may lead to a reduction in the severity of SARS-CoV-2 infection (Mirabelli et al. 2020). Besides, DPP-4 inhibitors increase the level of GLP-1 which by their anti-inflammatory and immunoregulatory properties may suppress SARS-CoV-2-induced hyperinflammation and immune dysregulation (Al-kuraishy et al. 2021d; Mirzaei et al. 2021).
Therefore, sitagliptin through attenuation of these inflammatory signaling pathways and augmentation of SDF-1 may decrease the pathogenesis of SARS-CoV-2 infection and could be a possible therapeutic modality in treating Covid-19 patients as shown in Fig. 2.
Fig. 2.
The potential role of DPP-4 inhibitors in Covid-19
Conclusions
DPP-4 receptors are highly expressed in T2DM and they are linked with the propagation of the inflammatory disorders. DPP-4 receptors are regarded as potential receptors for binding and entry of SARS-CoV-2. Inhibition of these receptors by the DPP-4 inhibitor, sitagliptin, can reduce the pathogenesis of SARS-CoV-2 infection and the associated activation of the inflammatory signaling pathways. This critical review excites for further clinical and preclinical studies to confirm the potential role of sitagliptin and other DPP-4 inhibitors in Covid-19.
Author contributions
H. Al-kuraishy, A. Al-Buhadily, A. Al-Gareeb, E. Elekhnawy, and G. Batiha conceived and designed research. H. Al-kuraishy, A. Al-Buhadily, A. Al-Gareeb, E. Elekhnawy, and G. Batiha conducted the review experiments. H. Al-kuraishy, A. Al-Buhadily, A. Al-Gareeb, E. Elekhnawy, and G. Batiha analyzed the graphical illustrations data. H. Al-kuraishy, A. Al-Buhadily, A. Al-Gareeb, E. Elekhnawy, and G. Batiha wrote the article. B.M. Alomair and M.D. Waard reviewed the review article. All the authors read and approved the article.
Funding
M.D.W. thanks the French Agence Nationale de la Recherche and the Région Pays de la Loire for financial support on Covid-19 research (ANR Flash COVID 19 call - name: CoV2-E-TARGET - grant number: 2020 07132).
Data availability
All data are available in the manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Engy Elekhnawy, Email: engy.ali@pharm.tanta.edu.eg.
Gaber El-Saber Batiha, Email: gaberbatiha@gmail.com.
References
- Al-Kuraishy HM, et al. Metformin and/or vildagliptin mitigate type II diabetes mellitus induced-oxidative stress: the intriguing effect. J Adv Pharm Technol Res. 2020;11(3):142. doi: 10.4103/japtr.JAPTR_18_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, et al. Niclosamide for Covid-19: bridging the gap. Mol Biol Rep. 2021;48(12):8195–8202. doi: 10.1007/s11033-021-06770-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, et al. Covid-19-induced dysautonomia: a menace of sympathetic storm. ASN Neuro. 2021;13:17590914211057635. doi: 10.1177/17590914211057635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, et al. COVID-19 and risk of acute ischemic stroke and acute lung injury in patients with type ii diabetes mellitus: the anti-inflammatory role of metformin. Front Med. 2021;8:110. doi: 10.3389/fmed.2021.644295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-kuraishy H, et al. COVID-19 in relation to hyperglycemia and diabetes mellitus. Front Cardiovasc Med. 2021;8:335. doi: 10.3389/fcvm.2021.644095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM et al (2021e) Impact of sitagliptin in non-diabetic Covid-19 patients. Curr Mol Pharmacol [DOI] [PubMed]
- Al-Kuraishy HM et al (2022a) The crucial role of prolactin-lactogenic hormone in Covid-19. Mol Cell Biochem 1–12 [DOI] [PMC free article] [PubMed]
- Al-Kuraishy HM et al (2022b) Neutrophil extracellular traps (NETs) and Covid-19: a new frontiers for therapeutic modality. Int Immunopharmacol 108516 [DOI] [PMC free article] [PubMed]
- Al-kuraishy HM et al (2022c) Vinpocetine is the forthcoming adjuvant agent in the management of COVID-19. Future Sci OA FSO797 [DOI] [PMC free article] [PubMed]
- Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA. 2007;298(2):194–206. doi: 10.1001/jama.298.2.194. [DOI] [PubMed] [Google Scholar]
- Arab HH, et al. Activation of autophagy by sitagliptin attenuates cadmium-induced testicular impairment in rats: targeting AMPK/mTOR and Nrf2/HO-1 pathways. Life Sci. 2021;269:119031. doi: 10.1016/j.lfs.2021.119031. [DOI] [PubMed] [Google Scholar]
- Attallah NG, El-Kadem AH, Negm WA, Elekhnawy E, El-Masry TA, Elmongy EI, Atwaijry N, Alanazi AS, Al-Hamoud GA, Ragab AE. Promising antiviral activity of Agrimonia pilosa phytochemicals against severe acute respiratory syndrome coronavirus 2 supported with in vivo mice study. Pharmaceuticals. 2021;14(12):1313. doi: 10.3390/ph14121313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardaweel SK, Hajjo R, Sabbah A. Sitagliptin: a potential drug for the treatment of COVID-19? Acta Pharm. 2021;71(2):175–184. doi: 10.2478/acph-2021-0013. [DOI] [PubMed] [Google Scholar]
- Bonora B, Avogaro A, Fadini G. Disentangling conflicting evidence on DPP-4 inhibitors and outcomes of COVID-19: narrative review and meta-analysis. J Endocrinol Invest. 2021;44(7):1379–1386. doi: 10.1007/s40618-021-01515-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elekhnawy EA, Sonbol FI, Elbanna TE, Abdelaziz AA. Evaluation of the impact of adaptation of Klebsiella pneumoniae clinical isolates to benzalkonium chloride on biofilm formation. Egypt J Med Hum Genet. 2021;22(1):1–6. doi: 10.1186/s43042-021-00170-z. [DOI] [Google Scholar]
- Elekhnawy E, Sonbol F, Abdelaziz A, Elbanna T. An investigation of the impact of triclosan adaptation on Proteus mirabilis clinical isolates from an Egyptian university hospital. Braz J Microbiol. 2021;52(2):927–937. doi: 10.1007/s42770-021-00485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elekhnawy E, et al. Histological assessment, anti-quorum sensing, and anti-biofilm activities of Dioon spinulosum extract: in vitro and in vivo approach. Sci Rep. 2022;12(1):1–15. doi: 10.1038/s41598-021-03953-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elekhnawy E, Negm W. The potential application of probiotics for the prevention and treatment of COVID-19. Egypt J Med Hum Genet. 2022;23(1):1–9. doi: 10.1186/s43042-022-00252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Kashef DH, Serrya MS. Sitagliptin ameliorates thioacetamide-induced acute liver injury via modulating TLR4/NF-KB signaling pathway in mice. Life Sci. 2019;228:266–273. doi: 10.1016/j.lfs.2019.05.019. [DOI] [PubMed] [Google Scholar]
- Gaohong L et al (2019) Effect of sitagliptin on apoptosis and p38 mitogen activated protein kinase pathway in renal tubular epithelial cells induced by high glucose. Chin J Diabetes Mellit 11(4)
- Grenet G, et al. DPP-4 inhibitors and respiratory infection: a systematic review and meta-analysis of the cardiovascular outcomes trials. Diabetes Care. 2021;44(3):e36–e37. doi: 10.2337/dc20-2018. [DOI] [PubMed] [Google Scholar]
- Krejner-Bienias A, Grzela K, Grzela T. DPP4 inhibitors and COVID-19–holy grail or another dead end? Arch Immunol Ther Exp. 2021;69(1):1–8. doi: 10.1007/s00005-020-00602-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirabelli M, et al. Potential benefits and harms of novel antidiabetic drugs during COVID-19 crisis. Int J Environ Res Public Health. 2020;17(10):3664. doi: 10.3390/ijerph17103664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzaei F et al (2021) Role of glucagon-like peptide-1 (GLP-1) agonists in the management of diabetic patients with or without COVID-19. Open Med Chem J 15(1)
- Mostafa-Hedeab G, et al. Selinexor and COVID-19: the neglected warden. Front Pharmacol. 2022;13:884228. doi: 10.3389/fphar.2022.884228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh Y, et al. Association between DPP-4 inhibitors and COVID-19–related outcomes among patients with type 2 diabetes. Diabetes Care. 2021;44(4):e64–e66. doi: 10.2337/dc20-1824. [DOI] [PubMed] [Google Scholar]
- Onohuean H, et al. Covid-19 and development of heart failure: mystery and truth. Naunyn Schmiedeberg’s Arch Pharmacol. 2021;394(10):2013–2021. doi: 10.1007/s00210-021-02147-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt F, et al. Plasma neutralization of the SARS-CoV-2 Omicron variant. N Engl J Med. 2022;386(6):599–601. doi: 10.1056/NEJMc2119641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solerte SB, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020;43(12):2999–3006. doi: 10.2337/dc20-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W, et al. DPP-4 inhibitors and risk of infections: a meta-analysis of randomized controlled trials. Diabetes Metab Res Rev. 2016;32(4):391–404. doi: 10.1002/dmrr.2723. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available in the manuscript.