INTRODUCTION:
Coronavirus disease 2019 rapidly shifted health care toward telehealth. We assessed satisfaction with and preferences for telehealth among patients with irritable bowel syndrome (IBS).
METHODS:
We conducted a cross-sectional survey in an integrated healthcare system in Southern California with members aged 18–90 years with an International Classification of Diseases 9 and 10 codes for IBS from office-based encounters between June 1, 2018, and June 1, 2020. Eligible patients were emailed a survey assessing telehealth satisfaction overall and by patient-related factors, IBS characteristics, health and technologic literacy, utilization, and coronavirus disease 2019 perceptions. We identified perceived telehealth benefits and challenges. Multivariable logistic regression identified predictors of telehealth dissatisfaction.
RESULTS:
Of 44,789 surveys sent, 5,832 (13.0%) patients responded and 1,632 (3.6%) had Rome IV IBS. Among 1,314 (22.5%) patients with IBS and prior telehealth use (mean age 52.6 years [17.4]; 84.9% female; and 59.4% non-Hispanic White, 29.0% Hispanic, and 5.6% non-Hispanic Black), 898 (68.3%) were satisfied, 130 (9.9%) were dissatisfied, and 286 (21.8%) felt neutral. In addition, 78.6% would use telehealth again. Independent predictors of telehealth dissatisfaction include social media use of once a week or less (adjusted odds ratio [OR] = 2.1; 1.3–3.5), duration of IBS for <1 year (adjusted OR = 8.2; 1.9–35.8), and willingness to travel 60 plus minutes for face-to-face visits (adjusted OR = 2.6; 1.4–3.7). Patients' main concern with telehealth was a lack of physical examination.
DISCUSSION:
Most of the patients with IBS are satisfied with telehealth. Shorter duration of IBS diagnosis, comfort with technology, and increased willingness to travel were associated with telehealth dissatisfaction. These predictors may help identify a target population for a focused IBS-telehealth program.
INTRODUCTION
With state-imposed stay-at-home mandates, social distancing, and heightened patient and provider fears, the coronavirus disease 2019 (COVID-19) pandemic prompted significant shifts in healthcare utilization and delivery. While emergency department visits (1), non-COVID-19-related hospitalizations (2) and outpatient office-based visits in the United States all declined (3) and telemedicine visits increased from 0.8 to 17.8 visits per 1,000 enrollees (2,125% change) in individuals with commercial or Medicare Advantage insurance (3). Telehealth studies in gastroenterology before the pandemic predominantly focused on feasibility and acceptability of telemedicine-based programs in academic settings for inflammatory bowel disease (4–8), chronic liver disease (9,10), and gastrointestinal (GI) motility (11). With widespread telehealth implementation in day-to-day clinical practice and a large percentage of GI visits focused on functional GI disorders (12), it is imperative that we understand the attitudes and perceptions of telehealth in patients with irritable bowel syndrome (IBS).
Although some data suggest telehealth is well-received among the general GI population, little is known about attitudes and preferences for telehealth in patients with IBS. We aimed to assess overall satisfaction with telehealth in patients with IBS, identify predictors of telehealth satisfaction, and clarify perceived benefits and challenges of telehealth use. To address this objective, we developed, pilot-tested, and electronically administered a survey called the Telemedicine in IBS during the SARS-CoV2 era (TIBS-CoV-2) to patients with Rome IV confirmed IBS.
METHODS
Survey development and pilot testing
Themes surrounding telehealth satisfaction were identified through a literature review and iteratively refined through 3 focus groups of internists and gastroenterologists from different institutions and practice settings. A 28-item survey was developed. Survey components included (i) symptom and subtype assessment adapted from the Bowel Symptom Questionnaire (13) to confirm a diagnosis of IBS by Rome IV criteria and a validated, patient-assessed overall GI symptom severity score ranging from 0 to 20 (20 = most severe) (13); (ii) demographic and clinical characteristics, e.g., marital status, income, and highest education level; (iii) Telehealth Usability Questionnaire (TUQ) (14), a validated survey that assesses telehealth usability as defined by usefulness, ease of use, interface and interaction quality, reliability, and satisfaction; and (iv) perceptions surrounding telehealth use. The TUQ was selected because of its widespread use, its incorporation of all usability factors, and its ease of use across a variety of telehealth systems including videoconferencing, computer-based systems, and mobile systems.
Pilot testing was completed for readability, clarity, question burden, and overall feedback in patients aged 18–90 years with International Classification of Disease, Ninth Revision and/or Tenth Revision, Clinical Modification (ICD-9-CM/ICD-10-CM) for IBS. A random sample of 200 patients received the survey by email. A total of 12 patients completed the survey and agreed to provide feedback. The research team conducted 10- to 15-minute one-on-one semistructured phone interviews with these participants. Common themes identified (see Supplemental File, Appendix 1a, Supplementary Digital Content 1, http://links.lww.com/CTG/A850) during pilot testing helped to refine the final survey (see Supplemental File, Appendix 1b, Supplementary Digital Content 1, http://links.lww.com/CTG/A850) before distribution. Of note, the TUQ remained unadulterated, given the validated nature of the survey.
Study design, setting, and patient population
A cross-sectional survey was conducted on patients aged 18–90 years who were active Kaiser Permanente members for at least 1 year from the time of survey distribution and were coded for IBS (ICD-9,564.1; ICD-10 K58.*) from an office-based encounter between June 1, 2018, and June 1, 2020, at any Kaiser Foundation Southern California hospital. Kaiser Permanente Southern California is an integrated health system that serves more than 4 million active members. Study exclusions included (i) active pregnancy at survey distribution; (ii) a history of inflammatory bowel disease, colorectal cancer, or celiac disease; and/or (iii) inability to complete the survey. This study was approved by the Kaiser Permanente Southern California Institutional Review Board.
Survey distribution and data collection
Eligible patients were emailed a link to the survey on November 5, 2020. Up to 3 email reminders were sent to nonresponders at 2, 4, and 8 weeks from the initial email with a recruitment end date of January 20, 2021, a period that overlapped with a surge in the COVID-19 pandemic. Survey data were collected and managed using Research Electronic Data Capture (15). Additional variables were extracted from the electronic health record (EHR). Patients with shared email addresses between family members (e.g., husband and wife), invalid emails, or surveys with unidentifiable medical record numbers were excluded. In the single case of a duplicate survey, the more recent survey was used.
We identified Rome IV confirmed patients based on survey responses. Rome IV IBS was defined as patients with symptom onset at least 6 months before the diagnosis, with recurrent abdominal pain at least 1 day a week in the past 3 months and 2 or more of the following: a relationship to defecation, association with a change in frequency, and/or form of stool for at least 30% of occasions.
Outcome variables
Our primary outcome was overall satisfaction with telehealth in patients with Rome IV confirmed IBS and at least 1 telehealth visit. We defined telehealth as a video, telephone, and/or e-visit. We asked patients to rate the following statement from the TUQ: “Overall, I am satisfied with this telehealth system” on a 5-point Likert scale (strongly agree, agree, neutral, disagree, and strongly disagree) with “satisfied” encompassing “strongly agree or agree” and dissatisfied as “strongly disagree or disagree.”
Patient variables and definitions
Patient demographics.
Patient-related factors abstracted from the EHR included age, sex, race/ethnicity, body mass index (BMI), Charlson Comorbidity Index (CCI), and total number of outpatient GI visits. Marital status, income, and highest level of education were ascertained from the patient. Race/ethnicity included 6 mutually exclusive categories: non-Hispanic White, non-Hispanic Black, Hispanic, Asian, Others, and unknown. BMI ranges were <18.5 (underweight), 18.5 to <25 (normal), 25 to <30 (overweight), and ≥30 (obese). CCI was scored 0, 1, 2, 3 + where higher scores reflect increased comorbid disease burden. CCI and outpatient GI visits were based on encounters from March 1, 2019, to March 1, 2020, 1 year before the start of the pandemic. We also inquired about the amount of travel time patients was willing to endure before accepting telehealth for care.
IBS characteristics
IBS characteristics collected through survey included duration of IBS in years, subtype, and patient-reported severity of GI symptoms rated on a visual scale (13) from 0 to 20 (mild: 0–6; moderate: 7–13; and severe: 14–20). In addition, we asked patients to rate their own knowledge of IBS on a scale from 0 to 100.
Health and technology literacy/utilization.
Perceived health and technologic literacy were assessed through confidence in filling out medical forms and frequency of social media use, respectively. We also asked patients to rate their willingness to adopt new technology based on the Roger technology adoption bell curve (16). We assessed healthcare and telehealth utilization by querying the EHR for the total number of outpatient GI visits, total number of telehealth visits, and time to last telehealth visit during 1 year before survey distribution. Finally, we asked patients about their perceptions surrounding telehealth during the COVID-19 pandemic.
Analyses
We (i) evaluated patient experience and satisfaction with telehealth, (ii) identified predictors of telehealth dissatisfaction, and (iii) elicited perceived benefits and challenges of telehealth use overall and stratified by telehealth satisfaction.
Statistical analyses
We used frequencies and proportions or means and SDs to describe patient demographic and clinical factors. To compare baseline patient demographic and clinical characteristics among satisfaction groups in patients with Rome IV confirmed IBS, we used the t test for continuous variables (e.g., age) and the χ2 test for categorical variables. To determine the factors associated with dissatisfaction, multivariable logistic regression was performed to estimate the odds ratio (OR) and 95% confidence interval (CI). We used χ2 to compare perceived benefits and challenges between satisfied and dissatisfied patients. All tests were 2-sided with a significance level of P < 0.05. All analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, NC).
RESULTS
Survey pilot results
Of 200 patients, 10 (5.0%) completed the survey. Semistructured interviews were completed in 9 of 12 (75.0%) patients; median survey completion time was 20 minutes. Feedback focused on (i) the specific purpose and setting of telehealth use (e.g., personal vs familial and IBS-related vs non-IBS-related care), (ii) pertinence of symptom questions to individual patients, and (iii) a definition of telehealth in layman terms. Revisions were made accordingly.
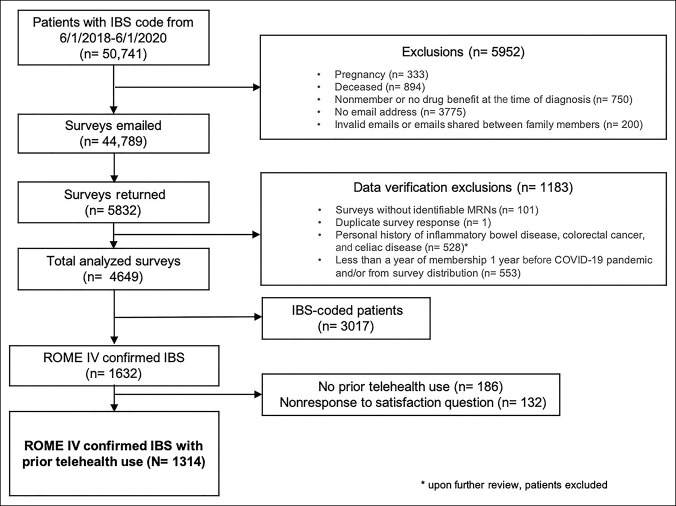
Descriptive characteristics of the study cohort
Of a total 44,789 surveys sent, 5,832 (13.0%) patients responded. After secondary exclusions, 1,632 (28.0%) of these respondents had Rome IV IBS based on survey responses and 1,314 (22.5%) had a prior telehealth experience (Figure 1). The mean age for the final study cohort was 52.6 ± 17.4 years, and 84.9% were female. The cohort consisted of 59.4% non-Hispanic White, 29.0% Hispanic, 5.6% non-Hispanic Black, and 2.7% Asian. Most of the patients were married (686, 52.2%), employed (681, 51.8%), and make less than $100,000 annually (831, 63.2%). In addition, over half of the patients reported more than 10 years of IBS symptoms. See Table 1 for additional patient characteristics.
Figure 1.
Consort diagram. IBS, irritable bowel syndrome.
Table 1.
Descriptive characteristics of the total study cohort (N = 1,314) and by satisfaction with telehealth use (n = 1,028)a
| Total Rome IV confirmed IBS patients with a prior telehealth experience | Patients with Rome IV IBS satisfied with telehealth Experience, n (%) |
Patients with Rome IV IBS dissatisfied with telehealth Experience, n (%) |
P valueb | |
| N = 1,314 | n = 898 | n = 130 | ||
| Mean age (SD) | 52.6 (17.40) | 51.0 (16.81) | 57.6 (17.81) | <0.0001 |
| Sex | ||||
| Female | 1,116 (84.93) | 774 (86.19) | 112 (86.15) | 0.99 |
| Male | 198 (15.07) | 124 (13.81) | 18 (13.85) | |
| Race/ethnicity | ||||
| White | 780 (59.36) | 519 (57.79) | 86 (66.15) | 0.24 |
| Hispanic | 381 (29.00) | 273 (30.40) | 28 (21.54) | |
| Black | 74 (5.63) | 55 (6.12) | 7 (5.38) | |
| Asian | 36 (2.74) | 23 (2.56) | 3 (2.31) | |
| Others | 23 (1.75) | 12 (1.34) | 4 (3.08) | |
| Unknown | 20 (1.52) | 16 (1.78) | 2 (1.54) | |
| Body mass index | ||||
| Obese | 568 (43.23) | 398 (44.32) | 51 (39.23) | 0.53 |
| Overweight | 345 (26.26) | 231 (25.72) | 39 (30.00) | |
| Normal | 383 (29.15) | 257 (28.62) | 37 (28.46) | |
| Underweight | 18 (1.37) | 12 (1.34) | 3 (2.31) | |
| Charlson Comorbidity Score | <0.0001 | |||
| 0 | 680 (51.75) | 502 (55.90) | 41 (31.54) | |
| 1 | 318 (24.20) | 198 (22.05) | 42 (32.31) | |
| 2 | 146 (11.11) | 99 (11.02) | 17 (13.08) | |
| 3+ | 170 (12.94) | 99 (11.02) | 30 (23.08) | |
| Marital status | ||||
| Married | 686 (52.21) | 482 (53.67) | 66 (50.77) | 0.03 |
| Single | 345 (26.26) | 242 (26.95) | 28 (21.54) | |
| Divorced/separated | 132 (10.05) | 73 (8.13) | 21 (16.15) | |
| Widowed | 51 (3.88) | 31 (3.45) | 8 (6.15) | |
| Others | 2 (0.15) | 1 (0.11) | 0 (0.00) | |
| Unknown | 98 (7.46) | 69 (7.68) | 7 (5.38) | |
| Income level | ||||
| <$50,000 | 407 (30.97) | 274 (30.51) | 38 (29.23) | <0.001 |
| $50,000–$100,000 | 424 (32.27) | 315 (35.08) | 30 (23.08) | |
| >$100,000 | 212 (16.13) | 153 (17.04) | 20 (15.38) | |
| Unknown | 271 (20.62) | 156 (17.37) | 42 (32.31) | |
| Employment status | ||||
| Full-time employment/student | 550 (41.86) | 414 (46.10) | 32 (24.62) | <0.0001 |
| Retired | 359 (27.32) | 219 (24.39) | 51 (39.23) | |
| Part-time employment/student | 131 (9.97) | 92 (10.24) | 13 (10.00) | |
| Other | 242 (18.42) | 159 (17.71) | 29 (22.31) | |
| Unknown | 32 (2.44) | 14 (1.56) | 5 (3.85) | |
| Highest level of education | ||||
| College degree or higher | 683 (51.98) | 492 (54.79) | 63 (48.46) | <0.001 |
| Some college/Associate degree | 450 (34.25) | 291 (32.41) | 53 (40.77) | |
| High school graduate/GED equivalent | 143 (10.88) | 94 (10.47) | 8 (6.15) | |
| Some high school or less | 16 (1.22) | 13 (1.45) | 0 (0.00) | |
| Unknown | 22 (1.67) | 8 (0.89) | 6 (4.62) | |
| Duration of IBS | ||||
| More than 10 yr | 767 (58.37) | 530 (59.02) | 78 (60.00) | 0.03 |
| 5–10 yr | 276 (21.00) | 182 (20.27) | 26 (20.00) | |
| 1–5 yr | 258 (19.63) | 181 (20.16) | 22 (16.92) | |
| Less than 1 yr | 13 (1.00) | 5 (0.56) | 4 (3.08) | |
| IBS subtype | ||||
| IBS_M | 551 (41.93) | 366 (40.76) | 58 (44.62) | 0.86 |
| IBS_D | 499 (37.98) | 347 (38.64) | 46 (35.38) | |
| IBS_C | 241 (18.34) | 170 (18.93) | 24 (18.46) | |
| IBS_U | 23 (1.75) | 15 (1.67) | 2 (1.54) | |
| IBS severity | ||||
| Mild | 263 (20.02) | 186 (20.71) | 25 (19.23) | 0.43 |
| Moderate | 589 (44.82) | 405 (45.10) | 53 (40.77) | |
| Severe | 462 (35.16) | 307 (34.19) | 52 (40.00) | |
| No. of telehealth visits in 1 yr | ||||
| None | 56 (4.3) | 43 (4.8) | 4 (3.1) | 0.10 |
| 1-4 | 340 (25.9) | 248 (27.6) | 26 (20.0) | |
| 5+ | 918 (69.9) | 607 (67.6) | 100 (76.9) | |
| Time to the last telehealth visit | ||||
| None | 56 (4.3) | 43 (4.8) | 4 (3.1) | 0.12 |
| < 3 mo | 941 (71.6) | 629 (70.0) | 103 (79.2) | |
| 3–6 mo | 191 (14.5) | 137 (15.3) | 11 (8.5) | |
| 6–12 mo | 126 (9.6) | 89 (9.9) | 12 (9.2) | |
See appendix for additional variables, Supplementary Digital Content 2, http://links.lww.com/CTG/A851.
IBS, irritable bowel syndrome; GED, General Educational Development.
Patients who felt neutral about telehealth use (n = 286) were not included.
P values are for comparison between satisfied and dissatisfied patients.
Experience and satisfaction with telehealth
Of 1,314 (80.5%) patients with Rome IV IBS who completed the survey entirely and used telehealth for their care, 898 (68.3%) were satisfied, 130 (9.9%) were dissatisfied, and 286 (21.8%) felt neutral about their experience. In addition, 1,072 (81.8%) patients reported that telehealth was simple to use, and 1,030 (78.6%) would use telehealth again. Satisfied patients considered telehealth as good or better than face-to-face (F2F) visits as compared with dissatisfied patients (736 [82.0%] vs 16 [12.3%], P < 0.0001). In total, 852 (92.3%) patients were more likely to use telehealth now because of the COVID-19 pandemic; 920 (96.6%) and 759 (91.0%) patients felt that telehealth limited exposure risk to and relieved anxiety of contracting the virus from the healthcare setting, respectively.
Satisfaction by patient demographics
Telehealth dissatisfaction was higher in older (57.6 vs 51.0 years, P < 0.0001) and sicker patients (CCI 3+: 23.1% vs 11.0%, P < 0.0001). In univariate analysis, no significant differences were seen with sex, race/ethnicity, and BMI between satisfied and dissatisfied groups. Patients making less than $100,000 annually were more satisfied with telehealth (65.6% vs 52.3%, P < 0.005). Satisfied patients would consider telehealth over a F2F visit for a travel time of 30–59 minutes (328/898, 36.5%, P < 0.01); dissatisfied patients did not consider travel time a factor (39/130, 30.0%, P < 0.005).
Satisfaction based on IBS characteristics
Patients with less than a year of IBS were more dissatisfied with telehealth (3.1% vs 0.6%, P < 0.05). All other IBS-related variables were not significantly different.
Health and technologic literacy/utilization
Among IBS patients with telehealth use, 92.9% were extremely confident in their level of health literacy and 74.8% use social media at least once a day. Patients with higher self-perceived health literacy (93.2% vs 85.4%, P < 0.01), daily use of social media (77.3% vs 57.7%, P < 0.0001), and readiness to try new technology (32.4% vs 20.0%, P < 0.01) were more satisfied with telehealth. Nearly 60% of the satisfied patients had 2 or less GI clinic visits 1 year before the pandemic as compared with 41.5% of the dissatisfied patients (P < 0.001), whereas dissatisfied patients sought GI care 5 or more times compared with their satisfied counterparts (40.8% vs 28.8%, P < 0.05) (see Appendix 2, Supplementary Digital Content 1, http://links.lww.com/CTG/A850).
COVID-19 perceptions and satisfaction with telehealth
Patients satisfied with telehealth felt safer using telehealth during the COVID-19 pandemic as compared with dissatisfied patients (74.4% vs 35.4%, P < 0.0001). Satisfied patients reported that telehealth limited exposure risk to (98.9% vs 75.8%, P < 0.0001) and relieved anxiety around contracting SARs-CoV2 from the healthcare setting (96.3% vs 44.7%, P < 0.0001). Interestingly, 75.8% of the dissatisfied patients felt their exposure risk was limited with telehealth, yet 64.4% did not feel safer using telehealth during the pandemic.
Predictors of telehealth dissatisfaction
Multivariable analysis identified predictors of dissatisfaction in all domains: patient-related factors, IBS characteristics, and health and technologic literacy. Patients with a CCI of 1 or 3+ were more likely to be dissatisfied with telehealth (adjusted OR = 2.1; 95% CI = 1.3–3.5 and adjusted OR = 2.5; 95% CI = 1.3–4.6, respectively) compared with those with a CCI of 0. For income, patients who chose not to respond were more likely to be dissatisfied (adjusted OR = 2.1; 1.3–3.7). Patients with a willingness to travel more than 60 minutes had 2.2 times higher odds of dissatisfaction than those willing to travel less than 60 minutes.
We analyzed several IBS characteristics including IBS duration, subtype, and severity. Among these, only shorter duration of IBS was significant on the multivariable analysis (<1 year: adjusted OR = 8.2; 95% CI = 1.8–35.8).
Similar to income, patients who preferred not to answer for health literacy tended to be more dissatisfied (adjusted OR = 2.1; 1.3–3.7). Patients who used social media once a week or less had 2.1 times higher odds of telehealth dissatisfaction compared with those with daily use (adjusted OR = 2.1; 95% CI = 1.3–3.5) (Table 2).
Table 2.
Predictors of dissatisfaction with telehealth use in patients with Rome IV confirmed IBS
| Variable | Total number of patients per group | No. of dissatisfied patients | Adjusted odds ratio (95% CI) |
| CCI | 0 | ||
| 0 | 543 | 41 | Ref |
| 1 | 240 | 42 | 2.13 (1.29, 3.52)a |
| 2 | 116 | 17 | 1.41 (0.71, 2.77) |
| 3+ | 129 | 30 | 2.46 (1.30, 4.65)a |
| Income | |||
| <$50,000 | 312 | 38 | Ref |
| $50,000-$100,000 | 345 | 30 | 0.86 (0.49, 1.50) |
| >$100,000 | 173 | 20 | 1.22 (0.63, 2.35) |
| Unknown | 198 | 42 | 2.14 (1.25, 3.66)a |
| Duration of IBS | |||
| One or more years | 1,019 | 126 | Ref |
| Less than 1 yr | 9 | 4 | 8.15 (1.85-35.84a |
| IBS subtype | |||
| Constipation-predominant | 194 | 24 | Ref |
| Diarrhea-predominant | 393 | 46 | 1.19 (0.66–2.15) |
| Mixed-type | 424 | 58 | 1.15 (0.65, 2.03) |
| Undefined | 17 | 2 | 1.9 (0.37, 9.38) |
| IBS severity | |||
| Mild | 211 | 25 | Ref |
| Moderate | 458 | 53 | 1.12 (0.65–1.94) |
| Severe | 359 | 52 | 1.47 (0.84, 2.57) |
| Health literacy | |||
| Extremely confident | 948 | 111 | Ref |
| Somewhat or not confident | 72 | 15 | 1.76 (0.89–3.47) |
| Unknown | 8 | 4 | 6.32 (1.38, 28.97)a |
| Technology literacy | |||
| At least once a day | 769 | 75 | Ref |
| Once a week or less | 144 | 33 | 2.13 (1.29–3.51)a |
| Never | 8 | 22 | 1.40 (0.77, 2.55) |
| Travel time threshold | |||
| Less than 60 minutes | 631 | 58 | Ref |
| 60 or more minutes | 198 | 33 | 2.26 (1.37–3.71)a |
| Travel time is not a factor | 199 | 39 | 2.30 (1.43, 3.69)a |
Data are presented as odds ratios (95% CI). The final logistic regression model included the following variables: age, sex, race/ethnicity, CCI, marital status, income, employment, health literacy, technologic literacy, IBS duration, subtype, severity and travel time. Age, sex, race/ethnicity, marital status, and employment status were not significant.
CI, confidence interval; CCI, Charlson Comorbidity Index; IBS, irritable bowel syndrome.
P < 0.05.
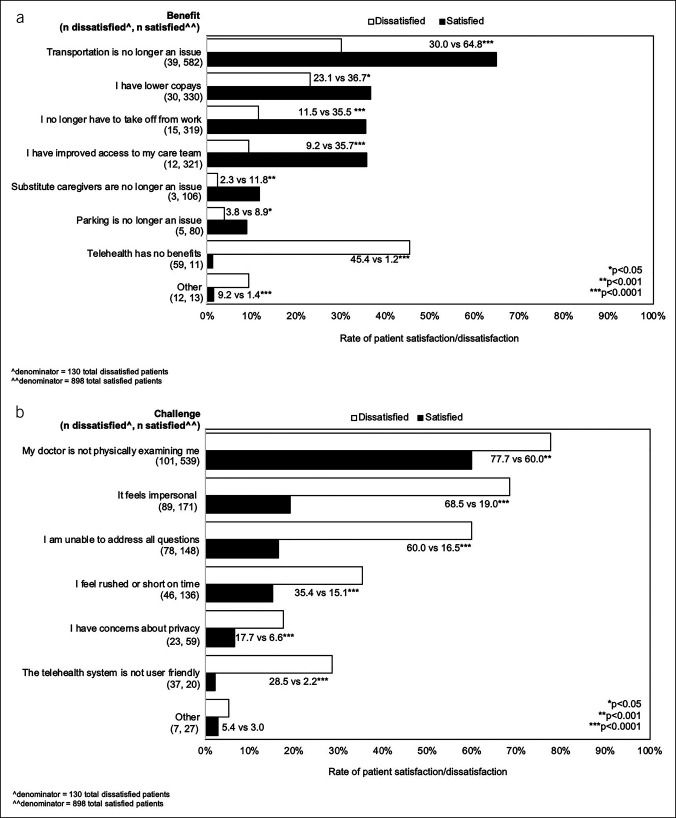
Benefits and challenges of telehealth use
A total of 958 (93.2%) and 726 (70.6%) patients with Rome IV IBS indicated that telehealth was beneficial and convenient, respectively. Patient-reported issues experienced with F2F visits that were considered less problematic with telehealth included transportation (621, 60.4%), higher copays (360, 35.0%), absence from work (334, 32.5%), and finding substitute caregivers (109, 10.6%). Nearly one-third of patients felt that they had better access to their care team. All benefits were significantly different between satisfied and dissatisfied groups (Figure 2a).
Figure 2.
(a) Benefits of telehealth in patients with Rome IV confirmed irritable bowel syndrome and prior telehealth experience, stratified by satisfaction with prior telehealth use. (b) Challenges of telehealth in patients with Rome IV confirmed irritable bowel syndrome and prior telehealth experience, stratified by satisfaction with prior telehealth use.
Despite the benefits, 731 (71.1%) patients indicated that telehealth still has its challenges. The most commonly reported challenges with telehealth included the absence of physical examination (640, 62.3%), feeling impersonal (260, 25.3%), being unable to address all of their issues/concerns (226, 22.0%), and feeling rushed (182, 17.7%). These challenges were significantly more common in patients dissatisfied with telehealth (Figure 2b).
DISCUSSION
In this cross-sectional study, we developed, refined, and administered a survey to evaluate telehealth satisfaction in patients with IBS during the COVID-19 pandemic. Overall, patients reported high satisfaction rates and ease of use with telehealth. A majority felt that telehealth was as good or better than F2F visits and would use telehealth for future care. Despite this, approximately 10% of the patients remain dissatisfied. Sicker patients (CCI 1+) and those with a diagnosis of IBS for less than a year, a travel time more than 60 minutes for F2F appointments and/or use of social media once a week or less were more likely to be dissatisfied. However, 69.5% of the patients felt safer using telehealth due to the COVID-19 pandemic, and more than 90% of the patients felt that telehealth limited exposure to and allayed fears of contracting the virus from the healthcare setting. Benefits to telehealth include diminished issues with transportation, high copays, work absenteeism, and the need for substitute caregivers; notable challenges were the absence of physical examinations, feelings of impersonality, and incapacity to address patient concerns.
COVID-19 transformed healthcare delivery almost overnight. Relaxed regulatory and licensure barriers and changes to reimbursement made widespread adoption of telehealth possible. Emerging literature suggests that these changes may continue in the postpandemic era (17,18), and in the past year, telehealth has demonstrated high patient satisfaction with a reduction in costs to all stakeholders (9,19,20). Thus, it is ever more important to understand the successes and limitations of telehealth, dive more deeply into determinants of telehealth care, and use reported benefits and challenges of telehealth to identify target populations for telehealth programs (17). One such population are those with IBS, a chronic illness affecting more than 15 million people (12) with an average of 2.7 million visits annually (21) and direct and indirect annual costs of $1,562–$7,547 and $791–$7,737, respectively (22).
Currently, there are limited data on satisfaction and perceptions of telehealth in patients with IBS during the COVID-19 pandemic. Only 2 studies exist to date in the general GI population (9,20). Although rates of future telehealth use and identified barriers were similar in the general GI population and our IBS population, telehealth satisfaction rates were lower in our study (68.3% vs 78–80%). Although recall bias may have explained this discrepancy when comparing our study with that of Serper et al (9) where surveys were administered through patient portal and telephone, survey administration was similar between our study and that of Dobrusin et al. (20). This raises the question of inherently lower rates of satisfaction in patients with IBS as compared with the general GI population. Studies have shown that patients with IBS are less resilient (23), often unhappy with available pharmacologic therapies (24) and more satisfied with increased diagnostic testing, higher number of recommendations, and higher number of follow-up visits (25,26).
In addition, our study had a much lower response rate as compared with other survey-based studies among patients with IBS (13.0% vs 53.8–83.8% (27,28)). Our initial cohort was identified through ICD-9-CM/ICD-10-CM coding, whereas other studies confirmed a diagnosis of IBS through a chart review. This discrepancy in response rates supports prior findings of high levels of inaccuracy with provider coding and administrative data (29,30). In addition, other studies offered small renumerations for participation, whereas ours did not.
Telehealth has immense potential in the care of patients with IBS as a tool to improve access without supplanting individualized in-person care. This survey helps to identify barriers to telehealth use in a broader context and provides insight into new avenues for research. Barriers should be addressed to improve the telehealth experience, specifically the loss of reassurance provided during face-to-face consultations and a clinical care tool that is critical to improving symptoms of the gut-brain interaction. The development of an IBS-focused telecare pathway may help to decrease economic burden, healthcare utilization, and access issues, but accommodations for patients with a newer diagnosis of IBS, those who lack health and technologic literacy, and those with more comorbidities should be considered for programmatic success.
Our study has several strengths. First, our survey confirmed a diagnosis of IBS by Rome IV criteria and subtyped patients' symptoms, especially given the inaccuracies of ICD-9 CM/ICD-10 CM coding in identifying and subtyping IBS (29,30). In addition, the survey was developed and refined by both providers of differing specialties and levels of training and practice and direct patient feedback. The TUQ validation population and our study population shared similar characteristics including majority non-Hispanic White, women, and recent telehealth experience within 3 months of survey distribution. Because the survey was sent electronically, we reviewed preliminary data to ensure no logistical or technical errors occurred during survey administration. The study was also conducted in a diverse patient population of a large integrated health system. Patients and their IBS were well characterized and phenotyped, respectively, as confirmed by the survey results with readily accessible variables from the EHR and often unattainable patient-reported variables from the survey. Finally, the study was well-powered to observe subtle differences between comparator groups. This was especially clear when examining duration of IBS of less than a year as an independent predictor of telehealth dissatisfaction.
There were several limitations to this study. Overall, the percentage of responders was limited highlighting a significant selection bias. The survey was conducted exclusively in English and distributed in California, both of which limit generalizability of the study. In addition, we used email as the sole mode of distribution, which may have led to an overestimation of telehealth satisfaction. Patients were required to opt into the online survey, potentially introducing self-selection bias. There was also risk of recall bias because the survey was not administered immediately after the use of telehealth, rather patients were asked to evaluate their prior experiences with telehealth. Finally, patient unease with income and health literacy questions may have made some responses difficult to interpret.
In conclusion, 90% of the patients with IBS were satisfied with telehealth. The remaining 10% expressed dissatisfaction. Independent predictors of dissatisfaction included social media use of once a week or less, duration of IBS for <1 year, CCI score 1 or more, and willingness to travel of 60 minutes of more. Patients' main concerns were a lack of physical examination and feelings of impersonality with telehealth. Incorporating these factors into an IBS-focused telehealth program offers an opportunity to improve access to care, optimize patient satisfaction, and ensure efficient resource utilization through the expansion of virtual care delivery.
CONFLICTS OF INTEREST
Guarantor of the article: Christine Yu, MD.
Specific author contributions: C.Y.: overall study supervision; study concept and design, acquisition of data, conceptual model, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript; approval of final draft submitted. S.T.: acquisition of data, critical revision of the manuscript; approval of final draft submitted. J.S.: analysis and interpretation of data; critical revision of the manuscript; approval of final draft submitted. A.P.: acquisition of data, critical revision of the manuscript; approval of final draft submitted. D.P.: acquisition of data, critical revision of the manuscript; approval of final draft submitted. W.K.v.D.: study concept and design; critical revision of the manuscript; approval of final draft submitted. C.V.A.: study concept and design; critical revision of the manuscript; approval of final draft submitted. B.U.W.: overall study supervision; study concept and design, conceptual model, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript; approval of final draft submitted.
Financial support: This research was supported by a grant from the Regional Research Committee of Kaiser Permanente Southern California, RRC Grant No.: KP-RRC-20200506.
Potential competing interests: None to report.
Previous presentation: Data were presented as a virtual poster at the 2021 Digestive Diseases Week; May 22-25, 2021.
Study Highlights.
WHAT IS KNOWN
✓ High rates of telehealth satisfaction in the general GI population.
✓ Data on satisfaction and perceptions of telehealth in patients with irritable bowel syndrome (IBS) are limited.
WHAT IS NEW HERE
✓ High rates of overall telehealth satisfaction in patients with IBS.
✓ Sicker patients, a shorter diagnosis of IBS, less frequent social media use, and willingness to travel longer for a face-to-face visit are associated with telehealth dissatisfaction.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A850, http://links.lww.com/CTG/A851
Contributor Information
Stephanie Tovar, Email: stephanie.tovar@kp.org.
Jiaxiao Shi, Email: jiaxiao.m.shi@kp.org.
Ariadna Padilla, Email: ariadna.padilla@kp.org.
Dana Pounds, Email: dana.pounds@kp.org.
Welmoed K. van Deen, Email: vandeen@eshpm.eur.nl.
Christopher V. Almario, Email: christopher.almario@csmc.edu.
Bechien U. Wu, Email: bechien.u.wu@kp.org.
REFERENCES
- 1.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med 2020;38(9):1732–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jeffery MM, D'Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med 2020;180(10):1328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel SY, Mehrotra A, Huskamp HA, et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med 2021;181(3):388–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cross RK, Cheevers N, Rustgi A, et al. Randomized, controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT). Inflamm Bowel Dis 2012;18(6):1018–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Regueiro MD, Greer JB, Binion DG, et al. The inflammatory bowel disease live interinstitutional and interdisciplinary videoconference education (IBD LIVE) series. Inflamm Bowel Dis 2014;20(10):1687–95. [DOI] [PubMed] [Google Scholar]
- 6.Elkjaer M, Shuhaibar M, Burisch J, et al. E-Health empowers patients with ulcerative colitis: A randomised controlled trial of the web-guided ‘constant-care’ approach. Gut 2010;59(12):1652–61. [DOI] [PubMed] [Google Scholar]
- 7.Castro HK, Cross RK, Finkelstein J. Using a home automated telemanagement (HAT) system: Experiences and perceptions of patients with inflammatory bowel disease. AMIA Annu Symp Proceedings AMIA Symp 2006:872 (http://www.ncbi.nlm.nih.gov/pubmed/17238492). [PMC free article] [PubMed] [Google Scholar]
- 8.de Jong MJ, Boonen A, van der Meulen-de Jong AE, et al. Cost-effectiveness of telemedicine-directed specialized vs standard care for patients with inflammatory bowel diseases in a randomized trial. Clin Gastroenterol Hepatol 2020;18(8):1744–52. [DOI] [PubMed] [Google Scholar]
- 9.Serper M, Nunes F, Ahmad N, et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology 2020;159(4):1589–91. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su GL, Glass L, Tapper EB, et al. Virtual consultations through the veterans administration SCAN-ECHO project improves survival for veterans with liver disease. Hepatology 2018;68(6):2317–24. [DOI] [PubMed] [Google Scholar]
- 11.Brennan S. American journal of gastroenterology lecture: How digital health will transform gastroenterology. Am J Gastroenterol 20152016;111:624–30. [DOI] [PubMed] [Google Scholar]
- 12.Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology 2002;122(5):1500–11. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel B, Strickland A, Naliboff BD, et al. Predictors of patient-assessed illness severity in irritable bowel syndrome. Am J Gastroenterol 2008;103(10):2536–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parmanto B, Lewis AN, Jr, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ). Int J telerehabilitation 2016;8(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers EM. Diffusion of Innovations. New York: Free Press of Glencoe, 2005. [Google Scholar]
- 17.Shah ED, Amann ST, Karlitz JJ. The time is now: A guide to sustainable telemedicine during COVID-19 and beyond. Am J Gastroenterol 2020;115(9):1371–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.George LA, Cross RK. Telemedicine in gastroenterology in the wake of COVID-19. Expert Rev Gastroenterol Hepatol 2020;14(11):1013–5. [DOI] [PubMed] [Google Scholar]
- 19.Keihanian T, Sharma P, Goyal J, et al. Telehealth utilization in gastroenterology clinics amid the COVID-19 pandemic: Impact on clinical practice and gastroenterology training. Gastroenterology 2020;159(4):1598–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobrusin A, Hawa F, Gladshteyn M, et al. Gastroenterologists and patients report high satisfaction rates with telehealth services during the novel Coronavirus 2019 pandemic. Clin Gastroenterol Hepatol 2020;18(11):2393–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma C, Congly SE, Novak KL, et al. Epidemiologic burden and treatment of chronic symptomatic functional bowel disorders in the United States: A nationwide analysis. Gastroenterology 2021;160(1):88–98.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nellesen D, Yee K, Chawla A, et al. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J Manag Care Pharm 2013;19(9):755–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parker CH, Naliboff BD, Shih W, et al. The role of resilience in irritable bowel syndrome, other chronic gastrointestinal conditions, and the general population. Clin Gastroenterol Hepatol 2021;19:2541–50.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rangan V, Ballou S, Shin A, Camilleri M; Beth Israel Deaconess Medical Center GI Motility Working Group, Lembo A. Use of treatments for irritable bowel syndrome and patient satisfaction based on the IBS in America survey. Gastroenterology 2020;158(3):786–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quigley BM, Sova CC, Brenner DM, et al. Can't get No) patient satisfaction: The predictive power of demographic, GI, and psychological factors in IBS patients. J Clin Gastroenterol 2018;52(7):614–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh P, Ballou S, Katon J, et al. Symptom severity, mood, and healthcare use are associated with satisfaction in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2020;18(13):2945–51. doi: .e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang C, Xu Y, Sharma S, et al. Psychosocial factors associated with irritable bowel syndrome development in Chinese college freshmen. J Neurogastroenterol Motil 2019;25(2):233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ballou S, McMahon C, Lee H-N, et al. Effects of irritable bowel syndrome on daily activities vary among subtypes based on results from the IBS in America survey. Clin Gastroenterol Hepatol 2019;17(12):2471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goff SL, Feld A, Andrade SE, et al. Administrative data used to identify patients with irritable bowel syndrome. J Clin Epidemiol 2008;61(6):617–21. [DOI] [PubMed] [Google Scholar]
- 30.Lix LM, Yogendran MS, Shaw SY, et al. Comparing administrative and survey data for ascertaining cases of irritable bowel syndrome: A population-based investigation. BMC Health Serv Res 2010;10:31. [DOI] [PMC free article] [PubMed] [Google Scholar]