Abstract
Vaccine development and implementation decisions need to be guided by accurate and robust burden of disease data. We developed an innovative systematic framework outlining the properties of such data that are needed to advance vaccine development and evaluation, and prioritize research and surveillance activities. We focus on 4 objectives—advocacy, regulatory oversight and licensure, policy and post-licensure evaluation, and post-licensure financing—and identify key stakeholders and specific requirements for burden of disease data aligned with each objective. We apply this framework to group A Streptococcus, a pathogen with an underrecognized global burden, and give specific examples pertinent to 8 clinical endpoints. This dynamic framework can be adapted for any disease with a vaccine in development and can be updated as vaccine candidates progress through clinical trials. This framework will also help with research and innovation priority setting of the Immunization Agenda 2030 (IA2030) and accelerate development of future vaccines.
Keywords: burden of disease, vaccine policy, vaccine development, group A streptococcal diseases
We introduce an innovative systematic framework prioritizing burden of disease data requirements for vaccines through advocacy, regulatory and licensing, policy and post-introduction evaluation, and financing. We apply this framework to group A Streptococcus to aid efforts to accelerate vaccine development.
Vaccines are an important public health tool to prevent infectious diseases and improve population health and well-being [1, 2]. Multiple factors influence decision making during vaccine development, from the preclinical phase through large-scale vaccine trials and policy formation. Establishing credible burden of disease estimates should be the cornerstone of new vaccine development [3]; however, decisions are not always informed by such estimates. “Burden of disease” encompasses a broad range of outcomes, including the entire spectrum of associated morbidities and sequelae, and health-related costs of an illness. It incorporates multiple data types, including acute disease incidence, disability-adjusted life-years (DALYs), health service utilization rates, prevalence of associated chronic diseases, and mortality rates. The perceived credibility of the estimates and how they are packaged and presented within the context of overall public health priorities can influence vaccine development and implementation. Thus, the importance of accurate, robust data should neither be dismissed nor underestimated. High-quality data can be used in post-implementation evaluations to measure and improve vaccine program performance. Furthermore, data-enabled decision making is 1 of 4 core principles in the World Health Organization’s (WHO’s) Immunization Agenda 2030 (IA2030) [4].
Beyond incorporating traditional disease burden measures, a systematic framework for prioritizing burden of disease should also include estimates of social and economic impact, community acceptability, and recognition of the need for adding vaccines to existing prevention and control measures. The global effort to rapidly develop, evaluate, and implement coronavirus disease 2019 (COVID-19) vaccines in the face of the largest global pandemic in modern history exemplifies how high rates of disease burden, widespread economic disruption, and the scientific, political, and community demand for vaccination can drive vaccine development [5]. This can potentially alter perceptions on the value of vaccines in preventing infectious diseases [6].
Despite the global success of some vaccines, vaccine development for other pathogens with an established high burden have faced impediments. Group A Streptococcus (Streptococcus pyogenes, herein referred to as Strep A), which is recognized as a WHO vaccination priority, is 1 example [7, 8]. Vaccine research and development investments for this pathogen remain minimal [9]. Despite an estimated annual 800 million infections and 639 000 deaths globally [10], the burden of Strep A disease remains underappreciated, especially in low- to middle-income countries (LMICs). There is a need to improve the robustness of Strep A disease burden estimates and widely communicate the potential value of vaccination to bolster the rationale for prioritizing vaccine development and implementation. Such a robust approach is a priority of the Wellcome Trust–funded Strep A Vaccine Consortium (SAVAC; www.savac.ivi.int).
We describe the properties of burden of disease data that are needed to progress vaccine development, evaluation, and policy making and a framework to prioritize studies and surveillance activities that would yield robust data addressing different vaccine objectives. Using this framework, we aimed to provide specific examples for Strep A and identify future research priorities.
FRAMEWORK DEVELOPMENT
SAVAC established an expert Burden of Disease Working Group (BoDWG) comprising 13 members from 7 geographically diverse countries, with wide-ranging expertise in Strep A and other vaccine-preventable diseases (VPDs), disease surveillance, and vaccine implementation. The BoDWG identified and reached consensus on 4 overarching vaccine objectives (advocacy, regulatory oversight and licensure, policy and post-licensure evaluation, and post-licensure financing) through iterative discussion to build a framework (Table 1). We describe 4 key elements for consideration across each objective. For key stakeholders, the framework prioritizes the most relevant disease burden data necessary to inform vaccine clinical development and introduction activities. We illustrate the application of these vaccine objectives to existing vaccines (Supplementary Table 1).
Table 1.
Framework for Prioritizing Burden of Disease Data for Vaccine Development and Evaluation Objectives
| Vaccine Objective | ||||
|---|---|---|---|---|
| Element | Advocacy | Regulatory/Licensure | Policy and Post-Licensure Evaluation | Financing |
| Stage of vaccine pipeline | All stages | Pre-licensure and licensure/pre-qualification stages, with some continuation for post-licensure commitments | Post-licensure, but early analyses needed pre-licensure period | Required for post-licensure decision making, but evidence needed pre-licensure for 5-year Vaccine Investment Strategy decision making by Gavi and others |
| Key audience/stakeholders |
|
|
|
|
| Data purpose |
|
|
|
|
| Overarching data requirements |
|
|
|
|
Abbreviations: CSO, civil society organization; DALY, disability-adjusted life-year; EPI, Expanded Programme of Immunisation; Gavi, Gavi, the Vaccine Alliance; GNN, Global NITAG Network; IA2030, Immunization Agenda 2030; NITAG, National Immunization Technical Advisory Group; NRA, National Regulator Agency; QALY, quality-adjusted life-year; RITAG, Regional Immunization Technical Advisory Group; SAGE, Strategic Advisory Group of Experts on Immunization; SDG, Sustainable Development Goal; WHO, World Health Organization.
Advocacy
Creating partnerships with private- and public-sector stakeholders, communicating the evidence-based value of an intervention, and seeking political commitment are key advocacy objectives for successful implementation of immunization and other public health prevention programs [2, 11, 12]. For a vaccine to be prioritized for introduction, the need for vaccination—both globally and among populations where the vaccine is to be used—must be well recognized [13]. However, the exact data needs and how they are described may vary for different stakeholders. Public health authorities may be most interested in health benefits, reduction in health service utilization, and cost-effectiveness; political leaders may focus on avoidable deaths or returns on investments from a vaccination program; public and private donors may prioritize the impact of new vaccines (or treatments) arising from research; and the general public may respond most to individual stories and data relevant to vulnerable groups such as children or the elderly.
An effective advocacy tool enables comparisons between the burden of the targeted disease and other diseases already prioritized for vaccine introduction or diseases with high public awareness. Communicating burden of disease data within the context of global public health goals (eg, Sustainable Development Goals [SDGs], specifically SDG3 targeting good health and well-being through prevention of communicable diseases [1]) and the potential contribution of interventions such as vaccination in achieving these goals, is important to capture the attention of global and national decision-makers. Ideally, burden of disease data should encompass the complete disease spectrum of a pathogen to accurately convey its importance, while also focusing on clinical manifestations (and accompanying data) of the greatest public health significance. Where country-specific estimates of disease burden are lacking, it is important to provide regional estimates to assist with decision making [14].
Regulatory Oversight and Licensure
Vaccine licensure requires well-designed vaccine efficacy studies (or studies of accepted correlates of protection such as immunogenicity) that measure the impact of the vaccine candidate on prevention of well-defined, pathogen-specific disease endpoints of clinically significant severity, as well as a careful assessment of vaccine-associated adverse events. Contemporary local disease data are needed to identify clinical trial sites for conducting such efficacy studies. Age-specific incidence estimates of the clinical disease endpoint that the vaccine is targeting are needed to design adequately powered trials. These disease endpoints, key clinical indications, and target populations are often defined in WHO Preferred Product Characteristics. Background rates of disease-related conditions using standard burden of disease measures from populations where vaccine trials are being conducted can provide context for evaluations of potential of vaccine-associated disease [15]. Data describing the natural progression of disease from acute infection to associated sequelae or chronic disease as well as safety data are important considerations for this objective. Key stakeholders include vaccine developers and manufacturers, clinical trial sponsors, and regulatory authorities, as well as global, regional, and national vaccine policy-making bodies (Table 1). To facilitate swift and successful implementation, vaccine developers and those synthesizing burden of disease data should have a good understanding of the needs for regulatory approval and for funding decisions.
Policy and Post-Licensure Evaluation
Burden of disease estimates are among the key considerations for policy decisions on vaccine introduction. These estimates, along with cost-effectiveness data, enable comparison with other public health priorities and facilitate prioritization of a vaccine for inclusion in national programs. Population-level socioeconomic indicators (eg, income level, access to healthcare, water, and sanitation) and environmental factors that influence disease burden are also important considerations in making equity-based vaccination policies and maximizing their impact [16].
In addition, high-quality surveillance is essential to fill data gaps, enhance the credibility of the burden estimates, and provide epidemiological data needed to optimize the use of preventive strategies. The establishment of surveillance systems using standardized methods is essential for measurements of “real world” vaccine effectiveness and impact, and for monitoring epidemiological trends (eg, changes in peak age of infection or in serotype or genotype prevalence of the pathogen) post-implementation. These assessments may be useful for justifying the continued use of the vaccine and informing vaccination policies and schedules. For certain vaccines (eg, pneumococcal conjugate vaccine), WHO recommends at least 2 years of pre-vaccine data and 3–5 years of post-vaccine data to appropriately make such decisions [17].
In addition to measuring the performance of a vaccine, vaccine efficacy trials can be used to estimate vaccine-preventable disease burden by measuring the proportion of non-specific clinical syndromes prevented by the vaccine [18]. Such clinical syndromes of public health importance that can be caused by multiple pathogens include pneumonia, diarrhea, and meningitis. Data requirements for this objective should therefore include pathogen-specific and non-specific disease endpoints and, where feasible, be population-based. This differs from data required to measure efficacy against a pathogen-specific disease endpoint observed in phase III clinical trials conducted in the setting of idealized standard-of-care and Good Clinical Practice.
The key stakeholders for the policy objective are the immunization technical advisory groups at global, regional, and national levels and global bodies, like WHO, which many resource-poor countries look to for advice and guidance.
Financing
The financing objective refers to the post-licensure financing of vaccine introduction and scale-up, as opposed to financing pre-licensure vaccine research. A key global stakeholder is Gavi, the Vaccine Alliance, which supports the introduction of new vaccines in the poorest countries. Its vaccine investment strategy analyses provide ranking criteria for the evaluation of vaccines that includes the economic impact (direct and indirect costs averted) and health impact (cases and deaths averted) [19]. However, national governments are primarily responsible for long-term sustainable financing of their immunization programs. High-quality disease data facilitate economic analyses, including cost-effectiveness, benefit–cost, and societal return on investment analyses of vaccination. Burden of disease data on, and economic analysis of, all clinical endpoints are important as the drivers of a vaccine’s value may be from endpoints that are of lesser severity but may contribute significantly to population-level healthcare costs compared with those outcomes requiring high individual medical care but a low population incidence. The full societal value of a vaccine, which may include the value from changes in educational attainment, labor force participation and productivity, antimicrobial resistance (AMR) levels, public health surveillance expenditure, and social equity, should also be considered, and has become important for COVID-19 vaccines [6].
APPLICATIONS TO STREP A VACCINE DEVELOPMENT
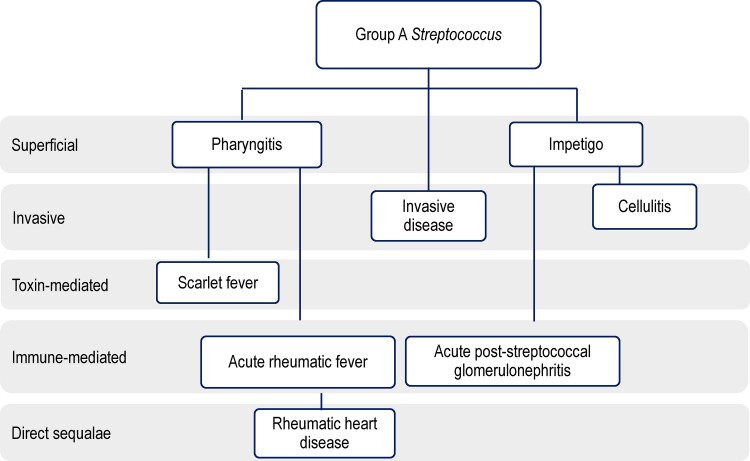
The clinical spectrum of Strep A is broad (Figure 1). The lack of a single, focused disease entity likely contributes to the lack of consensus on its public health priority and affects advocacy efforts for disease prevention through development of a Strep A vaccine. Additionally, while some clinical endpoints are specific to Strep A, others (eg, cellulitis, pharyngitis) have multiple etiologies.
Figure 1.
Key group A Streptococcus disease syndromes. Colonization of upper respiratory infection and skin is not included. Note this is a simplified figure of the diseases associated with group A Streptococcus. Locally invasive disease and invasive disease can also include bacteremia, meningitis, puerperal sepsis, and necrotizing fasciitis. Toxin-mediated diseases can also include streptococcal toxic shock syndrome. Direct sequelae can also include chronic kidney disease. Figure adapted with permission by Cannon et al [20].
To address this challenge and highlight the need for a Strep A vaccine, we used our framework to provide a roadmap and identify priority data requirements specific to key Strep A clinical endpoints, grouped into acute diseases (Table 2) and immune-mediated sequelae (Table 3). Some data purposes differ between high-income countries (HICs) and LMICs. However, the HIC/LMIC dichotomy does not account for the large heterogeneity within some HICs. For example, Australia has the highest reported rates of impetigo [21] and rheumatic heart disease (RHD) [22] in the world among First Nations people; hence, burden of disease data requirements in these populations in Australia may reflect more of an LMIC prioritization than an HIC. Furthermore, the simple dichotomy does not account for the transition from low-income to middle-income country status, which is particularly important for Gavi funding considerations and future vaccine implementation [23].
Table 2.
Priorities for Data Requirements Describing Burden of Disease Across Vaccine Development and Evaluation Objectives for Acute Group A Streptococcus Diseases
| Clinical Endpoint | Vaccine Objective | |||
|---|---|---|---|---|
| Advocacy | Regulatory/Licensure | Policy and Post-Licensure Evaluation | Financing | |
| Pharyngitis (children) |
|
|
|
|
| Impetigo (children) |
|
|
|
|
| Cellulitis |
|
|
|
|
| Invasive Strep A |
|
|
|
|
| Scarlet fever |
|
|
|
|
Abbreviations: AMR, antimicrobial resistance; DALY, disability-adjusted life-year; HIC, high-income country; LMIC, low- and middle-income country; Strep A, group A Streptococcus.
Table 3.
Priorities for Data Requirements Describing Burden of Disease Across Vaccine Development and Evaluation Objectives for Immune-Mediated Sequalae of Group A Streptococcus
| Objective | ||||
|---|---|---|---|---|
| Clinical Endpoint | Advocacy | Regulatory/Licensure | Policy and Post-Licensure Evaluation | Financing |
| ARF |
|
|
|
|
| RHD |
|
|
|
|
| APSGN |
|
|
|
|
Abbreviations: APSGN, acute post-streptococcal glomerulonephritis; ARF, acute rheumatic fever; HIC, high-income country; LMIC, low- and middle-income country; RHD, rheumatic heart disease.
In application of this framework to Strep A, we have considered the target population, established by the WHO Preferred Product Characteristics [24], to be infants and/or young children. Pharyngitis and impetigo have been strategically targeted as initial, feasible clinical endpoints of a Strep A vaccine [24]. Both are associated with considerable health burden and are assumed to be primary intermediates on the causal pathway to immune-mediated diseases, such as acute rheumatic fever (ARF) and RHD, and a proportion of invasive Strep A diseases. While these efficacy targets have been set irrespective of the strain and serotype coverage of a future Strep A vaccine, we consider the importance of strain-specific data for certain vaccine objectives—in particular, advocacy and regulatory oversight and licensure. This is particularly important as the emm types of Strep A causing disease vary across geographical settings and over time [25]. While some vaccine candidates are not serotype specific, varying multivalent vaccines are also in development [26] and serotype replacement may be an important consideration when collating or evaluating data on Strep A burden of disease.
Acute Diseases
Prioritization of disease burden estimates of acute Strep A clinical syndromes varies by vaccine objective. For advocacy, it is important to focus on clinical endpoints that are most likely to influence decision making, such as invasive Strep A, which is the highest driver of overall Strep A deaths in most HICs. The incidence of invasive Strep A has remained high or is increasing in multiple countries (eg, the United States [27], United Kingdom [28], and Australia [29]) but likely to be underrecognized in LMICs, potentially hampering advocacy requirements. Scarlet fever has also recently increased across the United Kingdom [30]. Data to support vaccine acceptability are also critical to support advocacy efforts, given that vaccine hesitancy is a well-recognized global issue [31].
For the regulatory/licensure objective, burden of disease data need to be pathogen- and, where possible, strain-specific. Active prospective surveillance with laboratory-confirmed clinical endpoints and focused on the early vaccine development targets (pharyngitis and impetigo) will be necessary to generate burden of disease data for this objective. Sites with established active surveillance for pharyngitis or impetigo can transition to become phase II or III vaccine trial sites.
Policy review often assesses the impact of vaccination on all-cause disease syndromes (eg, all-cause pharyngitis, cellulitis, pneumonia, or sepsis). Due to the mild–moderate symptomatology of Strep A pharyngitis, estimates of disease incidence should include community surveillance data and data from primary care, healthcare clinics, and emergency departments to enable policy decisions within the health sector. While impetigo is generally seen as an issue requiring primary care and also requires community surveillance, a high hospitalization burden in First Nations populations (eg, Australia [32]) has been noted using International Classification of Diseases, 10th Revision (ICD-10), coded skin infections. These data will prove useful for post-licensure population studies evaluating disease trends pre- and post-vaccine introduction. Given increasing global concerns of AMR, the use of burden of disease data to measure vaccine impact on AMR and estimate reductions in antibiotic use is an additional important requirement for the policy objective [33].
Cost-of-illness data are essential for financing decisions. However, the drivers of costs differ across acute Strep A endpoints and different socioeconomic settings. For pharyngitis, the associated consequences of increasing AMR and parental productivity losses are likely key drivers for the value of vaccination; the importance of population AMR trends is recognized by WHO’s vaccine roadmap [24]. It was recently estimated that 17% of antibiotic prescriptions for pharyngitis among US children could be prevented by a Strep A vaccine [34]. For invasive Strep A, the drivers of burden are more likely to be hospitalizations and mortality; hence, data requirements need to be targeted to address these.
Immune-Mediated Sequelae
Rheumatic heart disease has been a major focus of Strep A burden of disease research [35, 36] and more advocacy efforts, including the need for a safe and effective vaccine, are established (eg, the global call to action from the American Heart Association and the World Health Assembly [37]) compared with those for other Strep A endpoints. While initial efficacy of a Strep A vaccine is primarily focused on acute endpoints, data to describe the progression from acute and common conditions (eg, pharyngitis and impetigo) [38] to chronic conditions like ARF and RHD are needed, in particular for the policy and financing objectives. This will provide key stakeholders critical information necessary to alleviate any vaccine safety concerns and have sufficient confidence in modeling forecasts that estimate vaccine impact on severe outcomes.
For policy evaluation, longitudinal data describing the changes in incidence and prevalence will be needed pre- and post-vaccine introduction to assist in understanding population vaccine impact. Knowledge of background ARF and RHD rates in jurisdictions of high incidence is important, especially in light of concerns of enhanced disease following vaccination—one of the prior impediments to a Strep A vaccine development [39]. Additionally, for LMICs, data on country-level socioeconomic indicators are likely to be important determinants of population-level disease burden.
IDENTIFICATION OF RESEARCH PRIORITIES
Guided by this framework, we have identified 4 research priorities for Strep A burden of disease.
Establish sentinel surveillance sites for pharyngitis (and impetigo) measuring age-specific disease burden. To address the regulatory and licensure objective, surveillance sites need to be established to facilitate future vaccine trials. Such activities are underway through the Australian Strep A Vaccine Initiative (ASAVI; www.asavi.org.au) and surveillance activities in remote Australia [40], but surveillance sites in LMICs are needed. For LMICs, adequate local surveillance infrastructure is necessary to build awareness of future benefits of a vaccine [3, 41].
Collate data to describe the incidence of invasive Strep A in LMICs. There is currently a dearth of published age-specific data in LMICs, which is critical for advocacy, policy evaluation, and financing vaccine objectives. Leveraging Strep A data from existing surveillance networks, focusing on LMICs, presents an option to fill this data gap.
Assess the attributable fraction of Strep A to cellulitis. Cellulitis has been demonstrated as a major contributor to Strep A burden, cost, and therefore value of a vaccine in Australia [20] and New Zealand [42]. The burden of Strep A cellulitis in other jurisdictions is unknown. Synthesis and analysis of existing data or designing prospective studies are critical to understanding age-specific rates for advocacy objectives. This will likely become increasingly important with future Strep A vaccines targeting adult populations [24].
Develop Strep A burden of disease estimates through the Global Burden of Disease (GBD) Project. There are few Strep A–specific burden estimates. These will become increasingly important, especially for advocacy, to compare its disease burden with that of other diseases within and across countries.
Other research priorities identified include the following: (1) the need to better understand the drivers of country, regional, and international vaccine decision making with increased connections through the relevant immunization technical advisory groups; (2) multi-country epidemiological record linkage studies using administrative health data across all Strep A endpoints; and (3) quantifying antibiotic use for pharyngitis.
CONCLUSIONS
We developed a framework that describes the different requirements and components of burden of disease data to address 4 interrelated but distinct vaccine objectives—advocacy, regulatory oversight and licensure, policy, and financing. By using these 4 different lenses, we described the data needs across the spectrum of Strep A clinical outcomes and identified research priorities that map to and will facilitate achieving each of these critical vaccine objectives. This framework is meant to be dynamic, being both updated as Strep A vaccine candidates progress through clinical trials and development, as well as adapted for other diseases with defined vaccine needs. Importantly, its use is envisaged in coordinating the vaccine research and development efforts among international stakeholders and setting the IA2030 research and innovation agenda for Strep A and other important diseases on the vaccine development horizon.
Supplementary Material
Contributor Information
Hannah C Moore, Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Western Australia, Australia.
Jeffrey W Cannon, Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Western Australia, Australia; Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA.
David C Kaslow, PATH, Seattle, Washington, USA.
Theresa Lamagni, UK Health Security Agency, London, United Kingdom.
Asha C Bowen, Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Western Australia, Australia; Perth Children’s Hospital, Perth, Western Australia, Australia.
Kate M Miller, Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Western Australia, Australia.
Thomas Cherian, MMGH Consulting, Geneva, Switzerland.
Jonathan Carapetis, Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Western Australia, Australia; Perth Children’s Hospital, Perth, Western Australia, Australia.
Chris Van Beneden, CDC Foundation, Atlanta, Georgia, USA.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Patient Consent for Publication
This study did not receive nor require ethics approval, as it does not involve human and animal participants.
Notes
Author Contributions. H. C. M., J. W. C., D. C. K., J. C., and C. V. B. developed the framework through consultation with the SAVAC Burden of Disease Working Group (BoDWG). The BoDWG includes 13 members from 7 geographically diverse countries (representing all except for 1 of the 6 WHO regions), with expertise covering Strep A and other VPDs, disease surveillance, and vaccine program implementation. Further details on the BoDWG can be found at https://savac.ivi.int/what_we_do. The BoDWG operates on a purely volunteer basis with no operational budget and meets virtually. All members agreed on the 4 vaccine objectives and were invited to provide detailed comments on the structure and content of the framework. H. C. M. drafted the first version of the manuscript. All other co-authors provided input into the framework. All named authors reviewed the manuscript and provided feedback and edits. All authors approved the final manuscript and the decision to submit for publication.
Acknowledgments. The authors thank Jean-Louis Excler for his helpful comments on the framework.
Financial support. This work was supported by the International Vaccine Institute, the Wellcome Trust (grant number 215490/Z/19/Z), and the National Health and Medical Research Council of Australia (to A. C. B. and J. W. C.).
Members of the SAVAC Burden of Disease Working Group. Jonathan Carapetis, Chris Van Beneden, David C. Kaslow, Thomas Cherian, Theresa Lamagni, Mark Engel, Jeffrey W. Cannon, Hannah C. Moore, Asha C. Bowen, Anna Seale, Gagandeep Kang, David Watkins and Sam Kariuki.
References
- 1. UNICEF Sustainable Development Goals (SDGs) for children. 2021. Available at: https://data.unicef.org/sdgs/. Accessed 26 August 2021.
- 2. Lindstrand A, Cherian T, Chang-Blanc D, Feikin D, O’Brien KL. The world of immunization: achievements, challenges, and strategic vision for the next decade. J Infect Dis 2021; 224:S452–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levine OS, Hajjeh R, Wecker J, et al. A policy framework for accelerating adoption of new vaccines. Human Vaccines 2010; 6:1021–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization Immunization Agenda 2030: a global strategy to leave no one behind. 2020. Available at: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030. Accessed 1 April 2020.
- 5. Le TT, Cramer JP, Chen R, Mayhew S. Evolution of the COVID-19 vaccine development landscape. Nat Rev Drug Discov 2020; 19:667–8. [DOI] [PubMed] [Google Scholar]
- 6. Bloom DE, Cadarette D, Ferranna M. The societal value of vaccination in the age of COVID-19. Am J Public Health 2021; 111:1049–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim L, Rha B, Abramson JS, et al. Identifying gaps in respiratory syncytial virus disease epidemiology in the United States prior to the introduction of vaccines. Clin Infect Dis 2017; 65:1020–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shawar YR, Shiffman J. Generating global priority for addressing rheumatic heart disease: a qualitative policy analysis. J Am Heart Assoc 2020; 9:e014800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Macleod CK, Bright P, Steer AC, Kim J, Mabey D, Parks T. Neglecting the neglected: the objective evidence of underfunding in rheumatic heart disease. Trans R Soc Trop Med Hyg 2019; 113:287–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hand RM, Snelling TL, Carapetis JR.. 40—Group A Streptococcus. In: Ryan ET, Hill DR, Solomon T, Aronson NE, Endy TP, eds. Hunter’s Tropical Medicine and Emerging Infectious Diseases. 10th ed. London: Elsevier; 2020:429–38. [Google Scholar]
- 11. Frieden TR. Six components necessary for effective public health program implementation. Am J Public Health 2014; 104:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. GAVI The Vaccine Alliance, PATH Advocacy for immunization: how to generate and and maintain support for vaccination programs. 2001.. Available at: https://www.who.int/immunization/hpv/communicate/advocacy_for_immunization_gavi_path_2001.pdf. Accessed 1 April 2021.
- 13. Hajjeh R. Accelerating introduction of new vaccines: barriers to introduction and lessons learned from the recent Haemophilus influenzae type B vaccine experience. Philos Trans R Soc Lond B Biol Sci 2011; 366:2827–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tapia-Conyer R, Betancourt-Cravioto M, Saucedo-Martínez R, Motta-Murguía L, Gallardo-Rincón H. Strengthening vaccination policies in Latin America: an evidence-based approach. Vaccine 2013; 31:3826–33. [DOI] [PubMed] [Google Scholar]
- 15. Munoz FM, Cramer JP, Dekker CL, et al. Vaccine-associated enhanced disease: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine 2021; 39:3053–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Menkir TF, Jbaily A, Verguet S. Incorporating equity in infectious disease modeling: case study of a distributional impact framework for measles transmission. Vaccine 2021; 39:2894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization Measuring impact of streptococcus pneumoniae and Haemophilus influenzae type b conjugate vaccination. World Health Organization. 2012. Available at: https://apps.who.int/iris/handle/10665/75835:https://apps.who.int/iris/handle/10665/75835. Accessed 1 April 2021. [Google Scholar]
- 18. Mulholland EK. Use of vaccine trials to estimate burden of disease. J Health Popul Nutr 2004; 22:257–67. [PubMed] [Google Scholar]
- 19. GAVI The Vaccine Alliance. Report to the Board June 2018—vaccine investment strategy: short list 2018 6-7 June 2018. Available at: https://www.gavi.org/about/strategy/vaccine-investment-strategy/:https://www.gavi.org/about/strategy/vaccine-investment-strategy/. Accessed 1 April 2021.
- 20. Cannon JW, Jack S, Wu Y, et al. An economic case for a vaccine to prevent group A streptococcus skin infections. Vaccine 2018; 36:6968–78. [DOI] [PubMed] [Google Scholar]
- 21. Bowen AC, Mahé A, Hay RJ, et al. The global epidemiology of impetigo: a systematic review of the population prevalence of impetigo and pyoderma. PLoS One 2015; 10:e0136789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Katzenellenbogen JM, Seth R, Bond-Smith D, Wyber R, Noonan K, Halkon C. Overview of the epidemiology of Strep A infections, ARF and RHD in Australia: a contemporary snapshot from the ERASE project. Med J Aust 2020; 213:S5–8. [Google Scholar]
- 23. Cernuschi T, Gaglione S, Bozzani F. Challenges to sustainable immunization systems in Gavi transitioning countries. Vaccine 2018; 36:6858–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vekemans J, Gouvea-Reis F, Kim JH, et al. The path to group A Streptococcus vaccines: World Health Organization Research and Development Technology roadmap and preferred product characteristics. Clin Infect Dis 2019; 69:877–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Steer AC, Law I, Matatolu L, Beall BW, Carapetis JR. Global emm type distribution of group A streptococci: systematic review and implications for vaccine development. Lancet Infect Dis 2009; 9:611–6. [DOI] [PubMed] [Google Scholar]
- 26. Dale JB, Walker MJ. Update on group A streptococcal vaccine development. Curr Opin Infect Dis 2020; 33:244–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nelson GE, Pondo T, Toews K-A, et al. Epidemiology of invasive group A streptococcal infections in the United States, 2005–2012. Rev Infect Dis 2016; 63:478–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Public Health England Laboratory surveillance of pyogenic and non-pyogenic streptococcal bacteraemia in England, Wales and Northern Ireland: 2018. 2019. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/847147/hpr4119_pnp-strptccc.pdf:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/847147/hpr4119_pnp-strptccc.pdf. Accessed 26 August 2021.
- 29. Wright CM, Moorin R, Pearson G, Dyer JR, Carapetis JR, Manning L. Increasing incidence of invasive group A streptococcal disease in Western Australia, particularly among Indigenous people. Med J Aust 2021; 215:36–41. [DOI] [PubMed] [Google Scholar]
- 30. Lamagni T, Guy R, Chand M, et al. Resurgence of scarlet fever in England, 2014–16: a population-based surveillance study. Lancet Infect Dis 2018; 18:180–7. [DOI] [PubMed] [Google Scholar]
- 31. Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Hum Vaccines Immunother 2013; 9:1763–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Abdalla T, Hendrickx D, Fathima P, et al. Hospital admissions for skin infections among Western Australian children and adolescents from 1996 to 2012. PLoS One 2017; 12:e0188803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jansen KU, Anderson AS. The role of vaccines in fighting antimicrobial resistance (AMR). Hum Vaccines Immunother 2018; 14:2142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lewnard JA, King LM, Fleming-Dutra KE, Link-Gelles R, Van Beneden CA. Incidence of pharyngitis, sinusitis, acute otitis media, and outpatient antibiotic prescribing preventable by vaccination against group A Streptococcus in the United States. Clin Infect Dis 2020; 73:e47–58. [DOI] [PubMed] [Google Scholar]
- 35. Noubiap JJ, Agbor VN, Bigna JJ, Kaze AD, Nyaga UF, Mayosi BM. Prevalence and progression of rheumatic heart disease: a global systematic review and meta-analysis of population-based echocardiographic studies. Sci Rep 2019; 9:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med 2017; 377:713–22. [DOI] [PubMed] [Google Scholar]
- 37. Beaton A, Kamalembo FB, Dale J, et al. The American Heart Association’s call to action for reducing the global burden of rheumatic heart disease: a policy statement from the American Heart Association. Circulation 2020; 142:e358–68. [DOI] [PubMed] [Google Scholar]
- 38. Yeoh DK, Anderson A, Cleland G, Bowen AC. Are scabies and impetigo ‘normalised’? A cross-sectional comparative study of hospitalised children in northern Australia assessing clinical recognition and treatment of skin infections. PLoS Negl Trop Dis 2017; 11:e0005726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Massell BF, Honikman LH, Amezcua J. Rheumatic fever following streptococcal vaccination: report of three cases. JAMA 1969; 207:1115–9. [PubMed] [Google Scholar]
- 40. Barth D, Mullane MJ, Sampson C, et al. Missing Piece Study protocol: prospective surveillance to determine the epidemiology of group A streptococcal pharyngitis and impetigo in remote Western Australia. BMJ Open 2022; 12:e057296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ngcobo NJ, Cameron NA. The decision making process on new vaccines introduction in South Africa. Vaccine 2012; 30:C9–13. [DOI] [PubMed] [Google Scholar]
- 42. Cannon JW, Zhung J, Bennett J, et al. The economic and health burdens of diseases caused by group A Streptococcus in New Zealand. Int J Infect Dis 2021; 103:176–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.