Abstract
The recommendations of the AGO Breast Committee on the surgical therapy of breast cancer were last updated in March 2022 (www.ago-online.de). Since surgical therapy is one of several partial steps in the treatment of breast cancer, extensive diagnostic and oncological expertise of a breast surgeon and good interdisciplinary cooperation with diagnostic radiologists is of great importance. The most important changes concern localization techniques, resection margins, axillary management in the neoadjuvant setting and the evaluation of the meshes in reconstructive surgery. Based on meta-analyses of randomized studies, the level of recommendation of an intraoperative breast ultrasound for the localization of non-palpable lesions was elevated to “++”. Thus, the technique is considered to be equivalent to wire localization, provided that it is a lesion which can be well represented by sonography, the surgeon has extensive experience in breast ultrasound and has access to a suitable ultrasound device during the operation. In invasive breast cancer, the aim is to reach negative resection margins (“no tumor on ink”), regardless of whether an extensive intraductal component is present or not. Oncoplastic operations can also replace a mastectomy in selected cases due to the large number of existing techniques, and are equivalent to segmental resection in terms of oncological safety at comparable rates of complications. Sentinel node excision is recommended for patients with cN0 status receiving neoadjuvant chemotherapy after completion of chemotherapy. Minimally invasive biopsy is recommended for initially suspect lymph nodes. After neoadjuvant chemotherapy, patients with initially 1 – 3 suspicious lymph nodes and a good response (ycN0) can receive the targeted axillary dissection and the axillary dissection as equivalent options.
Key words: breast cancer, breast surgery, surgical therapy, guidelines, neoadjuvant chemotherapy
Introduction
The Breast Committee of the Working Group for Gynecological Oncology, e. V. (AGO Mamma) last updated the recommendations for the diagnosis and therapy of breast cancer in March 2022 ( www.ago-online.de ) 1 . The new study results and current congress contributions were taken into account. Two out of a total of 26 chapters deal with surgical treatment:
Breast Cancer Surgery – Oncological Aspects
Oncoplastic and Reconstructive Surgery
This year, both chapters were consulted for the first time with the AWOgyn (Working Group for Reconstructive Surgery in Oncology-Gynecology). Prior to the vote, the current evidence was discussed thoroughly within the Committee. In 2022, the Committee focused on the following topics: Resection margins, localization techniques and axillary surgical management in the neoadjuvant setting. Since surgical therapy is one of several partial steps in the treatment of breast cancer, extensive diagnostic and oncological expertise of a breast surgeon and good interdisciplinary cooperation with diagnostic radiologists is of great importance. The following article presents the recommendations and current evidence for surgical and plastic-reconstructive therapy of the breast.
Surgical Therapy of the Breast
Oncological safety of breast-conserving therapy
Breast-conserving therapy (BCT), defined as breast-conserving surgery (BCS), followed by radiotherapy, became the standard procedure in the 1990s, after several large randomized studies were able to show that overall survival (OS) and breast cancer-specific survival (BCSS) after BCT and a mastectomy are identical 2 , 3 . Meanwhile, results from several prospective registers from different countries are available, suggesting a superiority of BCT 4 , 5 , 6 , 7 , 8 . The latest study comes from Sweden. De Boniface et al. from the Karolinska Institute evaluated clinical courses of 48 986 women 7 . After a median follow-up time of 6.2 years, OS and BCSS were significantly longer in women receiving BCT than after a mastectomy with or without radiation therapy. Other possible confounders, such as age and socio-economic status, were taken into account. Patients who are not receiving neoadjuvant chemotherapy should only be recommended to undergo a mastectomy if the tumor size in relation to the breast size does not permit a breast-conserving procedure, the negative resection margins are not reached despite repeated secondary resection, or inflammatory breast cancer is present.
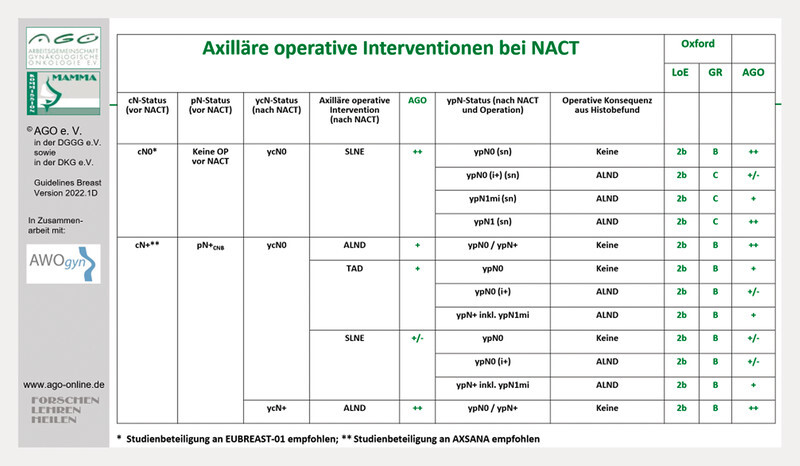
Localization of non-palpable breast lesions
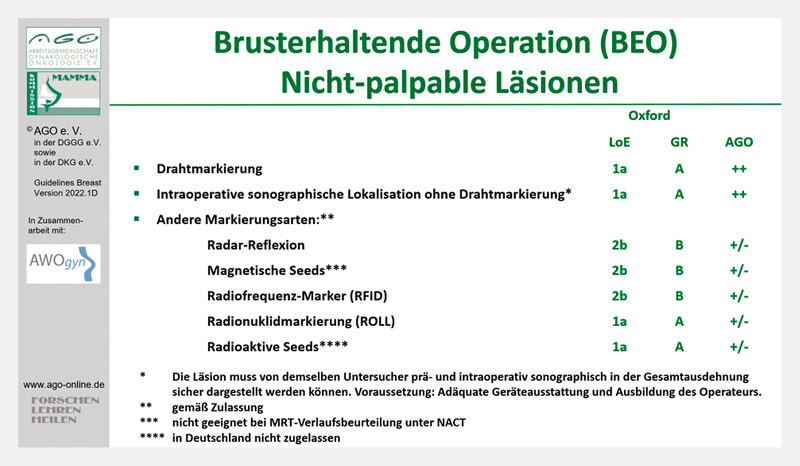
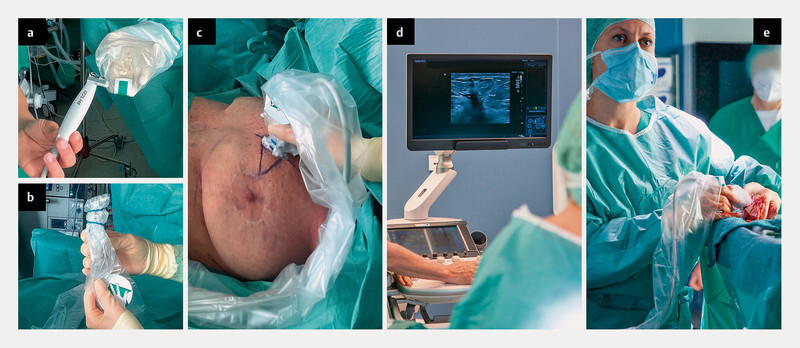
70 – 80% of all breast cancer patients nowadays undergo conserving surgery 9 . Many of these tumors are non-palpable and their removal must be supported by imaging. Various techniques are available for this ( Fig. 1 ). In addition to the wire localization, which has long been regarded as the gold standard, sonographically visible lesions can be localized with the aid of intraoperative sonography ( Fig. 2 ). This option has been awarded a double plus recommendation (++) in 2022 (for definitions of the AGO recommendation levels, see Table 1 ). The recommendation is based on meta-analyses of randomized studies, which confirmed that R0 resection is achieved significantly more frequently with the use of intraoperative breast ultrasound compared to wire localization 10 , 11 . In palpable breast cancer, the advantages of intraoperative sonography compared to palpation-guided surgery have also been demonstrated: the R0 resection rate can be increased and the rate of secondary resection can be reduced 11 , 12 . Interestingly, resection volumes could be reduced by the use of intraoperative sonography in some studies 12 , 13 , 14 . Thus, the technique allows the targeted removal of the tumor and at the same time spares healthy tissue.
Fig. 1.
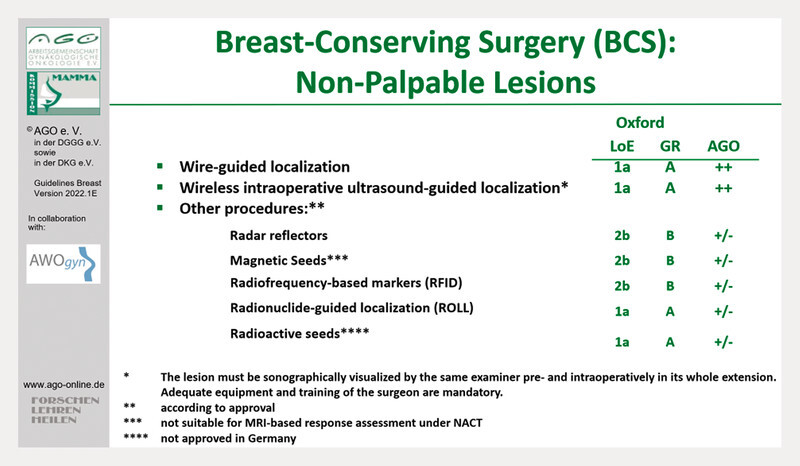
Current recommendations of the AGO Breast Committee on the localization techniques for non-palpable lesions.
Fig. 2.
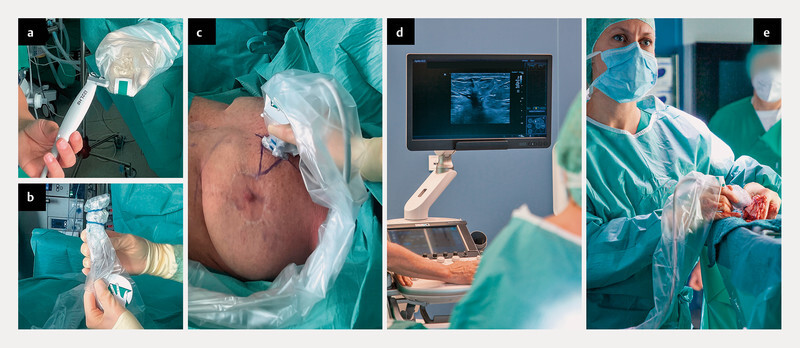
Practical use of intraoperative breast ultrasound: a The sonographic linear probe is obtained in a sterile manner. There should be sufficient gel between the probe and the film. b The sterile cover is fixed to the probe. c, d Imaging of the lesion by the surgeon. During the operation, the lesion is imaged intermittently in order to ensure a sufficient resection distance in all directions. e Immediately after removal of the tissue, the specimen is examined by ultrasound.
Table 1 Recommendation levels of the AGO Breast Committee.
| ++ | This investigation or therapeutic intervention is highly beneficial for patients, can be recommended without restriction, and should be performed. |
| + | This investigation or therapeutic intervention is of limited benefit to patients and can be performed. |
| +/− | This investigation or therapeutic intervention has not shown benefit for patients and may be performed only in individual cases. According to current knowledge, a general recommendation cannot be given. |
| − | This investigation or therapeutic intervention can be of disadvantage to patients and might not be performed. |
| − − | This investigation or therapeutic intervention is of clear disadvantage for patients and should be avoided or omitted in any case. |
Important prerequisites for the use of intraoperative sonography are:
The lesion must be sonographically visualized by the same examiner pre- and intraoperatively in its whole extension.
The surgeon must have adequate training in breast ultrasound. A preoperative sonographic examination by the surgeon is necessary to assess whether the lesion is suitable for this technique.
A high-quality ultrasound device must be available during the operation.
This year, the modern probe-guided detection methods were thoroughly discussed. In these techniques, a marker is placed in the lesion preoperatively and located during the operation using a special probe (e.g., magnetic, radio-frequency- or radar-based). With the exception of radioactive techniques (radioactive seeds and radionuclide labelling), which are widespread abroad but have not been approved in Germany, these methods have so far been mainly investigated in single-arm, industry-initiated studies. For this reason, they are rated +/−. There is an urgent need for independent studies that will compare these procedures with wire localization and intraoperative sonography in a real-world setting. One of the upcoming studies is the Intergroup Trial MELODY ( http://melody.eubreast.com ). It must also be kept in mind that magnetic markers in particular significantly limit the diagnostic power of MRI in the assessment of the response to therapy due to susceptibility artifacts. Regardless of the localization technique, specimen radiography or specimen sonography is mandatory (AGO ++).
Resection margins
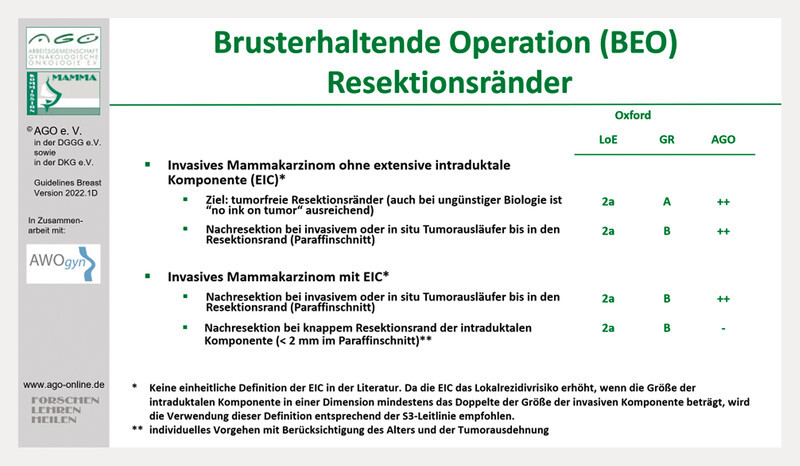
In the case of invasive breast cancer, no secondary resection has been recommended for several years when the “no tumor on ink” situation is reached (i.e., no tumor cell touches the edge of the specimen). In contrast, a resection margin of 2 mm is aimed for in the case of pure DCIS. One of the most frequently discussed questions in the tumor boards concerns the optimal resection margin in invasive breast cancer with a DCIS component ( Fig. 3 ). In this situation, the prognosis and the adjuvant therapy decision are determined by the invasive component. The goal here is also to achieve a “no tumor on ink” situation, even in patients with an additional extensive intraductal component. Routine secondary excision should not be performed in case of a negative, but “close” resection margin. In selected cases, however, an individualized decision is possible, taking into account the extent of the invasive and intraductal components and the patient-related factors such as age.
Fig. 3.
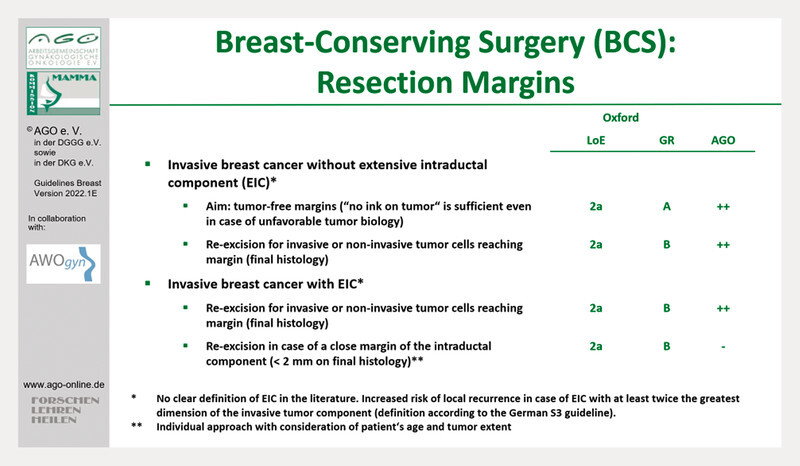
Current recommendations of the AGO Breast Committee on resection margins in invasive breast cancer.
Surgical therapy of the breast after neoadjuvant chemotherapy
In patients receiving neoadjuvant therapy, the tumor should be marked prior to system therapy. A clip/coil is usually used for this purpose, but the probe-guided localization methods are also available. It is important to accurately document the extent and localization of the lesion(s) at the time of diagnosis, as well as the position of the marker, in order to enable correct surgical planning after neoadjuvant therapy. If the tumor responds to therapy, the lesion is resected within so-called new borders.
Surgical Therapy of Ductal Carcinoma in Situ
The ductal carcinoma in situ (DCIS) corresponds to a heterogeneous group of neoplastic lesions in the breast, in which the tumor cells spread within the milk ducts and do not infiltrate the basement membrane. The DCIS, which occurs alone and without any further invasive component, is generally detected via mammography screening by suspicious areas of microcalcification, and accounts for about 25% of all breast cancers. The most important treatment objective is to avoid invasive recurrences. An operation is the most important treatment method. Adjuvant radiotherapy can reduce non-invasive and invasive recurrence by about 50% in the case of a breast-conserving procedure. Adjuvant endocrine therapy can be offered as prevention, but does not affect the local recurrence rate after a DCIS. For this reason, the operation represents the basic therapy of the DCIS, while adjuvant radiation or endocrine therapy should be indicated in consideration of risk reduction and side effects.
In 5 – 25% of patients, up-staging to an invasive carcinoma is observed after breast-conserving surgery of DCIS confirmed by biopsy. Ipsilateral recurrence occurs after 10 years in about 25% of women who do not receive adjuvant radiotherapy and in 10% with radiation. Breast cancer-specific mortality is 3.3%. This means that women with a DCIS have a 1.8- to 3-fold increased risk of death compared to the normal population 15 .
Preoperative diagnosis by means of clinical examination, mammography and sonography is necessary to assess the extent and to exclude an accompanying invasive component. The standard therapy of the (non-palpable) DCIS, which is dependent on tumor size in relation to breast size, is primarily the excision after stereotactic marking with intraoperative specimen radiography. If imaging shows that the target lesion has not been completely removed, an immediate re-excision is required. In rare cases and depending on the extent, a mastectomy may also be necessary in order to achieve adequate safety margin. The desired free margin is 2 mm for pure DCIS without an invasive component. This applies to patients receiving adjuvant radiotherapy after the operation. For patients for whom no radiotherapy is planned, there are no evidence-based recommendations for optimal resection margins.
Axillary staging (sentinel lymph node excision, SLNE) is generally not recommended in patients receiving breast-conserving surgery. This also applies in the case of an increased risk for the later detection of an invasive component (extent, grading). In this case, a secondary SLNE is possible. SLNE is recommended in patients undergoing a mastectomy. The reason lies in the fact that in the case of a histologically detectable invasion, breast removal destroys the lymphatic drainage paths, which means that later SLNE is then no longer possible for technical reasons.
Oncoplastic Operations
An oncoplastic operation is defined as a plastic surgical technique at the time of tumor removal to achieve safe resection borders and to preserve an aesthetic shape to the breast. The focus should be on favorable scar placement, adequate soft tissue formation, the choice of a suitable reconstruction method, and a possible adaptation operation of the contralateral breast in order to achieve a symmetrical result. A wide variety of techniques can be considered, such as intramammary or dermoglandular rotation, the round block or batwing technique, B-plasty or a mastopexy or reduction mammoplasty adapted to the tumor position, to name just a few. In order to be able to adequately document the surgical costs to the payers as well, it is helpful to use one of the available classifications, for example the classification according to Hoffmann, which defines different degrees of complexity and thus reproducibly describes the outlay of the operation 16 .
An oncoplastic operation can also replace a mastectomy in selected cases (LoE 2b/B/AGO +) due to the large number of existing techniques, and is equivalent to a regular segmental resection in terms of oncological safety at comparable rates of complications.
Breast Reconstruction
Various options are available for breast reconstruction. Both the one-stage use of silicone implants or the two-stage reconstruction in combination with expanders or the autologous reconstruction with pedicled or free tissue transfer are rated as “+” by the AGO. The reconstruction can be carried out both as an immediate reconstruction, especially in the case of skin-sparing or nipple-sparing mastectomy (SSM/NSM), and as a two-stage procedure (LoE 3b/B/AGO ++). However, in the case of the latter, the loss of the skin mantle needs to be taken into account. A delayed reconstruction is also frequently carried out in the clinical routine, usually in the case of an autologous reconstruction. In this case, the implant after an SSM/NSM is inserted only temporarily (as a “placeholder”) in order to be replaced later by autologous tissue. The advantage of this strategy is to perform the definitive reconstruction after receiving the final histology and possibly completed radiotherapy (LoE 3b/B/AGO +).
Peri-/intraoperative antisepsis/antibiosis
Peri-/intraoperative treatment with local antiseptic and/or antibiotic therapy in breast reconstruction is associated with a statistically significant advantage compared with no such treatment. A meta-analysis of 11 studies with 15 966 mastectomies showed that the rate of infection of the reconstructed breast could be significantly reduced (RR = 0.26, 95% CI: 0.12 – 0.60, p = 0.001). In contrast, it was not possible to show a corresponding advantage by prolonging intravenous antibiosis compared with antibiotics for 24 hours (RR = 0.80, 95% CI: 0.60 – 1.08, p = 0.13). Therefore, perioperative antibiotic prophylaxis is only recommended for a maximum of 24 hours (LoE 2a/B/+) 17 , 18 .
Mesh/ADM-based implant reconstruction
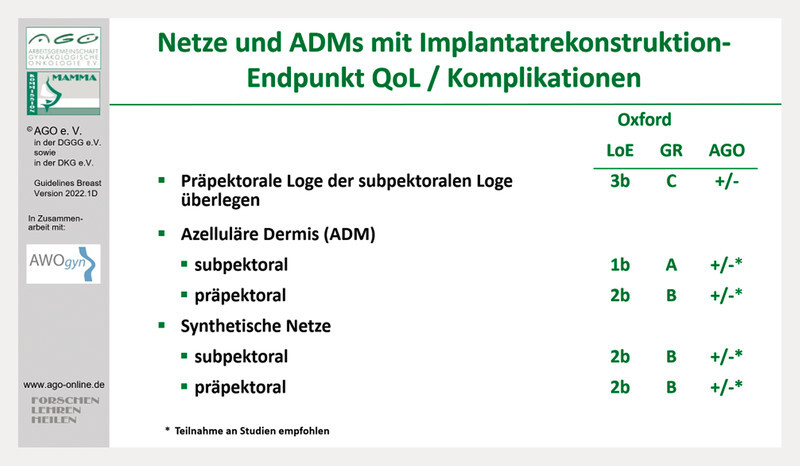
While, until a few years ago, a subpectoral implant position was still the usual choice in implant reconstruction, the epipectoral implantation has become increasingly popular. Improved implants, nets/mesh pockets, acellular dermal matrices (ADMs) or tissue matrices as well as the possibility of a later modelling of the reconstructed breast by means of lipofilling, today guarantee cosmetically better and lastingly stable results ( Fig. 4 ). A large selection of meshes and ADMs is currently commercially available and has been reviewed in studies 19 , 20 , but a prospectively randomized head-to-head comparison is missing. The question of subpectoral vs. prepectoral positioning has also not yet been sufficiently clarified 21 . Here, the ongoing prospective randomized PREPEC study (NCT04293146) may provide additional information. A German study currently being planned will also examine whether mesh- or ADM-supported implant reconstruction and implant reconstruction without additional material have the same outcomes.
Fig. 4.
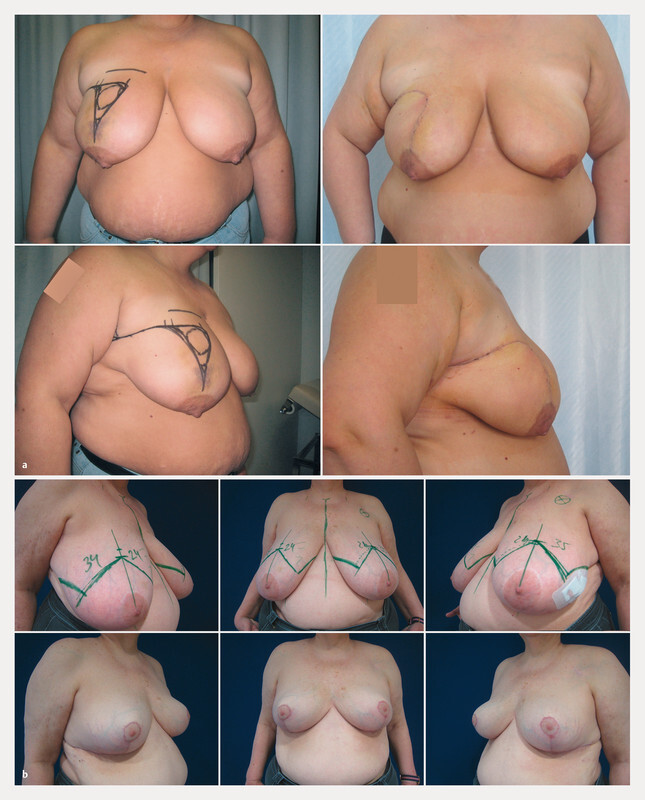
Oncoplastic breast surgery using two examples: a dermoglandular rotation on the right in the case of a large tumor to avoid a change in height of the nipple-areola complex. b Tumor-adapted reduction mammoplasty on the left with matching surgery on the right in inverse T-incision technique with cranial nipple pedicle.
Due to the limited evidence, the AGO Breast Committee cannot currently make any recommendation that favors the sub- vs. the prepectoral implant position (LoE 3b/C/AGO +/−) or a mesh- vs. an ADM-based technique ( Fig. 5 ). The surgeon should tailor the respective decision individually to the patient.
Fig. 5.
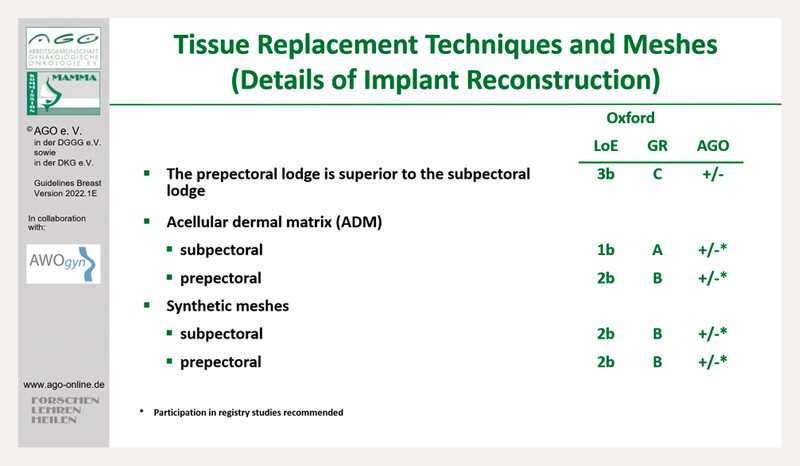
Meshes and ADMs with implant reconstruction (endpoint quality of life/complications).
Although prospectively randomized studies on the important questions are missing, it is currently evident that the complication rates in ADM-based vs. mesh-based implant reconstruction are higher 22 .
SSM/NSM and reconstruction
Irrespective of the above discussion on implant position and possible materials, it should, however, now be clear that SSM and NSM are also oncologically safe (LoE 2b/B/AGO ++) and lead to an increased quality of life for the patient (LoE 2b/B/AGO ++). With regard to the different approaches, the AGO Breast Committee does not differentiate; however, inferolateral access via the inframammary fold has the lowest complication rate. However, care should be taken during surgery to minimize the use of retractors to avoid skin necrosis.
Prevention of capsular fibrosis
The development of capsular fibrosis depends on the type of operation. In breast augmentation, it is about 2 – 8%, in reconstruction after an SSM/NSM, it is about 20%, and after additional radiotherapy, it is about 40% 23 .
Sufficient evidence for the reduction of capsular fibrosis is available for the use of textured vs. smooth implants (LoE 1a/A/AGO +) 24 . However, in particular in the case of textured implants, the risk of a breast implant-associated large-cell anaplastic lymphoma (BIA-ALCL) must be considered, which can occur with an incidence of 1 : 3000 to 1 : 30 000. The use of mesh (LoE 3a/C/AGO +) or an ADM (LoE 2a/B/AGO +) vs. nil can also lead to a reduction in capsular fibrosis 25 . The use of an intraoperative local antibiotic/antiseptic rinse can also cause a reduction in capsular fibrosis (LoE 2a/B/AGO +) 26 , but with limited evidence due to poor study quality. The use of the leukotriene antagonists montelukast and zafirlukast, which are known from asthma therapy, should be approached with caution. Data are extremely limited and data on long-term toxicity are not available 27 . A recently published systematic review could not show any advantage of massaging the breast tissue, so that everything remains the same here and a massage has no effect on the development of capsular fibrosis (LoE 3a/C/AGO −) 28 .
Surgical Management of the Axilla
Nodal status has long been regarded as the most important prognostic factor and decision-making aid for adjuvant systemic and radiotherapy. With the growing understanding of tumor biology, systemic therapy is now carried out according to the intrinsic subtypes. On the other hand, earlier tumor stages with less frequent axillary metastasis are discovered within the mammography screening 29 . The sonography of the axillary lymph nodes has also been improved technically and in terms of personnel to such an extent that sentinel lymph nodes (SLN) are only rarely affected. The question thus arises of a de-escalation of axillary surgery 30 .
Surgical management of the axilla in the adjuvant setting
The development of the SLNE at the beginning of the present millennium was a milestone in the therapy of invasive breast cancer 31 . Randomized studies have shown that the false negative rate (FNR) for SLNE is 5 – 8% and does not affect disease-free survival and overall survival 32 . Currently, an estimated 50 – 60% of all breast cancer patients at initial diagnosis are clinically nodal-negative (cN0), and patients from mammography screening even at 75% 29 .
The lymph node status at the time of diagnosis is examined clinically and sonographically. For patients with clinically and sonographically unsuspicious axillary lymph nodes, the SLNE alone is the standard (LoE 1b/A/AGO ++). The same applies to patients with breast cancer during pregnancy or breastfeeding. However, only 99m technetium colloid should be used here. In any case, 99m technetium colloid with LoE1a/GRA/AGO + has the highest recommendation level, while all other marking techniques are rated AGO +/− or AGO −. Particularly when using magnetic nanoparticles for sentinel marking, it must be taken into account that a significant limitation of the informative power of MRI imaging can also occur over several years after injection, if MRI is necessary in follow-up care, e.g., in high-risk patients. In patients with tumors > 5 cm, multifocal or multicenter breast cancer, DCIS with a planned mastectomy, male breast cancer and after previous tumor removal, SLNE should also be performed (AGO +).
Although SLNE is less radical than the classic axillary dissection (ALND), it is still an invasive procedure, which can lead to postoperative complications 33 , 34 :
Lymphedema: 10 – 20% ALND vs. 5 – 7% SLNE
Diminished quality of life: 35% ALND vs. 23% SLNE
Pain in the arm or numbness/tingling: 31% ALND vs. 11% SLNE
Ongoing prospective randomized studies (SOUND, NCT02167490; INSEMA, NCT02466737; BOOG 2013-08; NCT02271828) investigate the need for SLNE in clinically nodal-negative breast cancers and breast-conserving surgery, as SLNE is likely to have little therapeutic benefit in these patients. The optimal procedure in the case of a mastectomy is currently being researched in further prospective studies (POSNOC, NCT02401685; SENOMAC, NCT02240472).
In the INSEMA study – a prospectively randomized study comparing SLNE vs. no SLNE in patients with early invasive breast cancer (≤ 5 cm, cN0) and breast-conserving therapy – data on patient-reported outcomes in terms of quality of life were presented for the first time in 2021. The absence of SLNE was associated with clinically significant lower arm symptoms (pain in the arm or shoulder, swelling of the arm or hand and arm mobility) compared to patients with SLNE and even more compared to patients with ALND 35 .
Due to the available evidence, the ASCO recommended as early as 2021 that any axillary intervention – including SLNE – be omitted in patients over 70 years of age with favorable tumor biology (hormone receptor positive HER2-negative, T1 N0), who would receive endocrine therapy alone 36 . The AGO Breast Committee also permits refraining from axillary surgery in elderly patients with cN0 status under certain conditions (> 70 years, comorbidity, pT1, HR+, HER2-negative). In this case, SLNE is rated +/−. The indication should be made individually here. Data on the oncological outcome is expected for the SOUND study (2022) and for the INSEMA study (end of 2024).
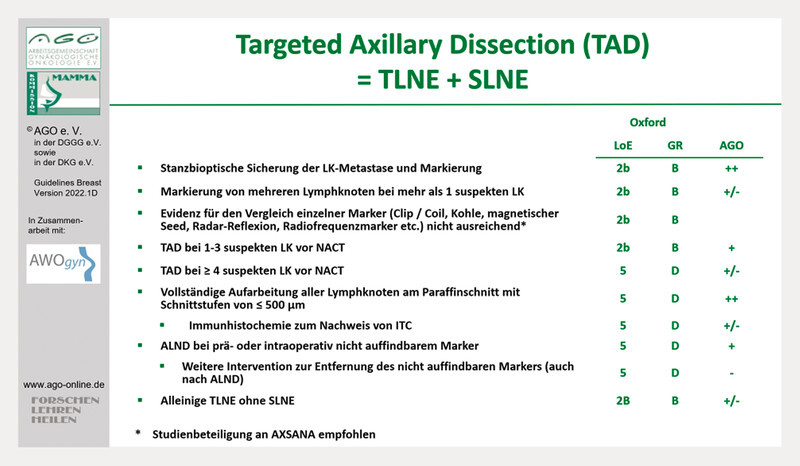
Surgical management of the axilla in the neoadjuvant setting
Patients with an indication for neoadjuvant chemotherapy (NACT) and initially clinically negative axillary lymph nodes (cN0) should not undergo surgical intervention or a core needle biopsy (CNB) before NACT. For post-NACT ycN0, only SLNE (AGO ++) is recommended. Since the axillary lymph node status is of crucial importance for the further escalation or de-escalation of post-neoadjuvant systemic therapy, ALND with different levels of recommendation is advised when tumor cells are detected ( Fig. 6 ) 37 , 38 :
Fig. 6.
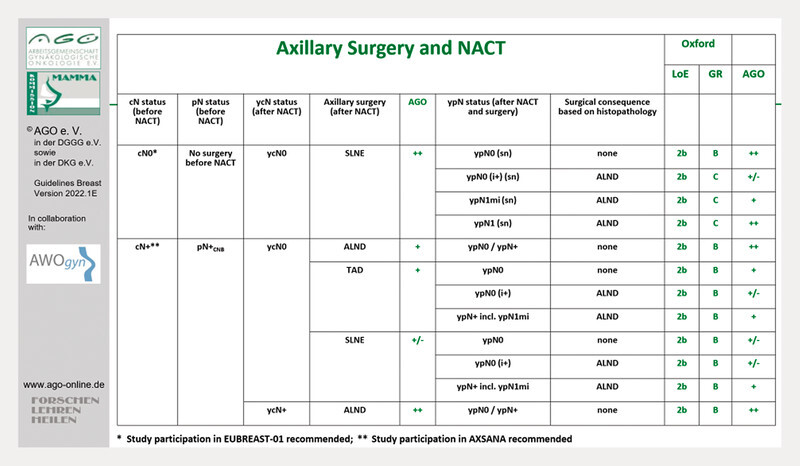
Current recommendations of the AGO Breast Committee on surgical axillary intervention in the neoadjuvant chemotherapy setting.
ypN0(i+) (sn): AGO +/−
ypN1mi (sn): AGO +
ypN1 (sn): AGO ++
A retrospective analysis of the US National Cancer Data Base (NCDB) was able to find a histopathological involvement of axillary lymph nodes in only 1.6% of cases for initially cN0 patients (N = 5377) with HER2-positive or triple-negative (TNBC) breast cancer and a pathological complete response in the breast (breast pCR) 39 . If no pCR was found in the breast, the rate of affected lymph nodes was 27% 39 . In a similar study with 290 cN0 patients and HER2+/TNBC, all patients with breast pCR (40.4%) had tumor-free axillary lymph nodes (ypN0), while 6% of patients with breast non-pCR showed positive lymph nodes (ypN+) 40 . The authors of both studies no longer consider axillary intervention in the subpopulation of the initial cN0 HER2+/TNBC and breast PCR to be necessary. The prerequisite for this, however, is the determination of the breast pCR by means of an operation 41 . Whether the safe determination of breast pCR will be possible in future through minimally invasive methods using artificial intelligence remains to be seen 42 . The prospective EUBREAST-01 study (NCT04101851) examines the absence of any form of axillary intervention in initial cN0 HER2-positive or TNBC and clinically complete remission in the breast.
In patients who have a clinically and/or sonographically positive axillary lymph node status (cN+) prior to systemic therapy, this should be confirmed using a minimally invasive core biopsy. In this context, a marking of the biopsied lymph node is often carried out in Germany. However, this is not an international standard. There is insufficient evidence for the comparison of individual markers (clip/coil, coal, magnetic seed, radar reflection, radio frequency markers, etc.), so that participation in the AXSANA study (NCT04373655) is recommended by the AGO Breast Committee 10 , 43 . ALND (AGO ++) is recommended for patients who continue to have clinically apparent lymph node involvement after NACT (ycN+). The assessment of the axillary response to NACT by imaging is of limited accuracy 44 , 45 . Current research focuses on optimal management in patients who achieve so-called axillary conversion (cN+ → ycN0). In this group, different techniques are used worldwide: ALND, SLNE, and so-called “Targeted Axillary Dissection” (TAD). To perform TAD, at least one of the affected lymph nodes must be marked before the start of NACT. This lymph node is referred to as the target lymph node. TAD is defined as the removal of the sentinel lymph node and the target lymph node. In patients who initially had a limited nodal involvement (1 – 3 suspicious lymph nodes before NACT), TAD and ALND are recommended as equivalent techniques (AGO +). In the case of higher-grade nodal involvement (4 or more suspicious lymph nodes), TAD is scored +/−, because the false-negative rate in this group may be higher ( Fig. 7 ) 46 . Depending on the histopathological findings of the lymph nodes removed during TAD, further therapy of the axilla may be recommended ( Fig. 6 ). SLNE alone in the cN+ → ycN0 collective is only rated AGO +/– and is not a standard in Germany. In contrast, SLNE alone is performed more frequently abroad. According to observational studies, the local recurrence rate is very low if three or more negative sentinel lymph nodes have been removed after NACT and radiotherapy has been performed 47 . Since “blind” axillary sampling is not indicated in these patients, TAD offers an alternative. Caudle et al. were able to demonstrate a significant reduction in the false negative rate from 10.1% with SLNE alone and 4.2% for the removal of the target lymph node (TLNE = Targeted Lymph Node Extirpation) to 1.4% for TAD 48 . If histopathology detects micro- or macrometastases at TAD, the ALND should be performed. In the case of residual isolated tumor cells (ypN0 [i+]), the therapeutic consequences are still unclear and should be investigated further in studies (e.g., AXSANA) (LoE2b/B/AGO +/−) 43 . Further studies investigate the optimal radiotherapeutic management in this setting (TAXIS, ALLIANCE A011202).
Fig. 7.
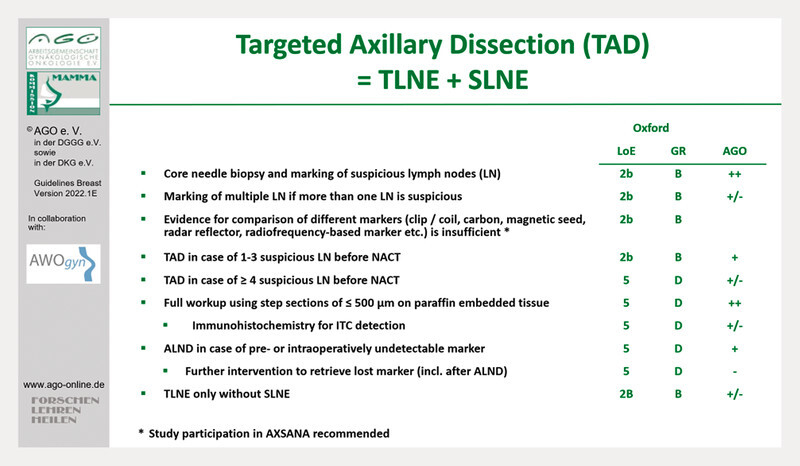
Current recommendations of the AGO Breast Committee on the Targeted Axillary Dissection.
Summary
The surgical treatment of breast cancer has undergone a change over the last two decades. The focus of research is on the de-escalation of surgical treatment. Thus, the frequency of radical surgical procedures, such as mastectomy and axillary dissection, decreases. More and more patients are recommended to undergo (oncoplastic) breast-conserving operations and techniques such as sentinel lymph node excision or targeted axillary dissection. The most important innovations in the updated version of the AGO recommendations include the upgrading of intraoperative sonography to localize non-palpable lesions and the introduction of the “no tumor on ink” target in invasive breast cancer with DCIS component, regardless of whether an extensive intraductal component is present or not. The prerequisites for a targeted axillary dissection were also defined more precisely. In particular, in patients with higher grade nodal involvement (≥ 4 suspicious lymph nodes before starting neoadjuvant chemotherapy), the technique should only be used after careful consideration.
Footnotes
Conflict of Interest/Interessenkonflikt Maggie Banys-Paluchowski received fees for lectures and consultancy activities from Roche, Novartis, Pfizer, pfm, Eli Lilly, Onkowissen, Seagen, AstraZeneca, Eisai, AstraZeneca, Amgen, Samsung, MSD, GSK, Daiichi Sankyo, Gilead, Sirius Pintuition, Pierre Fabre and study support from EndoMag, Mammotome, MeritMedical. Marcus Schmidt reports that he received personal fees for lectures and consulting activities from AstraZeneca, BioNTech, Daiichi Sankyo, Eisai, Lilly, MSD, Novartis, Pantarhei Bioscience, Pfizer, Roche and SeaGen, which are not related to this publication. Jens Huober: Research support: Celgene, Novartis, Hexal, Lilly. Lecture activity: Lilly, Novartis, Roche, Pfizer, AstraZeneca, MSD, Celgene; Eisai, Abbvie, Seagen, Gilead. Consultancy: Lilly, Novartis, Roche, Pfizer, Hexal, AstraZeneca, MSD, Celgene, Abbvie. Travel expenses: Roche, Pfizer, Novartis, Celgene, Daiichi Sankyo. Peter Dall: Lecture fees: Novartis, Pfizer, AstraZeneca, Roche, Lilly. Ad Boards: Novartis, Seagen, Daiichi Sankyo, AstraZeneca, Roche, Gilead. David Krug: honoraria from Merck Sharp & Dohme and Pfizer as well as research funding from Merck KGaA. Other authors do not indicate any conflicts of interest./ Maggie Banys-Paluchowski erhielt Honorare für Vorträge und beratende Tätigkeiten von Roche, Novartis, Pfizer, pfm, Eli Lilly, Onkowissen, Seagen, AstraZeneca, Eisai, AstraZeneca, Amgen, Samsung, MSD, GSK, Daiichi Sankyo, Gilead, Sirius Pintuition, Pierre Fabre und Studienunterstützung von EndoMag, Mammotome, MeritMedical. Marcus Schmidt berichtet, persönliche Honorare für Vorträge und Beratungstätigkeiten von AstraZeneca, BioNTech, Daiichi Sankyo, Eisai, Lilly, MSD, Novartis, Pantarhei Bioscience, Pfizer, Roche und SeaGen erhalten zu haben, die nicht im Zusammenhang mit der vorliegenden Publikation stehen. Jens Huober: Forschungsunterstützung: Celgene, Novartis, Hexal, Lilly. Vortragstätigkeit: Lilly, Novartis, Roche, Pfizer, AstraZeneca, MSD, Celgene; Eisai, Abbvie, Seagen, Gilead. Beratertätigkeit: Lilly, Novartis, Roche, Pfizer, Hexal, AstraZeneca, MSD, Celgene, Abbvie. Reisekosten: Roche, Pfizer, Novartis, Celgene, Daiichi Sankyo. Peter Dall: Vortragshonorare: Novartis, Pfizer, AstraZeneca, Roche, Lilly. Ad-Boards: Novartis, Seagen, Daiichi Sankyo, AstraZeneca, Roche, Gilead. David Krug: honoraria from Merck Sharp & Dohme and Pfizer as well as research funding from Merck KGaA. Weitere AutorInnen geben keine Interessenkonflikte an.
References/Literatur
- 1.Ditsch N, Woeckel A, Untch M. AGO Recommendations for the Diagnosis and Treatment of Patients with Early Breast Cancer (EBC): Update 2022. Breast Care. 2022 doi: 10.1159/000524879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Veronesi U, Cascinelli N, Mariani L. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–1232. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Jeong J H, Anderson S. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347:567–575. doi: 10.1056/NEJMoa020128. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal S, Pappas L, Neumayer L. Effect of breast conservation therapy vs. mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg. 2014;149:267–274. doi: 10.1001/jamasurg.2013.3049. [DOI] [PubMed] [Google Scholar]
- 5.Hofvind S, Holen A, Aas T. Women treated with breast conserving surgery do better than those with mastectomy independent of detection mode, prognostic and predictive tumor characteristics. Eur J Surg Oncol. 2015;41:1417–1422. doi: 10.1016/j.ejso.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 6.van Maaren M C, de Munck L, de Bock G H. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol. 2016;17:1158–1170. doi: 10.1016/S1470-2045(16)30067-5. [DOI] [PubMed] [Google Scholar]
- 7.de Boniface J, Szulkin R, Johansson A LV. Survival After Breast Conservation vs. Mastectomy Adjusted for Comorbidity and Socioeconomic Status: A Swedish National 6-Year Follow-up of 48986 Women. JAMA Surg. 2021;156:628–637. doi: 10.1001/jamasurg.2021.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christiansen P, Carstensen S L, Ejlertsen B. Breast conserving surgery versus mastectomy: overall and relative survival-a population based study by the Danish Breast Cancer Cooperative Group (DBCG) Acta Oncol. 2018;57:19–25. doi: 10.1080/0284186X.2017.1403042. [DOI] [PubMed] [Google Scholar]
- 9.Jahresbericht der zertifizierten Brustkrebszentren: Auditjahr 2019/Kennzahlenjahr 2018. Herausgeber: Deutsche Krebsgesellschaft (DKG), Berlin in Zusammenarbeit mit OnkoZert, Neu-Ulm. 2020. https://www.onkozert.de/2022/04/20/jahresberichte-der-zertifizierungssysteme-2022/ https://www.onkozert.de/2022/04/20/jahresberichte-der-zertifizierungssysteme-2022/
- 10.Athanasiou C, Mallidis E, Tuffaha H. Comparative effectiveness of different localization techniques for non-palpable breast cancer. A systematic review and network meta-analysis. Eur J Surg Oncol. 2022;48:53–59. doi: 10.1016/j.ejso.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Banys-Paluchowski M, Rubio I T, Karadeniz Cakmak G. Intraoperative Ultrasound-Guided Excision of Non-Palpable and Palpable Breast Cancer: Systematic Review and Meta-Analysis. Ultraschall Med. 2022 doi: 10.1055/a-1821-8559. [DOI] [PubMed] [Google Scholar]
- 12.Volders J H, Haloua M H, Krekel N M. Intraoperative ultrasound guidance in breast-conserving surgery shows superiority in oncological outcome, long-term cosmetic and patient-reported outcomes: Final outcomes of a randomized controlled trial (COBALT) Eur J Surg Oncol. 2017;43:649–657. doi: 10.1016/j.ejso.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann J, Marx M, Hengstmann A. Ultrasound-Assisted Tumor Surgery in Breast Cancer – A Prospective, Randomized, Single-Center Study (MAC001) Ultraschall Med. 2019;40:326–332. doi: 10.1055/a-0637-1725. [DOI] [PubMed] [Google Scholar]
- 14.Krishna K L, Srinath B S, Santosh D. A comparative study of perioperative techniques to attain negative margins and spare healthy breast tissue in breast conserving surgery. Breast Dis. 2020;39:127–135. doi: 10.3233/BD-200443. [DOI] [PubMed] [Google Scholar]
- 15.Narod S A, Iqbal J, Giannakeas V. Breast Cancer Mortality After a Diagnosis of Ductal Carcinoma In Situ. JAMA Oncol. 2015;1:888–896. doi: 10.1001/jamaoncol.2015.2510. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann J, Wallwiener D. Classifying breast cancer surgery: a novel, complexity-based system for oncological, oncoplastic and reconstructive procedures, and proof of principle by analysis of 1225 operations in 1166 patients. BMC Cancer. 2009;9:108. doi: 10.1186/1471-2407-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hai Y, Chong W, Lazar M A. Extended Prophylactic Antibiotics for Mastectomy with Immediate Breast Reconstruction: A Meta-analysis. Plast Reconstr Surg Glob Open. 2020;8:e2613. doi: 10.1097/GOX.0000000000002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamin F, Nouri A, McAuliffe P. Routine Postoperative Antibiotics After Tissue Expander Placement Postmastectomy Does Not Improve Outcome. Ann Plast Surg. 2021;87:S28–S30. doi: 10.1097/SAP.0000000000002826. [DOI] [PubMed] [Google Scholar]
- 19.iBAG Working Group . Masià J. The largest multicentre data collection on prepectoral breast reconstruction: The iBAG study. J Surg Oncol. 2020;122:848–860. doi: 10.1002/jso.26073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thill M, Faridi A, Meire A. Patient reported outcome and cosmetic evaluation following implant-based breast-reconstruction with a titanized polypropylene mesh (TiLOOP(R) Bra): A prospective clinical study in 269 patients. Eur J Surg Oncol. 2020;46:1484–1490. doi: 10.1016/j.ejso.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Saldanha I J, Cao W, Broyles J M.Breast Reconstruction After Mastectomy: A Systematic Review and Meta-Analysis [Internet] Rockville (MD)Agency for Healthcare Research and Quality (US)2021. Report No.: 21-EHC027 [PubMed] [Google Scholar]
- 22.Ganesh Kumar N, Berlin N L, Kim H M. Development of an evidence-based approach to the use of acellular dermal matrix in immediate expander-implant-based breast reconstruction. J Plast Reconstr Aesthet Surg. 2021;74:30–40. doi: 10.1016/j.bjps.2020.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Cabalag M S, Rostek M, Miller G S. Alloplastic adjuncts in breast reconstruction. Gland Surg. 2016;5:158–173. doi: 10.3978/j.issn.2227-684X.2015.06.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu X, Zhou L, Pan F. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: a cumulative meta-analysis. PLoS One. 2015;10:e0116071. doi: 10.1371/journal.pone.0116071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallberg H, Rafnsdottir S, Selvaggi G. Benefits and risks with acellular dermal matrix (ADM) and mesh support in immediate breast reconstruction: a systematic review and meta-analysis. J Plast Surg Hand Surg. 2018;52:130–147. doi: 10.1080/2000656X.2017.1419141. [DOI] [PubMed] [Google Scholar]
- 26.Samargandi O A, Joukhadar N, Al Youha S. Antibiotic Irrigation of Pocket for Implant-Based Breast Augmentation to Prevent Capsular Contracture: A Systematic Review. Plast Surg (Oakv) 2018;26:110–119. doi: 10.1177/2292550317747854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Y, Tian J, Liu J. Suppressive Effect of Leukotriene Antagonists on Capsular Contracture in Patients Who Underwent Breast Surgery with Prosthesis: A Meta-Analysis. Plast Reconstr Surg. 2020;145:901–911. doi: 10.1097/PRS.0000000000006629. [DOI] [PubMed] [Google Scholar]
- 28.Sood A, Xue E Y, Sangiovanni C. Breast Massage, Implant Displacement, and Prevention of Capsular Contracture After Breast Augmentation With Implants: A Review of the Literature. Eplasty. 2017;17:e41. [PMC free article] [PubMed] [Google Scholar]
- 29.Mammographie-Screening-Programm Geschäftsbericht 2021. 2022Accessed September 2, 2022 at:https://newsroom.mammo-programm.de/
- 30.Friedrich M, Kuhn T, Janni W. AGO Recommendations for the Surgical Therapy of the Axilla After Neoadjuvant Chemotherapy: 2021 Update. Geburtshilfe Frauenheilkd. 2021;81:1112–1120. doi: 10.1055/a-1499-8431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz G F, Guiliano A E, Veronesi U. Proceeding of the consensus conference of the role of sentinel lymph node biopsy in carcinoma or the breast April 19–22, 2001, Philadelphia, PA, USA. Breast J. 2002;8:124–138. doi: 10.1046/j.1524-4741.2002.08315.x. [DOI] [PubMed] [Google Scholar]
- 32.Lyman G H, Temin S, Edge S B. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32:1365–1383. doi: 10.1200/JCO.2013.54.1177. [DOI] [PubMed] [Google Scholar]
- 33.Elfgen C, Güth U, Gruber G. Breast-conserving surgery with intraoperative radiotherapy in recurrent breast cancer: the patientʼs perspective. Breast Cancer. 2020;27:1107–1113. doi: 10.1007/s12282-020-01114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rao R, Euhus D, Mayo H G. Axillary node interventions in breast cancer: a systematic review. JAMA. 2013;310:1385–1394. doi: 10.1001/jama.2013.277804. [DOI] [PubMed] [Google Scholar]
- 35.Gerber B, Stachs A, Veselinovic K. Patient reported outcomes (PROS) for the intergroup sentinel mammastudie INSEMA: Persistent impact of axillary surgery on arm and breast. San Antonio Breast Cancer Symposium 2021, 07-10122021
- 36.Brackstone M, Baldassarre F G, Perera F E. Management of the Axilla in Early-Stage Breast Cancer: Ontario Health (Cancer Care Ontario) and ASCO Guideline. J Clin Oncol. 2021;39:3056–3082. doi: 10.1200/JCO.21.00934. [DOI] [PubMed] [Google Scholar]
- 37.Moo T A, Jochelson M S, Zabor E C. Is Clinical Exam of the Axilla Sufficient to Select Node-Positive Patients Who Downstage After NAC for SLNB? A Comparison of the Accuracy of Clinical Exam Versus MRI. Ann Surg Oncol. 2019;26:4238–4243. doi: 10.1245/s10434-019-07867-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerber B, Schneeweiss A, Möbus V. Pathological Response in the Breast and Axillary Lymph Nodes after Neoadjuvant Systemic Treatment in Patients with Initially Node-Positive Breast Cancer Correlates with Disease Free Survival: An Exploratory Analysis of the GeparOcto Trial. Cancers (Basel) 2022;14:521. doi: 10.3390/cancers14030521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barron A U, Hoskin T L, Day C N. Association of Low Nodal Positivity Rate Among Patients With ERBB2-Positive or Triple-Negative Breast Cancer and Breast Pathologic Complete Response to Neoadjuvant Chemotherapy. JAMA Surg. 2018;153:1120–1126. doi: 10.1001/jamasurg.2018.2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tadros A B, Yang W T, Krishnamurthy S. Identification of Patients With Documented Pathologic Complete Response in the Breast After Neoadjuvant Chemotherapy for Omission of Axillary Surgery. JAMA Surg. 2017;152:665–670. doi: 10.1001/jamasurg.2017.0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heil J, Pfob A, Sinn H P. Diagnosing Pathologic Complete Response in the Breast After Neoadjuvant Systemic Treatment of Breast Cancer Patients by Minimal Invasive Biopsy: Oral Presentation at the San Antonio Breast Cancer Symposium on Friday, December 13, 2019, Program Number GS5-03. Ann Surg. 2022;275:576–581. doi: 10.1097/SLA.0000000000004246. [DOI] [PubMed] [Google Scholar]
- 42.Pfob A, Sidey-Gibbons C, Rauch G. Intelligent Vacuum-Assisted Biopsy to Identify Breast Cancer Patients With Pathologic Complete Response (ypT0 and ypN0) After Neoadjuvant Systemic Treatment for Omission of Breast and Axillary Surgery. J Clin Oncol. 2022;40:1903–1915. doi: 10.1200/jco.21.02439. [DOI] [PubMed] [Google Scholar]
- 43.The Axsana Study Group . Banys-Paluchowski M, Gasparri M L, de Boniface J. Surgical Management of the Axilla in Clinically Node-Positive Breast Cancer Patients Converting to Clinical Node Negativity through Neoadjuvant Chemotherapy: Current Status, Knowledge Gaps, and Rationale for the EUBREAST-03 AXSANA Study. Cancers (Basel) 2021;13:1565. doi: 10.3390/cancers13071565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwentner L, Helms G, Nekljudova V. Using ultrasound and palpation for predicting axillary lymph node status following neoadjuvant chemotherapy – Results from the multi-center SENTINA trial. Breast. 2017;31:202–207. doi: 10.1016/j.breast.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 45.Banys-Paluchowski M, Gruber I V, Hartkopf A. Axillary ultrasound for prediction of response to neoadjuvant therapy in the context of surgical strategies to axillary dissection in primary breast cancer: a systematic review of the current literature. Arch Gynecol Obstet. 2020;301:341–353. doi: 10.1007/s00404-019-05428-x. [DOI] [PubMed] [Google Scholar]
- 46.Kirkilesis G, Constantinidou A, Kontos M. False Negativity of Targeted Axillary Dissection in Breast Cancer. Breast Care (Basel) 2021;16:532–538. doi: 10.1159/000513037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barrio A V, Montagna G, Mamtani A. Nodal Recurrence in Patients With Node-Positive Breast Cancer Treated With Sentinel Node Biopsy Alone After Neoadjuvant Chemotherapy-A Rare Event. JAMA Oncol. 2021;7:1851–1855. doi: 10.1001/jamaoncol.2021.4394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Caudle A S, Yang W T, Krishnamurthy S. Improved Axillary Evaluation Following Neoadjuvant Therapy for Patients With Node-Positive Breast Cancer Using Selective Evaluation of Clipped Nodes: Implementation of Targeted Axillary Dissection. J Clin Oncol. 2016;34:1072–1078. doi: 10.1200/JCO.2015.64.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]