Abstract
Purpose
Analyzing parents’ and physicians’ opinions regarding phone-based encounters in emergency shifts of a French pediatric epilepsy center compared to traditional face-to-face encounters during the first lockdown of the COVID-19 pandemic
Methods
Prospective monocentric study on remote encounters at Necker rare epilepsy reference center from March 20th, 2020 to April 23rd, 2020 due to lockdown measures. This study was conducted with a survey based on 5-point Likert scales (LS-2/2) designed for both parents and physicians. We compared first versus follow-up encounters as well as physicians’ and parents’ opinions.
Results
We had a total of 224 responses, among which 204 were completed by physicians (91%) and 173 (84,4%) by parents. Twenty five were first encounters (14,2%). Physicians pointed out the need for clinical examination (42.6%), mainly for first encounters (p=0.0004). Physicians rated the quality of communication lower (p=0.003) as their capacity to answer parents’ questions (p=0.004). They were significantly less satisfied with remote encounters compared to parents (p<10−4). We identified six urgent (2.9%) and 50 semi-urgent (24%) situations requiring programming face-to-face encounter during or shortly after the lockdown.
Conclusion
Remote encounters could be a helpful practice for pediatric patients with epilepsy in emergency situations such as pandemics. It allowed the identification and prioritization of emergency situations. Physicians were less positive than parents. We raised the possible use of remote encounters in association to face-to-face encounters for routine follow-up of pediatric patients with epilepsy.
Keywords: Telemedicine, EEG, Virtual care, Telehealth, Child neurology, Follow-up
1. Introduction
The COVID-19 pandemic turned the world upside down in a matter of weeks [1,2]. Health care facilities were overwhelmed and had to urgently adjust inpatient and outpatient care management, in order to follow governments’ guidelines [3]. The lack of national health planning for such an unprecedented crisis compelled medical providers to act rapidly, following experience and current availability of means and methods, in order to offer the best possible assistance to patients [4]. In these circumstances, individuals with chronic diseases were deprioritized and many of their encounters had to be postponed [5].
In 2003, a survey conducted in China during the severe acute respiratory syndrome (SARS) epidemic showed that the restricted access to medical care led to an important withdrawal in anti-seizures medications (ASM) for patients with epilepsy, resulting in increased seizure frequency [6]. The lockdown policy related to the coronavirus pandemic 2019 (COVID-19) resulted in a similar impact for individuals with epilepsy [7], [8], [9]. In addition, lockdown was associated with an increase of anxiety, depression and isolation in patients [7,10,11].
On 17th March 2020, the French government declared a lockdown in Paris, restricting the access to Health structures, prioritizing emergencies and COVID-19 patients. Necker's reference center for rare epilepsies decided to maintain all its scheduled outpatients’ encounters transforming them into phone-based remote encounters. Our goal was to maintain the best follow-up for patients and families and to detect situations needing urgent interventions despite the lockdown measures.
The aim of this study was to evaluate and compare the opinions of physicians and families regarding remote encounters and to explore the possible contribution of such encounters beyond the health crisis, in routine practice of a tertiary pediatric epilepsy center.
2. Methods
2.1. Study design and participants
The reference center for rare epilepsies of the pediatric neurology department at Necker Hospital decided to maintain all scheduled outpatient epilepsy medical encounters from March 20th, transforming them into remote encounters. To facilitate the shift from face-to-face to remote encounters, a coordinated action was undertaken to inform the families through three channels: phone and email messages, website notifications (health institution and center websites) and information added to the emails’ signature of all medical and administrative members of the reference center team. All families received an email or phone call at least 48 hours prior to their encounter's scheduled date to confirm that their appointment is maintained at the same time slot and its conversion to a remote mode. Additional explanation was provided by voice mail as well as a link to our website (CReER, maladies rares, Necker Enfants Malades) with detailed explanation on the remote encounter and its modalities.
To evaluate this abrupt shift in our practice, we conducted a monocentric prospective survey from March 20th, 2020 to April 23rd, 2020 exploring the opinion of physicians and families on remote encounters during this period. The surveys were developed by the coordinator of the reference centre for rare epilepsies at Necker (RN) and the coordination nurse (TT). Four other physicians of the team with over five years of experience reviewed the surveys and suggested some modifications. The final version was obtained after a pre-test on a small population of families and physicians. At the end of each remote encounter, the physicians answered a 19-item electronic questionnaire on the quality of the encounter and their satisfaction, comparing it to their previous experience in face-to-face encounters (Appendix A). A similar questionnaire (Appendix B) was sent electronically to the parents, followed by a reminder 15 days later if the questionnaire remained unanswered. A consent form was included at the beginning of the questionnaire explaining the aim of the study. A signed consent was mandatory to access the survey. The answers were mainly based on 5-point Likert scale (LS-2/2: strongly agree: 2, agree: 1, neutral: 0, disagree: -1; strongly disagree: -2).
2.2. Statistical analysis
Descriptive statistics were expressed as median [interquartile], due to the lack of normality of the different variables. To compare the first and follow-up encounters from the physicians' point of view we used a logistic regression analysis. First, we performed one-factor logistic regressions (χ2 tests for categorical variables and one-factor logistic regressions otherwise), then we included the significant factors (p<0.1) in a multivariate analysis. The dependent variable was the status of the remote encounters (first versus follow-up) and the independent variables were their impressions, coded by the Likert scales, on the similarities between remote and face-to-face encounters in terms of duration and conduct, the need for clinical examination, the ability to answer all parents’ questions, the description of patients’ symptoms by parents, the communication quality, their overall satisfaction and the need of an urgent or semi-urgent face-to-face encounter. A similar approach was used to compare the opinion of first time consulting and regularly followed families. Next, we compared the opinion of physicians and families for the same remote encounter (Wilcoxon signed-rank test).
This study was approved by the ethics committee of our institution (Necker Hospital, APHP). Parents were asked to confirm their consent at the beginning of the survey (see supplementary table 2). For statistical analysis, p-value<0.05 was considered as significant, and p-value<0.1 as a tendency. We assumed that Likert scale provides linear ordinal data. The statistical analyses were performed using R software [12].
3. Results
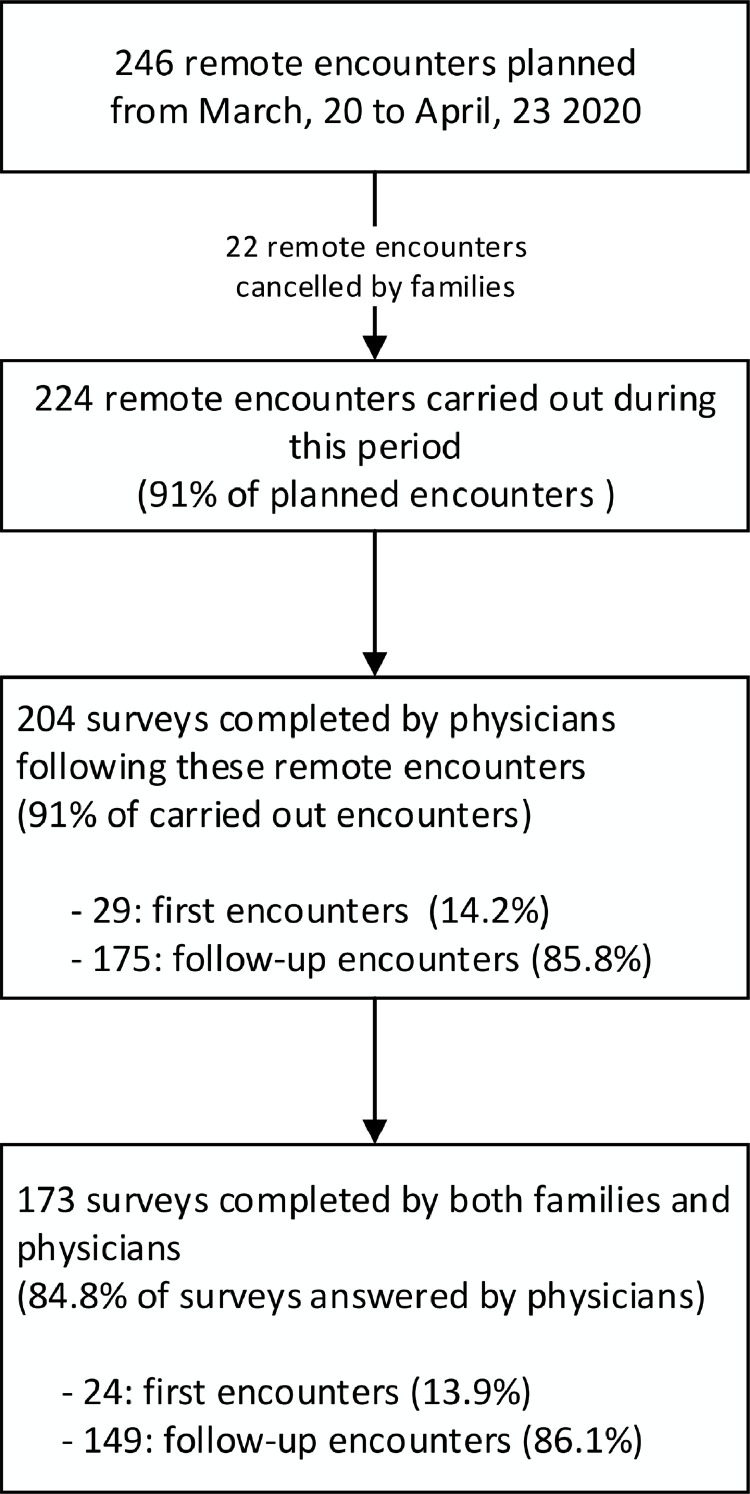
During the first month lockdown period, 246 remote encounters were planned and 224 remote encounters, corresponding to 224 individuals, took place (22 cancelled by families, Figure 1 ). Physicians responded to 204 questionnaires (91.1% of the 224 remote encounters). Twenty-nine individuals had their first encounter (14.2%) while the remote encounter was part of the routine follow-up of the remaining 175 (85.8%). The median patients’ age was 8.7 [4.5-12.8] years. The epilepsy type or syndromes were as follow: developmental and epileptic encephalopathies (n=51, 25%), focal epilepsies (n=34, 16.7%), generalized (genetic) idiopathic epilepsies (n=27, 13.2%), myoclonic atonic epilepsy (n=14, 6.9%), tuberous sclerosis (n=12, 5.9%), complex febrile seizures (n=12, 5.9%), self-limited epilepsies (n=11, 5.4%), Sturge-Weber syndrome (n=11, 5.4%) and Febrile infection-related epilepsy syndrome (n=1, 0.5%). Epilepsy type was unclassified in 15.2% cases (n=31).
Fig. 1.
Flow diagram for study participants.
Of the 204 questionnaires filled by the physicians, 84.8% were also filled by the families (n=173, including 24 individuals having their first encounter in our center). The questionnaires were filled at 100% due to the restrictions imposed by the electronic software.
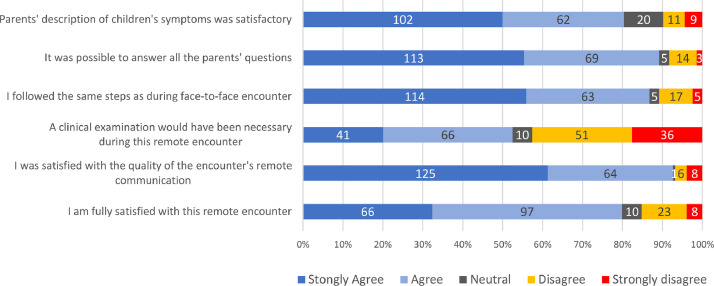
3.1. Physicians’ perspective (Fig. 2)
Fig. 2.
Physicians' impression on their remote encounters, with comparisons to their usual face-to-face encounters.
Physicians rated the quality of communication as satisfactory in 93.1% of the encounters (n=200, strongly agree: 125, agree: 65). They were satisfied with the parents' description of their children's symptoms (n=164, 80.4%) and were able to answer all parents’ questions (n=182, 89.2%). The conduct of remote encounters was similar to that of the face-to-face encounters (n=177, 86.7%). The main concern expressed by physicians was the lack of clinical examination. Indeed, they stated that it did not impact the encounter in 107 individuals (51.4%) but was judged as necessary in 87 individuals (42.6%) including all first encounters. The duration of the remote encounters was estimated similar to that of the face-to-face encounters, except in 34 cases (16.6%, really longer, n=17 and 16, 6% really shorter, n=17).
In fifty individuals with an EEG programmed prior to the encounter (24.5% of the 204 remote encounters), 38 (76%) had their EEG canceled due to lockdown. In addition to EEGs cancellation, remote encounters had an impact on the management of antiseizure medicine (ASM). Withdrawal of ASM was postponed in 11 patients and introduction of ASM in 9 others. Announcement of genetic results has been postponed in all three cases and pre-surgical evaluation of epilepsies in eight. To our knowledge, none of the other patients was addressed to emergencies for unstable epilepsy and only one family had some difficulty obtaining their ASM.
Physicians were satisfied in 79.9% (n=163) including very satisfied in 47.5% (n=97) and satisfied in 32.3%, (n=66). Only 6 patients (2.9%) required an urgent face-to-face evaluation after remote encounter. Fifty appointments had to be planned in face-to-face encounter just after the lockdown period (24.5%) for relatively urgent issues. For the others (n=148, 72.5%), remote encounter was considered as equivalent to face-to-face encounter. Interestingly, physicians considered that the next encounter could be remote in 19.6% of cases (29/148).
Comparing first and follow-up encounters, physicians reported less similarity with face to face encounters for the first group (LS-2/2: 1[0;2] versus the second 2[1;2], p=0.02) and longer duration of the first encounter (LS-2/2: 0[-1;1.5] versus 0[-1;0], p=0.03) . Moreover, the need of clinical examination was noted as more important in first versus follow-up encounters (LS-2/2: 1[1;2] versus -1[-1;1], p=0.0004) and physicians were less able to answer all parents’ questions (LS-2/2: 1[0.5;2] versus 2[1;2], p=0.008). The communication quality was evaluated as lower (LS-2/2: 1 [1;2] versus 2[1;2], p=0.039). However, the description of patients’ symptoms by the family, the evaluation of the urgent need of face-to-face encounter and the overall satisfaction were not significantly different. Multivariate logistic model confirmed the significant higher need of clinical examination in first compared to follow-up encounters (p=0.002).
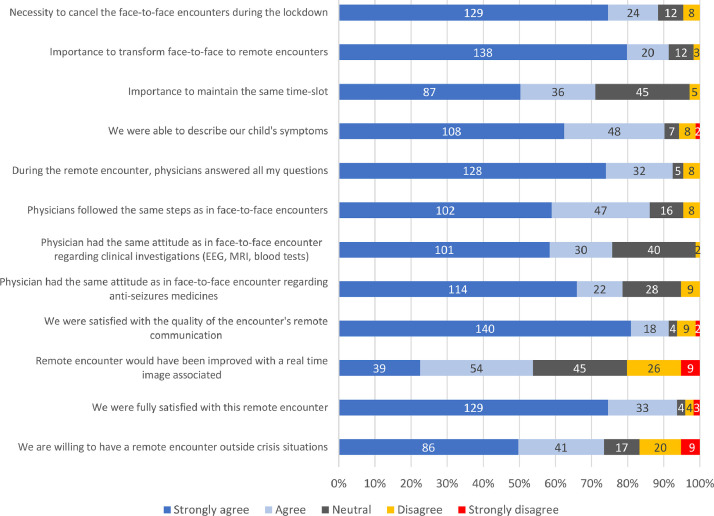
3.2. Parents’ perspective (Fig.3)
Fig. 3.
Parents' impression on their remote encounters, with comparisons to their usual face-to-face encounters.
The majority of the families, 90.2% (n=156 out of 173 responses), were satisfied with the information they received for the change of the encounter from face-to-face to remote. One hundred fifty-three parents agreed that face-to-face encounters should be cancelled due to COVID-19 pandemic (88.4%) while 8 disagreed (4.7%). One hundred fifty-eight parents (91.3%) agreed to replace face-to-face encounter by remote encounters preserving the same timeslot (n=123, 71.1%). The vast majority (n=158, 91.3%) evaluated as satisfactory (n=18, 10.4%) and very satisfactory (n=140, 80.9%) the quality of the communication during the encounters. A simultaneous real-time image would have been appreciated by 93 of cases (53.8%) versus not appreciated by 35 (20.2%) and 45 (26%) remained neutral on the subject. Parents reported that describing their children's symptoms was simple (n=156, 90.2%) and that physicians answered all their questions (n=160, 92.5%). Remote encounter followed the same steps as the face-to-face encounters (n=149, 86.1%) with a similar estimated duration (n=155, 89.6%). They considered physicians’ attitudes regarding prescription of ASM (n=136, 78.6%) and clinical investigations, namely EEG and blood tests (n=131, 75.7%), similar in remote compared to face-to-face encounters. Overall, 93.6% (n=162) of parents were satisfied from the remote encounters, 74.5% (n=129) rated them as very satisfactory and 19.1% (n=33) as satisfactory. Finally, 73.4% of the parents agreed to continue remote encounters outside crisis situations (n=127).
Twenty nine families had a first appointment with our team during this period and 19 had already consulted a pediatric neurology previously in another institution and were referred for a second or third opinion. Quality of communication, necessity to replace face-to-face by remote encounters, organization of remote encounters, physicians’ capacity to answer their questions, their ability to describe their children's symptoms, overall satisfaction, duration of the remote encounter, interest of real-time image and possible future use of remote encounters outside the crisis situation showed no significant difference between this group and those who had follow-up encounters.
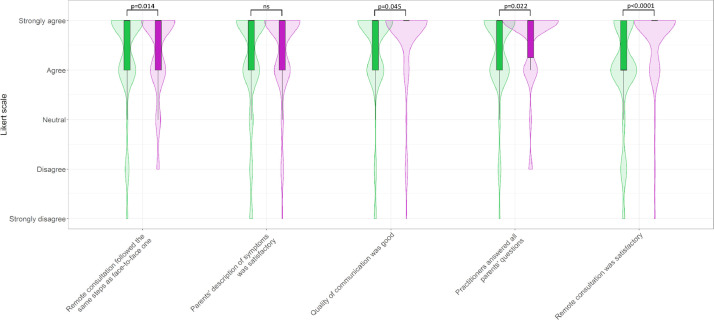
3.3. Comparison of points of view between physicians and families (Fig. 4)
Fig. 4.
Comparisons of physicians’ and families’ point of views about their remote encounters.
Physicians rated the communication quality during remote encounters significantly lower than parents (2[1;2] versus 2[2;2], p=0.045). Although physicians considered that the remote encounters followed almost the same steps as face-to-face, their scores were significantly lower than the families (2[1;2] versus 2[1;2] for parents, p=0.014). They also rated significantly lower their capacity to answer parents’ questions (2[1;2] versus 2[1.25;2] for parents, p=0.022). Their evaluation of the families’ ability to describe their children’ symptoms was not significantly different from that of the parents. Finally, physicians were overall less satisfied by the remote encounters than parents (1[1;2] versus 2[2;2], p<10−4).
4. Discussion
This study is the first, to our knowledge, to compare the experience of physicians and families regarding remote encounters. Parents were fully aware of the need to replace face-to-face by remote encounters due to COVID-19 pandemic. The strategy we developed to face this lockdown using the website of the institution, personal emails and phones messages with a link added to the signature of all the members of our team showed to be efficient. This acute shift was satisfactory and only 8.9% of families cancelled their encounter during this first month of lockdown, thus avoiding patients being "lost in lockdown". We were able to identify the six patients who needed an urgent face-to-face evaluation. To our knowledge, none of the other patients was addressed to emergencies and only one family had some difficulty obtaining their ASM.
Facing the COVID-19 pandemic, use of remote systems for clinical practice increased significantly all over the world [8,[13], [14], [15]]. The overall satisfaction of physicians and families concerning remote encounters were in line with studies conducted in countries with national policies of lockdown [9,16,17]. This transition was important in order to address the risk of increased frequency of seizures, depression, anxiety, and ASM withdrawal [7,10,11]. Similarly, difficulties in accessing health care or treatment would exacerbate this situation. A self-administered survey conducted in US, identified that 72.7% of people with epilepsy had much more difficulties in obtaining ASM and 42.5% in reaching healthcare providers [10].
Conserving on the other hand the same time slots allowed the epilepsy team to participate to activities dedicated to COVID-19 out of their usual clinics slots and to keep on an organized agenda for the whole department. In our study, both physicians and families agreed that the conduct of remote encounters was similar to the face-to-face encounters. Encounters were carried out through telephone call, and almost half of the parents did not feel that adding a video link would have improved the consultation. Phone calls were first used due to an overwhelmed internet system that aimed to increase the availability of telemedicine settings for all. Adding video to the encounter and being able to see the child and facial expressions of the families would be helpful in our opinion. Indeed, we are currently promoting the use of institutional telemedicine system with video for all remote encounters and contact with the families and patients. Parents felt that they were able to accurately describe their child's symptoms and to ask all their questions which were satisfactorily answered. Patients were also satisfied with physicians’ attitude concerning ASM prescriptions and follow-up instructions regarding the requests of EEG and blood tests. A large majority of parents agreed to pursue remote clinics outside crisis situations (73 %), a rate similar to the 72.2% in a study concerning ketogenic diet in children with epilepsy using telemedicine during COVID-19 [18]. However, this transformation of face-to-face clinics into remote ones is not suitable for all situations. Indeed, it is difficult to adapt for people with cognitive disorders or who have visual and/or hearing impairments without the support of a third party [19,20].
Before COVID-19 pandemic, remote clinics were used worldwide particularly in isolated regions in Canada or in low income countries [21], [22], [23], [24]. Tertiary specialized centers in Canada are located in major cities whereas the population is dispersed all over the country. Satellite medical centers are organized with videoconference facilities for remote consultations with the presence of local physicians helping the experts connected to the system. Such remote encounters showed a significant decrease in travel time and costs for the families [21]. Indeed, in our reference center, 50% of patients need to reach our center a mean of 2 hours. This might partly explain why families tended to be more satisfied with remote consultations. We can assume that physicians have a less impact of time saving and that the impossibility to perform clinical examination, a key time of the medical evaluation and a medico-legal issue, made them less enthusiastic about this shift to remote encounters. In addition, although the conduct of remote encounters was quite similar to face-to-face clinics, physicians’ attitude changed in relation to ASM. For instance, in some cases they postponed introduction or withdrawal of ASM. Physicians intended to avoid possible consequences that would necessitate an emergency room referal while medical emergency teams were dedicated mostly to COVID-19 patients. That was also the main reason why more than 60% of the 66 epileptologists changed anti-seizures treatments less frequently in Spain [16]. Unlike the international study on the management of children with epilepsy during COVID-19 pandemic [8], we did not "dramatically" modify our clinical management, probably due to our rapid and organized shift and to the partial preservation of pediatric settings for emergencies not related to COVID-19. Indeed, we were able to identify emergencies and hospitalize patients such as, for instance, for onset of infantile spasms [8].
EEG performance practice changed because of remote encounters. Only 24% of EEGs planed before remote encounters were carried out. Another worldwide study showed that 90.6 % of pediatric neurologists report a significantly reduced access to EEG during the CoVid-19 pandemic [8]. During remote encounters, physicians had to rely on seizure semiology or on videos provided by families. The strict use of families’ description of seizures without EEGs reinstated seizure semiology as a reliable indicator that should be used by physicians in countries with limited resources to classify seizure and epilepsy types [25]. Some syndromes such as childhood absence epilepsy can be efficiently identified and can allow initiation of ASM therapy [26]. Most difficulties arose with first encounters, physicians stated that they would have needed a physical examination and were less comfortable answering the parents’ questions. Patients referred to our centre are often seeking a second or third opinion, therefore they had already at least one consultation with a clinical examination by a pediatric neurologist. They present often with complex epilepsies and first encounter at our centre aims to answer questions concerning diagnosis, prognosis, treatment, and novelties in clinical trials. Although such discussion might be more difficult to have through a remote first encounter, we decided not to postpone this first encounter in order to detect urgent situations and to avoid “lost in pandemic” patients and families. This decision to maintain the first encounter and to do it remotely was not shared by many Spanish adults neurologists who decided to postpone up to 38% first encounters during the outbreak [16].
The present study has some limitations. It is a single-center study in a reference epilepsy center treating mostly complex cases referred with families travelling long distances to reach our centre. The sample size is small, but the results were significant and can help better understand the use of remote encounters. Other studies conducted over the same lockdown period that explored the impact of COVID-19 pandemic in patients with epilepsy did not recruit larger numbers although multicentric [9,11,17]. It is also important to keep in mind that the small number of practitioners partaking in the study could add a selection bias. Furthermore, our aim was to obtain a timely picture of the urgent shift during the first month of lockdown and before physicians and families had gotten used to these remote encounters. In addition, this pilot study focused on remote encounters shift and urgent situations during the study length but did not consider a longer-term perspective on epilepsy course. Our goal was to understand how our strategy could be successful while facing such an emergency and explore the opinion of physicians and families. Finally, we cannot exclude that due to the stressful context linked to lockdown, the families were ready to openly embrace any alternative solutions. This might have contributed to an over-enthusiastic evaluation of the remote encounters.
5. Conclusion
Our study showed that remote encounters could be a viable alternative to face-to-face encounters in urgent situation such as pandemics. Physicians were less positive than families but both had a positive opinion on remote encounters. This study allowed an objective and concerted evaluation of all the patients that should have attended our outpatient clinics. We were able to identify emergency situations and prioritize the access of patients to face to face clinics or other in hospital facilities. This approach seems less suitable for first encounters, especially when a face-to-face clinic is available. In conclusion, remote encounters worth an evaluation outside urgent situations as pandemic in order to confirm the benefit of its use in association with face-to-face encounters for follow-up of patients with epilepsy. We believe that remote encounters are particularly suitable for chronically monitored patients who are already well known and have relatively stable epilepsy.
Disclosures and funding
The authors have stated that they had no interests which might be perceived as posing a conflict or bias. RN was supported by State funding from the Agence Nationale de la Recherche under “Investissements d'avenir” program (ANR-10-IAHU-01) and the “Fondation Bettencourt Schueller”.
Data statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Acknowledgement
The authors thank the families and the physicians that participated in this study. They also thank Nawras Georgi for his technical support.
References
- 1.Gates B. Responding to Covid-19 - a once-in-a-century pandemic? N Engl J Med. 2020;382:1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA - J Am Med Assoc. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Janssen M, van der Voort H. Agile and adaptive governance in crisis response: lessons from the COVID-19 pandemic. Int J Inf Manage. 2020;55 doi: 10.1016/j.ijinfomgt.2020.102180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: a Call to Action. JMIR Public Heal Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu N, Huang R, Baldacchino T, Sud A, Sud K, Khadra M, et al. Telehealth for noncritical patients with chronic diseases during the COVID-19 pandemic. J Med Internet Res. 2020;22:e19493. doi: 10.2196/19493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai SL, Hsu MT, Chen SS. The impact of SARS on epilepsy: The experience of drug withdrawal in epileptic patients. Seizure. 2005;14:557–561. doi: 10.1016/j.seizure.2005.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang S, Wu C, Jia Y, Li G, Zhu Z, Lu K, et al. COVID-19 outbreak: the impact of stress on seizures in patients with epilepsy. Epilepsia. 2020;00:1–10. doi: 10.1111/epi.16635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wirrell EC, Grinspan ZM, Knupp KG, Jiang Y, Hammeed B, Mytinger JR, et al. Care Delivery for Children With Epilepsy During the COVID-19 Pandemic: an international survey of clinicians. J Child Neurol. 2020;2020:924–933. doi: 10.1177/0883073820940189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fonseca E, Quintana M, Lallana S, Restrepo JL, Abraira L, Santamarina E, et al. Epilepsy in time of COVID-19. a survey-based study. Acta Neurol Scand. 2020:0–3. doi: 10.1111/ane.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller WR, Von Gaudecker J, Tanner A, Buelow JM. Epilepsy self-management during a pandemic: experiences of people with epilepsy. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Hees S, Siewe Fodjo JN, Wijtvliet V, Van den Bergh R, Faria de Moura Villela E, da Silva CF, et al. Access to healthcare and prevalence of anxiety and depression in persons with epilepsy during the COVID-19 pandemic: a multicountry online survey. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.3.5.1. RDCT . Vol. 2. R Found Stat Comput; 2018. (A Language and Environment for Statistical Computing). https://www.R-project.orghttp://www.r-project.org (accessed May 22, 2020) [Google Scholar]
- 13.Kuchenbuch M, D'Onofrio G, Wirrell E, Jiang Y, Dupont S, Grinspan ZM, et al. An accelerated shift in the use of remote systems in epilepsy due to the COVID-19 pandemic. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chudasama Y.V., Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr Clin Res Rev. 2020;14:965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27:1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conde-Blanco E, Centeno M, Tio E, Muriana D, García-Peñas JJ, Serrano P, et al. Emergency implementation of telemedicine for epilepsy in Spain: results of a survey during SARS-CoV-2 pandemic. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Panda PPK, Dawman L, Panda PPK, Sharawat IK. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Semprino M, Fasulo L, Fortini S, Martorell Molina CI, González L, Ramos PA, et al. Telemedicine, drug-resistant epilepsy, and ketogenic dietary therapies: a patient survey of a pediatric remote-care program during the COVID-19 pandemic. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloem BR, Dorsey ER, Okun MS. The coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurol. 2020;77:927–928. doi: 10.1001/jamaneurol.2020.1452. [DOI] [PubMed] [Google Scholar]
- 20.Kuroda N. Decision Making on Telemedicine for Patients With Epilepsy During the Coronavirus Disease 2019 (COVID-19) Crisis. Front Neurol. 2020;11:1–4. doi: 10.3389/fneur.2020.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed SN, Mann C, Sinclair DB, Heino A, Iskiw B, Quigley D, et al. Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient's perspective. Epilepsia. 2008;49:573–585. doi: 10.1111/j.1528-1167.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 22.Sarfo FS, Adamu S, Awuah D, Ovbiagele B. Tele-neurology in sub-Saharan Africa: a systematic review of the literature. J Neurol Sci. 2017;380:196–199. doi: 10.1016/j.jns.2017.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fortini S, Espeche A, Caraballo R. 2020. Telemedicine and epilepsy: A patient satisfaction survey of a pediatric remote care program. [DOI] [PubMed] [Google Scholar]
- 24.Rasmusson KA, Hartshorn JC. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia. 2005;46:767–770. doi: 10.1111/j.1528-1167.2005.44804.x. [DOI] [PubMed] [Google Scholar]
- 25.Kumar S, Singh MB, Shukla G, Vishnubhatla S, Srivastava MVP, Goyal V, et al. Effective clinical classification of chronic epilepsy into focal and generalized: a cross sectional study. Seizure. 2017;53:81–85. doi: 10.1016/j.seizure.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Stafstrom CE, Sun LR, Kossoff EH, Dabrowski AK, Singhi S, Kelley SA. Diagnosing and managing childhood absence epilepsy by telemedicine. Epilepsy Behav. 2020 doi: 10.1016/j.yebeh.2020.107404. [DOI] [PubMed] [Google Scholar]