Abstract
Background and Objective
Cannabidiol, one of the main components of the Cannabis sativa plant, is a non-psychotropic cannabinoid that has recently drawn the attention of researchers and clinicians for its potential therapeutic applications. In this systematic review, we aim to describe the possible effects of cannabidiol in appetite and body weight.
Methods
Both authors independently ran a thorough search in both PubMed and Cochrane databases up to 31 July, 2022 and included every peer-reviewed, original randomized controlled clinical trial that reported data on either of the said outcomes. Risk of assessment bias was performed with Cochrane’s risk of bias tool and results were summarized in tables.
Results
A total of 11 trials were included in this review. Of these, the majority reported on cannabidiol reducing appetite and/or body weight whilst some have found no significant changes and one trial described an increase in appetite.
Conclusions
This systematic review suggests that cannabidiol has an anorexigenic effect, correlated with a decrease in body weight. However, most of the studies included in the present review raised some concerns in terms of risk of bias. We believe further research is needed in order to clarify potential mechanisms involved in the effect of cannabidiol on feeding/appetite.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40261-022-01205-y.
Key Points
| Cannabidiol reduces the appetite and/or body weight or body mass index in most of the clinical trials. |
| Most of the studies included in the present review raised some concerns in terms of risk of bias. |
Introduction
In recent decades, the endocannabinoid system (which includes cannabinoid receptors, endocannabinoids, and the enzymes responsible for their biosynthesis and degradation) has attracted considerable interest because of its involvement in several physiological processes such as energy balance, appetite stimulation, blood pressure, pain modulation, embryogenesis, nausea and vomiting control, memory, learning, and immune response and as a potential therapeutic target in numerous pathological conditions including neurological diseases such as Parkinson’s and Alzheimer’s disease and multiple sclerosis, as well as anorexia and irritable bowel syndrome [1–3].
Cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) are two of the major phytocannabinoids present in the Cannabis sativa plant. While both have become a major staple in cannabinoid research, according to the World Health Organization, CBD lacks the latter’s psychoactive and abuse potential [4]. In addition, its favorable safety and tolerability profile makes it a prime candidate for use in the clinical setting. Indeed, this cannabinoid presents mild and infrequent side effects, mainly sleepiness and diarrhea [5, 6].
Differently from Δ9-THC, CBD is a weak agonist of cannabinoid receptor type 1 (CB1) and an antagonist of cannabinoid receptor type 2 (CB2), while also taking part in other signaling pathways involving the serotonin 1A receptor, G protein-coupled receptors 55 and 18, and the transient receptor potential cation channel subfamily V member 1 receptors, among others [7]. The wide array of effects and multiple clinical applications of CBD explains the increasing interest of the scientific community in this substance—there are currently more than 170 ongoing clinical trials investigating this cannabinoid, its therapeutic potential and interactions. In fact, this alkaloid compound has garnered attention for its anti-inflammatory, anti-oxidant [8], analgesic [9], and anticonvulsant [10] effects.
Despite all the interest in this compound, Epidiolex® remains the only CBD medicine approved by the US Food and Drug Administration, an oral solution indicated for use in Lennox–Gastaut and Dravet syndrome, two rare forms of epilepsy, and tuberous sclerosis complex. In the European Union and Canada, Sativex®, an oromucosal spray consisting of both CBD and Δ9-THC, was the first CBD-containing drug approved. It is currently used for controlling spasticity in patients with multiple sclerosis. Epidyolex® was approved by the European Medicines Agency in 2019.
However, CBD is also available to the general population. Indeed, the ambiguous legal status of CBD has allowed its presence in over-the-counter preparations (labeled as health or food supplements) that have not been evaluated in clinical trials and are readily available at hemp shops. These preparations not only possess varying doses of CBD (range 5–20 mg) but also usually contain other cannabinoids. Being a new and poorly regulated market, these products often contain a much lower or higher dose of the substance and may be mislabeled [11]. Despite the heterogeneity in accessibility to these preparations worldwide, this blossoming industry is expected to grow in the future, as the distinction between the use of CBD as a medicine and as an over-the-counter supplement is increasingly less clear [12]. Because of the expected growth in this market, and with more CBD-rich medicines expected to be approved in the future, the number of individuals exposed to this substance is anticipated to increase steadily.
In relation to eating behavior, emerging evidence points to an important role of cannabinoids in regulating appetite, and consequently food intake. Additionally, cannabinoids are also an important player in the reward circuitries [13–16]. Thus, we found it timely to conduct a review in order to better clarify the potential impact of CBD on appetite and body weight in humans. Indeed, in the context of CBD human use, it is relevant that the literature is lacking information on how it may affect appetite and anthropometric parameters such as body weight, not only per se but also as a result of potential interactions with other drugs. Not only this has a huge pharmacodynamic interest, but it can also lead researchers to investigate new therapeutic avenues for this cannabinoid, mainly regarding the treatment of diabetes mellitus, obesity, and other metabolic disorders. In this systematic review, we aim to gather and summarize the available body of evidence relating to the effects of CBD on appetite and body weight changes in order to fill this gap in the literature.
Methods
This systematic review was structured in accordance with the 2020 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [17].
Search Strategy
The present review included all the relevant literature obtained through a search in the PubMed and Cochrane databases from inception up to 31 July, 2022. The search term ‘cannabidiol’ was combined with the terms ‘weight’ or ‘appetite,’ using the query “cannabidiol AND (weight OR appetite)” in both the PubMed and the Cochrane Library databases. In the latter case, only results under the tab ‘trials’ were retrieved. This search was conducted by two independent investigators, JP and FM, who comprehensively evaluated studies for eligibility according to the inclusion and exclusion criteria detailed below.
Inclusion/Exclusion Criteria
In order to evaluate the effects of CBD on body weight and appetite, we included every peer-reviewed, original randomized placebo-controlled trial of CBD in humans that reported data on either of the outcomes (either specifically or as adverse events, in a safety analysis). Articles that failed to specify the dose of CBD or used structural isomers, chemical analogs, or derivates of CBD as their intervention were excluded. When CBD was administered together with other cannabinoids (such as Δ9-THC), the study was only included if the ratio of CBD to other cannabinoids favored CBD. No restrictions were applied in relation to participant characteristics or disease.
Data Acquisition and Analysis
After being screened for eligibility, the papers were then evaluated by full-text screening. Again, two investigators (JP and FM) independently extracted data agreed upon beforehand: type of study, population and number of participants, type of intervention and dosage, time of exposure to the intervention and relevant outcomes (appetite and body weight changes), as well as author details (name and year of publication). These results were retrieved, analyzed, and summarized in a table and posteriorly cross-checked by both authors. Any discrepancies among the investigators were resolved through consensus. Risk of bias of the randomized controlled trials was evaluated using the 2019 Cochrane Collaboration’s tool for assessing risk of bias 2 and the 2021 Cochrane Collaboration’s tool for crossover trials (risk of bias 2 for crossover trials) [17].
Results
Selection of Articles and Characteristics
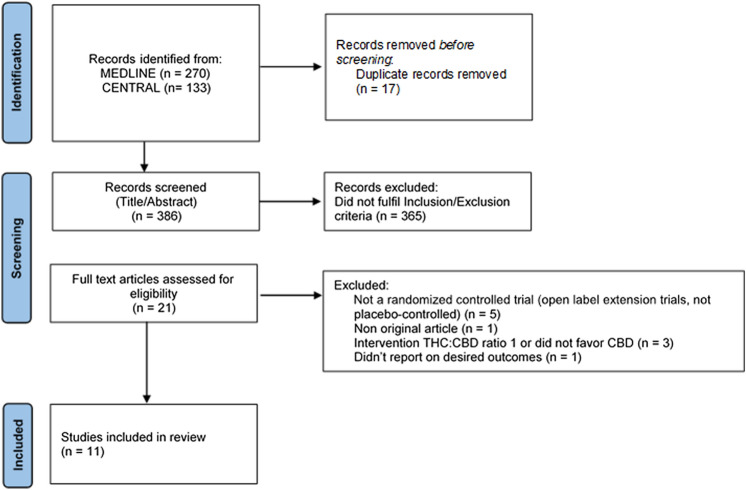
The initial search though PubMed and Cochrane databases yielded, respectively, 270 and 133 results, which were assessed via title and abstract (if available) or other basic information. After this initial screening, 17 duplicate records were identified and removed and another 365 were excluded for failing to meet the predetermined inclusion and exclusion criteria. This includes one article that was in Hebrew and our attempt to contact the authors in order to provide us a copy in English was unsuccessful. The full text of the remaining 21 articles was then retrieved and analyzed. Ultimately, 11 randomized controlled trials were included and ten articles were excluded because five followed another study design (open-label extension trials) or were not placebo controlled, one was not an original article, three used a cannabinoid formulation with both CBD and Δ9-THC at equal concentrations or a higher concentration of the latter, and one failed to report on appetite or body weight changes. The flowchart on Fig. 1 represents the progressive study selection stages. A description of each study is summarized in Table 1.
Fig. 1.
Flowchart of study retrieval and selection. CBD cannabidiol, THC tetrahydrocannabinol
Table 1.
Characteristics of included studies
| Study | Clinical population | Total number of participants | Age (years) | CBD dose and scheme | Type of CBD | Formulation/route | Duration of treatment | Metabolic effects |
|---|---|---|---|---|---|---|---|---|
| De Bruijn et al. [18] | Healthy male subjects | 10 | Mean: 23.4 ± 1 | An initial (25 mg) and a top-up dose (10 mg), 35 minutes later |
Dried, milled, and homogenized flowers of a variety of the plant Cannabis sativa (Office of Medical Cannabis; the Netherlands), variety Bedrolite (<1% Δ9-THC, 9% CBD) |
Inhalation (MINIVAP vaporizer) |
No change in food preference No change in hunger No change in ad libitum intake of a sweet food No change in sweet taste intensity perception Decrease in desire to eat Increase in fullness rating |
|
| Hundal et al. [19] | Male and female subjects with non-clinical high paranoia | 32 | 18–50, mean: 25–26 | 600 mg | Provided by GW Pharmaceuticals, Ltd | Oral capsules | 130 minutes prior to immersion in a controlled 3D virtual-reality scenario | 12.5% of volunteers reported increased appetite/hunger |
| Jadoon et al. [20] | Male and female patients with non-insulin-treated type 2 diabetes mellitus | 62 |
>18; mean: 56.8 |
100 mg (twice daily) | Provided by Jazz Pharmaceuticals | Oral capsules | 13 weeks |
No change in visceral adiposity No change in anthropometric parameters including weight (BMI), waist circumference, waist-to-hip ratio, neck circumference, and skinfold thickness No effect on appetite |
| Devinsky et al. [21] | Children and young adults with Dravet syndrome | 120 | 2–18; mean: 9–10 | 20 mg/kg/day | Provided by GW Pharmaceuticals, Ltd | Oral solution (twice a day) | 14 weeks |
Decrease in appetite: 5% of persons, placebo group 28% of persons, CBD group |
| Devinsky et al. [22] | Children with Dravet syndrome | 34 | 4–10; mean: 7–9 | 5, 10, or 20 mg/kg/day |
Provided by GW Pharmaceuticals, Ltd |
Oral solution | 3 weeks |
Decrease in appetite: 0% of persons, placebo group 0% of persons, 5-mg group 13% of persons, 10-mg group 44% of persons, 20-mg group |
| Miller et al. [23] | Children with Dravet syndrome | 199 | 2–18; mean: 9–10 | 10 or 20 mg/kg/day | A Cannabis sativa-derived, highly purified CBD (Epidiolex® in the US and Epidyolex® in the EU), GW Pharmaceuticals, Ltd | Oral solution | 14 weeks |
Decrease in appetite: 17% of persons, placebo group 17% of persons, 10-mg group 29% of persons, 2-mg group |
| Devinsky et al. [24] | Male and female patients with Lennox–Gastaut syndrome | 225 | 2–55; mean: 15–16 | 10 or 20 mg/kg/day | A plant-derived pharmaceutical formulation of purified CBD | Oral solution (twice a day) | 14 weeks |
Decrease in appetite: 8% of persons, placebo group 16% of persons, 10-mg group 26% of persons, 20-mg group |
| Thiele et al. [25] | Male and female patients with Lennox–Gastaut syndrome | 171 | 2–55; mean: 15–16 | 20 mg/kg/ day | Provided by GW Pharmaceuticals, Ltd | Oral solution | 14 weeks |
Decrease in appetite: 1% of persons, placebo group 9% of persons, 20-mg group |
| Aran et al. [26] |
Children with an autism spectrum disorder diagnosis per DSM-V criteria |
150 | 5–21; mean: 11-12 | 5.5 mg/kg/day | A whole-plant cannabis extract containing CBD and Δ9-THC at a 20:1 ratio and pure CBD and pure Δ9-THC at the same ratio and concentration | Oral/sublingual (whenever possible); 3 daily doses | 12 weeks |
No effect on appetite: 15% of persons, placebo group 22% of persons, pure CBD group 24% of persons, extract CBD group No effect on weight loss: 4% of persons, placebo group 13% of persons, pure CBD group 12% of persons, extract CBD group |
| Crippa et al. [27] | Patients with mild and moderate COVID-19 | 105 | Mean: 38.7–40.9 | 300 mg/day | CBD (99.6% purity; PurMed Global, Delray Beach, FL, USA) | Oral solution (twice a day) | 14 days |
No difference in appetite No difference in body weight |
| Taylor et al. [28] | Healthy male and female subjects | 30 | Mean: 25.3 | 750 mg twice daily for 4 weeks (followed by 750 mg twice daily for another 2 weeks) | A Cannabis sativa-derived, highly purified CBD (Epidiolex® in the USA and Epidyolex® in the EU), GW Pharmaceuticals, Ltd | Oral solution | Decreased appetite: 6.7% of volunteers |
3D three-dimensional, Δ9-THC delta-9-tetrahidrocannabidiol, BMI body mass index, CBD cannabidiol, COVID-19 coronavirus disease 2019, DSM-V Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, EU European Union
Effects of CBD on Body Weight and Appetite
In a crossover design clinical trial, ten healthy male participants were given CBD-rich C. sativa (<1% Δ9-THC, 9% CBD) by inhalation divided in two doses (25 mg initially and 10 mg 35 minutes later). Reported hunger, sweet food intake, and food preference did not significantly differ between interventions but a decrease in the desire to eat and a higher fullness was rated with CBD (compared to Δ9-THC-rich C. sativa and placebo) [18].
Another trial tested the effect of short-term administration of a single 600-mg dose of CBD on persecutory ideation and anxiety of 16 participants with paranoid traits 130 minutes prior to immersion in a controlled three-dimensional virtual-reality scenario. 12.5% of the participants (n = 2) of the CBD group reported increased appetite/hunger, while none did in the placebo arm of the trial [19].
In a trial with 62 adult subjects with non-insulin-treated type 2 diabetes, CBD was administered orally at a dose of 100 mg, twice daily, for 13 weeks (n = 13). Authors reported that CBD alone had no effect on appetite and did not change anthropometric parameters such as body mass index (BMI), waist circumference, visceral adiposity, waist-to-hip ratio, neck circumference, and skinfold thickness [20].
In a clinical trial involving 120 children with Dravet syndrome with drug-resistant seizures, CBD was tested as an add-on therapy to antiepileptic drugs to reduce the frequency of seizures. The participants were randomly allocated to either 20 mg/kg/day of oral CBD or placebo for 14 weeks. At the end of the study, 28% of children in the intervention group reported a decreased appetite while only 5% did in the placebo group [21].
Another trial conducted in 34 children (ages 4–10 years) also diagnosed with Dravet syndrome aimed to investigate the safety and preliminary pharmacokinetics of a pharmaceutical formulation of purified CBD. Participants were either assigned an oral dose of 5 mg/kg/day (n = 10), 10 mg/kg/day (n = 8), or 20 mg/kg/day (n = 9) of CBD for 3 weeks and a safety evaluation found that a decreased appetite was a common adverse event. Of note, this was the only outcome where a dose relationship was observed. In fact, while none of the individuals in the placebo and the 5-mg/kg/day arms reported a decreased appetite, 13% and 44% of the children assigned to the 10-mg/kg/day and 20-mg/kg/day arms, respectively, experienced this adverse event [22].
A bigger trial with the same objectives enrolled 199 children and young adults (ages 2–18 years) with Dravet syndrome and tested an oral CBD dose of either 10 mg/kg/day (n = 67) or 20 mg/kg/day (n = 67) for 14 weeks. Again, one of the most common adverse events was a decreased appetite with an apparent dose-relationship observed. Although the same percentage of participants in the placebo and lower dose groups experienced a decreased appetite (both 17%), a more significant portion (29%) presented with a decreased appetite in the group having the higher dose of CBD. Only one patient experienced a severely decreased appetite, he was assigned the 200-mg/kg/day dose of CBD [23].
Similarly, another study where 225 patients with Lennox–Gastaut syndrome were enrolled in a trial receiving a CBD oral solution at a dose of either 10 mg/kg (n = 73) or 20 mg/kg (n = 76) for 14 weeks showed that one of the most common adverse events among patients taking CBD was a decreased appetite, which was more common in the higher dose arm (16% vs 26%). Indeed, one patient assigned the 20-mg/kg dose of CBD experienced a severely decreased appetite [24].
In another trial with 171 patients with treatment-resistant Lennox–Gastaut syndrome, the same oral CBD 20-mg/kg dose (n = 86) was administered daily for 14 weeks. A decreased appetite was also one of the most common adverse events, with 9% of participants assigned the CBD reporting it. Again, one patient in this group reported a severe decrease in appetite [25].
In a recent crossover-type randomized controlled trial, 150 children and adolescents with a diagnosis of autism spectrum disorder were assigned either a solution of purified CBD and Δ9-THC at a 20:1 ratio (n = 50) or a whole-plant cannabis extract at the same ratio and concentration (n = 50). Following dose titration up to CBD 10 mg/kg/day for participants weighing 20–40 kg or up to CBD 7.5 mg/kg/day for those weighing more than 40 kg, participants were exposed to their intervention for 12 weeks. Both formulas elicited a decrease in appetite, although no statistically significant difference was found between them—24% receiving the plant extract and 22% receiving the purified formula. The same applies to weight loss and BMI, but notably, participants with a higher BMI at baseline had a more prominent decrease in this parameter following cannabinoid treatment [26].
A trial with 105 adult participants investigating the effects of CBD in coronavirus disease 2019 randomly allocated 49 individuals to receive a plant-derived, highly purified CBD oral solution at either 10 mg/kg/day or 20 mg/kg/day for 2 weeks. No differences in appetite or weight changes were found between the CBD group and the placebo group [27].
Finally, in a study aimed at investigating potential withdrawal symptoms in CBD users, 30 volunteers received a highly purified pharmaceutical formulation of CBD at a high dose (750 mg twice a day) for 4 weeks. After this period, participants were randomly allocated to receive either placebo or continue the same intervention for 2 more weeks. 6.7% (n = 2) of individuals experienced a decreased appetite in the first part of the trial but none did in the last 2 weeks [28].
Discussion
To the best of our knowledge, this is the first systematic review reporting on the effects of CBD specifically in appetite and body weight. We identified a total of 11 trials with CBD that reported on these outcomes.
Regarding appetite, most of the trials pointed to the cannabinoid in question apparently having an anorexigenic effect in some individuals (indeed, in seven of these studies, a decrease in appetite was reported by a higher percentage of the participants in the intervention arm while an eighth study reported increased fullness). Conversely, only one study reported on CBD possibly increasing appetite and two of the trials did not find any significant effect on either direction. Although not included in this review because the data were obtained through an online survey to parents, an increase in appetite following CBD administration to children with infantile spasms and Lennox–Gastaut syndrome was also previously reported [29].
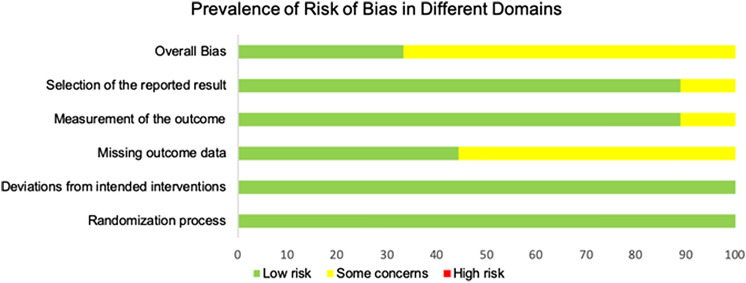
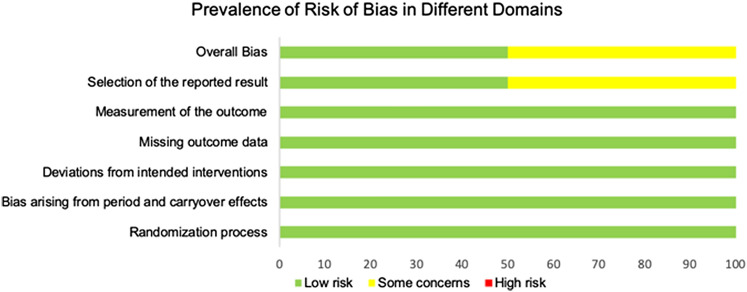
The prevalence of risk of bias (in different domains and overall) in the randomized controlled trials included is represented in bar plots in Figs. 2 and 3. In general, among the included randomized controlled trials, four were deemed as a low risk of bias and eight were labeled as raising some concerns. The randomization process, the selection of reported results, and especially the missing outcome data were the domains identified as major potential sources of bias. In this regard, a common problem identified within the studies was the lack of a sensitivity analysis for missing outcome data (in regard to body weight and/or appetite), which in most cases could have depended on its true value. The omission or unclear descriptions of certain study procedures such as when unblinding and protocol amendments took place were also accounted as sources of bias. Detailed data regarding the assessment of risk of bias is available in the Electronic Supplementary Material. Because of this risk of bias, the results of this systematic review should be interpreted with caution.
Fig. 2.
Prevalence of risk of bias in five different domains and overall bias among all randomized controlled trials included
Fig. 3.
Prevalence of risk of bias in five different domains and overall bias among all crossover-type randomized controlled trials included
It is known for some time that the endocannabinoid system plays an important role in regulating feeding circuits. Cannabinoid type 1 receptors (widely agreed to be the main responsible for the behavioral effects of cannabinoids) are present in the hypothalamus, the central regulator of energy balance, where they modulate not only neurotransmitter release but also neuroendocrine responses [30]. It is thus not surprising that modulation of this system by exogenous phytocannabinoids influences food intake, by mimicking their endogenous correspondents. In fact, it is proved that Δ9-THC (a CB1 receptor agonist) has a potent orexigenic effect, having been used in the 1990s for the treatment of appetite loss and wasting in patients with AIDS and cancer, for example [31, 32].
Later, new data emerged showing that a cannabinoid-receptor blockade can suppress feeding—rimonabant, a selective CB1 receptor inverse agonist, was able to attenuate the naturally hyperphagic actions of exogenous and endogenous cannabinoids [33]. As a matter of fact, this molecule was approved for obesity treatment by the Food and Drug Administration and the European Medicines Agency, before being withdrawn because of adverse psychiatric side effects such as depression and mood alterations [34]. Although the pharmacodynamic mechanisms of CBD are still fairly dubious, this molecule was proven to act also as a CB1 receptor inverse agonist at low concentrations [35]. We can hypothesize that this might be one of the reasons why most of the collected evidence in this review seems to point to an anorexigenic effect of CBD, even if research on cannabinoid receptor-independent pathways is still lacking.
However, it is also important to address certain study design options that might have overestimated the impact of CBD on appetite. One of the main concerns is the fact that in many of the trials included in this review, CBD was used as an add-on therapy to other medications, namely antiepileptic drugs, in populations with very rare forms of epilepsies (Dravet syndrome and Lennox–Gastaut syndrome). In fact, in five of the trials, participants were concomitantly taking topiramate, a drug that is known to decrease appetite and body weight [36]. For instance, one such trial described that the same percentage of participants receiving placebo and a lower dose of CBD reported a decrease in appetite [23]. However, as the randomization process seemed to be adequate in these studies, with no significantly different baseline characteristics between intervention groups, we can still assume the eventual effects to be CBD-dependent.
More importantly, the trials on epilepsies and autism spectrum disorder involved young participants (sometimes as young as 3 years of age) and it is not clear in which cases the assessments of appetite changes were reported by the participants directly or their caregivers. This point is important because there exists a strong cultural influence on caregivers’ perception and the interpretation of appetite and there is currently a lack of validated tools that take into account this cultural context [37].
A more objective way of measuring appetite changes and consequently the potential impact on feeding patterns would have been the assessment of body weight changes but unfortunately only three trials reported on this outcome [20, 26, 27]. In these three trials, no significant difference in appetite between the groups correlated with no difference in body weight. However, it is worth mentioning that, in one of these studies, although no difference in body weight was found between groups, participants in the CBD group with a higher BMI at baseline had a more prominent decrease in body weight following CBD treatment (the decrease in BMI was positively correlated with baseline BMI [p < 0.05]) [19]. More studies assessing anthropometric changes in CBD users are needed to establish such a potential correlation.
Another important factor to take into account is the possible influence (even if small) of Δ9-THC in the outcomes reviewed here. In two of the trials, the interventions consisted of both Δ9-THC and CBD, even if in one the CBD content was 20 times higher and in another, Δ9-THC accounted for less than 1% of the product’s content. In these two studies, it is thus difficult to isolate the effect of CBD and thus care should be taken when concluding about the effect of CBD.
In relation to the dosing regimen of CBD used in the different trials, they ranged from a minimum of 5 mg/kg/day up to a maximum of 750 mg twice daily. This difference in CBD doses between studies may explain the different effects of CBD on appetite/body weight found and even the lack of effect in some studies. Importantly, although a statistical correlation between dosage and effect was mentioned only in one study [22], this tendency is also suggested in other trials also included in this review, where higher doses of CBD elicited an increase in the number of participants experiencing a decreased appetite and/or in the severity of this effect [23–25]. This observation may indicate that for example in the context of epilepsy, CBD in lower doses may have a small effect on appetite (which is many times considered to be an adverse event) and still reduce the number of seizures, but that at higher doses, CBD may prompt more significant changes in feeding behavior.
In summary, we consider as limitations of this systematic review the fact that (1) in most of the studies, CBD was used as an add-on therapy to other medications, (2) the effect of CBD on body weight was evaluated only in some of the studies, (3) it is not clear if the assessment of appetite in children was reported directly by the participants or instead by their caregivers, (4) there may exist an influence of Δ9-THC (yet small) in two of the studies, and, finally, that (5) different dosages of CBD were used in the studies included.
Finally, as to the mechanisms that mediate CBD-induced loss of appetite, very little is known. In addition to the CB1-mediated anorexigenic effect mentioned above, the anti-obesity effect of CBD was mentioned to be CB2-mediated [32] or dependent on the induction of β-adrenergic receptors [38]. Moreover, some preclinical animal and in vitro data using cell cultures have identified some mechanisms of action that may contribute to these effects of CBD, including an increase in lipolysis [39, 40], an increase in thermogenesis, a decrease in lipogenesis and an increase in browning of white adipocytes [41], and an increase in insulin secretion [42]. In this context, in one of the trials included in this review, CBD at a dose of 100 mg (taken twice a day) rendered a significant increase in the plasma level of gastric inhibitory polypeptide while reducing the levels of plasma resistin in a population of patients with type 2 diabetes. Gastric inhibitory polypeptide is an incretin that has shown to preserve beta pancreatic cells [43], while high levels of resistin have previously been associated with obesity [44]. Finally, it is also possible that CBD-induced alterations in the gastrointestinal tract, for example, diarrhea [2], may also contribute to weight loss.
Conclusions
In light of the available evidence, CBD appears to have an anorexigenic effect that may be more substantial in individuals with a higher BMI. Cannabinoids are known to have an orexigenic effect mediated by CB1 and CB2 receptors, but distinctly from Δ9-THC, which possesses an orexigenic effect, CBD appears to decrease food intake. This observation is very interesting and clearly relevant in the context of obesity, a disease whose prevalence is increasing worldwide and which constitutes a risk factor for the development of comorbid conditions such as hyperinsulinemia, insulin resistance, type 2 diabetes, hypertension, dyslipidemia, coronary heart disease, gallbladder disease, and certain malignancies [45, 46]. Therefore, the evidence presented in the present work points to the need for additional primary research in order to unveil and clarify mechanisms of not only appetite modulation by CBD, but also on other metabolic effects of CBD that may contribute to changes in body weight.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
The authors thank Prof. Maria Augusta Vieira-Coelho for challenging us to develop this body of work. Without her initial counseling and guidance, this paper would not have been possible.
Declarations
Authors’ Contributions
Joaquim S. Pinto was responsible for the article design, data collection, and analysis as well as writing the first draft of the manuscript. Fátima Martel was responsible for the data collection and analysis as well as reviewing and editing the manuscript.
Funding
No funding was received for the preparation of this article.
Conflicts of Interest
Joaquim S. Pinto and Fátima Martel have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
References
- 1.Fraguas-Sánchez AI, Torres-Suárez AI. Medical use of cannabinoids. Drugs. 2018;78:1665–1703. doi: 10.1007/s40265-018-0996-1. [DOI] [PubMed] [Google Scholar]
- 2.Uranga JA, Vera G, Abalo R. Cannabinoid pharmacology and therapy in gut disorders. Biochem Pharmacol. 2018;157:134–147. doi: 10.1016/j.bcp.2018.07.048. [DOI] [PubMed] [Google Scholar]
- 3.Lowe H, Toyang N, Steele B, et al. The endocannabinoid system: a potential target for the treatment of various diseases. Int J Mol Sci. 2021;22(17):9472. doi: 10.3390/ijms22179472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Cannabidiol (CBD): World Health Organization Expert Committee on Drug Dependence Thirty‐ninth Meeting. 2017. Available from: https://www.who.int/medicines/access/controlled-substances/5.2_ CBD.pdf. Accessed 10 Jan 2022.
- 5.Bloomfield MAP, Hindocha C, Green SF, et al. The neuropsychopharmacology of cannabis: a review of human imaging studies. Pharmacol Ther. 2019;195:132–161. doi: 10.1016/j.pharmthera.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grof CPL. Cannabis, from plant to pill. Br J Clin Pharmacol. 2018;84(11):2463–2467. doi: 10.1111/bcp.13618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McPartland JM, Duncan M, Di Marzo V, et al. Are cannabidiol and Δ(9) -tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br J Pharmacol. 2015;172(3):737–753. doi: 10.1111/bph.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito G, Filippis DD, Cirillo C, et al. Cannabidiol in inflammatory bowel diseases: a brief overview. Phytother Res. 2013;27(5):633–636. doi: 10.1002/ptr.4781. [DOI] [PubMed] [Google Scholar]
- 9.Boychuk DG, Goddard G, Mauro G, et al. The effectiveness of cannabinoids in the management of chronic nonmalignant neuropathic pain: a systematic review. J Oral Facial Pain Headache. 2015;29(1):7–14. doi: 10.11607/ofph.1274. [DOI] [PubMed] [Google Scholar]
- 10.Devinsky O, Marsh E, Friedman D, et al. Cannabidiol in patients with treatment-resistant epilepsy: an open-label interventional trial. Lancet Neurol. 2016;15(3):270–278. doi: 10.1016/S1474-4422(15)00379-8. [DOI] [PubMed] [Google Scholar]
- 11.Freeman TP, Hindocha C, Green SF, et al. Medicinal use of cannabis based products and cannabinoids. BMJ. 2019;365:l1141. doi: 10.1136/bmj.l1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hazekamp A. The trouble with CBD oil. Med Cannabis Cannabinoids. 2018;1(1):65–72. doi: 10.1159/000489287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navarrete C, Garcia-Martin A, DeMesa J, et al. Cannabinoids in metabolic syndrome and cardiac fibrosis. Curr Hypertens Rep. 2020;22(12):98. doi: 10.1007/s11906-020-01112-7. [DOI] [PubMed] [Google Scholar]
- 14.Mastinu A, Premoli M, Ferrari-Toninelli G, et al. Cannabinoids in health and disease: pharmacological potential in metabolic syndrome and neuroinflammation. Horm Mol Biol Clin Investig. 2018 doi: 10.1515/hmbci-2018-0013. [DOI] [PubMed] [Google Scholar]
- 15.Rossi F, Punzo F, Umano GR, et al. Role of cannabinoids in obesity. Int J Mol Sci. 2018;19(9):2690. doi: 10.3390/ijms19092690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jesudason D, Wittert G. Endocannabinoid system in food intake and metabolic regulation. Curr Opin Lipidol. 2008;19(4):344–348. doi: 10.1097/MOL.0b013e328304b62b. [DOI] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Bruijn SEM, de Graaf C, Witkamp RF, et al. Explorative placebo-controlled double-blind intervention study with low doses of inhaled Δ9-tetrahydrocannabinol and cannabidiol reveals no effect on sweet taste intensity perception and liking in humans. Cannabis Cannabinoid Res. 2017;2(1):114–122. doi: 10.1089/can.2017.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hundal H, Lister R, Evans N, et al. The effects of cannabidiol on persecutory ideation and anxiety in a high trait paranoid group. J Psychopharmacol. 2018;32(3):276–282. doi: 10.1177/0269881117737400. [DOI] [PubMed] [Google Scholar]
- 20.Jadoon KA, Ratcliffe SH, Barrett DA, et al. Efficacy and safety of cannabidiol and tetrahydrocannabivarin on glycemic and lipid parameters in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel group pilot study. Diabetes Care. 2016;39(10):1777–1786. doi: 10.2337/dc16-0650. [DOI] [PubMed] [Google Scholar]
- 21.Devinsky O, Cross JH, Laux L, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. 2017;376(21):2011–2020. doi: 10.1056/NEJMoa1611618. [DOI] [PubMed] [Google Scholar]
- 22.Devinsky O, Patel AD, Thiele EA, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90(14):e1204–e1211. doi: 10.1212/WNL.000000000000525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller I, Scheffer IE, Gunning B, et al. Dose-ranging effect of adjunctive oral cannabidiol vs placebo on convulsive seizure frequency in Dravet syndrome: a randomized clinical trial. JAMA Neurol. 2020;77(5):613–621. doi: 10.1001/jamaneurol.2020.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the Lennox-Gastaut syndrome. N Engl J Med. 2018;378(20):1888–1897. doi: 10.1056/NEJMoa1714631. [DOI] [PubMed] [Google Scholar]
- 25.Thiele EA, Marsh ED, French JA, et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391(10125):1085–1096. doi: 10.1016/S0140-6736(18)30136-3. [DOI] [PubMed] [Google Scholar]
- 26.Aran A, Harel M, Cassuto H, et al. Cannabinoid treatment for autism: a proof-of-concept randomized trial. Mol Autism. 2021;12(1):6. doi: 10.1186/s13229-021-00420-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crippa JAS, Pacheco JC, Zuardi AW, et al. Cannabidiol for COVID-19 patients with mild to moderate symptoms (CANDIDATE Study): a randomized, double-blind, placebo-controlled clinical trial. Cannabis Cannabinoid Res. 2021 doi: 10.1089/can.2021.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor L, Crockett J, Tayo B, et al. Abrupt withdrawal of cannabidiol (CBD): a randomized trial. Epilepsy Behav. 2020;104(Pt A):106938. doi: 10.1016/j.yebeh.2020.106938. [DOI] [PubMed] [Google Scholar]
- 29.Hussain S, Zhou R, Jacobson C, et al. Perceived efficacy of cannabidiol-enriched cannabis extracts for treatment of pediatric epilepsy: a potential role for infantile spasms and Lennox-Gastaut syndrome. Epilepsy Behav. 2015;47:138–141. doi: 10.1016/j.yebeh.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Lau BK, Cota D, Cristino L, et al. Endocannabinoid modulation of homeostatic and non-homeostatic feeding circuits. Neuropharmacology. 2017;124:38–51. doi: 10.1016/j.neuropharm.2017.05.033. [DOI] [PubMed] [Google Scholar]
- 31.Beal JE, Olson R, Laubenstein L, et al. Dronabinol as a treatment for anorexia associated with weight loss in patients with AIDS. J Pain Symptom Manag. 1995;10(2):89–97. doi: 10.1016/0885-3924(94)00117-4. [DOI] [PubMed] [Google Scholar]
- 32.Plasse TF, Gorter RW, Krasnow SH, et al. Recent clinical experience with dronabinol. Pharmacol Biochem Behav. 1991;40(3):695–700. doi: 10.1016/0091-3057(91)90385-f. [DOI] [PubMed] [Google Scholar]
- 33.Curioni C, André C. Rimonabant for overweight or obesity. Cochrane Database Syst Rev. 2006;4:6162. doi: 10.1002/14651858.CD006162.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sam AH, Salem V. Ghatei MA Rimonabant: from RIO to Ban. J Obes. 2011;2011:432607. doi: 10.1155/2011/432607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pertwee RG. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. 2008;153(2):199–215. doi: 10.1038/sj.bjp.0707442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khalil NY, AlRabiah HK, Al Rashoud SS, et al. Topiramate: comprehensive profile. Profiles Drug Subst Excip Relat Methodol. 2019;44:333–378. doi: 10.1016/bs.podrm.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Molfino A, Kaysen GA, Chertow GM, et al. Validating appetite assessment tools among patients receiving hemodialysis. J Ren Nutr. 2016;26(2):103–110. doi: 10.1053/j.jrn.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ignatowska-Jankowska B, Jankowski MM, Swiergiel AH. Cannabidiol decreases body weight gain in rats: involvement of CB2 receptors. Neurosci Lett. 2011;490(1):82–84. doi: 10.1016/j.neulet.2010.12.031. [DOI] [PubMed] [Google Scholar]
- 39.Ramlugon S, Levendal R-A, Frost CL. Time-dependent effect of phytocannabinoid treatments in fat cells. Phytother Res. 2018;32(6):1080–1089. doi: 10.1002/ptr.6047. [DOI] [PubMed] [Google Scholar]
- 40.Silvestri C, Paris D, Martella A, et al. Two non-psychoactive cannabinoids reduce intracellular lipid levels and inhibit hepatosteatosis. J Hepatol. 2015;62(6):1382–1390. doi: 10.1016/j.jhep.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 41.Parray HA, Yun JW. Cannabidiol promotes browning in 3T3-L1 adipocytes. Mol Cell Biochem. 2016;416(1–2):131–139. doi: 10.1007/s11010-016-2702-5. [DOI] [PubMed] [Google Scholar]
- 42.Liu B, Song S, Ruz-Maldonado I, et al. GPR55-dependent stimulation of insulin secretion from isolated mouse and human islets of Langerhans. Diabetes Obes Metab. 2016;18(12):1263–1273. doi: 10.1111/dom.12780. [DOI] [PubMed] [Google Scholar]
- 43.Irwin N, Flatt PR. Evidence for beneficial effects of compromised gastric inhibitory polypeptide action in obesity-related diabetes and possible therapeutic implications. Diabetologia. 2009;52(9):1724–1731. doi: 10.1007/s00125-009-1422-8. [DOI] [PubMed] [Google Scholar]
- 44.Steppan CM, Bailey ST, Bhat S, et al. The hormone resistin links obesity to diabetes. Nature. 2001;409(6818):307–312. doi: 10.1038/35053000. [DOI] [PubMed] [Google Scholar]
- 45.Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. doi: 10.1007/978-3-319-48382-5_1. [DOI] [PubMed] [Google Scholar]
- 46.Lin X, Li H. Obesity: epidemiology, pathophysiology, and therapeutics. Front Endocrinol. 2021;12:706978. doi: 10.3389/fendo.2021.706978. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.