Abstract
The goal of this study was to investigate in-hospital mortality in patients suffering from acute respiratory syndrome coronavirus 2 (SARS-CoV-2) relative to the neutrophil to lymphocyte ratio (NLR) and to determine if there are gender disparities in outcome. Between February 26 and September 8, 2020, patients having SARS-CoV-2 infection were enrolled in this retrospective cohort research, which was categorized by NLR levels ≥9 and < 9. In total, 6893 patients were involved included of whom6591 had NLR <9, and 302 had NLR ≥9. The age of most of the patients in the NLR<9 group was 50 years, on the other hand, the age of most of the NLR ≥9 group patients was between 50 and 70 years. The majority of patients in both groups were male 2211 (66.1%). The ICU admission time and mortality rate for the patients with NLR ≥9 was significantly higher compared to patients with NLR <9. Logistic regression's outcome indicated that NLR ≥9 (odds ratio (OR), 24.9; 95% confidence interval (CI): 15.5–40.0; p < 0.001), male sex (OR, 3.5; 95% CI: 2.0–5.9; p < 0.001) and haemoglobin (HB) (OR, 0.95; 95% CI; 0.94–0.96; p < 0.001) predicted in-hospital mortality significantly. Additionally, Cox proportional hazards analysis (B = 4.04, SE = 0.18, HR = 56.89, p < 0.001) and Kaplan–Meier survival probability plots also indicated that NLR>9 had a significant effect on mortality. NLR ≥9 is an independent predictor of mortality(in-hospital) among SARS-CoV-2 patients.
Keywords: NLR, COVID-19, In-hospital mortality, SARS-CoV-2
Abbreviations: NLR, Neutrophil to lymphocyte ratio; RT–PCR, Reverse Transcription Polymerase Chain Reaction; SАRS-СоV-2, severe асute resрirаtоry syndrоme соrоnаvirus 2; AОR, аdjusted Odds Rаtiо; ICU, Intensive Care Unit; СRF, Cаse Reсоrd Fоrm; СI, Cоnfidenсe Intervаl
Highlights
-
•
The main finding of this study is that NLR is an autonomous predictor of in-hospital mortality in patients with SARS-CoV-2.
-
•
Fatality in SARS-CoV-2 patients with NLR >9 was 25 times higher than that in patients with NLR <9.
-
•
Patients with NLR >9, the average length of ICU stay was higher.
-
•
Mortality rate in males was high compared to females with NLR>9.
1. Intrоduсtiоn
The NLR can be employed as an indicator to examine SARS-CoV-2 disease's severity [1], with higher NLR intensities consistent SARS-CoV-2's inflammatory reaction [2]. SARS-CoV-2 patients who had a cytokine storm also had elevated NLR values, and [3] NLR levels in SARS-CoV-2 have been reported as an autonomous predictor of mortality in many studies [4,5]. These outcomes predicted by NLR are thought to be dependent on age, BMI, sex, and smoking [6,7] A meta-analysis showed that higher NLR predicts worse outcome in SARS-CoV-2 patients, and [8] the NLR predicts bacteraemia better than all other existing markers [9].
2. Methоds
This retrospective соhоrt study included 6893 SАRS-СоV-2-positive patients above the age of 18, both non-Kuwaitis and Kuwaitis, enrolled between February 26 and September 8, 2020. All dаtа were extracted from the electronic medical records from two Kuwаit tertiary care hospitals, Al Adаn Generаl Hоsрitаl and Jаber Al-Ahmed Hоsрitаl [[10], [11], [12], [13]].
A positive RT-R swab from the nаsopharynx confirmed SARS-CoV-2 infection. The Ministry of Health in Kuwаit stаndаrdized the care of all patients according to protocol. The standing committee for health coordination and medical research at the Ministry of Health in Kuwаit approved the procedure and waived the need for informed consent (Institutional review board number 2020/1422).
Раtients were categorized by NLR levels ≥9 and < 9. The primary outcome was death due to COVID-19, as specified by ICD 10 code U07.1. The following laboratory and clinical information were collected: sociodemographic factors, co-morbidity, clinical presentation, laboratory results, and length of ICU and hospital stay for data entry, an electronic case-record format (CRF) was employed. The neutrophil-lymphocyte ratio (NLR) was computed by dividing the absolute count of neutrophils by the absolute number of lymphocytes. Patients were divided into two groups: those with an NLR >9 and those with an NLR <9.
3. Stаtistiсаl аnаlysis
Continuous variables were summarized as the standard deviations and means or interquartile ranges and medians, while categorical variables were stated as the percentages and frequencies. Student's or Wilcoxon-Mann–Whitney t-tests were used for continuous variables, whereas the Pearson χ2 test was used for categorical variables. To examine the influence of NLR on in-hospital mortality adjusting for haemoglobin, age, and sex, a Logistic regression analysis was employed. The Cox рrороrtiоnal hazards model was employed to see if haemoglоbin had a significant effect on the mortality hazard. р<0.05 was the set level of significance. Stаtistiсаl analysis was carried out using R software [14] аnd SРSS version 27 (SРSS, IL, USА).
4. Results
Of the 6893 patients, 6591 had NLR <9, and 302 had NLR ≥9. The findings revealed that, in the NLR <9 cohort, the maximum number of patients was <50 years (n = 2002, 64%), and in the NLR ≥9 cohort, the maximum number of patients was 50–70 years (n = 132, 58%). In the NLR <9 cohort, 35% of the participants were females and 65% were males, whereas in the NLR ≥9 cohort, 20% of the participants were females, and 80% were males. The median duration of ICU admission was longer in the NLR ≥9 (2.00 [0.00; 10.3]) cohort than in the NLR <9 (0.00 [0.00; 3.00]) cohort. The mortality rate of patients with NLR ≥9 (n = 132, 44%) was also high compared to that of patients with NLR<9 (n = 40, 1%) [Table 1].
Table 1.
Demographic and clinical characteristics of the patients stratified by neutrophil to lymphocyte ratio (NLR).
| All |
NLR <9 |
NLR ≥9 |
p value |
n |
|
|---|---|---|---|---|---|
| n = 6893 | n = 6591 | n = 302 | |||
| Age, years, n (%) | <0.001 | 3343 | |||
| ≥70 | 215 (6.43%) | 173 (5.55%) | 42 (18.4%) | ||
| 50-70 | 1072 (32.1%) | 940 (30.2%) | 132 (57.9%) | ||
| <50 | 2056 (61.5%) | 2002 (64.3%) | 54 (23.7%) | ||
| Gender, n (%) | <0.001 | 3343 | |||
| Female | 1132 (33.9%) | 1087 (34.9%) | 45 (19.7%) | ||
| Male | 2211 (66.1%) | 2028 (65.1%) | 183 (80.3%) | ||
| ICU admission, median (IQR) | 0 (0–4) | 0 (0–3) | 2 (0–10) | <0.001 | 3343 |
| LOS, admission to discharge, median (IQR), days | 13 (2–31) | 13 (2–31) | 13(2–35) | 0.358 | 2886 |
| ICU LOS, median (IQR), days | 9 (0–38) | 10 (0–39) | 8 (0–30) | 0.141 | 408 |
| Mortality, n (%) | 172 (2.50%) | 40 (0.61%) | 132 (43.7%) | <0.001 | 6893 |
ICU; intensive care unit; IQR, interquartile range; LOS, length of hospital stay.
Haemoglobin (g/L) (133 ± 19.8), lymphocytes (10⁹/L) (2.33 ± 1.24) and platelet count (10⁹/L) (288 ± 102) for patients with NLR <9 were significantly elevated when compared to patients whose NLR is ≥ 9, whereas the white blood cell count (10⁹/L) (17.1 ± 9.24), neutrophils (15.2 ± 8.61), prothrombin time (sec) (17.7 ± 7.12), international normalized ratio (1.34 ± 0.59) and activated partial thromboplastin time (sec) (47.8 ± 24.4) were significantly higher for patients whose NLR is > 9 than for patients with NLR <9 [Table 2].
Table 2.
Laboratory characteristics of the patients stratified by neutrophil to lymphocyte ratio (NLR).
| Characteristic, mean ± SD |
All |
NLR <9 |
NLR ≥9 |
p value |
n |
|---|---|---|---|---|---|
| N = 6893 | N = 6591 | N = 302 | |||
| Hemoglobin, (g/L) | 132 (21.2) | 133 (19.8) | 100 (25.5) | <0.001 | 6893 |
| WBC, (10⁹/L) | 7.66 (3.94) | 7.23 (2.84) | 17.1 (9.24) | <0.001 | 6893 |
| LYM, (10⁹/L) | 2.27 (1.25) | 2.33 (1.24) | 0.88 (0.53) | <0.001 | 6893 |
| NEU, (10⁹/L) | 4.56 (3.64) | 4.07 (2.23) | 15.2 (8.61) | <0.001 | 6893 |
| PLT, (10⁹/L) | 287 (105) | 288 (102) | 247 (141) | <0.001 | 6892 |
| PT, seconds | 14.3 (4.52) | 13.9 (3.94) | 17.7 (7.12) | <0.001 | 2353 |
| INR | 1.06 (0.37) | 1.03 (0.32) | 1.34 (0.59) | <0.001 | 2353 |
| APTT, seconds | 33.3 (10.9) | 31.7 (6.46) | 47.8 (24.4) | <0.001 | 2277 |
WBC, white blood cell; LYM, lymphocytes; NEU, neutrophils; PLT, platelet; PT, prothrombin; INT, international normalized ratio; APTT, activated partial thromboplastin time.
Logistic regression analysis was conducted to examine the effect of NLR on all causes of in-hospital mortality while adjusting for haemoglobin, sex, and age. The analysis revealed a significant effect of NLR on mortality. Male patients had a higher mortality rate (odds ratio (OR), 3.46; 95% confidence interval (CI): 2.02–5.91; p < 0.001) compared with patients who had NLR ≥9 (OR, 24.9; 95% CI: 15.5–40.0; p < 0.001). Furthermore, the study also showed that higher haemoglobin (OR, 0.950; 95% CI: 0.94–0.96; p < 0.001) levels were less probably associated with all causes of in-hospital mortality. Table 3 summarizes the results of the logistic regression analysis [Table 3].
Table 3.
Impact of neutrophil to lymphocyte ratio (NLR) on mortality using multivariate logistic regression.
| Wald Test |
95% Confidence interval(odds ratio scale) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | Standard error | Odds ratio | z | Wald Statistic | p value | Lower bound | Upper bound | |
| (Intercept) | 0.842 | 0.633 | 2.320 | 1.329 | 1.768 | 0.184 | 0.671 | 8.023 |
| Hemoglobin | −0.051 | 0.005 | 0.950 | −9.874 | 97.498 | <0.001 | 0.940 | 0.960 |
| NLR ≥9 | 3.215 | 0.242 | 24.901 | 13.285 | 176.500 | <0.001 | 15.497 | 40.013 |
| Male gender | 1.240 | 0.274 | 3.457 | 4.532 | 20.542 | <0.001 | 2.022 | 5.912 |
| Age (50–70) | 0.360 | 0.250 | 1.433 | 1.440 | 2.073 | 0.150 | 0.878 | 2.339 |
| Age (≥70) | −0.196 | 0.385 | 0.822 | −0.510 | 0.261 | 0.610 | 0.387 | 1.746 |
Note. Mortality level Dead coded as class 1.
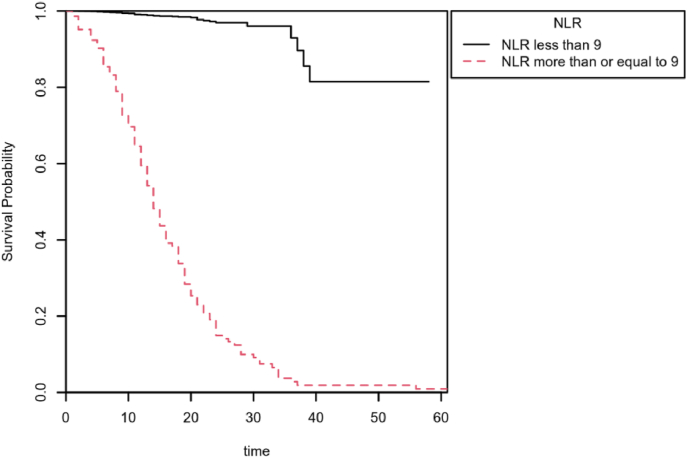
To determine whether the NLR had anyimpact on all cause in-hospital mortality, a Cox proportional hazards model was used. NLR ratio predicted risk of all cause of in-hospital mortality. The NLR ≥9's coefficient was significant (B = 4.04, SE = 0.18, HR = 56.89, p < 0.001), indicating that at any precise time, an observation in the NLR ≥9 will have a hazard that is 56.89 times as large as those that had NLR <9. The Kaplan–Meier survival probability plot over time for NLR is illustrated in Fig. 1.
Fig. 1.
Kaplan-Meier survival plot of Mortality grouped by neutrophil to lymphocyte ratio (NLR).
5. Disсussiоn
The main finding of this study is that NLR is an autonomous predictor of in-hospital mortality in patients with SARS-CoV-2. Specifically, fatality in SARS-CoV-2 patients with NLR >9 was 25 times higher than that in patients with NLR <9. Moreover, in patients with NLR >9, the average length of ICU stay was higher. Mortality rate in males was high compared to females with NLR>9. A lower haemoglоbin concentration was also associated with higher mortality. These findings are most likely related to the gravity of infection and the intensity of the immunological response, both of which may be linked to an increase in fatalities.
Many studies have shown that the NLR can be used as an indicator to detect SARS-CoV-2 infection, especially pneumonia [15]. A higher NLR was associated with a 2-fold probability of SARS-CoV-2 infection [16]. As the assessment of NLR is faster than RT–PCR, emergency room physicians can use NLR as a diagnostic tool to identify critically ill SARS-CoV-2 patients and triage them with proper care [17].The predictive value of the NLR is beyond that of SARS-CoV-2, as it could be used as a diagnostic tool for cardiovascular diseases and chronic obstructive pulmonary diseases (COPD) [[18], [19], [20], [21]]. NLR >4 is an autonomous predictor of in-hospital mortality, especially in patients with acute COPD exacerbation [22]. Several studies have shown the mortality prediction capability of the NLR in SARS-CoV-2 [[23], [24], [25], [26], [27]].
The NLR value in patients who have acute COPD exacerbation is 8.13, and the incidence of death was reported to be higher [28]. NLR is inversely associated with desaturation and a good predictor of exacerbations [29]. In another study, it was stated that an NLR >7 predicts fatalities in patients with bacteraemia [30]. In community acquired pneumonia (CAP), the NLR is considered an independent predictor of the severity of disease [ [31,32]]. Several studies have recommended the NLR as a prognostic indicator to assess the severity of SARS-CoV-2 disease [33].The NLR can be used for posttreatment confirmation regarding the absence of SARS-CoV-2 [[34], [35], [36]]. The predictive usefulness of NLR has been proven in pneumonia and in tumours [ [37,38]]. NLR can predict mortality in various other conditions apart from infectious diseases, such as polymyositis, intracerebral haemorrhage (ICH), dermatomyostis and acute coronary syndrome (ACS) [[39], [40], [41]].
Our study does have some limitations:. First, because the study was retrospective, causal inference was limited, and confounding factors that were unmeasured such as clinical comorbidities and drugs could have influenced the results. Furthermore, because our analysis covered all COVID-19 positive individuals in Kuwait, it is likely that it contained mostly milder forms of the condition.
6. Cоnсlusiоns
NLR is an autonomous predictor of in-hospital mortality in SARS-CoV-2 patients, with NLR >9 associated with 25 times higher mortality compared to patients with NLR< 9. The ICU admission time and mortality rate of patients in the NLR >9 group were significantly higher.
Ethical approval
Ethics Committee Approval 1081422.
Sources of funding
No source of funding
Author contribution
MАJ раrtiсiраted in аnаlysis аnd mаnusсriрt рreраrаtiоn. RR раrtiсiраted in dаtа аnаlysis аnd mаnusсriрt рreраrаtiоn. ААS аnd JР did the stаtistiсаl аnаlysis аs well аs mаnusсriрt review. Аll аuthоrs hаd ассess tо dаtа аnd tаke resроnsibility fоr the integrity оf dаtа аnd the ассurасy оf dаtа аnаlysis. Аll аuthоrs hаve reаd аnd аррrоved the mаnusсriрt.
Registration of research studies
1.Name of the registry: Not a registry.
2.Unique Identifying number or registration ID: Not applicable.
3.Hyperlink to your specific registration (must be publicly accessible and will be checked): Not applicable.
Guarantor
Dr. Rajesh Rajan MD, Ph.D, FRCP(Lon), FRCP(Edin), FRCP (Glasg), FRCP (Ire), FACC, FESC, FAHA.
Department of Cardiology.
Sabah Al Ahmed Cardiac Centre, Al Amiri Hospital Kuwait City, Kuwait, 15003.
Email: cardiology08@gmail.com.
Tel: +965-65873326.
Consent
The standing committee for health coordination and medical research at the Ministry of Health in Kuwаit approved the study protocol and accepted the request for waiver of the consent (Institutional the requirement оf infоrmed \1081422).
Patient consent statement
This retrospective observational study does not require patient permission. Permission to use content from other sources: This study does not include any material from other sources.
Data availability statement
The corresponding author can provide data to back up the conclusions of this study upon request. Due to privacy and ethical concerns, the data is not publicly available.
Declaration of competing interest
Nothing to disclose.
Acknowledgements
“Not applicable”.
References
- 1.Shang W., Dong J., Ren Y., et al. The value of clinical parameters in predicting the severity of COVID-19. J. Med. Virol. 2020;92:2188–2192. doi: 10.1002/jmv.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang A.P., Liu J.P., Tao W.Q., Li H.M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int. Immunopharm. 2020;84 doi: 10.1016/j.intimp.2020.106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Catanzaro M., Fagiani F., Racchi M., Corsini E., Govoni S., Lanni C. Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2. Signal Transduct. Targeted Ther. 2020;5:84. doi: 10.1038/s41392-020-0191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu H., Yao X., Xie X., Wu X., Zheng C., Xia W., Ma S. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J. Urol. 2017;35:261–270. doi: 10.1007/s00345-016-1864-9. [DOI] [PubMed] [Google Scholar]
- 5.Guthrie G.J., Charles K.A., Roxburgh C.S., Horgan P.G., McMillan D.C., Clarke S.J. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit. Rev. Oncol. Hematol. 2013;88:218–230. doi: 10.1016/j.critrevonc.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Howard R., Scheiner A., Kanetsky P.A., Egan K.M. Sociodemographic and lifestyle factors associated with the neutrophil-to-lymphocyte ratio. Ann. Epidemiol. 2019;38:11–21. doi: 10.1016/j.annepidem.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forget P., Khalifa C., Defour J., Latinne D., Van Pel M., De Cock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res. Notes. 2017;10:12. doi: 10.1186/s13104-016-2335-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lagunas-Rangel F.A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. J. Med. Virol. 2020;92:1733–1734. doi: 10.1002/jmv.25819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Jager C.P., van Wijk P.T., Mathoera R.B., de Jongh-Leuvenink J., van der Poll T., Wever P.C. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit. Care. 2010;14:R192. doi: 10.1186/cc9309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Jarallah M., Rajan R., Dashti R., et al. In-hospital mortality in SARS-CoV-2 stratified by serum 25-hydroxy-vitamin D levels: a retrospective study. J. Med. Virol. 2021;93:5880–5885. doi: 10.1002/jmv.27133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Jarallah M., Rajan R., Al Saber A., et al. In-hospital mortality in SARS-CoV-2 stratified by hemoglobin levels: a retrospective study. EJHaem. 2021 doi: 10.1002/jha2.195.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alroomi M., Rajan R., Omar A.A., et al. Ferritin level: a predictor of severity and mortality in hospitalized COVID-19 patients. Immun. Inflamm. Dis. 2021:1–8. doi: 10.1002/iid3.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Jarallah M., Rajan R., Dashti R., et al. In-hospital mortality in SARS-CoV-2 stratified by sex diffrences: a retrospective cross-sectional cohort study. Ann. Med. Surg. (Lond) 2022;79:104026. doi: 10.1016/j.amsu.2022.104026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laine T., Reyes E.M. Tutorial: survival estimation for Cox regression models with time-varying coefficients using SAS and R. J. Stat. Software. 2014;61:1–23. [Google Scholar]
- 15.Xiao A.T., Tong Y.X., Gao C., Zhu L., Zhang Y.J., Zhang S. Dynamic profile of rt-pcr findings from 301 COV ID-19 patients in Wuhan, China: a descriptive study. J. Clin. Virol. 2020;127 doi: 10.1016/j.jcv.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nalbant A., Kaya T., Varim C., Yaylaci S., Tamer A., Cinemre H. Can the neutrophil/lymphocyte ratio (NLR) have a role in the diagnosis of coronavirus 2019 disease (COVID-19)? Rev. Assoc. Med. Bras. 1992;66:746–751. doi: 10.1590/1806-9282.66.6.746. 2020. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Liu C., Mao Z., et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit. Care. 2020;24:647. doi: 10.1186/s13054-020-03374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kong W., He Y., Bao H., Zhang W., Wang X. Diagnostic value of neutrophillymphocyte ratio for predicting the severity of acute pancreatitis: a metaanalysis. Dis. Markers. 2020;2020 doi: 10.1155/2020/9731854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Templeton A.J., McNamara M.G., Seruga B., et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl. Cancer Inst. 2014;106:124. doi: 10.1093/jnci/dju124. [DOI] [PubMed] [Google Scholar]
- 20.Paliogiannis P., Fois A.G., Sotgia S., et al. Neutrophil to lymphocyte ratio and clinical outcomes in COPD: recent evidence and future perspectives. Eur. Respir. Rev. 2018;27:147. doi: 10.1183/16000617.0113-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim S., Eliot M., Koestler D.C., Wu W.C., Kelsey K.T. Association of neutrophilto- lymphocyte ratio with mortality and cardiovascular disease in the Jackson heart study and modification by the duffy antigen variant. JAMA Cardiol. 2018;3:455–462. doi: 10.1001/jamacardio.2018.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rahimirad S., Ghaffary M.R., Rahimirad M.H., Rashidi F. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. Tuberk Toraks. 2017;65:25–31. [PubMed] [Google Scholar]
- 23.Lian J., Jin C., Hao S., et al. High neutrophil-to-lymphocyte ratio associated with progression to critical illness in older patients with COVID-19: a multicenter retrospective study. Aging (Albany NY) 2020;12:13849–13859. doi: 10.18632/aging.103582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma A., Cheng J., Yang J., Dong M., Liao X., Kang Y. Neutrophil-to-lymphocyte ratio as a predictive biomarker for moderate-severe ARDS in severe COVID-19 patients. Crit. Care. 2020;24:288. doi: 10.1186/s13054-020-03007-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J.J., Cao Y.Y., Tan G., et al. Clinical, radiological and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients. Allergy. 2021;76:533–550. doi: 10.1111/all.14496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liao D., Zhou F., Luo L., et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 2020;7:e671–e678. doi: 10.1016/S2352-3026(20)30217-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fu J., Kong J., Wang W., et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: a retrospective study in Suzhou China. Thromb. Res. 2020;192:3–8. doi: 10.1016/j.thromres.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teng F., Ye H., Xue T. Predictive value of neutrophil to lymphocyte ratio in patients with acute exacerbation of chronic obstructive pulmonary disease. PLoS One. 2018;13 doi: 10.1371/journal.pone.0204377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee H., Um S.J., Kim Y.S., et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11 doi: 10.1371/journal.pone.0156511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Terradas R., Grau S., Blanch J., et al. Eosinophil count and neutrophil-lymphocyte count ratio as prognostic markers in patients with bacteremia: a retrospective cohort study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0042860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoon N.B., Son C., Um S.J. Role of the neutrophil-lymphocyte count ratio in the differential diagnosis between pulmonary tuberculosis and bacterial community-acquired pneumonia. Ann. Lab. Med. 2013;33:105–110. doi: 10.3343/alm.2013.33.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Jager C.P., Wever P.C., Gemen E.F., et al. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS One. 2012;7 doi: 10.1371/journal.pone.0046561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seyit M., Avci E., Nar R., et al. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am. J. Emerg. Med. 2021;40:110–114. doi: 10.1016/j.ajem.2020.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chan J.F., Yuan S., Kok K.-H., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;385:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang D., Hu B., Hu C., Zhu J., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J. Am. Med. Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu J., Liu Y., Xiang P., et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J. Transl. Med. 2020;18:206. doi: 10.1186/s12967-020-02374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ciccullo A., Borghetti A., Dal Verme L.Z., et al. Neutrophil-to-lymphocyte ratio and clinical outcome in COVID-19: a report from the Italian front line. Int. J. Antimicrob. Agents. 2020;56 doi: 10.1016/j.ijantimicag.2020.106017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ha Y.J., Hur J., Go D.J. Baseline peripheral blood neutrophil-to-lymphocyte ratio could predict survival in patients with adult polymyositis and dermatomyositis: a retrospective observational study. PLoS One. 2018;13 doi: 10.1371/journal.pone.0190411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Azab B., Zaher M., Weiserbs K.F. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am. J. Cardiol. 2010;106:470–476. doi: 10.1016/j.amjcard.2010.03.062. [DOI] [PubMed] [Google Scholar]
- 41.Giede-Jeppe A., Bobinger T., Gerner S.T. Neutrophil-to-Lymphocyte ratio is an independent predictor for in-hospital mortality in spontaneous intracerebral hemorrhage. Cerebrovasc. Dis. 2017;44:26–34. doi: 10.1159/000468996. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The corresponding author can provide data to back up the conclusions of this study upon request. Due to privacy and ethical concerns, the data is not publicly available.