Abstract
Objective:
The present study aimed to examine factors that may account for race/ethnicity differences in psychotic-like experiences (PLEs) in a middle childhood sample, including evidence for experiences of discrimination as a psychosocial mediator of these differences.
Method:
Within a sample of 10,839 9 to 10-year-olds from the Adolescent Brain Cognitive Development℠ study, we compared PLEs across racial/ethnic groups. We also examined whether experiences of discrimination indirectly linked racial/ethnic identity and PLEs, and whether social support moderated this indirect association.
Results:
Results indicated differences between racial/ethnic groups in the endorsement of PLEs, such that Black and Hispanic participants endorsed higher levels of PLEs as compared to Asian, Multiracial/Multiethnic, and White individuals. We found these differences were accounted for in part by experiences of discrimination, an indirect effect that was in turn attenuated by increased social support.
Conclusion:
This is the first study to suggest that the experience of discrimination may indirectly link the association between racial/ethnic differences and endorsement of PLEs using the PQ-BC, and additionally that social support may act as a moderator of this mediation. Results provide evidence that social inequities such as racial discrimination may contribute to increases in psychotic-like experiences. These findings shed further light on a possible mechanism linking structural racism and mental health inequities for people in minoritized groups.
Keywords: psychotic-like experiences, race, ethnicity, experiences of discrimination, ABCD Study
Lay Summary:
Using data from the Adolescent Brain Cognitive Development℠ study, the present study examined factors that underlie differences in psychotic-like experiences across individuals from racial and ethnic groups. The current study found evidence that differences in endorsement of psychotic-like experiences across racial and ethnic groups were accounted for in part by experiences of discrimination. The present study also identified a potentially modifiable factor, social support, that showed evidence of partially alleviating the indirect effect of experiences of discrimination. This evidence indicates that it is important for clinicians and researchers to consider contextual factors (e.g., experiences of discrimination) in understanding psychotic-like experiences across individuals from racial and ethnic groups.
Introduction
Psychotic-like experiences (PLEs) are common in the general population,1 with approximately two-thirds of 9-12-years-olds reporting at least one PLE.2-4 These experiences are often associated with distress and indicate a roughly 3.5 increased risk for developing a psychotic disorder.5 Independent of future psychotic disorder, PLEs in middle childhood and adolescence are often associated with several negative outcomes, including poor functioning,6,7 suicidal behavior,8,9 and major mental illness.9,10 Given these negative outcomes, early identification of PLEs may aid in mitigation or even prevention of negative clinical outcomes.11
Prevalence rates of PLEs may not be equal in people of different racial or ethnic groups. Studies have found increased endorsement of PLEs in people of minoritized racial and ethnic status,12-15 possibly indicative of early stages of mental health inequities. There are several potential contributors to these differences, including possible racial/ethnic variance in how PLEs are understood during measurement as well as true differences in prevalence. If it is the case, as evidence suggests, that there are some true group differences in PLE prevalence across racial/ethnic groups, the question remains as to what accounts for these differences. Psychosocial factors, including but not limited to experiences of discrimination (EOD) associated with historically marginalized ethnic/racial status, likely at least partially explain group differences in PLE prevalence.16,17 Marginalization, discrimination, and general disenfranchisement likely synergistically contribute to high and persistent stress.18,19 Persistent stress may in turn lead to PLEs through several mechanisms, including altered hypothalamic-pituitary-adrenal (HPA) functioning, which may interact with the already altered hormonal and neurobiological changes associated with adolescence.20,21 Despite the documented link between psychosocial factors such as EOD, PLEs, and historically marginalized status, to our knowledge, studies have not examined whether there is evidence consistent with EOD indirectly linking the association between racial/ethnic identity and PLEs.
Furthermore, the contribution of psychosocial factors such as EOD to risk for PLEs is complex, with multiple factors contributing to risk and resilience. For example, there is evidence that social support may be a particularly important resiliency factor and may mitigate risk factors for PLEs and psychosis.22-24 Along these lines, there is evidence that social support may buffer against altered HPA functioning in response to stress.25,26 Social support may be particularly important during possible sensitive periods of social development throughout adolescence.27
There are a number of additional factors that likely contribute to any group differences, including language ability, which may contribute to difficulties in understanding item content, as well as adverse experiences. According to biopsychosocial models of racism, it is important to account for the disproportionate exposure to stressors brought on by being part of a historically marginalized group, which may include the effects of intergenerational trauma and the experiences of adverse childhood events.28 Therefore, although we are not able to capture the entirety of likely adverse influences, the current study examined whether any group differences remained after accounting for potentially influential variables such as financial hardship, EOD, and adverse childhood experiences (ACEs), as well as variables reflecting cultural factors, including being born outside of the United States and language ability. It is expected that associations between group differences with PLEs will be either eliminated or substantially attenuated after accounting for these contextualizing factors.
The timing at which stressors occur may be of particular importance, as the developing brain has periods of relative sensitivity to stress,29,30 particularly pertinent for people who are at risk for psychosis.31-33 Most work examining PLEs in individuals from historically marginalized racial and ethnic groups has been conducted in late adolescence or early adulthood. Fewer studies have investigated EOD and PLEs in pre-adolescence, though existing evidence suggests that PLEs endorsed during this life stage can still be clinically significant.4,34,35 Further, to our knowledge no studies have explored potential mediators between race/ethnicity and PLEs in preadolescence. This age group presents a unique opportunity to look at very early factors that may contribute to the emergence of psychosis spectrum risk during important periods of brain and psychosocial development in many cases prior to the impact of treatment (psychopharmacological or otherwise).
The present study aimed to examine race/ethnicity differences in PLEs using ABCD Study® data. The paper’s primary aim was to examine what factors may underlie observed differences in PLEs across individuals from racial and ethnic groups. This study is the first to our knowledge to examine whether group differences remained after accounting for several potential influential factors, including language abilities, being born outside of the U.S., and metrics of adverse events, including financial adversity and ACEs. After assessing whether groups differ in endorsement of PLEs, the current paper is also the first to our knowledge to explore the possible mechanisms underlying this association in middle childhood, including whether EOD indirectly links race/ethnicity and PLEs, as well as the extent to which this indirect effect is conditional upon social support.
Methods
Participants
A sample of 11,875 individuals was obtained from the ABCD Study® (Data Release 3.0), a large-scale study tracking 9-10-years-olds recruited from 21 research sites across the United States.36 ABCD Study® data were accessed from the National Institutes of Mental Health Data Archive (Acknowledgments). All measures were collected at the ABCD Study® baseline assessment wave unless otherwise stated. The final sample size was 10,839 individuals (47.9% female; 2.2% Asian, 13.9% Black, 19.7% Hispanic, 10.5% Multiracial/Multiethnic [note, in addition to Multiracial/Multiethnic participants (82.5%), this group also included Native American/Alaskan Native (3.1%), Native Hawaiian or Other Pacific Islander (1.0%), or individuals that endorsed “Other” (13.4%)], and 53.8% White) for hierarchical linear models (Table 1 for sample characteristics).
Table 1.
Demographic and Measure Characteristicsa
| Sample (N=10,839) | ||
|---|---|---|
| Variables | M (SD) | Range |
| Distressing Psychotic-Like Experiences | 6.14 (10.41) | 0-104 |
| Experiences of Discrimination | 1.18 (0.39) | 1-5 |
| Social Support (number of close friends) | 5.92 (5.90) | 0-35 |
| Caregiver Rating of Youth’s English Proficiency | 3.71 (0.52) | 1-4 |
| Financial Adversity | 0.44 (1.07) | 0-7 |
| Adverse Childhood Experiences | 2.45 (2.28) | 0-20 |
| Age (in years) | 9.95 (0.63) | 9-11 |
| % | N | |
| Sex (% female) | 47.9 | 5182 |
| Race/Ethnicity | ||
| Asian | 2.2 | 236 |
| Black | 13.9 | 1503 |
| Hispanic | 19.7 | 2134 |
| Multiracial/Multiethnic | 10.5 | 1135 |
| White | 53.8 | 5831 |
| Born in the U.S. | 97.0 | 10513 |
Abbreviations. M=mean; SD=standard deviation; %=percentage; SE=standard error.
See methods section for details on definitions of these variables.
Measures
Race and Ethnicity
In the ABCD Study, the caregiver was asked to report on the youth’s race and ethnicity. First, the caregiver was asked “What race do you consider the child to be?” and was asked to check all that apply (e.g., White, Black/African American, Asian). Then the caregiver was asked “Do you consider the child Hispanic/Latino/Latina?” and could respond either ‘yes’ or ‘no’. Based on this information, the ABCD Study Data Releases contain a “race/ethnicity” variable, which is a 5-level variable coded as either White/Not Hispanic, Black/Not Hispanic, Hispanic, Asian, or Multiracial/Multiethnic (i.e., see Participants section for further explanation). Although this 5-level definition of race and Hispanic ethnicity conflates race and ethnicity, we also examined race and ethnicity separately (Supplement 1, available online; see Limitations section for additional discussion of these decisions with regards to the operationalization of these social constructs).
Psychotic-like Experiences
Youth completed the Prodromal Questionnaire-Brief Child Version (PQ-BC), a 21-item self-report questionnaire assessing psychotic-like experiences over the past month, previously validated for use with school-age children using the ABCD Study® sample.37 Youth first answered each question either yes or no. For each “yes”, youth were instructed to answer the follow-up question, “Did it bother you?”. If the youth endorsed “yes”, they were subsequently asked: “Please choose the number below the appropriate picture that shows us how much that bothered you when it happened.”, with the numbers corresponding to the pictures ranging from 1 to 5, in which participants were asked to rate distress from 1=strongly disagree to 5=strongly agree. Consistent with this previous research,37 the current study examined total and distress PQ-BC scores. Total scores were calculated as the total number of endorsed items (i.e., sum of answering ‘yes’ to the 21 items). Distress scores were calculated as the total score weighted by level of distress [i.e., 0=no, 1=yes (but no distress), 2-6=yes (1+score on distress scale)]. Although total scores index the entire dimension of PLEs, distress scores may reflect PLEs with greater clinical relevance.
Experiences of Discrimination (EOD)
The Perceived Discrimination Scale38 (PDS) is a 7-item youth-report questionnaire asking participants how often they experienced discrimination over the past 12 months: 1) from teachers, 2) from other adults outside the school, 3) from other students based on their ethnicity, 4) how often others behaved unfairly towards their ethnic group, 5) how often they felt not wanted in society, 6) how often they felt not accepted by other Americans, and 7) how often they felt Americans have something against them. Items are rated on a 5-point scale from ‘Almost Never’ to ‘Very Often’. For analyses, we examined the average of these EOD ratings. The PDS data were collected at the 1-year follow-up data collection wave.
Social Support
Youth reported on the number of male and female close friends,39 with the current study examining the summation of the number of reported close friendships.
Language Ability
Language ability was assessed by asking “How well do you speak English?” rated from 1=Poor to 4=Excellent (from the youth version of the Acculturation Survey Modified from PhenX40).
Financial Adversity
Financial adversity was measured as a summation of endorsement from seven questions of caregiver-rated financial difficulties (1=yes, 0=no): 1) Needed food but couldn't afford to buy it or couldn't afford to go out to get it?, 2) Were without telephone service because you could not afford it?, 3) Didn't pay the full amount of the rent or mortgage because you could not afford it?, 4) Were evicted from your home for not paying the rent or mortgage?, 5) Had services turned off by the gas or electric company, or the oil company wouldn't deliver oil because payments were not made?, 6) Had someone who needed to see a doctor or go to the hospital but didn't go because you could not afford it?, 7) Had someone who needed a dentist but couldn't go because you could not afford it? Financial adversity was chosen as a measure of financial hardship. This variable was chosen instead of an index of caregiver income due to the high number of missingness income data (missing n=1025), and because financial adversity measures the experiences of financial difficulties, experiences that are not necessarily captured with an income index.
Adverse Childhood Experiences (ACEs)
The PhenX Adverse Life Events scale measures 25 self-reported ACEs experienced by the child.41 Following the endorsement of an ACE, the child is asked whether this was a positive or negative event. Following previous research, we calculated ACEs as the summation of items that the child judged as negative.41 Although this measure was obtained at 1-year follow-up, it assessed lifetime ACEs.
Statistical Analyses
First, we aimed to replicate and extend previous measurement invariance analyses by examining whether each race/ethnicity group showed evidence of measurement invariance compared to all other race/ethnicity groups (i.e., Black, Hispanic, Multiracial/Multiethnic, White), as opposed to the original analyses2,42 which included all groups together in one model (Supplement 1, available online). If the stepwise tests indicate invariance across groups, mean comparisons can be meaningfully conducted across groups.43 The remainder of analyses used hierarchical linear models (HLMs), with all comparisons False Discovery Rate corrected (FDR-corrected) for each of the ten race/ethnicity category comparisons. Analyses were conducted in R lme4 package44 (lsmeans package for multiple comparison analyses45), with family unit and the 21 research sites modeled as random intercepts to account for nonindependence of observations, and age and sex included as covariates. Follow-up analyses examined whether results remained consistent when accounting for the youth’s English-speaking abilities, whether the youth was born in the United States, financial adversity, and ACEs. HLMs analyzed the relations between PQ-BC scores and both race/ethnicity and EOD, as well as between race/ethnicity and EOD. Based on these results, we performed mediation analyses using the lavaan package in R46 to examine whether there was evidence consistent with EOD potentially mediating associations between race/ethnicity and PLEs [note, for comprehensiveness, we also examined whether there was evidence consistent with PLEs indirectly linking the associations between race/ethnicity and EOD]. Significant mediation analyses were followed up with conditional process models to examine whether social support moderated any indirect effects of race/ethnicity category and PLEs through EOD. Specifically, we examined whether social support moderated the link between EOD and PLEs (model 14), with models separately examining each race/ethnicity category using the PROCESS R function.47 The present study aimed to follow guidelines for conducting scientific research involving topics related to health equities.48
Results
Mean Level Differences
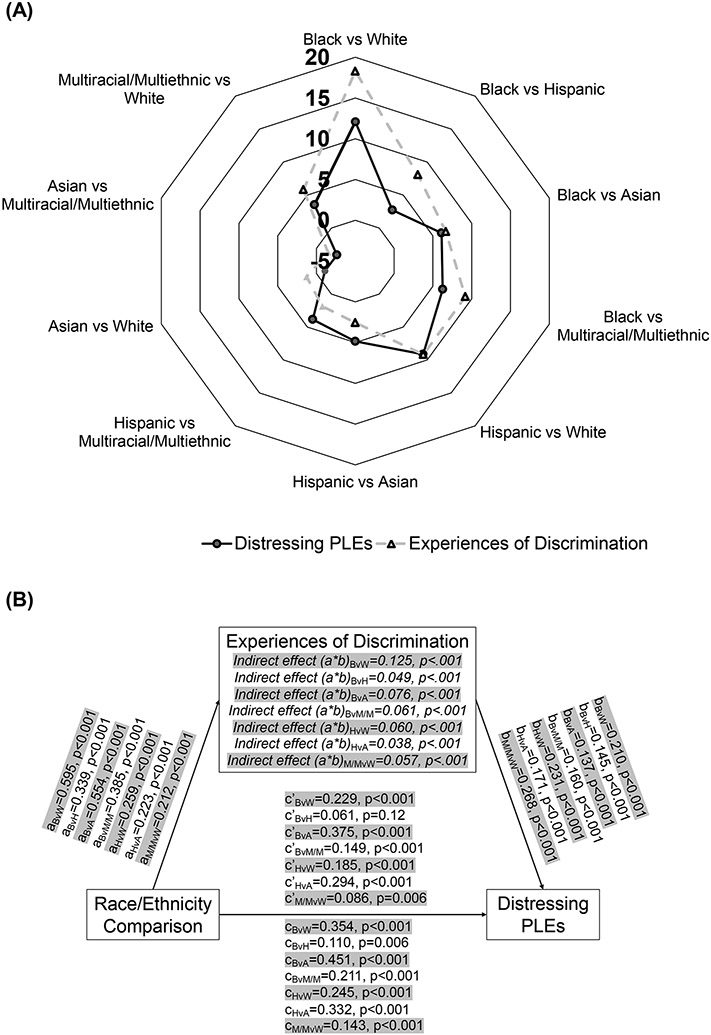
Given the measurement invariance results (Supplement 1, available online; although note analyses suggested some evidence of modest item bias between groups), we next examined race/ethnicity mean-level differences on PQ-BC scores. As can be seen in Figure 1a and Table 2, Black, Hispanic, and Multiracial/Multiethnic participants showed higher mean PQ-BC scores than Asian or White participants (all ∣Zs∣>2.32, all FDRps<.05), while Asian and White participants did not significantly differ for either PQ-BC score (all Zs<−1.09, all FDRps>.27; Table 2 for PQ-BC Distress score means; Table S1 for Total scores and Table S2 for Total score group comparisons, available online). Further, Black participants showed higher scores than the Hispanic or Multiracial/Multiethnic participants (Table 3; all Zs>2.72, all FDRps<.01). Lastly, Hispanic participants showed higher scores than Multiracial/Multiethnic participants (all Zs>3.34, all FDRps<.01) for both PQ-BC scores.
Figure 1. Overall Summary of Group Comparisons and Mediation Models.
Note: (A) Overall summary depicting Z statistics for false discovery rate (FDR)–corrected group comparisons comparing every race/ethnicity category for distressing psychotic-like experiences (PLEs) and experiences of discrimination. For race/ethnicity group comparisons that survived FDR correction (ie, FDR-corrected p < .05), the marker is outlined in black. (B) Depiction of a series of mediation models examining evidence for experiences of discrimination mediating the association between each individual race/ethnicity comparison with distressing PLEs. Each mediation model depicted includes unstandardized regression coefficients. A = Asian; B = Black; H = Hispanic; M/M = multiracial/multiethnic; W = White.
Table 2.
Means and Standard Errors (SE) for Distressing Psychotic-Like Experiences (PLEs) and Experiences of Discrimination (EOD) by Race/Ethnicity
| Distressing PLEs | EOD | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Upper CI | Lower CI | SE | Mean | Upper CI | Lower CI | SE | |
| Asian | 4.3 | 6.43 | 2.18 | 0.83 | 1.15 | 1.22 | 1.08 | 0.03 |
| Black | 8.76 | 10.18 | 7.34 | 0.55 | 1.34 | 1.37 | 1.30 | 0.01 |
| Hispanic | 7.75 | 9.15 | 6.36 | 0.54 | 1.22 | 1.25 | 1.19 | 0.01 |
| Multiracial/Multiethnic | 6.24 | 7.71 | 4.77 | 0.57 | 1.19 | 1.23 | 1.16 | 0.01 |
| White | 5.06 | 6.36 | 3.76 | 0.50 | 1.12 | 1.14 | 1.09 | 0.01 |
Abbreviations: CI=confidence interval; SE=standard error.
Table 3.
Group Comparisons for Distressing Psychotic-Like Experiences (PLEs) and Experiences of Discrimination (EOD), Including Comparisons Accounting for Follow-up Covariatesa
| Distressing PLEs | Distressing PLEs Including Follow-Up Covariatesa |
EOD | EOD Including Follow-Up Covariatesa |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comparison | Est. | Z | p | Est. | Z | p | Est. | Z | p | Est. | Z | p |
| Black and White | 3.71 | 12.08 | <.001 | 2.426 | 7.614 | <.001 | 0.218 | 18.269 | <.001 | 0.168 | 14.058 | <.001 |
| Black and Hispanic | 1.01 | 2.72 | .008 | 0.46 | 1.213 | .28 | 0.116 | 8.074 | <.001 | 0.094 | 6.642 | <.001 |
| Black and Asian | 4.46 | 6.11 | <.001 | 2.281 | 3.086 | .004 | 0.185 | 6.667 | <.001 | 0.120 | 4.317 | <.001 |
| Black and Multiracial/Multiethnic | 2.52 | 6.26 | <.001 | 1.698 | 4.174 | <.001 | 0.143 | 9.180 | <.001 | 0.115 | 7.467 | <.001 |
| Hispanic and White | 2.70 | 9.14 | <.001 | 1.966 | 6.588 | <.001 | 0.102 | 9.178 | <.001 | 0.075 | 6.808 | <.001 |
| Hispanic and Asian | 3.45 | 4.86 | <.001 | 1.821 | 2.564 | .02 | 0.069 | 2.569 | .01 | 0.026 | 0.981 | .36 |
| Hispanic and Multiracial/Multiethnic | 1.51 | 3.87 | <.001 | 1.237 | 3.169 | .004 | 0.028 | 1.859 | .08 | 0.021 | 1.428 | .19 |
| Asian and White | −0.75 | −1.09 | .28 | 0.146 | 0.211 | .83 | 0.033 | 1.269 | .20 | 0.049 | 1.868 | .09 |
| Asian and Multiracial/Multiethnic | −1.94 | −2.63 | .01 | −0.583 | −0.792 | .48 | −0.041 | −1.479 | .15 | −0.005 | −0.192 | .85 |
| Multiracial/Multiethnic and White | 1.18 | 3.53 | .001 | 0.729 | 2.186 | .04 | 0.074 | 5.800 | <.001 | 0.054 | 4.291 | <.001 |
Abbreviations: Est.=mean differences; Z=Z statistics; p=p-value.
Follow-up covariates included caregiver-rating of the youth’s English proficiency, whether the youth was born in the United States, financial adversity, and adverse childhood experiences.
In terms of covariates, lower age and male sex were associated with increased PLEs (see Table S3, available online). While lower rating of the youth’s English-speaking abilities, being born in the U.S., higher financial adversity, and higher ACEs were all associated with greater PLEs, results between race/ethnicity comparisons and PLEs generally remained consistent but diminished while accounting for these variables (Table 3). However, the Black and Hispanic comparison and the Asian and Multiracial/Multiethnic comparison no longer passed FDR thresholds (FDRps>.28) after inclusion of these influential variables.
Associations between EOD, PLEs, and Race/Ethnicity
Higher PLEs were associated with increased endorsement of EOD, β=0.21; 95%CI=0.19,0.23, and this association remained when including race/ethnicity in the model (β=0.20, 95%CI=0.18,0.22). When comparing the groups on EOD, Black participants reported greater experiences with discrimination compared to every other group (zs>6.67, FDRPs<.001; Table 3 and Figure 1a; see Table 2 for means), Hispanic participants reported greater experiences compared to Asian and White participants (zs>2.57, FDRPs<.01), Multiracial/Multiethnic group participants reported greater experiences compared to White participants (z=5.81,FDRP<.001), with none of the other groups significantly differing (∣zs∣<1.27, FDRPs>.08; Table S4 for group comparisons for the individual discrimination questions, available online). Further, most associations remained significant when accounting for ratings of the youth’s English-speaking abilities, being born in the U.S., financial adversity, and ACEs (Table 3), with the exception of the Hispanic and Asian comparison (FDRP=.36).
Furthermore, each of the aforementioned associations between race/ethnicity and PLEs (Mean Level Differences section) remained when accounting for EOD (FDRP<.05; see Table S5, available online). We next examined whether there was evidence consistent with EOD indirectly linking the associations between race/ethnicity and PLEs. As seen in Figure 1b, there was evidence consistent with EOD partially indirectly linking the relation between race/ethnicity and PLEs for each of the group comparisons showing a significant association with PLEs, with the estimated proportion mediated ranging from 11.45% for the Hispanic and Asian group comparison to 44.55% for the Black and Hispanic group comparison. We also examined whether there was evidence consistent with PLEs indirectly linking the associations between race/ethnicity and EOD. As can be seen in Figure S1, available online, there was also evidence consistent with PLEs partially indirectly linking the relation between race/ethnicity and EOD, although the estimated proportion mediated was lower than the original mediation analyses (i.e., with EOD as the mediator), ranging from 5.60% for the Black and Hispanic group comparison to 24.66% for the Hispanic and Asian group comparison.
In terms of social support as a potential moderator of the indirect effect, the results indicate that for Black (index of moderated mediation: −0.027, 95%CI: −0.048, −0.004) and Hispanic (index of moderated mediation: −0.027, 95%CI: −0.013, −0.001) groups compared to the other race/ethnicity categories, the indirect effect of race/ethnicity category on PLEs through EOD is increasingly weakened as social support increases (see Figure S2; see Table S6 for conditional indirect effects, available online). There was no strong evidence of a conditional indirect effect for the Multiracial/Multiethnic group compared to the other race/ethnicity categories (index of moderated mediation: −0.004, 95%CI: −0.009, 0.000).
Discussion
The current study demonstrated differences in endorsement of PLEs between racial/ethnic identities and found evidence consistent with EOD partially accounting for this association. We found group differences were attenuated after accounting for potentially influential variables related to adverse experiences and cultural factors. Further, we found evidence that increased social support attenuated the evidence of EOD indirectly linking racial/ethnicity to PLEs. Collectively, this study provides important insights regarding the nature of the association between racial/ethnic identities and PLEs, including factors such as EOD that may influence this association.
First, prior to examining mean differences between groups, we more comprehensively examined measurement invariance (Supplement 1, available online). Measurement invariance analyses across all groups suggested that variability on the PQ-BC reflected actual differences in PLEs and not the properties of the construct or individual items of the measure functioning differently across groups. This finding replicated and extended previous measurement invariances findings for the PQ-BC.2,42 With these considerations in mind, DIF analysis suggested some evidence of modest item bias between groups, suggesting people from different racial/ethnic backgrounds might perform slightly differently on several individual items (Supplement 1, available online).
In terms of mean level differences, Black, Hispanic, and Multiracial/Multiethnic participants (note this group included Multiracial/Multiethnic, Native American/Alaskan Native, Native Hawaiian or Other Pacific Islander, or endorsed “Other”) had higher mean PQ-BC scores than Asian or White participant groups.14,49,50 Our findings are generally consistent with previous research, including findings that Black individuals report some of the highest levels of PLEs among the major racial/ethnic groups in the U.S.51,52 Hispanic individuals also often score highly on measures of PLEs compared with other racial and ethnic groups,49,50,53 though not always.54 Similarly, previous studies have found relatively fewer PLEs in White participants with research on PLEs in Asian participants showing mixed results.55-57
The question remains as to why people of different racial/ethnic groups may experience higher levels of PLEs. One prominent explanatory model for these differences suggests that, in general, people of historically marginalized racial/ethnic status experience increased hardships and decreased access to resources and opportunities that contributes to chronic stress throughout the lifespan,13,19,58 particularly during impactful stages of development such as childhood and adolescence.59 Although speculative, this line of reasoning suggests that efforts to eliminate structural racism should result in a reduction of race/ethnicity differences in PLEs.
In order to begin to account for group differences, we examined whether variables related to systemic inequities, including cultural factors and adverse experiences, may attenuate group differences. Most group comparisons (Table 3) remained similar but diminished after accounting for influential variables (i.e., rating of the youth’s English-speaking abilities, being born in the U.S., financial adversity, ACEs, EOD, and social support). However, the Black and Hispanic, as well as the Asian and Multiracial/Multiethnic comparisons no longer passed significance threshold, suggesting these findings are perhaps better accounted for by these cultural factors and proxies of systemic racism. It is important to note that the data was collected prior to the beginning of the COVID-19 pandemic, and experiences of discrimination may have increased for certain groups (i.e., Asian participants) during the pandemic.
Additionally, given the association between racial/ethnic identity and endorsement of PLEs, we sought to understand psychosocial factors that may indirectly link these relations; specifically, experiences of racial discrimination (EOD). As expected,60,61 higher PLEs were associated with increased endorsement of EOD, with Black participants reporting higher EOD compared to every other group. EOD accounted for some, though not all, of the variance in the relation between race/ethnicity and PLEs, and associations between race/ethnicity and PLEs remained significant, even when accounting for EOD. Taken together, these findings are consistent with the hypotheses outlined above that EOD in this study may be functioning as a proxy for the chronic stressful effects of structural racism, likely contributing to, but not fully accounting for, the associations between race/ethnicity and PLEs.
Further, for Black and Hispanic groups, increased social support may provide a protective effect against the link between PLEs and EOD. This is consistent with previous work suggesting that increased social support may be an important resiliency factor.22-24 In particular, for individuals of historically marginalized racial or ethnic status, living in a neighborhood predominantly composed of people of a similar racial/ethnic identity is associated with decreased PLEs,59,62 perhaps due to more socially supportive environments18,63 and reduced incidence of racial discrimination. The current findings may help identify potentially modifiable factors, including social support and stress, that may modulate the effect that EOD has on the development and maintenance of PLEs.
The results of the current study, and the broader literature in which it sits, provide empirical basis for improvements in the psychological assessment and treatment of individuals in minoritized groups. To minimize perpetuation of inequities in marginalized groups of people, our findings suggest that clinicians and researchers should be mindful to recognize the impact of societal factors in how clients and research participants might respond to measures of psychopathology. Results from our study indicate a strong link between self-reported PLEs and factors such as EOD, financial adversity, immigration status, English language abilities, and ACEs. Clinicians and researchers who do not consider these external influences when working with individuals from historically marginalized groups run the risk of misattributing the sources of challenges, over-pathologizing, stigmatizing, and ultimately steering clients towards inappropriate treatment. Individual clinicians and researchers can actively seek awareness of their own potential biases. Bias can be minimized through a) educating oneself on the diversity of human experiences and practicing cultural humility, b) incorporating culturally competent therapeutic frameworks to address the impact of EOD on mental health,64 c) acknowledging one’s own implicit biases, d) seeking education and understanding of intersectionality among race/ethnicity and other individual differences, e) making oneself aware of biases innate to measures, and f) contributing to the development and use of measures invariant to racial or ethnic differences.
Interpretations of the results are bounded by the ways in which the variables are measured, including the limitations of the way race/ethnicity, sex, and financial adversity are measured. This study used racial/ethnic categories as a proxy for groups of people who may experience marginalization and/or differential treatment within society. Interpretations of the results are limited by the framework of racialized categories. We contend that race and ethnicity are social constructs, with unclear and mutable boundaries and tremendous within-group heterogeneity, originally created as a means of disenfranchising minoritized groups of people.65 There are always cost/benefit decisions to be made when deciding whether to lump vs. split racial/ethnic groups in analyses. Grouping creates overgeneralization and possible erasure of smaller minoritized groups (e.g. inclusion of Native American people in the Multiracial/Multiethnic group, as these groups have very different experiences, and groups with very small sample sizes may be too diluted to be represented). Separation creates groups with numbers too small to include in many analyses, thereby necessitating exclusion from analyses, and resulting in a lack of representation for these groups. We use these categories as an imperfect means to understanding the diversity of experiences people of color experience and how these experiences may relate to the endorsement, assessment, and interpretation of PLEs. To account for the experiences of people who identify as Hispanic, we combined the racial and ethnic categories, with Hispanic ethnic identity superseding any racial identities. This grouping was made in part due to recent studies indicating that, in the US, many people feel that “Hispanic” is their racial identity, or part of their racial identity.66,67 However, in the ABCD study, people were not afforded the opportunity to specify the identity, or intersection of identities, most prominent to them. We ran analyses with race and ethnicity separated and found similar results (Supplement 1, available online). Measuring ethnicity in a binary manner (i.e., Hispanic/non-Hispanic), as was done in the ABCD Study, does not fully capture many participant’s ethnic identities. Future work should examine analyses more fully reflecting the racial and ethnic identities of participants, and provide opportunities for participants to specify what identities are most salient.
EOD was reported retrospectively over the past year. The current analyses cannot address the possibility that EOD exclusively occurred after the development of PLEs. However, we also conducted analyses examining whether PLEs partially indirectly linked associations between race/ethnicity and EOD. Although there was some evidence for these indirect effects, the estimated proportion mediated was smaller in comparison to analyses examining whether EOD indirectly linked associations between race/ethnicity and PLEs. Thus, while PLEs may account for a portion of the association between race/ethnicity and EOD, there is stronger evidence for EOD partially indirectly linking associations between race/ethnicity and PLEs. This finding is consistent with biopsychosocial models of racism positing that the experience of stressors such as EOD over time influence the development or worsening of mental health concerns such as PLEs.68 Additionally, while the data are non-experimental and PLEs were measured at baseline whereas EOD were measured at 1-year follow-up (although results remain consistent if using 1-year follow-up PLEs), this does not preclude conducting mediation analyses,47 although analyses should not be interpreted by themselves to imply causation. Future directions include examining associations with cultural values, the influence of other environmental risk factors, and examining changes in associations over time.
This is the first study examining experiences of discrimination as a mediator of racial/ethnic differences in endorsement of PLEs using the PQ-BC. Our findings contribute to the understanding of racial/ethnic differences in the assessment of PLEs in middle childhood/early adolescence, an important developmental period which may set the stage for later functioning and symptom progression. Understanding of the nature of the associations between racial/ethnic identities and PLEs, including both the potential mechanisms (e.g. EOD) as well as factors that may contribute to these symptoms (e.g., social support) is helpful for identifying clinically, as well as societally, relevant factors that may be modifiable. Overall, the current study indicates that modifying psychosocial proxies of structural racism, such as EOD, could have important long-term implications for altering trajectories of PLEs.
Supplementary Material
Acknowledgments
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041028, U01DA041048, U01DA041089, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, U24DA041147, U01DA041093, and U01DA041025. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/Consortium_Members.pdf. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators.
The ABCD data repository grows and changes over time. The ABCD data used in this report came from DOI 10.15154/1519007.
Financial Disclosures:
N.R.K. receives funding from NIMH (K23MH121792-01 and L30 MH120574-01 to N.R.K.). J.S. receives funding from SAMHSA (SM081092-01) and NIMH (R01 MH112545-03, U01 MH124639-01). N.E. receives funding from the National Science Foundation (DGE-1745038). M.K., R.L.T., and S.Y.J. report no biomedical financial interests or potential conflicts of interest.
Additional Acknowledgments:
We thank the families participating in the Adolescent Brain and Cognitive Development study. In conducting analyses, drafting, and editing the paper, all authors have considered their positionality and proximity to the race/ethnicity groups described in the current paper. The authors would also like to thank the ABCD Justice Equity Diversity and Inclusion (JEDI) Responsible Use of Data workgroup for their work ensuring the responsible use of ABCD Study data.
References
- 1.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- 2.Karcher NR, Barch DM, Avenevoli S, et al. Assessment of the Prodromal Questionnaire-Brief Child Version for Measurement of Self-reported Psychoticlike Experiences in Childhood. JAMA Psychiatry. 2018;75(8):853–861. 10.1001/jamapsychiatry.2018.1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laurens KR, Cullen AE. Toward earlier identification and preventative intervention in schizophrenia: evidence from the London Child Health and Development Study. Social psychiatry and psychiatric epidemiology. 2016;51(4):475–491. 10.1007/s00127-015-1151-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laurens KR, Hodgins S, Maughan B, Murray RM, Rutter ML, Taylor EA. Community screening for psychotic-like experiences and other putative antecedents of schizophrenia in children aged 9-12 years. Schizophr Res. 2007;90(1-3):130–146. 10.1016/j.schres.2006.11.006 [DOI] [PubMed] [Google Scholar]
- 5.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. 10.1017/S0033291712001626 [DOI] [PubMed] [Google Scholar]
- 6.Brandizzi M, Schultze-Lutter F, Masillo A, et al. Self-reported attenuated psychotic-like experiences in help-seeking adolescents and their association with age, functioning and psychopathology. Schizophr Res. 2014;160(1-3):110–117. 10.1016/j.schres.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 7.Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42(9):1857–1863. 10.1017/S0033291711002960 [DOI] [PubMed] [Google Scholar]
- 8.Cederlof M, Kuja-Halkola R, Larsson H, et al. A longitudinal study of adolescent psychotic experiences and later development of substance use disorder and suicidal behavior. Schizophr Res. 2017;181:13–16. 10.1016/j.schres.2016.08.029 [DOI] [PubMed] [Google Scholar]
- 9.Fisher H, Caspi A, Poulton R, et al. Specificity of childhood psychotic symptoms for predicting schizophrenia by 38 years of age: a birth cohort study. Psychological medicine. 2013;43(10):2077–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rimvall MK, van Os J, Verhulst F, et al. Mental Health Service Use and Psychopharmacological Treatment Following Psychotic Experiences in Preadolescence. Am J Psychiatry. 2020;177(4):318–326. 10.1176/appi.ajp.2019.19070724 [DOI] [PubMed] [Google Scholar]
- 11.McGrath JJ, Saha S, Al-Hamzawi A, et al. The Bidirectional Associations Between Psychotic Experiences and DSM-IV Mental Disorders. Am J Psychiatry. 2016;173(10):997–1006. 10.1176/appi.ajp.2016.15101293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Earl TR, Fortuna LR, Gao S, et al. An exploration of how psychotic-like symptoms are experienced, endorsed, and understood from the National Latino and Asian American Study and National Survey of American Life. Ethn Health. 2015;20(3):273–292. 10.1080/13557858.2014.921888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leaune E, Dealberto MJ, Luck D, et al. Ethnic minority position and migrant status as risk factors for psychotic symptoms in the general population: a meta-analysis. Psychol Med. 2019;49(4):545–558. 10.1017/s0033291718002271 [DOI] [PubMed] [Google Scholar]
- 14.Paksarian D, Merikangas KR, Calkins ME, Gur RE. Racial-ethnic disparities in empirically-derived subtypes of subclinical psychosis among a U.S. sample of youths. Schizophr Res. 2016;170(1):205–210. 10.1016/j.schres.2015.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Ven E, Selten JP. Migrant and ethnic minority status as risk indicators for schizophrenia: new findings. Curr Opin Psychiatry. 2018;31(3):231–236. 10.1097/YCO.0000000000000405 [DOI] [PubMed] [Google Scholar]
- 16.Veling W, Susser E, Selten JP, Hoek HW. Social disorganization of neighborhoods and incidence of psychotic disorders: a 7-year first-contact incidence study. Psychol Med. 2015;45(9):1789–1798. 10.1017/S0033291714002682 [DOI] [PubMed] [Google Scholar]
- 17.McGrath JJ, Saha S, Al-Hamzawi A, et al. Psychotic Experiences in the General Population: A Cross-National Analysis Based on 31,261 Respondents From 18 Countries. JAMA Psychiatry. 2015;72(7):697–705. 10.1001/jamapsychiatry.2015.0575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schofield P, Das-Munshi J, Becares L, et al. Minority status and mental distress: a comparison of group density effects. Psychol Med. 2016;46(14):3051–3059. 10.1017/S0033291716001835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anglin DM, Greenspoon M, Lighty Q, Ellman LM. Race-based rejection sensitivity partially accounts for the relationship between racial discrimination and distressing attenuated positive psychotic symptoms. Early Interv Psychiatry. 2016;10(5):411–418. 10.1111/eip.12184 [DOI] [PubMed] [Google Scholar]
- 20.Pruessner M, Cullen AE, Aas M, Walker EF. The neural diathesis-stress model of schizophrenia revisited: An update on recent findings considering illness stage and neurobiological and methodological complexities. Neuroscience and biobehavioral reviews. 2017;73:191–218. 10.1016/j.neubiorev.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 21.Walker E, Mittal V, Tessner K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annual review of clinical psychology. 2008;4:189–216. 10.1146/annurev.clinpsy.4.022007.141248 [DOI] [PubMed] [Google Scholar]
- 22.Crush E, Arseneault L, Fisher HL. Girls get by with a little help from their friends: gender differences in protective effects of social support for psychotic phenomena amongst poly-victimised adolescents. Soc Psychiatry Psychiatr Epidemiol. 2018;53(12):1413–1417. 10.1007/s00127-018-1599-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crush E, Arseneault L, Danese A, Jaffee SR, Fisher HL. Using discordant twin methods to investigate an environmentally mediated pathway between social support and the reduced likelihood of adolescent psychotic experiences. Psychol Med. 2020;50(11):1898–1905. 10.1017/S0033291719001983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brett C, Heriot-Maitland C, McGuire P, Peters E. Predictors of distress associated with psychotic-like anomalous experiences in clinical and non-clinical populations. Br J Clin Psychol. 2014;53(2):213–227. 10.1111/bjc.12036 [DOI] [PubMed] [Google Scholar]
- 25.Wang S-w, Campos B. Cultural experiences, social ties, and stress: Focusing on the HPA axis. Handbook of culture and biology. 2017:317–343. [Google Scholar]
- 26.Wittig RM, Crockford C, Weltring A, Langergraber KE, Deschner T, Zuberbühler K. Social support reduces stress hormone levels in wild chimpanzees across stressful events and everyday affiliations. Nature communications. 2016;7(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blakemore SJ, Mills KL. Is adolescence a sensitive period for sociocultural processing? Annu Rev Psychol. 2014;65:187–207. 10.1146/annurev-psych-010213-115202 [DOI] [PubMed] [Google Scholar]
- 28.Goosby BJ, Heidbrink C. The transgenerational consequences of discrimination on African-American health outcomes. Sociology compass. 2013;7(8):630–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Belsky J, de Haan M. Annual Research Review: Parenting and children's brain development: the end of the beginning. J Child Psychol Psychiatry. 2011;52(4):409–428. 10.1111/j.1469-7610.2010.02281.x [DOI] [PubMed] [Google Scholar]
- 30.Humphreys KL, King LS, Sacchet MD, et al. Evidence for a sensitive period in the effects of early life stress on hippocampal volume. Dev Sci. 2019;22(3):e12775. 10.1111/desc.12775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mizrahi R, Addington J, Rusjan PM, et al. Increased stress-induced dopamine release in psychosis. Biol Psychiatry. 2012;71(6):561–567. 10.1016/j.biopsych.2011.10.009 [DOI] [PubMed] [Google Scholar]
- 32.Mizrahi R, Kenk M, Suridjan I, et al. Stress-induced dopamine response in subjects at clinical high risk for schizophrenia with and without concurrent cannabis use. Neuropsychopharmacology. 2014;39(6):1479–1489. 10.1038/npp.2013.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reininghaus U, Kempton MJ, Valmaggia L, et al. Stress Sensitivity, Aberrant Salience, and Threat Anticipation in Early Psychosis: An Experience Sampling Study. Schizophrenia Bulletin. 2016;42(3):712–722. 10.1093/schbul/sbv190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rimvall MK, Gundersen S, Clemmensen L, et al. Evidence that self-reported psychotic experiences in children are clinically relevant. Schizophr Res. 2019;204:415–416. 10.1016/j.schres.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 35.Gutteridge TP, Lang CP, Turner AM, Jacobs BW, Laurens KR. Criterion validity of the Psychotic-Like Experiences Questionnaire for Children (PLEQ-C). Schizophr Res. 2020;220:78–84. 10.1016/j.schres.2020.03.067 [DOI] [PubMed] [Google Scholar]
- 36.Barch DM, Albaugh MD, Avenevoli S, et al. Special Issue: Adolescent Brain and Cognitive Development Demographic, Physical and Mental Health Assessments in the Adolescent Brain and Cognitive Development Study: Rationale and Description. Developmental Cognitive Neuroscience.In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karcher NR, Barch DM, Avenevoli S, et al. Assessment of the Prodromal Questionnaire-Brief Child Version for Measurement of Self-reported Psychoticlike Experiences in Childhood. JAMA Psychiatry. 2018. 10.1001/jamapsychiatry.2018.1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phinney JS, Madden T, Santos LJ. Psychological variables as predictors of perceived ethnic discrimination among minority and immigrant adolescents 1. Journal of Applied Social Psychology. 1998;28(11):937–953. [Google Scholar]
- 39.Barch DM, Albaugh MD, Avenevoli S, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev Cogn Neurosci. 2018;32:55–66. 10.1016/j.dcn.2017.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alegria M, Takeuchi D, Canino G, et al. Considering context, place and culture: the National Latino and Asian American Study. International journal of methods in psychiatric research. 2004;13(4):208–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tiet QQ, Bird HR, Hoven CW, et al. Relationship between specific adverse life events and psychiatric disorders. Journal of abnormal child psychology. 2001;29(2):153–164. [DOI] [PubMed] [Google Scholar]
- 42.Karcher NR, Loewy RL, Savill M, et al. Replication of Associations with Psychotic-like Experiences in Middle Childhood from the Adolescent Brain Cognitive Development (ABCD) study. Schizophrenia Bulletin Open. 2020;1:sgaa009. 10.1093/schizbullopen/sgaa009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen FF. What happens if we compare chopsticks with forks? The impact of making inappropriate comparisons in cross-cultural research. Journal of personality and social psychology. 2008;95(5):1005. [DOI] [PubMed] [Google Scholar]
- 44.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. arXiv preprint arXiv:14065823. 2014. [Google Scholar]
- 45.Lenth RV. Least-Squares Means: The R Package lsmeans. 2016. 2016;69(1):33. 10.18637/jss.v069.i01 [DOI] [Google Scholar]
- 46.Rosseel Y lavaan: An R Package for Structural Equation Modeling. J Stat Softw. 2012;48(2):1–36. <Go to ISI>://WOS:000305117100001. [Google Scholar]
- 47.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford publications; 2017. [Google Scholar]
- 48.Flanagin A, Frey T, Christiansen SL, Bauchner H. The Reporting of Race and Ethnicity in Medical and Science Journals: Comments Invited. Jama. 2021;325(11):1049–1052. 10.1001/jama.2021.2104 [DOI] [PubMed] [Google Scholar]
- 49.Cohen CI, Marino L. Racial and ethnic differences in the prevalence of psychotic symptoms in the general population. Psychiatr Serv. 2013;64(11):1103–1109. 10.1176/appi.ps.201200348 [DOI] [PubMed] [Google Scholar]
- 50.Olfson M, Lewis-Fernandez R, Weissman MM, Feder A, Gameroff MJ, Pilowsky D, Fuentes M Psychotic symptoms in an urban general medicine practice. Am J Psychiatry. 2002;159:1412–1419. [DOI] [PubMed] [Google Scholar]
- 51.Oh H, Yang LH, Anglin DM, DeVylder JE. Perceived discrimination and psychotic experiences across multiple ethnic groups in the United States. Schizophr Res. 2014;157(1-3):259–265. 10.1016/j.schres.2014.04.036 [DOI] [PubMed] [Google Scholar]
- 52.DeVylder JE, Oh HY, Corcoran CM, Lukens EP. Treatment seeking and unmet need for care among persons reporting psychosis-like experiences. Psychiatr Serv. 2014;65(6):774–780. 10.1176/appi.ps.201300254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oh H, Abe J, Negi N, DeVylder J. Immigration and psychotic experiences in the United States: Another example of the epidemiological paradox? Psychiatry Res. 2015;229(3):784–790. 10.1016/j.psychres.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 54.Cicero DC, Krieg A, Martin EA. Measurement Invariance of the Prodromal Questionnaire-Brief Among White, Asian, Hispanic, and Multiracial Populations. Assessment. 2017:1073191116687391. 10.1177/1073191116687391 [DOI] [PubMed] [Google Scholar]
- 55.Cicero DC, Krieg A, Martin EA. Measurement Invariance of the Prodromal Questionnaire-Brief Among White, Asian, Hispanic, and Multiracial Populations. Assessment. 2019;26(2):294–304. 10.1177/1073191116687391 [DOI] [PubMed] [Google Scholar]
- 56.Cicero DC. Measurement invariance of the schizotypal personality questionnaire in Asian, Pacific Islander, White, and Multiethnic populations. Psychological Assessment 2016;28(4):351–361. 10.1037/pas0000180 [DOI] [PubMed] [Google Scholar]
- 57.Schiffman J Schizotypal traits in a non-clinical sample from Hawai'i. Pacific health dialog. 2004;11(1):84–86. [PubMed] [Google Scholar]
- 58.Morgan C, Fisher H, Hutchinson G, et al. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta psychiatrica Scandinavica. 2009;119(3):226–235. 10.1111/j.1600-0447.2008.01301.x [DOI] [PubMed] [Google Scholar]
- 59.Anglin DM, Lui F, Schneider M, Ellman LM. Changes in perceived neighborhood ethnic density among racial and ethnic minorities over time and psychotic-like experiences. Schizophr Res. 2020;216:330–338. 10.1016/j.schres.2019.11.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oh H, Cogburn CD, Anglin D, Lukens E, DeVylder J. Major discriminatory events and risk for psychotic experiences among Black Americans. Am J Orthopsychiatry. 2016;86(3):277–285. 10.1037/ort0000158 [DOI] [PubMed] [Google Scholar]
- 61.Anglin DM, Lui F, Espinosa A, Tikhonov A, Ellman L. Ethnic identity, racial discrimination and attenuated psychotic symptoms in an urban population of emerging adults. Early Interv Psychiatry. 2018;12(3):380–390. 10.1111/eip.12314 [DOI] [PubMed] [Google Scholar]
- 62.Das-Munshi J, Becares L, Boydell JE, et al. Ethnic density as a buffer for psychotic experiences: findings from a national survey (EMPIRIC). Br J Psychiatry. 2012;201(4):282–290. 10.1192/bjp.bp.111.102376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kirkbride JB, Stochl J, Zimbron J, et al. Social and spatial heterogeneity in psychosis proneness in a multilevel case-prodrome-control study. Acta Psychiatr Scand. 2015;132(4):283–292. 10.1111/acps.12384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Opara I, Assan MA, Pierre K, et al. Suicide among Black children: An integrated model of the interpersonal-psychological theory of suicide and intersectionality theory for researchers and clinicians. Journal of Black Studies. 2020;51(6):611–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guess T The social construct of whiteness: racism by intent, racism by consequence. Critical Sociology. 2006;32(4):649–673. [Google Scholar]
- 66.Telles E Latinos, Race, and the U.S. Census. The ANNALS of the American Academy of Political and Social Science. 2018;677(1):153–164. 10.1177/0002716218766463 [DOI] [Google Scholar]
- 67.Deaux K Ethnic/Racial Identity: Fuzzy Categories and Shifting Positions. The ANNALS of the American Academy of Political and Social Science. 2018;677(1):39–47. 10.1177/0002716218754834 [DOI] [Google Scholar]
- 68.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American psychologist. 1999;54(10):805. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.