Abstract
Inflammatory activation and oxidative stress promote the proliferation of vascular smooth muscle cells (VSMCs), which accounts for pathological vascular remodeling in hypertension. ELABELA (ELA) is the second endogenous ligand for angiotensin receptor-like 1 (APJ) receptor that has been discovered thus far. In this study, we investigated whether ELA regulated VSMC proliferation and vascular remodeling in spontaneously hypertensive rats (SHRs). We showed that compared to that in Wistar-Kyoto rats (WKYs), ELA expression was markedly decreased in the VSMCs of SHRs. Exogenous ELA-21 significantly inhibited inflammatory cytokines and NADPH oxidase 1 expression, reactive oxygen species production and VSMC proliferation and increased the nuclear translocation of nuclear factor erythroid 2-related factor (Nrf2) in VSMCs. Osmotic minipump infusion of exogenous ELA-21 in SHRs for 4 weeks significantly decreased diastolic blood pressure, alleviated vascular remodeling and ameliorated vascular inflammation and oxidative stress in SHRs. In VSMCs of WKY, angiotensin II (Ang II)-induced inflammatory activation, oxidative stress and VSMC proliferation were attenuated by pretreatment with exogenous ELA-21 but were exacerbated by ELA knockdown. Moreover, ELA-21 inhibited the expression of matrix metalloproteinase 2 and 9 in both SHR-VSMCs and Ang II-treated WKY-VSMCs. We further revealed that exogenous ELA-21-induced inhibition of proliferation and PI3K/Akt signaling were amplified by the PI3K/Akt inhibitor LY294002, while the APJ receptor antagonist F13A abolished ELA-21-induced PI3K/Akt inhibition and Nrf2 activation in VSMCs. In conclusion, we demonstrate that ELA-21 alleviates vascular remodeling through anti-inflammatory, anti-oxidative and anti-proliferative effects in SHRs, indicating that ELA-21 may be a therapeutic agent for treating hypertension.
Keywords: ELABELA peptide, hypertension, proliferation, vascular remodeling, inflammation, oxidative stress
Introduction
The global prevalence of hypertension is 26% and may rise to 30% by 2025 [1]. Hypertension is a complex and multifactorial disorder that involves interactions among genetic, environmental and pathophysiologic factors. Common molecular mechanisms, especially oxidative stress and inflammation, have been proposed to be major drivers coordinating diverse cellular events and organ systems in the context of hypertension [2, 3].
Vascular smooth muscle cells (VSMCs), which are major components of the arterial wall, maintain vascular tone in response to hemodynamic changes and humoral stimulation [4]. VSMC dysfunction, including increased oxidative stress, inflammation, migration and hypertrophy, play critical roles in the pathogenesis of atherosclerosis and hypertension. Upon exposure to local proinflammatory stimuli, inflammation is activated in VSMCs, which is a pervasive feature in hypertension development in humans and experimental models [5–7]. We previously reported that VSMC proliferation was closely linked with vascular remodeling and stiffening in the context of hypertension [8, 9]. It is well known that oxidative stress is a critical promoter of cell proliferation [2]. Excessive reactive oxygen species (ROS) can damage vessel walls by generating unstable free radicals and recruiting proinflammatory cells [10]. Vascular inflammation and oxidative stress promote VSMC proliferation, thereby stimulating vascular remodeling in hypertension and vascular diseases [11]. Therefore, it is of considerable therapeutic importance to explore effective agents for inhibiting oxidative stress, inflammatory responses and VSMC proliferation.
ELABELA/APELA (ELA) is a new ligand of the APJ/apelin receptor. The APJ receptor was initially cloned as an orphan G-protein-coupled receptor that shares 30% homology with angiotensin receptor 1, while apelin was thought to be the only ligand for APJ until ELA was discovered. ELA and apelin share the same receptor and exert similar biological effects. A family consisting of ELA, apelin, and APJ is known as the apelinergic system, which is highly expressed in the cardiovascular system and is involved in the development of the fetal heart and blood vessels and regulating vascular tension in adults [12]. Clinical and experimental studies clearly support multiple cardioprotective effects of the apelin–APJ axis [13, 14]. Moreover, animal studies have shown that ELA had a more significant effect on reducing systemic vasodilation than apelin [15]. However, the underlying mechanisms of the ELA-APJ axis remain largely unclear despite their clinical importance. Three ELA peptides (ELA-32, ELA-21 and ELA-11) are full agonists that activate APJ and G protein signaling with comparable potency to [Pyr1]apelin-13 [16]. Our previous studies showed that when administered centrally versus peripherally, ELA-21 has opposite effects on hypertension. Peripheral administration of ELA-21 decreases mean arterial pressure (MAP) in spontaneously hypertensive rats (SHRs) [17], while central microinjection increases MAP. Furthermore, exogenous ELA treatment exerts antihypertensive effects on angiotensin II (Ang II)-infused mice, high salt-fed and Dahl salt-sensitive rats and rodent pulmonary arterial hypertension models [18–20]. At present, no reports have examined the association of ELA with VSMC function. Sufficient evidence has shown the effects and mechanisms of apelin in VSMC proliferation [21, 22], but whether ELA also plays an important role in VSMC proliferation remains unclear. The aim of this study was to identify the role of ELA-21 in VSMC proliferation and vascular remodeling in the context of hypertension.
Materials and methods
Animals
Twelve-week-old male Wistar-Kyoto rats (WKYs) and SHRs were obtained from Vital River Laboratory Animal Technology (Beijing, China) and housed in a temperature controlled room at 22–26 °C and 40%–50% humidity with a 12 h light/dark cycle and free access to standard chow and tap water. Experiments were approved by the Experimental Animal Care and Use Committee of Nanjing Medical University and conformed to the Guide for the Care and Use of Laboratory Animals (National Institutes of Health, NIH publication, 8th ed., 2011). SHRs with systolic blood pressure higher than 150 mmHg were included in this study. At the end of the experiments, each rat was euthanized with an overdose of pentobarbital sodium (150 mg/kg, iv), and the vascular vessels were harvested for histological and molecular biological analyses.
Cell culture
SHR is the best animal model of human essential hypertension. Ang II is commonly used to induce VSMC proliferation, oxidative stress and inflammation in vitro [23]. In the present study, VSMCs from SHRs and Ang II-treated VSMCs from WKYs were used to establish in vitro models of VSMC proliferation in the context of hypertension. Primary VSMCs were isolated from the media of the thoracic aortas of WKYs and SHRs using previously described methods [24]. Briefly, rat thoracic aortas were isolated after perivascular fat tissue removal. Each aorta was longitudinally cut open and stripped of its intima. Then, the aortic media was carefully separated from the adventitia and treated with 0.4% collagenase II in Dulbecco’s Minimum Essential Medium (DMEM; Gibco, Grand Island, NY) for 30 min. After the cells had migrated from the tissue pieces in DMEM supplemented with 20% fetal bovine serum (FBS), the VSMCs were collected and cultured in DMEM supplemented with 10% FBS, 100 IU/mL penicillin and 10 mg/mL streptomycin in a humidified atmosphere containing 5% CO2 at 37 °C. VSMCs in the third, fourth and fifth passages were harvested for mRNA/protein analyses or functional testing. Each experiment was performed at least three times with triplicate cultures.
Evaluation of cell proliferation
VSMC proliferation was evaluated with a cell counting kit-8 (CCK-8) kit, 5-ethynyl-2’-deoxyuridine (EdU) assay and proliferating cell nuclear antigen (PCNA) expression assay as previously reported [8]. A CCK-8 kit (Beyotime Biotechnology, Shanghai, China) was used and the absorbance was measured at 450 nm with a microplate reader (ELX800, BioTek, Vermont, USA). For DNA synthesis examination, a Cell-Light™ EdU Apollo®567 In Vitro Imaging Kit (RiboBio, Guangzhou, China) was used with an EdU incorporation assay. Images were captured with a fluorescence microscope (DP70, Olympus Optical, Tokyo, Japan). The number of EdU-positive cells was normalized to the total number of cells. PCNA expression was determined by Western blot and quantitative real-time PCR (qRT-PCR).
RNA extraction and PCR analysis
Total RNA was extracted from rat aortas or VSMCs using TRIzol reagent (Invitrogen) according to the manufacturer’s protocol as previously reported [17]. Reverse transcription PCR was conducted with total RNA (1 μg) using the Prime Script RT Master Mix kit (Takara, Japan). For semi-quantitative PCR, DreamTaq Green PCR Master Mix (Invitrogen) was used and PCR products were separated on a 2% agarose gel. For qRT-PCR, SYBR Green Master Mix (Takara, Japan) was used on a StepOne Plus system. The sequences of the primers used in this study are listed in Supplementary Table 1.
Western blot analysis
The protein expression levels of tumor necrosis factor-α (TNF-α), interleukin 6 (IL-6), monocyte chemoattractant protein-1 (MCP-1), inducible nitric oxide synthase (iNOS), heme oxygenase-1 (HO-1), NADPH quinone oxidoreductase 1 (NQO1), glutamate cysteine ligase catalytic subunit (GCLC), glutamate cysteine ligase modulatory subunit (GCLM), matrix metalloproteinase 2 (MMP2), matrix metalloproteinase 9 (MMP9), NADPH oxidase 1 (NOX1), NADPH oxidase 4 (NOX4), PCNA, phosphatidylinositol-3-kinase (PI3K)-p85α, p-PI3K-p85α, p-Akt and Akt in aortas or VSMCs were examined by Western blot. Total protein concentrations in the supernatants of the samples were determined with a BCA protein assay kit (Thermo Fisher Scientific, IL, USA). Protein extracts were electrophoresed, blotted, and then incubated with the corresponding primary antibodies and appropriate HRP-conjugated secondary antibodies as previously reported [25]. Antibodies against TNF-α (ab205587), IL-6 (ab259341), iNOS (ab178945), HO-1 (ab68477), NQO1 (ab80588), GCLC (ab190685), GCLM (ab178945), and MMP9 (ab228402) were obtained from Abcam (Cambridge, MA, USA). Antibodies against NOX1 (#DF8684), NOX4 (#DF6924), PI3K-p85α (#AF6241), and p-PI3k-p85α (#AF3241) were obtained from Affinity Biosciences (OH, USA). Antibodies against PCNA (#10205-2-AP), MCP-1(#66272-1-lg), and MMP2 (#10373-2-AP) were purchased from Protein Tech Group Inc. (Chicago, IL, USA). Antibodies against Akt (#4691) and p-Akt (#4060) were obtained from Cell Signaling Technology (Beverly, MA, USA).
Immunofluorescence staining
Nuclear factor erythroid 2-related factor (Nrf2) expression in the VSMCs was determined by immunofluorescence staining. Cells were incubated at 4 °C overnight with anti-Nrf2 (1:400 dilution) (16396-1-AP, Protein Tech Group Inc. Chicago, USA). The cells were then incubated with fluorescence-labeled secondary antibodies (1:1000 dilution) for 2 h at room temperature. DAPI (1:1000 dilution) was used for nuclear staining. A fluorescence microscope (Leica Microsystems, Oberkochen, Germany) was used for image capture.
Immunohistochemistry
Immunohistochemistry was used to examine the expression of vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) in the aortas of SHRs. The sections were incubated with anti-VCAM-1 or anti-ICAM-1 (sc-13160 and sc-8439, Santa Cruz, CA, USA) primary antibodies at a dilution of 1:100. Immunostaining was carried out with a commercially modified avidin-biotin-peroxidase complex technique, and the samples were counterstained with hematoxylin. All images were captured with a light microscope (BX-51, Olympus, Tokyo, Japan). Quantitative analysis was performed with ImageJ software.
Dihydroethidium (DHE) fluorescence staining
DHE fluorescence staining in the aorta or VSMCs was used to evaluate intracellular ROS production. Sections of OCT-embedded aortas were incubated with equal concentrations of DHE for 5 min at room temperature. Then, the sections were rinsed twice with PBS. Cells (3 × 105 cells/mL) in 6-well plates were incubated with DHE (10 μM) in PBS for 30 min in a dark and humidified container at 37 °C. After being washed twice with cold PBS, DAPI (1:1000 dilution) was used for nuclear staining. The fluorescence of the sections was examined with a fluorescence microscope (DP70, Olympus Optical, Tokyo, Japan) with an excitation wavelength of 518 nm and an emission wavelength of at 605 nm.
Measurement of superoxide anion level and NADPH oxidase activity
Using a lucigenin-derived chemiluminescence method, superoxide anion levels and NADPH oxidase activity were measured as previously reported [26]. To examine superoxide anion levels, the photon emission was triggered by adding dark-adapted lucigenin (5 μM). To measure NADPH oxidase activity, photon emission was initiated by adding both dark-adapted lucigenin (5 μM) and NADPH (100 μM). Light emission was measured with a luminometer (Model 20/20 n, Turner, CA, USA) 10 times in 10 min. Background chemiluminescence was also measured in buffer containing lucigenin (5 μM). Mean light unit (MLU)·min-1·mg-1 protein represents the superoxide anion levels and NADPH oxidase activity in the samples.
Cell apoptosis assay
To quantify the rate of apoptosis, an Annexin V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) cell apoptosis kit was used according to the manufacturer’s instructions (Vazyme Biotech Co.,Ltd, Nanjing, China). In brief, the cells were washed twice with PBS buffer (pH 7.4), and resuspended in 100 μL of binding buffer. Subsequently, 5 μL of Annexin V/FITC and 5 μL of PI were mixed with the VSMCs. After 10 min of incubation at room temperature, 400 μL of binding buffer was added to a flow tube, and the cells were analyzed using a FACSCalibur flow cytometer (BD Biosciences, USA). The percentage of apoptotic cells is indicated by the sum of the numerical values represented in the upper right and lower right quadrants. The cell apoptosis rate was equivalent to the average apoptosis rate from five flow cytometry analyses.
Hematoxylin and eosin staining and Masson’s staining
Sections of aortas and mesenteric arteries (MAs) from SHRs were dissected and stained with hematoxylin and eosin or Masson’s trichrome staining, as previously reported [17]. All images were captured with a light microscope (BX-51, Olympus, Tokyo, Japan). Quantitative analysis was performed with ImageJ software. Vascular remodeling was evaluated based on the media thickness, the lumen diameter, the ratio of media thickness to lumen diameter and intima-media thickness (IMT).
Blood pressure measurement
The blood pressure of the tail artery was examined in conscious SHRs with a noninvasive computerized tail cuff system (NIBP, ADInstruments, Sydney, Australia). The blood pressure and heart rate values were calculated by averaging six measurements.
Small interfering RNA transfection
VSMCs were pre-treated with specific small interfering RNA (siRNA) against ELA (ELA-siRNA). The ELA-specific siRNA (sense sequence: 5′-CACGGAAGAGAAATCAGTT-3′) was purchased from RiboBio (Guangzhou, China). Negative siRNAs (NC-siRNA) with no sequence homology to any known rat genes were used as a control. VSMCs were transfected with 50 nM siRNA using Lipofectamine 3000 reagent (Invitrogen). To examine the knockdown efficiencies, cells were lysed 48 h after transfection, and ELA expression was analyzed.
Osmotic minipumps infusion
For ELA infusion, an Alzet osmotic pump (Model 2004, DURECT) was subcutaneously implanted over the scapula in SHRs to infuse ELA-21 (6 nmol/d, 1 nmol/μL) or saline for 4 weeks, as previously reported [17].
Chemicals
ELA-21 and F13A were obtained from Phoenix Pharmaceuticals (Belmont, USA). LY294002 was obtained from Sigma Chemical Co. (St Louis, USA), and 740-YP was purchased from MedChem Express (Greenville, USA).
Statistical analysis
All data are expressed as the mean ± SEM. Student’s t test was used to compare differences between two groups. One-way or two-way ANOVA followed by the Bonferroni test for post hoc analysis was used for multiple comparisons. A value of P < 0.05 was considered statistically significant.
Results
ELA expression was downregulated in VSMCs of SHRs
We reported that peripheral plasma ELA levels were significantly decreased in SHRs compared with WKYs [17]. A recent study showed that APJ protein expression was increased, while apelin protein expression was reduced in the VSMCs of SHRs compared with those of WKYs, which suggested that apelin/APJ may play an important role in regulating VSMCs [27]. In the present study, we found that ELA expression was downregulated in the VSMCs of SHRs (Fig. 1a), suggesting that ELA may also be involved in regulating VSMCs.
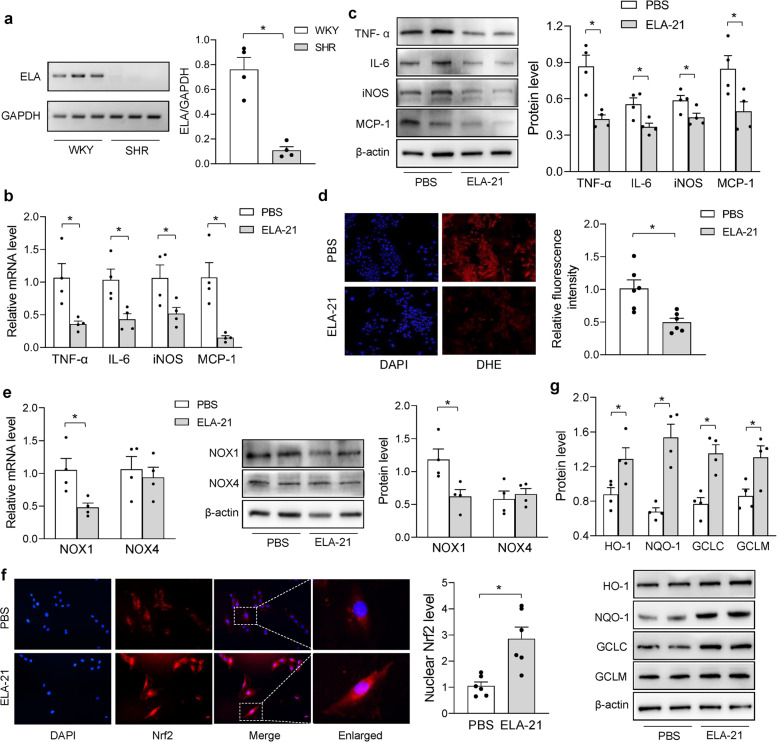
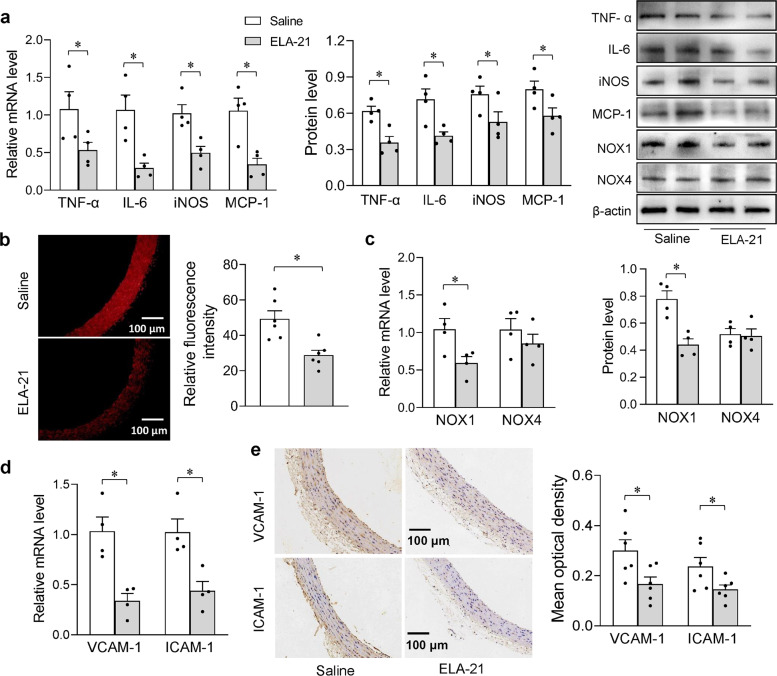
Fig. 1. ELA-21 alleviated VSMC inflammation and oxidative stress of SHRs.
a ELA expression in VSMCs of WKY and SHR determined by semi-quantitative PCR. b, c inflammatory cytokines mRNA and protein level in SHR-VSMCs. d DHE fluorescence staining for detecting reactive oxygen species (ROS) in SHR-VSMCs. e NOX1, NOX4 mRNA and protein level in SHR-VSMCs. f Nuclear Nrf2 expression determined by immunofluorescent staining in SHR-VSMCs. g Nrf2 downstream protein (HO-1, NQO-1, GCLC and GCLM) expression in SHR-VSMCs. The measurements were made 24 h after ELA-21 (200 nM) was added to the medium of SHR-VSMCs. n = 4 per group in a–c, e and g; n = 6 per group in d and f. Values are mean ± SEM. *P < 0.05.
ELA-21 attenuated VSMC inflammation and oxidative stress in SHRs
To assess the roles of ELA in hypertension, we first investigated the effects of ELA-21 on VSMC inflammation and oxidative stress in SHRs. Western blot and qRT-PCR revealed downregulated expression of proinflammatory cytokines, such as TNF-α, IL-6, MCP-1 and iNOS, in the ELA-21-treated VSMCs of SHRs (Fig. 1b, c). DHE staining showed that ROS production in SHR-VSMCs was also attenuated by ELA-21 (Fig. 1d). Using a lucigenin-derived chemiluminescence method, we found that ELA-21 reduced superoxide anion production and NADPH oxidase activity in SHR-VSMCs (Supplementary Fig. 1). Furthermore, ELA-21 decreased the mRNA and protein levels of NOX1 but not NOX4 (Fig. 1e). Nrf2 is considered to be a cytoprotective factor that regulates the expression of genes that code for anti-oxidative and anti-inflammatory responses [28, 29]. Activated Nrf2 translocates from the cytoplasm to the nucleus, and then promotes the transcription and subsequent expression of Nrf2-dependent antioxidant genes, including HO-1, NQO1, GCLC and GCLM. Immunofluorescence staining revealed that ELA-21 significantly increased nuclear Nrf2 expression in SHR-VSMCs (Fig. 1f). Moreover, the expression of the Nrf2 downstream genes HO-1, NQO-1, GCLC and GCLM was also upregulated in SHR-VSMCs after ELA-21 administration (Fig. 1g and Supplementary Fig. 2a). Together, these results confirmed the anti-oxidant and anti-inflammatory effects of ELA-21 on the VSMCs of SHRs.
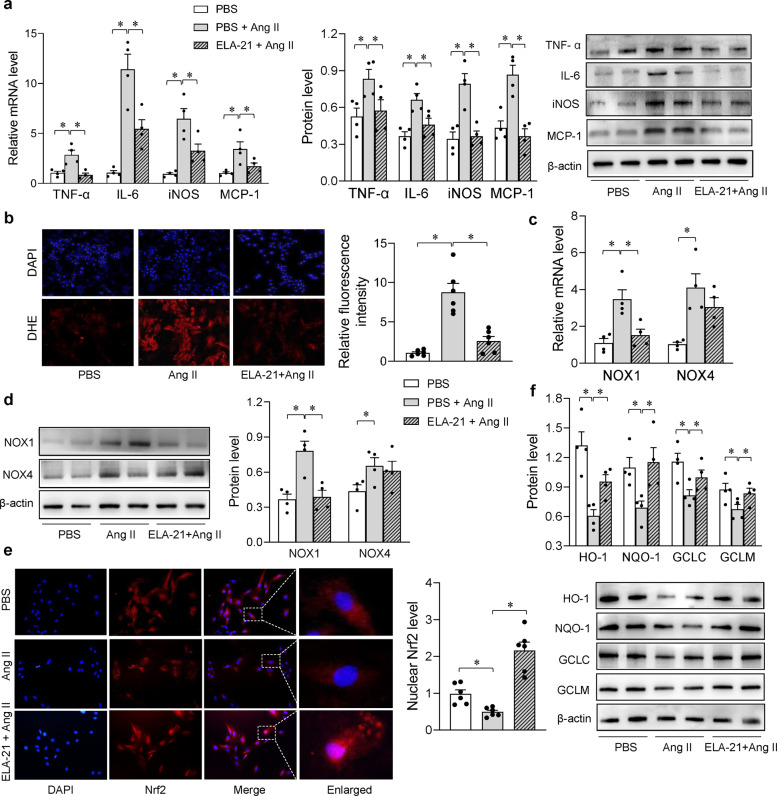
ELA-21 alleviated Ang II-induced VSMC inflammation and oxidative stress in WKYs
Ang II can bind to the Ang II type 1 receptor and activate NADPH oxidase to promote ROS generation, which induces VSMC proliferation [30, 31]. Thus, Ang II is widely used to induce a model of VSMC proliferation in vitro. The beneficial effects of ELA-21 on SHR-VSMCs prompted us to investigate whether exogenous ELA-21 plays similar roles in Ang II-induced WKY-VSMCs. As shown in Fig. 2a, inflammatory cytokines were upregulated in Ang II-treated WKY-VSMCs, while ELA-21 significantly inhibited inflammatory responses. Similarly, ROS production was increased in Ang II-treated WKY-VSMCs but was attenuated by ELA-21 (Fig. 2b). Furthermore, ELA-21 inhibited the Ang II-induced upregulation of NOX1 expression but not NOX4 expression (Fig. 2c, d). On the other hand, Ang II reduced nuclear Nrf2 expression and Nrf2 downstream gene (HO-1, NQO-1, GCLC and GCLM) expression in WKY-VSMCs, whereas ELA-21 prevented this downregulation (Fig. 2e, f; Supplementary Fig. 2b). These findings confirmed the anti-oxidative and anti-inflammatory effects of ELA-21 on Ang II-treated VSMCs of WKYs.
Fig. 2. ELA-21 alleviated Ang II-induced VSMC inflammation and oxidative stress of WKYs.
a Inflammatory cytokines mRNA and protein level in WKY-VSMCs. b DHE fluorescence staining for detecting reactive oxygen species (ROS) in WKY-VSMCs. c, d NOX1, NOX4 mRNA and protein level in WKY-VSMCs. e Nuclear Nrf2 expression determined by immunofluorescent staining in WKY-VSMCs. f Nrf2 downstream protein (HO-1, NQO-1, GCLC and GCLM) expression. The cells were treated with ELA-21 (200 nM) for 2 h followed by Ang II (100 nM) for 24 h in WKY-VSMCs. n = 4 per group in a, c, d and f; n = 6 per group in b and e. Values are mean ± SEM. *P < 0.05.
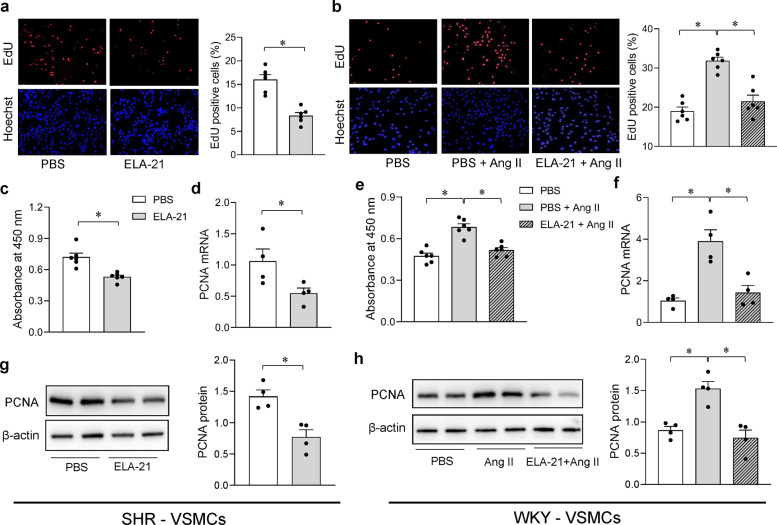
ELA-21 inhibited VSMC proliferation in SHRs
Since the effects of ELA-21 on VSMC inflammation and oxidative stress were confirmed, we further examined the effects of ELA-21 on VSMC proliferation. We used a CCK-8 kit, EdU assay and PCNA expression assay to evaluate VSMC proliferation. As shown in Fig. 3a, the number of EdU-positive cells was decreased following ELA-21 administration, suggesting that ELA-21 inhibited VSMC proliferation in SHRs. These inhibitory effects were further confirmed by CCK-8 assay and PCNA expression (Fig. 3c, d, g). Moreover, ELA-21 concentration-dependently inhibited VSMC proliferation in SHRs, which showed maximal effects at a concentration of 200 nM (Supplementary Fig. 3). As shown in Supplementary Fig. 4, ELA-21 had no significant effect on apoptosis in SHR-VSMCs using Annexin V/PI staining and flow cytometry analysis. The anti-oxidant and anti-inflammatory effects of ELA-21 might partially contribute to the inhibition of VSMC proliferation in SHRs.
Fig. 3. ELA-21 inhibited proliferation in SHR-VSMCs and Ang II-stimulated WKY-VSMCs.
The VSMC proliferation was evaluated with EdU-positive cells, CCK-8 kits and PCNA expression. a, b EdU-positive cells; c, e CCK-8 kits; d, f mRNA level of PCNA; g, h protein level of PCNA. For SHR-VSMCs, the cells were treated with ELA-21 (200 nM) for 24 h. For WKY-VSMCs, the cells were treated with ELA-21 (200 nM) for 2 h followed by Ang II (100 nM) for 24 h. n = 6 per group in a–c and e; n = 4 per group in d, f–h. Values are mean ± SEM. *P < 0.05.
ELA-21 inhibited Ang II-induced VSMC proliferation in WKYs
As shown in Fig. 3b, ELA-21 inhibited the Ang II-induced increase in the number of EdU-positive cells among WKY-VSMCs. Similarly, the CCK-8 assay revealed that AngII-induced VSMC proliferation was inhibited by ELA-21 (Fig. 3e). The anti-proliferative effects of ELA-21 were further confirmed by measuring PCNA expression (Fig. 3f, h).
ELA-21 inhibited extracellular matrix (ECM) degradation in SHR-VSMCs and Ang II-stimulated WKY-VSMCs
We next investigated the effects of ELA-21 on MMPs expression. It is known that the activation of MMPs plays a key role in extracellular matrix (ECM) degradation and vascular remodeling, thus facilitating VSMC proliferation and migration [32]. Of the MMP family members, MMP2 and MMP9 are central to vascular remodeling processes [33, 34]. As indicated in Supplementary Fig. 5, ELA-21 suppressed the expression of MMP2 and MMP9 in both SHR-VSMCs and Ang II-stimulated WKY-VSMCs, suggesting that ELA-21 inhibited ECM degradation.
ELA knockdown intensified Ang II-induced VSMC inflammation, oxidative stress and proliferation in WKYs
Given that exogenous ELA-21 exhibited anti-oxidative, anti-inflammatory and anti-proliferative effects, we further investigated the effects of ELA knockdown on Ang II-induced VSMC inflammation, oxidative stress and proliferation. The downregulation of ELA expression confirmed the effectiveness of siRNA-mediated ELA knockdown, while Ang II reduced ELA mRNA expression in VSMCs (Supplementary Fig. 6). ELA knockdown exacerbated Ang II-induced VSMC inflammation, as evidenced by the upregulated expression of inflammatory genes (Supplementary Fig. 7a, b). ELA knockdown had no significant effect on NOX4 expression but aggravated Ang II-induced NOX1 upregulation in VSMCs (Supplementary Fig. 7c). Moreover, Ang II-induced VSMC proliferation was intensified by ELA knockdown (Supplementary Fig. 7d).
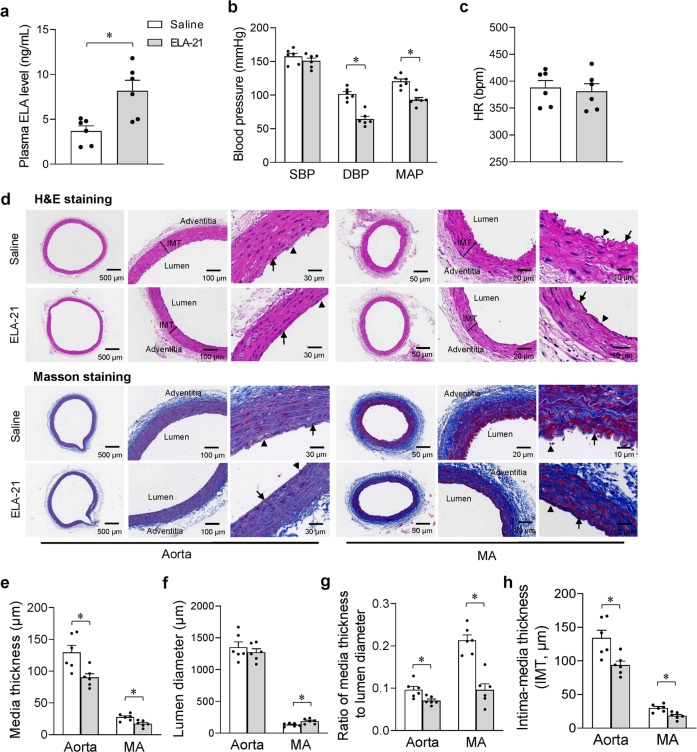
ELA-21 infusion lowered blood pressure and attenuated vascular remodeling in SHRs
We next aimed to assess the in vivo effects of ELA-21 on hypertension and vascular remodeling. Long-term administration of ELA-21 was attained by osmotic minipump infusion for 4 weeks. The effectiveness of ELA-21 infusion was confirmed by the increased plasma ELA levels in SHRs (Fig. 4a). Importantly, plasma ELA levels in SHRs with ELA-21 infusion were close to the endogenous levels of WKYs, suggesting that the dose we used for infusion achieved a physiological level to exert its effects (Supplementary Fig. 8). Chronic ELA-21 infusion reduced diastolic blood pressure (DBP) and MAP but not systolic blood pressure (SBP) or heart rate (HR) in SHRs (Fig. 4b, c). Representative photographs of the hematoxylin and eosin-stained and Masson-stained arteries are shown in Fig. 4d. Media thickness (M), lumen diameter (L), M/L and intima-media thickness (IMT) were used as indices of vascular remodeling [35, 36]. The media thickness, M/L and IMT of the aortas and MAs of SHRs were decreased by long-term administration of ELA-21, suggesting that vascular remodeling in SHRs was significantly attenuated (Fig. 4e–h).
Fig. 4. ELA-21 infusion for 4 weeks attenuated vascular remodeling and lowered blood pressure in SHRs.
a ELA level in plasma determined by ELISA; b, c systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and heart rate (HR) in a conscious state; d representative photographs of aorta and mesenteric artery (MA) by hematoxylin and eosin staining and Masson’s staining; e–h media thickness, lumen diameter, ratio of media thickness to lumen diameter and intima-media thickness (IMT) in aorta and MA. Arrows indicate the internal elastic lamina (IEL); Arrowhead denotes the endothelial cells. IMT is defined as the distance from endothelium to media-adventitia transition. n = 6 per group. Values are mean ± SEM. *P < 0.05.
ELA-21 infusion attenuated vascular inflammation and oxidative stress in SHRs
To further explore the potential mechanisms of ELA-21 in the context of hypertension and vascular remodeling, we examined whether ELA-21 had beneficial effects on vascular inflammation and oxidative stress in SHRs. Chronic administration of ELA-21 attenuated vascular inflammation, as reflected by decreased mRNA and protein expression of inflammatory cytokines in the aortas (Fig. 5a). Compared with saline infusion, ELA-21 infusion significantly reduced ROS production and downregulated NOX1 expression in the aortas of SHRs (Fig. 5b, c). In response to inflammatory mediators, vascular endothelial cells promote inflammatory changes, which increase leukocyte adhesion and promote the expression of different combinations of leukocyte adhesion molecules including VCAM-1 and ICAM-1. As shown in Fig. 5d, e, both VCAM-1 and ICAM-1 were greatly reduced in the aortas after ELA-21 infusion. Taken together, these findings indicate that chronic ELA-21 infusion attenuates vascular inflammation and oxidative stress, partially contributing to the beneficial effects of ELA-21 on vascular remodeling in SHRs.
Fig. 5. ELA-21 infusion for 4 weeks attenuated vascular inflammation and oxidative stress in SHRs.
a Inflammatory cytokines mRNA and protein level in aorta; b ROS detected by dihydroethidium (DHE) staining in aorta; c NOX1 and NOX4 mRNA and protein level in aorta; d VCAM-1 and ICAM-1 gene expression in aorta; e immunohistochemical staining of VCAM-1 and ICAM-1 in aorta. Brown deposits indicate positive staining; n = 4 per group in a, c, d; n = 6 per group in b and e. Values are mean ± SEM. *P < 0.05.
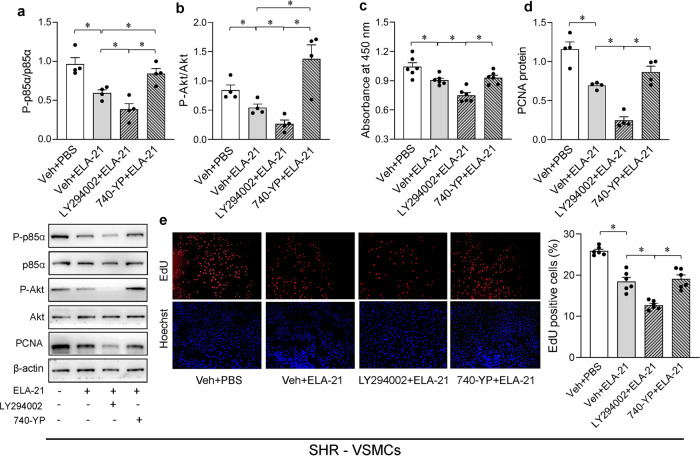
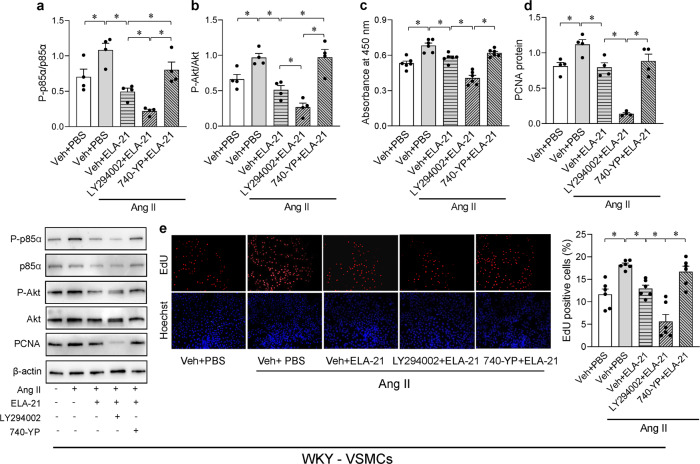
The PI3K/Akt pathway regulated the effects of ELA-21 on VSMC proliferation
The PI3K/Akt pathway transduces signals to trigger cell proliferation [37]. Our previous study confirmed the role of the PI3K/Akt pathway in the effects of central ELA-21 on hypertension [17]. Hence, to further establish whether the PI3K/Akt pathway is involved in the effects of ELA-21 on VSMC proliferation, cells were treated with the PI3K/Akt inhibitor LY294002 or activator 740-YP, and then with ELA-21, and the effects on VSMC proliferation and PI3K/Akt phosphorylation were examined. As shown in Fig. 6a, b, SHR-VSMCs treated with ELA-21 alone inhibited PI3K-p85α and Akt phosphorylation. This inhibition was abolished by 740-YP but was amplified by LY294002. Similarly, Ang II-induced PI3K/Akt activation was significantly attenuated by ELA-21, while LY294002 augmented and 740-YP abolished ELA-21-induced PI3K/Akt inhibition in WKY-VSMCs (Fig. 7a, b). Moreover, the inhibitory effects of ELA-21 on VSMC proliferation (determined by EdU staining, CCK-8 assay and PCNA expression) were further amplified by LY294002 in both SHR-VSMCs and Ang II-treated WKY-VSMCs (Figs. 6c–e and 7c–e), suggesting that the PI3K/Akt pathway mediated the effects of ELA-21 on VSMC proliferation.
Fig. 6. PI3K/Akt pathway mediated the effects of ELA-21 on VSMC proliferation of SHRs.
a, b Phosphoinositide 3-kinase (PI3K) p85α and Akt phosphorylation in SHR-VSMCs; VSMC proliferation were evaluated with CCK-8 kits (c), PCNA expression (d) and EdU-positive cells (e). The PI3K/Akt inhibitor LY294002 (10 μM) and activator 740-YP (10 μM) were added into the medium 0.5 h before administration of ELA-21 (200 nM). The measurements were made 24 h after ELA-21 treatment. n = 4 per group in a, b and d; n = 6 per group in c and e. Values are mean ± SEM. *P < 0.05.
Fig. 7. PI3K/Akt pathway mediated the effects of ELA-21 on Ang II-induced VSMC proliferation of WKYs.
a, b Phosphoinositide3-kinase (PI3K) p85α and Akt phosphorylation in WKY-VSMCs; VSMC proliferation were evaluated with CCK-8 kits (c), PCNA expression (d) and EdU-positive cells (e). The PI3K/Akt inhibitor LY294002 (10 μM) and activator 740-YP (10 μM) were added into the medium 0.5 h before administration of ELA-21 (200 nM). The cells were treated with ELA-21 for 2 h followed by Ang II (100 nM) for 24 h in WKY-VSMCs. n = 4 per group in a, b and d; n = 6 per group in c and e. Values are mean ± SEM. *P < 0.05.
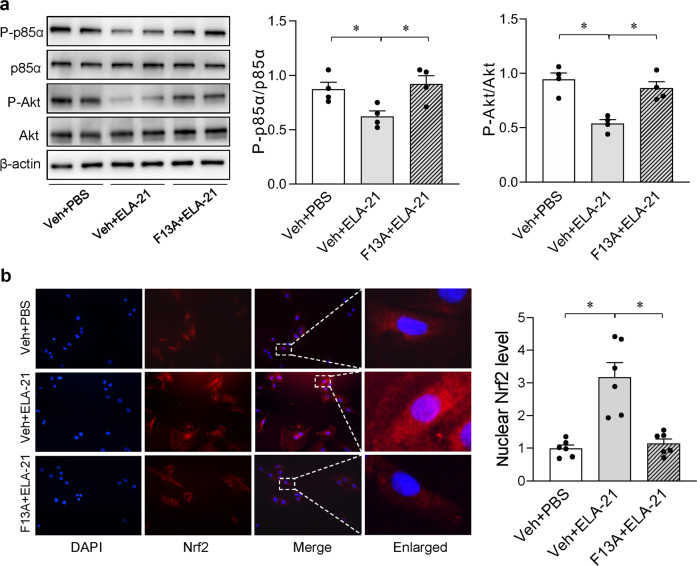
ELA-21 activated Nrf2 and inhibited the PI3K/Akt signaling through APJ
We further investigated whether the effects of ELA-21 were APJ-dependent. As shown in Fig. 8, ELA-21-induced inhibition of PI3K/Akt and activation of Nrf2 in SHR-VSMCs were abolished by pretreatment with the APJ receptor antagonist F13A. Taken together, these findings indicate that ELA-21-induced Nrf2 activation and PI3K/Akt inhibition were mediated by the APJ receptor.
Fig. 8. ELA-21 inhibited PI3K/Akt pathway and activated Nrf2 through APJ receptor in SHR-VSMCs.
a Phosphoinositide3-kinase (PI3K) p85α and Akt phosphorylation. b nuclear Nrf2 expression determining by immunofluorescent staining. APJ receptor antagonist F13A (1 μM) was added into the medium 0.5 h before administration of ELA-21 (200 nM) in SHR-VSMCs. The measurements were made 24 h after ELA-21 treatment. n = 4 in a, and n = 6 in b. Values are mean ± SEM. *P < 0.05.
Discussion
Increased oxidative stress and proinflammatory cytokine production induce VSMC proliferation and subsequent pathological vascular remodeling. Therefore, suppression of vascular inflammation, oxidative stress and VSMC proliferation may curb the development of hypertension. In the present study, the association of ELA-21 with VSMC proliferation was first examined. The intriguing finding shows that exogenous ELA-21 alleviates inflammation, oxidative stress and proliferation in VSMCs, which may contribute to protection against vascular remodeling in the context of hypertension. Furthermore, the effects of ELA-21 on PI3K/Akt inhibition and Nrf2 activation were APJ-dependent.
It is well known that inhibiting excessive VSMC proliferation is beneficial for attenuating vascular remodeling and hypertension [38]. ELA expression was downregulated in VSMCs of SHRs, while exogenous ELA-21 inhibited VSMC proliferation in SHR-VSMCs. Moreover, Ang II reduced ELA expression in VSMCs, while ELA-21 prevented Ang II-induced VSMC proliferation. These findings indicate that the downregulation of ELA may induce VSMC proliferation in both SHR-VSMCs and Ang II-treated WKY-VSMCs. Exogenous ELA-21 attenuated, while ELA knockdown enhanced VSMC proliferation, indicating that ELA may inhibit VSMC proliferation. More importantly, chronic administration of ELA-21 in SHRs alleviated vascular remodeling in the aortas and MAs of SHRs, which provided in vivo evidence of the effects of ELA-21. Taken together, these findings confirmed that the downregulation of ELA in VSMCs plays important roles in the development of vascular remodeling and hypertension in SHRs.
Extensive inflammation and oxidative stress are critical events in the occurrence and development of hypertension and cardiovascular complications. NADPH oxidases, which are the main source of ROS in the vasculature, can be activated by Ang II to promote ROS generation and subsequent VSMC inflammation and proliferation [30]. We found that Ang II-induced inflammation and NOX1 upregulation were dampened by ELA-21 but exacerbated by ELA knockdown in VSMCs. These observations were also supported by an in vivo study in which ELA-21 infusion alleviated vascular inflammation, NOX1 expression and ROS production but had no significant effect on NOX4 upregulation in the aortas of SHRs. In the antioxidant defense system, Nrf2 is one of the most important transcription factors that regulates multiple antioxidants [39]. Evidence has shown that NOX1 inhibition reduces ROS generation and reverses diabetes-induced downregulation of Nrf2 expression in VSMCs [40]. Considering the association between NOX1 and Nrf2 and our finding that ELA-21 upregulated nuclear Nrf2 expression in SHR-VSMCs, we hypothesize that ELA-21 may attenuate oxidative stress through NOX1 inhibition and subsequent Nrf2 activation.
Accumulating evidence has shown that the endogenous ELA homolog apelin regulates oxidative stress and inflammation by binding to its receptor APJ. However, whether this regulation is beneficial remains controversial. Foussal et al. reported that apelin reduces oxidative stress and prevents pressure overload-induced left ventricular hypertrophy [41]. In contrast, evidence has also shown that apelin induces cardiac hypertrophy by increasing ROS production and NADPH oxidase expression [42, 43]. Unlike those about apelin, studies about ELA are limited. In the present study, we first revealed that ELA-21 inhibited VSMC proliferation, which partially contributed to the attenuation of vascular remodeling and hypertension in SHRs. Our data are consistent with those in a previous study showing that ELA represses the NADPH oxidase/ROS/NLRP3 pathway to attenuate DOCA/salt-induced hypertension [44]. The researchers demonstrated that the antihypertensive effect of ELA did not rely on the G protein-coupled receptor APJ. A similar report also showed that ELA can function independently of APJ [45]. However, in the present study, we found that the PI3K/Akt pathway mediated the anti-proliferative effects of ELA-21, and ELA-21-mediated PI3K/Akt inhibition in SHR-VSMCs was abolished by pretreatment with the APJ receptor antagonist F13A. These findings indicate that the anti-proliferative effect of ELA-21 is mediated by APJ. Importantly, F13A also abolished ELA-21-induced Nrf2 activation. Therefore, we provide evidence that the protective effects of ELA-21 rely on APJ-mediated PI3K/Akt inhibition and Nrf2 activation. The limitations of our study are that we did not complete the in vivo studies including whether Akt inhibition or Nrf2 activation are essential for ELA-21-mediated protective effects.
It is noteworthy that plasma ELA levels in SHRs with ELA-21 infusion were close to endogenous levels of WKYs, suggesting that the dose of ELA-21 used in this study achieved physiological levels. In our previous study, we found that plasma ELA levels were significantly decreased in SHRs compared with that in WKYs. Here, we first showed that the increase in ELA-21 in SHRs exerted beneficial effects on vascular remodeling, vascular inflammation and oxidative stress. Furthermore, ELA was downregulated in both SHR-VSMCs and Ang II-treated WKY-VSMCs, while exogenous ELA-21 significantly attenuated inflammation, oxidative stress and proliferation in VSMCs in the context of hypertension. Taken together, these findings further support our hypothesis that ELA downregulation is involved in the development of hypertension.
Long-term administration of ELA-21 reduced DBP and MAP but had no significant effect on SBP. DBP is controlled by vessel contraction. In contrast, SBP is mainly governed by cardiac output. We observed significant attenuation of vascular remodeling in MAs than in the aortas in the present study, indicating that ELA-21 mainly acts on resistance vessels and modulates peripheral vascular resistance through its beneficial effects on pathological vascular remodeling. Moreover, ELA-21 infusion caused a slight decrease in SBP, but there was no significant difference. We hypothesize that 4 weeks may have been too brief to show a significant difference in SBP in the present study. Future studies are needed to investigate whether a longer time of ELA infusion can induce a significant decrease in SBP.
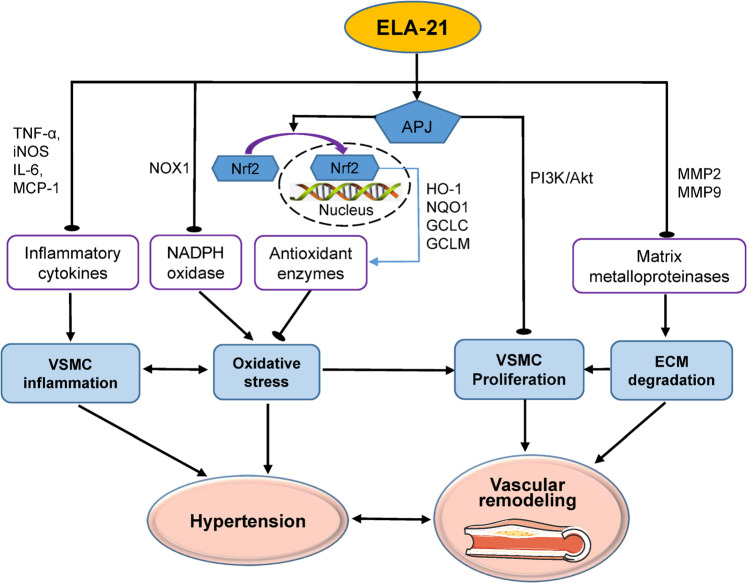
In summary, we have uncovered critical roles of ELA-21 in VSMC proliferation, inflammation, oxidative stress and vascular remodeling (Fig. 9). ELA expression was downregulated in the VSMCs of SHRs. Exogenous ELA-21 inhibited oxidative stress and inflammation in VSMCs, attenuating VSMC proliferation and pathological vascular remodeling in the context of hypertension. ELA-21 therefore represents an attractive therapeutic agent in the treatment of hypertension and related cardiovascular diseases.
Fig. 9. Schematic diagram showing that ELA-21 exerted its protective function on VSMCs via inhibiting inflammation, oxidative stress and proliferation, which contributed to the attenuated vascular remodeling in hypertension.
VSMCs vascular smooth muscle cells, ELA ELABELA, NOX1 NADPH oxidase 1, Nrf2 nuclear factor erythroid 2-related factor, TNF-α tumor necrosis factor-α, IL-6 interleukin-6, MCP-1 monocyte chemoattractant protein-1, iNOS inducible nitric oxide synthase. MMP2 matrix metalloproteinase 2, MMP9 matrix metalloproteinase 9, HO-1 heme oxygenase-1, NQO1 NADPH quinone oxidoreductase 1, GCLC glutamate cysteine ligase catalytic subunit, GCLM glutamate cysteine ligase modulatory subunit, ECM extracellular matrix.
Supplementary information
Acknowledgements
The authors thank the generous support of Collaborative Innovation Center for Cardiovascular Disease Translational Medicine. This work was supported by National Nature Science Foundation of China (81600323 & 81970356).
Author contributions
CY and XQX planned the experiment. CY, ZG, LLZ and FZ performed the experiments. YBZ and CY analyzed the data. XQX and GQZ wrote the paper. All authors read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Chao Ye and Zhi Geng
Supplementary information
The online version contains supplementary material available at 10.1038/s41401-022-00875-w.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Touyz RM, Rios FJ, Alves-Lopes R, Neves KB, Camargo LL, Montezano AC. Oxidative stress: a unifying paradigm in hypertension. Can J Cardiol. 2020;36:659–70.. doi: 10.1016/j.cjca.2020.02.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrison DG. The mosaic theory revisited: common molecular mechanisms coordinating diverse organ and cellular events in hypertension. J Am Soc Hypertens. 2013;7:68–74. doi: 10.1016/j.jash.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das S, Zhang E, Senapati P, Amaram V, Reddy MA, Stapleton K, et al. A novel angiotensin II-induced long noncoding RNA giver regulates oxidative stress, inflammation, and proliferation in vascular smooth muscle cells. Circ Res. 2018;123:1298–312.. doi: 10.1161/CIRCRESAHA.118.313207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun HJ, Ren XS, Xiong XQ, Chen YZ, Zhao MX, Wang JJ, et al. NLRP3 inflammasome activation contributes to VSMC phenotypic transformation and proliferation in hypertension. Cell Death Dis. 2017;8:e3074. doi: 10.1038/cddis.2017.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siti HN, Kamisah Y, Kamsiah J. The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review) Vasc Pharmacol. 2015;71:40–56. doi: 10.1016/j.vph.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Caillon A, Schiffrin EL. Role of inflammation and immunity in hypertension: recent epidemiological, laboratory, and clinical evidence. Curr Hypertens Rep. 2016;18:21. doi: 10.1007/s11906-016-0628-7. [DOI] [PubMed] [Google Scholar]
- 8.Ren XS, Tong Y, Qiu Y, Ye C, Wu N, Xiong XQ, et al. MiR155-5p in adventitial fibroblasts-derived extracellular vesicles inhibits vascular smooth muscle cell proliferation via suppressing angiotensin-converting enzyme expression. J Extracell Vesicles. 2020;9:1698795. doi: 10.1080/20013078.2019.1698795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ye C, Tong Y, Wu N, Wan GW, Zheng F, Chen JY, et al. Inhibition of miR-135a-5p attenuates vascular smooth muscle cell proliferation and vascular remodeling in hypertensive rats. Acta Pharmacol Sin. 2020;42:1798–807. doi: 10.1038/s41401-020-00608-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starke RM, Chalouhi N, Ding D, Raper DM, McKisic MS, Owens GK, et al. Vascular smooth muscle cells in cerebral aneurysm pathogenesis. Transl Stroke Res. 2014;5:338–46. doi: 10.1007/s12975-013-0290-1. [DOI] [PubMed] [Google Scholar]
- 11.Sena CM, Leandro A, Azul L, Seiça R, Perry G. Vascular oxidative stress: impact and therapeutic approaches. Front Physiol. 2018;9:1668. doi: 10.3389/fphys.2018.01668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu W, Yan J, Pan W, Tang M. Apelin/Elabela-APJ: a novel therapeutic target in the cardiovascular system. Ann Transl Med. 2020;8:243. doi: 10.21037/atm.2020.02.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ureche C, Tapoi L, Volovat S, Voroneanu L, Kanbay M, Covic A. Cardioprotective apelin effects and the cardiac-renal axis: review of existing science and potential therapeutic applications of synthetic and native regulated apelin. J Hum Hypertens. 2019;33:429–35.. doi: 10.1038/s41371-019-0163-5. [DOI] [PubMed] [Google Scholar]
- 14.Folino A, Montarolo PG, Samaja M, Rastaldo R. Effects of apelin on the cardiovascular system. Heart Fail Rev. 2015;20:505–18. doi: 10.1007/s10741-015-9475-x. [DOI] [PubMed] [Google Scholar]
- 15.Murza A, Sainsily X, Coquerel D, Côté J, Marx P, Besserer-Offroy É, et al. Discovery and structure-activity relationship of a bioactive fragment of ELABELA that modulates vascular and cardiac functions. J Med Chem. 2016;59:2962–72. doi: 10.1021/acs.jmedchem.5b01549. [DOI] [PubMed] [Google Scholar]
- 16.Yang P, Read C, Kuc RE, Buonincontri G, Southwood M, Torella R, et al. Elabela/Toddler is an endogenous agonist of the Apelin APJ receptor in the adult cardiovascular system, and exogenous administration of the peptide compensates for the downregulation of its expression in pulmonary arterial hypertension. Circulation. 2017;135:1160–73.. doi: 10.1161/CIRCULATIONAHA.116.023218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geng Z, Ye C, Tong Y, Zhang F, Zhou YB, Xiong XQ. Exacerbated pressor and sympathoexcitatory effects of central Elabela in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2020;318:H124–h34.. doi: 10.1152/ajpheart.00449.2019. [DOI] [PubMed] [Google Scholar]
- 18.Schreiber CA, Holditch SJ, Generous A, Ikeda Y. Sustained ELABELA gene therapy in high-salt diet-induced hypertensive rats. Curr Gene Ther. 2017;16:349–60.. doi: 10.2174/1566523217666161121111906. [DOI] [PubMed] [Google Scholar]
- 19.Sato T, Sato C, Kadowaki A, Watanabe H, Ho L, Ishida J, et al. ELABELA-APJ axis protects from pressure overload heart failure and angiotensin II-induced cardiac damage. Cardiovasc Res. 2017;113:760–9. doi: 10.1093/cvr/cvx061. [DOI] [PubMed] [Google Scholar]
- 20.Yang X, Gu D. Response by Yang and Gu to letter regarding article, “Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (prediction for ASCVD risk in China)”. Circulation. 2017;135:e822–e3.. doi: 10.1161/CIRCULATIONAHA.116.027159. [DOI] [PubMed] [Google Scholar]
- 21.Liu QF, Yu HW, Sun LL, You L, Tao GZ, Qu BZ. Apelin-13 upregulates Egr-1 expression in rat vascular smooth muscle cells through the PI3K/Akt and PKC signaling pathways. Biochem Biophys Res Commun. 2015;468:617–21. doi: 10.1016/j.bbrc.2015.10.171. [DOI] [PubMed] [Google Scholar]
- 22.Li L, Li L, Xie F, Zhang Z, Guo Y, Tang G, et al. Jagged-1/Notch3 signaling transduction pathway is involved in apelin-13-induced vascular smooth muscle cells proliferation. Acta Biochim Biophys Sin (Shanghai) 2013;45:875–81. doi: 10.1093/abbs/gmt085. [DOI] [PubMed] [Google Scholar]
- 23.Nolze A, Köhler C, Ruhs S, Quarch K, Strätz N, Gekle M, et al. Calcineurin (PPP3CB) regulates angiotensin II-dependent vascular remodelling by potentiating EGFR signalling in mice. Acta Physiol (Oxf). 2021;233:e13715. [DOI] [PubMed]
- 24.Ling L, Chen D, Tong Y, Zang YH, Ren XS, Zhou H, et al. Fibronectin type III domain containing 5 attenuates NLRP3 inflammasome activation and phenotypic transformation of adventitial fibroblasts in spontaneously hypertensive rats. J Hypertens. 2018;36:1104–14.. doi: 10.1097/HJH.0000000000001654. [DOI] [PubMed] [Google Scholar]
- 25.Liu TY, Shi CX, Gao R, Sun HJ, Xiong XQ, Ding L, et al. Irisin inhibits hepatic gluconeogenesis and increases glycogen synthesis via the PI3K/Akt pathway in type 2 diabetic mice and hepatocytes. Clin Sci. 2015;129:839–50. doi: 10.1042/CS20150009. [DOI] [PubMed] [Google Scholar]
- 26.Zheng F, Ye C, Wan GW, Zhou B, Tong Y, Lei JZ, et al. Interleukin-1β in hypothalamic paraventricular nucleus mediates excitatory renal reflex. Pflug Arch. 2020;472:1577–86.. doi: 10.1007/s00424-020-02461-7. [DOI] [PubMed] [Google Scholar]
- 27.Xu T, Jia J, Xu N, Ye C, Zheng F, Yuan Y, et al. Apelin receptor upregulation in spontaneously hypertensive rat contributes to the enhanced vascular smooth muscle cell proliferation by activating autophagy. Ann Transl Med. 2021;9:627. doi: 10.21037/atm-20-6891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loboda A, Damulewicz M, Pyza E, Jozkowicz A, Dulak J. Role of Nrf2/HO-1 system in development, oxidative stress response and diseases: an evolutionarily conserved mechanism. Cell Mol Life Sci. 2016;73:3221–47. doi: 10.1007/s00018-016-2223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merry TL, Ristow M. Nuclear factor erythroid-derived 2-like 2 (NFE2L2, Nrf2) mediates exercise-induced mitochondrial biogenesis and the anti-oxidant response in mice. J Physiol. 2016;594:5195–207. doi: 10.1113/JP271957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW. Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ Res. 1994;74:1141–8. doi: 10.1161/01.RES.74.6.1141. [DOI] [PubMed] [Google Scholar]
- 31.Gusan S, Anand-Srivastava MB. cAMP attenuates the enhanced expression of Gi proteins and hyperproliferation of vascular smooth muscle cells from SHR: role of ROS and ROS-mediated signaling. Am J Physiol Cell Physiol. 2013;304:C1198–209. doi: 10.1152/ajpcell.00269.2012. [DOI] [PubMed] [Google Scholar]
- 32.Seo KW, Lee SJ, Ye BH, Kim YW, Bae SS, Kim CD. Mechanical stretch enhances the expression and activity of osteopontin and MMP-2 via the Akt1/AP-1 pathways in VSMC. J Mol Cell Cardiol. 2015;85:13–24. doi: 10.1016/j.yjmcc.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Chase AJ, Newby AC. Regulation of matrix metalloproteinase (matrixin) genes in blood vessels: a multi-step recruitment model for pathological remodelling. J Vasc Res. 2003;40:329–43. doi: 10.1159/000072697. [DOI] [PubMed] [Google Scholar]
- 34.Hu J, Van den Steen PE, Sang QX, Opdenakker G. Matrix metalloproteinase inhibitors as therapy for inflammatory and vascular diseases. Nat Rev Drug Discov. 2007;6:480–98. doi: 10.1038/nrd2308. [DOI] [PubMed] [Google Scholar]
- 35.Fan ZD, Zhang L, Shi Z, Gan XB, Gao XY, Zhu GQ. Artificial microRNA interference targeting AT(1a) receptors in paraventricular nucleus attenuates hypertension in rats. Gene Ther. 2012;19:810–7. doi: 10.1038/gt.2011.145. [DOI] [PubMed] [Google Scholar]
- 36.Su YT, Cheng YP, Zhang X, Xie XP, Chang YM, Bao JX. Acid sphingomyelinase/ceramide mediates structural remodeling of cerebral artery and small mesenteric artery in simulated weightless rats. Life Sci. 2020;243:117253. doi: 10.1016/j.lfs.2019.117253. [DOI] [PubMed] [Google Scholar]
- 37.Liu B, Lin J, Bai L, Zhou Y, Lu R, Zhang P, et al. Paeoniflorin inhibits mesangial cell proliferation and inflammatory response in rats with mesangial proliferative glomerulonephritis through PI3K/AKT/GSK-3β pathway. Front Pharmacol. 2019;10:978. doi: 10.3389/fphar.2019.00978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Briet M, Schiffrin EL. Treatment of arterial remodeling in essential hypertension. Curr Hypertens Rep. 2013;15:3–9. doi: 10.1007/s11906-012-0325-0. [DOI] [PubMed] [Google Scholar]
- 39.Ruan H, Wang L, Wang J, Sun H. Sika deer antler protein against acetaminophen-induced oxidative stress and apoptosis in HK-2 cells via activating Nrf2/keap1/HO-1 pathway. J Food Biochem. 2019;43:e13067. [DOI] [PubMed]
- 40.Alves-Lopes R, Neves KB, Montezano AC, Harvey A, Carneiro FS, Touyz RM, et al. Internal pudental artery dysfunction in diabetes mellitus is mediated by NOX1-derived ROS-, Nrf2-, and Rho kinase-dependent mechanisms. Hypertension. 2016;68:1056–64. doi: 10.1161/HYPERTENSIONAHA.116.07518. [DOI] [PubMed] [Google Scholar]
- 41.Foussal C, Lairez O, Calise D, Pathak A, Guilbeau-Frugier C, Valet P, et al. Activation of catalase by apelin prevents oxidative stress-linked cardiac hypertrophy. FEBS Lett. 2010;584:2363–70. doi: 10.1016/j.febslet.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 42.Koguchi W, Kobayashi N, Takeshima H, Ishikawa M, Sugiyama F, Ishimitsu T. Cardioprotective effect of apelin-13 on cardiac performance and remodeling in end-stage heart failure. Circ J. 2012;76:137–44. doi: 10.1253/circj.CJ-11-0689. [DOI] [PubMed] [Google Scholar]
- 43.Xie F, Wu D, Huang SF, Cao JG, Li HN, He L, et al. The endoplasmic reticulum stress-autophagy pathway is involved in apelin-13-induced cardiomyocyte hypertrophy in vitro. Acta Pharmacol Sin. 2017;38:1589–600.. doi: 10.1038/aps.2017.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen Z, Wu C, Liu Y, Li H, Zhu Y, Huang C, et al. ELABELA attenuates deoxycorticosterone acetate/salt-induced hypertension and renal injury by inhibition of NADPH oxidase/ROS/NLRP3 inflammasome pathway. Cell Death Dis. 2020;11:698. doi: 10.1038/s41419-020-02912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen H, Wang L, Wang W, Cheng C, Zhang Y, Zhou Y, et al. ELABELA and an ELABELA fragment protect against AKI. J Am Soc Nephrol. 2017;28:2694–707.. doi: 10.1681/ASN.2016111210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.