Abstract
Aim
Tracheal intubation is a vital resuscitation procedure in the pediatric emergency department (ED). Despite its importance, little is known about the current status of emergency airway management in Japan. In this context, we aimed to investigate the airway management characteristics—particularly the location, patient, and provider factors—in the pediatric ED.
Methods
We conducted a multicenter, prospective study of five pediatric EDs in Japan from October 2018 to June 2020. The study included all children (aged ≤18 years) who underwent intubation at the pre‐ED or ED setting by physicians and those who were transferred from the ED to the operation room (OR) or pediatric intensive care unit (PICU) for intubation. We described the airway management characteristics according to the location, patient, and provider factors.
Results
Of 231 children, 9 (4%) were transferred to the OR or PICU for airway management. Among the remaining 222 children, 45 were intubated at the pre‐ED setting and 177 were intubated in the ED. The overall first‐attempt success rate was 72%, with the rate varying by location, patient, and provider factors—for example, 68% at the pre‐ED setting, 67% for children <2 years, 56% for children with airway‐related anatomical anomalies, and 61% with intubation by a resident physician. Intubation‐related adverse events were observed in 17%, most of which were hypoxemia (14%).
Conclusions
Based on data from a multicenter prospective study, the overall first‐attempt intubation success rate in pediatric EDs in Japan was 72%, with large variations by location, patient, and provider factors.
Keywords: Airway management, children, congenital anomaly, first attempt success, intubation
In this multicenter prospective observational study of 231 emergency department (ED) children in Japan, we found that the overall first‐attempt success rate was 72%. However, the rate varied across location, patients, and provider factors (e.g., 68% at the pre‐ED setting, 67% for children <2 years, 56% for children with airway‐related anatomical anomalies, and 61% with intubation by a resident physician). Implementing high‐quality airway management for patients with these factors is required in the pediatric emergency department.
INTRODUCTION
Emergency airway management is a critical resuscitation procedure in the pediatric emergency department (ED). Airway management in children demands great caution because of their age‐dependent differences in anatomical and physiological characteristics and limited physiological reserve. 1 Nevertheless, the frequency of pediatric patients undergoing emergency tracheal intubation in the pediatric ED is small (2–33/10,000 ED visits), 2 , 3 , 4 , 5 so we have often depended on findings from the operation room (OR) or pediatric intensive care unit (PICU). However, EDs have different characteristics from those settings, such as limited medical resources and time, so ED‐specific knowledge is required. 6 , 7 Recently, a large registry of general (i.e., nonpediatric) ED settings has revealed pediatric findings—variations in the intubation success rate by patient's age and provider training level. 6 , 8 , 9 , 10 , 11 Successful first‐attempt intubation is important because studies have shown that repeated intubations are associated with a higher rate of complications. 8 , 11
However, the characteristics of patients who present to the general ED differ from those in the pediatric ED. 12 For example, in Japan, high‐risk children—such as those with underlying medical conditions (e.g., congenital airway–related malformations, congenital heart diseases)—are rarely intubated by emergency physicians in the general ED. They are often referred directly to the pediatric ED of a children's hospital or tertiary hospital and are sometimes transferred by the pediatric transport team. Furthermore, in Japan, there is no board certification system for pediatric emergency medicine. Board‐certified physicians working in the pediatric ED are likely pediatricians, emergency physicians, or trainees in those fields. The impact of these factors on the intubation performance remains unclear.
To address the knowledge gap in the literature, we conducted a multicenter prospective study of airway management in pediatric EDs to elucidate the characteristics of children who undergo emergency airway management. We categorized these into three main factors: location, patient, and provider to investigate first‐attempt success rates. A better understanding of these important issues in ED children should inform the development of optimal airway management strategies and education systems.
METHODS
Study design, participants, and settings
This is an analysis of data from the 4th Japanese Emergency Airway Network (JEAN‐4) study. JEAN‐4 is an ongoing prospective multicenter study, which was initiated in October 2018 as a consortium of five pediatric EDs in the children's hospital or community medical centers in Japan (Aichi Children's Health and Medical Center, Gifu Prefectural General Medical Center, National Center for Child Health and Development, Saitama Children's Medical Center, and Tokyo Metropolitan Children's Medical Center). The number of annual ED visits in the participating institutions ranged from 5,300 to 34,000.
The JEAN‐4 study includes all children aged ≤18 years who underwent emergency tracheal intubation by a physician at the pre‐ED setting (e.g., during the patient transport) or in one of the EDs. JEAN‐4 also includes children who were considered as high risk for airway management in the ED and transferred to the OR or PICU for emergency tracheal intubation. The reason for including these cases was that it would be inadequate to represent the actual status of airway management in the ED without knowing the number and characteristics of such high‐risk cases that require emergent airway management—the target population of interest. Emergency tracheal intubation in this study was defined as tracheal intubation without prior planning. For this analysis, we analyzed the data of all children in JEAN‐4 from October 2018 to June 2020. The study was approved by the institutional review board of each participating center, including the Institutional Review Board of Tokyo Metropolitan Children's Medical Center, with the waiver of informed consent before data collection.
Data measurements
JEAN‐4 prospectively measures characteristics related to location, patients, health care providers, and airway management. A list of the variables measured is provided in Table 1. This study utilized the following measurements from this comprehensive registry of airway management. First, the location characteristics included the location of intubation (pre‐ED [other hospital/clinic to transport, transport vehicle, scene], ED). Second, the patient factors included age, sex, body weight, congenital diseases (airway‐related anatomical anomalies and circulatory physiological anomalies), and primary indication for intubation (Table 1, see section “C”). Bodyweight was either provided by parents or estimated by appearance prior to the emergency tracheal intubation. Third, the provider factors included intubator's level of training (resident, fellow, attending) and specialty (emergency medicine, pediatrics, critical care medicine, anesthesiology, others). A resident physician was defined as a trainee in the residency program, while a fellow was defined as an advanced‐level trainee who undergoes subspecialty training (pediatric emergency medicine, pediatric critical care medicine, pediatric hospital medicine, others) after completing his/her residency training. Lastly, the airway management characteristics included the methods of intubation, intubation devices, Cormack–Lehane classification, intubation outcome at each attempt, and intubation‐associated adverse events. An intubation attempt was defined as a single insertion of the laryngoscope (or other devices) past the teeth. 13 , 14 An intubation success was confirmed by quantitative or colorimetric end‐tidal carbon dioxide monitoring after the tracheal tube was placed through the vocal cords. 13 , 14 Adverse events were a priori defined as airway management–related events 15 : death, cardiac arrest, hypotension requiring intervention (fluid and/or vasopressors), hypoxemia, dysrhythmia, esophageal intubation with/without delayed recognition, vomiting with/without aspiration, main‐stem bronchial intubation, dental or lip trauma, airway trauma, and errors in drug administration. Hypoxemia was defined as pulse oximetry saturation <90% during an intubation attempt, not a result of esophageal intubation. In a patient with a circulatory physiological anomaly, hypoxemia was defined as a 10% decrease from the baseline value.
Table 1.
All measured variables in the 4th Japanese Emergency Airway Network (JEAN‐4) study
|
A. Basic information
B. Patient information
C. Primary indication of intubation (single answer)
D. Methods of airway management (multiple answer)
E. Predictors of difficult airway (yes, no, unknown)
F. Airway management characteristics (per every attempt)
G. Prognosis information
H. Free comment if necessary |
ED, emergency department; OR, operation room; PICU, pediatric intensive care unit.
Data analysis
This study described the following measurements: (i) patient characteristics (age, sex, weight, congenital diseases, primary indication), (ii) airway management characteristics (the location of intubation, intubator's level of training and specialty, methods of intubation, intubation devices, Cormack–Lehane classification), and (iii) intubation outcomes. In this study, we used descriptive statistics, including the median (with interquartile range) and the number with proportion, as appropriate. We also examined the intubation success rates (with 95% confidence intervals [95% CIs]) according to the number of attempts, by location, patient, and provider factors. We performed all statistical analyses with JMP 9 software (SAS Institute, Inc, Cary, NC, USA).
RESULTS
Location factors of emergency airway management
During the 21‐month period, 231 children were enrolled in the JEAN‐4 study (capture rate, 100%). The location of intubation in these patients is summarized in Fig. 1. Most patients (n = 222, 96%) were intubated in the pre‐ED (n = 44, 19%) or ED (n = 178, 77%) setting. A total of 9 (4%) children were transferred from the ED to the OR or PICU for airway management.
Fig. 1.
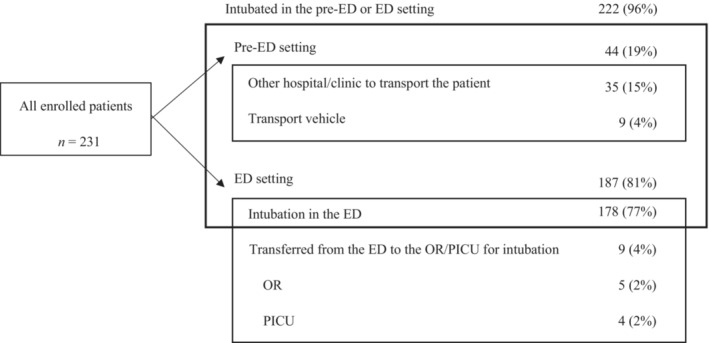
Flow of study children who underwent emergency airway management. The 4th Japanese Emergency Airway Network (JEAN‐4) study enrolled 231 children (aged ≤ 18 years) who underwent intubation at the pre‐emergency department (ED) or ED setting by physicians and those who were considered as high risk and transferred from the ED to the operation room (OR) or pediatric intensive care unit (PICU) for intubation. All data are presented as n (%).
Patient factors of emergency airway management
The patient demographics and primary indications for intubation are shown in Table 2. The median age was 1 year (interquartile range, 0–4 years), and 56% were boys. Overall, 14% of children had congenital diseases (airway‐related anatomical anomalies [11%], circulatory physiological anomalies [5%]). The medical indication accounted for 84%, and the remaining (16%) children were intubated for trauma or other injuries. The most common indication was respiratory failure (26%), followed by seizure (23%) and medical or traumatic cardiac arrest (13%). In addition, all five patients transferred to the OR were for the management of upper airway obstruction, while those transferred to the PICU were intubated for respiratory failure (n = 2) and cardiogenic shock (n = 2).
Table 2.
Patient characteristics and primary indication for intubation in children who underwent emergency airway management (N = 231)
| Characteristics | Value |
|---|---|
| Age (year), median (interquartile range) | 1 (0–4) |
| Boys, n (%) | 129 (56) |
| Weight (kg), median (interquartile range) | 10 (6–16) |
| Congenital diseases, n (%) | 33 (14) |
| Airway‐related anatomical anomalies † | 25 (11) |
| Circulatory physiological anomalies ‡ | 12 (5) |
| Primary indication, n (%) | |
| Medical (nontrauma) indication | 195 (84) |
| Respiratory failure | 61 (26) |
| Seizure | 53 (23) |
| Cardiac arrest | 24 (10) |
| Altered mental status (excluding seizure) | 17 (7) |
| Airway obstruction | 11 (5) |
| Frequency apnea | 11 (5) |
| Shock (noncardiac) | 9 (4) |
| Shock (cardiac) | 4 (2) |
| Airway management for elective procedures or transport | 2 (1) |
| Asthma | 2 (1) |
| Anaphylaxis | 1 (0.4) |
| Trauma indication | 36 (16) |
| Airway management for elective procedures or transport | 12 (5) |
| Head trauma | 11 (5) |
| Cardiac arrest (trauma) | 4 (2) |
| Cardiac arrest (drowning or choking) | 3 (1) |
| Face or neck trauma | 2 (1) |
| Shock (trauma) | 2 (1) |
| Multiple trauma | 2 (1) |
Congenital malformation syndrome or tracheal and bronchial stenosis.
Glenn–Fontan circulation, right‐to‐left shunt, or pulmonary hypertension.
Airway management characteristics and provider factors
Most initial intubation was performed by fellows (62%), while attending and resident physicians performed 22% and 16% of intubations, respectively. Specific in the pre‐ED setting, fellows (pediatric emergency medicine, pediatric critical care medicine) and attendings accounted for 98% of the total. Emergency medicine (including pediatric emergency medicine) was the most common specialty of intubators (61%), followed by pediatrics (31%), critical care medicine (5%), and anesthesiology (3%). The most common method of initial intubation attempt was rapid sequence intubation (69%). The devices used for initial intubation were a direct laryngoscope in 74%, while a video laryngoscope was used in 26%. There was no fiberoptic intubation or surgical airway management. Approximately three‐fourths of Cormack–Lehane classifications were grade 1, while 8% comprised grade 4.
Airway management outcomes
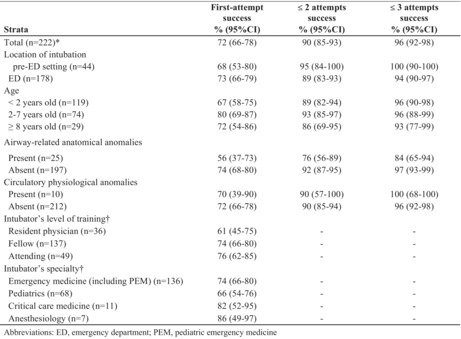
Table 3 presents the success rates by location, patient, and provider factors. Overall, the first‐attempt success rate was 72% (95% CI 66%–78%). The success rate within two attempts was 90% (95% CI 85%–93%), and that within three attempts was 96% (95% CI 92%–98%). The success rate varied widely by location, patient, and provider factors. For example, the first‐attempt success rate was 68% (95% CI 53%–80%) in the pre‐ED setting, whereas it was 73% (95% CI 66%–79%) in the ED setting. Furthermore, the first‐attempt success rate varied by age—for example, 67% (95% CI 58%–75%) in age <2 years versus 80% (95% CI 69%–87%) in age 2–7 years. Likewise, the first‐attempt success rate was low in children with an airway‐related anatomical anomaly (56%; 95% CI 37%–73%), with persistently low rates across the following attempts (e.g., 84% [95% CI 65%–94%] within three attempts). Lastly, the first‐attempt success rate varied by the level of training—for example, 61% (95% CI 45%–75%) by resident physicians versus 76% (95% CI 62%–85%) by attending physicians.
Table 3.
Success rates by location, patient, and provider factors in children who underwent intubation in the ED or pre‐ED setting
| First‐attempt success | ≤2 attempts success | ≤3 attempts success | |
|---|---|---|---|
| Strata | % (95% CI) | % (95% CI) | % (95% CI) |
| Total (N = 222) † | 72 (66–78) | 90 (85–93) | 96 (92–98) |
| Location of intubation | |||
| Pre‐ED setting (n = 44) | 68 (53–80) | 95 (84–100) | 100 (90–100) |
| ED (n = 178) | 73 (66–79) | 89 (83–93) | 94 (90–97) |
| Age | |||
| <2 years old (n = 119) | 67 (58–75) | 89 (82–94) | 96 (90–98) |
| 2–7 years old (n = 74) | 80 (69–87) | 93 (85–97) | 96 (88–99) |
| ≥8 years old (n = 29) | 72 (54–86) | 86 (69–95) | 93 (77–99) |
| Airway‐related anatomical anomalies | |||
| Present (n = 25) | 56 (37–73) | 76 (56–89) | 84 (65–94) |
| Absent (n = 197) | 74 (68–80) | 92 (87–95) | 97 (93–99) |
| Circulatory physiological anomalies | |||
| Present (n = 10) | 70 (39–90) | 90 (57–100) | 100 (68–100) |
| Absent (n = 212) | 72 (66–78) | 90 (85–94) | 96 (92–98) |
| Intubator's level of training ‡ | |||
| Resident physician (n = 36) | 61 (45–75) | — | — |
| Fellow (n = 137) | 74 (66–80) | — | — |
| Attending (n = 49) | 76 (62–85) | — | — |
| Intubator's specialty ‡ | |||
| Emergency medicine (including PEM) (n = 136) | 74 (66–80) | — | — |
| Pediatrics (n = 68) | 66 (54–76) | — | — |
| Critical care medicine (n = 11) | 82 (52–95) | — | — |
| Anesthesiology (n = 7) | 86 (49–97) | — | — |
CI, confidence interval; ED, emergency department; PEM, pediatric emergency medicine.
Nine of the 231 patients were transferred to the OR or PICU for emergency intubation.
The second and third attempts were not analyzed because there were few cases in which the same intubator performed multiple attempts.
Lastly, intubation‐related adverse events were observed in 17%, most of which were hypoxemia (14%), followed by esophageal intubation (5%) and hypotension (1%). There was no cardiac arrest or death related to airway management.
DISCUSSION
In this multicenter prospective study of 231 ED children in Japan, we comprehensively described their clinical and airway management characteristics. The study observed that the first‐attempt success rate was 72%, with large differences by location, patient, and provider factors. For example, the first‐attempt success rate was 68% in the pre‐ED setting, 56% in children with an airway‐related anatomical anomaly, and 61% by resident physicians. We also observed that one in six children had an intubation‐related adverse event and most were hypoxemia. To the best of our knowledge, this is the first investigation that has investigated the current airway management in pediatric EDs in Japan.
Differences in success rates by location factors
In this study, approximately 4% of children considered as being at high risk were transferred to the OR or PICU for airway management. All children transferred to the OR had upper airway obstruction. In an earlier study of the PICU setting, signs of upper airway obstruction were reported to be a significant predictor for difficult intubation. 16 For example, in children with severe croup, ED physicians avoid unnecessary stimuli (e.g., an intravenous line placement) in the ED to mitigate the risk of further airway compromise. In these cases, children are transferred to the OR for airway management with a slow induction of anesthesia with inhalation anesthetic agents, such as nitrous oxide or sevoflurane. Furthermore, in this study, four children with respiratory failure or cardiogenic shock were intubated in the PICU, potentially due to the access to more advanced medical devices, such as extracorporeal membrane oxygenation. In the pre‐ED setting, the first‐attempt success rate was 69%, which was modestly lower than that in the ED setting. The initial intubation success rate in the prehospital setting by Danish anesthesiologists was 75%, and 54% in the group of patients <2 years. 17 Even anesthesiologists had lower first‐attempt success rates in unstable settings. In this study, the success rate increased materially after the initial attempt, although the exact mechanism(s) remains unclear. It is possible that physicians intubating the patient in the pre‐ED setting—who are mostly fellows and attendings (pediatric emergency medicine, pediatric critical care medicine)—failed the first attempt in an uncontrolled setting, but achieved an intubation success at the subsequent attempts through self‐feedback.
Differences in success rates by patient factors
Concordant with the literature reporting younger age as a risk factor for intubation failures, 2 , 9 , 10 , 18 this study also demonstrated that the first‐attempt success rate was low (67%) in patients aged <2 years. In most airway management studies, including ours, an intubation “attempt” is defined as a single insertion of the laryngoscope. 13 , 14 Therefore, it is counted as an attempt if the patient returns to mask ventilation after suctioning of secretion under a laryngoscopic exposure. Younger children who have a larger amount of secretions or a more rapid decrease in the oxygen saturation may have been affected by this type of procedure, thereby leading to the lower first‐attempt success rate. Patient factors such as patients aged <2 years and respiratory indication for intubation have been reported to be significantly associated with desaturation. 18 In younger children, a single attempt at suctioning may not be equivalent to a single unsuccessful intubation attempt.
Several congenital diseases (e.g., maxillary/mandibular hypoplasia, laryngeal/tracheal stenosis) are known risk factors for the difficult airway. 19 In the study of neonatal and pediatric transport, the presence of comorbidity was associated with a higher risk of failed tracheal intubation. 20 In the PICU setting, cardiac patients had a higher incidence of cardiac arrest and hypoxemia associated with tracheal intubation, after adjusting for patient and provider differences. 21 However, there is a dearth of research that has examined the prevalence and characteristics of children with an airway‐related anatomical or circulatory anomaly who underwent airway management in the ED. In this study, compared with children without congenital anomalies, those with an airway‐related anatomical anomaly had a lower success rate of intubation. By contrast, the success rate in children with circulatory physiology anomalies did not substantially differ from those without such anomalies. As unstable hemodynamics has been reported as a risk factor for the occurrence of adverse events, 22 we considered the presence of circulatory physiology anomalies as a potential risk factor, but the results showed otherwise. To successfully intubate a child with a potential physiological instability, systematic preparations for intubation (e.g., optimal preoxygenation, adequate fluid load prior to intubation to maintain circulation, selection of medications and devices, preparation for rescue intubations) should be performed. This may be the result of efforts by providers to maintain hemodynamics in the ED, an environment of limited time and limited medical resources.
Differences in success rates by provider factors
In agreement with previous studies, 10 , 11 , 23 , 24 this study demonstrated that the first‐attempt success rate varied by the level of training. In this study, compared with resident physicians, fellows and attending physicians had higher first‐attempt success rates (61% versus 74% and 76%). In addition, among the different specialties, emergency medicine had a higher rate than pediatrics (74% versus 66%). According to a systematic review of the learning curve for tracheal intubations, in mostly elective circumstances, at least 50 intubations with no more than two attempts need to be performed to reach a success rate of at least 90% in the real‐world setting. 25 However, for most nonanesthesiologists, their experience in advanced airway management in children may be limited. 2 , 3 , 4 , 5 The lack of training opportunities to optimally perform advanced airway management in children, but the need for extensive experience, is a critical limitation in pediatric emergency medicine training. The higher success rate in emergency medicine than in pediatrics may suggest that intubation experiences in adult patients may have had a spillover effect on pediatric patients. To ensure the acquisition of skills, alternative methods—such as training in adult emergency medicine or anesthesiology to increase intubation experiences—should be considered.
In this study, the use of video laryngoscopes was low at 25%. A Japanese study of emergency tracheal intubation in the general EDs found that the rate of video laryngoscopy as an initial intubation device increased from 2% in 2010 to 40% in 2016. 26 In Japanese pediatric EDs, the video laryngoscopy may be used as a rescue device rather than as an initial intubation device. Although the use of a video laryngoscopy might lead to improved vocal cord visualization, there is still no evidence of improved success rates in children compared with those receiving direct laryngoscopy. 27 , 28 , 29 The use of video laryngoscopy in pediatric EDs in Japan is in a transitional period. Changes in success rates and adverse events would be valuable data as the rate of use is likely to increase in the future.
Intubation‐related adverse events
In this study, intubation‐related adverse events were 17%. The incidence of adverse events in pediatric EDs varies from 10% to 39%. 2 , 4 , 6 , 7 , 30 , 31 , 32 There were differences in median patient's age and level of intubator's training between the studies. Improving first‐attempt success rates is important because multiple attempts of intubation procedures increase adverse events. 8 , 33 However, first‐attempt success rates and adverse event rates are not absolutely comparable across the studies, and it is necessary to adjust for factors that influence them.
The success of intubation is attributable to a complex interaction between location, patient, and provider factors. Notwithstanding the complexity, the variation in intubation performance in the pediatric EDs is an important finding. Our data should advance the research into the development of optimal airway management strategies and education systems in pediatric EDs.
Limitations
Our study has several potential limitations. First, the passive surveillance of this study data has a potential self‐reporting bias. Therefore, the patient characteristics, intubation outcomes, and adverse events may have been misclassified. Regardless, the JEAN‐4 study used a previously applied data collection system with structured data forms and uniform definition, 8 , 10 , 13 , 15 and achieved a high capture rate (100%). Second, the study sample consisted of five pediatric EDs. The majority of pediatric emergency care in Japan is currently provided outside of pediatric EDs (general EDs and pediatric departments). Thus, our inference may not be representative of pediatric emergency care in Japan. However, our data should facilitate further investigations into the improvement of pediatric emergency medicine in Japan. Finally, the range of 95% CIs for first‐attempt success rates for each factor is largely due to the number of cases. With a priori sample size calculation based on data from a multicenter observational study in Japanese general EDs (the first attempt success rate for pediatric tracheal intubation of 60%–64%) 8 , 10 and the assumption of the success rate to be 10% higher in pediatric EDs, the range of 95% CI would be within 13%.
CONCLUSIONS
In this multicenter prospective study of ED children, we comprehensively described their clinical and airway management characteristics. The first‐attempt success rate was 72%, indicating that location, patient, and provider factors may have influenced the success rate. The study also showed that one in six children had an intubation‐related adverse event. For researchers, our data should facilitate further investigations into the development of optimal airway management strategies in ED children. Our findings should also encourage pediatric emergency physicians to identify barriers to the delivery of high‐quality airway management, which will, in turn, improve the outcome of critically ill children.
DISCLOSURE
Approval of the research protocol with approval No. and committee Name: H30b‐62, Tokyo Metropolitan Children's Medical Center.
Informed Consent: N/A, opt out.
Registry and the Registration No. of the study/Trial: None.
Animal Studies: N/A.
Conflict of Interest: None declared.
ACKNOWLEDGMENTS
This study was supported by a grant from the Tokyo Metropolitan Government Hospital (protocol number, H30b‐62). Data management was provided by the Data Center at the Clinical Research Support Center, Tokyo Metropolitan Children's Medical Center, Tokyo, Japan.
REFERENCES
- 1. Santillanes G, Gausche‐Hill M. Pediatric airway management. Emerg. Med. Clin. North Am. 2008; 26: 961–75, ix. [DOI] [PubMed] [Google Scholar]
- 2. Pek JH, Ong GY. Emergency intubations in a high‐volume pediatric emergency department. Pediatr. Emerg. Care 2018; 34: 852–6. [DOI] [PubMed] [Google Scholar]
- 3. Yurtseven A, Turan C, Kilinc MA, Ulas SE. Frequency and outcomes of endotracheal intubation in the pediatric emergency department. Turk. J. Pediatr. 2017; 59: 524–30. [DOI] [PubMed] [Google Scholar]
- 4. Long E, Sabato S, Babl FE. Endotracheal intubation in the pediatric emergency department. Paediatr. Anaesth. 2014; 24: 1204–11. [DOI] [PubMed] [Google Scholar]
- 5. Losek JD, Olson LR, Dobson JV, Glaeser PW. Tracheal intubation practice and maintaining skill competency: survey of pediatric emergency department medical directors. Pediatr. Emerg. Care 2008; 24: 294–9. [DOI] [PubMed] [Google Scholar]
- 6. To YH, Ong YG, Chong SL et al. Differences in intubation outcomes for pediatric patients between pediatric and general Emergency Departments. Paediatr. Anaesth. 2021; 31: 713–9. [DOI] [PubMed] [Google Scholar]
- 7. Capone CA, Emerson B, Sweberg T et al. Intubation practice and outcomes among pediatric emergency departments: A report from National Emergency Airway Registry for Children (NEAR4KIDS). Acad. Emerg. Med. 2021; 29: 406–14. [DOI] [PubMed] [Google Scholar]
- 8. Funakoshi H, Kunitani Y, Goto T et al. Association between repeated tracheal intubation attempts and adverse events in children in the emergency department. Pediatr. Emerg. Care 2021; 38: e563–8. [DOI] [PubMed] [Google Scholar]
- 9. Pallin DJ, Dwyer RC, Walls RM, Brown CA 3rd, Investigators NI. Techniques and trends, success rates, and adverse events in emergency department pediatric intubations: a report from the national emergency airway registry. Ann. Emerg. Med. 2016; 67: 610–5 e1. [DOI] [PubMed] [Google Scholar]
- 10. Goto T, Gibo K, Hagiwara Y et al. Factors associated with first‐pass success in pediatric intubation in the emergency department. West. J. Emerg. Med. 2016; 17: 129–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Choi HJ, Je SM, Kim JH, Kim E, Korean Emergency Airway Registry I . The factors associated with successful paediatric endotracheal intubation on the first attempt in emergency departments: a 13‐emergency‐department registry study. Resuscitation 2012; 83: 1363–8. [DOI] [PubMed] [Google Scholar]
- 12. Bourgeois FT, Shannon MW. Emergency care for children in pediatric and general emergency departments. Pediatr. Emerg. Care 2007; 23: 94–102. [DOI] [PubMed] [Google Scholar]
- 13. Hasegawa K, Hagiwara Y, Chiba T et al. Emergency airway management in Japan: Interim analysis of a multi‐center prospective observational study. Resuscitation 2012; 83: 428–33. [DOI] [PubMed] [Google Scholar]
- 14. Walls RM, Brown CA 3rd, Bair AE, Pallin DJ. Emergency airway management: a multi‐center report of 8937 emergency department intubations. J. Emerg. Med. 2011; 41: 347–54. [DOI] [PubMed] [Google Scholar]
- 15. Hasegawa K, Shigemitsu K, Hagiwara Y et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann. Emerg. Med. 2012; 60: 749–54 e2. [DOI] [PubMed] [Google Scholar]
- 16. Graciano AL, Tamburro R, Thompson AE, Fiadjoe J, Nadkarni VM, Nishisaki A. Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: a report from National Emergency Airway Registry for Children: NEAR4KIDS. Intensive Care Med. 2014; 40: 1659–69. [DOI] [PubMed] [Google Scholar]
- 17. Tarpgaard M, Hansen TM, Rognas L. Anaesthetist‐provided pre‐hospital advanced airway management in children: a descriptive study. Scand. J. Trauma Resusc. Emerg. Med. 2015; 23: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rinderknecht AS, Mittiga MR, Meinzen‐Derr J, Geis GL, Kerrey BT. Factors associated with oxyhemoglobin desaturation during rapid sequence intubation in a pediatric emergency department: findings from multivariable analyses of video review data. Acad. Emerg. Med. 2015; 22: 431–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hall SC. The difficult pediatric airway ‐ recognition, evaluation, and management. Can. J. Anaesth. 2001; 48 (Suppl 1): R22–R5. [DOI] [PubMed] [Google Scholar]
- 20. Smith KA, Gothard MD, Schwartz HP, Giuliano JS Jr, Forbes M, Bigham MT. Risk factors for failed tracheal intubation in pediatric and neonatal critical care specialty transport. Prehosp. Emerg. Care 2015; 19: 17–22. [DOI] [PubMed] [Google Scholar]
- 21. Gradidge EA, Bakar A, Tellez D et al. Safety of tracheal intubation in the presence of cardiac disease in paediatric ICUs. Cardiol. Young 2018; 28: 928–37. [DOI] [PubMed] [Google Scholar]
- 22. Nishisaki A, Turner DA, Brown CA 3rd, Walls RM, Nadkarni VM. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Crit. Care Med. 2013; 41: 874–85. [DOI] [PubMed] [Google Scholar]
- 23. Kerrey BT, Rinderknecht AS, Geis GL, Nigrovic LE, Mittiga MR. Rapid sequence intubation for pediatric emergency patients: higher frequency of failed attempts and adverse effects found by video review. Ann. Emerg. Med. 2012; 60: 251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sanders RC Jr, Giuliano JS Jr, Sullivan JE et al. Level of trainee and tracheal intubation outcomes. Pediatrics 2013; 131: e821–8. [DOI] [PubMed] [Google Scholar]
- 25. Buis ML, Maissan IM, Hoeks SE, Klimek M, Stolker RJ. Defining the learning curve for endotracheal intubation using direct laryngoscopy: a systematic review. Resuscitation 2016; 99: 63–71. [DOI] [PubMed] [Google Scholar]
- 26. Goto Y, Goto T, Hagiwara Y et al. Techniques and outcomes of emergency airway management in Japan: an analysis of two multicentre prospective observational studies, 2010‐2016. Resuscitation 2017; 114: 14–20. [DOI] [PubMed] [Google Scholar]
- 27. Abdelgadir IS, Phillips RS, Singh D, Moncreiff MP, Lumsden JL. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst. Rev. 2017; 5: CD011413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Donoghue A, O'Connell K, Neubrand T, Myers S, Nishisaki A, Kerrey B. videographic assessment of tracheal intubation technique in a network of pediatric emergency departments: a report by the Videography in Pediatric Resuscitation (VIPER) Collaborative. Ann. Emerg. Med. 2022; 79: 333–43. [DOI] [PubMed] [Google Scholar]
- 29. Miller KA, Nagler J. Advances in emergent airway management in pediatrics. Emerg. Med. Clin. North Am. 2019; 37: 473–91. [DOI] [PubMed] [Google Scholar]
- 30. Abid ES, Miller KA, Monuteaux MC, Nagler J. Association between the number of endotracheal intubation attempts and rates of adverse events in a paediatric emergency department. Emerg. Med. J. 2021; 39: 601–7. [DOI] [PubMed] [Google Scholar]
- 31. Lollgen RMC, Pontin J, Gow M, McCaskill ME. Adverse events and risk factors during emergency intubation in a tertiary paediatric emergency department. Eur. J. Emerg. Med. 2018; 25: 209–15. [DOI] [PubMed] [Google Scholar]
- 32. Ghedina N, Alkhouri H, Badge H, Fogg T, McCarthy S. Paediatric intubation in Australasian emergency departments: a report from the ANZEDAR. Emerg. Med. Australas. 2020; 32: 401–8. [DOI] [PubMed] [Google Scholar]
- 33. Lee JH, Turner DA, Kamat P et al. The number of tracheal intubation attempts matters! A prospective multi‐institutional pediatric observational study. BMC Pediatr. 2016; 16: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]


