Abstract
Ligaments are peritoneal duplications that contain venous and lymphatic vessels that can potentially be pathways for the spread of infection. Primary inflammation of one of the peritoneal ligaments is very rare. Abscess of the falciform ligament (FLA) is a rare pathological substrate whose pathophysiology is still unknown or poorly understood, but most often occurs as a consequence of a local inflammatory process such as acute cholangitis, cholecystitis, pancreatitis or pylephlebitis. The diagnosis of the primary site of inflammation as well as FLA is established by radiological methods—ultrasound (US), computed tomography (CT) and magnetic resonance (MR), while the therapy is most often combined—conservative and surgical, but interventional radiology methods can also be used. In this report, we present a 67-year-old patient with the falciform ligament abscess that developed during epizode of acute cholecystitis with left portal vein thrombosis, which was diagnosed by US and CT and effectively managed with antibiotic treatment. FLA is a severe inflammatory condition that requires prompt diagnosis and aggressive antibiotic therapy to avoid surgical treatment.
Keywords: Falciform ligament, Abscess, Ultrasound, Antibiotics
Introduction
The falciform ligament is one of the suspensory ligaments of the liver, which contains the ligament teres and an umbilical vein remnant [1]. Ligaments are peritoneal duplications that contain venous and lymphatic vessels that can potentially be pathways for the spread of infection. Primary inflammation of one of the peritoneal ligaments is very rare.
Abscess of the falciform ligament (FLA) is a rare pathological substrate whose pathophysiology is still unknown or poorly understood, but most often occurs as a consequence of a local inflammatory process such as acute cholangitis, cholecystitis, pancreatitis or pylephlebitis. The diagnosis of the primary site of inflammation as well as FLA is established by radiological methods—ultrasound (US), computed tomography (CT) and magnetic resonance (MR), while the therapy is most often combined—conservative and surgical, but interventional radiology methods can also be used.
In this report, we present a 67-year-old patient with the falciform ligament abscess that developed during epizode of acute cholecystitis with left portal vein thrombosis, which was diagnosed by US and CT and effectively managed with antibiotic treatment.
Case report
Clinical history and examination
A 67-year-old female patient presented with 3 days present epigastric pain followed by nausea, vomiting and flatulation. No history of fever, jaundice or weight loss. At physical examination the upper right quadrant of the abdomen and epigastrium revealed tenderness. Past medical history is negative.
Blood tests
The patient's blood tests demonstrated an elevated white cell count of 16 × 103/μl, C reactive protein 25 mg/dL and serum fibrinogen 600 mg/dL with normal levels of bilirubin and transaminase.
Imaging findings
US showed normal sized and homogeneous liver, without focal lesion, with signs of periportal edema. US also detected partially distended gallbladder with mural thickening, and cholelithiasis, consistent with acute cholecystitis. There was no dilatation of extrahepatic biliary duct, with no choledoholythiasis detected. US revealed enlarged and hyperechoic falciform ligament with irregular fluid collection measured 30 mm × 21 mm (Figs. 1 and 2). The color Doppler exam showed the absence of flow in the left branch of the portal vein (Fig. 3), which has thickened walls so the US diagnosis of portal vein thrombophlebitis (pylephlebitis) was made.
Fig. 1.
Abdominal ultrasound: transverse scan in epigastrium showed enlargement and hyperechogenic reaction of falciform ligament (star) with intraligamentary fluid collection - abscess (arrow).
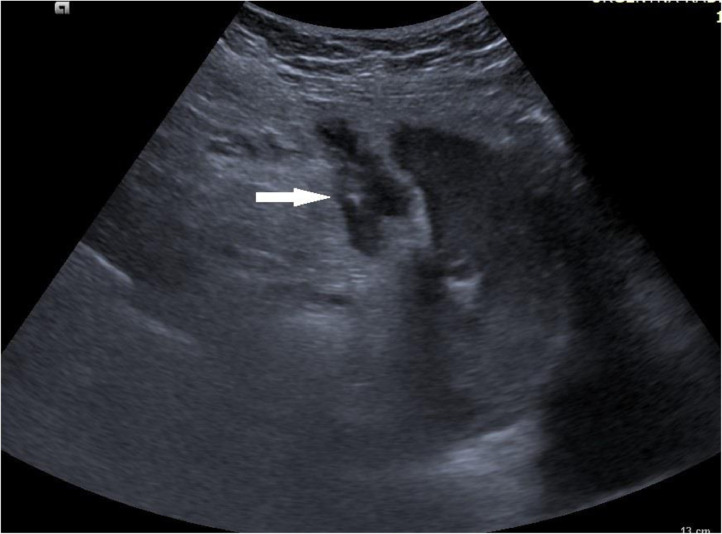
Fig. 2.
Abdominal ultrasound: transverse scan in epigastrium showed abscess in falciform ligament (arrow).
Fig. 3.
Color Doppler revealed the absence of flow in the left branch of the portal vein which has thickened walls – thrombophlebitis (pylephlebitis).
CT demonstrated a filling defect and well opacified walls of the left portal branch, probably indicating secondary thrombophlebitis (pylephlebitis) without thrombosis of main portal vein. CT also detected enlargement and “fat-stranding” of falciform ligament with intraligamentary localized fluid collection—the findings suggests inflammation and abscessus of falciform ligament. Extrahepatic biliary duct was 5 mm diameter, without calculosis but with low cystic duct insertion. Based on the US and CT examination, conclusion was that the cause of FLA is acute cholecystitis and pyhlebitis of the left branch of the portal vein, and the patient was hospitalized.
Therapy and recovery
Considering the clinical history, size of the abscess and biochemical analysis, it was decided that the therapy should initially be conservative with antibiotic therapy. Based on a diagnosis of falciform ligament infection and abscess, we administered conservative therapy with aggressive antibiotics (double antibiotic therapy—metronidasol and ciprofloxacin) as well as anticoagulant therapy in the form of subcutaneous injections of Fraxiparin. The patient's general condition and laboratory data improved after 10 days so control US examination of the abdomen was performed, which showed a complete regression of acute cholecystitis, persistent left portal vein thrombosis and a significant reduction in the size of the FLA (Fig. 4). Patient was discharged with advice for anticoagulant therapy and regular follow-up US and Doppler examinations. Follow-up color Doppler scan one month after showed incomplete left portal vein recanalization with organized thrombus and the patient was asymptomatic with no clinical consequence from this.
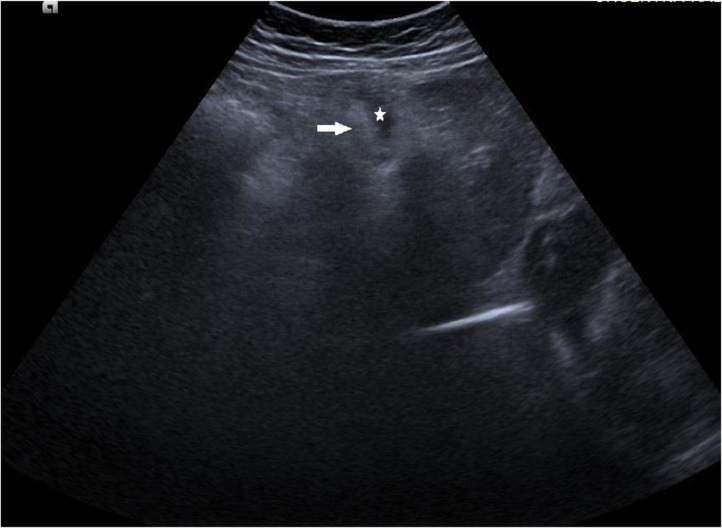
Fig. 4.
Follow-up abdominal ultrasound after therapy: a transverse scan in the epigastrium showed regression in the size of the falciform ligament (arrow) and abscess collection (star).
Discussion
Falciform ligament divides left lobe of liver into lateral and medial segments and extends from inferior surface of diaphragm to supraumbilical part of anterior abdominal wall [2]. It is composed of peritoneal layers within obliterated umbilical vein as ligamentum teres and variable amount of adipose tissue. Inflammation of falciform ligament is an uncommon cause of acute abdominal pain and can mimic the clinical presentation of cholecystitis, perforated duodenal ulcer and pancreatitis. US and CT are helpful for the assessment of the cause [3].
Pylephlebitis is defined as an inflamed thrombosis of the portal vein. It is a rare complication of an intraabdominal infection, and the diagnosis is often missed due to its nonspecific clinical presentation. Symptoms may include abdominal pain, fever, chills, fatigue, nausea, and vomiting. It is important to consider this differential when a patient presents with signs of abdominal sepsis since it has a high mortality rate and is often diagnosed postmortem. Pylephlebitis can be diagnosed via abdominal US or CT demonstrating a thrombus in the portal vein, and it must be treated early and aggressively with broad-spectrum antibiotics [4].
Primary inflammation of the falciform ligament is very rare and the most common cause is inflammation of the ligamentous cyst [5]. The causes of falciform ligament abscesses vary, whether in the pediatric population or in adults. In children, the most common cause is omphalitis, and in adults lymphatic, venous or per continuitatem spreading of the inflammatory process of gallbladder, bile ducts, liver or pancreas origin [6,7].
The characteristic US appearance of the falciform ligament is an echogenic focus at the junction of the quadrate and left lobes of the liver. Recognition of the typical location of the falciform ligament is especially important to distinguish it from other intrahepatic masses [8]. In such cases, US is a very important diagnostic procedure that can indicate the typical presentation of FLA (hypoechoic and anechoic changes in hyperechoic walls located in the area between the quadrate and left lobes of the liver, which continues to the abdominal wall) but also possible causes.
In our case, US revealed signs of acute cholecystitis which probably were primary pathological process leading to left portal branch thrombophlebitis and secondary inflammation and FLA. The mechanism of the falciform ligament inflammation in acute cholecystitis is most often the translocation of bacteria through pericholedochal veins directly into the portal vein, while in cholangitis it spreads through the paraumbilical veins [9]. Portal vein thrombosis can occur for various reasons including hematologic disorders, liver cirrhosis, inflammation and neoplastic changes, while the presence of inflammation in the adjanced structures is necessary for the development of pylephlebitis, which in our patient was acute cholecystitis. The patient was hospitalized and treated with double antibiotic therapy (metronidasol, ciprofloxacin) and anticoagulant drugs. In our case, the early US diagnosis of FLA enabled the rapid hospitalization of the patient and the initiation of aggressive antibiotic therapy with a good therapeutic response, thus avoiding percutaneous drainage of abscess or surgical treatment.
After treatment US control showed significant regression of cholecystitis, left portal branch thrombosis and necrosis of falciform ligament with good response to therapy. Antibiotic and anticoagulant therapy was proceeded for one more week.
Conclusion
FLA is a severe inflammatory condition that requires prompt diagnosis and aggressive antibiotic therapy to avoid surgical treatment. The role of clinical examination, biochemical analyzes and especially imaging modalities such as US or CT is very important in assessing the severity and causes of FLA. Also, their role is significant in monitoring the therapeutic effects of antibiotics in order to make a timely decision on possible surgical treatment.
Patient consent
We confirm that written, informed consent for publication of this case was obtained from the patient.
Footnotes
Competing Interests: None.
References
- 1.Lee MA, Jeong SL, Mu SL, Seung HK, Kyung RL, Yoon JK, et al. Minimally invasive treatment of falciform ligament abscess in a 25-day-old neonate: a case report. J Korean Soc Radiol. 2018;79(5):271–275. [Google Scholar]
- 2.Wong KS, Weisman D, Patrice K. Pylephlebitis: a rare complication of an intra-abdominal infection. J Community Hosp Intern Med Perspect. 2013;3(2):1–4. doi: 10.3402/jchimp.v3i2.20732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nolthenius CJ, Bruinsma WE, Knook MT, Puylaert JB. Acute appendagitis of the ligamentum teres hepatis: clinical, ultrasound, and computed tomographic findings. J Clin Ultrasound. 2013;41:108–112. doi: 10.1002/jcu.21934. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd T. Primary torsion of the falciform ligament: computed tomography and ultrasound findings. Australas Radiol. 2006;50:252–254. doi: 10.1111/j.1440-1673.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 5.Losanoff JE, Kjossev KT. Isolated gangrene of the round and falciform liver ligaments: a rare cause of peritonitis: case report and review of the world literature. Am Surg. 2002;68:751–755. [PubMed] [Google Scholar]
- 6.De Melo VA, De Melo GB, Silva RL, Aragão JF, Rosa JE. Falciform ligament abscess: report of a case. Rev Hosp Clín. 2003;58:37–38. doi: 10.1590/s0041-87812003000100008. [DOI] [PubMed] [Google Scholar]
- 7.Kuribara T, Shigeyoshi I, Ichikawa T, Osa K, Inoue T, Ono S, et al. Falciform ligament abscess with disseminated intrahepatic foci: a case report. Surg Case Rep. 2022;8:112. doi: 10.1186/s40792-022-01466-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hillman BJ, D'Orsi CJ, Smith EH, Bartrum RJ. Ultrasonic appearance of the falciform ligament. AJR Am J Roentgenol. 1979;132:205–206. doi: 10.2214/ajr.132.2.205. [DOI] [PubMed] [Google Scholar]
- 9.Warren LR, Chandrasegaram MD, Madigan DJ, Dolan PM, Neo EL, Worthley CS. Falciform ligament abscess from left sided portal pyemia following malignant obstructive cholangitis. World J Surg Oncol. 2012;10:278. doi: 10.1186/1477-7819-10-278. [DOI] [PMC free article] [PubMed] [Google Scholar]