Abstract
With the emergence of the coronavirus disease 2019 pandemic as a threat to mental health, the demand for online interventions that can replace face-to-face approaches for the prevention of mental health problems is increasing. Although several previous reviews on online interventions have targeted adolescents with symptoms of or those diagnosed with mental illness, there is still a lack of evidence on the effectiveness of online preventive interventions for general and at-risk adolescents. Therefore, this review aimed to evaluate the effectiveness of online interventions on the prevention of an increase in the scores of stress, anxiety, and depression in general and at-risk adolescents. A search was performed using PubMed, EMBASE, and Cochrane Library CENTRAL. Altogether, 19 studies were included, and 16 studies were used for the meta-analysis. Our results showed that cognitive behavioral therapy and family-based interventions were most commonly used. Twelve and seven studies conducted universal and selective preventive interventions, respectively. The meta-analysis showed that online interventions significantly prevent an increase in depression score but not in stress and anxiety scores. Evidence regarding the prevention of increases in stress and anxiety scores is limited, suggesting the need for further randomized controlled trials on online interventions for stress and anxiety in adolescents.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11121-022-01443-8.
Keywords: Adolescent, Anxiety, Depression, Meta-analysis, Online intervention, Prevention, Stress, Systematic review
Mental health problems among adolescents account for a considerable portion of the disease burden, which is a worldwide concern (World Health Organization, 2012). In particular, the coronavirus disease 2019 (COVID-19) pandemic has led to enormous stress associated with social distancing, lack of support from peers or schools, and reorganization of family life, which has increased the risk of depression and anxiety in adolescents (Fegert et al., 2020).
For guarding the mental health of adolescents, school-based, community-based, individual and family-based, and digital platform-based interventions have been conducted (Das et al., 2016). However, the face-to-face group approach through schools or communities has been restricted to control the spread of COVID-19, which has made it difficult to prevent mental health problems in adolescents. Therefore, there has been a growing demand for online interventions to prevent mental health problems, which can replace the face-to-face approach at present. With increased access to online technology, such as computers, smartphones, and tablets, among adolescents. Adolescents are reportedly not only willing to use online therapies for mental health problems but also have generally positive perceptions toward them (Sweeney et al., 2019).
According to the Institute of Medicine’s classifications, preventive interventions are classified into the following three categories based on the risk level of the target population: “universal preventive interventions,” which target the general/whole population that has not been identified as having a specific risk; “selective preventive interventions,” which are directed to at-risk groups or individuals with physical, psychological, or social risk factors associated with mental illness development; and “indicated preventive interventions,” which target identified or screened individuals who have symptoms that are precursors of a mental illness but have not yet been diagnosed with a mental illness (National Research Council and Institute of Medicine, 2009). Because several previous reviews on online interventions have targeted adolescents with symptoms of or those diagnosed with mental illness (Ebert et al., 2015; Grist et al., 2019; Vigerland et al., 2016), evidence on the effectiveness of online preventive interventions for general and at-risk adolescents is still lacking. This systematic review and meta-analysis focused on universal and selective preventive interventions and aimed to evaluate the effectiveness of online interventions in preventing the increases in scores of stress, anxiety, and depression for general and at-risk adolescents.
Methods
The reporting of this systematic review conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Checklist (Page et al., 2021).
Eligibility Criteria
We used the population, interventions, comparators, outcomes, and study design framework to define the inclusion criteria for studies. The criteria for including studies for this review were (a) general adolescents or at-risk adolescents with risk factors developing mental health problems, aged 10–24 years; this age range is an expanded definition of adolescence appropriate nowadays for adolescent development (Sawyer et al., 2018); (b) interventions delivered online, via the internet, websites, or mobile applications; (c) a control condition including a waiting list control, no intervention, placebo, standard care, or usual care; (d) at least one outcome among stress, anxiety, and depression; (e) individually randomized parallel-group trials.
This review excluded studies in which the sample participants included individuals aged ≥ 25 years or ≤ 9 years. Studies that did not specify the age range were also excluded. Studies targeting participants who had symptoms of a mental illness or who were diagnosed with a mental illness were excluded. Studies that used a blended approach of online sessions and face-to-face sessions were excluded to separately evaluate the effectiveness of online interventions. Studies without the control conditions, such as a waiting list control, no intervention, placebo, standard care, or usual care, were excluded. Cluster randomized trials, non-randomized experimental studies, secondary data analyses, study protocols, reviews, editorials, conference proceedings, national and international reports, and gray literature were excluded.
Search Methods
A systematic search using PubMed, EMBASE, and Cochrane Library CENTRAL was conducted on December 11, 2020, and the reference lists of included articles were also screened. We used a search strategy with high sensitivity but relatively low precision with the assistance of a medical librarian. The search was limited to articles published in English from January 2000 to December 2020. Supplementary Table S1 outlines the PubMed search strategy used herein.
Study Selection
Two independent researchers conducted the process of study selection. Records identified through the database search and manual searches through the reference lists of included articles were merged using EndNote X7 (Clarivate™, Philadelphia, PA). After the removal of duplicate articles, the remaining articles were screened. After screening the titles and abstracts for articles, we excluded articles that were not relevant to our research question. Next, we reviewed the full-text articles for eligibility to be included in the final review. Among the finally included studies, meta-analyses were conducted for the studies that reported sufficient numerical data to calculate effect sizes.
Data Extraction
Two independent reviewers extracted data from the included studies using a data extraction form and resolved disagreements through discussion. The extracted data were study citation, study design, recruitment source, characteristics of participants, characteristics of the intervention, comparison conditions, outcomes, measures, results, and the risk of bias data.
Risk of Bias Assessments
The risks of bias in individual randomized controlled trials (RCTs) were appraised using the Cochrane Collaboration tool for assessing the risk of bias in randomized trials (Higgins et al., 2011). This tool evaluates the following seven domains: (a) random sequence generation (selection bias); (b) allocation concealment (selection bias); (c) blinding of participants and personnel (performance bias); (d) blinding of outcome assessment (detection bias); (e) incomplete outcome data (attrition bias); (f) selective reporting (reporting bias); (g) other bias. Each domain was rated as (a) low risk of bias, (b) unclear risk of bias, or (c) high risk of bias. Two independent reviewers independently assessed each study and reached a consensus about the final assessments through discussion. We generated a risk of bias graph using the Cochrane Collaboration’s Review Manager Version 5.4.1. Publication bias was also assessed using Egger’s regression test (Egger et al., 1997).
Summary Measures
If the included studies reported standard errors (SEs), we calculated the standard deviation (SD) from the SE by multiplying it by the square root of the sample size (Higgins et al., 2021). When summary statistics of two eligible intervention groups with slightly different interventions and two placebo-control groups were reported in one study, we combined the summary statistics of the two experimental and two control groups into those of a single experimental group and a single control group using formulas for combining means and SDs across two groups (Higgins et al., 2021). When the summary statistics of an experimental group receiving an appropriate intervention that met the inclusion criteria of this review and another experimental group that did not meet the inclusion criteria were reported separately in one study, we entered only data of the eligible experimental group. In the case of assessing the same outcome using two or more scales in one study, summary statistics of the scale considered the primary measure in the included study were selected for the meta-analysis.
Synthesis of Results
The effect size was based on the standardized mean difference (SMD), defined as the difference between the standardized mean change for the experimental and control groups (Morris, 2008). In each group, the standardized mean change was calculated as the mean difference between posttest and pretest scores, divided by the pooled SD. The formula for the SMD is as follows:
| 1 |
with Mpre, E, Mpost, E, Mpre, C, Mpost, C, and σ denoting the mean for the experimental group pretest, mean for the experimental group posttest, mean for the control group pretest, mean for the control group posttest, and pooled SD, respectively.
The formula for the pooled SD is
| 2 |
with nE and nC denoting the experimental sample size and control sample size, respectively, and SDpre, E, SDpost, E, SDpre, C, and SDpost, C denoting the standard deviation for the experimental group pretest, the experimental group posttest, the control group pretest, and the control group posttest, respectively.
We computed the effect size of Hedges’s g by multiplying the above SMD by a correction factor for small samples and calculated the 95% confidence intervals (CIs) around each obtained mean effect size. Because the studies had heterogeneous populations and interventions and were of unequal sizes, we used random-effects meta-analyses. We used the Hartung–Knapp–Sidik–Jonkman method as an estimator of the heterogeneity variance (Hartung & Knapp, 2001; Sidik & Jonkman, 2002). When the 95% CI excluded zero, we interpreted the effect size to be statistically significant. In addition, 95% prediction intervals (PIs) were computed to report heterogeneity by estimating the expected range of true effects in future settings.
We performed a separate meta-analysis for each outcome of anxiety, depression, and stress. To compare the effect size of universal prevention with the effect size of selective prevention, we grouped all included studies by the preventive level and set up the preventive level as a categorical moderator. For each outcome, we conducted a separate subgroup analysis within each preventive level and an overall analysis across all the levels. The meta-analyses were conducted using R program 3.1.2 and the meta-analysis package “matafor.”
Results
Study Selection
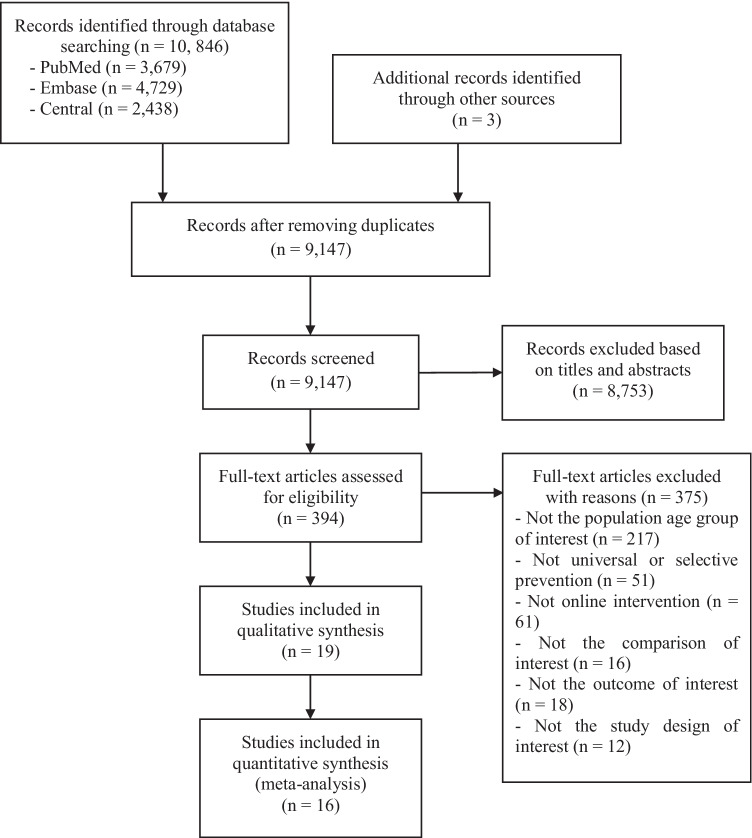
Figure 1 presents a flow diagram of the study selection process. We identified 10,849 studies through database searching and additional manual searching. After the removal of 1702 duplicates, 9147 studies remained. After screening of titles and abstracts, 8753 studies irrelevant to our research question were excluded, and 394 studies were subjected to full-text review. Among a total of 19 eligible studies, 16 studies that reported sufficient numerical data were suitable for quantitative data synthesis.
Fig. 1.
Flow diagram of the study selection process according to the PRISMA guidelines
Study Characteristics
The characteristics of the reviewed studies are presented in Table 1. Although this review screened the literature from 2000 to 2020, the studies included were from 2009 to 2020. The 19 RCTs included were conducted in various countries: 8 in the USA, 3 in the Netherlands, 2 in Australia, 2 in Sweden, 1 in China, 1 in Finland, 1 in New Zealand, and 1 in the UK.
Table 1.
Detailed description of reviewed articles
| First author (year) | Country; recruitment sources | Study participants | Intervention; prevention level | Comparison | Outcomes (measures) |
|---|---|---|---|---|---|
| Antonson (2018) | Sweden; two secondary schools | Upper secondary school students; aged 15–19 years; 70.3% female | Internet-based self-help mindfulness-based program accessible through computers, smartphones, and tablets; Universal prevention | Wait-list | Stress (14-item Perceived Stress Scale) |
| Bonnert (2017) | Sweden; primary, secondar,y and tertiary care clinics | Adolescents diagnosed irritable bowel syndrome; aged 13–17 years; 61.0% female | Internet-delivered cognitive behavior therapy; selective prevention | Wait-list |
Anxiety (Spence Children’s Anxiety Scale) Stress (10-item Perceived Stress Scale) |
| De Voogd (2016a)_1 | Netherlands; 14 regular high schools | Students in the 1st to 6th grade of high schools; aged 11–18 years; 57.6% female | Online attentional bias modification training (visual search attention training, dot-probe attention training); universal prevention | Placebo (visual search placebo, dot-probe placebo) |
Anxiety (Screen for Child Anxiety Related Emotional Disorders) Depression (Children’s Depression Inventory) |
| De Voogd (2016b)_2 | The Netherlands; 14 regular high schools | High school students; aged 11–18 years; 60.1% female | Online emotional working memory training; universal prevention | Placebo |
Anxiety (Screen for Child Anxiety Related Emotional Disorders) Depression (Children’s Depression Inventory) |
| De Voogd (2018) | The Netherlands; 14 regular high schools | Students in the 1st to 6th grade of high schools; aged 11–19 years; 60.7% female | Online interpretation bias modification training; universal prevention | Placebo |
Anxiety (Screen for Child Anxiety Related Emotional Disorders) Depression (Children’s Depression Inventory) |
| Duan (2017) | China; one university | Undergraduate students; aged 17–24 years; 71.1% female | Web-based multiple health behavior intervention for physical activity and fruit and vegetable intake based on health action process approach; universal prevention | No intervention | Depression (Center for Epidemiologic Studies Depression) |
| Fang (2010) | USA; Asian community service agencies in 19 states with significant Asian populations | Asian–American adolescent girls; aged 11–14 years; all females | Web-based Mother-Daughter program (family-oriented substance use prevention program based on family interaction theory); universal prevention | No intervention | Depression (Children’s Depression Inventory) |
| Greene (2012) | USA; eight universities | Undergraduate students of freshmen, sophomores, and juniors; aged 18–24 years; 63% female | Online healthful eating and physical activity program; universal prevention | Wait-list |
Stress (12-item General Health Questionnaire) |
| Kattelmann (2014) | USA; 13 college campuses | College student; aged 18–24 years; 67.2% female | Web-delivered Young Adults Eating and Active for Health program; universal prevention | Wait-list | Stress (14-item Perceived Stress Scale) |
| Law (2015) | USA; a headache clinic | Adolescents with recurrent headache; aged 11–17 years; 81.9% female | Internet-delivered family-based cognitive behavioral therapy program with headache treatment; selective prevention | Headache treatment |
Anxiety (Revised Children’s Manifest Anxiety Scale, Second Edition) Depression (Children’s Depression Inventory) |
| Levin (2014) | USA; two local university and community college campuses, as well as advertisements in the local school newspapers and school websites | Undergraduate first-year students; aged 18–20 years; 53.9% female | Web-based acceptance and commitment therapy prevention program; universal prevention | Wait-list |
Anxiety (7-item subscale assessing anxiety of the 21-item version of the Depression, Anxiety and Stress Scale) Depression (7-item subscale assessing depression of the 21-item version of the Depression, Anxiety and Stress Scale) Stress (7-item subscale assessing stress of the 21-item version of the Depression, Anxiety, and Stress Scale) |
| Newcombe (2012) | Australia; a respiratory outpatient clinic | Children and adolescents with a chronic respiratory condition; aged 10–17 years; 51.3% female | Internet-based problem-solving program; selective prevention | Wait-list | Depression (Center for Epidemiologic Studies Depression Scale for Children) |
| O’Dea (2020) | Australia; advertisement on Facebook campaign targeting young people | adolescents; aged 12–16 years; 86.5% female | Relationship-focused mobile phone application based on cognitive behavioral therapy and social learning theory; universal prevention | Wait-list |
Anxiety (Spence Children’s Anxiety Scale) Depression (Patient Health Questionnaire for Adolescents) |
| Palermo (2009) | USA; multidisciplinary pediatric pain clinic, pediatric neurology clinic, and pediatric gastroenterology clinic at an academic health center | Children and adolescents with chronic pain; aged 11–17 years; 72.9% female | Internet-delivered family cognitive behavioral therapy intervention; selective prevention | Wait-list |
Depression (Major depressive disorder subscale of the Revised Child Anxiety and Depression Scale) |
| Puolakanaho (2019) | Finland; two municipalities in Central Finland | Ninth-grade adolescents; aged 15–16 years; 49.0% female | Web- and mobile-delivered program based on acceptance and commitment therapy; universal prevention | Usual support from school | Stress (Single-item measure assessing overall stress) |
| Ruggiero (2015) | USA; two regions that sustained severe impact from tornadoes | Adolescents affected by devastating tornadoes; aged 12–17 years; 51.0% female | Web-based intervention for disaster-affected adolescents and parents; selective prevention | No intervention |
Depression (National Survey of Adolescents Depression module) |
| Schwinn (2014) | USA; publicly subsidized housing | Adolescent girls lived in publicly subsidized housing; aged 10–12 years; all females | Web-based, family-involvement health promotion program; selective prevention | No intervention | Stress (6-item Perceived Stress Scale) |
| Whittaker (2017) | New Zealand; 15 secondary schools | Attending years 9–12 at participating schools; aged 13–17 years; 68.0% female | Mobile phone-delivered cognitive behavioral therapy-based program; universal prevention | Placebo |
Depression (Children’s Depression Rating Scale-Revised) |
| Williamson (2019) | UK; primary care practices and charities | Adolescents with appearance-affecting conditions experiencing appearance-related distress, teasing or bullying; aged 12–17 years; 74.5% females | Web-based self-help psychosocial intervention integrating cognitive behavioral therapy and social skills training; selective prevention | Usual care | Social anxiety (22-item Social Anxiety Scale) |
The 12 included studies focused on universal preventive interventions for general adolescents, and 9 of them recruited participants from schools. The seven remaining studies concentrated on selective preventive interventions for adolescents exposed to physical, psychological, or social risk factors. Some of the studies were directed to participants exhibiting physical problems such as irritable bowel syndrome, recurrent headaches, chronic pain, or chronic respiratory illness. Psychosocial risk factors, such as experiencing a natural disaster, appearance-related distress, teasing or bullying, and living in publicly subsidized housing programs, were also noted.
The online preventive interventions conducted in the included studies were categorized according to the intervention type. Six studies used cognitive behavioral therapy (CBT)-based interventions (Bonnert et al., 2017; Law et al., 2015; O’Dea et al., 2020; Palermo et al., 2009; Whittaker et al., 2017; Williamson et al., 2019) and five studies employed family-based interventions (Fang et al., 2010; Law et al., 2015; Palermo et al., 2009; Ruggiero et al., 2015; Schwinn et al., 2014); among them, two studies conducted family-based CBT (Law et al., 2015; Palermo et al., 2009). Three studies evaluated cognitive training, such as attentional bias modification training (de Voogd et al., 2016a, b), emotional working memory training (de Voogd et al., 2016a, b), and interpretation bias modification training (de Voogd et al., 2018). Health behavior interventions for healthy eating and physical activity were conducted in three studies (Duan et al., 2017; Greene et al., 2012; Kattelmann et al., 2014). Acceptance and commitment therapy (ACT) was employed in two studies (Levin et al., 2014; Puolakanaho et al., 2019), mindfulness-based intervention in one study (Antonson et al., 2018), and problem-solving program in one study (Newcombe et al., 2012).
Regarding outcome variables and instruments, four instruments in seven studies were used to measure stress, among which the Perceived Stress Scale was used in four studies. Five instruments in eight studies were used to measure anxiety, among which the Screen for Child Anxiety Related Emotional Disorders was used in three studies and the Spence Children’s Anxiety Scale was used in two studies. Eight instruments in 12 studies were used to measure depression, among which the Children’s Depression Inventory was used in five studies and the Center for Epidemiologic Studies Depression was used in two studies.
Risk of Bias Assessments
A plot of the percentage of risk of bias assessments per domain is presented in Supplementary Figure S1. Most included studies (n = 13) provided adequate information to assess random sequence generation, and the remaining six studies had insufficient information regarding the sequence generation process. Regarding allocation concealment, 12 studies adequately provided the method of allocation concealment, and 7 studies had insufficient information to permit judgment. Performance bias was low in four studies, indicating that both participants and study personnel were blinded to allocation. Conversely, six studies had unclear risk, and nine studies of single-blinded researchers or open trials were determined as having a high risk of performance bias. Detection bias was low in five studies that mentioned about the blinding of outcome assessors; however, seven studies had insufficient information to permit judgment and seven studies that used participant-reported outcomes, in which participants were not blinded, were determined to be at high risk. Attrition bias was low in 14 studies that used intention-to-treat analysis, including dropouts; however, five studies were considered to be at high risk because they used “as-treated” analysis with substantial attrition. Reporting bias was low in seven studies in which all prespecified outcomes in their protocol were reported. Alternatively, 10 studies had insufficient information to permit judgment, and two studies in which not all the prespecified outcomes in their protocol were reported or were incompletely reported were judged to be at high risk. Two studies were judged to be at high risk of other sources of bias because one study reported that age and sex between experimental and control groups were statistically different (Duan et al., 2017) and one study reported that some participants of the control group were exposed to the intervention (Greene et al., 2012). The remaining 17 studies were judged to be at low risk of other bias. In addition, Egger’s regression test showed no significant publication bias in terms of stress, anxiety, and depression (p = 0.948, 0.534, and 0.494, respectively).
Effects of Online Interventions on Stress, Anxiety, and Depression
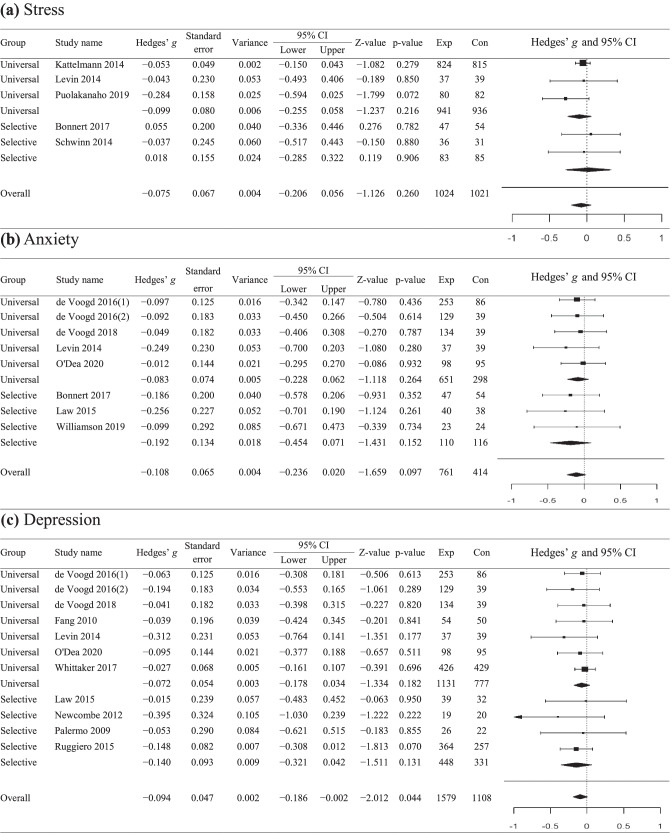
Figure 2 depicts the forest plot showing the effect size of the change in stress, anxiety, and depression between intervention and control groups. Although stress was assessed in seven studies (Antonson et al., 2018; Bonnert et al., 2017; Greene et al., 2012; Kattelmann et al., 2014; Levin et al., 2014; Puolakanaho et al., 2019; Schwinn et al., 2014), a meta-analysis on change in stress scores synthesized five studies (Bonnert et al., 2017; Kattelmann et al., 2014; Levin et al., 2014; Puolakanaho et al., 2019; Schwinn et al., 2014) reporting sufficient numerical data. The results of the meta-analysis combining the five studies with an overall sample size of n = 2045 (1024 intervention and 1021 control participants) found no significant difference in change in stress scores between the intervention and control groups (g, −0.075; 95% CI, −0.206 to 0.056; 95% PI, −0.265 to 0.115). Subgroup analyses by the preventive level showed that both universal (g, −0.099; 95% CI, −0.255 to 0.058; 95% PI, −0.324 to 0.126) and selective preventive interventions (g, 0.018; 95% CI, −0.285 to 0.322) showed no significant difference in stress change compared with the control groups.
Fig. 2.
Forest plot showing the effect size of change in stress, anxiety, and depression scores
A meta-analysis combining the results of eight studies assessing anxiety (Bonnert et al., 2017; de Voogd et al., 2016a, b, 2018; Law et al., 2015; Levin et al., 2014; O’Dea et al., 2020; Williamson et al., 2019) with an overall sample size of n = 1175 (761 intervention and 414 control participants) showed no significant difference in change in anxiety scores between intervention and control groups (g, −0.108; 95% CI, −0.236 to 0.020; 95% PI, −0.254 to 0.037). Subgroup meta-analyses by preventive level showed that both universal (g, −0.083; 95% CI, −0.228 to 0.062; 95% PI, −0.242 to 0.076) and selective preventive interventions (g, −0.192; 95% CI, −0.454 to 0.071; 95% PI, −0.457 to 0.073) did not significantly differ in terms of change in anxiety scores compared with control groups.
Although 12 studies (de Voogd et al., 2016a, b, 2018; Duan et al., 2017; Fang et al., 2010; Law et al., 2015; Levin et al., 2014; Newcombe et al., 2012; O’Dea et al., 2020; Palermo et al., 2009; Ruggiero et al., 2015; Whittaker et al., 2017) assessed depression, a meta-analysis on depression change synthesized 11 studies (de Voogd et al., 2016a, b, 2018; Fang et al., 2010; Law et al., 2015; Levin et al., 2014; Newcombe et al., 2012; O’Dea et al., 2020; Palermo et al., 2009; Ruggiero et al., 2015; Whittaker et al., 2017) reporting sufficient numerical data. On combining 11 studies with an overall sample size of n = 2687 (1579 intervention and 1108 control participants), a significant difference in change in depression scores for online interventions over control condition was found (g, −0.094; 95% CI, −0.186 to −0.002). The resulting 95% PI (−0.240 to 0.051) may be interpreted as a true effect size that varies from a g-value of −0.240 in some studies to 0.051 in others. Following grouping by preventive level, both universal (g, −0.072; 95% CI −0.178 to 0.034; 95% PI, −0.214 to 0.070) and selective preventive interventions (g, −0.140; 95% CI, −0.321 to 0.042, 95% PI −0.374 to 0.095) showed no significant difference in change in depression scores between intervention and control groups.
Discussion
This systematic review aimed to evaluate the effectiveness of online preventive interventions for changes in stress, anxiety, and depression among general and at-risk adolescents. Among the 19 reviewed studies, 7 studies (36.8%) were published between 2009 and 2014, and 12 studies (63.2%) were published between 2015 and 2020, which indicates that research regarding online interventions has been actively conducted over the past 6 years.
Among the online interventions conducted in the reviewed studies, CBT and family-based interventions were most commonly used. Some previous systematic reviews (Calear & Christensen, 2010; Clarke et al., 2015) have reported that CBT-based online interventions were used most frequently; however, they did not identify family-based online interventions. This review has importance in that it identified five family-based programs involving adolescents and their parents to be feasible online because adolescent mental health is closely associated with the parent–adolescent relationship (Chen & Harris, 2019).
We found that online interventions for general and at-risk adolescents were significantly beneficial in preventing the increase in depression scores but not in stress and anxiety scores. The overall effect size for change in depression score was smaller in this study (g = 0.094) than in previous meta-analyses on technology-delivered interventions (g = 0.43 (Grist et al., 2019)) and on internet and computer-based CBTs (g = 0.56; Ebert et al., 2015). Additionally, the anxiety change was not significantly different between the intervention and control groups in this study, but the significant effect sizes for anxiety reported in the two previous reviews were g = 0.41 (Grist et al., 2019) and g = 0.65 (Ebert et al., 2015). This study reviewed preventive interventions for general and at-risk adolescents, whereas the two previous reviews involved interventions targeting depression or anxiety among children and adolescents with depressive/anxiety symptoms or a diagnosis of depression or anxiety disorder. Therefore, differences in the results between this review and previous reviews may be explained by the fact that individuals with related symptoms have substantially more room for improvement in terms of the relevant scores as a result of the interventions (Edmonds et al., 2018).
Although we found that online interventions were associated with a significant improvement in depression change, reflected by a g-value of −0.094 with a 95% CI −0.186 to −0.002, the 95% PI −0.240 to 0.051 contained null effects or effects in the opposite direction. The 95% PI contained values below zero, which correspond to depression prevention, with a best case of a g-value of −0.240 after interventions compared with controls. However, the PI also contained values greater than zero, which means that the effect of the interventions may exhibit null or even opposite effects, with the worst case of a g-value of 0.051. This finding of heterogeneity may be because of the diversity in the context wherein the interventions occurred, as well as in the contents and period of interventions. The studies synthesized in a meta-analysis on depression change were conducted in various countries, including the USA, the Netherlands, Australia, and New Zealand. The participants were recruited from school (de Voogd et al., 2016a, b, 2018; Levin et al., 2014; Whittaker et al., 2017), community (Fang et al., 2010; O’Dea et al., 2020; Ruggiero et al., 2015), and hospital (Law et al., 2015; Newcombe et al., 2012; Palermo et al., 2009) settings. Furthermore, the interventions applied varied, including CBT-based interventions, family-based interventions, cognitive training, ACT, and problem-solving programs. Post-test timing varied from 3 weeks (Levin et al., 2014) to 12 months (Ruggiero et al., 2015; Whittaker et al., 2017). These differences may have acted as potential drivers of the variation in the effects. The PI enables more informed decision-making (IntHout et al., 2016); therefore, because of the expected variation in true effects, caution is required in decision-making regarding online interventions for the prevention of adolescent depression.
Strengths and Limitations of This Review
Although previous reviews have focused on adolescents with symptoms of mental illness, a strength of this study is that it reviewed online preventive interventions for both general and at-risk adolescents. It also demonstrated that family-based online programs were feasible and the included interventions were significantly beneficial in preventing an increase in depression scores, even when the effect size was small. The effects on stress and anxiety were not supported in this review. However, the number of studies combined in the meta-analyses on stress and anxiety was small. Therefore, more RCTs are warranted to determine the effectiveness of online preventive interventions on stress and anxiety.
There were several limitations of this study. First, this review was exclusively based on studies published in English, which may introduce language bias. Second, this review did not include gray literature or unpublished studies, which may introduce publication bias. Third, the focus of this review was online interventions, compared with control conditions, including a waiting list control, no intervention, placebo, standard care, or usual care. Therefore, the results of studies conducting interventions delivered online combined with interventions delivered through face-to-face programs and studies without the control conditions were excluded. Fourth, because we designed the scope of this review to include only individually randomized trials, further systematic reviews are required to incorporate the results of cluster randomized trials. Finally, three included studies were excluded from the meta-analysis because of insufficient effect size data.
Conclusions
This systematic review showed that the most frequently used online preventive interventions were CBT-based interventions and family-based interventions involving adolescents and their parents. There were universal and selective preventive interventions, and most universal preventive interventions were delivered in school settings. The meta-analyses showed that online interventions for general and at-risk adolescents exhibited significant benefits in preventing an increase in depression scores. However, there is limited evidence regarding the effectiveness of online interventions for stress and anxiety, suggesting the need for further RCTs on online preventive interventions for them.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (no. NRF-2018R1C1B5041097).
Declarations
Ethics Approval
This is a review of papers already in the public domain. No ethical approval was required.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Antonson C, Thorsén F, Sundquist J, Sundquist K. Upper secondary school students’ compliance with two internet-based self-help programmes: A randomised controlled trial. European Child and Adolescent Psychiatry. 2018;27:191–200. doi: 10.1007/s00787-017-1035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnert M, Olén O, Lalouni M, Benninga MA, Bottai M, Engelbrektsson J, Hedman E, Lenhard F, Melin B, Simrén M, Vigerland S, Serlachius E, Ljótsson B. Internet-delivered cognitive behavior therapy for adolescents with irritable bowel syndrome: A randomized controlled trial. American Journal of Gastroenterology. 2017;112:152–162. doi: 10.1038/ajg.2016.503. [DOI] [PubMed] [Google Scholar]
- Calear AL, Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Medical Journal of Australia. 2010;192:S12–S14. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- Chen, P., & Harris, K. M. (2019). Association of positive family relationships with mental health trajectories from adolescence to midlife. Journal of the American Medical Association Pediatrics,173, e193336. 10.1001/jamapediatrics.2019.3336 [DOI] [PMC free article] [PubMed]
- Clarke AM, Kuosmanen T, Barry MM. A systematic review of online youth mental health promotion and prevention interventions. Journal of Youth and Adolescence. 2015;44:90–113. doi: 10.1007/s10964-014-0165-0. [DOI] [PubMed] [Google Scholar]
- Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, Bhutta ZA. Interventions for adolescent mental health: An overview of systematic reviews. Journal of Adolescent Health. 2016;59:S49–S60. doi: 10.1016/j.jadohealth.2016.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Voogd EL, Wiers RW, Prins PJM, de Jong PJ, Boendermaker WJ, Zwitser RJ, Salemink E. Online attentional bias modification training targeting anxiety and depression in unselected adolescents: Short- and long-term effects of a randomized controlled trial. Behaviour Research and Therapy. 2016;87:11–22. doi: 10.1016/j.brat.2016.08.018. [DOI] [PubMed] [Google Scholar]
- de Voogd EL, Wiers RW, Zwitser RJ, Salemink E. Emotional working memory training as an online intervention for adolescent anxiety and depression: A randomised controlled trial. Australian Journal of Psychology. 2016;68:228–238. doi: 10.1111/ajpy.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Voogd L, Wiers RW, de Jong PJ, Zwitser RJ, Salemink E. A randomized controlled trial of multi-session online interpretation bias modification training: Short- and long-term effects on anxiety and depression in unselected adolescents. PLoS ONE. 2018;13:e0194274. doi: 10.1371/journal.pone.0194274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan YP, Wienert J, Hu C, Si GY, Lippke S. Web-based intervention for physical activity and fruit and vegetable intake among Chinese university students: A randomized controlled trial. Journal of Medical Internet Research. 2017;19:e106. doi: 10.2196/jmir.7152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert DD, Zarski AC, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, Riper H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS ONE. 2015;10:e0119895. doi: 10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmonds M, Hadjistavropoulos HD, Schneider LH, Dear BF, Titov N. Who benefits most from therapist-assisted internet-delivered cognitive behaviour therapy in clinical practice? Predictors of symptom change and dropout. Journal of Anxiety Disorders. 2018;54:24–32. doi: 10.1016/j.janxdis.2018.01.003. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang L, Schinke SP, Cole KCA. Preventing substance use among early Asian-American adolescent girls: Initial evaluation of a web-based, mother–daughter program. Journal of Adolescent Health. 2010;47:529–532. doi: 10.1016/j.jadohealth.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene GW, White AA, Hoerr SL, Lohse B, Schembre SM, Riebe D, Patterson J, Kattelmann KK, Shoff S, Horacek T, Blissmer B, Phillips BW. Impact of an online healthful eating and physical activity program for college students. American Journal of Health Promotion. 2012;27:e47–e58. doi: 10.4278/ajhp.110606-QUAN-239. [DOI] [PubMed] [Google Scholar]
- Grist R, Croker A, Denne M, Stallard P. Technology delivered interventions for depression and anxiety in children and adolescents: A systematic review and meta-analysis. Clinical Child and Family Psychology Review. 2019;22:147–171. doi: 10.1007/s10567-018-0271-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartung J, Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Statistics in Medicine. 2001;20:3875–3889. doi: 10.1002/sim.1009. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savović, J., Schulz, K. F., Weeks, L., & Sterne, J. A., Cochrane Bias Methods Group, & Cochrane Statistical Methods Group. (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal,343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed]
- Higgins J. P. T., Li T., & Deeks, J. J. (2021). Chapter 6. Choosing effect measures and computing estimates of effect. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane Handbook for Systematic Reviews of Interventions version 6.2. Cochrane. https://www.training.cochrane.org/handbook
- IntHout J, Ioannidis JPA, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. British Medical Journal Open. 2016;6:e010247. doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kattelmann KK, Bredbenner CB, White AA, Greene GW, Hoerr SL, Kidd T, Colby S, Horacek TM, Phillips BW, Koenings MM, Brown ON, Olfert MD, Shelnutt KP, Morrell JS. The effects of young adults eating and active for health (YEAH): A theory-based web-delivered intervention. Journal of Nutrition Education and Behavior. 2014;46:S27–S41. doi: 10.1016/j.jneb.2014.08.007. [DOI] [PubMed] [Google Scholar]
- Law EF, Beals-Erickson SE, Noel M, Claar R, Palermo TM. Pilot randomized controlled trial of internet-delivered cognitive-behavioral treatment for pediatric headache. Headache. 2015;55:1410–1425. doi: 10.1111/head.12635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin ME, Pistorello J, Seeley JR, Hayes SC. Feasibility of a prototype web-based acceptance and commitment therapy prevention program for college students. Journal of American College Health. 2014;62:20–30. doi: 10.1080/07448481.2013.843533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris, S. B. (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. 10.1177/1094428106291059
- National Research Council and Institute of Medicine. (2009). Committee on the prevention of mental disorders and substance abuse among children, youth, and young adults: Research advances and promising interventions. In M. E. O’Connell, T. Boat, & K. E. Warner (Eds.). Preventing mental, emotional, and behavioral disorders among Young people: Progress and possibilities. National Academies Press: US [PubMed]
- Newcombe PA, Dunn TL, Casey LM, Sheffield JK, Petsky H, Anderson-James S, Chang AB. Breathe easier online: Evaluation of a randomized controlled pilot trial of an internet-based intervention to improve well-being in children and adolescents with a chronic respiratory condition. Journal of Medical Internet Research. 2012;14:e23. doi: 10.2196/jmir.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dea B, Han J, Batterham PJ, Achilles MR, Calear AL, Werner-Seidler A, Parker B, Shand F, Christensen H. A randomised controlled trial of a relationship-focussed mobile phone application for improving adolescents' mental health. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2020;61:899–913. doi: 10.1111/jcpp.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H. Randomized controlled trial of an internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009;146:205–213. doi: 10.1016/j.pain.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puolakanaho A, Lappalainen R, Lappalainen P, Muotka JS, Hirvonen R, Eklund KM, Ahonen TPS, Kiuru N. Reducing stress and enhancing academic buoyancy among adolescents using a brief web-based program based on acceptance and commitment therapy: A randomized controlled trial. Journal of Youth and Adolescence. 2019;48:287–305. doi: 10.1007/s10964-018-0973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero KJ, Price M, Adams Z, Stauffacher K, McCauley J, Danielson CK, Knapp R, Hanson RF, Davidson TM, Amstadter AB, Carpenter MJ, Saunders BE, Kilpatrick DG, Resnick HS. Web intervention for adolescents affected by disaster: Population-based randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:709–717. doi: 10.1016/j.jaac.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet. Child & Adolescent Health. 2018;2:223–228. doi: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- Schwinn TM, Schinke S, Fang L, Kandasamy S. A web-based, health promotion program for adolescent girls and their mothers who reside in public housing. Addictive Behaviors. 2014;39:757–760. doi: 10.1016/j.addbeh.2013.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidik K, Jonkman JN. A simple confidence interval for meta-analysis. Statistics in Medicine. 2002;21:3153–3159. doi: 10.1002/sim.1262. [DOI] [PubMed] [Google Scholar]
- Sweeney GM, Donovan CL, March S, Forbes Y. Logging into therapy: Adolescent perceptions of online therapies for mental health problems. Internet Interventions. 2019;15:93–99. doi: 10.1016/j.invent.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Ahlen J, Olén O, Serlachius E, Ljótsson B. Internet-delivered cognitive behavior therapy for children and adolescents: A systematic review and meta-analysis. Clinical Psychology Review. 2016;50:1–10. doi: 10.1016/j.cpr.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Whittaker R, Stasiak K, McDowell H, Doherty I, Shepherd M, Chua S, Dorey E, Parag V, Ameratunga S, Rodgers A, Merry S. MEMO: An mHealth intervention to prevent the onset of depression in adolescents: A double-blind, randomised, placebo-controlled trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2017;58:1014–1022. doi: 10.1111/jcpp.12753. [DOI] [PubMed] [Google Scholar]
- Williamson, H., Hamlet, C., White, P., Marques, E. M. R., Paling, T., Cadogan, J., Perera, R., Rumsey, N., Hayward, L., & Harcourt, D. (2019). A web-based self-help psychosocial intervention for adolescents distressed by appearance-affecting conditions and injuries (Young Persons’ Face IT): Feasibility study for a parallel randomized controlled trial. Journal of Medical Internet Research Mental Health,6. 10.2196/14776 [DOI] [PMC free article] [PubMed]
- World Health Organization. (2012). Global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level: report by the Secretariat (Report No. A65/10). Retrieved from https://apps.who.int/iris/handle/10665/78898
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.