An 85-year-old woman, with a history of biliopancreatic diversion for bariatric surgery 10 years before, presented with obstructive jaundice.
Computed tomographic scan showed dilation of the biliary tree with evidence of a stricture in the distal common bile duct (CBD).
Due to multiple comorbidities, the patient was deemed unfit for surgery; thus, an adequate tissue sampling and biliary drainage were required to confirm the diagnosis and to palliate jaundice.
A transpapillary biliary drainage by enteroscopy-assisted ERCP was unsuccessfully attempted due to a long jejunal limb.
The patient was therefore referred to our unit to perform an EUS-guided hepaticogastrostomy (EUS-HGS).
EUS evaluation through the gastric remnant demonstrated dilation of the left intrahepatic bile ducts and failed to visualize the distal CBD.
Under EUS and fluoroscopy guidance, a dilated left intrahepatic duct was identified and punctured with a 19-gauge needle with injection of contrast to provide a cholangiogram. Subsequently, a 0.025-inch guidewire was advanced into the biliary system [Figure 1 and Video 1]. A 6 Fr cystotome was inserted over the wire and used to dilate the tract. A dedicated 10 mm × 80 mm partially-covered self-expandable metal stent (HANARO stent BPE, M.I. Tech, Seoul, Rep. South Korea) was released through the gastric wall into the intrahepatic duct [Figure 2].
Figure 1.
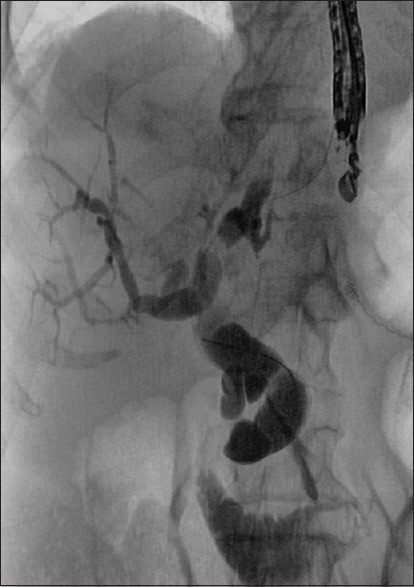
Fluoroscopic view of cholangiogram with a 0.025-inch guidewire in the biliary system with distal common bile duct stricture
Figure 2.
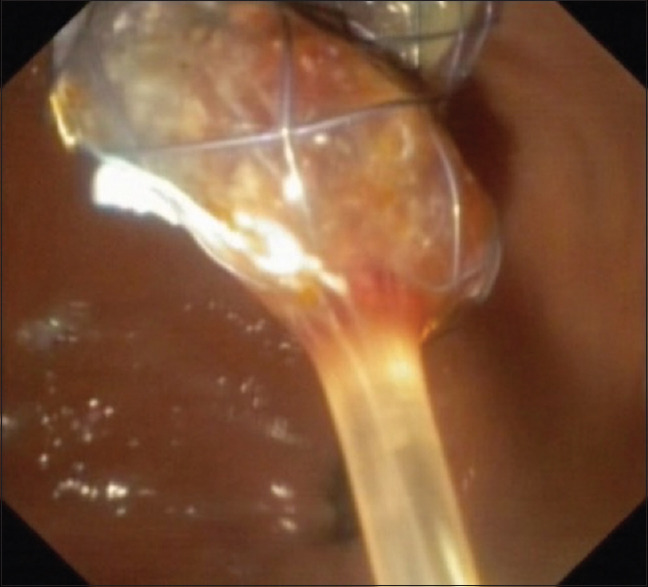
Endoscopic view of the stent released for creation of a EUS-guided hepaticogastrostomy in the gastric remnant
To obtain a histological diagnosis of the indeterminate biliary stricture, a direct peroral cholangioscopy (DPOC) through the newly created HGS was performed.
First of all, the stent was dilated with a pneumatic balloon up to 9 mm (CRE, Boston Scientific Corporation Inc., Marlborough, MA, USA) through the EUS scope [Figure 3].
Figure 3.
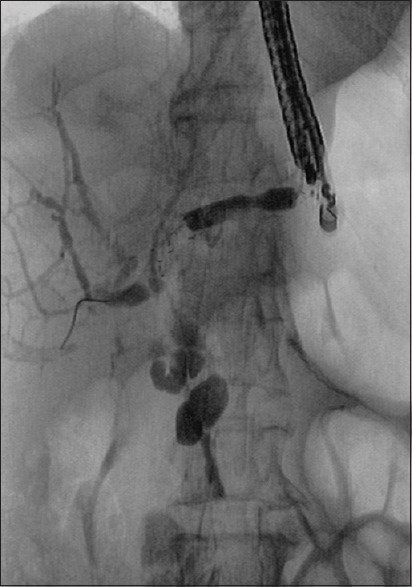
Pneumatic dilation of the stent through the EUS scope under fluoroscopic control
A 5.9-mm ultraslim endoscope (Fujifilm EG-580NW2, Tokyo, Japan) was advanced under CO2 insufflation across the HGS into the biliary system with fluoroscopic guidance to avoid misplacement of the stent.
An obstructing lesion with dilated and tortuous vessels in the distal CBD was revealed [Figure 4]. Under direct endoscopic visualization, multiple targeted biopsy specimens were obtained with forceps for histopathologic analysis.
Figure 4.
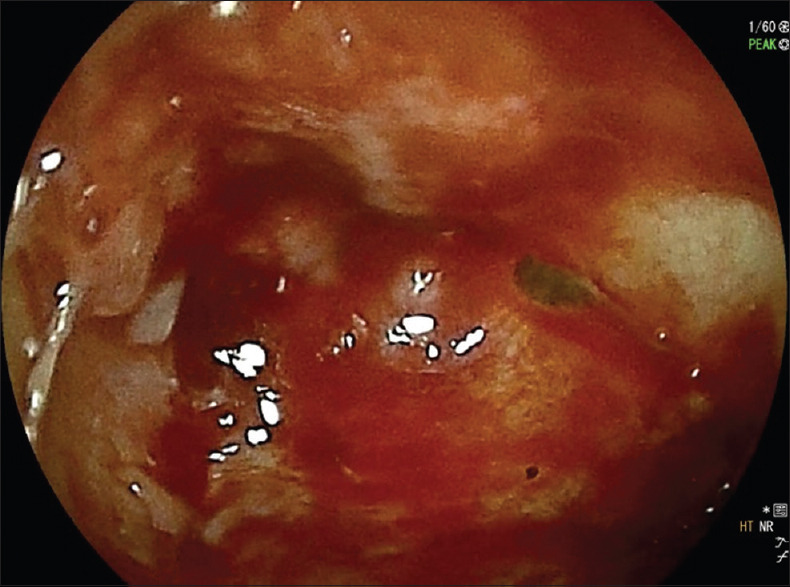
Direct peroral cholangioscopy showing the lesion in the distal common bile duct
Histologic analysis revealed cholangiocarcinoma [Figure 5]. Neither adverse events occurred during the procedure nor at the subsequent follow-up.
Figure 5.
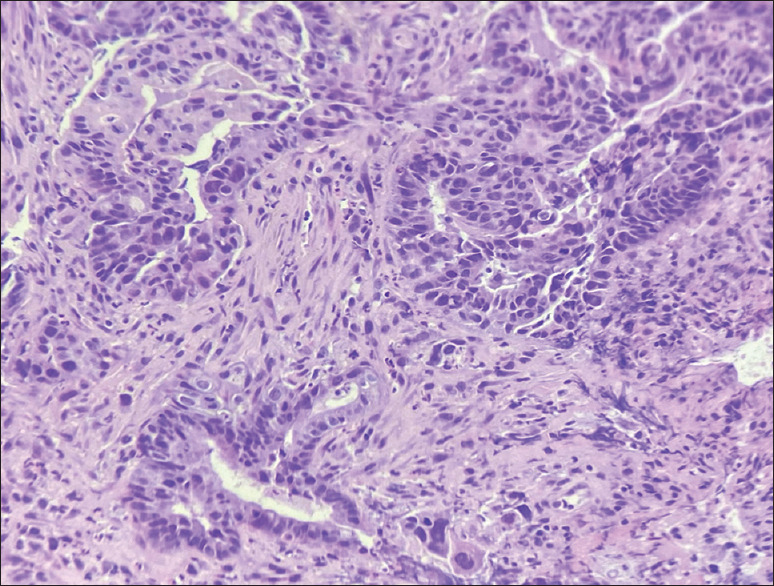
H and E staining showing a focus of high-grade biliary intraepithelial neoplasia/carcinoma in situ (on the top right) and a focus of invasive cholangiocarcinoma with glandular architecture and in isolated cells (at the bottom)
The management of pancreatobiliary diseases in patients with surgically altered anatomy (SAA) is technically challenging and associated with a significant number of failures.[1,2] EUS-HGS has emerged as an alternative procedure for achieving an endoscopic internal biliary drainage showing promising data in term of efficacy and safety, especially in SAA patients.[3,4] Recently, a case of DPOC few days after EUS-HGS for the management of difficult intrahepatic stones has been reported.[5]
EUS-HGS could be considered not only as a viable alternative for palliation of malignant jaundice but also as an entry port for therapeutic and diagnostic purposes.
Furthermore, to the best of our knowledge, this case first demonstrated that single session of EUS-HGS with DPOC might represent an effective alternative approach for biliary drainage and the assessment of CBD strictures in patients with SAA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Video Available on: www.eusjournal.com
REFERENCES
- 1.Fugazza A, Anderloni A, Paduano D, et al. Underwater cap-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: a pilot study [published online ahead of print, 2020 Nov 16] Endoscopy. 2020 doi: 10.1055/a-1311-9779. 10.1055/a-1311-9779. doi:10.1055/a-1311-9779. [DOI] [PubMed] [Google Scholar]
- 2.Mangiavillano B, Carrara S, Eusebi LH, et al. Water-filled technique for therapeutic pancreato-biliary EUS in patients with surgically altered anatomy. Endosc Int Open. 2021;9:E487–9. doi: 10.1055/a-1339-0690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khashab MA, El Zein MH, Sharzehi K, et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: An international comparative study. Endosc Int Open. 2016;4:E1322–7. doi: 10.1055/s-0042-110790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderloni A, Troncone E, Fugazza A, et al. Lumen-apposing metal stents for malignant biliary obstruction: Is this the ultimate horizon of our experience? World J Gastroenterol. 2019;25:3857–69. doi: 10.3748/wjg.v25.i29.3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parsa N, Runge T, Ichkhanian Y, et al. EUS-guided hepaticogastrostomy to facilitate cholangioscopy and electrohydraulic lithotripsy of massive intraductal stones after Roux-en-Y hepaticojejunostomy. VideoGIE. 2020;5:418–20. doi: 10.1016/j.vgie.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


