Abstract
Purpose:
To evaluate the effectiveness of Salud, Educación, Prevención, y Autocuidad/Health, Education, Prevention and Self-care (SEPA) to increase human immunodeficiency virus (HIV)/sexually transmitted infections (STI) prevention behaviors for Hispanic women delivered in a real-world setting.
Design:
Randomized controlled trial.
Setting:
Participants were recruited from the Miami Refugee Center, the Florida Department of Health, and publiclocations in Miami.
Participants:
Three hundred twenty Hispanic women.
Intervention:
The SEPA is a culturally tailored intervention developed to address HIV/STI risk behaviors among Hispanic women. The SEPA intervention consisted of three 2.5 hour sessions per week conducted with small groups. The SEPA sessions consisted of group discussions, role playing, negotiation skills, partner communication, and skills building as part of the methodology.
Measures:
Acculturation, HIV/STI risk behaviors, HIV knowledge, partner communication, intimate partner violence, drug/alcohol use, condom use.
Analysis:
Differences at baseline by group were assessed using Wilcoxon rank sum test, χ2, and a negative-binomial model. Changes in dependent variables, compared to baseline, were analyzed in separate models. Log-binomial models and negative binomial models were used for dichotomous and count/rate-type dependent variables.
Results:
Significant outcome improvements were observed in the SEPA group at 6 and 12 months follow-up. The adjusted prevalence of any condom use was 30% and 37% higher at each follow-up. The adjusted prevalence of answering 10/12 HIV knowledge questions correctly rose by 57% and 63% at each follow-up. Intimate partner violence was significantly lower at each subsequent time point (62% and 41% of baseline). Moderate depressive symptoms were reduced to 50% and 42%, getting drunk was reduced to 20% and 30%, and condom use self-efficacy was significantly higher (84% and 96%).
Conclusion:
The SEPA intervention reduced HIV/STI risk-related behaviors when delivered in a real-world setting. The results suggest that SEPA can be implemented in various settings to reach Hispanic women, and that SEPA could reach large numbers of women in an efficient, cost-effective way.
Keywords: Hispanic, women, HIV, community, health promotion
Introduction
Human immunodeficiency virus (HIV) infection can cause serious health problems among women and can generate new challenges related to care of the family, finding access to care and treatment, stigma, and immense individual and social economic costs.1–5 Medical costs of treating HIV represent a large fraction of the economic burden of HIV/AIDS.3 It is estimated that of all women living with HIV, only 45% are engaged in care and only 32% have achieved viral suppression.6
Despite efforts to decrease HIV infection, some groups of people in the United States are more affected by HIV/AIDS than others.6 Hispanics are the largest racial minority group in the United States and may face several challenges in getting the care they need to protect their health, including lack of insurance, language barriers, and higher rates of poverty than non-Hispanic whites.5,7 Hispanic women, in particular, have been identified as one of the groups most affected by HIV.7 In fact, in 2014 they were almost 4 times more likely to acquire HIV than their non-Hispanic white counterparts, with heterosexual transmission accounting for 86% of new cases of HIV in this group.8
Among Hispanic women, vulnerability to HIV has been shown to be influenced by factors including cultural values, substance abuse, depression, and intimate partner violence (IPV).9,10 Previous research indicates that cultural norms about gender roles and sexuality among Hispanics interact with IPV risk among women to disproportionately place them at risk for HIV. At the same time, the cultural values of machismo and marianismo promote controlling and risk-taking behaviors for Hispanic men and modesty and obedience in Hispanic women.11 These norms make it difficult for Hispanic women to talk about their sexuality with others, often limiting their knowledge regarding HIV risk and prevention, and interfere with their ability to communicate with their partners about safer sexual practices.12 In addition, the majority of Hispanic women do not feel susceptible to acquiring HIV, which reduces their awareness of their exposure to high-risk behaviors.13 All of these factors create a unique configuration of HIV risk among Hispanic women and make adoption of HIV prevention behaviors, a complex process for this population.
Although Hispanic women are disproportionately affected by HIV, few HIV sexual risk reduction interventions have demonstrated efficacy in decreasing HIV risky behaviors.14,15 Gender and culturally specific HIV prevention programs are needed to address the prevention of HIV infection among Hispanic women. The HIV/AIDS Prevention Research Synthesis project16 compiled a list of evidence-based interventions and best practices for HIV prevention. Only 2 intervention programs in the list specifically target heterosexual Hispanic women: Amigas, Mujeres Latinas, Informándonos, Guiándonos y Apoyándonos Contra El Sida/Friends, Latina women, informing, guiding and supporting each other against AIDS (AMIGAS)14 and Salud, Educación, Prevención y Autocuidado/Health, Education, Prevention and Self-care (SEPA).15 These interventions have documented improvements in condom use and other HIV risk reduction practices. In addition, the SEPA intervention has been found to be efficacious in preventing the biological risk for HIV (ie, preventing sexually transmitted infections [STI]) and decreasing IPV.15 Despite the promise of the SEPA intervention in reducing HIV risk among Hispanic women, this intervention was delivered only in controlled environments with highly trained research staff. Behavioral interventions for HIV prevention must be not only effective, but also cost-effective, efficient, and ready for implementation in real-world settings with fidelity.17 Successfully translating research into population based-interventions that promote HIV risk prevention and behavioral change in the community is of vital importance to improve minority health and to eliminate health disparities.
The aim of this study was to evaluate the effectiveness of SEPA to increase HIV prevention behaviors and to reduce the incidence of STIs for Hispanic women when delivered in a real-world setting by community agency personnel.
Methods
Design
This is a randomized controlled experimental study with adult Hispanic women in Miami-Dade County, Florida, that compared SEPA to a delayed intervention control; SEPA stands for Salud, Educacion, Prevencion y Autocuidado, which translates to Health, Education, Prevention, and Self-Care.
Sample and Setting
A sample of 320 Hispanic women participated in the study. Most women (96%) were born outside the United States. The majority of participants were women born in Cuba (54.7%), followed by Nicaragua (9.4%), and Colombia (9.1%). Only 14 (4.4%) were born in the United States. The rest of the women (22.4%) were from other countries in Central and South America (eg, Honduras, Dominican Republic, and Venezuela). Power analyses were conducted using Monte Carlo simulation to determine the sample size assuming 30% attrition by the final follow-up.18 Eligibility criteria included (a) being age 18 to 50; (b) self-identified as a Hispanic woman; (c) sexual activity within the last 3 months; (d) not having ever participated in a previous SEPA trial.15,19 Participants were women recruited from the Miami Refugee Center and the Florida Department of Health, as well as by distribution of flyers and outreach at public locations, including grocery stores, churches, and community organizations near the study office in downtown Miami, an area predominantly Hispanic (70%) in population.20 The interviews, group sessions and testing were conducted in a private room at the University of Miami Hospital. We selected this place because participants were familiar with the site and could easily access this location.
The study obtained institutional review board approval from the Florida Department of Health. After participants read and signed the informed consent form, trained bilingual female research staff conducted private interviews in the participants’ preferred language (Spanish or English) employing a standardized protocol, each lasting approximately 2 hours. Participants were assessed at baseline and subsequently at intervals of 6 and 12 months post-baseline utilizing secure web-based software (e-Velos) for electronic documentation of responses. After each assessment, all women in the study were tested for STIs (chlamydia, gonorrhea, and trichomoniasis), received HIV testing and counseling, and finally were randomized using a permuted-block randomization procedure.
In relation to STI testing, chlamydia and gonorrhea testing was performed using amplified DNA assays in urine. Trichomoniasis testing was performed using the APTIMA Trichomonas vaginalis assay, also with a sample of voided urine. Rapid HIV test and counseling was also offered to all participants. Food and Drug Administration approved rapid finger stick blood HIV test, OraQuick Advance Rapid Antibody Test HIV-1/2 was used. Testing was entirely voluntary for participants, and HIV-certified counselors provided pre- and posttest HIV counseling. The result of the HIV rapid test was provided to each participant during posttest counseling, approximately 30 minutes after the test was performed. In addition, women expressing concerns regarding IPV were provided appropriate services. None of the women refused HIV testing and counseling in the study.
Intervention
The SEPA is a culturally tailored program developed to address HIV and other STI risk behaviors, including substance abuse and IPV among Hispanic women.21 The SEPA intervention consisted of three 2.5 hour sessions per week conducted with small groups of 6 to 8 participants. Participants chose whether groups were conducted in English or Spanish according to their preference. The SEPA sessions consisted of group discussions, role playing, negotiation skills, partner communication, and skill building as part of the methodology. Sessions were facilitated by bilingual Hispanic bicultural facilitators from the Department of Health. All facilitators possessed bachelor’s degree in education. None of the facilitators had previous SEPA experience which provided a “real-world” context for this study, in contrast to the original trial, for which all facilitators were research assistants trained and certified by the National Faculty of the American Red Cross as HIV instructors and counselors. All facilitators received 3 days of training from experienced facilitators and received feedback about the implementation of the intervention during the sessions (fidelity assessment). To assist in the training and ensure fidelity, a copyrighted manual available in English and Spanish was used during the training. These manuals were designed for this intervention to be used in the training of community agency facilitators. Implementation fidelity for SEPA was assessed utilizing a SEPA Implementation Fidelity Assessment Check-list. This checklist includes techniques that the SEPA facilitators must follow to conduct the intervention properly. The checklist includes 3 main sections (ie, Rapport and Trust, Communication and Group Dynamics, and Content of Session) and contains a total of 20 items. This checklist was used in the prior efficacy studies. In the past studies, fidelity ratings have been very high with facilitators adhering to over 80% of the intervention’s required behaviors. In this study, 2 co-investigators who also were former facilitators conducted fidelity ratings together with each facilitator. Fidelity was conducted until each facilitator adhered to over 80% of the intervention’s required behaviors. This occurred before the end of the first intervention for each facilitator. The interrater reliability was above 90%. The following observations were rated by both facilitators as completely carried out: (a) role of the facilitator during the session (eg, facilitator is organized and familiar with the intervention, models skills appropriately according to the contents of the session), (b) feedback and verbal communication skills (eg, facilitator offers verbal encouragement and praise on an ongoing basis), (c) group process skills (eg, members talk to one another about session topics), and (d) facilitator’s behaviors for the session as a whole (eg, discuss sensitive issues in a comfortable manner). Overall, the assessment of the facilitators was rated as excellent (on a scale from 1 to 5, with 1 = poor and 5 = excellent).
The conceptual model of SEPA integrates Freire’s pedagogy22 and Bandura’s Social Cognitive model.23 Freire’s pedagogy informed the establishment of an atmosphere that encouraged women to engage actively in discussion and activities during the sessions, affirming the importance of each participant and enhancing the skills and knowledge generated during the program. By providing the opportunity to engage in the performance of key behaviors, participants were able to augment outcome expectancies (expectations of positive rather than negative outcomes) and in turn encourage self-efficacy (confidence in the ability to perform a behavior). In accordance with the Social Cognitive model, building the skills of outcome expectancies and self-efficacy is crucial because individuals who believe they have the capability to perform an action will be more likely to engage in the action. In this context, this multifaceted approach instructs participants regarding the benefits of condom use and elicits behavior change. Previous research indicates the Social Cognitive Model may be an especially relevant theory for the examination of Hispanic sexual behavior.24
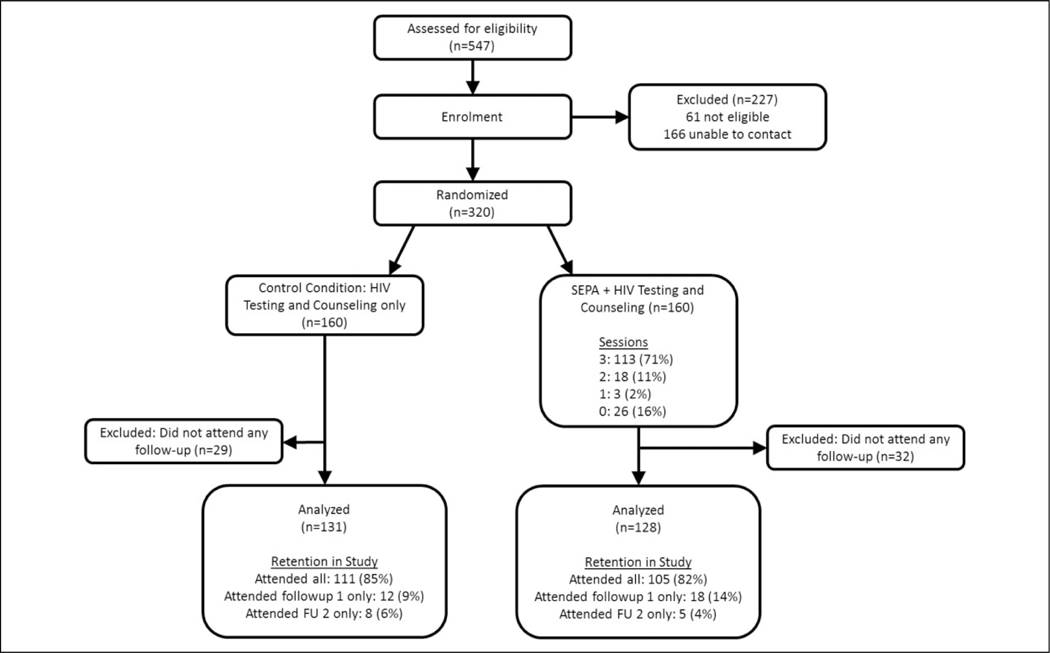
All 36 groups were conducted in Spanish for this study. Of the 160 women randomized to the SEPA condition, the majority (113, 84%) attended all the 3 sessions; 18 (13%) attended 2 sessions, 3 (2%) attended 1 session; and 26 (19%) women attended no sessions.
Control Condition
After women in the control condition completed their 12-month assessment, they were invited to participate in the SEPA intervention. The 3-session intervention was condensed in 1 day for these participants.
Retention
Participant retention strategies included collecting multiple communication contacts from each participant, conducting interviews at community sites easily accessible for participants, and following up with telephone calls and mail correspondence when necessary. For each study interview, participants were compensated $50. Participants were also provided $20 per SEPA session attended to support the costs of transportation and childcare. Monetary compensation for attending study sessions may not be necessary in all settings, but in the city where this study was conducted the cost of transportation may have been an important barrier to participation.
Measures
All measures in the interview were available in Spanish and English and had been used in previous research with Hispanic samples. As part of the interview, each participant was administered a survey to collect demographic information.
Acculturation
The Bidimensional Acculturation Scale25 includes 24 items to assess how acculturated Hispanics are to the US culture (Americanism) and their culture of origin (Hispanicism). The 12 items that measure each cultural domain are averaged separately. At baseline in this sample, both the Hispanicism and Americanism subscales had high internal consistency (α = .83 and .96, respectively).
Human immunodeficiency virus/STI risk behaviors
The survey included several questions asking the participant to report HIV/STI risk behaviors and information about partners. Questions asked whether the participants had a main/regular partner and/or partner(s) who were not main/regular partners in the past 30 days. Women also reported the number of times they had oral, anal or vaginal sex and the number of times condoms were used. The following measures analyzed for observations where at least 1 sex event was reported and set as missing if no sex events were reported: (a) percent of sex events for which a condom was used, (b) any condom use (yes/no), and (c) the number of condomless sex events.
Human immunodeficiency virus Knowledge
Human immunodeficiency virus knowledge was assessed with a 12-item scale26 containing questions about HIV transmission, prevention, and consequences, for example, “Condoms cause men physical pain.” Items answered correctly were summed to a total score. The measure was dichotomized based upon whether each participant answered at least 10 of the 12 questions (83%) correctly to indicate a relatively high level of HIV-related knowledge.
Partner Communication
Partner communication was assessed using the Communication with Partner Scale,27 which has 10 items (eg, “Asked your partner(s) how he felt about using condoms before you had intercourse?”) about whether (yes or no) the woman discussed topics related to HIV/STI concerns with their primary sexual partner. This scale had good internal consistency across all 3 time points (α = .89). To correct for extreme skew, a positive response to any of these behaviors was coded as yes” and none as “no.”
Intimate Partner Violence
Intimate partner violence was assessed using the Partner-to-you scale and You-to-partner scales from the Revised Conflict Tactics Scale short form.28 The scale has items to assess the frequency of 12 behaviors (eg, “insulted you,” “beat you up,” “forced you to have sex”), which are summed for a total score. The scale has an extreme positive skew, so a positive response to any of these behaviors was coded as “yes,” while none was coded as “no.” In this sample, Cronbach α was .89 for the Partner-to-you scale and .83 for the You-to-partner scale.
Depressive Symptoms
Symptoms were measured with the Patient Health Questionnaire (PHQ-9),29 a 9-item scale commonly used for depression screening in primary care and other health settings. The items are on a 4-point Likert scale, from 0 (not at all) to 3 (every day). The PHQ-9 had high internal consistency (α =.90) in this sample. The scale was dichotomized to categorize moderate depression (based upon a score of 10 or more).28
Drug and Alcohol Use
Participants also reported drug and alcohol use during the last 3 months, and 2 dichotomous measures were constructed that queried whether the participant had been high on drugs or had been drunk.
Self-Efficacy Condom Use
Self-efficacy was a 7-item measure.19 Examples of items are “it would be easy to make my partner(s) use condoms,” and “I feel confident that I can put on a condom on myself/my partner so it won’t break or come off.” Each item had a 4-point scale, from 1 (strongly disagree) to 4 (strongly agree), assessing confidence with each behavior. This scale had internal consistency across all 3 assessments (α = .79). To correct for extreme skew, this variable was dichotomized using a median split (median = 3.57).
Analyses.
The data analyses were conducted among all participants who completed the baseline survey and at least 1 follow-up survey. Participants were analyzed in their original assigned treatment condition regardless of SEPA sessions attended to support an intent-to-treat analysis protocol. Participant characteristics including demographics, cultural and relationship attributes, HIV/STI risk behaviors with primary partner, and potential mediators/other outcomes were described. Differences in characteristics at baseline by study group were assessed using the Wilcoxon rank sum test for continuous variables, χ2 for proportions, and a negative-binomial model for the rate of sex events with condoms used per the total number of sex events. Summary measures (means and percentages) were generated for dependent variables by study group and time point. Changes in dependent variables at each follow-up as compared to baseline were assessed in separate models by study group. Log-binomial models and negative binomial models were used for dichotomous and count/rate-type dependent variables, respectively. Variables associated with missing either follow-up were included in the models. These included age, whether the participant was born in the United States, and years of education. To assess significant differences in changes at follow-up by study group, models including both groups and an interaction term between follow-up and group were also conducted.
Results
Of the n = 320 who were randomized, n = 259 (81%) were included in the analyses (Figure 1). Participants who did not attend any follow-up data collection surveys were excluded from both the SEPA intervention group (n = 32 excluded) and the comparison group (n = 29 excluded). Overall, individuals who were excluded due to not having a follow-up were older (mean age 35.5 compared to 31.6 among those analyzed, P < .01), and, among those not born in the United States, had been in the country longer (mean of 8.2 compared to 6.0 years). No other statistically significant differences were observed based upon exclusion. Among those analyzed, more than 80% completed both follow-up surveys.
Figure 1.
Summary of exclusions and lossess to follow-up, randomized tiral of SEPA, 2013–2017. SEPA indicates Salud, Educacion, Prevencion, y Autocuidado/Health, Education, Prevention and Self-care.
Participant characteristics at baseline are summarized in Table 1. Most participants were born outside of the United States, less than half had health insurance, and more than half were living with their partner. Fewer than one-third were employed. At baseline, condoms were used in 31% of sex events reported in each group, and the mean number of condomless sex events in the past 30 days was 7.5 for SEPA participants and 6.9 for comparison group participants. Any condom use was reported by 35% and 40% of SEPA and comparison group participants, respectively. Just over half of the participants correctly answered at least 10 of the 12 HIV knowledge questions. Intimate partner violence from their partner was reported by 47% and 41% of the SEPA and comparison participants, respectively. Drug use was infrequently reported (<4%), and being drunk one or more times was reported by less than 13% of the participants. No statistically significant differences were observed when comparing the attributes of the SEPA group to the comparison group.
Table 1.
Characteristics of Participants at Baseline in a Randomized Trial of SEPA, 2013–2017.a
| Characteristics | SEPA, n = 128 | Control, n = 131 | P Value |
|---|---|---|---|
| Demographic, cultural, and relationship attributes | |||
| Age, mean (SD) | 35.23 (8.93) | 35.73 (9.32) | .5668 |
| Education in years, mean (SD) | 13.84 (3.22) | 13.35 (3.35) | .2603 |
| Family income in $/month, mean (SD) | 1667.76 (976.60) | 1643.87 (926.50) | .8737 |
| Born outside of United States, % | 96.9 | 94.7 | .3761 |
| Years in United States, mean (SD) | 8.29 (7.91) | 8.06 (6.97) | .9306 |
| Americanism, mean (SD) | 2.05 (0.80) | 1.95 (0.76) | .2950 |
| Hispanicism, mean (SD) | 3.49 (0.39) | 3.50 (0.35) | .7908 |
| Employed, % | 29.7 | 29.0 | .9044 |
| Has health insurance, % | 44.5 | 41.2 | .5905 |
| Living with partner, % | 65.6 | 70.2 | .4273 |
| HIV/STIs risk behaviors with primary partner,b (last 30 days) | |||
| % of sex events condoms used,c mean (SD) | 30.97 (44.49) | 30.98 (42.61) | .8172 |
| Any condom use,c % | 35.0 | 39.7 | .4668 |
| Number of condomless sex events, mean (SD) | 7.51 (8.16) | 6.86 (7.79) | .6469 |
| Potential mediators and other outcomes | |||
| HIV knowledge (≥ 80%), % | 50.8 | 51.1 | .9533 |
| Partner communication regarding sex (any), % | 69.3 | 68.7 | .9185 |
| Intimate partner violence from partner (any), % | 46.9 | 41.2 | .3595 |
| Intimate partner violence toward partner (any), % | 39.8 | 36.6 | .5959 |
| Depressive symptoms (moderate/10+), % | 13.3 | 12.2 | .7967 |
| Drunk (last 3 months, 1+ times), % | 12.5 | 12.2 | .9442 |
| Self-efficacy (7 items, above median of 3.57), % | 32.0 | 33.6 | .7897 |
Abbreviations: SD, standard deviation; SEPA, Salud, Educacion, Prevencion, y Autocuidado/Health, Education, Prevention and Self-care; STI, sexually transmitted infections.
Statistical testing for differences was conducted using a Wilcoxon rank sum test for continuous variables and χ2 for proportions (presented as percentages), and a negative-binomial model for the rate of sex events with condoms used per the total number of sex events (presented as a percentage).
Oral, anal, and/or vaginal partners.
Denominator includes observations where one or more of the sex event type was reported.
Changes in dependent variables by study group at each time point are summarized in Table 2. Several significant improvements in outcomes were observed in the SEPA group at follow-up (Table 3). These included a higher percentage of sex events where condoms were used at follow-up 2. For the SEPA group, the adjusted prevalence of any condom use was 30% and 37% higher at follow-up 1 and 2, respectively. The adjusted prevalence of answering at least 10/12 HIV knowledge questions correctly rose by 57% and 63% at each successive follow-up. Intimate partner violence from partner was significantly lower at each time subsequent point (62% and 41% of baseline), as was IPV toward partner (63% and 31% of baseline). Moderate depressive symptoms were reduced to 50% and 42%, getting drunk in the last 3 months was reduced to 20% and 30%, and condom use self-efficacy was significantly higher (84% and 96% increase in the prevalence of higher than the median).
Table 2.
Description of Outcomes Among Participants of SEPA and Control Group Preintervention and 6/12 Months After the Intervention, 2013 to 2017.a
| Condition | Baseline | 6 Months | 12 Months | |
|---|---|---|---|---|
| HIV/STIs risk behaviors,b (last 30 days) | ||||
| % of sex events condoms used,c mean (SD) | SEPA | 30.97 (44.49) | 31.75 (41.52) | 38.35 (44.60) |
| Control | 30.98 (42.61) | 40.17 (44.80) | 42.73 (44.41) | |
| Any condom use,c % | SEPA | 35.0 | 44.4 | 47.4 |
| Control | 39.7 | 49.0 | 53.9 | |
| Number of condomless sex events, mean (SD) | SEPA | 7.51 (8.16) | 7.31 (7.82) | 5.91 (6.38) |
| Control | 6.86 (7.79) | 5.89 (8.30) | 6.28 (9.10) | |
| Potential mediators and other outcomes | ||||
| HIV knowledge (≥80%), % | SEPA | 50.8 | 78.9 | 82.7 |
| Control | 51.1 | 58.5 | 75.6 | |
| Partner communication regarding sex (any), % | SEPA | 69.3 | 60.3 | 62.4 |
| Control | 68.7 | 62.2 | 69.6 | |
| Intimate partner violence from partner (any), % | SEPA | 46.9 | 28.5 | 19.1 |
| Control | 41.2 | 23.6 | 16.9 | |
| Intimate partner violence toward partner (any), % | SEPA | 39.8 | 25.2 | 12.7 |
| Control | 36.6 | 14.6 | 16.1 | |
| Depressive symptoms (moderate/10+), % | SEPA | 13.3 | 6.5 | 5.5 |
| Control | 12.2 | 7.3 | 7.6 | |
| High on drugs (last 3 months, 1+ times), % | SEPA | 1.6 | 0.8 | 0 |
| Control | 3.8 | 0 | 0 | |
| Drunk (last 3 months, 1+ times), % | SEPA | 12.5 | 2.4 | 3.6 |
| Control | 12.2 | 4.9 | 3.4 | |
| Self-efficacy (7 items, above median of 3.57), % | SEPA | 32.0 | 57.7 | 61.8 |
| Control | 33.6 | 43.9 | 48.7 |
Abbreviations: SEPA, Salud, Educacion, Prevencion y Autocuidado/Health, Education, Prevention and Self-care; STIs, sexually transmitted infections.
n = 128 SEPA participants and n = 131 control participants.
Oral, anal, and/or vaginal partners.
Denominator includes observations where one or more of the sex event type was reported.
Table 3.
Changes in Outcomes Among Participants of SEPA Participants, Comparing Follow-Up at 6/12 Months After the Intervention to Baseline/Preintervention, 2013 to 2017.
| SEPA Participants, n = 128 | Comparison Group, n = 131 | |||
|---|---|---|---|---|
|
|
|
|||
| 6 Months, Ref = Baseline | 12 Months, Ref = Baseline | 6 months, Ref = Baseline | 12 Months, Ref = Baseline | |
| HIV/STIs risk behaviors,a (last 30 days) | ||||
| % of sex events condoms used,b aRR (95% CI) | 1.08 (0.84–1.37) | 1.27 (1.01–1.59)c | 1.29 (1.02, 1.64)c | 1.38 (1.07–1.77)c |
| Any condom use,b aPR (95% CI) | 1.30 (1.03–1.63)c | 1.37 (1.10–1.70)d | 1.25 (1.00–1.56)c | 1.37 (1.09–1.73)d |
| Number of condomless sex events, aRR (95% CI) | 0.96 (0.77–1.20) | 0.80 (0.66–0.97)c | 0.88 (0.70–1.11) | 0.92 (0.69–1.22) |
| Potential mediators and other outcomes | ||||
| HIV knowledge (≥80%), aPR (95% CI) | 1.57 (1.33–1.86)e | 1.63 (1.37–1.95)e | 1.15 (0.94–1.40) | 1.49 (1.24–1.78)e |
| Partner communication regarding sex (any), aPR (95% CI) | 0.88 (0.75–1.03) | 0.91 (0.78–1.05) | 0.91 (0.78–1.07) | 1.02 (0.87–1.20) |
| Intimate partner violence from partner (any), aPR (95% CI) | 0.62 (0.46–0.83)d | 0.41 (0.28–0.58)e | 0.60 (0.44–0.80)e | 0.42 (0.28–0.63)e |
| Intimate partner violence toward partner (any), aPR (95% CI) | 0.63 (0.46–0.86)d | 0.31 (0.19–0.53)e | 0.42 (0.27–0.65)e | 0.45 (0.29–0.69)e |
| Depressive symptoms (Moderate/10+), PR (95% CI)f | 0.50 (0.25–0.99)c | 0.42 (0.18–0.96)c | 0.61 (0.31–1.18) | 0.64 (0.35–1.16) |
| Drunk (last 3 months, 1+ times), aPR (95% CI) | 0.20 (0.06–0.66)d | 0.30 (0.11–0.83)c | 0.46 (0.19–1.10) | 0.29 (0.11–0.75)c |
| Self-efficacy (7 items, above median of 3.57) aPR (95% CI) | 1.84 (1.40–2.43)e | 1.96 (1.50–2.56)e | 1.30 (0.99–1.71) | 1.44 (1.11–1.88)d |
Abbreviations: aPR, adjusted prevalence ratio (log binomial model); aRR, adjusted rate ratio (negative binomial model); CI, confidence interval; NC, model was nonconvergent; models adjusted for age, born in the United States, and years of education; SEPA, Salud, Educacion, Prevencion y Autocuidado/Health, Education, Prevention and Self-care; STIs, sexually transmitted infections.
Oral, anal, and/or vaginal partners.
Denominator includes observations where one or more of the sex event type was reported.
P < .05.
P < .01.
P < .001.
Unadjusted (adjusted model did not converge); reporting getting high on drugs could not be analyzed due to a small number of positive responses.
Similar improvements in outcomes were observed in the comparison group. Significant improvements in the percentage of sex events with condoms used was observed at follow-up 1 in the comparison group only, and both groups were significantly improved at the second follow-up. For some other outcomes, significant improvements were observed in the SEPA group but not in the comparison group. These include the number of condomless sex events at follow-up 2, moderate depressive symptoms at both follow-ups, condom use self-efficacy at follow-up 1, being drunk in the past 3 months, and HIV knowledge. In the model assessing the interaction between follow-up and SEPA participation (results not shown), HIV knowledge improved more significantly at the first follow-up for the SEPA group (adjusted prevalence ratio = 1.37, P < .05), but no other significantly better improvements were observed in the SEPA group as compared to the comparison group.
Discussion
In this study, we found significant improvements in HIV/STI risk behaviors, HIV knowledge, condom self-efficacy, IPV, depressive symptoms, and drug/alcohol use among participants after completing the SEPA intervention compared to their delayed intervention controls. These findings are consistent with previous efficacy trials of SEPA in 2 different urban areas in the United States, Chicago, and South Florida,15,19 as well as in a more rural farmworker community.30 More specifically, in the first efficacy trial of SEPA, Puerto Rican and Mexican adult female participants randomized to the intervention group reported significant improvements in HIV knowledge, partner communication, risk-reduction behavioral intentions, and condom use.19 The second trial of SEPA expanded upon these initial findings to demonstrate that the intervention was also effective for more diverse groups of Hispanic women (ie, countries of origin, economic levels, and ages) and had an impact on reducing IPV, substance abuse, and the incidence of STIs (ie, chlamydia), well established risk factors for HIV.15 The findings from the present study add to this literature by demonstrating the effectiveness of SEPA when delivered in less controlled, real-world settings.
The increase in HIV knowledge among SEPA participants significantly exceeded increases among nonparticipants 6 months after the intervention. This is important given that studies have highlighted the prevalence of low HIV knowledge among Hispanic women.13,31,32 Poor HIV knowledge has been associated with engagement in risky sexual behaviors,33 while increased knowledge encourages testing,34 timely receipt of care, and engagement in treatment to successfully manage disease if infected.35 A recent systematic review and meta-analysis of HIV prevention interventions for ethnic minority women observed increase in HIV knowledge as an outcome measure, along with behavior change and STI transmission reduction, underscoring the overall effectiveness of interventions.36 Our study provides evidence that exposing Hispanic women to culturally tailored programs aimed at improving HIV knowledge, when combined with strategies that address skills, can significantly reduce their participation in risky behaviors, reducing their risk of HIV infection.
Another finding from our study was the significant improvement in condom use self-efficacy among participants in the SEPA intervention group. The impact of this outcome should be considered in the context that the greatest risk for HIV transmission for Hispanic women is from heterosexual intercourse.6,37 Furthermore, the Centers for Disease Control and Prevention38 recommends using condoms for every anal and vaginal sexual activity to prevent HIV infection. Thus, this highlights the importance of condom-use self-efficacy in HIV prevention. Male condoms are the most commonly used in heterosexual relationships,39 and this often requires a certain level of relationship power from the females to negotiate condom use during sexual activity.39 The SEPA’s measure of condom use self-efficacy estimates not only how confident women feel about putting on condoms themselves, but also how confident they feel about putting it on their partners.15 Thus, this is an equally good estimate of their negotiating power is requesting condom use from their partners. Positive correlations have been observed between condom use self-efficacy and condom use consistency among men and women,39 which can contribute to HIV/STI prevention outcomes.
In addition to reducing HIV/STI risk, SEPA reduced exposure to IPV and drug/alcohol use. These factors have been commonly cited in the literature as having associations with increased risk of HIV infection, particularly among Hispanic women.10,13,40,41
Depressive symptoms had also significantly reduced by the 12-month follow up of SEPA. The importance of this outcome in validating the effectiveness of the SEPA program should be examined within the context that females and persons of Hispanic origins respectively have the highest and second highest rates of depression in the United States.42 More importantly, significant associations between depressive symptoms and HIV risk among Hispanic women exist in the literature.40 Depressive symptoms have also been found to inversely correlate with self-esteem among Hispanic women.43 The decreased incidence of depressive symptoms in our study may have resulted from the cultural tailoring of the SEPA program, which allowed women to openly discuss their concerns and fears about HIV infection. The SEPA might have also provided a comfortable, cultural forum for these women to empower themselves, enhance their HIV knowledge, and experience higher levels of self-esteem. This is evidenced by the persistent and statistically significant increases in HIV knowledge and self-efficacy at the 6- and 12-month follow-up among women in the SEPA group.
Retention in the SEPA program was higher among participants in this study than it was in a previous trial. Of the n = 160 intervention participants, all sessions were attended by 71% of the participants in the SEPA group, and only 16% failed to attend one or more sessions. By comparison, 60% of intervention participants in a trial published in 2012 attended one or more sessions, and 52% received 3 or more sessions.15 The retention rate observed in the program could be explained by the high level of engagement among women enrolled in it. Furthermore, engagement in the program could have been facilitated by its cultural underpinnings, the relevant topics addressed therein, and its enactment in a real-life community setting.
In this study, the comparison group did receive services that overlapped with those provided as part of the SEPA intervention. Comparison clients were offered HIV testing and counseling, and, if needed, services for IPV, resulting in a comparison between competing interventions. We observed significant improvements in HIV/STI risk behaviors, HIV knowledge, IPV, alcohol use, and condom self-efficacy in the comparison group as a result, although the increase in HIV knowledge was significantly higher for SEPA participants. This receipt of overlapping services limited our ability to draw conclusions regarding differential changes in the SEPA group after the intervention. Future comparative effectiveness research is needed to examine the cost-benefit of adding behavioral interventions such as SEPA to standard HIV testing and counseling. Despite this limitation, however, knowledge improved significantly more in the group that received SEPA than in the control group, and several outcomes significantly improved after SEPA participation. Both the treatment and comparison groups experienced similar high losses to follow-up, which may limit the external validity of our results. In contrast to a highly controlled efficacy trial, however, this study was designed to reflect “real world” implementation of SEPA at community-based organizations. Individuals who are older or have been in the United States for a longer period of time experienced a higher rate of loss, and more support to retain individuals in those groups may be warranted in future evaluation studies.
Limitations
Limitations of this study are as follows: (a) the results were mostly self-reported and, as such, possibly subject to recall bias by the participants; (b) the sample consisted of a geographically secluded portion of this unique population, which may not lend itself to extrapolate to a larger population; (c) participants in the intervention group received 20 dollars per session as an incentive for participation, this can represent a potential limitation for future implementation.
Conclusion
When considered as a whole, the results of this study have broad implications for the implementation of SEPA in a real-world setting by community agency personnel offering culturally tailored HIV prevention. The SEPA has the potential to address several important HIV risk factors for Hispanic women including IPV, depression, and lack of knowledge about HIV, which can play a crucial role in prevention transmission of the virus.
SO WHAT?
Hispanic women have been identified as one of the groups most affected by HIV. They are almost 4 times more likely to acquire HIV than their Caucasian counter-parts, with heterosexual transmission accounting for 86% of new cases.
What does this article add?
This study evaluates effectiveness of the SEPA intervention to increase HIV/sexually transmitted infections (STI) prevention behaviors for Hispanic women. The SEPA consists of 3 sessions delivered in a real-world setting by community agency personnel in South Florida covering HIV/STI prevention (eg, communication, condom use, violence). Results showed significant improvements in HIV/STI risk behaviors, HIV knowledge, condom self-efficacy, intimate partner violence, depressive symptoms, and drug/alcohol use after participation in SEPA.
What are the implications for health promotion practice or research?
Successfully translating research into population based-interventions that promote HIV prevention and behavioral change in the community is vital to improve minority health and to eliminate health disparities.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities grant P60MD002266.
Footnotes
Authors’ Note
Rosina Cianelli is also affiliated with Escuela de Enfermeria, Pontificia Universidad Catolica de Chile, San Joaquin, Region Metropolitana, Chile.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.HIV.gov. HIV and women’s health. 2018. https://www.hiv.gov/hiv-basics/staying-in-hiv-care/other-related-health-issues/womens-health-issues/. Accessed October 11, 2018.
- 2.Alexander L, LaRosa J, Bader H, Garfield S, Alexander W. New Dimensions in Women’s Health. 5th ed. Sudbury, MA: Jones and Bartlett Publishers; 2010. [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV cost-effectiveness. 2017. http://www.cdc.gov/hiv/prevention/ongoing/costeffectiveness/. Accessed October 11, 2018.
- 4.Centers for Disease Control and Prevention. CDC’s HIV prevention progress in the United States, 2015. http://www.cdc.gov/hiv/dhap/progress/index.html. Accessed October 11, 2018.
- 5.Centers for Disease Control and Prevention. Hispanic health. 2015. https://www.cdc.gov/vitalsigns/hispanic-health/index.html. Accessed October 11, 2018.
- 6.Centers for Disease Control and Prevention. HIV among Hispanics/Latinos. 2018. https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html. Accessed October 11, 2018.
- 7.Paz K, Massey KP. Health disparity among Latina women: comparison with non-Latina women. Clin Med Insights Womens Health. 2016;9(suppl 1):71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. HIV surveillance report; 2018. https://www.cdc.gov/hiv/pdf/library/repvailableorts/surveillance/cdc-hiv-surveillance-report-us.pdf. Accessed October 11, 2018.
- 9.González-Guarda RM, Florom-Smith AL, Thomas T. A syndemic model of substance abuse, intimate partner violence, HIV infection, and mental health among Hispanics. Public Health Nurs. 2011;28(4):366–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez-Guarda RM, McCabe BE, Florom-Smith A, Cianelli R,Peragallo N. Substance abuse, violence, HIV, and depression: an underlying syndemic factor among Latinas. Nurs Res. 2011;60(3):182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cianelli R, Ferrer L, McElmurry B. Issues on HIV prevention among low-income Chilean women: machismo, marianismo and HIV misconceptions. Cult Health Sex. 2008;10(3):297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cianelli R, Villegas N, Lawson S, et al. Unique factors that placeolder Hispanic women at risk for HIV: intimate partner violence, machismo, and marianismo. J Assoc Nurses AIDS Care. 2013;24(4):341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cianelli R, Villegas N, Gonzalez-Guarda R, Kaelber L, PeragalloN. HIV susceptibility among Hispanic women in South Florida. J Community Health Nurs. 2010;27(4):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wingood GM, Diclemente RJ, Villamizar K, et al. Efficacy of ahealth educator-delivered HIV prevention intervention for Latina women: a randomized controlled trial. Am J Public Health. 2011; 101(12):2245–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peragallo N, Gonzalez-Guarda R, McCabe B, Cianelli R. Theefficacy of an HIV risk reduction intervention for Hispanic women. AIDS Behav. 2012;16(5):1316–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Archived interventions, 2017. https://www.cdc.gov/hiv/research/interventionresearch/compendium/rr/archive.html. Accessed October 11, 2018.
- 17.Collins L, Kugler K, Gwadz M. Optimization of multicomponent behavioral and biobehavioral interventions for the prevention and treatment of HIV/AIDS. AIDS Behav. 2016;20(suppl 1):S197–S214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muthén LK, Muthén BO. Mplus User’s Guide. 5th ed. Los Angeles, CA: Muthén and Muthén; 2007. [Google Scholar]
- 19.Peragallo N, DeForge B, O’campo P, et al. A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nurs Res. 2005;54(2):108–118. [DOI] [PubMed] [Google Scholar]
- 20.City of Miami Planning and Zoning. Census 2010. 2013. http://www.miamigov.com/planning/census2010.html. Accessed October 11, 2018.
- 21.Centers for Disease Control and Prevention. HIV/AIDS REP Packages, 2017. https://www.cdc.gov/hiv/research/interventionresearch/rep/packages/index.html. Accessed October 11, 2018.
- 22.Freire P. Pedagogy of the Oppressed. Trans. Myra Bergman Ramos. New York: Continuum; 1970: 65–80. [Google Scholar]
- 23.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 24.Wingood GM, DiClemente RJ. HIV sexual risk reduction interventions for women: a review. Am J Prev Med. 1996;12(3):209–217. [PubMed] [Google Scholar]
- 25.Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS). Hisp J Behav Sci. 1996;18(3):297–316. [Google Scholar]
- 26.Heckman TG, Kelly JA, Sikkema K, et al. HIV risk characteristics of young adult, adult, and older adult women who live in innercity housing developments: implications for prevention. J Women’s Health. 1995;4(4):397–406. [Google Scholar]
- 27.Catania J. Dyadic Sexual Communication Scale: Handbook of Sexuality Related Measures. Thousand Oaks, California: SAGE Publications; 1986. [Google Scholar]
- 28.Straus MA, Douglas EM. A short form of the revised conflicttactics scales, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanchez M, Rojas P, Li T, et al. Evaluating a culturally tailored HIV risk reduction intervention among Latina immigrants in the farmworker community. World Medical Health Policy. 2016; 8(3):245–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knowledge Hillman J., attitudes, and experience regarding HIV/AIDS among older adult inner-city Latinos. Int J Aging Hum Dev. 2008;66(3):243–257. [DOI] [PubMed] [Google Scholar]
- 32.Torres ME, Murray A, Meetze EG, Gaul Z, Sutton MY. HIV knowledge among pregnant Latinas in rural South Carolina. J Immigr Minor Health. 2017;19(4):897–904. [DOI] [PubMed] [Google Scholar]
- 33.Kassa GM, Degu G, Yitayew M, et al. Risky sexual behaviors and associated factors among Jiga high school and preparatory school students, Amhara region, Ethiopia. Int Sch Res Notices. 2016; 2016:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen ZW, Dai SY, Ye DQ. Intention to undergo HIV testing and associated factors among women in one high-HIV prevalence city. Int J Nurs Prac. 2017;23(3):1–6. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Selected national HIV prevention and care outcomes in the United States, 2018. https://www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-national-hiv-care-outcomes.pdf. Accessed October 11, 2018.
- 36.Ruiz-Perez I, Murphy M, Pastor-Moreno G, Rojas-García A, Rodríguez-Barranco M. The effectiveness of HIV prevention interventions in socioeconomically disadvantaged ethnic minority women: a systematic review and meta-analysis. Am J Public Health. 2017;107(12):e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. HIV among women.2019. https://www.cdc.gov/hiv/group/gender/women/index.html. Accessed October 11, 2018.
- 38.Centers for Disease Control and Prevention. HIV prevention.2018. https://www.cdc.gov/actagainstaids/basics/prevention.html. Accessed October 11, 2018.
- 39.Stokes LR, Harvey SM, Warren JT. Individual, interpersonal, and structural power: associations with condom use in a sample of young adult Latinos. Health Care Women Int. 2016;37(2):216–236. [DOI] [PubMed] [Google Scholar]
- 40.McCabe BE, Schaefer Solle N, Peragallo Montano N, Mitrani VB. Alcohol misuse, depressive symptoms, and HIV/STI risks of US Hispanic women. Ethn Health. 2017;22(5):528–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Villegas N, Cianelli R, Gonzalez-Guarda R, Kaelber L, Ferrer L,Peragallo N. Predictors of self-efficacy for HIV prevention among Hispanic women in South Florida. J Assoc Nurses AIDS Care. 2013;24(1):27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Oliveira G, Cianelli R, Gattamorta K, Kowalski N, Peragallo N. Social determinants of depression among Hispanic women. J Am Psychiatr Nurses Assoc. 2017;23(1):28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vermeesch AL, Gonzalez-Guarda RM, Hall R, McCabe BE, Cianelli R, Peragallo NP. Predictors of depressive symptoms among Hispanic women in South Florida. West J Nurs Res. 2013;35(10): 1325–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]