Abstract
The effect of cumulative biological, psychosocial, and demographic risk and infant sleep on infant social-emotional functioning in 12-month-old infants (46% female) was examined in data from racially (30% Black, 60% White, 10% multiracial/other) and socioeconomically (41% below median income) diverse caregivers (N = 468, M = 30.42 years old, SD = 5.65) recruited from two midwestern states in 2019–2020. Due to the major changes in sleep patterns during infancy and the reported association between sleep and social-emotional functioning, this study also examined whether sleep moderates the association between risk and infant social-emotional functioning and potentially promotes healthy social-emotional functioning despite risk. Greater cumulative risk was associated with poorer sleep efficiency and more social-emotional problems, but was not associated with the general acquisition of social-emotional milestones. Results also suggested that poorer sleep efficiency was associated with more social-emotional problems and poorer social-emotional milestone acquisition. No significant interaction effects were found between cumulative risk and infant sleep. Risk and sleep appear to have unique associations with infant social-emotional problems and development; thus both could be targeted in early intervention to promote social-emotional functioning during infancy and early childhood.
Keywords: Infant, Sleep, social-emotional, cumulative risk
1. Introduction
Social-emotional functioning refers to a child’s ability to experience, recognize, and regulate their emotions as well as engage in prosocial behaviors and cultivate positive relationships with others (Thompson et al., 2012). Social-emotional problems can present early in life and often endure through elementary school (Briggs-Gowen & Carter, 2008), adolescence (Pihlakoski et al., 2006; Mesman et al., 2001), even adulthood (Althoff, 2010), and there are a multitude of risk factors that contribute to these social-emotional difficulties. Factors such as parental psychopathology, lower family socioeconomic status (SES), and parenting stress, can place children at risk for poor social-emotional functioning (Holtmann, 2011; Mantymaa et al., 2012). Due to the long-lasting nature of social-emotional struggles, addressing early modifiable factors that promote healthy social-emotional functioning becomes a logical target for intervention. Despite this need to target early identification and intervention, little research has focused on identifying and understanding social-emotional problems in infancy. Major changes in sleep patterns throughout infancy as well as the reported association between nocturnal, uninterrupted sleep and favorable social-emotional functioning suggest that infant sleep may be a possible target for promoting healthy social-emotional development and behavior (Sadeh et al., 2015; Scher et al., 2009; Tham et al., 2017).
Sleep may moderate the observed relation between certain risk factors and social-emotional functioning. El-Sheikh and colleagues (2010) demonstrated that sleep moderated the relationship between SES and social-emotional problems in a cohort of 5th grade children, such that children of higher SES exhibited relatively few social-emotional problems regardless of their sleep efficiency while children of lower SES who had poorer sleep efficiency demonstrated more social-emotional problems. A similar moderating effect of sleep was found on the relationship between maternal education and adolescent executive functioning (Anderson et al., 2009) such that adolescents’ measured executive abilities were more contingent on their sleep in those with mothers of lower educational attainment. Thus, compared to children with less risk, better sleep may serve as a protective factor for children who experience greater risk. Research on this topic, however, is sparse and has not been extended to in infancy and early childhood. Furthermore, it is important to clarify how risk may impact the acquisition of social-emotional milestones versus the emergence of social-emotional problem behaviors. The current investigation extends this research to examine whether sleep may play a role in moderating the relationship between risk and social-emotional functioning in infancy. In this study, social-emotional functioning is operationalized as both the acquisition of social-emotional milestones and social-emotional problems.
1.1. Risk and Protective Factors Related to Social-Emotional Functioning
1.1.1. Risk Factors
Throughout development, children encounter risk factors, which are “environmental or individual attributes that are associated with a negative developmental outcome” (Naglieri, 2013, p. 262). Bronfenbrenner’s bioecological model is one conceptual frame from which to examine the determinants of risk that may affect a child’s social-emotional functioning (Bronfenbrenner & Morris, 1998), and includes biological (e.g., temperament, gestational age), psychosocial (e.g., parental psychopathology), or broader social-contextual factors (e.g., socioeconomic status, maternal education) (Bagner et al., 2012; Mantymaa et al., 2012).
Within the biological domain, this study examined gestational age at birth, postnatal medical complications and temperamental negative affectivity as potential risk factors. Children born preterm experience more prenatal and perinatal complications and are at higher risk for a variety of developmental delays including delays social-emotional development (Glass et al., 2017; Haller et al., 2016; Klebermass-Schrehof et al., 2012; Lee et al., 2005; Quigley et al., 2012; Robertson et al., 1992). Negative affectivity in infancy has also been associated with social-emotional problems in toddlers (Gartstein et al., 2012).
Psychosocial risks such as caregiver depression, parenting stress, and stressful life experiences were also examined. Caregiver depression is associated with infant negative affect, heightened emotionality, dysregulated aggression, anxiety, attentional problems, and less secure attachments, among other concerns, beginning in infancy and extending through adolescence (Goodman & Tully, 2006). Additionally, parenting stress has been shown to negatively affect a child’s social-emotional functioning from infancy through school-age (Bayer et al., 2012; Briggs-Gowan, 1996; Mantymaa et al., 2012). Research has also shown that stressful life experiences are predictive of poorer social-emotional development in infants and preschool children (Kerker et al., 2015).
Within the demographic domain, household income, maternal education, and marital status were examined as risk factors. Children from single parent households (Weitzman et al., 2014), with lower maternal education and fewer economic resources also have higher levels of social-emotional problems (Holtmann et al., 2011) . Marital status may provide information about the availability of economic or social support resources, which may help explain why living in a single parent household is associated with more problematic social-emotional functioning in infants and preschool children.
While it is important to identify risk factors that affect development, it is quite rare that a child will be exposed to a single risk factor in isolation. While individual risk factors have been identified, it is common for risk factors to overlap, such that children are exposed to several related factors (O’Dougherty Wright et al., 2013). Prior research has repeatedly demonstrated that higher cumulative biological, psychosocial, and demographic risk is associated with more social-emotional problems from infancy through school age (e.g., Clarkson Freeman, 2014; Weitzman et al., 2014).
1.1.2. Sleep as a Protective Factor?
While risk factors increase the likelihood of maladaptive outcomes, many children who have experienced adversity are able to adapt quite well (Cicchetti & Rogosch, 1996). Therefore, it is important to identify protective factors, which are “environmental and individual attributes that counter the impact of risk and decrease the likelihood of negative outcomes” (Naglieri, 2013, p. 263). Promoting good quality sleep during infancy and early childhood has benefits for a variety of developmental outcomes, including cognitive abilities and social-emotional development (Sadeh et al., 2015). Broadly, sleep development can be viewed in terms of consolidation and regulation. Throughout infancy, toddlerhood, and preschool, a child’s amount of daytime sleep decreases and nighttime sleep increases, consolidating into a single period of nighttime sleep (Sadeh, 2004). The ability to regulate back to sleep following a nighttime awakening develops more rapidly, with many parents reporting that their infant is sleeping through the night by 6 months of age (Tham et al., 2017). Additionally, children experience fewer night wakings with age, resulting in increased sleep efficiency, or the percentage of time in bed that is spent asleep (Reed & Sacco, 2016; Tham et al., 2017). Whether through more total time asleep or more efficient sleep, better sleep is associated with fewer social-emotional problems (Scharf, 2013; Sadeh et al., 2015).
1.2. The Present Study
This study sought to extend the literature on infant social-emotional functioning by examining the effects of cumulative risk and sleep efficiency on the acquisition social-emotional milestones and on social-emotional problems in a sample of 9- to 12-month-old children. Sleep efficiency is an important indicator of sleep regulation, as it reflects a child’s ability to manage transitions between wakefulness and sleep both at initial sleep onset and after night wakings. Our first aim was to examine the effect of cumulative risk on infant sleep efficiency and social-emotional functioning, the latter for which we examined both social-emotional milestones and social-emotional problems. We hypothesized that children with greater cumulative risk would experience lower sleep efficiency and poorer social-emotional functioning. In our second aim, we sought to characterize the relation between infant sleep efficiency and social-emotional functioning. We expected that children with poorer 9-month sleep efficiency would experience poorer social-emotional functioning at 12 months.
Our third aim was to extend previous research regarding the protective effect of sleep on positive outcomes in the presence of risk to a younger population. The moderating effect of sleep efficiency on the relation between cumulative risk and social-emotional functioning was examined. We hypothesized that efficient sleep would have a protective effect on social-emotional functioning for infants with high cumulative risk and poor sleep efficiency would be associated with poorer social-emotional outcomes in those same infants; conversely, in children with low cumulative risk, we did not expect sleep to have a large effect on their social-emotional outcomes. Figure 1 illustrates the proposed conceptual model of the current study.
Figure 1.
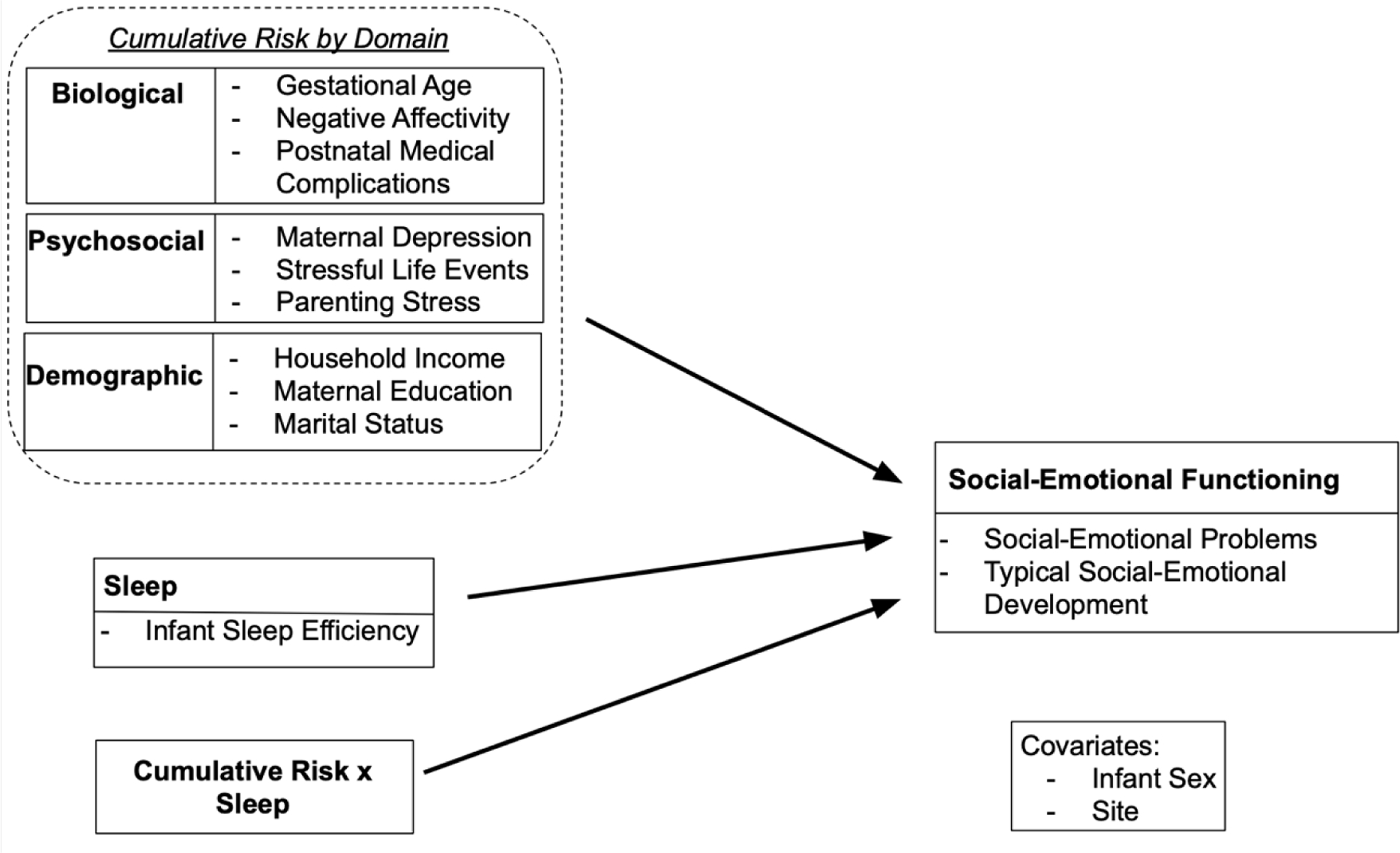
Proposed Conceptual Model of Infant Sleep Moderating the Association Between Cumulative Risk and Social-Emotional Functioning.
While past research has examined the association between infant sleep and social-emotional development, to our knowledge, the directionality of this relationship has not been fully explored. Though our data does not allow for the exploration of directionality between poor sleep efficiency and elevated social-emotional problems, the repeated measures methodology by which information about typical social-emotional milestones was gathered supported the examination of this question with the latter construct. An exploratory aim of the study was to assess the directionality of association between infant sleep efficiency and typical social-emotional development.
2. Method
2.1. Participants
The current study is part of a larger longitudinal multi-site investigation with repeated measures focused on the development and validation of PediaTrac v3.0™, a caregiver report, web-based tool to monitor and track infant and toddler development (Lajiness-O’Neill et al., 2018; Lajiness O’Neill et al., 2021). Participating dyads were enrolled at birth into a term or preterm group and followed longitudinally for 18–24 months at one of three sites in Michigan or Ohio. The current investigation utilized data from a subset of 468 caregiver/infant dyads from the larger study who had completed the 12-month assessment. Data collection began in January 2019 and is ongoing.
2.1.1. Inclusion/Exclusion Criteria.
Term infants had a gestational age > 37 weeks, a minimum birth weight of 2,500 grams, and no history of prenatal or intrapartum complication, brain injury, neurological illness, or disease (e.g., seizures). Infants were excluded if they were diagnosed with neonatal abstinence syndrome or Down syndrome. Preterm infants were born < 37 weeks gestational age. Participating caregivers were required to be (a) the infant’s primary caregiver, (b) at least 18 years of age, (c) fluent in English, and (d) have an internet-connected device (e.g., smartphone, laptop) to complete study materials online.
2.1.2. Demographic Characteristics
Demographic characteristics of the current sample are presented in Table 1. Of the 468 caregivers included in the current sample, 98% were mothers and the remaining 2% were fathers. Data from Sites 1 and 2 were combined and compared to data from Site 3. Sites 1 and 2 were combined for two main reasons: (1) Site 1 (n = 181) and Site 3 (n = 209) each had over twice the number of participants of Site 2 (n = 78), so the sample size differences that would result from comparing the three sites would lead to a concern in computing reliable standard errors; (2) there are no differences between participants from Site 1 and Site 2 on important demographic characteristics (e.g., infant sex, infant/caregiver race/ethnicity, household income, maternal education, marital status). About half of all participating infants were female, with no differences by site (p = .90). The majority of caregivers and infants were identified as non-Hispanic. Approximately half of caregivers and infants were identified as White, roughly one-third were Black, and the remainder were multiracial or other. Significantly more caregivers and infants at Site 1|2 identified as Black, while significantly more caregivers and infants at Site 3 identified as White.
Table 1.
Demographic Characteristics of the Full Sample and by Site
| Full Sample (N = 468) |
Site 1|2 (n = 259) |
Site 3 (n = 209) |
χ 2 | V | |
|---|---|---|---|---|---|
| Infant Sex | 0.31 | .03 | |||
| % Female | 46.15 | 47.49 | 44.50 | ||
| Infant Ethnicity | 0.00 | .00 | |||
| % Spanish/Hispanic/Latino | 6.85 | 6.17 | 6.69 | ||
| Infant Race (n = 463) | 107.52*** | .48 | |||
| % Black|African American | 30.45 | 49.61 | 6.76 | ||
| % White | 54.21 | 35.16 | 77.78 | ||
| % Multiracial | 12.31 | 12.50 | 12.07 | ||
| % Other | 3.02 | 2.73 | 3.38 | ||
| Maternal Ethnicity | 0.09 | .02 | |||
| % Spanish/Hispanic/Latino | 3.85 | 2.70 | 5.26 | ||
| Maternal Race (n = 465) | 109.22*** | .48 | |||
| % Black|African American | 30.97 | 50.39 | 7.17 | ||
| % White | 60.92 | 39.45 | 82.78 | ||
| % Multiracial | 6.24 | 7.42 | 4.78 | ||
| % Other | 3.87 | 2.73 | 5.26 |
Note. Chi-square tests of independence compared demographic characteristics between Site 1|2 and Site 3 and Cramer’s V was used to measure effect size.
p < .05.
p < .01.
p < .001.
2.2. Procedures
Infant-caregiver dyads were recruited from three large metropolitan academic hospital systems and a community health center in the Midwest. Caregivers were either recruited at one of three sites in their last trimester of pregnancy, in the hospital soon after their infants’ birth, or at their infant’s first newborn visit, with consent provided after birth. Primary caregivers of term infants completed their first study materials soon after birth, whereas caregivers of preterm infants completed them soon after their infants had reached a postmenstrual age of 39 weeks. All subsequent data collection time points were based on corrected age for preterm infants.
Caregivers completed the PediaTrac™ survey at 8 time periods that correspond to well child visits (newborn (NB), 2, 4, 6, 9, 12, 15, and 18 months). PediaTrac queries multiple developmental domains, including Feeding/Eating/Elimination, Sleep, Social/Communication/Cognition, Sensorimotor, Early Relational Health, and Social/Sensory Information Processing. Survey questions about demographics, as well as family and perinatal medical characteristics were completed during the NB period, with information on the family environment and infant medical status updated in all subsequent assessments. The PediaTrac™ survey was sent via email through REDCap and completed online (Harris et al., 2009; Harris et al., 2019). Participants also completed between two to six established developmental, behavioral, and caregiver paper-pencil questionnaires at each sampling period. For the purpose of this investigation, only the Brief Infant-Toddler Social-Emotional Assessment (BITSEA) (Briggs-Gowan & Carter, 2002), Brief Infant Sleep Questionnaire (BISQ) (Sadeh, 2004), Infant Behavior Questionnaire – Revised (IBQ-R-SF) (Putnam, et al., 2014), and the Parenting Stress Index-4-Short Form (PSI-4-SF) (Abidin, 2012) were used. A number of strategies were employed to minimize attrition. Total attrition was 12.08%. Specifically, 7.36% of attrition was due to participants being lost to follow up, 4.03% was due to participants withdrawing from the study, and 0.70% was due to death of an infant. The study adhered to all ethical standards and was approved by all involved Institutional Review Boards. For continued discussion of study methods and procedures, please refer to Lajiness-O’Neill et al., 2021.
2.3. Measures
2.3.1. Assessments of Infant Sleep and Social-Emotional Functioning
2.3.1.1. Brief Infant-Toddler Social-Emotional Assessment (BITSEA).
The BITSEA is a 42-item questionnaire that assesses parent-reported social-emotional problems and social-emotional competence of 12- to 36-month-old children (Briggs-Gowan & Carter, 2002). Each item describes a feeling or behavior the child may exhibit, and parents indicate whether the statement has been “not true/rarely,” “somewhat true/sometimes,” or “very true/often” for their child in the past month (Briggs-Gowan et al., 2004). The 31-item problem scale was used as a measure of problematic social-emotional development at 12 months in the current study. Research has documented acceptable internal consistency (α = .79-.87), test-retest reliability (r = .65-.87), and inter-rater reliability of the problem scale (ρ = .66; r = .68; Briggs-Gowan et al., 2004; Hungerford et al., 2015; Karabekiroglu et al., 2010).
2.3.1.2. Brief Infant Sleep Questionnaire (BISQ) – Expanded Version.
The Brief Infant Sleep Questionnaire (BISQ) is a parent report questionnaire used to screen for sleep problems in children from birth to 36 months of age (Sadeh, 2004). Test-retest reliability of the BISQ ranges from .82 to .95. Research has also demonstrated convergent validity, as the BISQ correlates significantly with sleep as measured by actigraphy (r = .23-.54) and daily sleep logs (r = .27-.83; Sadeh, 2004). The current study administered an adapted version of the BISQ at 9 months. Demographic questions were removed while questions regarding sleep patterns and sleep ecology were retained. The 22 retained items asked parents to consider different aspects of their infant’s sleep within the previous 2 weeks, including sleep patterns (e.g., How many times does your child typically wake during the night), sleeping arrangements (e.g., Where does your child sleep most of the time?), bedtime rituals (e.g., Which of the following usually occurs on most nights for your child in the hour before bedtime?), and parental sleep-related interventions (e.g., When your child wakes up during the night, what do you do?) (Sadeh et al., 2009). Information about infant sleep patterns from the BISQ (e.g., nighttime sleep duration, sleep onset latency, number and duration of night wakings) at 9 months was used to calculate an infant’s sleep efficiency in the current study. Sleep efficiency was operationalized as a ratio of a child’s total sleep time divided by the duration of the sleep episode (DSE). DSE was defined as the sum of sleep onset latency, total sleep time, and time awake after initial sleep onset but before the final awakening (Reed & Sacco, 2016).
2.3.1.3. PediaTrac™ Social/Communication/Cognition and Sleep Domains.
The social/communication/cognition (SCG) domain was of interest in the current investigation, as it assesses an infant’s response to stimulation, expression of emotion, communication, and acquisition of knowledge. It was examined as a measure of social-emotional development at 9 and 12 months (71 and 73 items at these ages, respectively), as it assesses the acquisition of social-emotional milestones. Caregivers read a series of questions related to their infant’s social-emotional development and indicated how often their child engaged in a particular behavior on a 5 point scale from never (1) to always (5). In the SCG domain, caregivers reported on their child’s eye contact, response to name, imitation of facial expressions and emotions, engagement in joint attention, differential responding to familiar caregivers compared to strangers, and their tendency to seek out and enjoy social interaction, among other related abilities. SCG percent of maximum possible (POMP) scores were calculated, which reflect the current skill level of the child compared to the maximum possible SCG skill level at each time period, such that higher scores indicate more developed social-emotional abilities. The SCG domain from PediaTrac v2.0 (Version 2.0) has shown good reliability via IRT modeling (0.93). Convergent and divergent validity have also been demonstrated with Version 2.0 (Lajiness-O’Neill, 2018). Additionally, information from the sleep domain of PediaTrac was utilized to calculate sleep efficiency at 9 and 12 months. While there are 24 total sleep items repeated at each age, only those used to calculate sleep efficiency in the same manner described above (total sleep time / DSE) were employed.
2.3.2. Cumulative Risk Domains
2.3.2.1. Biological.
Biological risk included an infant’s gestational age (in weeks), temperamental negative affectivity, and postnatal medical complications. Gestational age was obtained from the PediaTrac™ general medical domain. Negative affectivity was measured by the Infant Behavior Questionnaire – Revised, Short form (IBQ-R-SF) at 9 months. The IBQ-R is a 191-item measure assessing infant temperament from 3 to 12 months (Gartstein & Rothbart, 2003). The Short Form consists of 91 items. Each item asks about the frequency of a behavior, which the respondent rates on a 7-point scale from “never” to “always.” Research indicates that the internal consistency is adequate for all subscales on the Short Form (α = .63 - .86), including those used in the negative affectivity subscale (α ranges from .72 to .80). Estimated test-retest reliability for the subscales used to calculate negative affectivity ranges from .65 to .82, and estimated inter-parent agreement on these subscales ranges from .20 to .76 (Putnam et al., 2014). The current study utilized the negative affectivity domain of the Short Form as a measure of infant temperament at 9 months (25 items). This domain is composed of positive contributions from the distress to limitations, fear, and sadness subscales as well as a negative contribution from the falling reactivity subscale (Gartstein & Rothbart, 2003). Information about the following postnatal medical complications were obtained during eligibility screening: stroke, more than one seizure, neurological illness, intraventricular hemorrhage or hypoxic ischemic injury, bronchopulmonary dysplasia, retinopathy of prematurity, neonatal sepsis, or a transfer to the neonatal intensive care unit (NICU). Each infant received one point for every medical complication they experienced to create a sum score ranging from 0 (no medical complications) to 8 (every medical complication).
2.3.2.2. Psychosocial.
The psychosocial risk domain included parenting stress and parental depressive symptoms as well as the number of stressful life events experienced by the child. The Parenting Stress Index-4-Short Form (PSI-4-SF) is a 36-item parent self-report measure for parents of children 3 months to 12 years of age. It assesses three domains of parenting stress: parental distress, parent-child dysfunctional interaction, and difficult child (Abidin, 2012). Respondents indicate their level of agreement with each item on a 5-point scale of “strongly disagree” to “strongly agree.” The three domains combine to form a total parenting stress scale, which was utilized in the current study as a measure of parenting stress at 6 months. Research indicates that the total parenting stress scale has excellent internal consistency (α = .90-.92) and good test-retest reliability (ICC = .77-.78; r = .84; Abadin, 2012; Barroso et al., 2016). The Brief Symptom Inventory (BSI) is a 53-item self-report measure that asks about a variety of mental health symptoms (Derogatis & Melisaratos, 1983). Respondents are asked to indicate how often they have been distressed by a symptom in the past week on a 5-point scale, ranging from “not at all” to “extremely.” For the current study, T-scores from the depression subscale were utilized as a measure of parental depressive symptoms at 9 months. The depression subscale from the BSI has been shown to have adequate internal consistency (α = .85-.88) and test-retest reliability (r = .84; Adawi et al., 2019; Gerogatis & Melisaratos, 1983; Mohammadkhani et al., 2010). The 6- and 9-month periods, respectively, were chosen based on when these constructs were assessed in the larger study. Number of stressful life events was obtained from the PediaTrac™ general medical domain. At each time period, caregivers indicated which events happened in their immediate family since the previous time period: illness, break up or divorce, death, loss of job, loss of wages, change in living location, incarceration, alcohol or drug problem, violence between adults in the home, and a primary caregiver returned to work. Caregivers’ responses to this item from the newborn through 9-month periods were summed to create a variable that ranged from 0 (“no stressful life events”) to 50 (“all stressful life events”).
2.3.2.3. Demographic.
Information for the demographic risk domain was obtained from the PediaTrac™ demographic domain at the newborn sampling period and included household income, maternal education, and marital status. Household income was characterized relative to the U.S. Department of Health and Human Services Poverty Guidelines (2019) and median household income in Michigan and Ohio. Dyads were categorized as: below poverty, below median, at/above median, at/above twice median, above $150,000. Level of maternal education was categorized as: some/completed high school, some college/trade school, college graduate, post-graduate/professional. Marital status was dichotomously coded as married or not married.
2.3.3. Overall Cumulative Risk Index
The overall cumulative risk index was calculated by dichotomizing each risk factor (0 = low risk, 1 = high risk) based on standardized normed cutoffs, prior research, or the distributional properties of our sample. The method and justification for dichotomizing each risk factor is summarized in Table 2. The scores were then summed within each domain to create three domain specific risk scores that each range from 0 (no risk) to 3 (all risk factors endorsed). Finally, the scores of each domain were summed to create an overall cumulative risk index that ranges from 0 (no risk) to 9 (all risk factors endorsed).
Table 2.
Risk factors included in the domain specific and overall cumulative risk indices.
| Risk factor | Low risk = 0 | High Risk = 1 | Justification |
|---|---|---|---|
| Biological | |||
| Gestational Age | ≥ 37 weeks | < 37 weeks | Based on term status |
| Negative Affect (IBQ-R-SF) | < 1 SD above mean | ≥ 1 SD above mean | Above normal/average levels |
| Postnatal Medical Complications | < 1 | ≥ 1 | Established risk factor |
| Psychosocial | |||
| Caregiver Depression (BSI)a | T-score < 63 | T-score ≥ 63 | Normed cutoff |
| Stressful Life Eventsb | < 4 events | ≥ 4 events | Established risk factor |
| Parenting Stress (PSI-4-SF)c | < 1 SD above mean on total stress scale | ≥ 1 SD above mean on total stress scale | Above normal or average levels |
| Demographic | |||
| Household Incomed | Above poverty line | At/below poverty line | Established risk factor |
| Maternal Educatione | Completed high school | No high school diploma or equivalent | Established risk factor |
| Marital Statusf | Married | Not married | Established risk factor |
Note. IBQ-R = Infant Behavior Questionnaire - Revised-Short Form; PSI-4-SF = Parenting Stress Index-4-Short Form Total Problem Scale; BSI = Brief Symptom Inventory
(Abidin, 2012).
2.4. Statistical Analysis
2.4.1. Preliminary Analyses
Statistical analyses were conducted using R (R Core Team, 2020). Descriptive statistics (frequencies, M, and SD) are presented for variables of interest, and parametric tests (t-tests or ANOVAs) were computed as appropriate to examine site differences. Exploratory analyses were conducted to ensure that the assumptions of correlation and regression were met. Missing data were handled using the mice package (van Buuren & Groothuis-Oudsboorn, 2011) in R to conduct multiple imputation. Multiple imputation was based on the variables included in the cumulative risk composite, sleep variables, social-emotional problems (BITSEA) and social-emotional milestones (PediaTrac SCG), infant sex, and data collection site. Gestational age, postnatal medical complications, and marital status did not have any missing data, so multiple imputation was not necessary. After generating 20 data sets with imputed values, correlation, regression, and cross-lag panel models were iteratively fit to all 20 data sets. The parameter estimates, standard errors, and confidence intervals reflect the pooled values. Importantly, the findings were largely the same when analyses were performed with pairwise deletion. Prior to multiple imputation, the number of missing observations were as follows: 328 participants were not missing any data, 82 participants were missing data on one variable, 25 participants were missing data on two variables, 14 participants were missing data on three variables, nine participants were missing data on four variables, seven participants were missing data on five variables, and three participants were missing data on six variables.
2.4.2. Main Analyses
Pearson r correlations were calculated to examine the relations between overall cumulative risk, sleep efficiency, social-emotional problems (BITSEA Total Problem Scale), and social-emotional development (i.e., milestone acquisition) (SCG POMP scores). To examine sleep as a moderator of the relationship between overall cumulative risk and infant social-emotional functioning, moderation analyses were conducted separately for the two social-emotional functioning outcome measures (BITSEA Total Problem Scale scores and SCG POMP scores) as well as for the two sleep efficiency measures (BISQ and PediaTrac™). Predictors (sleep efficiency and cumulative risk) were mean centered before the creation of interaction terms and inclusion in the models. Cumulative risk, sleep efficiency, and covariates (infant sex and recruitment site) were entered in Step 1. The interaction between cumulative risk and sleep efficiency was entered in Step 2.
2.4.3. Exploratory Analyses
To address the exploratory aim of directionality, a cross-lagged panel analysis was conducted using SCG POMP scores and PediaTrac sleep efficiency from both the 9- and 12-month sampling periods. Similar analysis could not be completed using sleep efficiency as measured by the BISQ or social-emotional problems as measured by the BITSEA because these measures were only given at 9 or 12 months, respectively.
3. Results
3.1. Cumulative Risk Descriptive Statistics
Table 3 presents descriptive information for each cumulative risk index factor. Supplemental Table 1 provides information about the percentage of caregiver/infant dyads characterized as high and low risk for each risk factor. Site differences were observed in negative affectivity, income, maternal education, and marital status. Compared to Sites 1|2, participants at Site 3 reported lower negative affectivity, higher household income, and more maternal education, and were more likely to be married. Sites did not differ in infant gestational age, number of postnatal medical complications, parental depression, parenting stress, or number of stressful life events.
Table 3.
Risk Factor Descriptive Statistics by Site
| Overall Sample (N = 468) |
Site 1|2 (n = 209) |
Site 3 (n = 259) |
Statistic | Effect Size | |
|---|---|---|---|---|---|
| Biological Risk | |||||
| Variables [M(SD)] | |||||
| Weeks Gestation | 36.58 (3.69) | 37.00 (3.08) | 36.06 (4.28) | t = 2.66** | d = 0.28 |
| Negative Affectivity (IBQ-R-SF) | 3.59 (0.75) | 3.68 (0.76) | 3.48 (0.71) | t = 2.85** | d = 0.27 |
| Postnatal Medical Complications | 0.40 (0.64) | 0.29 (0.55) | 0.52 (0.73) | t = 3.73*** | d = 0.38 |
| Psychosocial Risk | |||||
| Variables [M(SD)] | |||||
| Caregiver Depression (BSI)a | 49.70 (8.47) | 49.15 (8.50) | 50.33 (8.41) | t = 1.43 | d = 0.14 |
| Parenting Stress (PSI-4-SF)b | 27.44 (22.13) | 26.59 (22.54) | 28.39 (21.68) | t = 0.83 | d = 0.08 |
| Stressful Life Events | 1.94 (2.79) | 2.25 (2.72) | 1.59 (2.44) | t = 2.77*** | d = 0.28 |
| Demographic Risk | |||||
| Variables | |||||
| Income | t = 10.80*** | d = 1.05 | |||
| % Below Poverty | 27.97 | 43.91 | 9.55 | ||
| % Below Median | 13.05 | 14.78 | 11.05 | ||
| % At/Above Median | 25.17 | 25.65 | 24.62 | ||
| % Above Twice Median | 19.34 | 10.00 | 30.15 | ||
| % Above $150,000 | 14.45 | 5.65 | 24.62 | ||
| Maternal Education | t = 10.46*** | d = 0.98 | |||
| % Some High School | 3.63 | 5.79 | 0.95 | ||
| % High School Graduate | 15.17 | 25.09 | 2.87 | ||
| % Some College | 24.15 | 28.57 | 18.66 | ||
| % Trade/Technical/Vocational Training | 3.42 | 4.24 | 2.39 | ||
| % College Graduate | 25.64 | 21.24 | 31.10 | ||
| % Some Post-Graduate | 1.92 | 2.70 | 0.95 | ||
| % Post-Graduate or Professional Degree | 26.07 | 12.36 | 43.06 | ||
| Marital Status | χ2 = 97.52*** | V = 0.46 | |||
| % Married | 59.40 | 39.15 | 84.69 | ||
| % Not Married | 40.60 | 60.85 | 15.31 | ||
Note. IBQ-R-SF = Infant Behavior Questionnaire – Revised, Short form; BSI = Brief Symptom Inventory; PSI-4-SF = Parenting Stress Index-4-Short Form.
Caregiver depression is measured as a T-score, M = 50, SD = 10.
Parenting stress is measured as a percentile, M = 50.
p < .05.
p < .01.
p < .001.
3.2. Results of Main Analyses
Descriptive statistics for the outcome variables of interest (sleep efficiency, BITSEA Total Problem Scale scores, and SCG POMP scores) and correlations between all study variables are presented in Table 4.
Table 4.
Descriptive Statistics and Bivariate Correlations for Variables of Interest
| M(SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. Cumulative Risk Sleep efficiency (%) | 1.91 (1.48) | – | −.15** | −.17*** | −.12* | .08 | −.03 | .29*** |
| 2. BISQ 9 months | 92.09 (10.23) | −.15* | – | .41*** | .38*** | −.05 | .06 | −.17*** |
| 3. PT 9 months | 97.10 (3.93) | −.18** | .43*** | – | .47*** | .04 | .10* | −.21*** |
| 4. PT 12 months | 97.62 (2.85) | −.13* | .28*** | .58*** | – | .05 | .13* | −.19*** |
| Socioemotional development | ||||||||
| 5. PT SCG: 9 months | 0.68 (0.08) | .10 | −.09 | .02 | .08 | – | .70*** | .05 |
| 6. PT SCG: 12 months | 0.76 (0.09) | −.05 | .03 | .07 | .12* | .71*** | – | −.05 |
| 7. BITSEA: 12 | 7.59 (5.10) | .28*** | −.21** | −.25*** | −.22*** | .08 | −.03 | – |
Note. BISQ = Brief Infant Sleep Questionnaire – Expanded Version. PT = PediaTrac, SCG = Social/Communication/Cognition Domain. BITSEA = Brief Infant-Toddler Social-Emotional Assessment. Values above the diagonal are pooled estimates of 20 data sets created with multiple imputation and values below the diagonal and the descriptive statistics are from the original data.
p < .05.
p < .01.
p < .001.
3.2.1. Aim 1: The Effect of Cumulative Risk on Infant Sleep and Social-Emotional Development
Correlational analyses revealed that cumulative risk was associated with sleep efficiency, such that children with greater cumulative risk were more likely to experience poorer sleep efficiency measured by the BISQ at 9 months and the PediaTrac sleep domain at 9 and 12 months. Furthermore, cumulative risk was significantly correlated with BITSEA Total Problem Scale scores at 12 months, but not SCG POMP scores at 9 or 12 months. Infants who experienced more cumulative risk were more likely to have higher levels of reported social-emotional problems measured by the BITSEA. On the other hand, level of cumulative risk was not significantly correlated with an infant’s social-emotional abilities measured by SCG POMP scores.
3.2.2. Aim 2: The Effect of Infant Sleep Efficiency on Infant Social-Emotional Functioning
To characterize the association between infant sleep and social-emotional functioning, concurrent and longitudinal correlations were examined at 9 and 12 months of age (Table 4). When examined concurrently at 9 months, sleep efficiency was not significantly correlated with SCG POMP scores (i.e., milestone acquisition) (p > .05). Contrary to expectations, children with more efficient sleep did not necessarily have better SCG POMP scores than children with less efficient sleep at 9 months. On the other hand, sleep efficiency at 12 months was significantly correlated with 12 month social-emotional problems measured by the BITSEA and 12 month typical social-emotional development measured by SCG POMP scores. At 12 months, children with poorer sleep efficiency were likely to have higher BITSEA Total Problem Scale scores and lower SCG POMP scores.
When examining the longitudinal correlations between infant sleep efficiency at 9 months and social-emotional functioning at 12 months, 9-month sleep efficiency, whether measured by the BISQ or PediaTrac sleep domain, predicted social-emotional problems on the BITSEA at 12 months. Specifically, infants with poorer sleep efficiency were likely to have higher BITSEA Total Problem Scale scores. On the other hand, 9-month sleep efficiency was weakly correlated with 12-month SCG POMP scores when sleep efficiency was measured by PediaTrac, but not when measured by the BISQ. Unexpectedly, infants with poorer PediaTrac sleep efficiency were likely to have higher SCG POMP scores.
3.2.3. Aim 3: Moderating Effects of Infant Sleep on the Association Between Cumulative Risk and Infant Social-Emotional Functioning
Moderation analyses indicated that sleep efficiency did not significantly moderate the relationship between cumulative risk and BITSEA Total Problem Scale scores or between cumulative risk and SCG POMP scores (Tables 5–8). However, cumulative risk and sleep efficiency were significant predictors of BITSEA Total Problem Scale scores. Furthermore, the magnitude of the effect was similar whether sleep efficiency was measured by the BISQ [F(4, 463) = 13.58, p < .001, R2 = .11] (Table 5) or PediaTrac [F(4, 463) = 14.34, p < .001, R2 = .13] (Table 6). Greater cumulative risk and poorer sleep efficiency at 9 months was predictive of higher BITSEA Total Problem Scale scores at 12 months.
Table 5.
Unstandardized and Standardized Regression Models Predicting BITSEA Total Problem Scale Scores at 12 months Using BISQ Sleep Efficiency
| Variable | B | 95% CI for B |
SE B | β | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Step 1 | |||||
| Constant | 11.51*** | 6.38 | 16.63 | 2.59 | |
| BISQ Sleep Efficiency | −0.07* | −0.12 | −0.01 | 0.03 | −0.13 |
| Cumulative Risk | 0.88*** | 0.54 | 1.22 | 0.17 | 0.26 |
| Infant Sexa | 0.46 | −0.50 | 1.42 | 0.49 | 0.04 |
| Siteb | 0.57 | −0.47 | 1.60 | 0.53 | 0.05 |
|
| |||||
| Step 2 | |||||
| Constant | 11.11*** | 6.03 | 16.19 | 2.58 | |
| BISQ Sleep Efficiency | −0.06* | −0.12 | −0.01 | 0.03 | −0.13 |
| Cumulative Risk | 0.86*** | 0.52 | 1.20 | 0.17 | 0.25 |
| Infant Sexa | 0.46 | −0.50 | 1.42 | 0.49 | 0.04 |
| Siteb | 0.58 | −0.45 | 1.62 | 0.53 | 0.06 |
| BISQ Sleep * Risk | −0.01 | −0.05 | 0.03 | 0.02 | −0.04 |
Note. Statistics were averaged across multiply imputed data sets (m = 20). Sleep efficiency was assessed at 9 months. Sleep efficiency and cumulative risk were mean centered prior to computing the interaction term. BITSEA = Brief Infant-Toddler Social-Emotional Assessment; BISQ = Brief Infant Sleep Questionnaire; CI = confidence interval; LL = lower limit; UL = upper limit
Infant sex was coded as 0 = female, 1 = male.
Site was coded as 0 = Site 3, 1 = Site 1|2.
p < .05.
p < .01.
p < .001.
Table 8.
Unstandardized and Standardized Regression Model Estimates Predicting SCG POMP Scores at 12 months Using PediaTrac Sleep Efficiency
| Variable | B | 95% CI for B |
SE B | β | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Step 1 | |||||
| Constant | 0.53*** | 0.32 | 0.73 | 0.11 | |
| PediaTrac Sleep Efficiency | 0.003* | 0.00 | 0.00 | 0.001 | 0.11 |
| Cumulative Risk | −0.001 | −0.01 | 0.00 | 0.003 | −0.02 |
| Infant Sexa | −0.02** | −0.04 | −0.01 | 0.008 | −0.13 |
| Siteb | 0.01 | −0.01 | 0.03 | 0.008 | 0.06 |
|
| |||||
| Step 2 | |||||
| Constant | 0.45*** | 0.21 | 0.70 | 0.12 | |
| PediaTrac Sleep Efficiency | 0.00327** | 0.00 | 0.01 | 0.001 | 0.14 |
| Cumulative Risk | −0.001 | −0.01 | 0.00 | 0.003 | −0.02 |
| Infant Sexa | −0.02** | −0.04 | −0.01 | 0.008 | −0.14 |
| Siteb | 0.01 | −0.01 | 0.03 | 0.008 | 0.06 |
| PediaTrac Sleep * Risk | −0.001 | 0.00 | 0.00 | 0.001 | −0.07 |
Note. Statistics were averaged across multiply imputed data sets (m = 20). Sleep efficiency was assessed at 9 months. Sleep efficiency and cumulative risk were mean centered prior to computing the interaction term. SCG POMP = Social/Communication/Cognition Proportion of Maximum; CI = confidence interval; LL = lower limit; UL = upper limit
Infant sex was coded as 0 = female, 1 = male.
Site was coded as 0 = Site 3, 1 = Site 1|2.
p < .05.
p < .01.
p < .001
Table 6.
Unstandardized and Standardized Regression Models Predicting BITSEA Total Problem Scale Scores at 12 months Using PediaTrac Sleep Efficiency
| Variable | B | 95% CI for B |
SE B | β | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Step 1 | |||||
| Constant | 27.47*** | 14.94 | 40.00 | 6.36 | |
| PediaTrac Sleep Efficiency | −0.23*** | −0.36 | −0.10 | 0.06 | −0.17 |
| Cumulative Risk | 0.85*** | 0.50 | 1.19 | 0.17 | 0.25 |
| Infant Sexa | 0.48 | −0.47 | 1.43 | 0.48 | 0.05 |
| Siteb | 0.71 | −0.29 | 1.71 | 0.51 | 0.07 |
|
| |||||
| Step 2 | |||||
| Constant | 25.54*** | 10.09 | 41.00 | 7.82 | |
| PediaTrac Sleep Efficiency | −0.21** | −0.37 | −0.05 | 0.08 | −0.16 |
| Cumulative Risk | 0.84*** | 0.50 | 1.19 | 0.18 | 0.25 |
| Infant Sexa | 0.47 | −0.48 | 1.42 | 0.48 | 0.05 |
| Siteb | 0.71 | −0.29 | 1.71 | 0.51 | 0.07 |
| PediaTrac Sleep * Risk | −0.03 | −0.13 | 0.08 | 0.05 | −0.03 |
Note. Statistics were averaged across multiply imputed data sets (m = 20). Sleep efficiency was assessed at 9 months. Sleep efficiency and cumulative risk were mean centered prior to computing the interaction term. BITSEA = Brief Infant-Toddler Social-Emotional Assessment; CI = confidence interval; LL = lower limit; UL = upper limit
Infant sex was coded as 0 = female, 1 = male.
Site was coded as 0 = Site 3, 1 = Site 1|2.
p < .05.
p < .01.
p < .001.
For SCG POMP scores, the findings depended on the measure of sleep efficiency. When the model included sleep efficiency measured with the BISQ, only infant sex was a statistically significant predictor of social-emotional milestone acquisition, F(4, 463) = 3.31, p = .01, R2 = .03 (Table 7). When sleep efficiency was measured by PediaTrac, both sleep efficiency and infant sex were statistically significant predictors of SCG POMP scores, F(4, 463) = 3.91, p = .003, R2 = .03 (Table 8). Male infants and those with poorer sleep efficiency (PediaTrac sleep only) were rated lower on SCG POMP scores.
Table 7.
Unstandardized and Standardized Regression Model Estimates Predicting SCG POMP Scores at 12 months Using BISQ Sleep Efficiency
| Variable | B | 95% CI for B |
SE B | β | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Step 1 | |||||
| Constant | 0.71*** | 0.63 | 0.79 | 0.0400 | |
| BISQ Sleep Efficiency | 0.0006 | 0.00 | 0.00 | 0.0004 | 0.07 |
| Cumulative Risk | −0.0016 | −0.01 | 0.00 | 0.0030 | −0.03 |
| Infant Sexa | −0.02** | −0.04 | −0.01 | 0.0081 | −0.13 |
| Siteb | 0.01 | −0.01 | 0.03 | 0.0086 | 0.07 |
|
| |||||
| Step 2 | |||||
| Constant | 0.71*** | 0.62 | 0.79 | 0.0400 | |
| BISQ Sleep Efficiency | 0.0007 | 0.00 | 0.00 | 0.0004 | 0.08 |
| Cumulative Risk | −0.0019 | −0.01 | 0.00 | 0.0030 | −0.03 |
| Infant Sexa | −0.02** | −0.04 | −0.01 | 0.0081 | −0.13 |
| Siteb | 0.01 | −0.01 | 0.03 | 0.0086 | 0.07 |
| BISQ Sleep * Risk | −0.0003 | 0.00 | 0.00 | 0.0003 | −0.05 |
Note. Statistics were averaged across multiply imputed data sets (m = 20). Sleep efficiency was assessed at 9 months. Sleep efficiency and cumulative risk were mean centered prior to computing the interaction term. SCG POMP = Social/Communication/Cognition Proportion of Maximum; BISQ = Brief Infant Sleep Questionnaire; CI = confidence interval; LL = lower limit; UL = upper limit
Infant sex was coded as 0 = female, 1 = male.
Site was coded as 0 = Site 3, 1 = Site 1|2.
p < .05.
p < .01.
p < .001
3.3. Results of Exploratory Analysis
Results of the cross-lagged panel model indicate that there was stability in each construct, indicating rank order stability for both PediaTrac sleep efficiency (b = 0.28, SE = 0.04, p < .001, β = 0.34) and SCG POMP scores (b = 0.69, SE = 0.04, p < .001, β = 0.73) from 9 to 12 months. The cross-lagged effects, however, were not significant. PediaTrac sleep efficiency at 9 months did not predict SCG POMP scores at 12 months (b = −0.14, SE = 0.11, p = .19, β = −0.05), and, SCG POMP scores at 9 months did not predict PediaTrac sleep efficiency at 12 months (b = 0.02, SE = 0.02, p = .12, β = 0.08).
4. Discussion
Social-emotional difficulties that present in early childhood often predict continued emotional and behavioral challenges as an individual develops (Althoff, 2010; Briggs-Gowan & Carter, 2008; Mesman et al., 2001). Due to the pervasiveness of these struggles, understanding risk factors and addressing social-emotional difficulties early in childhood is crucial. The goal of this investigation was to examine the effect of biological, psychosocial, and demographic risk factors on social-emotional functioning within the first year of life. Because some children will inevitably experience one or more of these risk factors, this study also examined sleep as a moderator and possible point of intervention to promote healthy development despite adversity. Infant sleep was chosen because it is amenable to change via educational and psychosocial interventions and displays associations with a child’s social-emotional functioning (e.g., Field, 2017; Sadeh et al., 2015).
Cumulative risk was found to be associated with infant sleep. As expected, infants with greater cumulative risk had poorer sleep efficiency, due to either increased sleep onset latency or longer and/or more frequent night wakings (Williamson et al., 2019; Williamson & Mindell, 2020). Greater cumulative risk was also associated with more parent-reported infant social-emotional problems in our sample, replicating previous findings (e.g., Weitzman et al., 2014). Importantly, our results suggest that the effect of biological, psychosocial, and demographic risk on social-emotional problems can be seen as early as 12 months. Achievement of typical social-emotional milestones (e.g., responding to name, responding appropriately to or mimicking others’ emotions) in our sample, on the other hand, appears unrelated to cumulative risk. It seems that infants from all risk backgrounds are equally likely to master typical social-emotional milestones according to parental report; however, infants with more risk are reported to have higher levels of problem behaviors. The absence of association between cumulative risk and the acquisition of social-emotional skill development in infancy may reflect a true null relationship. Conversely, this association may be difficult to detect within the first year of life, but may become more prominent as social-emotional functioning becomes more complex. This conjecture is supported by past research findings that preschool and early school-aged children with higher cumulative risk had poorer social-emotional competence (Chang et al., 2012; Marti et al., 2016).
The findings of this study suggest that concurrent relationships between sleep and infant social-emotional functioning depend on both the time period and whether social-emotional problems or typical social-emotional development is being measured. At 9 months, sleep efficiency was not associated with concurrent social-emotional abilities. The association may truly not exist, at least as measured in the current study, or, alternatively, the association may be unobservable until social-emotional functioning becomes more complex. Indeed, at 12 months, sleep efficiency had the hypothesized association with social-emotional functioning; children with less sleep efficiency experienced more social-emotional problems and lower levels of typical social-emotional development. This suggests that children who fall asleep faster and wake less, resulting in higher sleep efficiency, tend to have more positive social-emotional functioning. These results extend those from Belanger et al. (2018) and Sadeh et al. (2015), who found that lower quality sleep was associated with more behavior problems in preschool-age children.
Longitudinal associations between sleep and social-emotional functioning, irrespective of measurement method, indicated that poor sleep efficiency at 9 months was associated with greater infant social-emotional problems at 12 months. Again, difficulty falling asleep and waking more often–which contribute to less sleep efficiency–appear to occur more often in 9-month-old children who are later reported to have more social-emotional problems at 12 months. However, a child’s sleep efficiency at 9 months was not associated with their social-emotional abilities at 12 months, indicating that the development of typical social-emotional milestones may be relatively resilient even in the presence of poor sleep.
During infancy, establishing a healthy pattern of uninterrupted, nocturnal sleep is one of the most salient developmental tasks. Associations between infant sleep and social-emotional functioning have been reported, and suggest utility in exploring sleep as a point of intervention to promote social-emotional functioning. In both infants and toddlers, implementation of a variety of behavioral sleep interventions has been documented, which focus on educating parents about proper sleep hygiene, implementing appropriate bedtime routines, or other similar goals (Kempler et al., 2016; Reuter et al., 2020). While a number of studies suggest improvement in infant sleep following the intervention, methodological issues remain. The prevalence of parent-reported sleep outcomes, homogeneity of study samples, and use of slightly different intervention techniques across studies raises unanswered questions about the relative efficacy of different treatment elements and their effectiveness in diverse populations (Field, 2017; Reuter et al., 2020). Furthermore, interventions commonly suggested for improving infant sleep are examined using White, middle-class samples and are based on Westernized values that may not have global implications (Schwichtenberg et al., 2019). Despite these limitations, findings suggest that infant sleep may be improved with intervention, highlighting the importance of continuing to explore effective treatments. Identifying useful interventions may not only function to improve a child’s sleep, but may also be a practical method for promoting healthy social-emotional development despite experiencing risk. Contrary to expectation, the interaction effect of cumulative risk and infant sleep was not a significant predictor of social-emotional functioning. This suggests that sleep affects social-emotional abilities similarly for infants from all risk backgrounds. This finding is promising when considering the effectiveness of emerging interventions, as it suggests that targeting sleep efficiency could potentially be beneficial for all infants, not only those with certain levels of risk.
In moderation analyses, infant sex was a significant predictor of parent-reported achievement of typical social-emotional milestones. Parents of male infants reported lower social-emotional development than parents of female infants. Findings from previous research mirror the current finding that even among infants within the normal range of development, males may have lower typical social-emotional development than females from 12 to 42 months of age (Briggs-Gowan et al., 2004). While the majority of children develop similar social-emotional competencies eventually, this research suggests that females may develop them more quickly than males of the same age, at least as perceived by parents. Despite this observed sex difference in typical social-emotional development, infant sex was not a significant predictor of social-emotional problems. This is relatively consistent with other research, which suggests that there are no sex differences in social-emotional problems within the first 2 years of life (Briggs-Gowan et al., 2006; Squires et al., 2004).
Though findings from the current study provide important information about the association between risk, infant sleep, and social-emotional functioning, they must be interpreted in light of certain limitations. First, risk factors other than those in our cumulative risk index may potentially impact infant social-emotional functioning. Data examining considerations such as a family’s access to healthcare, neighborhood safety, or parenting style were not included in the larger data set, and therefore, could not be examined in the current study. Future research could include additional risk factors to gain a more complete understanding of the influences on infant social-emotional functioning.
Additionally, the slight differences in response options given by the BISQ and PediaTrac sleep domain are important to acknowledge when considering the findings related to sleep efficiency. When providing information about the amount of sleep received by each infant on the BISQ, caregivers indicated the infant’s exact sleep time in hours and minutes. On the other hand, PediaTrac asked caregivers to report their infant’s sleep by choosing a range of time (“4 to 5 hours,” “5 to 6 hours,” etc.). Due to these different response options, each infant may receive a slightly different sleep efficiency value based on the measure from which the data was being drawn.
When interpreting our findings, it is also important to remember that all data regarding infant sleep were gathered via caregiver report. Caregiver report is valuable due to their extensive involvement in bedtime and wake up routines. However, it is possible that some infants wake at night without signaling their caregivers, therefore leaving the caregiver unaware of the exact amount of sleep received by the infant. A comparison of the current results to data obtained from more objective measures, such as actigraphy, could provide more nuanced information. In clinical practice, however, this may not be an important or necessary distinction, as obtaining information about infant sleep via caregiver report is standard practice. Knowing the relationship between infant sleep measured via actigraphy, risk, and social-emotional outcomes may not be clinically useful, as a provider will typically not have access to actigraphy. Further, what may be most important is identifying wakings in which the child is unable to self-soothe back to sleep, as these wakings are qualitatively different from those in which the child does not require parental assistance. Examining signaled wakings may provide more information about the child’s regulatory abilities, which aligns with the measurement of sleep efficiency as a metric of developing sleep regulation. Understanding how caregiver reported infant sleep is associated with social-emotional development is applicable to clinical practice and can give healthcare providers important information when planning interventions.
Finally, cumulative risk models are conceptually easy to understand and provide meaningful information about how risk impacts development. Despite the utility of this approach (Evans et al., 2013; Felitti et al., 1998; Weitzman et al., 2014), critics note that dichotomizing continuous variables to create a cumulative risk index results in the loss of information about the risk severity (Lanier et al., 2018; McLaughlin & Sheridan, 2016). Additionally, equal weight is assigned each risk factor, despite the possibility that one may impact the outcome variable of interest more strongly than another (Lanier et al., 2018). In light of these considerations, it may be beneficial for future research to compare current results to analyses using alternative methods for operationalizing risk.
Despite the above limitations, the current study provides important information regarding how risk and sleep behavior may be associated with social-emotional functioning in the first year of life. The associations between greater cumulative risk, less efficient sleep, and more social-emotional problems highlight the potential benefits of targeted intervention for infants from high-risk backgrounds. The current study also provides evidence that better quality sleep is associated with more positive social-emotional functioning when examined both cross-sectionally and longitudinally. Therefore, sleep interventions may improve both current and future social-emotional functioning. The lack of an interaction between cumulative risk and infant sleep indicates that sleep interventions may promote positive development in these areas in all children, regardless of their risk exposure. Our study adds to the current body of literature by extension to a younger sample; these results demonstrate that the effects of higher risk exposure and more negative sleep behaviors on social-emotional functioning can be identified as early as 12 months. Additionally, our study represents a racially and socioeconomically diverse group of families who experience a unique range of challenges but are often overlooked in research. Addressing sleep difficulties and social-emotional problems in infancy may mitigate some of the more extreme challenges observed in high-risk preschool or school aged children who have not received any form of early intervention.
Supplementary Material
Highlights.
Cumulative risk was related to infant sleep and social-emotional problems.
The acquisition of social-emotional milestone at 12 months was unrelated to cumulative risk.
Infants with less efficient sleep had more social-emotional problems and poorer typical social-emotional development.
Enhancing sleep efficiency may promote social-emotional functioning despite risk.
Risk and sleep have unique associations with infant social-emotional problems.
Acknowledgements
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD095957. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Support also was provided by the Mildred E. Swanson Foundation (SW).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to disclose.
References
- Abidin RR (2012). Parenting Stress Index (PSI) manual PAR. [Google Scholar]
- Adawi M, Zerbetto R, Re TS, Bisharat B, Mahamid M, Amital H, Del Puente G, Bragazzi NL (2019). Psychometric properties of the Brief Symptom Inventory in nomophobic subjects: Insights from preliminary confirmatory factor, exploratory factor, and clustering analyses in a sample of healthy Italian volunteers. Psychology Research and Behavior Management, 12, 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, & van der Ende J (2010). Adult outcomes of childhood dysregulation: A 14-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 49(11), 1105–1116. 10.1016/j.jaac.2010.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline S (2009). Associations of executive function with sleepiness and sleep duration in adolescents. Pediatrics, 123(4), e701–e707. 10.1542/peds.2008-1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Rodriguez GM, Blake CA, Linares D, & Carter AS (2012). Assessment of behavioral and emotional problems in infancy: A systematic review. Clinical Child and Family Psychology Review, 15, 113–128. 10.1007/s10567-012-0110-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso NE, Hungerford GM, Garcia D, Graziano PA, & Bagner DM (2016). Psychometric properties of the Parenting Stress Index-Short Form (PSI-SF) in a high-risk sample of mothers and their infants. Psychological Assessment, 28(10), 1331–1335. 10.1037/pas0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer JK, Ukoumunne OC, Mathers M, Wake M, Abdi N, & Hiscock H (2012). Development of children’s internalizing and externalizing problems from infancy to five years of age. Australian & New Zealand Journal of Psychiatry, 46(7), 659–668. 10.1177/0004867412450076 [DOI] [PubMed] [Google Scholar]
- Belanger M, Bernier A, Simard V, Desrosiers K, & Carrier J (2018). Sleeping toward behavioral regulation: Relations between sleep and externalizing symptoms in toddlers and preschoolers. Journal of Clinical Child & Adolescent Psychology, 47(3), 366–373. 10.1080/15374416.2015.1079782 [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ (1996). A parent assessment of social-emotional and behavior problems and competence for infants and toddlers: Reliability, validity, and associations with maternal symptoms and parenting stress. Dissertation Abstracts International: Section B: The Sciences and Engineering, 57(6-B), 4051 [Google Scholar]
- Briggs-Gowan MJ, & Carter AS (2002). Brief Infant-Toddler Social and Emotional Assessment (BITSEA) manual, version 2.0. New Haven, CT: Yale University. Behavior Questionnaire. Infant Behavior & Development, 26, 64–86. [Google Scholar]
- Briggs-Gowan MJ, & Carter AS (2008). Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics, 121(5), 957–962. 10.1542/peds.2007-1948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, & Carter AS, Irwin JR, Wachtel K, & Cicchetti DV (2004). The Brief Infant-Toddler Social and Emotional Assessment: Screening for social-emotional problems and delays in competence. Journal of Pediatric Psychology, 29(2), 143–155. 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM (2006). Are infant-toddler social-emotional and behavioral problems transient? Journal of the American Academy Child & Adolescent Psychiatry, 45(7), 849–858. 10.1097/01.chi.0000220849.48650.59 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U, & Morris PA (1998). The ecology of developmental processes. In Damon W, & Lerner RM (Eds.), Handbook of Child Psychology, Vol. 1: Theoretical Models of Human Development (pp. 993–1028). Wiley [Google Scholar]
- Chang H, Shelleby EC, Cheong J, & Shaw DS (2012). Cumulative risk, negative emotionality, and emotional regulation as predictors of social competence in transition to school: A mediated moderation model. Social Development, 21(4), 780–800. 10.1111/j.1467-9507.2011.00648.x [DOI] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8, 597–600. 10.1017/S0954579400007318 [DOI] [Google Scholar]
- Clarkson Freeman PA (2014). Prevalence and relationship between adverse childhood experiences and child behavior among young children. Infant Mental Health Journal, 35(6), 544–554. 10.1002/imhj.21460 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. [PubMed] [Google Scholar]
- El-Sheikh M, Hinnant JB, Kelly RJ, & Erath S (2010). Maternal psychological control and child internalizing symptoms: Vulnerability and protective factors across bioregulatory and ecological domains. Journal of Child Psychology and Psychiatry, 51(2), 188–198. 10.1111/j.1469-7610.2009.02140.x [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P, Ting AH, Tesher HB, & Shannis D (2007). Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Developmental Psychology, 43(2), 341–351. 10.1037/0012-1649.43.2.341 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventative Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Field T (2017). Infant sleep problems and interventions: A review. Infant Behavior and Development, 47, 40–53. 10.1016/j.infbeh.2017.02.002 [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Putnam SP, & Rothbart MK (2012). Etiology of preschool behavior problems: Contributions of temperament attributes in early childhood. Infant Mental Health Journal, 33(2), 197–211. 10.1002/imhj.21312 [DOI] [PubMed] [Google Scholar]
- Gartstein MA, & Rothbart MK (2003). Studying infant temperament via the Revised Infant Behavior Questionnaire 10.1016/S0163-6383(02)00169-8 Pediatric Psychology Press. [DOI] [Google Scholar]
- Glass TJA, Chau V, Gardiner J, Foong J, Vinall J, Zwicker JG, Grunau RE, Synnes A, Poskitt KJ, & Miller SP (2017). Severe retinopathy of prematurity predicts delayed white matter maturation and poorer neurodevelopment. Archives of Disease in Childhood Fetal and Neonatal Edition, 102, F532–F537. 10.1136/archdischild-2016-312533 [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Tully E (2006). Depression in women who are mothers: An integrative model of risk for the development of psychopathology in their sons and daughters. In Keyes CLM & Goodman SH (Eds.), Women and depression: A handbook for the social, behavioral, and biomedical sciences (pp. 241–280). Cambridge University Press. 10.1017/CBO9780511841262.013 [DOI] [Google Scholar]
- Haller S, Deindl P, Cassini A, Suentens C, Zingg W, Abu Sin M, Velasco E, Weiss B, Ducomble T, Sixtensson M, Eckmanns T, Harder T (2016). Neurological sequelae of healthcare-associated sepsis in very-low-birthweight infants: Umbrella review and evidence-based outcome tree. Euro Surveillance, 21(8), 1–10. 10.2807/1560-7917.ES.2016.21.8.30143. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009). Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN (2019). The REDCap consortium: Building an international community of software partners. Journal of Biomedical Informatics, 95. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtmann M, Buchmann AR, Esser G, Schmidt MH, Banaschewski T, & Laucht M (2011). The Child Behavior Checklist-dysregulation profile predicts substance use, suicidality, and functional impairment: A longitudinal analysis. Journal of Child Psychology and Psychiatry, 52(2), 139–147. 10.1111/j.1469-7610.2010.02309.x [DOI] [PubMed] [Google Scholar]
- Hungerford GM, Garcia D, & Bagner DM (2015). Psychometric evaluation of the Brief Infant-Toddler Social and Emotional Assessment (BITSEA) in a predominately Hispanic,low-income sample. Journal of Psychopathology and Behavioral Assessment, 37, 493–503. 10.1007/s10862-015-9478-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karabekiroglu K, Briggs-Gowan MJ, Carter AS, Rodopman-Arman A, & Akbas S (2010). The clinical validity and reliability of the Brief Infant-Toddler Social and Emotional Assessment (BITSEA). Infant Behavior and Development, 33(4), 503–509. 10.1016/j.infbeh.2010.07.001 [DOI] [PubMed] [Google Scholar]
- Kempler L, Sharpe L, Miller CB, & Bartlett DJ (2016). Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Medicine Reviews, 29, 15–22. 10.1016/j.smrv.2015.08.002 [DOI] [PubMed] [Google Scholar]
- Kerker BD, Zhang J, Nadeem E, Stein REK, Hurlburt MS, Heneghan A, Landsverk J, & McCue Horwitz. (2015). Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Academic Pediatrics, 15(5), 510–517. 10.1016/j.acap.2015.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebermass-Schrehof K, Czaba C, Olischar M, Fuiko R, Waldhoer T, Rona Z, Pollak A, & Weninger M (2012). Impact of low-grade intraventricular hemorrhage on long-term neurodevelopmental outcome in preterm infants. Child’s Nervous System, 28, 2085–2092. 10.1007/s00381-012-1897-3 [DOI] [PubMed] [Google Scholar]
- Lajiness-O’Neill R, Brooks J, Lukomski A, Schilling S, Huth-Bocks A, Warschausky S, Flores A, Swick C, Nyman T, Andersen T, Morris N, Schmitt TA, Bell-Smith J, Moir B, Hodges EK, Lyddy JE (2018). Development and validation of PediaTrac™: A web-based tool to track developing infants. Infant Behavior and Development, 50, 224–237. 10.1016/j.infbeh.2018.01.008 [DOI] [PubMed] [Google Scholar]
- Lajiness-O’Neill R, Warschausky S, Huth-Bocks A, Taylor HG, Brooks J, Lukomski A, Raghunathan T, Berglund P, Staples A, Erdodi L, & Schilling S (2021). PediaTrac™ 3.0 Protocol: A prospective, longitudinal study of the development and validation of a web-based tool to measure and track infant and toddler development from birth through 18 months. BMJ Open [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Norman SB, Means-Christensen A, & Stein MB (2009). Abbreviated brief symptom inventory for use as an anxiety and depression screening instrument in primary care. Depression and Anxiety, 26, 537–543. 10.1002/da.20471 [DOI] [PubMed] [Google Scholar]
- Lanier P, Maguire-Jack K, Lombardi B, Frey J, Rose RA (2018). Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal, 22, 288–297. 10.1007/s10995-017-2365-1 [DOI] [PubMed] [Google Scholar]
- Lee J, Croen LA, Lindan C, Nash KB, Yoshida CK, Ferriero DM, Barkovich AJ, & Wu YW (2005). Predictors of outcome in perinatal arterial stroke: A population-based study. Annals of Neurology, 58(2), 303–308. 10.1002/ana.20557 [DOI] [PubMed] [Google Scholar]
- Lima J, Caughy M, Nettles SM, & O’Campo PJ (2010). Effects of cumulative risk on behavioral and psychological well-being in first grade: Moderation by neighborhood context. Social Science & Medicine, 71, 1447–1454. 10.1016/j.socscimed.2010.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantymaa M, Puura K, Luoma I, Latva R, Salmelin RK, Tamminen T (2012). Predicting internalizing and externalizing problems at five years by child and parental factors in infancy and toddlerhood. Child Psychiatry & Human Development, 43, 153–170. 10.1007/s10578-011-0255-0 [DOI] [PubMed] [Google Scholar]
- Marti M, Bonillo A, Jane MC, Fisher EM, Duch H (2016). Cumulative risk, the mother-child relationship, and social-emotional competence in Latino Head Start children. Early Education and Development, 27(5), 590–622. 10.1080/10409289.2016.1106202 [DOI] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesman J, Bongers IL, & Koot HM (2001). Preschool developmental pathways to preadolescent internalizing and externalizing problems. Journal of Child Psychology and Psychiatry, 42(5), 679–689. 10.1017/S0021963001007351 [DOI] [PubMed] [Google Scholar]
- Mohammadkhani P, Dobson KS, Amiri M, & Hosseini Ghafari F (2010). Psychometric properties of the Brief Symptom Inventory in a sample of recovered Iranian depressed patients. International Journal of Clinical and Health Psychology, 10(3), 541–551. https://doi.org/ [Google Scholar]
- Naglieri JA, LeBuffe PA, & Shapiro VB (2013). Assessment of social-emotional competencies related to resilience. In Goldstein S & Brooks RB (Eds.), Handbook of resilience in children (2nd ed., pp. 261–272). Springer. [Google Scholar]
- Pihlakoski L, Sourander A, Aromaa M, Rautava P, Helenius H, & Sillanpaa M (2006). The continuity of psychopathology from early childhood to preadolescence: A prospective cohort study of 3–12-year-old children. European Child & Adolescent Psychiatry, 15, 409–417. 10.1007/s00787-006-0548-1 [DOI] [PubMed] [Google Scholar]
- Putnam SP, Helbig AL, Gartstein MA, Rothbart MK, & Leerkes E (2014) Development and Assessment of Short and Very Short Forms of the Infant Behavior Questionnaire–Revised, Journal of Personality Assessment, 96:4, 445–458, DOI: 10.1080/00223891.2013.841171 [DOI] [PubMed] [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. [Google Scholar]
- Reed DL, & Sacco WP (2016). Measuring sleep efficiency: What should the denominator be? Journal of Clinical Sleep Medicine, 12, 263–266. 10.5664/jcsm.5498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter A, Silfverdal S, Lindblom K, Hjern A (2020). A systematic review of prevention and treatment of infant behavioral sleep problems. Acta Paediatrica, 109, 1717–1732. 10.1111/apa.15182 [DOI] [PubMed] [Google Scholar]
- Robertson CM, Etches PC Goldson E, Kyle JM (1992). Eight-year school performance, neurodevelopmental, and growth outcome of neonates with bronchopulmonary dysplasia, A comparative study. Pediatrics, 89, 365–372. [PubMed] [Google Scholar]
- Sadeh A (2004) A Brief Screening Questionnaire for infant sleep problems: validation and findings for an internet sample, Pediatrics, 15(13): 43–46. 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- Sadeh A, De Marcas G, Guri Y, Berger A, Tikotzky L, & Bar-Haim Y (2015) Infant sleep predicts attention regulation and behavior problems at 3–4 years of age, Developmental Neuropsychology, 40:3, 122–137. 10.1080/87565641.2014.973498 [DOI] [PubMed] [Google Scholar]
- Scharf RJ, Demmer RY, Silver EJ, & Stein REK (2013). Nighttime sleep duration and externalizing behaviors of preschool children. Journal of Developmental and Behavioral Pediatrics, 34(6), 384–391. 10.1097/DBP.0b013e31829a8a0d [DOI] [PubMed] [Google Scholar]
- Scher A, Hall WA, Zaidman-Zait A, & Weinberg J (2009). Sleep quality, cortisol levels, and behavioral regulation in toddlers. Developmental Psychobiology, 52, 44–53. 10.1002/dev.20410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwichtenberg AJ, Abel EA, Keys E, & Honaker SM (2019). Diversity in pediatric behavioral sleep intervention studies. Sleep Medicine Reviews, 47, 103–111. 10.1016/j.smrv.2019.07.004 [DOI] [PubMed] [Google Scholar]
- Tham EKH, Schneider N, & Broekman BFP (2017). Infant sleep and its relation with cognition and growth: A narrative review. Nature and Science of Sleep, 9, 135–149. 10.2147/NSS.S125992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA, Easterbrooks MA, & Padilla-Walker LM (2012). Social and emotional development in infancy. In Weiner IB, Lerner RM, Easterbrooks MA, & Mistry J (Eds.), Handbook of Psychology: Vol. 6. Developmental Psychology (2nd ed., pp. 91–112). John Wiley & Sons. 10.1002/9781118133880.hop206004 [DOI] [Google Scholar]
- United States Census Bureau. (2020). Quick facts: United States https://www.census.gov/quickfacts/fact/table/US/PST045219
- van Buuren S, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 10.18635/jss.v045.io3 [DOI] [Google Scholar]
- Weitzman C, Edmonds D, Davagnino J, Briggs-Gowan MJ (2014). Young child socioemotional/behavioral problems and cumulative psychosocial risk. Infant Mental Health Journal, 35(1), 1–9. 10.1002/imhj.21421 [DOI] [PubMed] [Google Scholar]
- Williamson AA, & Mindell JA (2020). Cumulative socio-demographic risk factors and sleep outcomes in early childhood. Sleep, 43(3), zsz233. 10.1093/sleep/zsz233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson AA, Mindell JA, Hiscock H, & Quach J (2019). Sleep problem trajectories and cumulative socio-ecological risks: Birth to school-age. The Journal of Pediatrics, 215, 299–237. 10.1016/j.jpeds.2019.07.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


