ABSTRACT
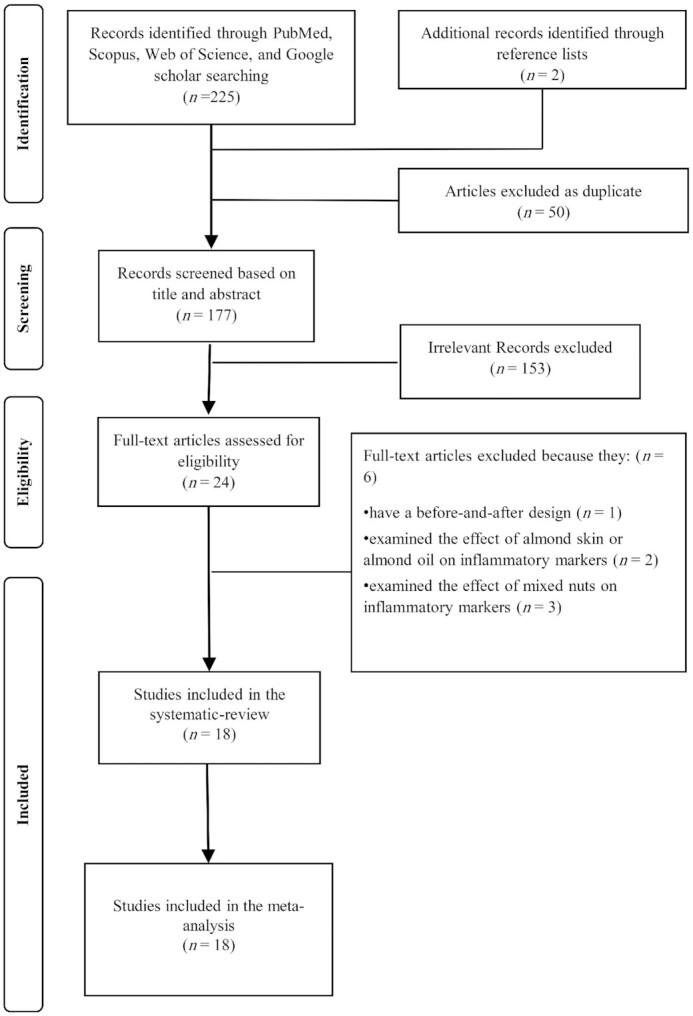
Conflicting findings have been reported regarding the effects of almond consumption on inflammatory markers. This study aimed to summarize the current literature to determine whether almonds can affect inflammatory markers. A systematic search was carried out in PubMed, Scopus, and ISI Web of Science up to March 2021. Randomized clinical trials that compared almond with no almond consumption were included. The outcomes of interest were changes in circulating C-reactive protein (CRP), IL-6, TNF-α, intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) concentrations. The random-effects model was used to find the mean differences. In total, 18 trials with 847 participants were eligible for the current analysis. Participants’ ages ranged from 26.3 to 69.6 y. Combining 16 studies, almond consumption significantly reduced serum concentrations of CRP [weighted mean difference (WMD): −0.25 mg/L; 95% CI: −0.43, −0.06 mg/L; I2 = 0.0%; P-heterogeneity = 0.633]. However, the beneficial effect of almond intake only occurred at doses <60 g/d. Pooling 11 effect sizes, almond interventions significantly decreased circulating IL-6 concentrations (WMD: −0.11 pg/mL; 95% CI: −0.21, −0.01 pg/mL; I2 = 19.9%; P-heterogeneity = 0.254). In subgroup analyses, effects on CRP and IL-6 were nonsignificant in unhealthy participants or those with obesity. In addition, almond consumption had no significant effect on TNF-α (WMD: −0.05 pg/mL; 95% CI: −0.11, 0.01 pg/mL; I2 = 0.0%; P-heterogeneity = 0.893; n = 6), ICAM-1 (WMD: 6.39 ng/mL; 95% CI: −9.44, 22.22 ng/mL; I2 = 66.6%; P-heterogeneity = 0.006; n = 7), or VCAM-1 (WMD: −8.31 ng/mL; 95% CI: −35.32, 18.71 ng/mL; I2 = 58.8%; P-heterogeneity = 0.033; n = 6). In conclusion, almond consumption beneficially affects CRP and IL-6 concentrations in adults. However, it has no beneficial effect on TNF-α, ICAM-1, or VCAM-1. More trials are needed to determine the effects of almonds on inflammation.
Keywords: almond, C-reactive protein, interleukin-6, inflammation, meta-analysis, clinical trial
Statement of Significance: This is the most comprehensive meta-analysis of randomized clinical trials examining the effects of almond consumption on inflammatory biomarkers. Almonds might have beneficial effects on CRP and IL-6 concentrations.
Introduction
Long-term inflammation has been linked to various diseases, including cardiovascular diseases (CVDs), diabetes, cancer, and metabolic syndrome, which are the primary causes of mortality (1–5). In this condition, abnormal concentrations of inflammatory biomarkers, including C-reactive protein (CRP), IL-6, TNF-α, intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) as well as anti-inflammatory biomarkers exist (6). Along with medications, lifestyle modifications including improvement in dietary habits and being more physically active could attenuate inflammation status (7).
It has been demonstrated that healthy dietary patterns such as the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) might improve inflammatory status (8, 9). Nut consumption is one of the recommendations in the 2 aforementioned diets (8, 9). The findings of observational studies revealed the link between nut consumption and chronic disease (10, 11). According to the previous studies, intake of different nuts could improve inflammation, as well as blood lipids, insulin resistance, and blood pressure due to the high contents of fiber, antioxidants, unsaturated fats, and phytosterols (6, 12, 13). Among nuts, the effect of almonds on CVD risk factors such as inflammation has gained increasing interest (14). Almonds might have favorable effects on inflammation because of the high content of magnesium, which could regulate proinflammatory gene expression (15). However, clinical trials examining the effects of almonds on inflammatory biomarkers have inconsistent findings (16–18). Two recent meta-analyses regarding the effects of almond consumption on inflammatory markers have included randomized clinical trials (RCTs) up to 2017 (19, 20). In Xiao et al.’s (20) meta-analysis, almond intake did not improve inflammatory markers, including CRP, IL-6, TNF-α, ICAM-1, and VCAM-1. Similarly, the other meta-analysis (19) did not find that almonds beneficially affect CRP concentrations. As far as we know, 7 new clinical trials have been published regarding the effect of almond consumption on inflammatory markers since 2017. Furthermore, clinical trials with comparison groups other than controls had not been included in the earlier meta-analyses, and some studies were missed. Given these aforesaid reasons, the current study was carried out to summarize the effect of almond consumption on inflammatory markers (including CRP, IL-6, ICAM-1, VCAM-1, and TNF-α) through a meta-analysis.
Methods
Data sources and search strategy
Findings from this systematic review and meta-analysis were reported based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (21). A comprehensive search was performed on the databases of PubMed, Scopus, and ISI Web of Science (SCI-EXPANDED, SSCI, and ESCI) up to March 22, 2021 without any time and language restriction. We used a mixture of the 3 following concepts of MeSH or non-MeSH terms: (almond OR “Prunus Amygdalus” OR “P. Amygdalus”) AND (interleukin OR IL OR Inflammation OR inflammatory OR “C-reactive protein” OR CRP OR “high‐sensitivity C‐reactive protein” OR “high-sensitivity CRP”) AND (intervention OR RCT OR “controlled trial” OR randomized OR random OR Randomly). Detailed information regarding the search items is presented in Supplemental Table 1. Furthermore, bibliographies of the relevant publications were checked to identify additional eligible studies. Then, duplicate articles were removed. The results of the search were screened by 2 researchers (SF and ED), independently. The study was registered at http://www.crd.york.ac.uk/Prospero (registration no. CRD42021249220).
Study selection
Publications were included if they met the following criteria: 1) clinical trials examining the effect of whole almond consumption on CRP, IL-6, ICAM-1, VCAM-1, or TNF-α in comparison with no-almond intervention (including control, placebo, or other nuts); 2) performed on adults aged ≥18 y; 3) had a minimum intervention period of 4 wk; and 4) reported both mean changes and SD values for the inflammatory markers, or baseline and follow-up means of the inflammatory markers and their corresponding SDs or values that are convertible to SDs (i.e., SE, IQR, CI). We also excluded publications that: 1) were review studies, animal studies, observational studies, and noninterventional studies; 2) had a before-and-after design; 3) examined the effect of almond skin or almond oil on inflammatory markers; or 4) examined mixed nuts consumption as the exposure.
Data extraction
Data from each article were extracted by 2 researchers (SF and KL) separately. The principal investigator (LA) resolved the disagreements. The extracted data included: first author's name, publication year, country, health status, type of study, study duration, number of participants in the intervention and control groups, gender and age of study participants, amount of almonds, blinding condition, inflammatory markers, and primary outcomes. We did not need to reach out to corresponding authors of the included studies to obtain missing or incomplete data.
Quality assessment
Two reviewers (SF and KL) assessed the quality of each included study using the risk of bias 2 (RoB-2) tool (22). Five items are examined based on the Cochrane risk-of-bias tool: 1) randomization process, 2) deviation from the intended interventions, 3) missing outcome data, 4) measurement of outcome, and 5) selection of the reported result. According to the Cochrane Handbook recommendations, items were labeled as “low risk of bias,” “high risk of bias,”, or “unclear” or unknown risk of bias.
Statistical analysis
The overall effect size was estimated using the mean changes in inflammatory biomarker concentrations and their SDs for both intervention and nonintervention groups. For the studies that did not report the mean changes, we subtracted baseline measures from values at the end of the intervention to calculate the mean changes. Based on previously published methods (23), we converted SEs (14), IQRs, and 95% CIs to SDs. A random-effects model was applied, which considers between-study variation, to assess the overall effect size. In the case of multiarm trials (17, 18, 24), we combined intervention groups to control possible unit of analysis errors (25). We used the I2 statistic and the Cochrane Q test to assess between-study heterogeneity. An I² value >50% or a P value < 0.1 for the Q test was considered as significant between-study heterogeneity (25). To find the potential sources of heterogeneity and to compare the effect of almond consumption in different conditions, we performed subgroup analyses based on participants’ age (≥50/<50 y), type of study (parallel/crossover), trial duration (4/>4 wk), almond dose (≥60/<60 g/d), individual's BMI (≥30 kg/m2 as obese/<30 as nonobese), health condition (healthy/unhealthy), blood glucose (<100 mg/dL or <5.6 mmol/L as normal/≥100 mg/dL or ≥5.6 mmol/L as elevated), LDL cholesterol (<130 mg/dL or <3.4 mmol/L as normal/≥130 mg/dL or ≥3.4 mmol/L as elevated), and blood pressure (<120/80 mmHg as normal/≥120/80 mmHg as elevated). We also performed subgroup analysis based on CRP and IL-6 at the baseline. For baselines of CRP, we used the cutoff value (≥3/<3) that was mostly used in the previous studies (26–28). Furthermore, we used (≥median/<median) as the cutoff for the baseline IL-6 subgroup (29). For the studies that reported almond dose as percentage of energy intake, we multiplied the reported percentage by the reported mean energy intake of the trial participants to recalculate the dosage in grams per day. Subgroup analysis based on the type of study was prespecified, whereas other subgroup analyses were added afterwards. Sensitivity analysis was carried out to explore the influence of each study on the overall effect size. Publication bias was examined by funnel plot asymmetry and the Egger test. These tests have low power to distinguish between chance and real asymmetry when <10 studies are included; therefore, we did not examine potential publication bias for TNF-α, ICAM-1, and VCAM-1. All of the statistical analyses were done using STATA (version 14; StataCorp LLC). Furthermore, a P value < 0.05 was considered statistically significant.
Results
Literature search
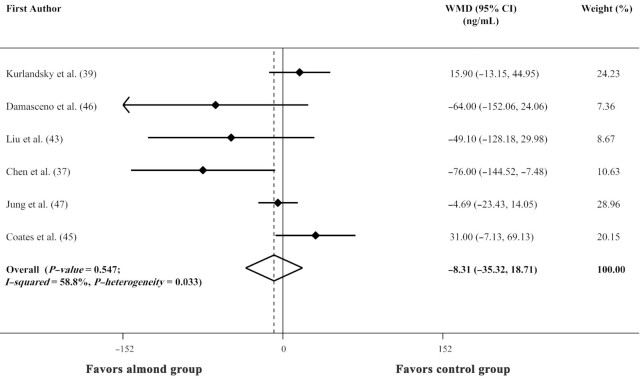
Initially, 227 articles were identified in our search. After excluding duplicate articles, 177 articles remained for title and abstract screening. Of these, 153 unrelated articles were removed. Among the 24 remaining articles, a trial with a before-and-after design was excluded (30). Furthermore, 5 studies that assessed the effect of almond oil, almond skin, and mixed nuts on inflammatory biomarkers were not included in the current study (31–35). Finally, 18 eligible clinical trials were included in the present systematic review and meta-analysis. Serum concentrations of IL-6, CRP, ICAM-1, VCAM-1, and TNF-α were respectively evaluated in 11, 16, 7, 6, and 6 trials. The flowchart of study selection is presented in Figure 1.
FIGURE 1.
Flowchart of the study selection process.
Study characteristics
The characteristics of 18 eligible trials are reported in Table 1. Studies had a total sample size of 847 participants, ranging in number from 18 to 128. The mean age of subjects ranged between 26.3 and 69.6 y. The mean BMI at baseline ranged from 22.6 to 35.2. Eight of the included studies had a parallel design, and 10 studies had a crossover design. These studies were published from 2002 to 2021 and were from the United States (16–18, 36–41), Taiwan (42, 43), Australia (44, 45), Spain (46), South Korea (47, 48), China (49), and Canada (24). Participants were followed from 4 to 24 wk. Two studies were performed in females (38, 39), and the others in both genders (16–18, 24, 36, 37, 40–49). Trials were performed on healthy individuals (17, 18, 24, 36, 39, 40, 44, 45, 47, 48), patients with type 2 diabetes (16, 42, 43, 49), hypercholesterolemia (46), coronary artery disease (37), women with polycystic ovary syndrome (38), and prediabetic individuals (41). The almond dosage used in studies varied from 41.14 to 100 g/d. Three studies (17, 18, 24) were multiarm trials (2 intervention groups compared with 1 no-intervention group) and others had 2 arms (1 intervention group compared with 1 no-intervention group).
TABLE 1.
Characteristics of the included randomized trials on the effects of almond consumption on inflammatory biomarkers in adults1
| Author (year) | Country | Study design | Gender | Sample size | Age,1 y | Health status | BMI,1 kg/m2 | Duration, wk | Almond dose | Comparison group | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kurlandsky and Stote (2006) (39) | USA | Parallel | Female | IG: 10CG: 10 | 43.7 | Healthy | 25.59 | 6 | 60 g/d | Self-selected diet avoiding nuts | CRP/ICAM-1/VCAM-1 |
| Chen et al. (2017) (42) | Taiwan | Crossover | Both | IG: 33CG: 33 | 54.9 | Type 2 diabetes | 25.45 | 12 | 60 g/d | NCEP step 2 diet | CRP/ICAM-1 |
| Lee et al. (2017) (40) | USA | Crossover | Both | IG: 31CG: 31 | 46.3 | Healthy | 29.6 | 4 | 42.5 g/d | 18 g cocoa powder, 43 g dark chocolate | CRP |
| Damasceno et al. (2011) (46) | Spain | Crossover | Both | IG: 18CG: 18 | 56 | Hypercholesterolemic patients | 25.7 | 4 | 22% energy (50–75 g/d) | 40–65 g walnuts | CRP/ICAM-1/VCAM-1 |
| Coates et al. (2020) (45) | Australia | Parallel | Both | IG: 63CG: 65 | 65 | Healthy | 30.4 | 12 | 15% energy | Nut-free diet | CRP/ICAM-1/VCAM-1 |
| Bowen et al. (2019) (44) | Australia | Parallel | Both | IG: 39CG: 35 | 60.7 | Healthy | 33.8 | 8 | 56 g/d | 72 g biscuit | CRP/IL-6/TNF-α |
| Chen et al. (2015) (37) | USA | Crossover | Both | IG: 45CG: 45 | 61.8 | Coronary artery disease | 30.2 | 6 | 85 g/d | NCEP step 1 diet | CRP/IL-6/VCAM-1/TNF-α |
| Kalgaonkar et al. (2011) (38) | USA | Parallel | Female | IG: 14CG: 17 | 33.45 | Polycystic ovary syndrome | 35.15 | 6 | 46 g/d | 36 g walnuts | CRP/IL-6/TNF-α |
| Sweazea et al. (2014) (16) | USA | Parallel | Both | IG: 10CG: 11 | 56.32 | Type 2 diabetes | 35.2 | 12 | 43 g/d | Control typical diet | CRP/IL-6/TNF-α |
| Palacios et al. (2020) (41) | USA | Crossover | Both | IG: 33CG: 33 | 48.3 | Prediabetes | 30.5 | 6 | 85 g/d | Carbohydrate-based foods | CRP/IL-6 |
| Jung et al. (2018) (47) | South Korea | Crossover | Both | IG: 84CG: 84 | 52.4 | Healthy | 25.4 | 4 | 56 g/d | Cookie | CRP/IL-6/ICAM-1/VCAM-1/TNF-α |
| Rajaram et al. (2010) (17) | USA | Crossover | Both | IG: 25CG: 25 | 41 | Healthy | >30 | 4 | 10% energy (41.16 g/d) | Control diet | CRP/IL-6 |
| 20% energy (82.96 g/d) | |||||||||||
| Liu et al. (2017) (48) | South Korea | Parallel | Both | IG: 58CG: 56 | 26.33 | Healthy | 22.59 | 16 | 56 g/d | High-carbohydrate isocaloric control food | IL-6 |
| Hou et al. (2018) (49) | China | Parallel | Both | IG: 14CG: 11 | 69.6 | Type 2 diabetes | 23.53 | 12 | Male: 55 g/dFemale: 45 g/d | 60 g peanuts for men50 g peanuts for women | IL-6 |
| Berryman et al. (2015) (36) | USA | Crossover | Both | IG: 48CG: 48 | 49.9 | Healthy | 26.2 | 6 | 42.5 g/d | Isocaloric muffin + 2.7 g butter | CRP |
| Jenkins et al. (2002) (24) | Canada | Crossover | Both | IG: 27CG: 27 | 64 | Healthy | 25.7 | 4 | 37 g/d | 75 g muffins | CRP |
| 73 g/d | 150 g muffins | ||||||||||
| Rakic et al. (2021) (18) | USA | Parallel | Both | IG1: 19IG2: 24CG: 27 | 61.51 | Healthy | 29 | 24 | 42 g/d84 g/d | 100 g/d snack mix | CRP/IL-6/ICAM-1 |
Values are means. CG, comparison group; CRP, C-reactive protein; ICAM-1, intercellular adhesion molecule-1; IG, intervention group; NCEP, US National Cholesterol Education Program; VCAM-1, vascular cell adhesion molecule-1.
Quality assessment
Having a low risk of bias for all domains of the RoB-2 risk-of-bias assessment tool, only 1 trial (44) was considered as a high-quality study. Five trials (17, 18, 39, 42, 46) had moderate quality, in which ≥1 domain had an unclear risk of bias. The remaining 12 studies (16, 24, 36–38, 40, 41, 43, 45, 47–49) were of low quality because they had a high risk of bias for ≥1 domain (Table 2).
TABLE 2.
Risk of bias for randomized clinical trials on the effects of almonds on inflammatory biomarkers in adults1
| First author (year) | Randomization process | Deviation from the intended interventions | Missing outcome data | Measurement of outcome | Selection of the reported result | Overall bias |
|---|---|---|---|---|---|---|
| Kurlandsky and Stote (2006) (39) | L | U | L | L | L | U |
| Chen et al. (2017) (42) | L | U | L | L | L | U |
| Lee et al. (2017) (40) | L | L | L | L | H | H |
| Damasceno et al. (2011) (46) | L | U | L | L | L | U |
| Coates et al. (2020) (45) | L | L | L | L | H | H |
| Liu et al. (2013) (43) | L | H | L | L | L | H |
| Bowen et al. (2019) (44) | L | L | L | L | L | L |
| Chen et al. (2015) (37) | L | H | L | L | L | H |
| Kalgaonkar et al. (2011) (38) | L | H | L | L | L | H |
| Sweazea et al. (2014) (16) | L | H | L | L | L | H |
| Palacios et al. (2020) (41) | L | H | L | L | H | H |
| Jung et al. (2018) (47) | L | H | L | L | L | H |
| Rajaram et al. (2010) (17) | L | U | L | L | L | U |
| Liu et al. (2017) (48) | L | U | L | L | H | H |
| Hou et al. (2018) (49) | L | L | L | L | H | H |
| Berryman et al. (2015) (36) | L | U | L | L | H | H |
| Jenkins et al. (2002) (24) | L | H | L | L | H | H |
| Rakic et al. (2021) (18) | L | U | L | L | L | U |
Using the new version of the Cochrane Handbook for Systematic Reviews of Interventions (V6.2). L, low risk of bias; H, high risk of bias; U, unclear risk of bias.
Findings from the systematic review
Among 11 RCTs evaluating the effect of almond consumption on serum concentrations of IL-6, 2 studies showed a beneficial effect (43, 47), whereas others reported no significant effect. Furthermore, of 16 RCTs that examined the effects of almond consumption on serum CRP concentrations, 3 studies reported a significant effect of almond consumption on reducing serum CRP concentrations (16, 17, 43). However, others found no significant change. For ICAM-1 and TNF-α, a significant beneficial effect was reported in only 1 study. Also, no trial showed a beneficial effect of almond consumption on VCAM-1.
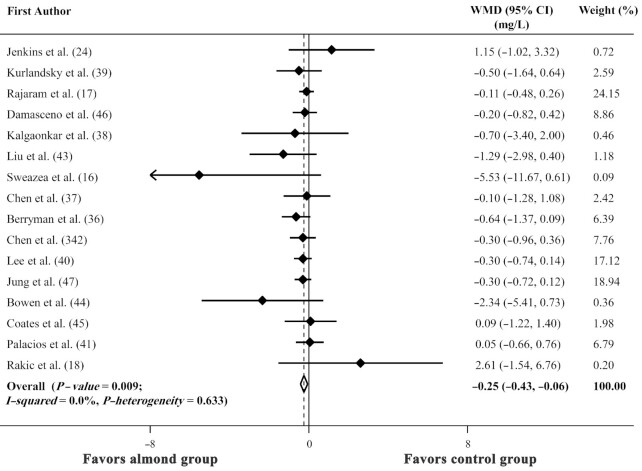
The effect of almond consumption on serum CRP concentrations
In total, 16 trials embracing 708 participants were eligible for this meta-analysis. Combining 16 effect sizes from these studies indicated that almond consumption compared with a comparison group had a favorable effect on CRP concentrations [weighted mean difference (WMD): −0.25 mg/L; 95% CI: −0.43, −0.06 mg/L; P-value = 0.009] (Figure 2). Between-study heterogeneity was nonsignificant (I2 = 0.0%; P-heterogeneity = 0.633). Results from subgroup analyses are reported in Table 3. In summary, almond consumption could have a favorable effect on CRP concentrations in healthy and nonobese adults. Also, the effect was significant only at doses <60 g/d. We also found a significant effect in participants with baseline CRP concentrations <3 mg/L and in those who had normal blood glucose and blood pressure. According to the sensitivity analysis, the exclusion of any single study did not influence the overall effect size. The Egger test showed no evidence of potential publication bias (P value = 0.437). Also, no asymmetry was visually observed in the funnel plot.
FIGURE 2.
Forest plot of the effect of almond consumption on C-reactive protein in adults, using the random effects model. WMD, weighted mean difference.
TABLE 3.
Results of subgroup analysis for the effects of almond consumption on inflammatory biomarkers in adults1
| Effect size, n | WMD (95% CI), pg/mL | P within2 | I 2, %3 | P between4 | |
|---|---|---|---|---|---|
| Subgroup analysis for the effect of almond consumption on serum IL-6 | |||||
| Overall | 11 | −0.11 (−0.21, −0.01) | 0.254 | 19.9 | |
| Age | 0.05 | ||||
| <50 y | 4 | −0.06 (−0.11, −0.01) | 0.463 | 0 | |
| ≥50 y | 7 | −0.20 (−0.35, −0.06) | 0.397 | 3.9 | |
| Dose | 0.812 | ||||
| <60 g | 8 | −0.14 (−0.29, 0.01) | 0.122 | 38.6 | |
| ≥60 g | 3 | −0.05 (−0.27, 0.18) | 0.600 | 0 | |
| BMI | 0.834 | ||||
| Nonobese | 5 | −0.14 (−0.27, −0.01) | 0.137 | 42.7 | |
| Obese | 6 | −0.05 (−0.29, 0.18) | 0.362 | 8.5 | |
| Duration | 0.712 | ||||
| >4 wk | 8 | −0.13 (−0.33, 0.06) | 0.090 | 43.3 | |
| 4 wk | 3 | −0.10 (−0.26, 0.05) | 0.994 | 0 | |
| Population | 0.827 | ||||
| Healthy | 5 | −0.14 (−0.34, 0.05) | 0.070 | 53.8 | |
| Unhealthy | 6 | −0.09 (−0.25, 0.06) | 0.582 | 0 | |
| Baseline IL-6 | 0.912 | ||||
| <Median | 4 | −0.15 (−0.33, 0.03) | 0.094 | 53.1 | |
| ≥Median | 7 | −0.08 (−0.24, 0.08) | 0.415 | 1.2 | |
| Baseline blood glucose | 0.047 | ||||
| Normal | 4 | −0.06 (−0.11, −0.02) | 0.602 | 0 | |
| Elevated | 4 | −0.05 (−0.28, 0.17) | 0.313 | 15.8 | |
| NR | 3 | −0.34 (−0.55, −0.13) | 0.628 | 0 | |
| Baseline serum LDL cholesterol | 0.743 | ||||
| Normal | 9 | −0.12 (−0.27, 0.02) | 0.156 | 32.7 | |
| Elevated | 1 | 2.65 (−5.26, 10.56) | — | — | |
| NR | 1 | −0.11 (−0.29, 0.07) | — | — | |
| Baseline blood pressure | 0.046 | ||||
| Normal (<120/80 mm Hg) | 3 | −0.26 (−0.46, −0.07) | 0.356 | 3.3 | |
| High (≥120/80 mm Hg) | 6 | −0.07 (−0.11, −0.02) | 0.839 | 0 | |
| NR | 2 | −3.64 (−20.50, 13.22) | 0.139 | 54.4 | |
| Study type | 0.886 | ||||
| Parallel | 6 | −0.18 (−0.47, 0.11) | 0.046 | 55.7 | |
| Crossover | 5 | −0.09 (−0.23, 0.05) | 0.880 | 0 | |
| Subgroup analysis for the effect of almond consumption on serum CRP | |||||
| Overall | 16 | −0.25 (−0.43, −0.06) | 0.633 | 0 | |
| Age | 0.839 | ||||
| <50 y | 6 | −0.23 (−0.47, 0.01) | 0.754 | 0 | |
| ≥50 y | 10 | −0.26 (−0.59, 0.06) | 0.358 | 9.2 | |
| Dose | 0.231 | ||||
| <60 g | 9 | −0.40 (−0.78, −0.02) | 0.259 | 20.7 | |
| ≥60 g | 7 | −0.14 (−0.39, 0.11) | 0.983 | 0 | |
| BMI | 0.282 | ||||
| Nonobese | 9 | −0.32 (−0.55, −0.09) | 0.653 | 0 | |
| Obese | 7 | −0.11 (−0.42, 0.19) | 0.483 | 0 | |
| Duration | 0.731 | ||||
| >4 wk | 10 | −0.30 (−0.64, 0.05) | 0.455 | 0 | |
| 4 wk | 6 | −0.22 (−0.44, −0.01) | 0.598 | 0 | |
| Population | 0.737 | ||||
| Healthy | 8 | −0.27 (−0.48, −0.05) | 0.566 | 0 | |
| Unhealthy | 8 | −0.20 (−0.54, 0.15) | 0.460 | 0 | |
| Baseline CRP | 0.216 | ||||
| <3 mg/L | 10 | −0.21 (−0.40, −0.02) | 0.737 | 0 | |
| ≥3 mg/L | 6 | −0.67 (−1.36, 0.03) | 0.412 | 0.7 | |
| Baseline blood glucose | 0.835 | ||||
| Normal | 7 | −0.25 (−0.46, −0.04) | 0.907 | 0 | |
| Elevated | 5 | −0.50 (−1.25, 0.25) | 0.150 | 40.7 | |
| NR | 4 | 0.01 (−0.82, 0.84) | 0.340 | 10.7 | |
| Baseline serum LDL cholesterol | 0.407 | ||||
| Normal | 11 | −0.20 (−0.42, 0.03) | 0.615 | 0 | |
| Elevated | 4 | −0.31 (−0.63, 0.01) | 0.447 | 0 | |
| NR | 1 | −1.29 (−2.98, 0.40) | — | — | |
| Baseline blood pressure | 0.624 | ||||
| Normal (<120/80 mm Hg) | 6 | −0.24 (−0.47, −0.01) | 0.396 | 3.3 | |
| High (≥120/80 mm Hg) | 7 | −0.20 (−0.54, 0.14) | 0.509 | 0 | |
| NR | 3 | −0.72 (−1.72, 0.27) | 0.545 | 0 | |
| Study type | 0.688 | ||||
| Parallel | 6 | −0.47 (−1.52, 0.57) | 0.232 | 27.0 | |
| Crossover | 10 | −0.24 (−0.43, −0.05) | 0.781 | 0 | |
| Subgroup analysis for the effect of almond consumption on serum TNF-α | |||||
| Overall | 6 | −0.05 (−0.11, 0.01) | 0.893 | 0 | |
| BMI | 0.745 | ||||
| Nonobese | 2 | −0.05 (−0.11, 0.01) | 0.553 | 0 | |
| Obese | 4 | −0.10 (−0.41, 0.20) | 0.751 | 0 | |
| Duration | 0.745 | ||||
| >4 wk | 4 | −0.10 (−0.41, 0.20) | 0.751 | 0 | |
| 4 wk | 2 | −0.05 (−0.11, 0.01) | 0.553 | 0 | |
| Population | 0.557 | ||||
| Healthy | 2 | −0.01 (−0.16, 0.14) | 0.790 | 0 | |
| Unhealthy | 4 | −0.06 (−0.13, 0.01) | 0.741 | 0 | |
| Subgroup analysis for the effect of almond consumption on serum ICAM-1 | |||||
| Overall | 7 | 6.39 (−9.44, 22.22) | 0.006 | 66.6 | |
| Dose | 0.854 | ||||
| <60 g | 3 | 10.83 (–19.49, 41.15) | 0.007 | 80.0 | |
| ≥60 g | 4 | 4.20 (–20.09, 28.50) | 0.048 | 62.1 | |
| Duration | 0.147 | ||||
| >4 wk | 4 | 10.17 (−16.82, 37.17) | 0.002 | 79.4 | |
| 4 wk | 3 | −5.21 (−13.79, 3.36) | 0.524 | 0 | |
| Population | 0.248 | ||||
| Healthy | 5 | 11.89 (−11.68, 35.45) | 0.002 | 79.2 | |
| Unhealthy | 3 | −8.17 (−26.77, 10.43) | 0.335 | 8.6 | |
| Subgroup analysis for the effect of almond consumption on serum VCAM-1 | |||||
| Overall | 6 | −8.31 (−35.32, 18.71) | 0.033 | 58.8 | |
| BMI | 0.662 | ||||
| Nonobese | 4 | −5.29 (−29.72, 19.13) | 0.187 | 37.5 | |
| Obese | 2 | −18.56 (−123.13, 86.02) | 0.007 | 86.0 | |
| Duration | 0.147 | ||||
| >4 wk | 3 | −0.30 (−47.11, 46.52) | 0.025 | 72.8 | |
| 4 wk | 3 | −19.23 (−53.39, 14.93) | 0.261 | 25.6 | |
| Population | 0.003 | ||||
| Healthy | 3 | 9.19 (−11.24, 29.63) | 0.188 | 40.2 | |
| Unhealthy | 3 | −64.34 (−108.98, −19.91) | 0.881 | 0 | |
CRP, C-reactive protein; ICAM-1, intercellular adhesion molecule-1; NR, not reported; VCAM-1, vascular cell adhesion molecule-1; WMD, weighted mean difference.
P for heterogeneity, within subgroup.
An I2 value >50% shows significant between-study heterogeneity.
P for heterogeneity, between subgroups.
Fourteen trials assessed high-sensitivity CRP, whereas 2 others (16, 43) considered CRP. Excluding the studies that considered CRP as the outcome of interest did not change our results (WMD: −0.23 mg/L; 95% CI: −0.41, −0.04 mg/L; P value = 0.016; I2 = 0.0%; P-heterogeneity = 0.827).
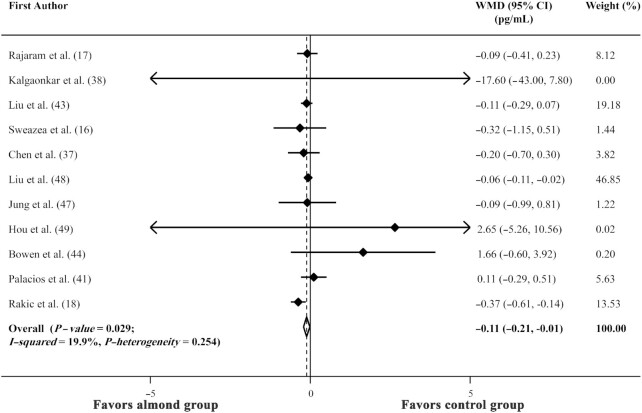
The effect of almond consumption on serum IL-6 concentrations
Combining 11 effect sizes, including an overall sample size of 547 participants, almond consumption, compared with a comparison group, led to a significant decrease in serum IL-6 concentrations (WMD: −0.11 pg/mL; 95% CI: −0.21, −0.01 pg/mL; P value = 0.029; I2 = 19.9%; P-heterogeneity = 0.254) (Figure 3). The results from subgroup analyses showed that almonds significantly lowered IL-6 concentrations in nonobese adults and those with normal blood glucose concentrations. We found that almonds might have more beneficial effects in adults aged ≥50 y. Also, significant heterogeneity was observed between age subgroups. More results are provided in Table 3. No significant changes in the overall effect size and the corresponding 95% CI were seen after performing sensitivity analysis. No asymmetry was seen in the funnel plot, and no evidence of publication bias was shown based on the Egger test (P value = 0.605).
FIGURE 3.
Forest plot of the effect of almond consumption on IL-6 in adults, using the random effects model. WMD, weighted mean difference.
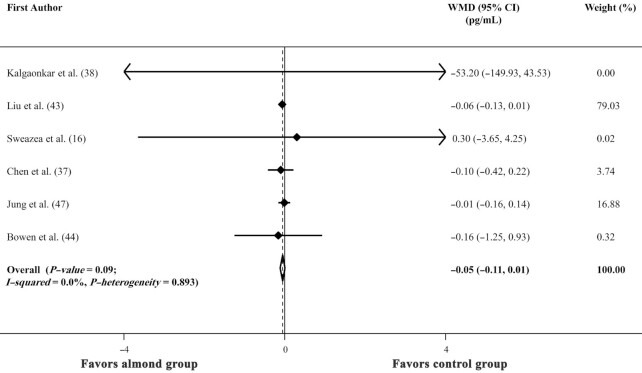
The effect of almond consumption on serum TNF-α concentrations
Findings from 6 trials revealed that almond consumption did not significantly lower TNF-α concentrations (WMD: −0.05 pg/mL; 95% CI: −0.11, 0.01 pg/mL; P value = 0.09; I2 = 0.0%; P-heterogeneity = 0.893) (Figure 4). Results remained nonsignificant in all subgroups (Table 3). Sensitivity analysis found no particular study would significantly affect the summary effects.
FIGURE 4.
Forest plot of the effect of almond consumption on TNF-α in adults, using the random effects model. WMD, weighted mean difference.
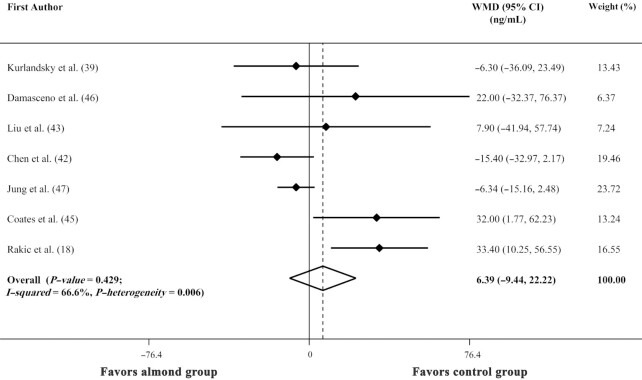
The effect of almond consumption on serum ICAM-1 and VCAM-1 concentrations
Combining 7 effect sizes from 7 trials, we found no beneficial effect of almonds in decreasing serum ICAM-1 concentrations (WMD: 6.39 ng/mL; 95% CI: −9.44, 22.22 ng/mL; P value = 0.429; I2 = 66.6%; P-heterogeneity = 0.006) (Figure 5). Our findings remained unchanged in all subgroups (Table 3). We found no significant changes in the overall effect size and the corresponding 95% CI according to sensitivity analysis.
FIGURE 5.
Forest plot of the effect of almond consumption on intercellular adhesion molecule-1 in adults, using the random effects model. WMD, weighted mean difference.
Results from 6 trials indicated no significant effect of almonds on VCAM-1 (WMD: −8.31 ng/mL; 95% CI: −35.32, 18.71 ng/mL; P value = 0.547; I2 = 58.8%; P-heterogeneity = 0.033) (Figure 6). Results did not change in all subgroups except for participants’ health status (Table 3). We found that almond consumption significantly decreased VCAM-1 in unhealthy participants (WMD: −64.34 ng/mL; 95% CI: −108.98, −19.91 ng/mL). However, it had no beneficial effect in healthy individuals. No particular study gave a significant change in the overall effect size based on sensitivity analysis.
FIGURE 6.
Forest plot of the effect of almond consumption on vascular cell adhesion molecule-1 in adults, using the random effects model. WMD, weighted mean difference.
Discussion
The current systematic review and meta-analysis revealed that almond consumption significantly alleviates IL-6 and CRP concentrations, 2 primary inflammatory markers. Also, subgroup analysis showed that these effects were significant in nonobese, as well as healthy individuals. Furthermore, no benefit for CRP was observed in daily doses >60 g almonds. Based on the subgroup analysis for study type, almond consumption significantly affected CRP concentrations in trials with a crossover design, whereas the results were not significant for parallel trials. On the other hand, we found no significant effect of almond consumption on TNF-α, ICAM-1, and VCAM-1. As far as we know, this is the most comprehensive study in which the effect of almond consumption on concentrations of inflammatory biomarkers is systematically reviewed and examined through a meta-analysis.
Studies have shown that increases in inflammatory factors could be a risk factor for some chronic diseases, such as metabolic syndrome (50), diabetes (51), cancers (52), coronary artery disease (53), and even mortality (54). Based on our findings, daily consumption of almonds can reduce CRP and IL-6 concentrations. However, almond consumption was found to have no significant effect on TNF-α, ICAM-1, and VCAM-1. Also, a previous meta-analysis revealed a significant effect of the DASH diet, in which consumption of nuts is highly recommended, in attenuating CRP concentrations (9). However, a study showed that mixed nuts consumption does not result in significant differences in CRP, IL-6, TNF-α, ICAM-1, and VCAM-1 (6). Similarly, a meta-analysis revealed that tree nuts (pistachios, almonds, macadamia nuts, pecans, hazelnuts, cashews, walnuts, and Brazil nuts) had no significant effect on CRP concentrations (13, 55). Given the results of studies regarding the effect of different nuts on inflammatory markers, daily intake of almonds in the context of a healthy diet (i.e., the DASH diet) could be recommended along with medications to attenuate inflammation. However, further studies are required to explore the particular effect of different nuts on inflammation status.
Our meta-analysis found beneficial effects of almond consumption on reducing CRP and IL-6 concentrations, whereas no significant effect was found in the case of other inflammatory markers. Prior to our study, 2 meta-analyses had examined the effect of almonds on inflammatory markers (19, 20). Xiao et al. (20) showed that nut consumption decreased the concentrations of ICAM-1 but had no significant effect on other inflammatory markers. Also, they found no significant effect of almonds on inflammatory biomarkers. Another meta-analysis depicted that consumption of almonds does not result in significant changes in high-sensitivity CRP (19). The inconsistency of our results regarding the effect of almond consumption on concentrations of CRP and IL-6 with those from the aforementioned meta-analyses might be due to the eligibility criteria of the studies. For example, Lee-Bravatti et al. (19) excluded some trials because of concerns regarding participants’ mismatches of energy intake. They also did not include trials in which almond consumption was compared with walnuts. Moreover, our review also includes more recently published research. Therefore, the lack of significant results found in other meta-analyses might be attributed to the limited number of included trials.
Other meta-analyses have also explored the effects of almond consumption on other cardiovascular risk factors. Asbaghi et al. (56) found that almonds could beneficially impact blood concentrations of triglycerides, total cholesterol, and LDL. However, they did not show a significant effect on HDL. Moreover, another meta-analysis revealed a significant effect of almonds on diastolic blood pressure, but no favorable effect was seen on systolic blood pressure (57).
Several mechanisms might explain the effect of almond consumption on CRP and IL-6. Almonds have high concentrations of magnesium, and a large cohort study showed that magnesium intake had an inverse association with some inflammatory factors such as CRP (58). Hypomagnesemia might increase inflammatory responses by: 1) activating phagocytic cells (59); 2) activating NF-κB signaling, which in turn upregulates transcription of some proinflammatory genes (59); and 3) decreasing nitric oxide, resolvins, lipoxins, and protectins, which are anti-inflammatory markers in the body (15). Furthermore, almonds contain considerable amounts of omega-3 (ω-3) fatty acids, which are precursors of eicosanoids with anti-inflammatory properties (60). The anti-inflammatory properties of ω-3 fatty acids might also be due to the suppression of IL-1β (61). Arginine is the most plentiful amino acid found in almonds (62, 63). It has been shown that increased consumption of arginine has an inverse association with CRP concentrations (59). Furthermore, almonds are rich in certain constituents, including α-tocopherol and phytonutrients (64–67), that might be modifiers of some inflammatory factors, but more studies are needed to entirely understand their role.
This is the most comprehensive meta-analysis to investigate the effects of almond consumption on inflammatory markers. Subgroup analyses were also performed for more accurate interpretation. However, several limitations in our study should also be acknowledged. The effects might be underestimated due to self-reporting of the participants’ compliance. Despite observing no significant heterogeneity in the overall effect sizes, the included trials had different methodological approaches. For example, some studies used fixed doses of almonds whereas others considered the amount of almond intake as a percentage of total energy intake. Also, eligible trials had different control strata, which might be a concern in case of heterogeneity. Also, the increased risk of type I error from analyzing several outcomes is another limitation of our study. Furthermore, our meta-analysis contained some trials with a small sample size, which could be a reason for nonsignificant findings as well as insufficient statistical power. Therefore, more high-quality studies with larger sample sizes are needed to overcome these limitations.
In conclusion, we found that almond consumption significantly reduces serum concentrations of CRP and IL-6, whereas no beneficial effect was seen for TNF-α, ICAM-1, and VCAM-1. More clinical trials are required to confirm our findings and to recommend almond consumption as a part of a healthy diet.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—SF: contributed to the literature search, screening, data extraction, and drafting of the manuscript; KL: contributed to the literature search, data extraction, statistical analyses, and drafting of the manuscript; ED: contributed to the literature search, screening, statistical analyses, interpretation of data, and drafting of the manuscript; LA: contributed to the conception, design, statistical analyses, interpretation of the data, and drafting of the manuscript, and supervised the study; and all authors: read and approved the final manuscript.
Notes
This study was funded by Tehran University of Medical Sciences, Tehran, Iran (project code: 99-3-212-51296).
Author disclosures: The authors report no conflicts of interest.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: CRP, C-reactive protein; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; ICAM-1, intercellular adhesion molecule-1; RCT, randomized clinical trial; VCAM-1, vascular cell adhesion molecule-1; WMD, weighted mean difference.
Contributor Information
Shahin Fatahi, Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran.
Elnaz Daneshzad, Non-Communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran.
Keyhan Lotfi, Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran.
Leila Azadbakht, Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran; Diabetes Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran; Department of Community Nutrition, School of Nutrition and Food Science, Isfahan University of Medical Sciences, Isfahan, Iran.
References
- 1. Singh N, Baby D, Rajguru JP, Patil PB, Thakkannavar SS, Pujari VB. Inflammation and cancer. Ann Afr Med. 2019;18(3):121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Golia E, Limongelli G, Natale F, Fimiani F, Maddaloni V, Pariggiano I, Bianchi R, Crisci M, D'Acierno L, Giordano Ret al. . Inflammation and cardiovascular disease: from pathogenesis to therapeutic target. Curr Atheroscler Rep. 2014;16(9):435. [DOI] [PubMed] [Google Scholar]
- 3. Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11(2):98–107. [DOI] [PubMed] [Google Scholar]
- 4. Lee JK, Bettencourt R, Brenner D, Le T-A, Barrett-Connor E, Loomba R. Association between serum interleukin-6 concentrations and mortality in older adults: the Rancho Bernardo study. PLoS One. 2012;7(4):e34218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–7. [DOI] [PubMed] [Google Scholar]
- 6. Neale EP, Tapsell LC, Guan V, Batterham MJ. The effect of nut consumption on markers of inflammation and endothelial function: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2017;7(11):e016863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ruiz-Núñez B, Pruimboom L, Dijck-Brouwer DJ, Muskiet FA. Lifestyle and nutritional imbalances associated with Western diseases: causes and consequences of chronic systemic low-grade inflammation in an evolutionary context. J Nutr Biochem. 2013;24(7):1183–201. [DOI] [PubMed] [Google Scholar]
- 8. Schwingshackl L, Hoffmann G. Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis. 2014;24(9):929–39. [DOI] [PubMed] [Google Scholar]
- 9. Soltani S, Chitsazi MJ, Salehi-Abargouei A. The effect of Dietary Approaches to Stop Hypertension (DASH) on serum inflammatory markers: a systematic review and meta-analysis of randomized trials. Clin Nutr. 2018;37(2):542–50. [DOI] [PubMed] [Google Scholar]
- 10. Becerra-Tomás N, Paz-Graniel I, Kendall CWC, Kahleova H, Rahelić D, Sievenpiper JL, Salas-Salvadó J. Nut consumption and incidence of cardiovascular diseases and cardiovascular disease mortality: a meta-analysis of prospective cohort studies. Nutr Rev. 2019;77(10):691–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Naghshi S, Sadeghian M, Nasiri M, Mobarak S, Asadi M, Sadeghi O. Association of total nut, tree nut, peanut, and peanut butter consumption with cancer incidence and mortality: a comprehensive systematic review and dose-response meta-analysis of observational studies. Adv Nutr. 2021;12(3):793–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tindall AM, Johnston EA, Kris-Etherton PM, Petersen KS. The effect of nuts on markers of glycemic control: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2019;109(2):297–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Del Gobbo LC, Falk MC, Feldman R, Lewis K, Mozaffarian D. Effects of tree nuts on blood lipids, apolipoproteins, and blood pressure: systematic review, meta-analysis, and dose-response of 61 controlled intervention trials. Am J Clin Nutr. 2015;102(6):1347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kalita S, Khandelwal S, Madan J, Pandya H, Sesikeran B, Krishnaswamy K. Almonds and cardiovascular health: a review. Nutrients. 2018;10(4):468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu M, Dudley SC. Magnesium, oxidative stress, inflammation, and cardiovascular disease. Antioxidants. 2020;9(10):907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sweazea KL, Johnston CS, Ricklefs KD, Petersen KN. Almond supplementation in the absence of dietary advice significantly reduces C-reactive protein in subjects with type 2 diabetes. J Funct Foods. 2014;10:252–9. [Google Scholar]
- 17. Rajaram S, Connell KM, Sabaté J. Effect of almond-enriched high-monounsaturated fat diet on selected markers of inflammation: a randomised, controlled, crossover study. Br J Nutr. 2010;103(6):907–12. [DOI] [PubMed] [Google Scholar]
- 18. Rakic JM, Tanprasertsuk J, Scott TM, Rasmussen HM, Mohn ES, Chen C-YO, Johnson EJ. Effects of daily almond consumption for six months on cognitive measures in healthy middle-aged to older adults: a randomized control trial. Nutr Neurosci. [Internet]2021:1–11.. doi:10.1080/1028415X.2020.1868805. [DOI] [PubMed] [Google Scholar]
- 19. Lee-Bravatti MA, Wang J, Avendano EE, King L, Johnson EJ, Raman G. Almond consumption and risk factors for cardiovascular disease: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2019;10(6):1076–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xiao Y, Xia J, Ke Y, Cheng J, Yuan J, Wu S, Lv Z, Huang S, Kim JH, Wong SY-S. Effects of nut consumption on selected inflammatory markers: a systematic review and meta-analysis of randomized controlled trials. Nutrition. 2018;54:129–43. [DOI] [PubMed] [Google Scholar]
- 21. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84. [DOI] [PubMed] [Google Scholar]
- 22. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:14898. [DOI] [PubMed] [Google Scholar]
- 23. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Method. 2005;5(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jenkins DJ, Kendall CW, Marchie A, Parker TL, Connelly PW, Qian W, Haight JS, Faulkner D, Vidgen E, Lapsley KG. Dose response of almonds on coronary heart disease risk factors: blood lipids, oxidized low-density lipoproteins, lipoprotein(a), homocysteine, and pulmonary nitric oxide: a randomized, controlled, crossover trial. Circulation. 2002;106(11):1327–32. [DOI] [PubMed] [Google Scholar]
- 25. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions: Hoboken (NJ): John Wiley & Sons; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saboori S, Falahi E, Rad EY, Asbaghi O, Khosroshahi MZ. Effects of ginseng on C-reactive protein level: a systematic review and meta-analysis of clinical trials. Complement Ther Med. 2019;45:98–103. [DOI] [PubMed] [Google Scholar]
- 27. Mohammadi-Sartang M, Mazloom Z, Sherafatmanesh S, Ghorbani M, Firoozi D. Effects of supplementation with quercetin on plasma C-reactive protein concentrations: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2017;71(9):1033–9. [DOI] [PubMed] [Google Scholar]
- 28. Saboori S, Shab-Bidar S, Speakman J, Rad EY, Djafarian K. Effect of vitamin E supplementation on serum C-reactive protein level: a meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2015;69(8):867–73. [DOI] [PubMed] [Google Scholar]
- 29. Su H, Liu R, Chang M, Huang J, Jin Q, Wang X. Effect of dietary alpha-linolenic acid on blood inflammatory markers: a systematic review and meta-analysis of randomized controlled trials. Eur J Nutr. 2018;57(3):877–91. [DOI] [PubMed] [Google Scholar]
- 30. Gulati S, Misra A, Pandey RM. Effect of almond supplementation on glycemia and cardiovascular risk factors in Asian Indians in north India with type 2 diabetes mellitus: a 24-week study. Metab Syndr Relat Disord. 2017;15(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fonollá J, Maldonado-Lobón JA, Luque R, Rodríguez C, Banuelos O, López-Larramendi JL, Olivares M, Blanco-Rojo R. Effects of a combination of extracts from olive fruit and almonds skin on oxidative and inflammation markers in hypercholesterolemic subjects: a randomized controlled trial. J Med Food. 2021;24(5):479–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schincaglia RM, Cuppari L, Neri HF, Cintra DE, Sant'Ana MR, Mota JF. Effects of baru almond oil (Dipteryx alata vog.) supplementation on body composition, inflammation, oxidative stress, lipid profile, and plasma fatty acids of hemodialysis patients: a randomized, double-blind, placebo-controlled clinical trial. Complement Ther Med. 2020;52:102479. [DOI] [PubMed] [Google Scholar]
- 33. Lee YJ, Nam GE, Seo JA, Yoon T, Seo I, Lee JH, Im D, Bahn KN, Jeong SA, Kang TSet al. . Nut consumption has favorable effects on lipid profiles of Korean women with metabolic syndrome. Nutr Res. 2014;34(9):814–20. [DOI] [PubMed] [Google Scholar]
- 34. Casas-Agustench P, López-Uriarte P, Bulló M, Ros E, Cabré-Vila JJ, Salas-Salvadó J. Effects of one serving of mixed nuts on serum lipids, insulin resistance and inflammatory markers in patients with the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2011;21(2):126–35. [DOI] [PubMed] [Google Scholar]
- 35. Ghanavati M, Hosseinabadi SM, Parsa SA, Safi M, Emamat H, Nasrollahzadeh J. Effect of a nut-enriched low-calorie diet on body weight and selected markers of inflammation in overweight and obese stable coronary artery disease patients: a randomized controlled study. Eur J Clin Nutr. 2021;75(7):1099–108. [DOI] [PubMed] [Google Scholar]
- 36. Berryman CE, West SG, Fleming JA, Bordi PL, Kris-Etherton PM. Effects of daily almond consumption on cardiometabolic risk and abdominal adiposity in healthy adults with elevated LDL-cholesterol: a randomized controlled trial. J Am Heart Assoc. 2015;4(1):e000993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chen CO, Holbrook M, Duess M-A, Dohadwala MM, Hamburg NM, Asztalos BF, Milbury PE, Blumberg JB, Vita JA. Effect of almond consumption on vascular function in patients with coronary artery disease: a randomized, controlled, cross-over trial. Nutr J. 2015;14(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kalgaonkar S, Almario R, Gurusinghe D, Garamendi E, Buchan W, Kim K, Karakas SE. Differential effects of walnuts vs almonds on improving metabolic and endocrine parameters in PCOS. Eur J Clin Nutr. 2011;65(3):386–93. [DOI] [PubMed] [Google Scholar]
- 39. Kurlandsky SB, Stote KS. Cardioprotective effects of chocolate and almond consumption in healthy women. Nutr Res. 2006;26(10):509–16. [Google Scholar]
- 40. Lee Y, Berryman CE, West SG, Chen CYO, Blumberg JB, Lapsley KG, Preston AG, Fleming JA, Kris-Etherton PM. Effects of dark chocolate and almonds on cardiovascular risk factors in overweight and obese individuals: a randomized controlled-feeding trial. J Am Heart Assoc. 2017;6(12):e005162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Palacios OM, Maki KC, Xiao D, Wilcox ML, Dicklin MR, Kramer M, Trivedi R, Burton-Freeman B, Edirisinghe I. Effects of consuming almonds on insulin sensitivity and other cardiometabolic health markers in adults with prediabetes. J Am Coll Nutr. 2020;39(5):397–406. [DOI] [PubMed] [Google Scholar]
- 42. Chen C-M, Liu J-F, Li S-C, Huang C-L, Hsirh A-T, Weng S-F, Chang M-L, Li H-T, Mohn E, Chen CO. Almonds ameliorate glycemic control in Chinese patients with better controlled type 2 diabetes: a randomized, crossover, controlled feeding trial. Nutr Metab. 2017;14(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liu J-F, Liu Y-H, Chen C-M, Chang W-H, Chen CO. The effect of almonds on inflammation and oxidative stress in Chinese patients with type 2 diabetes mellitus: a randomized crossover controlled feeding trial. Eur J Nutr. 2013;52(3):927–35. [DOI] [PubMed] [Google Scholar]
- 44. Bowen J, Luscombe-Marsh ND, Stonehouse W, Tran C, Rogers GB, Johnson N, Thompson CH, Brinkworth GD. Effects of almond consumption on metabolic function and liver fat in overweight and obese adults with elevated fasting blood glucose: a randomised controlled trial. Clin Nutr ESPEN. 2019;30:10–8. [DOI] [PubMed] [Google Scholar]
- 45. Coates AM, Morgillo S, Yandell C, Scholey A, Buckley JD, Dyer KA, Hill AM. Effect of a 12-week almond-enriched diet on biomarkers of cognitive performance, mood, and cardiometabolic health in older overweight adults. Nutrients. 2020;12(4):1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Damasceno N, Pérez-Heras A, Serra M, Cofán M, Sala-Vila A, Salas-Salvadó J, Ros E. Crossover study of diets enriched with virgin olive oil, walnuts or almonds. Effects on lipids and other cardiovascular risk markers. Nutr Metab Cardiovasc Dis. 2011;21:S14–20. [DOI] [PubMed] [Google Scholar]
- 47. Jung H, Chen C-YO, Blumberg JB, Kwak H-K. The effect of almonds on vitamin E status and cardiovascular risk factors in Korean adults: a randomized clinical trial. Eur J Nutr. 2018;57(6):2069–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liu Y, Hwang H-J, Ryu H, Lee Y-S, Kim H-S, Park H. The effects of daily intake timing of almond on the body composition and blood lipid profile of healthy adults. Nutr Res Pract. 2017;11(6):479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hou Y-Y, Ojo O, Wang L-L, Wang Q, Jiang Q, Shao X-Y, Wang X-H. A randomized controlled trial to compare the effect of peanuts and almonds on the cardio-metabolic and inflammatory parameters in patients with type 2 diabetes mellitus. Nutrients. 2018;10(11):1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Panagiotakos DB, Pitsavos C, Yannakoulia M, Chrysohoou C, Stefanadis C. The implication of obesity and central fat on markers of chronic inflammation: the ATTICA study. Atherosclerosis. 2005;183(2):308–15. [DOI] [PubMed] [Google Scholar]
- 51. Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R. Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation. 2005;111(11):1448–54. [DOI] [PubMed] [Google Scholar]
- 52. McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67(3):257–62. [DOI] [PubMed] [Google Scholar]
- 53. Banach J, Żekanowska E, Bujak R, Gilewski W, Błażejewski J, Karasek D, Balak W, Pietrzak J, Sinkiewicz W. Short-term alcohol consumption may have detrimental effect on fibrinolysis and endothelial function: preliminary report of prospective randomised study. Kardiol Pol. 2013;71(11):1161–7. [DOI] [PubMed] [Google Scholar]
- 54. Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55(2):648–58. [DOI] [PubMed] [Google Scholar]
- 55. Asbaghi O, Hadi A, Campbell MS, Venkatakrishnan K, Ghaedi E. Effects of pistachios on anthropometric indices, inflammatory markers, endothelial function, and blood pressure in adults: a systematic review and meta-analysis of randomized controlled trials. Br J Nutr. 2021;125(5):718–29. [DOI] [PubMed] [Google Scholar]
- 56. Asbaghi O, Moodi V, Hadi A, Eslampour E, Shirinbakhshmasoleh M, Ghaedi E, Miraghajani M. The effect of almond intake on lipid profile: a systematic review and meta-analysis of randomized controlled trials. Food Funct. 2021;12(5):1882–96. [DOI] [PubMed] [Google Scholar]
- 57. Eslampour E, Asbaghi O, Hadi A, Abedi S, Ghaedi E, Lazaridi AV, Miraghajani M. The effect of almond intake on blood pressure: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2020;50:102399. [DOI] [PubMed] [Google Scholar]
- 58. Song Y, Li TY, van Dam RM, Manson JE, Hu FB. Magnesium intake and plasma concentrations of markers of systemic inflammation and endothelial dysfunction in women. Am J Clin Nutr. 2007;85(4):1068–74. [DOI] [PubMed] [Google Scholar]
- 59. Wells BJ, Mainous AG III, Everett CJ. Association between dietary arginine and C-reactive protein. Nutrition. 2005;21(2):125–30. [DOI] [PubMed] [Google Scholar]
- 60. Salas-Salvadó J, Casas-Agustench P, Murphy MM, López-Uriarte P, Bulló M. The effect of nuts on inflammation. Asia Pac J Clin Nutr. 2008;17(Suppl 1):333–6. [PubMed] [Google Scholar]
- 61. Simopoulos AP. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002;21(6):495–505. [DOI] [PubMed] [Google Scholar]
- 62. Esteban Alvarez RM. Estudio comparativo de la calidad nutritiva de variedades de almendra del SE y NE español. Madrid: Instituto Nacional de Investigaciones Agrarias; 1984. [Google Scholar]
- 63. Saura Calixto F, Cañellas Mut J, Soler L. La almendra: composición, variedades, desarrollo y maduración. Madrid: Instituto Nacional de Investigaciones Agrarias; 1988. [Google Scholar]
- 64. Blomhoff R, Carlsen MH, Andersen LF, Jacobs DR. Health benefits of nuts: potential role of antioxidants. Br J Nutr. 2006;96(S2):S52–60. [DOI] [PubMed] [Google Scholar]
- 65. Huynh NN, Chin-Dusting J. Amino acids, arginase and nitric oxide in vascular health. Clin Exp Pharmacol Physiol. 2006;33(1–2):1–8. [DOI] [PubMed] [Google Scholar]
- 66. Jambazian PR, Haddad E, Rajaram S, Tanzman J, Sabaté J. Almonds in the diet simultaneously improve plasma α-tocopherol concentrations and reduce plasma lipids. J Am Diet Assoc. 2005;105(3):449–54. [DOI] [PubMed] [Google Scholar]
- 67. Ros E. Nuts: consumption, composition, health benefits and safety. CAB Rev. 2008;3(070). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.