Abstract
Background
We examined the association of non-cigarette tobacco use on chronic obstructive pulmonary disease (COPD) risk in the Population Assessment of Tobacco and Health (PATH) Study.
Methods
There were 13,752 participants ≥ 40 years with Wave 1 (W1) data for prevalence analyses, including 6945 adults without COPD for incidence analyses; W1–5 (2013–2019) data were analyzed. W1 tobacco use was modeled as 12 mutually-exclusive categories of past 30-day (P30D) single and polyuse, with two reference categories (current exclusive cigarette and never tobacco). Prevalence and incidence ratios of self-reported physician-diagnosed COPD were estimated using weighted multivariable Poisson regression.
Results
W1 mean (SE) age was 58.1(0.1) years; mean cigarette pack-years was similar for all categories involving cigarettes and exclusive use of e-cigarettes (all > 20), greater than exclusive cigar users (< 10); and COPD prevalence was 7.7%. Compared to P30D cigarette use, never tobacco, former tobacco, and cigar use were associated with lower COPD prevalence (RR = 0.33, (95% confidence interval—CI) [0.26, 0.42]; RR = 0.57, CI [0.47, 0.70]; RR = 0.46, CI [0.28, 0.76], respectively); compared to never tobacco use, all categories except cigar and smokeless tobacco use were associated with higher COPD prevalence (RR former = 1.72, CI [1.33, 2.23]; RR cigarette = 3.00, CI [2.37, 3.80]; RR e-cigarette = 2.22, CI [1.44, 3.42]; RR cigarette + e-cigarette = 3.10, CI [2.39, 4.02]; RR polycombusted = 3.37, CI [2.44, 4.65]; RR polycombusted plus noncombusted = 2.75, CI]1.99, 3.81]). COPD incidence from W2-5 was 5.8%. Never and former tobacco users had lower COPD risk compared to current cigarette smokers (RR = 0.52, CI [0.35, 0.77]; RR = 0.47, CI [0.32, 0.70], respectively). Compared to never use, cigarette, smokeless, cigarette plus e-cigarette, and polycombusted tobacco use were associated with higher COPD incidence (RR = 1.92, CI [1.29, 2.86]; RR = 2.08, CI [1.07, 4.03]; RR = 1.99, CI [1.29, 3.07]; RR = 2.59, CI [1.60, 4.21], respectively); exclusive use of e-cigarettes was not (RR = 1.36, CI [0.55, 3.39]).
Conclusions
E-cigarettes and all use categories involving cigarettes were associated with higher COPD prevalence compared to never use, reflecting, in part, the high burden of cigarette exposure in these groups. Cigarette—but not exclusive e-cigarette—use was also strongly associated with higher COPD incidence. Compared to cigarette use, only quitting tobacco was protective against COPD development.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12931-022-02197-1.
Keywords: Cigarette, COPD, E-cigarette, Epidemiology, Prevention, Respiratory disease, Smoking-related lung disease, Tobacco
Background
Chronic obstructive pulmonary disease (COPD) is a chronic, progressive respiratory disease associated with inhalational exposure to noxious gases and particles [1]. Cigarette smoking has long been linked to development of COPD [2], but less is known about the impact of other tobacco products, including e-cigarettes, on COPD epidemiology. Increased use of e-cigarette products among smokers who may be seeking to improve health outcomes or quit cigarette smoking has prompted investigation of their relationship with respiratory disease [3]. Given that cigarette smoking is a leading risk factor for COPD development, and that e-cigarette products have been suggested as a lower risk substitute [4, 5], understanding the impact of use of these products on COPD outcomes is a public health priority.
Studies that have examined the relationship between use of e-cigarette products and COPD outcomes show mixed results. A small cohort study of smokers with COPD demonstrated improvement in outcomes among those who switched from cigarette to e-cigarette use [6, 7]. Analyses of large United States (US) surveys suggest that e-cigarette use was associated with greater COPD prevalence among current, former, and never cigarette smokers [8–11]. Specifically, recent analyses of the Population Assessment of Tobacco and Health (PATH) Study found associations between e-cigarette use and COPD [8, 12–14]. While these prior studies have been helpful in identifying trends in tobacco use behavior, many included a large proportion of adults less than 40 years old, an age when COPD is rare [1], and failed to account for important confounding variables including pack-years of cigarette smoking. Similarly, prior work suggesting a relationship between cigar use and COPD has been limited by incomplete assessment of tobacco use history [15]. As such, additional studies examining the impact of tobacco product use over time are needed to clarify these relationships.
COPD is a progressive, incurable disease and a leading cause of morbidity and mortality worldwide that has clearly been associated with cigarette smoking. Understanding how other tobacco products may relate to COPD onset is important for communicating accurate risk information to smokers. The goal of this study, using PATH Study data, is to determine whether commonly used tobacco products, including e-cigarettes, are associated with prevalence and incidence of COPD in US adults aged 40 years and older.
Methods
Study design, setting, and participants
The PATH Study is an ongoing, nationally representative, longitudinal cohort study sponsored by the National Institute on Drug Abuse, National Institutes of Health and the Food and Drug Administration’s Center for Tobacco Products. The study collects self-reported information on tobacco-use patterns, health behaviors and medical history. Complete PATH Study design methods have previously been published in detail [16–18]. All adult respondents provided informed consent. The study was conducted by Westat and approved by the Westat Institutional Review Board.
Primary outcomes
At Wave 1 (W1) of the PATH Study participants were asked: “Has a doctor, nurse or other health professional EVER told you that you had any of the following lung or respiratory conditions? Choose all that apply: COPD, chronic bronchitis, emphysema, asthma, some other lung or respiratory condition, none of the above, don’t know, refused.” At subsequent waves, participants are asked about respiratory disease diagnoses over the past 12 months. For these analyses, COPD, chronic bronchitis, and emphysema diagnoses are combined to create one COPD measure and are referred to as COPD moving forward, similar to prior COPD prevalence studies using National Health and Nutrition Examination Survey (NHANES) data [19, 20], with which our prevalence estimates were compared. COPD at baseline (W1—2013–2014) and new COPD at follow-up (W2—2014–2015; W3—2015–2016; W4—2016–2017; W5—2018–2019) were assessed using a combination of the two questions above. Individuals with history of “some other lung or respiratory condition” were excluded.
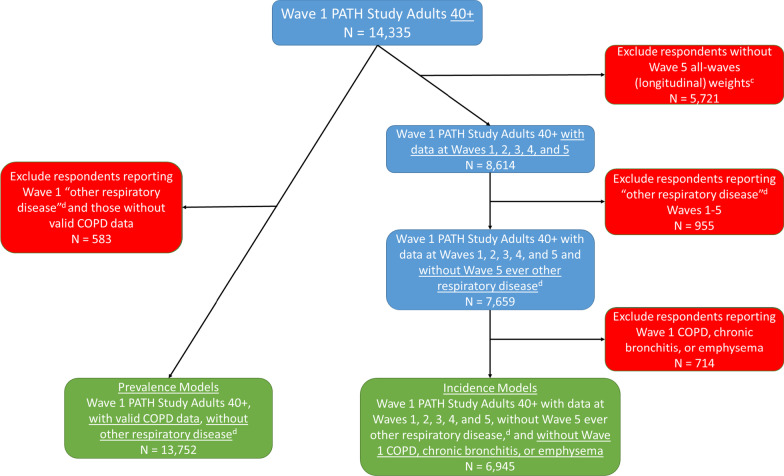
Given that COPD diagnoses are rarely made before age 40, and consistent with national COPD cohorts [20–22], we limited our sample to adults aged 40 years and over at W1. For W1 prevalence estimates, all W1 adults with valid COPD data aged ≥ 40 years were analyzed (N = 13,752); incidence analyses included adults aged ≥ 40 years without a diagnosis of COPD at W1, and for whom data at all five study waves are available (N = 6945) (Fig. 1). Missing data on age, gender, race, Hispanic ethnicity, and adult education were imputed as described in the PATH Study Restricted Use Files User Guide at https://doi.org/10.3886/Series606. The current study uses the W1–5 Adult Restricted Use Files [23].
Fig. 1.
Study flow aThis figure illustrates the sample determination from the Population Assessment of Tobacco and Health Study for the prevalence and incidence models (Tables 2 and 3) for COPD bCOPD Chronic Obstructive Pulmonary Disease, defined as self-report of emphysema, chronic bronchitis, or COPD; prevalence and incidence models. cWeights adjust for non-response. dOther non-asthma or COPD respiratory diseases
Exposures of interest
Participants reported lifetime and past 30-day use of combusted products (cigarettes, traditional cigars, cigarillos, filtered cigars, pipe tobacco, and hookah) and noncombusted products (snus pouches, other smokeless tobacco [loose snus, moist snuff, dip, spit, or chewing tobacco], and e-cigarettes) at W1.
Twelve mutually exclusive categories defined all past and current tobacco use possibilities (never or former experimental [e.g., lifetime use of < 100 cigarettes; or never used other products fairly regularly) users—hereafter referred to as never]; former established [e.g., lifetime use of more than 100 cigarettes; or ever used other products fairly regularly, and who haven’t used any tobacco products in the past 30 days—hereafter referred to as former]; exclusive past 30-day use of products: cigarettes, e-cigarettes, cigars [traditional, cigarillo, and filtered cigars], smokeless [smokeless tobacco and snus], hookah, pipe; past 30-day use of combinations: cigarettes and e-cigarettes; polycombusted; polycombusted and noncombusted; and e-cigarettes and smokeless).
Covariates
As described in Table 1, covariates were derived from W1 data and include variables that could be associated both with tobacco exposure and COPD. Sociodemographic variables included age, sex, race/ethnicity, education, and urbanicity (urban segments have a minimum population density of at least 2500 people based on US Census blocks and are non-urban otherwise). Other W1 smoke-related exposures included pack-years of cigarette smoking [24], past-month secondhand smoke exposure [25], and marijuana use [26]. Two medical history variables were included: ever asthma diagnosis and a disease comorbidity index score used in prior studies to capture important contributors to morbidity in COPD patients (range 0–9) [27]. For each analysis, models were run with three different levels of adjustment: (1) unadjusted; (2) adjusted for cigarette pack-years; and (3) fully adjusted models adding all other covariates.
Table 1.
Characteristics of Wave 1 participants with valid data on COPDa status (N = 13,752)
| Sociodemographics, Tobacco Use, and Medical History | Adults age 40 and above (N = 13,752) | Adults with self-reported doctor or other health professional diagnosis of COPDa (N = 1506) |
Adults without self-reported doctor or other health professional diagnosis of COPDa (N = 12,246) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Nb | Weighted %/Mean | SE | Nb | Weighted %/Mean | SE | Nb | Weighted %/Mean | SE | |
| Sociodemographics | |||||||||
| Age in years, mean | 13,752 | 58.1 | 0.1 | 1506 | 63.1 | 0.5 | 12,246 | 57.7 | 0.1 |
| Sex, N (%) male | 6943 | 47.2% | 0.2 | 627 | 41.2% | 1.7 | 6316 | 47.7% | 0.3 |
| Race, N (%) non-Hispanic white | 9306 | 71.4% | 0.3 | 1128 | 79.6% | 1.2 | 8178 | 70.7% | 0.4 |
| Hispanic ethnicity, N (%) | 1629 | 11.4% | 0.3 | 98 | 6.9% | 0.8 | 1531 | 11.8% | 0.3 |
| Less than high school education, N (%) | 2963 | 17.4% | 0.1 | 492 | 31.1% | 1.8 | 2471 | 16.3% | 0.2 |
| Live in urban area, N (%) | 10,157 | 75.5% | 1.8 | 1029 | 69.3% | 2.8 | 9128 | 76.0% | 1.7 |
| Tobacco use | |||||||||
| Ever (100+) cigarette smoker, N (%) | 7952 | 41.1% | 0.7 | 1207 | 70.2% | 1.7 | 6745 | 38.7% | 0.7 |
| Pack-yearsc, mean | 10,861 | 14.2 | 0.3 | 1394 | 29.4 | 0.8 | 9467 | 12.6 | 0.3 |
| Any past 30 day tobacco use categories | |||||||||
| P30D cigarette use, N (%) | 5983 | 18.3% | 0.3 | 1043 | 40.5% | 1.4 | 4940 | 16.5% | 0.3 |
| P30D cigar use, N (%) | 1265 | 4.4% | 0.1 | 168 | 7.1% | 0.6 | 1097 | 4.2% | 0.1 |
| P30D traditional cigar use, N (%) | 756 | 2.6% | 0.1 | 78 | 3.0% | 0.3 | 678 | 2.5% | 0.1 |
| P30D cigarillo use, N (%) | 586 | 2.0% | 0.1 | 74 | 3.1% | 0.4 | 512 | 1.9% | 0.1 |
| P30 filtered cigar use, N (%) | 403 | 1.3% | 0.1 | 94 | 3.9% | 0.5 | 309 | 1.1% | 0.1 |
| P30D hookah use, N (%) | 95 | 0.3% | 0.0 | 14 | 0.5% | 0.1 | 81 | 0.3% | 0.0 |
| P30D e-cigarette use, N (%) | 1393 | 4.1% | 0.1 | 265 | 9.8% | 0.7 | 1128 | 3.7% | 0.1 |
| P30D smokeless/snus use, N (%) | 746 | 2.4% | 0.1 | 49 | 2.1% | 0.4 | 697 | 2.5% | 0.1 |
| Mutually exclusive P30D tobacco use categoriesd | |||||||||
| Never use (Never or former experimental tobacco) | 3817 | 51.7% | 0.7 | 120 | 21.4% | 1.9 | 3697 | 54.2% | 0.7 |
| Former tobacco use | 2173 | 25.2% | 0.6 | 225 | 33.5% | 1.9 | 1948 | 24.5% | 0.6 |
| Exclusive cigarette use | 3773 | 12.5% | 0.3 | 634 | 27.4% | 1.3 | 3139 | 11.3% | 0.3 |
| Exclusive e-cigarette use | 198 | 0.6% | 0.0 | 26 | 1.0% | 0.2 | 172 | 0.6% | 0.0 |
| Exclusive cigar use | 391 | 1.6% | 0.1 | 18 | 1.0% | 0.2 | 373 | 1.7% | 0.1 |
| Exclusive smokeless/snus use | 482 | 1.7% | 0.1 | 27 | 1.3% | 0.4 | 455 | 1.8% | 0.1 |
| Exclusive P30D cigarette and e-cigarette use | 852 | 2.7% | 0.1 | 166 | 6.7% | 0.6 | 686 | 2.4% | 0.1 |
| Polycombusted tobacco use | 619 | 2.0% | 0.1 | 113 | 4.6% | 0.5 | 506 | 1.8% | 0.1 |
| Polycombusted and noncombusted use | 461 | 1.5% | 0.1 | 70 | 3.0% | 0.3 | 391 | 1.3% | 0.1 |
| Medical history (self-reported) | |||||||||
| Total COPDa diagnosis, N (%) | 1506 | 7.7% | 0.3 | 1506 | 100.0% | N/A | N/A | N/A | N/A |
| COPDe diagnosis, N (%) | 939 | 4.6% | 0.2 | 939 | 60.1% | 1.8 | N/A | N/A | N/A |
| Chronic bronchitis diagnosis, N (%) | 762 | 3.9% | 0.2 | 762 | 50.6% | 1.8 | N/A | N/A | N/A |
| Emphysema diagnosis, N (%) | 456 | 2.0% | 0.1 | 456 | 26.5% | 1.4 | N/A | N/A | N/A |
| BMI, kg/m2, mean | 13,465 | 28.4 | 0.1 | 1477 | 29.7 | 0.3 | 11,988 | 28.3 | 0.1 |
| Comorbidity index,f mean | 13,383 | 1.5 | 0.0 | 1466 | 2.6 | 0.1 | 11,917 | 1.4 | 0.0 |
aCOPD: Chronic Obstructive Pulmonary Disease, defined as self-report of emphysema, chronic bronchitis, or COPD
bUnweighted
cIn this table, mean pack-years is only calculated among ever users of cigarettes
dData are not presented for exclusive hookah, exclusive pipe, and dual e-cigarette + smokeless/snus users due to small sample size. Never tobacco user category includes former experimental (e.g., lifetime use of < 100 cigarettes or never used other products fairly regularly) users; former established user category includes all established users (e.g., lifetime use of more than 100 cigarettes or ever used other products fairly regularly) who did not use any tobacco products in the past 30 days
eCOPD only, not including emphysema or chronic bronchitis
fComorbidity index (range 0–9) is made up of self-reported ever-diagnosis of coronary heart disease, diabetes, congestive heart failure, stroke, osteoarthritis, hypertension, high cholesterol, stomach ulcers, and Wave 1 obesity based on BMI ≥ 30
Statistical analysis
We examined the associations between W1 COPD diagnosis and covariates using weighted comparisons of means or proportions, as appropriate. We estimated the weighted prevalence and risk ratio for the association of COPD prevalence and incidence, respectively (hereafter referred to as risk ratio [RR]), with tobacco exposure categories while adjusting for covariates using multivariable Poisson regression. To assess the independent risk of tobacco products and their RR compared to cigarettes, two separate analyses were run, each with a different reference category: (1) never tobacco use and (2) current exclusive cigarette smoking. The prevalence analyses were weighted using the W1 full-sample and replicate weights. The incidence analyses were weighted using the W5 longitudinal (all-waves) full-sample and replicate weights. Standard errors were derived using the Balanced Repeated Replication method [28] with Fay’s adjustment set to 0.3 to increase estimate stability [29]. Pack-years of cigarette smoking (non-zero values) and secondhand smoke exposure variables were Winsorized at the 95th and 99th (100 h) percentiles, respectively, to limit the influence of outliers [27]. Participants who were missing COPD diagnosis data, tobacco product use data, or covariate data were omitted from the analyses. All analyses were conducted using Stata survey data procedures, version 17.0 [30].
Sensitivity analyses
In a sensitivity analysis, individuals who had contributed to at least one follow-up wave after W1 were included to estimate the association of incident COPD with tobacco exposure categories while adjusting for covariates using Cox’s multivariable proportional hazards model. In this case, the dependent variable is the discrete time indicating the first wave at which COPD was diagnosed and otherwise censored after the last wave they participated in. In addition, separate sensitivity analyses (1) included all adults 18 and older, and (2) excluded adults with baseline (W1) asthma.
Results
At W1, among adults aged ≥ 40 years with valid COPD data (unweighted N = 13,752), 47.2% were male, 71.4% were white, and 11.4% were of Hispanic ethnicity; 17.4% completed less than high school education, and 75.5% lived in an urban area. Mean body mass index (BMI) was 28.4, and mean comorbidity index score was 1.5. Approximately 41.1% had ever smoked 100 or more cigarettes and among those, there was a mean pack-years of 14.3. In the past 30 days, 18.3% used cigarettes, 4.4% used cigars (the majority of which were traditional), 0.3% used hookah, 4.1% used e-cigarettes, and 2.4% used smokeless tobacco (Table 1).
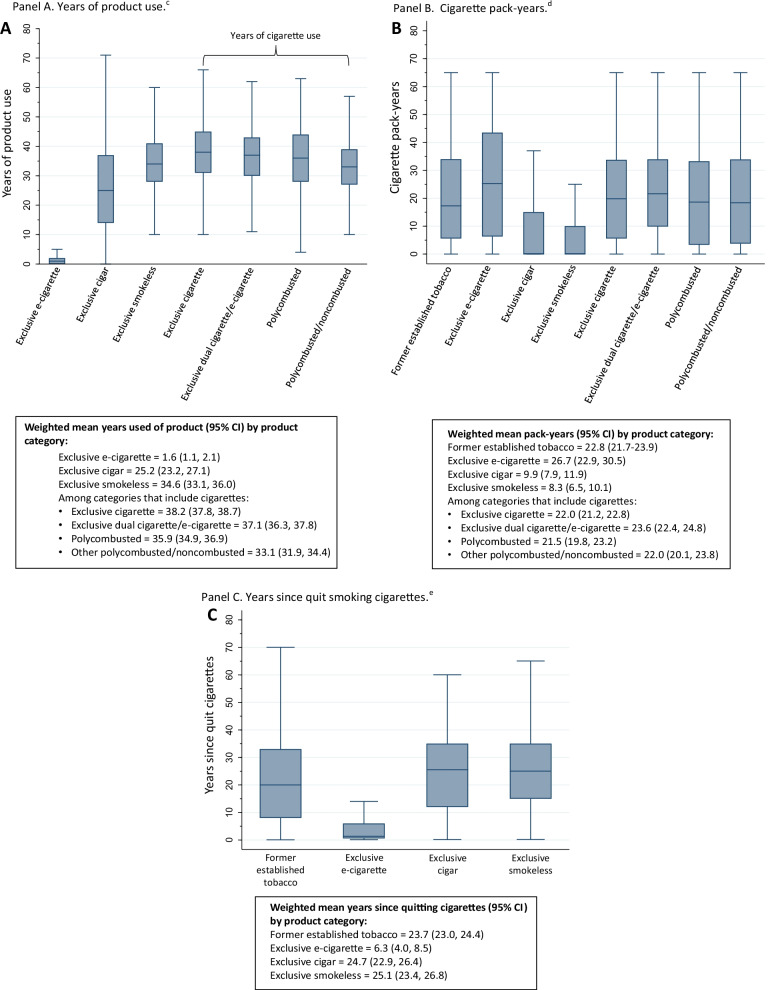
Cigarette smoking history among select tobacco use categories
Mean (95% confidence interval—CI) years of product use was greatest for exclusive cigarette users (38.2, CI [37.8, 38.7]) (Fig. 2A). Mean (95% CI) number of pack-years of cigarette smoking was highest in exclusive e-cigarette users (26.7, CI [22.9, 30.5]), dual users of e-cigarettes and cigarettes (23.6, CI [22.4, 24.8]), former tobacco users (22.8, CI [21.7, 23.9]), exclusive cigarette users (22.0, CI [21.2, 22.8]), polycombusted and noncombusted users (22.0, CI [20.1, 23.9]), and polycombusted users (21.5, CI [19.8, 23.2]) (Fig. 2B). Exclusive cigar and smokeless tobacco users had on average > 20 years since quitting cigarettes; exclusive e-cigarette users quit cigarette smoking 6.3 (4.0, 8.5) years ago (Fig. 2C).
Fig. 2.
Unweighted distribution for years of product use (A), cigarette pack-years (B) and years since quit smoking cigarettes (C) at Wave 1 for past 30-day exclusive product users. aOutside values are not plotted. A Years of product use. cUnweighted Ns: exclusive e-cigarette = 176; exclusive cigar = 352; exclusive smokeless = 475; exclusive cigarette = 3,760; exclusive dual cigarette and e-cigarette = 851; polycombusted = 613; polycombusted and noncombusted = 444. B Cigarette pack-years. dUnweighted Ns: former established tobacco = 1920; exclusive e-cigarette = 190; exclusive cigar = 353; exclusive smokeless = 442; exclusive cigarette = 3698; exclusive dual cigarette and e-cigarette = 842; polycombusted = 589; polycombusted and noncombusted = 443. C Years since quit smoking cigarettes. eUnweighted Ns: former established tobacco = 2135; exclusive e-cigarette = 190; exclusive cigar = 326; exclusive smokeless = 370..bFormer established user category includes all established users (e.g., lifetime use of more than 100 cigarettes or ever used other products fairly regularly) who did not use any tobacco products in the past 30 days
COPD prevalence
W1 COPD prevalence was 7.7%. Of those with self-reported COPD, 60.1%, 50.6%, and 26.5% had COPD, chronic bronchitis, and emphysema, respectively. In general, individuals with COPD were older, predominantly white, and had less than a high school degree. The majority of individuals with COPD were women. Individuals with COPD were also more likely to have ever smoked cigarettes, currently use cigarettes, cigars, hookah and e-cigarettes, and had greater mean pack-years (among ever cigarette smokers) compared to those without COPD. Individuals with COPD were less likely to live in an urban area or use smokeless tobacco in the past 30 days compared to those without COPD. In addition, individuals with COPD had a higher mean BMI and greater comorbidity count (Table 1). PATH Study prevalence of COPD and emphysema diagnoses were very similar to values from NHANES collected during the same time frame. Chronic bronchitis prevalence was lower in the PATH Study as compared to NHANES, making the composite variable of COPD prevalence slightly lower in the PATH Study vs. NHANES (Table 2).
Table 2.
Comparison of PATH Study COPDa prevalence with NHANESb COPD prevalencec
| Wave 1 PATH Study 2013–14 | NHANES 2013–2014 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Question | PATH Study ID | Response options | Unweighted Ns | Weighted prevalence (SE) | Question | NHANES ID | Response options | Unweighted Ns | Weighted prevalence (SE) |
| Has a doctor or other health professional ever told you that you had any of the following lung or respiratory conditions? COPD | R01_AX0119_01 |
Yes No |
1076 13,179 |
5.1% (0.3) 94.9% (0.3) |
Has a doctor or other health professional ever told [you/SP] that [you have/s/he/SP has] COPD? | MCQ160o |
Yes No |
186 3625 |
5.1% (0.8) 94.9% (0.8) |
| Has a doctor or other health professional ever told you that you had any of the following lung or respiratory conditions? Chronic bronchitis | R01_AX0119_02 |
Yes No |
876 13,379 |
4.4% (0.2) 95.7% (0.2) |
Has a doctor or other health professional ever told [you/SP] that [you/s/he]...had chronic bronchitis? | MCQ160k |
Yes No |
249 3560 |
6.9% (0.5) 93.1% (0.5) |
| Has a doctor or other health professional ever told you that you had any of the following lung or respiratory conditions? Emphysema | R01_AX0119_03 |
Yes No |
533 13,722 |
2.4% (0.1) 97.6% (0.1) |
Has a doctor or other health professional ever told [you/SP] that [you/s/he]...had emphysema? | MCQ160g |
Yes No |
90 3722 |
2.5% (0.5) 97.5% (0.5) |
| (Derived) Ever been diagnosed with COPD, chronic bronchitis, or emphysema | N/A |
Yes No |
1699 12,556 |
8.4% (0.3) 91.6% (0.3) |
(Derived) Ever been diagnosed with COPD, chronic bronchitis, or emphysema | N/A |
Yes No |
383 3424 |
10.5% (0.9) 89.5% (0.9) |
a COPD: Chronic Obstructive Pulmonary Disease
bPATH: Population Assessment of Tobacco and Health; NHANES: National Health and Nutrition Examination Survey
cPrevalence weighted to reflect estimate for the United States adult population. PATH Study data weighted using Wave 1 cross-sectional weights
ID: Identification, N: number, SE: Standard Error, Y/N: Yes/No, SP: sampled person
PATH Study unweighted Ns and prevalence estimates differ slightly from Table 1 as respondents with a history of “other respiratory disease” were not excluded, so as to mirror NHANES methods
Association of W1 tobacco product use with COPD prevalence at W1
Reference group: past 30-day exclusive cigarette use at W1
When compared to exclusive past 30-day cigarette use, never users (fully adjusted model RR = 0.33, CI [0.26–0.42]), former users (RR = 0.57, CI [0.47, 0.70]), and cigar users (RR = 0.46, CI [0.28, 0.76]) had lower COPD prevalence. Smokeless tobacco use was associated with lower COPD prevalence in the unadjusted and pack-years adjusted models (RR = 0.35, CI [0.18, 0.67] and RR = 0.49, CI [0.26, 0.94], respectively), but not when accounting for all potentially confounding variables (RR = 0.55, CI [0.28, 1.06]). Exclusive past 30-day e-cigarette use, and dual and polyuse categories were not associated with COPD (Table 3; Additional file 1: Table S1; all results and effect sizes for individual covariates can be found in online supplement).
Table 3.
Association between Wave 1 past 30-day tobacco use and COPDa prevalence at Wave 1 of the Population Assessment of Tobacco and Health Study
| Twelve mutually exclusive categories of Wave 1 tobacco useb | Weighted Percent with COPD (SE)c | Covariate adjustment | |||||
|---|---|---|---|---|---|---|---|
| Unadjusted (N = 12,838) |
Cigarette pack-years (N = 12,343) |
Fully adjustedd (N = 11,822) |
|||||
| Exclusive cigarette as the reference group | COPD prevalence (RR) | 95% CI | COPD prevalence (RR) | 95% CI | COPD prevalence (RR) | 95% CI | |
| Exclusive P30D cigarette | 16.7 (0.7) | Ref | Ref | Ref | Ref | Ref | Ref |
| Never use (Never or former experimental tobacco) | 3.2 (0.3) | 0.19*** | [0.15,0.24] | 0.38*** | [0.30,0.48] | 0.33*** | [0.26,0.42] |
| Former tobacco use | 10.1 (0.7) | 0.61*** | [0.52,0.71] | 0.63*** | [0.54,0.74] | 0.57*** | [0.47,0.70] |
| Exclusive P30D e-cigarette | 12.1 (2.9) | 0.73 | [0.44,1.20] | 0.64 | [0.39,1.05] | 0.74 | [0.46,1.19] |
| Exclusive P30D cigar | 4.6 (1.1) | 0.28*** | [0.18,0.43] | 0.37*** | [0.23,0.60] | 0.46** | [0.28,0.76] |
| Exclusive P30D smokeless/snus | 5.8 (1.8) | 0.35** | [0.18,0.67] | 0.49* | [0.26,0.94] | 0.55 | [0.28,1.06] |
| Exclusive P30D cigarette and e-cigarette | 18.6 (1.7) | 1.12 | [0.93,1.35] | 1.08 | [0.90,1.30] | 1.03 | [0.86,1.24] |
| P30D polycombusted tobacco use | 17.2 (1.7) | 1.03 | [0.84,1.28] | 1.05 | [0.86,1.28] | 1.12 | [0.91,1.38] |
| P30D polycombusted and noncombusted use | 15.6 (1.6) | 0.93 | [0.76,1.15] | 0.92 | [0.74,1.15] | 0.92 | [0.71,1.18] |
| Never tobacco use as the reference group | COPD prevalence (RR) | 95% CI | COPD prevalence (RR) | 95% CI | COPD prevalence (RR) | 95% CI | |
|---|---|---|---|---|---|---|---|
| Never use (Never or former experimental tobacco) | 3.2 (0.3) | Ref | Ref | Ref | Ref | Ref | Ref |
| Former tobacco use | 10.1 (0.7) | 3.21*** | [2.49,4.14] | 1.66*** | [1.27,2.17] | 1.72*** | [1.33,2.23] |
| Exclusive P30D cigarette | 16.7 (0.7) | 5.28*** | [4.25,6.57] | 2.63*** | [2.07,3.34] | 3.00*** | [2.37,3.80] |
| Exclusive P30D e-cigarette | 12.1 (2.9) | 3.84*** | [2.35,6.28] | 1.68* | [1.02,2.77] | 2.22*** | [1.44,3.42] |
| Exclusive P30D cigar | 4.6 (1.1) | 1.46 | [0.90,2.37] | 0.97 | [0.58,1.62] | 1.38 | [0.82,2.33] |
| Exclusive P30D smokeless/snus | 5.8 (1.8) | 1.85 | [0.95,3.62] | 1.29 | [0.67,2.48] | 1.63 | [0.87,3.07] |
| Exclusive P30D cigarette and e-cigarette | 18.6 (1.7) | 5.91*** | [4.55,7.67] | 2.84*** | [2.14,3.76] | 3.10*** | [2.39,4.02] |
| P30D polycombusted tobacco use | 17.2 (1.7) | 5.47*** | [4.05,7.37] | 2.75*** | [2.00,3.77] | 3.37*** | [2.44,4.65] |
| P30D polycombusted and noncombusted use | 15.6 (1.6) | 4.94*** | [3.67,6.65] | 2.42*** | [1.74,3.36] | 2.74*** | [1.98,3.80] |
a COPD: Chronic Obstructive Pulmonary Disease, defined as self-report of emphysema, chronic bronchitis, or COPD
bData are not presented for exclusive hookah, exclusive pipe, and dual e-cigarette + smokeless/snus users due to small sample size. Never tobacco user category includes former experimental (e.g., lifetime use of < 100 cigarettes or never used other products fairly regularly) users; former established user category includes all established users (e.g., lifetime use of more than 100 cigarettes or ever used other products fairly regularly) who did not use any tobacco products in the past 30 days
cOverall Wave 1 prevalence was 7.7% (SE = 0.3)
dFully adjusted = Risk ratios (RR) are adjusted for cigarette pack-years (never cigarette users were assigned 0 pack-years), past-week secondhand smoke exposure, past 30-day marijuana use, COPD comorbidity index, ever asthma diagnosis, age, sex, race/ethnicity, education, and urbanicity. See Additional file 1: Tablesecond
S1a and S1b for all covariate estimates
*p < 0.05, ** p < 0.01, *** p < 0.001
Reference group: never tobacco use at W1
When compared to never users, all categories featuring cigarette use had higher COPD prevalence in fully adjusted models (former users RR = 1.72, CI [1.33, 2.23]; past 30-day cigarette use RR = 3.00, CI [2.37, 3.80]; dual use of cigarettes and e-cigarettes RR = 3.10, CI [2.39, 4.02]; polycombusted use RR = 3.37, CI [2.44, 4.65]; polycombusted and noncombusted use RR = 2.74, CI [1.98, 3.80]). E-cigarette use was also associated with higher COPD prevalence (RR = 2.22, CI [1.44, 3.42]) (Table 3; Additional file 1: Table S1).
COPD incidence W2-5
Cumulative COPD incidence in W2-5 was 5.8% (SE = 0.3). Incidence was higher in past 30-day cigarette users vs non-cigarette users (13.6% [SE = 0.6] vs 4.4% [SE = 0.4]), and in past 30-day e-cigarette users vs non-e-cigarette users (12.0% [SE = 1.4] vs 5.6% [SE = 0.3]).
Association of W1 tobacco product use with COPD incidence at W2–5
Reference group: past 30-day exclusive cigarette use at W1
When compared to exclusive cigarette users at W1, never and former users had lower risk of COPD (fully adjusted model RR = 0.52, CI [0.35, 0.79] and RR = 0.47, CI [0.32, 0.70], respectively). In models accounting for pack-years of cigarettes, cigar use was associated with lower COPD risk (RR = 0.29, CI [0.15, 0.59] and RR = 0.42, CI [0.20, 0.88], respectively), but this relationship did not persist following adjustment for all confounders (RR = 0.55, CI [0.24, 1.26]). When unadjusted, past 30-day smokeless tobacco use was associated with lower COPD incidence (RR = 0.55, CI [0.34, 0.90]), but not in fully adjusted models (RR = 1.08, CI [0.58, 2.03]). Past 30-day e-cigarette, and dual and polyusers did not have higher COPD incidence (Table 4; Additional file 1: Table S2).
Table 4.
Association between Wave 1 past 30-day tobacco use and COPDa incidence Waves 2–5 of the Population Assessment of Tobacco and Health Study
| Twelve mutually exclusive categories of Wave 1 tobacco useb | Weighted Percent with new onset COPD W2-W5 (SE)c | Covariate adjustment | |||||
|---|---|---|---|---|---|---|---|
| Unadjusted (N = 6475) |
Cigarette pack-years (N = 6220) |
Fully adjustedd (N = 6018) |
|||||
| Exclusive cigarette as the reference group | COPD incidence (RR) | 95% CI | COPD incidence (RR) | 95% CI | COPD incidence (RR) | 95% CI | |
| Exclusive P30D cigarette | 13.4 (0.8) | Ref | Ref | Ref | Ref | Ref | Ref |
| Never use (Never or former experimental tobacco) | 3.8 (0.4) | 0.28*** | [0.22,0.37] | 0.50*** | [0.35,0.71] | 0.52** | [0.35,0.78] |
| Former tobacco use | 5.5 (0.7) | 0.41*** | [0.30,0.55] | 0.41*** | [0.31,0.55] | 0.47*** | [0.32,0.70] |
| Exclusive P30D e-cigarette | 9.5 (3.5)† | 0.71 | [0.28,1.78] | 0.63 | [0.26,1.49] | 0.71 | [0.26,1.92] |
| Exclusive P30D cigar | 3.9 (1.2)† | 0.29*** | [0.15,0.59] | 0.42* | [0.20,0.88] | 0.55 | [0.24,1.26] |
| Exclusive P30D smokeless/snus | 7.4 (1.7) | 0.55* | [0.34,0.90] | 0.77 | [0.46,1.30] | 1.08 | [0.58,2.03] |
| Exclusive P30D cigarette and e-cigarette | 14.2 (1.9) | 1.06 | [0.78,1.45] | 1.05 | [0.78,1.43] | 1.04 | [0.77,1.40] |
| P30D polycombusted tobacco use | 15.8 (2.4) | 1.18 | [0.84,1.66] | 1.18 | [0.84,1.67] | 1.35 | [0.92,1.99] |
| P30D polycombusted and noncombusted use | 8.5 (1.7) | 0.63* | [0.41,0.98] | 0.66 | [0.43,1.03] | 0.77 | [0.50,1.19] |
| Never tobacco use as the reference group | COPD incidence (RR) | 95% CI | COPD incidence (RR) | 95% CI | COPD incidence (RR) | 95% CI | |
|---|---|---|---|---|---|---|---|
| Never use (Never or former experimental tobacco) | 3.8 (0.4) | Ref | Ref | Ref | Ref | Ref | Ref |
| Former tobacco use | 5.5 (0.7) | 1.44* | [1.04,2.00] | 0.83 | [0.56,1.22] | 0.90 | [0.62,1.33] |
| Exclusive P30D cigarette | 13.4 (0.8) | 3.53*** | [2.73,4.57] | 2.02*** | [1.41,2.89] | 1.92** | [1.29,2.86] |
| Exclusive P30D e-cigarette | 9.5 (3.5)† | 2.49* | [1.00,6.19] | 1.27 | [0.54,2.98] | 1.36 | [0.55,3.39] |
| Exclusive P30D cigar | 3.9 (1.2)† | 1.03 | [0.51,2.10] | 0.86 | [0.42,1.73] | 1.05 | [0.49,2.25] |
| Exclusive P30D smokeless/snus | 7.4 (1.7) | 1.94* | [1.15,3.26] | 1.56 | [0.91,2.67] | 2.08* | [1.07,4.03] |
| Exclusive P30D cigarette and e-cigarette | 14.2 (1.9) | 3.74*** | [2.74,5.10] | 2.13*** | [1.48,3.06] | 1.99** | [1.29,3.07] |
| P30D polycombusted tobacco use | 15.8 (2.4) | 4.17*** | [2.87,6.06] | 2.39*** | [1.55,3.67] | 2.59*** | [1.60,4.21] |
| P30D polycombusted and noncombusted use | 8.5 (1.7) | 2.24*** | [1.45,3.45] | 1.34 | [0.86,2.08] | 1.48 | [0.92,2.39] |
aCOPD: Chronic Obstructive Pulmonary Disease, defined as self-report of emphysema, chronic bronchitis, or COPD
bData are not presented for exclusive hookah, exclusive pipe, and dual e-cigarette + smokeless/snus users due to small sample size. Never tobacco user category includes former experimental (e.g., lifetime use of < 100 cigarettes or never used other products fairly regularly) users; former established user category includes all established users (e.g., lifetime use of more than 100 cigarettes or ever used other products fairly regularly) who did not use any tobacco products in the past 30 days
cOverall cumulative COPD incidence in W2-5 was 5.8% (SE = 0.3)
dFully adjusted = Risk ratios (RR) are adjusted for cigarette pack-years (never cigarette users were assigned 0 pack-years), past-week secondhand smoke exposure, past 30-day marijuana use, COPD comorbidity index, ever asthma diagnosis, age, sex, race/ethnicity, education, and urbanicity. See Additional file 1: Table S2a and S2b for all covariate estimates
†Estimate should be interpreted with caution because it has low statistical precision. It is based on a denominator sample size of less than 50, or the coefficient of variation of the estimate or its complement is larger than 30%
*p < 0.05, ** p < 0.01, *** p < 0.001
Reference group: never tobacco use at W1
When compared to never users, most categories featuring cigarette use had higher COPD incidence in fully adjusted models (cigarette use RR = 1.92, CI [1.29, 2.86]; dual cigarette and e-cigarette use RR = 1.99, CI [1.29, 3.07]; polycombusted use RR = 2.59, CI [1.60, 4.21]). Smokeless tobacco use was associated with a higher COPD risk, although this group has a relatively wide CI due to the small number of new COPD cases (RR = 2.08, CI [1.07, 4.03]). There was no relationship between former tobacco, e-cigarette, cigar, or polycombusted and noncombusted use and COPD incidence (Table 4; Additional file 1: Table S2).
Sensitivity analyses
The incidence of COPD did not meaningfully differ when we included individuals who contributed data to two or more waves (n = 9470) (Additional file 1: Table S3), excluded participants with baseline asthma, and included all adults 18 years and older (data not shown).
Discussion
In a nationally representative sample of adults aged 40 years and older, past 30-day cigarette use was associated with higher COPD prevalence and incidence compared to never tobacco use. This association remained consistent regardless of what other tobacco products were used in conjunction with cigarettes. These results confirm the expected association between cigarette smoking and COPD outlined in the 1984 Surgeon General’s report and scores of observational studies [2, 31]. COPD prevalence was not found to be lower in exclusive e-cigarette users compared to exclusive cigarette smokers, and when compared to never tobacco use, current e-cigarette use and cigarette and e-cigarette dual use were associated with increased COPD prevalence. Importantly, the COPD prevalence bye-cigarette and cigarette use did not differ; only never use, former use, and cigar use were associated with lower COPD prevalence compared to current cigarette smoking. Similarly, when evaluating the association between tobacco products and COPD incidence, cigarette and cigarette and e-cigarette dual use were associated with greater COPD incidence compared to never tobacco use. Compared to cigarette smoking, only former and never tobacco users had lower COPD incidence; although some categories had relatively small sample sizes, no product was associated with less risk.
E-cigarettes generate particulate matter and trace metals [32–34], which may stimulate inflammation and lung damage to a degree similar to cigarette smoke, potentially contributing to respiratory disease progression [35]. We found an association between e-cigarette use and COPD prevalence, similar to two studies using Behavior Risk Factor Surveillance System (BRFSS) data. Osei et al. found an association between e-cigarette use and higher odds of self-reported COPD in never, former, and current smokers [10]. In a comparable analysis, Xie et al. found an association between e-cigarette use and increased odds of self-reported COPD, including in those who had never smoked cigarettes [11]. Prior work from W1 of the PATH Study also supports our prevalence findings. Perez et al. used propensity-matching to examine the relationship between e-cigarette use and COPD diagnosis, and found that e-cigarette use was associated with higher odds of COPD in both cigarette smokers and non-smokers [8]. Our study adds to this existing knowledge base by comparing COPD prevalence between e-cigarette users and cigarette smokers.
We are uncertain if the observed relationship between e-cigarette use and COPD prevalence is a reflection of the innate risk of e-cigarettes or a marker of higher burden of cigarette exposure. First, COPD develops as a result of decades long exposure to noxious particles and gases [1], such that the duration of e-cigarette use among contemporary users is likely not long enough to have a large influence on COPD onset. Second, the exclusive e-cigarette and exclusive cigarette users in this study had comparable cigarette smoking histories as measured by pack years, and exclusive e-cigarette users had only stopped smoking cigarettes somewhat recently, suggesting that cigarette exposure may be the main driver of the association with COPD. This is similar to the observed association between polyuse and COPD risk, which is likely driven by the cigarette component. While we emphasize the importance of considering pack-years of smoking exposure, we recognize the potential for unmeasured confounding that is not captured by pack-years, which has been shown to be an imperfect measure of overall cigarette smoking history [36].
These uncertainties are highlighted in our findings on COPD incidence. While we found an association between e-cigarette use and COPD incidence when compared to never use in the unadjusted models, this relationship did not persist after careful consideration of additional covariates. These results differ from those of Xie et al., who in their analysis of the first four waves of PATH Study data found an association between e-cigarette use and increased risk of respiratory disease, including COPD [13]. The authors included all adults over the age of 18 in their study, raising uncertainty about the COPD endpoint given that younger age is associated with misdiagnosis of COPD [37]. In addition, while pack-years of cigarette smoking was included as a covariate in the models for current cigarette smokers, it was not for former cigarette smokers. Given that the majority of exclusive e-cigarette users are former smokers, the association observed by Xie et al. may be in part due to a high burden of past cigarette smoking. Indeed, in our study, simply adjusting for cigarette pack-years eliminated the association between exclusive past 30-day e-cigarette smoking and COPD incidence.
Of interest is the association between cigar use and decreased COPD prevalence when compared to cigarettes. In a prior longitudinal study of over 17,000 men who never smoked cigarettes, cigar use was associated with a 45% increased risk of self-reported COPD [38]. Further, in a cross-sectional analysis of Multi-Ethnic Study of Atherosclerosis (MESA) Lung data, Rodriguez et al. found that an increase in cigar-years was associated with airflow obstruction, findings which were attenuated when restricting analysis to never cigarette smokers [15]. In our study, when comparing to never tobacco use, cigar use was not significantly associated with COPD prevalence nor incidence. Most exclusive cigar smokers in the current study had quit cigarette smoking > 20 years ago and had smoked fewer pack-years compared to exclusive cigarette users. In this context, it seems plausible that their risk for COPD tended to be more like former than current cigarette smokers. Furthermore, lower COPD prevalence with exclusive cigar use may be explained by the reduced smoke inhalation and lower frequency of smoking in exclusive users of traditional cigars [39], the predominant cigar type used by the study population [40].
Our study has several strengths. Analysis was limited to adults aged 40 years and older, a timeline consistent with the accepted principles of development of airflow obstruction following years of exposure to noxious particles and gases [1]. Further, our study benefits from the repeated outcome measures afforded by the PATH Study, as well as explicitly accounting for pack-years of smoking and additional confounders not captured by other studies. Using two reference categories (current exclusive cigarette smoking and never tobacco use) highlights the importance of accounting for multiple product use and the unique contributions of each tobacco product to COPD risk.
There are several limitations to note. The PATH Study relies on participant self-report of physician diagnosis and not spirometry to define COPD. While spirometric evidence of airflow obstruction is required to make a COPD diagnosis, spirometry is often underutilized in clinical settings, resulting in both a potential under-diagnosis and over-diagnosis of COPD [19, 41, 42]. As an example, physicians may be more likely to workup or diagnose COPD in a symptomatic individual who smokes compared to a never cigarette smoker, a population that is under-diagnosed with COPD [43] despite estimates that up to 25% of US individuals with COPD have never smoked [44]. The lack of spirometry in the PATH Study along with the potential of diagnostic and recall bias associated with self-report may introduce imprecision in the COPD diagnosis and confound the associations observed in our study. To help mitigate these concerns, the prevalence estimates of COPD in our study are largely consistent with those reported in NHANES analyses, which included spirometry in a subset of participants [19, 20], providing confidence in our study endpoint. Accounting for self-report of asthma as well as multiple other diseases that may share symptoms with COPD in our adjusted analysis helps to address concerns for misclassification of self-report of physician-diagnosed COPD, a potential limitation of survey research in general.
We examined tobacco product use at a single time point (W1), although prior PATH Study research has shown product-specific persistent use over time in adults [45]. Further, our definition of product use also does not allow for detection of a dose-related effect. In addition, residual confounding may exist despite our best efforts to control for cigarette exposure. Knowing that respiratory symptoms may influence an individual’s ability and choice to inhale tobacco products, the potential remains for reverse causality. The analysis considered the e-cigarette devices and flavorings used in W1 and these may have changed over time in ways relevant to COPD development. Further, the sample size for several tobacco products was somewhat limited. Exclusive e-cigarette use was relatively uncommon in adults ≥ 40 years of age, which limits the power to determine if they are a lower harm product in population studies. Future studies should extend this analysis with more waves of data to capture both the association of a longer of e-cigarette use with COPD risk as well to account for new adopters of e-cigarettes in a dynamic tobacco industry.
Conclusions
In summary, our longitudinal analysis of PATH Study W1-5 data supports existing, fundamental knowledge about the relationship between cigarette smoking, alone or in combination with other tobacco products, and COPD prevalence and incidence. These results further the need for continued focus on prevention of tobacco product initiation as well as effective behavioral and pharmacologic tobacco cessation therapies to decrease COPD incidence. We found an association between exclusive e-cigarette use and COPD prevalence when compared to never tobacco use, which may be due to a high burden of pack-years among users of these products; notably, we did not find an association between e-cigarette use and COPD incidence. Future work that examines a longer duration of e-cigarette use would be of value to better characterize the impact of these products on COPD outcomes.
Supplementary Information
Additional file 1. Association of tobacco product use with chronic obstructive pulmonary disease (COPD) prevalence and incidence in Waves 1 through 5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) Study.
Acknowledgements
Gabriella Anic contributed to this manuscript while she worked at the Food and Drug Administration’s Center for Tobacco Products.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
Abbreviations
- BMI
Body mass index
- BRFSS
Behavior Risk Factor Surveillance System
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- MESA
Multi-Ethnic Study of Atherosclerosis
- NHANES
National Health and Nutrition Examination Survey
- P30D
Past 30-day
- PATH
Population Assessment of Tobacco and Health
- RR
Risk ratio
- W1–5
Waves 1–5
Author contributions
LMP and JDS were involved with the initial conception of the research questions. LMP, MJH, KCE, KL, CAS, KT, DH, AH, TM, MCM, RN, DT, CB, WMC, LDG, HLK, DL, DM, and JDS were involved with the planning of the data analyses and interpretation of the data analyses. MJH analyzed the data. LMP and MJH wrote the manuscript. LMP, MJH, KCE, KL, CAS, KT, DH, AH, TM, MCM, RN, DT, CB, WMC, LDG, HLK, DL, DM, and JDS were involved with reviewing, editing and final approval of the manuscript. All authors read and approved the final manuscript.
Funding
This manuscript is supported with Federal funds from the National Institute on Drug Abuse (NIDA), National Institutes of Health (NIH), and the Center for Tobacco Products (CTP), Food and Drug Administration (FDA), Department of Health and Human Services, under contract to Westat (contract nos. HHSN271201100027C and HHSN271201600001C), and through an interagency agreement between NIH NIDA and FDA CTP. (NIDA Federal Author name) was substantially involved in the scientific management of and providing scientific expertise for contract nos. HHSN271201100027C and HHSN271201600001C.
Availability of data and materials
Details on accessing the PATH Study data are described in the PATH Study Restricted Use Files website located at https://doi.org/10.3886/ICPSR36231.v29. Access to these data is restricted. Users interested in obtaining these data must complete a Restricted Data Use Agreement.
Declarations
Ethics approval and consent to participate
All adult respondents provided informed consent. The study was conducted by Westat and approved by the Westat Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
Martin C. Mahoney has provided expert testimony on the health effects of smoking in lawsuits filed against the tobacco industry. He has also received research support from Pfizer, Inc., for a clinical trial of smoking cessation, and has previously served on external advisory panels sponsored by Pfizer to promote smoking cessation in clinical settings. Raymond Niaura receives funding from the Food and Drug Administration Center for Tobacco Products via contractual mechanisms with Westat and the National Institutes of Health. Within the past 3 years, he has served as a paid consultant to the Government of Canada via a contract with Industrial Economics Inc. and has received an honorarium for a virtual meeting from Pfizer Inc. Dr. Niaura was an unpaid grant reviewer for the Foundation for a Smoke Free World. Wilson Compton reports long-term stock holdings in General Electric, 3 M Company, and Pfizer Incorporated, unrelated to this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
3/8/2025
A Correction to this paper has been published: 10.1186/s12931-025-03166-0
References
- 1.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022).
- 2.Forey BA, Thornton AJ, Lee PN. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm Med. 2011;11(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claire SS, Gouda H, Schotte K, et al. Lung health, tobacco, and related products: gaps, challenges, new threats, and suggested research. Am J Physiol Lung Cell Mol Physiol. 2020;318(5):L1004–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hajek P, Phillips-Waller A, Przulj D, et al. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–37. [DOI] [PubMed] [Google Scholar]
- 5.Polosa R, Rodu B, Caponnetto P, Maglia M, Raciti C. A fresh look at tobacco harm reduction: the case for the electronic cigarette. Harm Reduct J. 2013;10:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polosa R, Morjaria JB, Prosperini U, et al. Health effects in COPD smokers who switch to electronic cigarettes: a retrospective-prospective 3-year follow-up. Int J Chron Obstruct Pulmon Dis. 2018;13:2533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polosa R, Morjaria JB, Prosperini U, et al. COPD smokers who switched to e-cigarettes: health outcomes at 5-year follow up. Ther Adv Chronic Dis. 2020;11:2040622320961617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perez MF, Atuegwu NC, Mead EL, Oncken C, Mortensen EM. Adult e-cigarettes use associated with a self-reported diagnosis of COPD. Int J Environ Res Public Health. 2019;16(20):3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wills TA, Pagano I, Williams RJ, Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend. 2019;194:363–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osei AD, Mirbolouk M, Orimoloye OA, et al. Association between E-Cigarette use and chronic obstructive pulmonary disease by smoking status: behavioral risk factor surveillance system 2016 and 2017. Am J Prevent Med. 2020;58(3):336–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie Z, Ossip DJ, Rahman I, Li D. Use of electronic cigarettes and self-reported chronic obstructive pulmonary disease diagnosis in adults. Nicotine Tob Res. 2020;22(7):1155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med. 2019;58(2):182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xie W, Kathuria H, Galiatsatos P, et al. Association of electronic cigarette use with incident respiratory conditions among US adults from 2013 to 2018. JAMA Netw Open. 2020;3(11):e2020816–e2020816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi H, Tavárez ZQ, Xie Z, et al. Association of flavored electronic nicotine delivery system (ENDS) use with self-reported chronic obstructive pulmonary disease (COPD): results from the Population Assessment of Tobacco and Health (PATH) study, Wave 4. Tob Induc Dis. 2020;18:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez J, Jiang R, Johnson WC, MacKenzie BA, Smith LJ, Barr RG. The association of pipe and cigar use with cotinine levels, lung function, and airflow obstruction: a cross-sectional study. Ann Intern Med. 2010;152(4):201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tourangeau R, Yan T, Sun H, Hyland A, Stanton CA. Population Assessment of Tobacco and Health (PATH) reliability and validity study: Selected reliability and validity estimates. Tob Control. 2019;28(6):663–8. [DOI] [PubMed] [Google Scholar]
- 18.Piesse A, Opsomer J, Dohrmann S, et al. Longitudinal uses of the population assessment of tobacco and health study. Tob Regul Sci. 2021;7(1):3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tilert T, Dillon C, Paulose-Ram R, Hnizdo E, Doney B. Estimating the U.S. prevalence of chronic obstructive pulmonary disease using pre- and post-bronchodilator spirometry: the National Health and Nutrition Examination Survey (NHANES) 2007–2010. Respir Res. 2013;14:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tilert T, Paulose-Ram R, Howard D, Butler J, Lee S, Wang MQ. Prevalence and factors associated with self-reported chronic obstructive pulmonary disease among adults aged 40–79: the National Health and Nutrition Examination Survey (NHANES) 2007–2012. EC Pulmonol Respir Med. 2018;7(9):650–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Couper D, Lavange LM, Han M, et al. Design of the subpopulations and intermediate outcomes in COPD Study (SPIROMICS). Thorax. 2013;69(5):492–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Regan EA, Hokanson JE, Murphy JR, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD. 2010;7(1):32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Department of Health Human Services, National Institutes of Health, National Institute on Drug Abuse, United States Department of Health Human Services, Food Drug Administration, Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Restricted-Use Files. In: Inter-university Consortium for Political and Social Research [distributor]; 2021.
- 24.Wu J-J, Xu H-R, Zhang Y-X, et al. The characteristics of the frequent exacerbators with chronic bronchitis phenotype and the asthma-chronic obstructive pulmonary disease overlap syndrome phenotype in chronic obstructive pulmonary disease patients: a meta-analysis and system review. Medicine. 2019;98(46):e17996–e17996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisner MD, Iribarren C, Yelin EH, et al. The impact of SHS exposure on health status and exacerbations among patients with COPD. Int J Chron Obstruct Pulmon Dis. 2009;4:169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghasemiesfe M, Ravi D, Vali M, et al. Marijuana Use, Respiratory Symptoms, and Pulmonary Function: A Systematic Review and Meta-analysis. Ann Intern Med. 2018;169(2):106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Putcha N, Puhan MA, Drummond MB, et al. A simplified score to quantify comorbidity in COPD. PLoS ONE. 2014;9(12): e114438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCarthy PJ. Pseudoreplication: further evaluation and applications of the balanced half-sample technique. 1969. [PubMed]
- 29.Judkins DR. Fay’s method for variance estimation. Journal of Official Statistics. 1990;6(3):223. [Google Scholar]
- 30.Stata Statistical Software: Release 17. [computer program]. College Station, TX: StataCorp LLC; 2019.
- 31.Office of the Surgeon G, Office on S, Health. Reports of the Surgeon General. In: The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2004. [PubMed]
- 32.Sakamaki-Ching S, Williams M, Hua M, et al. Correlation between biomarkers of exposure, effect and potential harm in the urine of electronic cigarette users. BMJ Open Respir Res. 2020;7(1): e000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Song MA, Freudenheim JL, Brasky TM, et al. Biomarkers of exposure and effect in the lungs of smokers, nonsmokers, and electronic cigarette users. Cancer Epidemiol. 2020;29(2):443–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olmedo P, Goessler W, Tanda S, et al. Metal concentrations in e-cigarette liquid and aerosol samples: the contribution of metallic coils. EnvironHealth Perspect. 2018;126(2): 027010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bozier J, Rutting S, Xenaki D, Peters M, Adcock I, Oliver BG. Heightened response to e-cigarettes in COPD. ERJ Open Research. 2019;5(1):00192–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pleasants RA, Rivera MP, Tilley SL, Bhatt SP. Both duration and pack-years of tobacco smoking should be used for clinical practice and research. Ann Am Thorac Soc. 2020;17(7):804–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gershon AS, Hwee J, Chapman KR, et al. Factors associated with undiagnosed and overdiagnosed COPD. Eur Respir J. 2016;48(2):561–4. [DOI] [PubMed] [Google Scholar]
- 38.Iribarren C, Tekawa IS, Sidney S, Friedman GD. Effect of cigar smoking on the risk of cardiovascular disease, chronic obstructive pulmonary disease, and cancer in men. N Engl J Med. 1999;340(23):1773–80. [DOI] [PubMed] [Google Scholar]
- 39.Baker F, Ainsworth SR, Dye JT, et al. Health risks associated with cigar smoking. JAMA. 2000;284(6):735–40. [DOI] [PubMed] [Google Scholar]
- 40.Edwards KC, Sharma E, Halenar MJ, et al. Longitudinal pathways of exclusive and polytobacco cigar use among youth, young adults and adults in the USA: findings from the PATH Study Waves 1–3 (2013–2016). Tob Control. 2020;29(Suppl 3):s163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diab N, Gershon AS, Sin DD, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–9. [DOI] [PubMed] [Google Scholar]
- 42.Ho T, Cusack RP, Chaudhary N, Satia I, Kurmi OP. Under- and over-diagnosis of COPD: a global perspective. Breathe (Sheff). 2019;15(1):24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lamprecht B, McBurnie MA, Vollmer WM, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011;139(4):752–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Syamlal G, Doney B, Mazurek JM. Chronic obstructive pulmonary disease prevalence among adults who have never smoked, by industry and occupation—United States, 2013–2017. Morb Mortal Wkly Rep. 2019;68(13):303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taylor KA, Sharma E, Edwards KC, et al. Longitudinal pathways of exclusive and polytobacco cigarette use among youth, young adults and adults in the USA: findings from the PATH Study Waves 1–3 (2013–2016). Tob Control. 2020;29(Suppl 3):s139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Association of tobacco product use with chronic obstructive pulmonary disease (COPD) prevalence and incidence in Waves 1 through 5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) Study.
Data Availability Statement
Details on accessing the PATH Study data are described in the PATH Study Restricted Use Files website located at https://doi.org/10.3886/ICPSR36231.v29. Access to these data is restricted. Users interested in obtaining these data must complete a Restricted Data Use Agreement.