Abstract
Background
The aim of the present work was to cross-culturally adapt the Postpartum Depression Literacy Scale (PoDLiS) and use a descriptive cross-sectional design to evaluate its psychometric properties in Chinese perinatal women.
Methods
Brislin’s translation theory was applied to translate the PoDLiS, with subsequent cultural adaptation. The reliability and validity of the PoDLiS were determined using a questionnaire in 635 Chinese perinatal women.
Results
Good internal consistency was found (omega coefficient, 0.894) for the Chinese version of the Postpartum Depression Literacy Scale (PoDLiS-C), with omega coefficients of the six dimensions of 0.865, 0.870, 0.838, 0.777, 0.837 and 0.794, and a test–retest reliability coefficient of 0.874. The item-level content validity index (CVI) ranged from 0.8 to 1 while the scale-level CVI was 0.968. Moreover, confirmatory factor analysis (CFA) determined satisfactory construct validity of the PoDLiS-C, with the six-factor model explaining 60.76% of the total variance, demonstrating good model fit (likelihood ratio χ2/df, 1.003; goodness-of-fit index, 0.916; adjusted goodness-of-fit index, 0.901; comparative fit index, 0.999; incremental fit index, 0.999; root mean square error of approximation, 0.003; and standardized root mean square error of approximation, 0.0478).
Conclusions
The PoDLiS-C has adequate psychometric properties. This tool could be used to assess the postpartum depression literacy of perinatal women in Chinese-speaking populations.
Keywords: Mental health literacy, Perinatal women, Psychometric properties, Postpartum depression literacy scale
Background
Postpartum depression (PPD) refers to a series of physical and psychological symptoms occurring during the perinatal period [1]. According to the DSM-V, PPD refers to a diagnosis of moderate-to-severe symptoms that occur during pregnancy or within 4 weeks of delivery. Its primary symptoms include persistent and severe depression, impaired creative thinking, lack of confidence in life, and decreased self-evaluation, as well as a series of symptoms such as anorexia, sleep disturbance, anxiety, fatigue, and even recurrent thoughts of death [2–4].
PPD has become a common perinatal complication [5], with a global prevalence of about 17% [6–8]. Furthermore, less developed countries with lower economic incomes have higher incidences of PPD [9, 10]. The incidence of PPD in Asian countries is about 21.8%, while its prevalence in China is around 27.37% and increasing annually [11–13]. The condition is now considered a public health problem that, in addition to impacting mothers and children’s health, undermines family relationships [10]. Additionally, PPD has been identified as the most disabling disease for women during the perinatal period [14].
The incidence of PPD is high, but the diagnosis rate of the disease is low, with only approximately 40% of women with PPD diagnosed [15]. PPD is very harmful, but the willingness to seek help in women with PPD is relatively low, at only 20% to 40% [16]. The majority of women do not try to get professional help to address the signs and symptoms of PPD, nor do they seek treatment for the disease. Moreover, women with PPD in less developed countries have a lower willingness to seek help [17]. Insufficient knowledge of the signs, symptoms, and treatment possibilities of PPD in perinatal women is considered to be a major obstacle in the path of women who would otherwise seek help [18, 19]. Therefore, the provision of relevant knowledge, beliefs, and attitudes is critical to help women to identify PPD and acquire efficacious treatment [18].
As defined by Jorm [20], mental health literacy (MHL) is the knowledge of and beliefs about mental illnesses that make them easy to identify, manage, or prevent. Jorm explains that MHL is not just about acquiring knowledge about mental health disorders, but is the application of that knowledge in addition to possible action to promote a person's mental health [21, 22]. MHL includes six components, namely (1) the ability to identify specific mental health conditions; (2) knowledge and beliefs of their risk factors and causes; (3) knowledge and beliefs of effective self-treatment strategies; (4) knowledge and beliefs of the available professional help and therapeutic options; (5) attitudes promoting recognition of the condition and adequate help-seeking behavior; and (6) knowledge of where to find mental health information. Most of the current assessment tools for MHL emphasize the recognition and understanding of depression [23], schizophrenia [24], and anxiety [25]. The awareness of PPD and other specific mental diseases is low.
PPD literacy assessment tools allow perinatal women and healthcare workers to understand their level of PPD literacy and to evaluate the effectiveness of various intervention strategies [26]. Using semi-structured interviews, Ransing [27] developed a 26-question, 3-point Likert scale to determine the mental health knowledge, attitudes, and awareness of a population in the perinatal period, which revealed low PPD literacy among Indian perinatal women and a misunderstanding regarding etiology and that nurse practitioner-based management may be a substantial obstacle to the delivery and utilization of PPD services. Therefore, PPD literacy must be urgently improved in perinatal women and nurse practitioners. Self-designed instruments, including the Knowledge about Postpartum Depression Questionnaire (KPPD-Q; 15 items) and the Attitudes about Postpartum Depression Questionnaire (APPD-Q; 17 items) [28] were used in the Portuguese general population. The results of the survey showed that, despite the existence of knowledge gaps and some stereotypes, the knowledge level and positive attitude of PPD were still good. A Portuguese version of the Depression Literacy Questionnaire (22 items), used to assess depression-related characteristics, identified moderate depression literacy in perinatal women [18]. Furthermore, Pamela Recto modified the Mental Health Literacy Scale (MHLS) and determined moderate PPD literacy in pregnant and postpartum Hispanic adolescents [4]. However, relatively few self-assessment tools addressing PPD in the framework of MHL have been designed. Furthermore, the inconsistency of these findings is possibly a reflection of the complexity of PPD literacy in the perinatal setting, which remains incompletely understood. Accordingly, it is meaningful to develop a PPD literacy assessment tool under the guidance of specific theory and to apply it to diverse samples.
Mirsalimi [26] developed a self-report scale to assess PPD literacy during the perinatal period (Postpartum Depression Literacy Scale [PoDLiS]), taking into account the specific aspects of MHL that have been found to become more evident in PPD while maintaining consistency with the multifaceted understanding of the theory of MHL. The PoDLiS items were built based on a review of all assessment tools for mental health literacy, qualitative research, definitions and frameworks of mental health literacy. Moreover, the PoDLiS was conceived to address critical aspects of PPD literacy. The original research, which included 692 women in the perinatal period, showed good construct and content validities and internal consistency reliability. Therefore, the scale may be used as a valuable tool for the measurement of PPD literacy levels in the perinatal period and may help us to better understand the complex mechanisms of PPD literacy.
There is no tool to measure PPD literacy in China. We thus aimed to culturally adapt and psychometrically test the PoDLiS in a Chinese sample of perinatal women.
Materials & methods
Setting and samples
In the current study, we used a cross-sectional design with convenience sampling. A newly developed questionnaire was implemented in two comprehensive tertiary hospitals in Yantai, China, from November 2020 to February 2021. Perinatal women were recruited from the obstetric clinic, maternity school, obstetric ward, and delivery room. According to the Kendall method for estimating sample size, we determined that the sample population would need to be from 5 to 10 times the number of items [29]. The current tool contained 31 items. Thus, considering that approximately 10% of the sample may be invalid, the required sample size was calculated to be 344 for item analysis, internal consistency and exploratory factor analysis (EFA) in the first study phase. In the second study phase, another 200 perinatal women were recruited which exceeded the minimum sample size suggested for CFA [30].
Women were considered potential participants if they a) were ≥ 20 years old; b) were currently pregnant or had given birth in the hospital participating in the study; c) had basic listening and writing skills and could read and understand the questionnaire contents on their own or with the help of others; and d) provided written informed consent. Women were excluded if they a) were undergoing in vitro fertilization; b) had severe pregnancy complications; or c) experienced stillbirths, neonatal malformations, or a baby with a serious illness. The women were explained the aims of the study and could freely refuse to participate or discontinue their participation at any time.
Measures
Demographic characteristics
We collected participants’ demographic variables and those related to the pregnancy, such as age, place of residence, marital status, education, household income, perinatal period, and history of depression.
The Postpartum Depression Literacy Scale( PoDLiS)
The original English-language form of the PoDLiS contains 31 items and is used to measure maternal PPD literacy levels [26]. The instrument includes seven factors, namely the ability to identify PPD (six items), knowledge of risk factors and causes (five items), knowledge and beliefs of self-care activities (five items), knowledge about the availability of professional help (two items), beliefs about available professional help (two items), attitudes facilitating the recognition of PPD and appropriate help-seeking (six items), and knowledge of how to seek information related to PPD (five items). The scale uses a Likert 5-point scoring method for items 7–11 on the scale, from not likely at all (1 point) to very likely (5 points), while the other items range from strongly disagree (1 point) to strongly agree (5 points). Its reliability and validity were found to be satisfactory. For the total original PoDLiS, the Cronbach's α coefficient is 0.78 and the content validity index (CVI) is between 0.80 and 1. The construct validity was demonstrated with a χ2/df of 1.38, root mean square error of approximation (RMSEA) of 0.040, standardized root mean square residual (SRMR) of 0.074, comparative fit index (CFI) of 0.919, incremental fit index (IFI) of 0.921, and goodness-of-fit index (GFI) of 0.871 [26]. A higher total score on the scale represents better maternal perinatal MHL. We have permission to use this instrument from the copyright holders.
The translation procedure
Authorization of the translation was obtained from the original author of the PoDLiS. We adhered to Brislin’s translation theory during the translation procedure [31] (Fig. 1). First, two bilingual postgraduate students independently translated the original scale into Chinese. Another bilingual postgraduate student separately compared and analyzed the two initial versions, consulted with the research team members to revise each item, and determined the synthesized translated version. Second, two additional translators, blinded to the original PoDLiS and with more than 1 year of overseas study experience, independently back-translated the synthesized translated version into English. Then, another bilingual English teacher, along with the research team, made a comparative analysis between the two versions and the original scale. The research team revised some wording to make the scale more culturally in line for use with a Chinese population. An incorporated back-translation version of the scale was then formed. The primary bilingual translators examined the cultural and the linguistic consistency among the back-translated version, synthesized translated version, and original English-language version, and any inconsistencies summarized in this procedure were reviewed with the author of the original version. Lastly, the synthesized version was modified to verify that the expressions maintained the original meaning.
Fig. 1.
The process followed for translating and adapting the postpartum depression literacy scale for perinatal women
Expert consultations
A panel of five experts, including a psychologist, obstetrician, two head nurses of the obstetrics department, and linguist, all of whom had knowledge of PPD literacy and relevant research experience, were asked to use a 4-point Likert scale (from “not relevant” [1 point] to “highly relevant” [4 points]) to assess the degree of relevance between each item and the conceptual framework of PPD literacy and provide comments. In that process, consensus concerning the suitability and language of the synthesized version, as well as its cultural and linguistic consistency, was reached.
Pilot testing
Thirty perinatal women were recruited to evaluate item comprehensibility. The participants required between 8 and 15 min to finish the questionnaire. The subjects thought that each item could be understood without modification. The final 31 items of our Chinese version of the PPD literacy scale (PoDLiS-C) were formed from this step and it was unanimously regarded as fluent and easy to understand.
Data collection
Before data collection, a two-hour training session was conducted by the researcher to two research assistants who have bachelor’s degree in nursing and data collection experience. The general information about the study aims and data collection procedure was introduced. Two research assistants were trained to recruit participants and administer the instrument with supervised practices until they were competent to collect the data independently.
A printed version of the questionnaire was given to perinatal women in obstetric clinics, maternity wards, and maternity schools. Data for phase I and phase II were collected in November to December 2020 and January to February 2021, respectively. Additionally, 30 of the participants from phase I were contacted again by telephone to fill out the questionnaires to evaluate the test–retest reliability. In order to limit the women's recall of previous answers and to reduce the possibility of participants' perception change, test–retest reliability was implemented 2 weeks after their original assessment [32].
Each questionnaire was number-coded (e.g., 1, 2, 3) once all perinatal women independently completed the anonymous questionnaire. Then, the questionnaires were checked and the validity was verified. A greater than 20% missing data rate rendered a questionnaire invalid, as well as a greater than 20% missing data rate or if all options were the same.
Psychometric testing of the scale
Item analysis
Item analysis was performed in accordance with the following principles: (1) extreme group comparison (meaning that items are able to discriminate between the upper 27% and lower 27% scoring groups [33]; and (2) item-total correlations (meaning that of the score of each item with the total score of the scale). We retained items that had a critical ratio greater than 3.0 or those with an item-total correlation from 0.30 to 0.80 [34].
Content validity
We evaluated two aspects of content validity: (1) item-level CVI (I-CVI); and (2) scale-level CVI (S-CVI). In accordance with Lynn [35], we considered an I-CVI ≥ 0.78 and an S-CVI ≥ 0.80 to be acceptable.
Construct validity
We used factor analysis to evaluate the construct validity of the PoDLiS-C. The normality was assessed by performing skewness and kurtosis statistics and inspecting Q-Q plot. The value of skewness less than 2 and the value of kurtosis less than 7 indicate that the data is normally distributed for the sample size larger than 300 [36]. The suitability of the factor analysis was assessed prior to the EFA using the Kaiser–Meyer–Olkin test and Bartlett’s test of sphericity. A Kaiser–Meyer–Olkin result ≥ 0.6 and a significant (p < 0.05) Bartlett’s test of sphericity would indicate the suitability of the scale for factor analysis [37]. Here, we divided the participants into two groups based on the data collection time for the EFA (n = 346) and CFA (n = 289).
Kaiser criterion (eigenvalue > 1.0) and parallel analysis were used to decide the number of factors to retain in EFA. Parallel analysis was more objective than scree plot and less arbitrary than Kaiser criterion (eigenvalue > 1.0) [38, 39]. Only initial eigenvalue that exceeded the eigenvalue from the parallel analysis were retained [38, 39]. Then, we performed the EFA with maximum likelihood method followed by a direct oblimin rotation to test the factor construct of all 31 items. A CFA was conducted to additionally assess the PoDLiS-C structure. The configural, measurement (in both measurement weights and measurement residuals) and structural invariance was tested based on two groups, which were participants in pregnancy period or postpartum period. The changes of CFI (△CFI) between the CFI value in unconstrained (configural) model and the CFI value for later three models less than 0.01 were acceptable [40]. The acceptable goodness-of-fit values were set at χ2/df < 3.0, RMSEA < 0.05, SRMR < 0.05, CFI > 0.9, and GFI > 0.9 [41]. Additionally, a factor loading of at least 0.3 is desirable in a CFA [30].
Reliability
We used McDonald’s omega coefficient to assess the internal consistency of the PoDLiS-C, which was considered satisfactory with omega coefficient exceeding 0.7 [42]. The intraclass correlation coefficient (ICC) and a two-way random model were used to assess test–retest reliability, which was considered satisfactory with an ICC exceeding 0.7.
Data analysis
All data analyses were conducted using SPSS ver. 24.0 and AMOS ver. 24.0. Two research assistants entered data and double-checked to ensure accurate data entry. Data cleaning was performed to ensure the validity of the data analysis. The frequency counts of categorical variables were checked to detect missing data. Participants with missing responses and unanswered items were eliminated from the data analysis. Frequency and percentages were used to describe the characteristics of the demographic information of the participants, while means ± standard deviations were used to report the continuous variables. A p value less than 0.05 was regarded as being significant.
Ethical considerations
Ethical approval for the study was received from the Yantai Yuhuangding Hospital Ethics Committee Ref: [2020] 283. The study was conducted according to the Declaration of Helsinki. All participants were informed of the aim of this study and had the right to refuse to participate or withdraw from the study without consequence. The written informed consent was obtained from the participants before starting the survey. All personal information and study data were kept strictly confidential. Hard copies of the data were stored in a locked cabinet, and electronic data were stored in a password-protected USB flash disk. Only the researcher could access the data.
Results
Characteristics of the participants
In the current study, 700 perinatal women (phase I: n = 400; phase II: n = 300) were recruited from November 2020 to February 2021, with 635 (phase I: n = 346; phase II: n = 289) completing the questionnaire according to the inclusion criteria, giving a response rate of 90.7%. The participants’ age ranged from 21 to 46 (31.79 ± 3.93) years. In general, most participants had a partner (97.5%), 69% had earned a specialty or bachelor’s degree, 78.1% were employed, 47.2% had a household monthly income > 1000 USD, 89.1% lived in urban areas, 92.3% were pregnant, and 2.7% had a history of depression. The participants’ sociodemographic characteristics are presented in Table 1.
Table 1.
Participant characteristics (n = 635)
| Variable | Frequency(n)/percentage(%) | ||
|---|---|---|---|
| Total (n = 635) |
Phase I (n = 346) |
Phase II (n = 289) |
|
| Age | |||
| 21–30 | 240 (37.8) | 128 (37.0) | 112 (38.8) |
| 31–40 | 375 (59.1) | 202 (58.4) | 173 (59.9) |
| 41–50 | 20 (3.1) | 16 (4.6) | 4 (1.4) |
| Marital status | |||
| With spouse | 619 (97.5) | 335 (96.8) | 284 (98.3) |
| Without spouse | 16 (2.5) | 11 (3.2) | 5 (1.7) |
| Educational status | |||
| Junior school or below | 26 (4.1) | 12 (3.5) | 14 (4.8) |
| High school/specialized secondary school | 107 (16.9) | 57 (16.5) | 50 (17.3) |
| Specialty/Bachelor | 438 (69.0) | 249 (72.0) | 189 (65.4) |
| Postgraduate or above | 64 (10.1) | 28 (8.1) | 36 (12.5) |
| Employment status | |||
| Employed | 496 (78.1) | 268 (77.5) | 228 (78.9) |
| Unemployed | 139(21.9) | 78 (22.5) | 61 (21.1) |
| Household monthly income (RMB) | |||
| < 2000 | 17 (2.7) | 6 (1.7) | 11 (3.8) |
| 2000–4000 | 116 (18.3) | 60 (17.3) | 56 (19.4) |
| 4001–6000 | 202 (31.8) | 112 (32.4) | 90 (31.1) |
| > 6000 | 300 (47.2) | 168 (48.6) | 132 (45.7) |
| Residence | |||
| Urban | 566 (89.1) | 304 (87.9) | 262 (90.7) |
| Rural | 69 (10.9) | 42 (12.1) | 27 (9.3) |
| Current status | |||
| Pregnancy period | 576(90.7) | 342 (98.8) | 234 (81.0) |
| Postpartum period | 59 (9.3) | 4 (1.2) | 55 (19.0) |
| The history of depression | |||
| Yes | 17 (2.7) | 5 (1.4) | 12 (4.2) |
| No | 618 (97.3) | 341 (98.6) | 277 (95.8) |
Item analysis
From the extreme group comparison, the critical ratio value of the 31 items was greater than 3.0. Subsequently, Pearson’s correlation was used to determine the correlation of the items with the total score. The results showed that all item scores were positively correlated with the total score of the scale and that the item-total correlation was between 0.40 and 0.61, with a statistically significant difference (Table 2).
Table 2.
Results of item analysis(31items)
| Item | CR | Item-total correlations | Cronbach’s α if item deleted | Note |
|---|---|---|---|---|
| Q1 | 8.980* | 0.552* | 0.892 | Retained |
| Q2 | 11.009* | 0.588* | 0.891 | Retained |
| Q3 | 11.765* | 0.576* | 0.892 | Retained |
| Q4 | 11.911* | 0.608* | 0.891 | Retained |
| Q5 | 8.675* | 0.609* | 0.891 | Retained |
| Q6 | 9.041* | 0.573* | 0.892 | Retained |
| Q7 | 9.215* | 0.469* | 0.894 | Retained |
| Q8 | 9.183* | 0.560* | 0.892 | Retained |
| Q9 | 8.047* | 0.556* | 0.892 | Retained |
| Q10 | 8.589* | 0.542* | 0.892 | Retained |
| Q11 | 9.781* | 0.572* | 0.892 | Retained |
| Q12 | 7.510* | 0.420* | 0.895 | Retained |
| Q13 | 9.155* | 0.566* | 0.892 | Retained |
| Q14 | 5.818* | 0.537* | 0.893 | Retained |
| Q15 | 6.936* | 0.490* | 0.893 | Retained |
| Q16 | 7.728* | 0.527* | 0.893 | Retained |
| Q17 | 9.013* | 0.532* | 0.893 | Retained |
| Q18 | 8.653* | 0.543* | 0.893 | Retained |
| Q19 | 7.887* | 0.447* | 0.894 | Retained |
| Q20 | 6.498* | 0.425* | 0.895 | Retained |
| Q21 | 6.400* | 0.430* | 0.894 | Retained |
| Q22 | 5.547* | 0.423* | 0.895 | Retained |
| Q23 | 7.280* | 0.435* | 0.894 | Retained |
| Q24 | 6.448* | 0.431* | 0.895 | Retained |
| Q25 | 7.161* | 0.446* | 0.894 | Retained |
| Q26 | 6.642* | 0.431* | 0.895 | Retained |
| Q27 | 7.086* | 0.410* | 0.895 | Retained |
| Q28 | 7.503* | 0.407* | 0.895 | Retained |
| Q29 | 8.407* | 0.434* | 0.894 | Retained |
| Q30 | 7.310* | 0.402* | 0.895 | Retained |
| Q31 | 8.215* | 0.408* | 0.895 | Retained |
*P < 0.01
Validity
Content validity
The results demonstrated that the I-CVI was between 0.8 and 1 and that the S-CVI was 0.968.
Construct validity
EFA was performed in the first-phase sample (n = 346) whose mean score of PoDLiS-C was 81.69 ± 12.80. The data satisfied the requirements of the normal distribution (skewness = 0.41 and kurtosis = 3.19). The Kaiser–Meyer–Olkin test value of 0.863 and the Bartlett record value of 5095.284 (p < 0.01) indicated the suitability of the PoDLiS-C for factor analysis.
By comparing with the initial eigenvalue and the eigenvalue from the parallel analysis, a six-factor structure was revealed, explaining 60.76% of the total variance. Therefore, maximum likelihood method with direct oblimin rotation was performed by extracting 6 factors (Tables 3 and 4). The extracted factors were given the following names: ability to recognize postpartum depression (Factor 1: item 1 to 6), knowledge of how to seek information related to PPD (Factor 2: item 27to 31), attitudes facilitating the identification of PPD and appropriate help-seeking (Factor 3: item 21 to 26), knowledge and beliefs concerning the available professional help for PPD (Factor 4: item 17 to 20), knowledge of PPD risk factors and causes (Factor 5: item 7 to 11), and knowledge and beliefs of PPD self-care activities (Factor 6: item 12 to 16).
Table 3.
Pattern Matrix for the Maximum Likelihood Analysis with Direct Oblimin Rotation of the 6-Facor Solution the PoDLiS-C (n = 346)
| Items | Factors | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Q1 Feeling unusually sad and teary may be a symptom of postpartum depression | 0.653 | |||||
| Q2 Sleeping too much or too little may be a sign of postpartum depression | 0.859 | |||||
| Q3 Eating too much or losing appetite may be a sign of postpartum depression | 0.852 | |||||
| Q4 Losing interest and joy in activities may be a symptom of postpartum depression | 0.660 | |||||
| Q5 Postpartum depression affects person’s memory and concentration | 0.391 | |||||
| Q6 Symptoms and signs of postpartum depression last for at least two weeks | 0.411 | |||||
| Q7 How likely is postpartum depression caused by problems related to gene or heredity? | 0.578 | |||||
| Q8 How likely is postpartum depression caused by stressful circumstances in life (e.g. death of a family member or divorce)? | 0.852 | |||||
| Q9 How likely is postpartum depression caused by the lack of social support (e.g. support from intimate partner)? | 0.700 | |||||
| Q10 How likely is postpartum depression caused by a previous history of depression? | 0.697 | |||||
| Q11 How likely is postpartum depression caused by a hormonal imbalance? | 0.624 | |||||
| Q12 Physical activity is effective in the prevention or management of postpartum depression | 0.558 | |||||
| Q13 Seeking help with tasks like baby care and housework from intimate partners and family members is helpful for the prevention or management of postpartum depression | 0.598 | |||||
| Q14 Religious practices, prayer and going to church are helpful for prevention or management of postpartum depression | 0.637 | |||||
| Q15 Balanced diet is helpful for the prevention or management of postpartum depression | 0.604 | |||||
| Q16 Good sleep is helpful for the prevention or management of postpartum depression | 0.632 | |||||
| Q17 Mental health professionals can treat postpartum depression effectively | 0.376 | |||||
| Q18 Psychotherapy (e.g. talk therapy or consultation) can effectively treat postpartum depression | 0.447 | |||||
| Q19 Antidepressants can be addictive | 0.871 | |||||
| Q20 Antidepressants can cause brain damage | 0.746 | |||||
| Q21 I would rather endure postpartum depression than suffer from mental treatment | 0.669 | |||||
| Q22 Although there are clinics for women with postpartum depression, I distrust them | 0.736 | |||||
| Q23 Most women with postpartum depression are violent | 0.448 | |||||
| Q24 It is best to avoid women with postpartum depression so that the problem will not happen to you | 0.656 | |||||
| Q25 If I have postpartum depression, I won’t tell anyone | 0.796 | |||||
| Q26 I’m worried about what my family and/or friends think about me because of my appointment in the psychology and/or psychiatric department | 0.659 | |||||
| Q27 I know where to find the information about postpartum depression | -0.447 | |||||
| Q28 I know how to use various resources to search for information | -0.586 | |||||
| Q29 I can appraise the accuracy of information about postpartum depression on the radio and television | -0.952 | |||||
| Q30 I can appraise the accuracy of information about postpartum depression on the Internet | -0.940 | |||||
| Q31 I can appraise the accuracy of the suggestions about postpartum depression given by friends and families | -0.782 | |||||
| % of the variance | 25.224 | 10.418 | 9.578 | 5.828 | 5.207 | 4.501 |
| Cumulative variance | 25.224 | 35.642 | 45.220 | 51.048 | 56.255 | 60.757 |
Table 4.
Structure Matrix for the Maximum Likelihood Analysis with Direct Oblimin Rotation of the 6-Facor Solution the PoDLiS-C (n = 346)
| Items | Factors | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Q1 Feeling unusually sad and teary may be a symptom of postpartum depression | 0.699 | |||||
| Q2 Sleeping too much or too little may be a sign of postpartum depression | 0.809 | |||||
| Q3 Eating too much or losing appetite may be a sign of postpartum depression | 0.814 | |||||
| Q4 Losing interest and joy in activities may be a symptom of postpartum depression | 0.734 | |||||
| Q5 Postpartum depression affects person’s memory and concentration | 0.603 | |||||
| Q6 Symptoms and signs of postpartum depression last for at least two weeks | 0.568 | |||||
| Q7 How likely is postpartum depression caused by problems related to gene or heredity? | 0.574 | |||||
| Q8 How likely is postpartum depression caused by stressful circumstances in life (e.g. death of a family member or divorce)? | 0.833 | |||||
| Q9 How likely is postpartum depression caused by the lack of social support (e.g. support from intimate partner)? | 0.744 | |||||
| Q10 How likely is postpartum depression caused by a previous history of depression? | 0.709 | |||||
| Q11 How likely is postpartum depression caused by a hormonal imbalance? | 0.701 | |||||
| Q12 Physical activity is effective in the prevention or management of postpartum depression | 0.551 | |||||
| Q13 Seeking help with tasks like baby care and housework from intimate partners and family members is helpful for the prevention or management of postpartum depression | 0.682 | |||||
| Q14 Religious practices, prayer and going to church are helpful for prevention or management of postpartum depression | 0.699 | |||||
| Q15 Balanced diet is helpful for the prevention or management of postpartum depression | 0.656 | |||||
| Q16 Good sleep is helpful for the prevention or management of postpartum depression | 0.687 | |||||
| Q17 Mental health professionals can treat postpartum depression effectively | 0.496 | |||||
| Q18 Psychotherapy (e.g. talk therapy or consultation) can effectively treat postpartum depression | 0.563 | |||||
| Q19 Antidepressants can be addictive | 0.846 | |||||
| Q20 Antidepressants can cause brain damage | 0.760 | |||||
| Q21 I would rather endure postpartum depression than suffer from mental treatment | 0.706 | |||||
| Q22 Although there are clinics for women with postpartum depression, I distrust them | 0.729 | |||||
| Q23 Most women with postpartum depression are violent | 0.513 | |||||
| Q24 It is best to avoid women with postpartum depression so that the problem will not happen to you | 0.667 | |||||
| Q25 If I have postpartum depression, I won’t tell anyone | 0.788 | |||||
| Q26 I’m worried about what my family and/or friends think about me because of my appointment in the psychology and/or psychiatric department | 0.670 | |||||
| Q27 I know where to find the information about postpartum depression | -0.499 | |||||
| Q28 I know how to use various resources to search for information | -0.612 | |||||
| Q29 I can appraise the accuracy of information about postpartum depression on the radio and television | -0.928 | |||||
| Q30 I can appraise the accuracy of information about postpartum depression on the Internet | -0.917 | |||||
| Q31 I can appraise the accuracy of the suggestions about postpartum depression given by friends and families | -0.768 | |||||
| % of the variance | 25.224 | 10.418 | 9.578 | 5.828 | 5.207 | 4.501 |
| Cumulative variance | 25.224 | 35.642 | 45.220 | 51.048 | 56.255 | 60.757 |
PoDLiS-C Chinese version of postpartum depression literacy scale
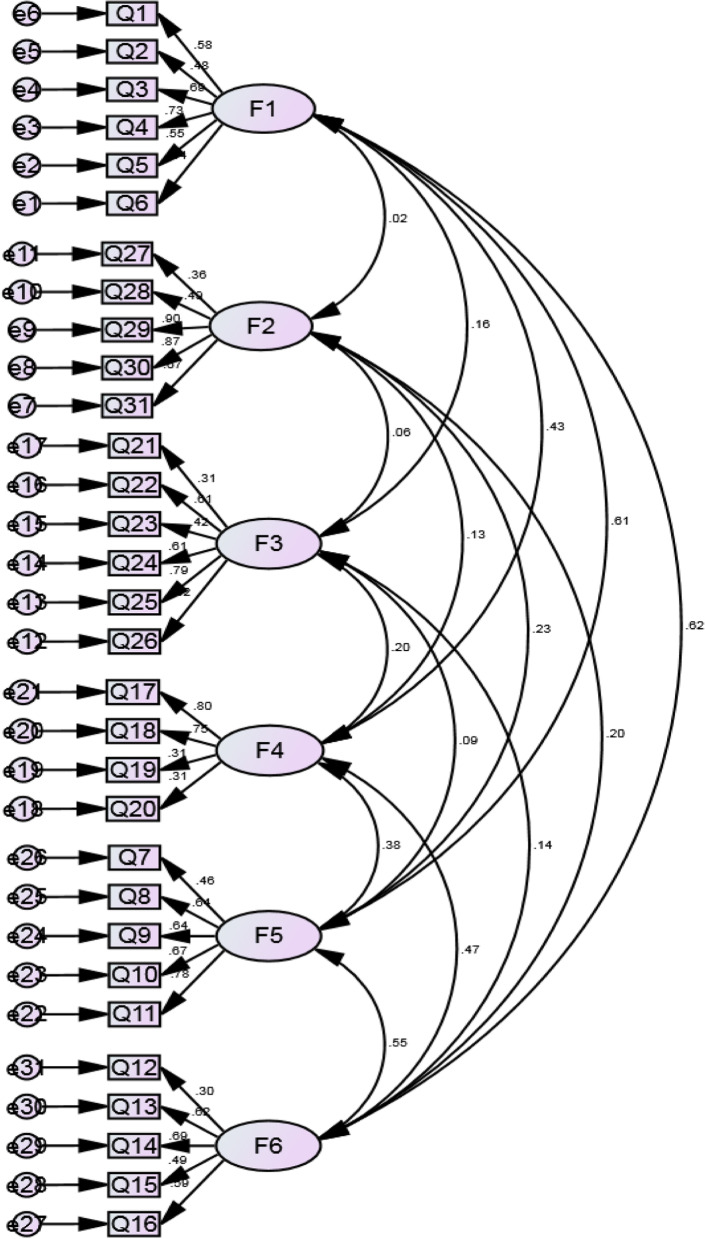
In accordance with the EFA results, a CFA was performed to verify the six-factor model. Compared with the one-factor model (χ2 = 1541.567, df = 434), the six-factor model (χ2 = 420.389, df = 419) appeared significant decrease of goodness-of-fit. The CFA obtained the following values: likelihood ratio (χ2/df), 1.003; RMSEA, 0.003; SRMR, 0.0478; GFI, 0.916; adjusted GFI, 0.901; IFI, 0.999; Tucker-Lewis index, 0.999; and CFI, 0.999 (Table 5). The CFA results suggested that the goodness-of-fit of the model of the model was acceptable (Fig. 2). As shown in Table 6, comparing with the CFI value of the unconstrained model, the changes of CFI (△CFI) in the models obtained by constraining (measurement weights, structural covariances and measurement residual) were less than 0.01. Therefore, the configural, measurement and structural invariance were ensured in this measurement model.
Table 5.
Goodness of fit indices for the six-factor model in confirmatory factor analysis (n = 289)
| χ2 | df | χ2/df | RMSEA | SRMR | GFI | AGFI | IFI | TLI | CFI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Criterion | < 3 | < 0.05 | < 0.05 | > 0.90 | > 0.90 | > 0.90 | > 0.90 | > 0.90 | ||
| Result | 420.389 | 419 | 1.003 | 0.003 | 0.0478 | 0.916 | 0.901 | 0.999 | 0.999 | 0.999 |
χ2 Chi-square, df Degrees of freedom, χ2/df Normed chi-square, RMSEA Root mean square error of approximation, SRMR Standardized root mean square residual, GFI Goodness-of-fit index, AGFI Adjusted goodness-of-fit index, IFI Incremental fit index, TLI Tucker-Lewis index, CFI Comparative fit index
Fig. 2.
Results of confirmatory factor analysis
Table 6.
Configural, measurement and structural invariance results by participants in pregnancy period or postpartum period
| Model | χ2 | df | χ2/df | RMSEA | SRMR | GFI | AGFI | IFI | TLI | CFI | △CFI |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unconstrained (Configural) | 1053.589 | 838 | 1.257 | 0.030 | 0.0527 | 0.834 | 0.803 | 0.911 | 0.897 | 0.907 | |
| Measurement weights | 1078.421 | 863 | 1.250 | 0.029 | 0.0529 | 0.831 | 0.805 | 0.910 | 0.900 | 0.907 | 0.000 |
| Structural covariances | 1095.188 | 884 | 1.239 | 0.029 | 0.0540 | 0.831 | 0.810 | 0.911 | 0.904 | 0.909 | 0.002 |
| Measurement residuals | 1144.184 | 915 | 1.250 | 0.030 | 0.0545 | 0.819 | 0.804 | 0.902 | 0.900 | 0.901 | 0.006 |
Reliability
The results showed the omega coefficient of the PoDLiS-C of 0.894 and obtained coefficients for the six subscales of 0.865, 0.870, 0.838, 0.777, 0.837 and 0.794, respectively (Table 7). Furthermore, the PoDLiS-C subscale internal consistency was determined to be good and not to benefit from the removal of additional items (Table 2). Therefore, all 31 items were temporarily retained. Moreover, the test–retest reliability test had a coefficient of 0.874.
Table 7.
Results of internal consistency
| Subscales | Items | Omega coefficient | Cronbach’α |
|---|---|---|---|
| 1. Ability to recognize postpartum depression (item 1 to 6) | 6 | 0.865 | 0.861 |
| 2. Knowledge of how to seek information related to postpartum depression (item 27 to 31) | 5 | 0.870 | 0.872 |
| 3. Attitudes which facilitate recognition of postpartum depression and appropriate help-seeking (item 21 to 26) | 6 | 0.838 | 0.835 |
| 4. Knowledge and beliefs about professional help available (item 17 to 20) | 4 | 0.777 | 0.770 |
| 5. Knowledge of risk factors and causes (item 7 to 11) | 5 | 0.837 | 0.834 |
| 6. Knowledge and beliefs of self-care activities (item 12 to 16) | 5 | 0.794 | 0.791 |
| PoDLiS-C scale | 31 | 0.894 | 0.896 |
PoDLis-C The postpartum depression literacy scale-Chinese version
Discussion
As a common psychological disorder, PPD has serious adverse effects on the mother, newborn, and family. PPD literacy is critically linked to the identification of PPD and to the help-seeking process [42]. The purpose of the current research was to translate, culturally adapt, and psychometrically evaluate the PoDLiS for China. In general, the PoDLiS-C was determined to be practicable in a domestic context and could be widely used to evaluate the PPD literacy of perinatal women.
The extreme group comparison results showed that the critical ratio values of the items ranged from 6.40 to 11.911. Thus, all were greater than 3.000 and were significant (p < 0.01). Moreover, the 95% confidence intervals of all items in the two groups did not include 0, indicating that the PoDLiS-C items could well identify the PPD literacy level of perinatal women. The item-total correlations were all between 0.40 and 0.61 and were significant, indicating a strong relationship to the total scale and thereby showing the relative homogeneity of these items.
In terms of content validity, the S-CVI of the PoDLiS-C was 0.968, which is higher than 0.8, and the I-CVI values were 0.8–1.0, all of which were greater than 0.78, suggesting that the content validity of the scale is satisfactory and that the item content is in good accordance with the conceptual framework. It is consistent with the content validity index of the original scale [26] and higher than the Content validity of PoDLiS in Malaysian [43] which may be related to the reason that the participates in this part are mostly pregnant women and parturients within one year after delivery, and the per capita monthly income of the family is mostly medium and high level, while the participates in Malaysia are parturients within 6 months after delivery. Household per capita monthly income is mostly associated with low and medium levels.
The seven dimensions of the original scale have not been empirically confirmed by EFA. However, the results of pattern matrix and structure matrix for the maximum likelihood analysis with direct oblimin rotation showed that the scale had six dimensions, one less than the original scale. The 7-factor model in Iran explained approximately 49% of the total variance [26], and ours comparably 60.76% of the variability. Although the factor loading value of item 5 and 17 was 0.391 and 0.376 respectively, this item was retained, given the influence of this item on the representativeness and structure of the scale.
CFA results indicated that the six-dimension structure of the PoDLiS-C yielded a largely acceptable fit for our data, with all factor loadings exceeding 0.30. Meanwhile, the dimension distribution of all items was appropriate and all items were positively related to each dimension. The six-dimension structure was more consistent with Jorm's six-factor model of MHL. This may be due to the different cultural backgrounds as well as the differences in the understanding of PPD literacy in perinatal women. Additionally, different survey samples may yield different statistical analysis results. Compared with the original research, the participants included in the current study had a higher education level and may have a stronger understanding of the value of seeking professional help. As a whole, the results of this study suggest that the PoDLiS-C model is suitable for future research work in China.
The omega coefficient was 0.894 for the overall scale and was between 0.777 and 0.870 for each subscale. These values were determined by EFA to be better than those of the original English-language scale, indicating the internal consistency reliability of the PoDLiS-C. The test–retest reliability was 0.874, showing that the stability of the PoDLiS-C was satisfactory.
The reliability and validity of the PoDLiS-C were both identified in this study. The results suggested that the scale can be used as an assessment tool for evaluating PPD literacy in Chinese perinatal women. Although the original scale has been modified in several places, all of the revisions were based on the advice of experts and were made with consideration of the Chinese cultural background. Therefore, the current instrument is more fitting for Chinese perinatal women. Community workers and healthcare providers can apply this instrument to assess the PPD literacy of perinatal women, to identify poor PPD literacy in individuals, and to design targeted interventions and public health measures in order to help to raise the public awareness of PPD and to promote the help-seeking behavior of perinatal women.
In particular, the cut-off value of the PoDLiS-C is crucial for assessing the PPD literacy of perinatal women. Future research should focus on this and develop a scientific and reasonable value to help to pinpoint women who have low PPD literacy.
Limitations
Despite the satisfactory results, the current study has some limitations. First, the participants were recruited using convenience sampling from two hospitals of the same level in Yantai City, Shandong Province, China. Therefore, the application of these results may be limited to those who seek healthcare at hospitals of this particular level, because the PPD literacy in perinatal women may vary widely at different hospital levels. Additionally, over half of the subjects were urban dwellers and had at least a specialty or bachelor’s degree. Therefore, our results are not representative of all perinatal women in China. Second, this work was performed at a single time point. Therefore, whether the tool is able to longitudinally predict outcomes remains to be seen. Third, because dropout and responsiveness analyses were not determined, we could not summarize the characteristics of perinatal women with invalid questionnaires. Fourth, the current study evaluated the reliability and validity of the PoDLiS-C. However, further assessments of the level of PPD literacy were not conducted. In addition, there was a detailed analysis of the factors influencing the results, such as the general self-efficacy and perceived social support. Therefore, it is necessary to further verify the PoDLiS-C level in a diverse population and identify its influencing factors.
Conclusions
To our knowledge, this is the first scale tailored to measure the PPD literacy of perinatal women in mainland China. Our findings provide evidence supporting the reliability and validity of the PoDLiS-C. Nonetheless, the PoDLiS-C and the original English scale have different factor structures. Therefore, we suggest that the sample size be increased for further reliability and validity testing. Due to the good psychometric characteristics of the scale in the current study, the PoDLiS-C has been demonstrated to be a credible and valuable instrument for enhancing the knowledge of PPD literacy as well as for boosting future investigations of PPD literacy during the perinatal period in Chinese-speaking populations.
Acknowledgements
We are grateful to Ali Montazeri and Fatemeh Mirsalimi for authorizing us to use the English version of the Postpartum Depression Literacy Scale. Furthermore, we would like to express the gratitude to the experts and perinatal women who participated in this study.
Abbreviations
- PPD
Postpartum Depression
- MHL
Mental Health Literacy
- MHLS
Mental Health Literacy Scale
- PoDLis
The Postpartum Depression Literacy Scale
- PoDLiS-C
Chinese version of postpartum depression literacy scale
- EFA
Exploratory factor analysis
- CFA
Confirmatory factor analysis
- CR
Critical ratio
- I-CVI
Item-level content validity index
- S-CVI
Scale-level content validity index
- ICC
Intraclass correlation coefficient
- RMSEA
Root mean square error of approximation
- SRMR
Standardized root mean square residual
- GFI
Goodness-of-fit index
- AGFI
Adjusted goodness-of-fit index
- IFI
Incremental fit index
- TLI
Tucker-Lewis index
- CFI
Comparative fit index
Authors’ contributions
WH, XL planed and designed the experiments. WH,ZW and NJ performed the experiments. WH and XZ analyzed and data. WH wrote the primary manuscript. All authors read and approved the final version of the manuscript.
Funding
The study is part of the results of the first author’s doctor’s thesis in nursing, which was financially supported by China Medical University. The study was also supported by Medical and health plan of Shandong Province No. 2018WS032.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Yan Tai Yuhuangding Hospital ( Approval ID: [2020]283). Participants were informed that the survey was anonymous and that all data were kept strictly confidential and used for scientific research only. Therefore, patients could express their true thoughts without the fear of jeopardizing treatment. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Qi W, Zhao F, Liu Y, Li Q, Hu J. Psychosocial risk factors for postpartum depression in Chinese women: a meta-analysis. BMC Pregnancy Childbirth. 2021;21(1):174. doi: 10.1186/s12884-021-03657-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Battle DE. Diagnostic and Statistical Manual of Mental Disorders (DSM) Codas. 2013;25(2):191–192. doi: 10.1590/s2317-17822013000200017. [DOI] [PubMed] [Google Scholar]
- 3.Chang HP, Chen JY, Huang YH, Tyan JY, Yeh CJ, Su PH, Chin-Hung CV. Prevalence and factors associated with depressive symptoms in mothers with infants or toddlers. Pediatr Neonatol. 2014;55(6):470–479. doi: 10.1016/j.pedneo.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 4.Recto P, Champion JD. Assessment of Mental Health Literacy among Perinatal Hispanic Adolescents. Issues Ment Health Nurs. 2017;38(12):1030–1038. doi: 10.1080/01612840.2017.1349224. [DOI] [PubMed] [Google Scholar]
- 5.Selix NW, Goyal D. Recent Policy Changes in Perinatal Depression Screening and Treatment. JNP J Nurs Pract. 2018;14(2):117–123. doi: 10.1016/j.nurpra.2017.11.016. [DOI] [Google Scholar]
- 6.Coast E, Leone T, Hirose A, Jones E. Poverty and postnatal depression: a systematic mapping of the evidence from low and lower middle income countries. Health Place. 2012;18(5):1188–1197. doi: 10.1016/j.healthplace.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-analysis, and Meta-Regression of 291 Studies from 56 Countries. Front Psychiatry. 2018;8:248. doi: 10.3389/fpsyt.2017.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J Psychiatr Research. 2018;104:235–248. doi: 10.1016/j.jpsychires.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shidhaye P, Giri P. Maternal depression: a hidden burden in developing countries. Ann Med Health Sci Res. 2014;4(4):463–465. doi: 10.4103/2141-9248.139268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng A-W, Xiong R-B, Jiang T-T, Luo Y-P, Chen W-Z. Prevalence and risk factors of postpartum depression in a population- based sample of women in Tangxia Community, Guangzhou. Asian Pac J Trop Med. 2014;7(3):244–249. doi: 10.1016/S1995-7645(14)60030-4. [DOI] [PubMed] [Google Scholar]
- 12.Mu T-Y, Li Y-H, Pan H-F, Zhang L, Zha D-H, Zhang C-L, Xu R-X. Postpartum depressive mood (PDM) among Chinese women: a meta-analysis. Archives of Womens Mental Health. 2019;22(2):279–287. doi: 10.1007/s00737-018-0885-3. [DOI] [PubMed] [Google Scholar]
- 13.Roomruangwong C, Epperson CN. Perinatal depression in Asian women: prevalence, associated factors, and cultural aspects. Asian Biomedicine. 2011;5(2):179–193. doi: 10.5372/1905-7415.0502.024. [DOI] [Google Scholar]
- 14.Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 15.Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt). 2012;21(8):830–836. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi W, Shen Z, Wang S, Hall BJ. Barriers to Professional Mental Health Help-Seeking Among Chinese Adults: A Systematic Review. Front Psychiatry. 2020;11:442. doi: 10.3389/fpsyt.2020.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fonseca A, Gorayeb R, Canavarro MC. Womens help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery. 2015;31(12):1177–1185. doi: 10.1016/j.midw.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Fonseca A, Silva S, Canavarro MC. Depression Literacy and Awareness of Psychopathological Symptoms During the Perinatal Period. J Obstet Gynecol Neonatal Nurs. 2017;46(2):197–208. doi: 10.1016/j.jogn.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Fonseca A, Moura-Ramos M, Canavarro MC. Attachment and Mental Help-Seeking in the Perinatal Period: The Role of Stigma. Community Ment Health J. 2018;54(1):92–101. doi: 10.1007/s10597-017-0138-3. [DOI] [PubMed] [Google Scholar]
- 20.Jorm AF. Mental health literacy. Public knowledge and beliefs about mental disorders. Br J psychiatry: J Mental Sci. 2000;177:396–401. doi: 10.1192/bjp.177.5.396. [DOI] [PubMed] [Google Scholar]
- 21.Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–243. doi: 10.1037/a0025957. [DOI] [PubMed] [Google Scholar]
- 22.Wei Y, McGrath PJ, Hayden J, Kutcher S. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry. 2015;15:291. doi: 10.1186/s12888-015-0681-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aluh DO, Anyachebelu OC, Anosike C, Anizoba EL. Mental health literacy: what do Nigerian adolescents know about depression? Int J Ment Health Syst. 2018;12:8. doi: 10.1186/s13033-018-0186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reddy C, Malik YK, Singh M, Jindal A, Shukla S, Singh SM. Mental health literacy and familiarity with the term schizophrenia in a community health care setting in North India. Asian J Psychiatr. 2021;55:102528. doi: 10.1016/j.ajp.2020.102528. [DOI] [PubMed] [Google Scholar]
- 25.Wickstead R, Furnham A. Comparing mental health literacy and physical health literacy: an exploratory study. J Ment Health. 2017;26(5):449–456. doi: 10.1080/09638237.2017.1294743. [DOI] [PubMed] [Google Scholar]
- 26.Mirsalimi F, Ghofranipour F, Noroozi A, Montazeri A. The postpartum depression literacy scale (PoDLiS): development and psychometric properties. BMC Pregnancy Childbirth. 2020;20(1):13. doi: 10.1186/s12884-019-2705-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ransing R, Kukreti P, Deshpande S, Godake S, Neelam N, Raghuveer P, Mahadevaiah M, Kataria D, Patil S, Puri M, et al. Perinatal depression-knowledge gap among service providers and service utilizers in India. Asian J Psychiatr. 2020;47:101822. doi: 10.1016/j.ajp.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Branquinho M, Canavarro MC, Fonseca A. Knowledge and attitudes about postpartum depression in the Portuguese general population. Midwifery. 2019;77:86–94. doi: 10.1016/j.midw.2019.06.016. [DOI] [PubMed] [Google Scholar]
- 29.Jaffe A, Redpath DP. Measurement theory in action: Case studies and exercises. Struct Equ Modeling Multidiscip J. 2006;13(4):646–648. doi: 10.1207/s15328007sem1304_8. [DOI] [Google Scholar]
- 30.Marsh HW, Hau KT, Balla JR, Grayson D. Is More Ever Too Much? The Number of Indicators per Factor in Confirmatory Factor Analysis. Multivariate Behav Res. 1998;33(2):181–220. doi: 10.1207/s15327906mbr3302_1. [DOI] [PubMed] [Google Scholar]
- 31.Chen L, Huang F, Yuan X, Song J, Chen L. An Assessment of the Reliability and Factorial Validity of the Chinese Version of the Health Professional Education in Patient Safety Survey (H-PEPSS) Front Psychol. 2019;10:2183. doi: 10.3389/fpsyg.2019.02183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matza LS, Van Brunt DL, Cates C, Murray LT. Test-retest reliability of two patient-report measures for use in adults with ADHD. J Atten Disord. 2011;15(7):557–563. doi: 10.1177/1087054710372488. [DOI] [PubMed] [Google Scholar]
- 33.Odukoya JA, Adekeye O, Igbinoba AO, Afolabi A. Item analysis of university-wide multiple choice objective examinations: the experience of a Nigerian private university. Qual Quant. 2018;52(3):983–997. doi: 10.1007/s11135-017-0499-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thoyre SM, Pados BF, Park J, Estrem H, McComish C, Hodges EA. The Pediatric Eating Assessment Tool: Factor Structure and Psychometric Properties. J Pediatr Gastroenterol Nutr. 2018;66(2):299–305. doi: 10.1097/MPG.0000000000001765. [DOI] [PubMed] [Google Scholar]
- 35.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–385. doi: 10.1097/00006199-198611000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth. 2019;22(1):67–72. doi: 10.4103/aca.ACA_157_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frank C, Asp M, Fridlund B, Baigi A. Questionnaire for patient participation in emergency departments: development and psychometric testing. J Adv Nurs. 2011;67(3):643–651. doi: 10.1111/j.1365-2648.2010.05472.x. [DOI] [PubMed] [Google Scholar]
- 38.Fabrigar LR. Exploratory Factor Analysis. Oxford: Oxford University Press; 2012. [Google Scholar]
- 39.O'Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and velicer's MAP test. Behav Res Methods Instrum Comput. 2000;32(3):396–402. doi: 10.3758/BF03200807. [DOI] [PubMed] [Google Scholar]
- 40.Tan Ş, Pektaş S. Examining the invariance of a measurement model by using the covariance structure approach. Int J Contemp Educ Res. 2020;7(2):27–39. [Google Scholar]
- 41.Qu J, Zhu Y, Cui L, Yang L, Lai Y, Ye X, Qu B. Psychometric properties of the Chinese version of the TeamSTEPPS teamwork perceptions questionnaire to measure teamwork perceptions of Chinese residents: a cross-sectional study. BMJ Open. 2020;10(11):e039566. doi: 10.1136/bmjopen-2020-039566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Viladrich C, Angulo-Brunet A, Doval E. A journey around alpha and omega to estimate internal consistency reliability. Ann Psychol. 2017;33(3):755–782. [Google Scholar]
- 43.O'Connor M, Casey L. The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. 2015;229(1–2):511–516. doi: 10.1016/j.psychres.2015.05.064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.