Abstract
Background
Impaction of mandibular third molars (M3) is one of the most common diseases. Extraction of M3 usually exacerbates osseous defects at the distal aspect of the adjacent second molar (M2). BonMaker® ATB has been cited as a novel autogenous bone grafting material. The aim of this pilot study was to introduce a novel method for repairing the distal osseous defects of M2 after the surgical removal of M3 with autogenous tooth graft powder (ATGP).
Method
A total of five patients were enrolled in this prospective split-mouth clinical pilot study. Four impacted wisdom teeth were extracted bilaterally from each patient with proximal alveolar bone loss ≥ 5 mm of M3. The ATGP was prepared chairside from two extracted one side third molars and randomly implanted in one of the M3 extraction sockets, and the other side was treated with a blank and considered the control site. Patients were followed up at 6 months.
Results
The five patients included three males and two females. Their ages ranged from 25 to 30 years, with a median of 27 years. Primary wound healing without complications was achieved in all the patients. There was a greater tendency for swelling of the cheeks and trismus to occur at the experimental site on the third postoperative day. Compared with the control site, the experimental site exhibited progressive bone filling and ossification in the sixth postoperative month. Moreover, the probing pocket depth of the experimental site was lower than that of the control site.
Conclusion
The results of this study demonstrate that ATGP effectively and economically repairs distal osseous defects of M2. Further study is required to validate the effectiveness with a larger study population.
Keywords: Impacted third molars, Autogenous tooth bone graft powder, Alveolar bone repair
Introduction
Impaction of mandibular third molars (M3) is one of the most common diseases, and the impaction rates range from 66 to 77% [1]. M3 generally gives rise to pericoronitis, maxillofacial space infection, odontogenic neoplastic changes, periodontitis, caries, and root resorption of adjacent second molars (M2) [2]. Extraction of M3 usually exacerbates alveolar bone resorption at the distal aspect of M2. Early studies showed that more than 40% of M3 cases presented probing pocket depth (PPD) ≥ 7 mm at the distal aspect of M2, and 33% of these study populations demonstrated worsening of the periodontal condition at the 2-year follow-up, with an increased PPD of at least 2 mm [3, 4]. Severe alveolar bone resorption eventually leads to the loss of M2. Therefore, early surgical removal of M3 plays an important role in the prevention of proximal alveolar bone loss [5].
Over the past three decades, extensive studies have investigated various methods to prevent and repair alveolar bone loss in order to improve the periodontal status of M2 after M3 extraction [6]. Compared with periodontal treatment and membrane placement, alveolar reconstructive procedures have demonstrated greater efficacy in inducing and accelerating bone regeneration. Bone graft substitutes include autogenous bone, mostly from mandible bone, allograft bone, synthetic bone and tissue engineered bone [7–10]. Platelet-rich plasma and platelet-rich fibrin combined with resorbable membranes have been shown to be effective alternative solutions [11, 12]. However, there is no therapeutic consensus algorithm. None of the existing repair methods are widely accepted and used as mainstream modalities in clinical practice because of their disadvantages, such as osteogenic instability, high cost and traumatic nature [6].
There is growing evidence for the use of autogenous tooth bone graft materials in alveolar bone reconstruction and bone augmentation, and this approach has achieved promising results [13–17]. Autogenous tooth bone graft materials have demonstrated the ideal characteristics of osteoconductivity, osteoinductivity, and osteogenicity, and these materials produce a nearly gold-standard graft and have low technique sensitivity [13, 18, 19]. BonMaker® ATB is a novel autogenous bone grafting material produced by the mechanical and chemical processing of natural teeth [15]. The aim of this pilot study was to introduce a novel method for repairing the distal osseous defects of M2 after the surgical removal of M3 with ATGP.
Materials and methods
Study design
This is a prospective split-mouth small sample observational clinical pilot study. Four impacted wisdom teeth were extracted bilaterally from each patient with proximal alveolar bone loss ≥ 5 mm of M3. The ATGP was prepared onsite from two extracted one side third molars and randomly implanted in one of the M3 extraction sockets (experimental site), and the other side was treated with a blank and was considered the control site. Patients were followed up at six months. The institutional review board of Shanghai Stomatological Hospital & School, Fudan University, China, approved the study.
Patients
From May 2021 to July 2021, five consecutive patients who had four third molars that needed to be extracted and were treated at the Department of Oral & Maxillofacial Surgery, Shanghai Stomatological Hospital and School, Fudan University, were enrolled. Inclusion criteria: (1) symmetrical proximal alveolar bone loss ≥ 5 mm of M3; (2) no history of systemic diseases, infectious diseases or genetic diseases; (3) no contraindications to conventional tooth extraction; (4) age of 25–30 years with good oral hygiene; (5) no history of drinking alcohol and smoking; and (6) no history of any other drug use. (7) Patients with proximal alveolar bone resorption of M3 found on oral examination and require M3 extraction. Exclusion Criteria: (1) M3 with severe pericoronitis and acute pulpitis that have not been effectively controlled; (2) pregnant or breastfeeding; and (3) M2 with periapical inflammation, crowding, ectasia, and torsion.
Surgical procedure
The enrolled patients were informed of the details of the procedures and nature of the study itself, and then, the patients signed an informed consent form. Complete medical and dental histories were obtained, and preoperative radiographic evaluation was performed with panoramic radiographs and cone-beam computed tomography (CBCT). Surgical extraction and ATGP implantation were performed by two surgeons (W. A. & Y–Z. C.) under local anesthesia with articaine 4% and epinephrine 1:100,000 (Ultracain, Sanofi Aventis, Paris, France). A triangular flap was applied uniformly, and a full thickness mucoperiosteal flap was flipped to expose M3. Minimally invasive extraction, debridement and root planing were performed consecutively. The ATGP was prepared onsite as previously described according to the manufacturer’s instructions (Z. Y. & H. Y.) (Fig. 1) [15]. The M3 extraction socket was filled and compacted in layers with freshly prepared ATGP. After the placement of a rubber drainage strip, the mucoperiosteal flap was repositioned and closed tightly with interrupted sutures. Antibiotics were routinely used for one week after surgery combined with 10 mg prednisone for three days. Continuous icing was arranged for 48 h after surgery. Patients were re-evaluated one week postoperatively, and the sutures were removed. Postoperative follow-up exams were scheduled at six months (H.F-K.).
Fig. 1.
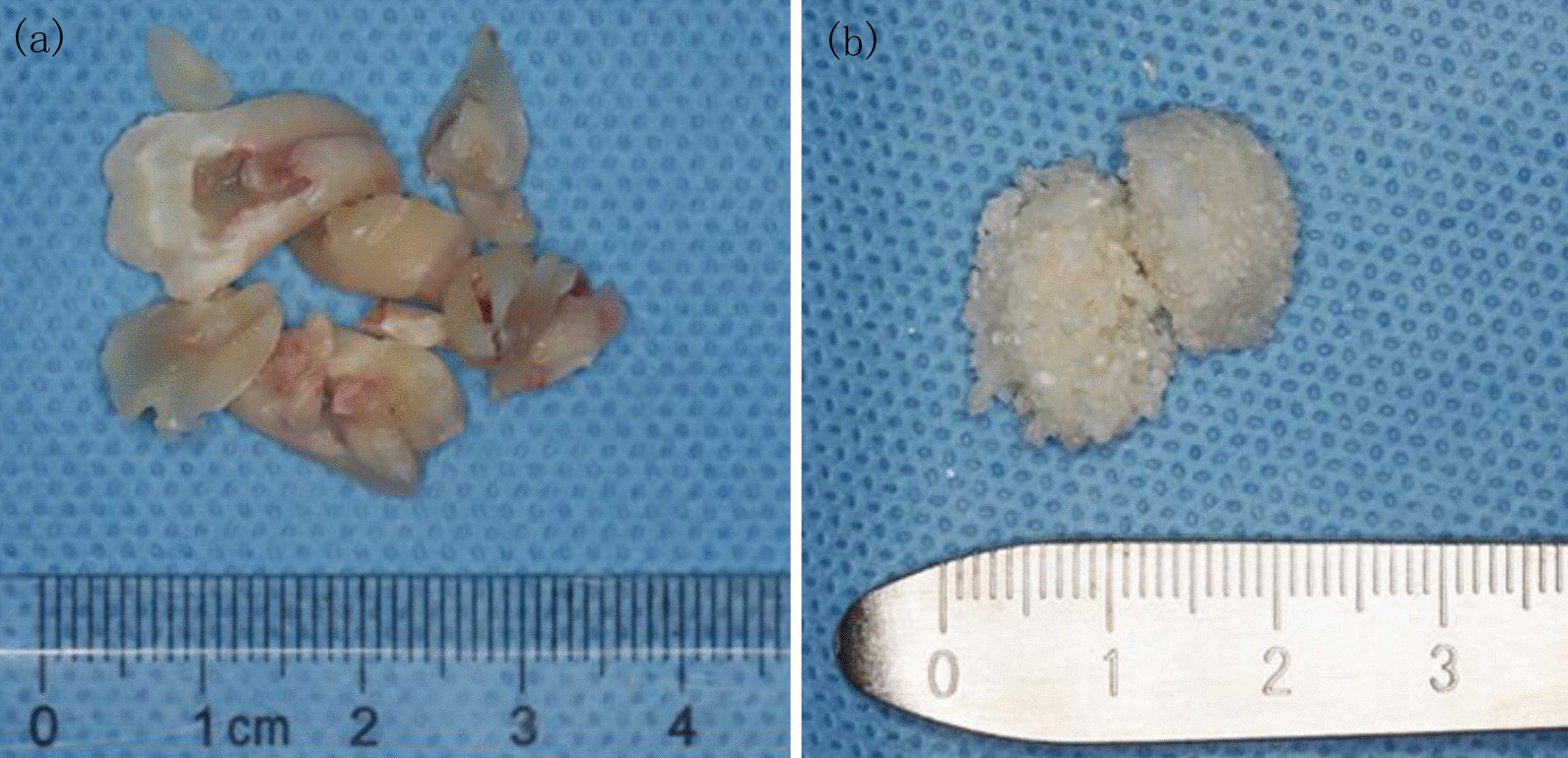
a Cleaned and dried extracted upper and lower third molar. b Autogenous tooth bone graft powder was prepared chair-side with the disinfected auto-tooth bone graft machine (BonMaker.®, Korea Dental Solutions Co. Ltd., South Korea)
Results
The five patients included three males and two females. Their ages ranged from 25 to 30 years, with a median of 27 years. The baseline characteristics of the included patients are presented in Table 1. Primary wound healing without complications was achieved in all the patients. There was a greater tendency for swelling of the cheeks and trismus to occur at the experimental site on the third postoperative day. None of the patients complained of any other pain or discomfort. Compared with the control site, the experimental site exhibited progressive bone filling and ossification in the sixth postoperative month. Moreover, the probing pocket depth of the experimental site was lower than that of the control site (Figs. 2, 3).
Table 1.
Baseline characteristics of included patients
| Patients | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age (years) | 25 | 27 | 28 | 30 | 26 |
| Gender | Male | Female | Female | Male | Male |
| Location | |||||
| Treatment | Left | Left | Right | Left | Right |
| Control | Right | Right | Left | Right | Left |
| Pell–Gregory classification | |||||
| Treatment | Class II, level B | Class I, level B | Class II, level B | Class II, level B | Class II, level B |
| Control | Class II, level A | Class I, level B | Class III, level B | Class II, level B | Class II, level C |
| Winter classification | |||||
| Treatment | Mesioangular | Mesioangular | Horizontal | Mesioangular | Mesioangular |
| Control | Horizontal | Mesioangular | Mesioangular | Mesioangular | Mesioangular |
| Proximity to the mandibular canal | |||||
| Treatment | No contact | Contact | No contact | No contact | No contact |
| Control | No contact | No contact | No contact | No contact | Contact |
| Buccal–lingual classification | |||||
| Treatment | Buccal | Central | Buccal | Central | Buccal |
| Control | Central | Central | Buccal | Buccal | Buccal |
| PD (mm) | |||||
| Treatment | 3.0 | 3.3 | 3.2 | 3.1 | 3.2 |
| Control | 3.3 | 3.7 | 3.6 | 3.5 | 3.4 |
Fig. 2.

Preoperative panoramic radiographs
Fig. 3.

Postoperative panoramic radiographs
Discussion
To date, many studies have confirmed that ATGP could be used as an alternative option, providing excellent biocompatibility without causing an immune response, contagion, or reaction to a foreign material in socket preservation, alveolar repair, and different kinds of bone augmentation in dental clinics [15, 20–27]. This study reached a similar conclusion. However, for the first time, we attempted to conduct a prospective clinical trial using ATGP prepared chairside from two extracted one side third molars to repair the distal osseous defects of M2. Within the investigation, ATGP is probably the most economical, convenient and effective bone substitute for repairing the distal osseous defects of M2 due to its rapid ossification, low absorption rate and good bone remodeling excellency.
Because of malposition and proximal alveolar bone loss, the M3 extraction sockets are usually larger than those of other teeth [1]. Physiological natural healing is often unsatisfactory. Due to the location, the self-cleaning of the M3 socket is relatively poor. If the wound is not closed, healing will be worse [2]. Therefore, two problems should be solved: first, the extraction socket should be filled, and second, the wound should be closed perfectly [6]. According to this study, the amount of ATGP prepared from two extracted third molars was exactly the amount needed to fill the M3 extraction socket. The distal osseous defect of M2 was repaired using graft power from a single extracted M3, and covering with a gelatin sponge also achieved a significant effect [28]. It could be inferred that spontaneous socket healing is the least common treatment option. Other advantages of ATGP are that no repairing periosteum is required [16, 18]. According to our observation, although the soft tissue swelling at the experimental site during the first three days after surgery was not mild, this process of ossification was occurred more quickly than the natural healing of the tooth extraction socket at the control site, and it occurred without any complications.
Autologous bone grafts remain the gold standard materials applied to optimize alveolar bone reconstruction and augmentation. However, the “rob Peter to pay Paul” supplying patterns are the greatest disadvantages of autologous bone grafts [10]. From a supply and demand perspective, extracted third molars are the best source for single tooth socket preservation and alveolar repair. If a patient has a smaller maxilla third molar or if the M3 was destroyed in the process of removal, insufficient amounts of ATGP would be obtained. When these cases occurred in this study, the root of M3 was filled with a gelatin sponge, the rest of the distal osseous defect of M2 was repaired with ATGP, and effective satisfactory results were also achieved. Bone resorption is another limitation of autologous bone grafts [29]. There have been no randomized controlled trials comparing autologous bone grafts with autogenous tooth bone grafts for the repair of alveolar bone defects. Regarding bone resorption, previous comparative single case studies have shown that autogenous tooth bone grafts are equivalent or superior to autologous bone grafts for repairing alveolar bone defects [13, 25, 30, 31].
Conclusion
This is an observational pilot study, and the study results demonstrate that ATGP, prepared onsite, effectively, economically and conveniently repairs the distal osseous defects of M2. Although the limited sample size decreases the reliability of the study results, reports on the clinical application of ATGP made from two extracted third molars are very rare, and this investigation is clinically valuable. Larger case series or prospective clinical trials are required to validate the use of ATGP as a preferred and probably best alternative option for the treatment of osseous defects after the extraction of impacted mandibular third molars.
Acknowledgements
We acknowledge American Journal Experts (https://www.aje.com, AJE, Durham, NC, USA) for reviewing the manuscript for grammar consistency (ID: LY8WBN4R).
Author contributions
AW, FH and ZY contributed to the conception and design of the study. AW, YZ, YH and ZY performed the experiments. YZ, YH, FH and AW collected and analyzed the data. AW wrote the manuscript. The authors reviewed and approved the final version of the manuscript.
Funding
This study was supported by the Scientific Research Project of Shanghai Municipal Health Commission (202040497).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
The research was approved by the institutional review board of Shanghai Stomatological Hospital & School, Fudan University, China. (File Number: [2020]0016). Informed consent was obtained from all the patients. All the methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
All radiographic images were captured at the Department of Oral & Maxillofacial Radiology, Shanghai Stomatological Hospital & School, Fudan University. All the patients signed consent forms for documentation.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alimujiang Wushou, Yan Zheng and Yu Han have contributed equally to this work
Contributor Information
Zhi-cheng Yang, Email: Zhicheng_yang1998@fudan.edu.cn.
Fang-kai Han, Email: Han_fangkai@fudan.edu.cn.
References
- 1.Kugelberg CF. Impacted lower third molars and periodontal health. An epidemiological, methodological, retrospective and prospective clinical, study. Swed Dent J Suppl. 1990;68:1–52. [PubMed] [Google Scholar]
- 2.Passarelli PC, Pasquantonio G, D’Addona A. Management of surgical third lower molar extraction and postoperative progress in patients with factor VII deficiency: a clinical protocol and focus on this rare pathologic entity. J Oral Maxillofac Surg. 2017;75(10):2070.e1-4. doi: 10.1016/j.joms.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Blakey GH, Hull DJ, Haug RH, Offenbacher S, Phillips C, White RP., Jr Changes in third molar and nonthird molar periodontal pathology over time. J Oral Maxillofac Surg. 2007;65(8):1577–83. doi: 10.1016/j.joms.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Blakey GH, Jacks MT, Offenbacher S, Nance PE, Phillips C, Haug RH, White RP., Jr Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J Oral Maxillofac Surg. 2006;64(2):189–93. doi: 10.1016/j.joms.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Shoshani-Dror D, Shilo D, Ginini JG, Emodi O, Rachmiel A. Controversy regarding the need for prophylactic removal of impacted third molars: an overview. Quintessence Int. 2018;49(8):653–62. doi: 10.3290/j.qi.a40784. [DOI] [PubMed] [Google Scholar]
- 6.Low SH, Lu SL, Lu HK. Evidence-based clinical decision making for the management of patients with periodontal osseous defect after impacted third molar extraction: a systematic review and meta-analysis. J Dent Sci. 2021;16(1):71–84. doi: 10.1016/j.jds.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Throndson RR, Sexton SB. Grafting mandibular third molar extraction sites: a comparison of bioactive glass to a nongrafted site. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(4):413–19. doi: 10.1067/moe.2002.127582. [DOI] [PubMed] [Google Scholar]
- 8.Tabrizi R, Khorshidi H, Shahidi S, Gholami M, Kalbasi S, Khayati A. Use of lincomycin-impregnated demineralized freeze-dried bone allograft in the periodontal defect after third molar surgery. J Oral Maxillofac Surg. 2014;72(5):850–57. doi: 10.1016/j.joms.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 9.Hassan KS, Marei HF, Alagl AS. Does grafting of third molar extraction sockets enhance periodontal measures in 30- to 35-year-old patients? J Oral Maxillofac Surg. 2012;70(4):757–64. doi: 10.1016/j.joms.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Ge J, Yang C, Zheng J, Hu Y. Autogenous bone grafting for treatment of osseous defect after impacted mandibular third molar extraction: A randomized controlled trial. Clin Implant Dent Relat Res. 2017;19(3):572–80. doi: 10.1111/cid.12466. [DOI] [PubMed] [Google Scholar]
- 11.Sammartino G, Tia M, Gentile E, Marenzi G, Claudio PP. Platelet-rich plasma and resorbable membrane for prevention of periodontal defects after deeply impacted lower third molar extraction. J Oral Maxillofac Surg. 2009;67(11):2369–73. doi: 10.1016/j.joms.2009.04.093. [DOI] [PubMed] [Google Scholar]
- 12.Kumar N, Prasad K, Ramanujam L, K R, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg. 2015;73(6):1042–49. doi: 10.1016/j.joms.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Kim YK, Kim SG, Yun PY, Yeo IS, Jin SC, Oh JS, Kim HJ, Yu SK, Lee SY, Kim JS, et al. Autogenous teeth used for bone grafting: a comparison with traditional grafting materials. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(1):e39–45. doi: 10.1016/j.oooo.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Kim YK, Lee J, Yun JY, Yun PY, Um IW. Comparison of autogenous tooth bone graft and synthetic bone graft materials used for bone resorption around implants after crestal approach sinus lifting: a retrospective study. J Periodontal Implant Sci. 2014;44(5):216–21. doi: 10.5051/jpis.2014.44.5.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radoczy-Drajko Z, Windisch P, Svidro E, Tajti P, Molnar B, Gerber G. Clinical, radiographical and histological evaluation of alveolar ridge preservation with an autogenous tooth derived particulate graft in EDS class 3–4 defects. BMC Oral Health. 2021;21(1):63. doi: 10.1186/s12903-021-01429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, Kim SY. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(4):496–503. doi: 10.1016/j.tripleo.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Jeong KI, Kim SG, Kim YK, Oh JS, Jeong MA, Park JJ. Clinical study of graft materials using autogenous teeth in maxillary sinus augmentation. Implant Dent. 2011;20(6):471–75. doi: 10.1097/ID.0b013e3182386d74. [DOI] [PubMed] [Google Scholar]
- 18.Kim YK, Kim SG, Oh JS, Jin SC, Son JS, Kim SY, Lim SY. Analysis of the inorganic component of autogenous tooth bone graft material. J Nanosci Nanotechnol. 2011;11(8):7442–45. doi: 10.1166/jnn.2011.4857. [DOI] [PubMed] [Google Scholar]
- 19.Zhang S, Li X, Qi Y, Ma X, Qiao S, Cai H, Zhao BC, Jiang HB, Lee ES. Comparison of autogenous tooth materials and other bone grafts. Tissue Eng Regen Med. 2021;18(3):327–41. doi: 10.1007/s13770-021-00333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korsch M, Peichl M. Retrospective study: lateral ridge augmentation using autogenous dentin: tooth-shell technique vs. bone-shell technique. Int J Environ Res Public Health. 2021;18(6):3174. doi: 10.3390/ijerph18063174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Korsch M. Tooth shell technique: a proof of concept with the use of autogenous dentin block grafts. Aust Dent J. 2021;66(2):159–68. doi: 10.1111/adj.12814. [DOI] [PubMed] [Google Scholar]
- 22.Elfana A, El-Kholy S, Saleh HA, Fawzy El-Sayed K. Alveolar ridge preservation using autogenous whole-tooth versus demineralized dentin grafts: a randomized controlled clinical trial. Clin Oral Implants Res. 2021;32(5):539–48. doi: 10.1111/clr.13722. [DOI] [PubMed] [Google Scholar]
- 23.Cervera-Maillo JM, Morales-Schwarz D, Morales-Melendez H, Mahesh L, Calvo-Guirado JL. Autologous tooth dentin graft: a retrospective study in humans. Medicina (Kaunas) 2021;58(1):56. doi: 10.3390/medicina58010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taşdemir U, Kirtay M, Keleş A, Çil N, Abban G, Dodurga Y. Autogenous tooth bone graft and simvastatin combination effect on bone healing. J Craniofac Surg. 2020;31(8):2350–54. doi: 10.1097/SCS.0000000000006707. [DOI] [PubMed] [Google Scholar]
- 25.Kim YK, Lee JH, Um IW, Cho WJ. Guided bone regeneration using demineralized dentin matrix: long-term follow-up. J Oral Maxillofac Surg. 2016;74(3):515.e1-9. doi: 10.1016/j.joms.2015.10.030. [DOI] [PubMed] [Google Scholar]
- 26.Kim ES. Autogenous fresh demineralized tooth graft prepared at chairside for dental implant. Maxillofac Plast Reconstr Surg. 2015;37(1):8. doi: 10.1186/s40902-015-0009-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim YK, Yun PY, Um IW, Lee HJ, Yi YJ, Bae JH, Lee J. Alveolar ridge preservation of an extraction socket using autogenous tooth bone graft material for implant site development: prospective case series. J Adv Prosthodont. 2014;6(6):521–27. doi: 10.4047/jap.2014.6.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sánchez-Labrador L, Martín-Ares M, Ortega-Aranegui R, López-Quiles J, Martínez-González JM. Autogenous dentin graft in bone defects after lower third molar extraction: a split-mouth clinical trial. Materials (Basel) 2020;13(14):3090. doi: 10.3390/ma13143090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Sousa CA, Lemos CAA, Santiago-Júnior JF, Faverani LP, Pellizzer EP. Bone augmentation using autogenous bone versus biomaterial in the posterior region of atrophic mandibles: a systematic review and meta-analysis. J Dent. 2018;76:1–8. doi: 10.1016/j.jdent.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 30.Kim YK, Kim SG, Bae JH, Um IW, Oh JS, Jeong KI. Guided bone regeneration using autogenous tooth bone graft in implant therapy: case series. Implant Dent. 2014;23(2):138–43. doi: 10.1097/ID.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 31.Kim YK, Kim SG, Um IW, Kim KW. Bone grafts using autogenous tooth blocks: a case series. Implant Dent. 2013;22(6):584–89. doi: 10.1097/ID.0000000000000011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


