Abstract
Intussusception is the invagination of a segment of bowel (intussusceptum) into the lumen of an adjacent segment (intussuscipiens). Adult intussusception is rare and typically asymptomatic, although bowel obstruction can be a predominant symptom, making it difficult to diagnose. Splenosis is an uncommon and benign disease, arising from the self-implantation of splenic tissue elsewhere in the body after splenectomy or splenic trauma. Colocolic intussusception secondary to splenosis is rare. We report a case of colon intussusception with a mass in the intussusception detected by ultrasound. Abdominal ultrasound identified the intussusception location but failed to distinguish its pathological properties. Colonoscopy revealed the exudation of necrotic and fibrous tissue. Surgery was performed because of suspicions of a malignant tumor.
Keywords: Splenosis, ultrasound, intussusception, colon, abdominal ultrasound, colonoscopy
Introduction
Adult intussusception (AI) is rare and its clinical presentations differ from those of intussusception in children. 1 AI was previously found in 1% of adult patients with bowel obstruction, and the incidence of ileocolic or colocolic intussusception is low in adults (0.3/100,000 inhabitants per year). 2 AIs can present with acute, intermittent, or chronic symptoms. 3 Despite advances in imaging procedures, intussusception is difficult to preoperatively diagnose.4,5 Colocolic intussusception is more commonly associated with malignant lead points (∼65%) than small bowel intussusception. 6 There have been a few reports of splenosis in the colon,7–9 but no documentation of colocolic intussusception secondary to splenosis. The present study reports an adult case of colocolic intussusception secondary to splenosis, and reviews the current literature.
Case report
A Chinese man in his early 30s visited our hospital with severe paroxysmal left upper abdominal pain that had persisted for 2 days with no obvious cause. He had undergone splenic surgery 10 years previously. His weight had not altered significantly during the past 3 months. His C-reactive protein levels and white blood cell count were increased at 14.30 mg/L and 11.0/L, respectively. Carbohydrate antigen 125, carbohydrate antigen 199, and prostate-specific antigen levels were all normal.
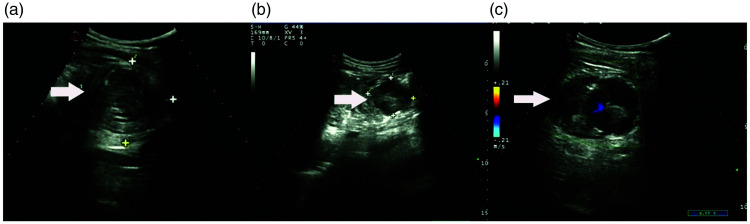
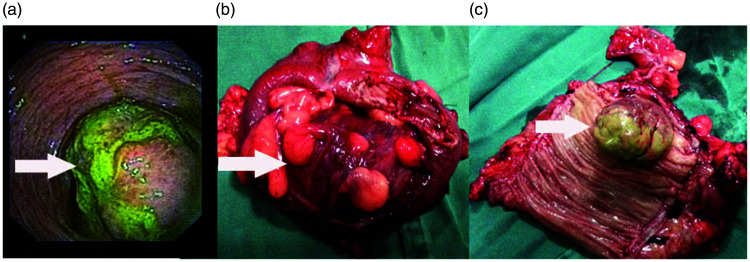
Ultrasound examination revealed an intussusception mass of approximately 6.2 × 5.9 cm in the left colon (Figure 1a). Within this mass, a nodule of approximately 4.4 × 3.8 cm (Figure 1b) was noted. The invagination depth was approximately 3.7 cm, and a star-shaped blood flow signal was seen in ultrasonic color Doppler (Figure 1c). Under ultrasound guidance, the intussusception was relieved with a normal saline enema. Colonoscopy was performed by inserting the lens 40 cm into the anus, which revealed a mass accounting for more than four-fifths of the intestinal cavity (Figure 2a). Biopsy results showed a small amount of necrotic and fibrous tissue exudation from the colon. Surgically, the transverse colon and descending colon were cut off 10 cm above and below the tumor, and side-to-side anastomosis of the distal and proximal bowels and transverse closure were performed. The diameter of the tumor was 4.5 cm (Figure 2b, 2c).
Figure 1.
(a) Ultrasound examination showing an intussusception mass approximately 6.2 × 5.9 cm in the left colon. (b) A nodule approximately 4.4 × 3.8 cm was seen in the mass and (c) A star-shaped blood flow signal was shown in color Doppler of the nodule.
Figure 2.
(a) Colonoscopy showing a mass accounting for greater than 4/5 of the intestinal cavity. (b) Diseased bowel covered with intestinal fat and (c) A mass of about 4.5 cm in diameter on the intestinal wall.
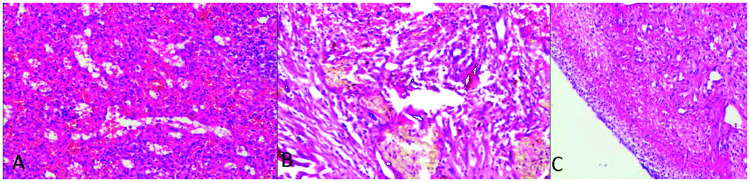
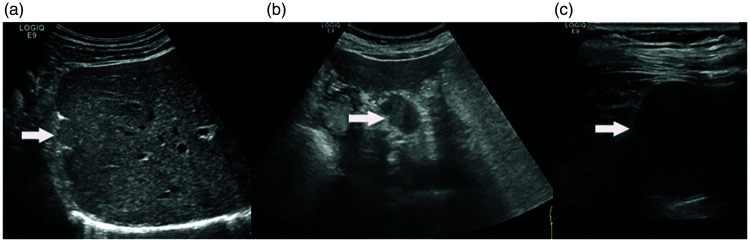
Hematoxylin and eosin staining of tumor sections showed red and white pulp, and the splenic sinus was dilated and extravasated (Figure 3a). An intramedullary hemorrhage (Figure 3b) and ulcers were observed (Figure 3c). Immunoenzyme labels 140083 and P53 were negative, and cluster of differentiation (CD)20, CD79a, CD34, CD15, CD30, and Ki-67 were not obviously expressed. Lesions were detected in the liver (Figure 4a), the space between the liver and stomach (Figure 4b), and the abdominal cavity (Figure 4c). All lesions were well-defined, round, or oval, and had a homogeneously hypoechoic echotexture identical to that of the spleen on ultrasound.
Figure 3.
(a) Hematoxylin and eosin staining of red and white pulp in the tumor, showing a dilated and extravasated splenic sinus. (b) Intramedullary hemorrhage, hemosiderin deposition, and connective tissue hyperplasia with a small amount of multinucleated giant cell reaction and (c) Surface exudation necrotic granulation tissue, and the formation of superficial ulcers.
Figure 4.
Splenosis located in the liver (a), the space between the liver and stomach (b), and the abdominal cavity (c).
Discussion
AIs typically involve a pathologic lead point, and up to 57% of reported cases are attributable to a malignant tumor.10,11 The main cause of colonic intussusception was reported to be primary adenocarcinoma, followed by lymphoma and metastatic arcinoma. 12 However, a few benign cases have been documented, such as those arising from adenoma 13 and ediculated lipoma. 14
Splenosis is an acquired benign condition resulting from the heterotopic transplantation of splenic tissue after splenic trauma or splenectomy. Its diagnosis is usually an incidental finding. 15 The incidence of splenosis development was reported to be <0.3% after splenectomy. 16 Frequent areas of splenosis include the peritoneum, omentum, and mesentery, but other locations such as the liver, colon, pericardium, subcutaneous tissue, and brain tissue have also been described.7,15,17
Patients often present with nonspecific, varied symptoms which differ depending on the location of ectopic splenic tissue. 18 Kwok et al. 19 reported the migration of erythrocytic progenitor cells via the portal vein following traumatic splenic rupture and the local induction of erythropoiesis by hypoxia. Our case had colonic splenosis rather than intrahepatic splenosis, and we have encountered three other splenosis cases in the past 10 years. Maillard et al.20 detected similar ultrasound features to those seen in our patient.
Ultrasound images can be masked by gas-filled loops of bowel. This makes diagnosis difficult because most AIs present with intestinal obstruction. 21 The preoperative diagnosis accuracy using ultrasonography is 60.0%, but this increases to 91.7% in cases of palpable abdominal masses. 5 Coloscopy can provide information about the benign or malignant nature of the lesion, potentially avoiding unnecessary surgery, although abdominal computed tomography was found to be the most accurate preoperative diagnostic method of diagnosing intussusception compared with ultrasonography, small bowel series, barium enema, and colonoscopy, with a pooled accuracy of 77.8%. 12 However, it has limited value in discriminating whether a lead point is malignant, benign, or idiopathic.
Splenic trauma or splenectomy are key events to recognize in the diagnosis of splenosis. In recent years, 99m-tagged heat-damaged erythrocyte scintigraphy and technetium-99m sulfur colloid scintigraphy have been developed to provide greater specificity in the identification of splenic tissue.22,23
Patients with asymptomatic splenosis do not require surgical treatment, although related therapies can be performed to treat corresponding symptoms in other locations. Because most AIs have underlying pathological lesions, laparotomy is usually agreed to be necessary. 24 However, it remains controversial whether intussusception should be reduced before resection.
In conclusion, when patients with abdominal tumors experience splenic trauma or splenectomy, it is important for clinicians to be aware of the possibility of splenosis. In patients with intussusception, ultrasound can help with diagnosis and relief, while coloscopy can provide pathological information about large bowel intussusception with tumors. Additionally, appropriate imaging and scintigraphy can be performed to recognize key features and avoid unnecessary invasive diagnostic procedures and surgery.
Footnotes
Declaration of conflicting interest: The authors declare no conflicts of interest.
Ethics statement: This case report was not required to be reviewed by the ethics review committee because it discusses the diagnosis and pathogenesis of a rare disease; no exploratory treatment was performed. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy this consent is available for review by the Editor-in-Chief of this journal. We have de-identified all patient details. The reporting of this study conforms to CARE guidelines. 25
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Youth Innovation Project of Sichuan Medical Association (No. Q20032).
ORCID iDs
Xuemei Tang https://orcid.org/0000-0003-0748-2201
Wenming Lu https://orcid.org/0000-0002-5600-0398
References
- 1.Cochran AA, Higgins GR, 3rd, Strout TD. Intussusception in traditional pediatric, nontraditional pediatric, and adult patients. Am J Emerg Med 2011; 29: 523–527. [DOI] [PubMed] [Google Scholar]
- 2.Azar T, Berger DL. Adult intussusception. Ann Surg 1997; 226: 134–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felix EL, Cohen MH, Bernstein AD, et al. Adult intussusception; Case report of recurrent intussusception and review of the literature. Am J Surg 1976; 131: 758–761. [DOI] [PubMed] [Google Scholar]
- 4.Ozogul B, Kisaoglu A, Ozturk G, et al. Adult intussusception: clinical experience from a single center. Indian J Surg 2015; 77: 490–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang N, Cui XY, Liu Y, et al. Adult intussusception: A retrospective review of 41 cases. World J Gastroenterol 2009; 15: 3303–3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: A review. World J Gastroenterol 2009; 15: 407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Ji B, Wang G, et al. Abdominal multiple splenosis mimicking liver and colon tumors: A case report and review of the literature. Int J Med Sci 2012; 9: 174–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Kheir A, Abdelnour M, Boutros JG. Simultaneous small bowel and colon obstruction due to splenosis. A case report and review of literature. Int J Surg Case Rep 2019; 58: 63–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obokhare ID, Beckman E, Beck DE, et al. Intramural colonic splenosis: A rare case of lower gastrointestinal bleeding. J Gastrointest Surg 2012; 16: 1632–1634. [DOI] [PubMed] [Google Scholar]
- 10.Honjo H, Mike M, Kusanagi H, et al. Adult intussusception: A retrospective review. World J Surg 2015; 39: 134–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanan B, Diniz TR, Da LM, et al. Intussusception in adults: A retrospective study. Colorectal Dis 2010; 12: 574–578. [DOI] [PubMed] [Google Scholar]
- 12.Hong KD, Kim J, Ji W, et al. Adult intussusception: A systematic review and meta-analysis. Tech Coloproctol 2019; 23: 315–324. [DOI] [PubMed] [Google Scholar]
- 13.Mahmud N, Wangensteen KJ. Colocolic intussusception. Arab J Gastroenterol 2019; 20: 107–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laleman W, Bisschops R, Vermeire S. Electronic clinical challenges and images in GI. Colocolonic intussusception of pediculated lipoma. Gastroenterology 2009; 136: e5–e6. [DOI] [PubMed] [Google Scholar]
- 15.Gupta K, Ahluwalia A, Jain T, et al. Abdominal splenosis mimicking peritoneal deposits – a case report. Pan Afr Med J 2014; 17: 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falcão de Santana M, Menezes Marques L, Lopes Gibara V, et al. Ectopic spleen mimicking hepatocellular carcinoma in the late post-operative period of bariatric surgery. Cell Mol Biol (Noisy-le-grand) 2018; 64: 113–115. [PubMed] [Google Scholar]
- 17.Ribeiro JC, Silva CM, Santos AR. Splenosis. A diagnosis to be considered. Int Braz J Urol 2006; 32: 678–680. [DOI] [PubMed] [Google Scholar]
- 18.Ksiadzyna D, Pena AS. Abdominal splenosis. Rev Esp Enferm Dig 2011; 103: 421–426. [PubMed] [Google Scholar]
- 19.Kwok CM, Chen YT, Lin HT, et al. Portal vein entrance of splenic erythrocytic progenitor cells and local hypoxia of liver, two events cause intrahepatic splenosis. Med Hypotheses 2006; 67: 1330–1332. [DOI] [PubMed] [Google Scholar]
- 20.Maillard JC, Menu Y, Scherrer A, et al. Intraperitoneal splenosis: Diagnosis by ultrasound and computed tomography. Gastrointest Radiol 1989; 14: 179–180. [DOI] [PubMed] [Google Scholar]
- 21.Erkan N, Haciyanli M, Yildirim M, et al. Intussusception in adults: An unusual and challenging condition for surgeons. Int J Colorectal Dis 2005; 20: 452–456. [DOI] [PubMed] [Google Scholar]
- 22.Alvarez R, Diehl KM, Avram A, et al. Localization of splenosis using 99mTc-damaged red blood cell SPECT/CT and intraoperative gamma probe measurements. Eur J Nucl Med Mol Imaging 2007; 34: 969. [DOI] [PubMed] [Google Scholar]
- 23.Franceschetto A, Casolo A, Cucca M, et al. Splenosis: 99MTc-labelled colloids provide the diagnosis in splenectomised patients. Eur J Nucl Med Mol Imaging 2006; 33: 1102. [DOI] [PubMed] [Google Scholar]
- 24.Gupta RK, Agrawal CS, Yadav R, et al. Intussusception in adults: Institutional review. Int J Surg 2011; 9: 91–95. [DOI] [PubMed] [Google Scholar]
- 25.Rubino M, Pragnell MVC. Guidelines for reporting case series of tumours of the colon and rectum. Techniques in Coloproctology 1999; 3: 93–97. [Google Scholar]