Abstract
Posttraumatic stress disorder (PTSD) is a severe condition that is associated with trauma-related guilt. We aimed at providing a comprehensive quantitative systematic review on the relationship between trauma-related guilt and adult PTSD. Database searches in Medline, PsycINFO, PTSDpubs and Web of Knowledge resulted in the inclusion of 163 eligible studies with a total of 35 020 trauma survivors. The studies reported on 157 cross-sectional and 19 longitudinal data points. Overall, we included 135 studies not included in previous meta-analyses. Random-effect models yielded a moderate cross-sectional correlation (r = 0.38, 95% CI 0.35–0.42, p < 0.001, I2 = 90.3%) and a small to moderate predictive correlation (r = 0.21, 95% CI 0.13–0.29, p < 0.001, I2 = 66.7%). The association appeared to be stable over time and was robust to sensitivity analyses. All symptom clusters significantly correlated with guilt. No effects were found for military v. civilian populations or clinical v. non-clinical samples. Effects were smaller for high-quality studies and larger for instruments based on DSM-5. Further significant moderators were type of guilt measure and trauma type. The largest association was found among participants reporting war-related trauma (r = 0.44, 95% CI 0.36–0.51) and the smallest among survivors of motor-vehicle accidents (r = 0.18, 95% CI 0.02–0.33). The results underpin the role of trauma-related guilt in the onset and maintenance of PTSD symptoms, which have important clinical implications. Future studies should further explore the change interactions of guilt and PTSD symptoms.
Key words: Guilt, meta-analysis, posttraumatic stress, PTSD, self-blame
Introduction
Posttraumatic stress disorder (PTSD) is a common and rather chronic disorder (Jellestad, Vital, Malamud, Taeymans, & Mueller-Pfeiffer, 2021). Ever since its first introduction into DSM-III (American Psychiatric Association, 1980), guilt and self-blame appraisals have been considered as part of diagnostic criteria for PTSD in various ways. Initially, the arousal and avoidance cluster included survivor guilt as one of six potential symptoms. After removal of survivor guilt in the DSM-III-R based on inconsistent findings regarding its manifestation, it was reported as associated feature until DSM-TR (American Psychiatric Association, 1987, 2000). With the implementation of a new cluster for negative alterations in cognitions and mood in DSM-5, distorted self-blame and a persistent negative emotional state, including guilt, were added (American Psychiatric Association, 2013).
Guilt can be defined as both dispositional and chronic (i.e. guilt-proneness) or as situation-specific and transient, such as trauma-related guilt. Research suggests that trauma-related guilt is highly prevalent in trauma populations (Miller et al., 2013; Murray, 2018) and is associated with increased psychopathology and suicidal ideation as well as reduced functioning (Browne, Trim, Myers, & Norman, 2015; Bryan, Morrow, Etienne, & Ray-Sannerud, 2013; Norman et al., 2018). Clinical trials making use of guilt measures have revealed that trauma-related guilt is a frequent residual symptom, which showed smaller changes over time relative to PTSD symptoms (Larsen, Fleming, & Resick, 2019). At the same time, shifts in trauma-related guilt during treatment were found to predict PTSD symptoms during and following treatment (Allard, Norman, Thorp, Browne, & Stein, 2018; Øktedalen, Hoffart, & Langkaas, 2015).
Theoretical models of trauma-related guilt
Research on guilt is based on various definitions that differ with respect to whether guilt contributes to psychopathology or rather represents a protective factor (Tilghman-Osborne, Cole, & Felton, 2010). Most theories define guilt as an emotional construct resulting from perceived moral transgression which may be related to social norms and linked to specific behaviours. Trauma-related guilt may involve a failure to acknowledge the multiple sources of causation of negative events (Kubany & Manke, 1995). A comprehensive model of trauma-related guilt by Kubany and coworkers implicates one component of affective distress and one of guilt-related cognitions (Kubany & Manke, 1995; Kubany & Watson, 2003). The distress component includes psychological distress and physical sensations when thinking about the traumatic event and the inflicted harm or loss. The cognitive component reflects one's own role in the event and includes perceived personal wrongdoing, responsibility for causing the event, lack of justification and false beliefs about pre-outcome knowledge. Norman and colleagues (Norman, 2022; Norman, Wilkins, Myers, and Allard, 2014) further distinguish in their model of Non-Adaptive Guilt and Shame (NAGS) between trauma survivors who do not experience guilt, those who use guilt to adjust behaviour in accordance with their personal values and those who enter a cycle of feelings of guilt and shame and beliefs about personal wrongdoing or wrongbeing. The authors propose that it is the cycle of negative beliefs and affect that contributes to psychopathology.
Cognitive models of PTSD suggest that maladaptive appraisals of the traumatic event or its sequelae induce a sense of current threat and thus represent a crucial factor in the development and maintenance of the disorder (Ehlers & Clark, 2000). This may manifest in the belief of one's own attraction to disaster or inability to recognise signs of imminent threat. These self-blame appraisals correspond to the guilt cognitions as defined by Kubany and coworkers. Lee, Scragg, and Turner (2001) suggest that guilt-based PTSD may emerge when the meaning of the traumatic event does not match the schematic representations of the self and others. It further appears to hinder emotional processing of the event (Brewin, Dalgleish, & Joseph, 1996). Guilt may be especially linked to the avoidance cluster of PTSD symptoms based on the appraisal of one's responsibility for bad things to happen (Ehlers & Clark, 2000) or when restitution is not possible (Kubany, 1998).
The notion of guilt is closely related to shame (Lewis, 2008; Wilson, Drozdek, & Turkovic, 2006). Although both represent self-conscious emotions, shame often refers to an identity-related attribution, whereas guilt often refers to a behaviour-related attribution (Lewis, 1971). While there is a debate on the conceptual differentiation and distinct effects of shame-free guilt and guilt-free shame on psychopathology (Lewis, 2014; Tangney & Dearing, 2002), research suggests that shame and guilt both represent unique predictors of PTSD (Cunningham, Davis, Wilson, & Resick, 2018; Shi, Ren, Zhao, Zhang, & Chan, 2021).
Current state of research
To our knowledge, three reviews and meta-analyses have investigated the association between guilt and PTSD. Pugh, Taylor, and Berry (2015) conducted a systematic review including 27 studies on the cross-sectional association between guilt and PTSD symptoms. The review focused on self-report measures of guilt; however, it included measures on the experience of guilt regarding everyday situations as well as general guilt-proneness. The authors concluded that despite evidence of the relationship between guilt and PTSD, the direction of association is yet unknown. Whereas guilt may be part of the causal mechanisms in the onset of PTSD, there might also be a reverse relation. Furthermore, guilt and PTSD may be co-occurring consequences of trauma that correlate but do not have a causal relation, or the relationship between PTSD and guilt may be mediated by other associated and overlapping constructs. Gómez de La Cuesta, Schweizer, Diehle, Young, and Meiser-Stedman (2019) reported in their meta-analysis a moderate relationship between self-blame appraisals and PTSD (r = 0.28; k = 57). However, analyses were restricted to the use of the Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999), which covers negative cognitions about the self, negative cognitions about the world and self-blame. Shi et al. (2021) found a moderate to large association between trauma-related guilt and PTSD (r = 0.43; k = 45). Yet, 11 of the included studies report on the same five samples, resulting in an overrepresentation of their results. Furthermore, the authors included studies on acute stress disorder and PTSD measures were not required to have been validated. Shi et al. concluded that their results support the addition of guilt in the diagnostic criteria of PTSD. This conclusion is, however, limited since several of the included studies had assessed PTSD based on DSM-5, which comprises guilt itself.
Several moderating variables have been examined in the previous meta-analyses. While Shi et al. (2021) found a larger association between guilt and PTSD in military populations, this difference was not significant in the meta-analysis on posttraumatic appraisals. Similarly, type of traumatic event appeared to be a significant moderator regarding guilt, but not posttraumatic appraisals. Type of measure was a significant moderator in both analyses, while gender was only significant regarding guilt.
The present study
This meta-analysis aimed at examining the relationship between trauma-related guilt and PTSD symptoms in trauma-exposed adults. Limitations from former meta-analyses were addressed by applying a comprehensive search strategy, sophisticated inclusion criteria, inclusion of longitudinal data and a careful consideration of risk of bias. To address the latter, we administered a quality rating for included studies. Alongside the cross-sectional association between trauma-related guilt and overall PTSD symptoms, we aimed at quantifying the association between guilt and individual PTSD symptom clusters, the predictive effect of guilt on PTSD and the impact of potential moderators.
Method
The aims and methods of this meta-analysis were registered on the PROSPERO database (CRD42021251144) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were followed (Moher, Liberati, Tetzlaff, & Altman, 2009).
Identification and selection of literature
We conducted an electronic database search including Medline, PsycINFO, PTSDpubs and Web of Knowledge. The search dated from inception to April 2021 and combined the following search terms: (guilt* OR culpabilit* OR blam* OR self-blam*) AND (‘traumatic stress’ OR ‘posttraumatic stress’ OR ‘post-traumatic stress’ OR PTSD OR PTSS). The full strategy is presented in online Supplementary Appendix A. Based on the aforementioned models of trauma-related guilt, we considered self-blame as the cognitive component of guilt and included both terms (i.e. guilt and self-blame) in our search and both constructs in our meta-analysis. Screening of titles and abstracts was conducted using Rayyan (Ouzzani, Hammady, Fedorowicz, & Elmagarmid, 2016). Two independent and blinded reviewers completed the initial screening, with a third reviewer being involved for any disagreements. For the review of full-texts, 10% of studies were assessed for eligibility by both reviewers (κ = 0.82; 93.2% agreement rate), the remaining studies were reviewed by one of the two reviewers. Electronic database search was supplemented by a manual search of relevant reference lists and google scholar. No publication restrictions were applied.
Records were considered eligible if they (a) included adults (mean age ⩾18 years), (b) assessed PTSD symptoms with a validated instrument based on DSM/ICD (including validated translations where applicable), (c) assessed guilt quantitatively as a continuous variable, and (d) reported on an observational or experimental study regarding the association between PTSD symptoms and guilt, or on a clinical trial with relevant pre-treatment data. Both cross-sectional and longitudinal studies were included. For studies including a PTSD v. non-PTSD group comparison, the PTSD group had to comprise a clinical sample, i.e. at least 70% had to meet full diagnostic PTSD criteria (Bisson, Roberts, Andrew, Cooper, & Lewis, 2013; Morina, Hoppen, & Kip, 2021).
Records were excluded if they reported on guilt associated with psychotic symptoms, reported on single-case studies or did not report correlations or sufficient data to calculate coefficients and authors did not provide sufficient data after two contact attempts. Guilt had to be related to a stressful event; thus, unspecific feelings of guilt regarding everyday situations or guilt proneness were excluded. Measures that did not distinguish between guilt and related constructs such as shame were excluded.
Data extraction
Two independent investigators coded and extracted data from each eligible study with all disagreements being discussed. The primary estimate was Pearson's correlation coefficient (r). PTSD v. non-PTSD group comparisons were converted into Pearson's r. We preferred clinician-rated data over self-report data. If two PTSD self-report measures were assessed, we considered the one that was more frequently reported across the included studies. Given the close link between the distress scale in the Trauma Related Guilt Inventory (TRGI; Kubany et al., 1996) and PTSD symptoms, we excluded this scale when possible, to prevent an inflated effect size. In studies with multiple assessments, we used the first eligible time point under consideration of the DSM time criterion for PTSD for the cross-sectional association. For the predictive association, we used PTSD data from the longest follow-up. Data were extracted regarding both total scores on PTSD measures as well as subscales reflecting the DSM symptom clusters.
Quality assessment
Given the various study types included in the meta-analysis and the lack of a recommended quality assessment tool that covers this heterogeneity, we developed a tool for the purpose of our review. The tool was based on McCarthy and Morina (2020) and quantitatively assessed study quality using five items: (1) Did the study include a clinical sample with PTSD diagnosis?; (2) Was PTSD diagnosis determined with a validated instrument?; (3) Was PTSD symptom severity assessed with a clinically-validated instrument?; (4) Was guilt measured with a validated instrument?; and (5) Was the sample size for guilt-related analyses underpinned with an a priori power analysis?. Items were scored on a three-point scale from 0 to 2. Further concerns were noted qualitatively, e.g. single-item assessment of guilt, student samples who received course credit or psychometric properties <0.7 (Bland & Altman, 1997; Nunnally & Bernstein, 1994). An instrument was deemed validated if data on convergent and discriminant validity were publicly available besides internal consistency or re-test reliability. The same criteria applied for translations of instruments. The complete quality assessment tool is displayed in the online Supplementary Appendix B. All studies were rated by two blinded and independent raters.
Data synthesis and analyses
Analyses were performed using R (v4.1.2; R Core Team, 2020). Given the various instruments to assess PTSD and guilt and the broad scope of study types and populations, we expected high heterogeneity and used random-effect models for all analyses. A Bonferroni–Holm correction for multiple comparisons was applied. To consider dependent effect sizes, studies that reported on different relevant subscales or instruments were averaged by using weights of a fixed-effects meta-analysis (Rosenthal & Rubin, 1986). Correlations were transformed into Fisher's z to reduce risk of bias due to range restrictions and to obtain an approximate normal sampling distribution (Harrer, Cuijpers, Toshi, Furukawa, & Ebert, 2021). Results were then back-transformed into Pearson's r for ease of interpretation. Correlations may be interpreted using Cohen's (1988) conventions of r ≈ 0.10 representing a small effect, r ≈ 0.30 a moderate effect and r ≈ 0.50 representing a large effect. Results were supplemented with 95% confidence intervals (CI) as well as 95% prediction intervals. The latter facilitate clinical interpretations by considering between-study heterogeneity and providing a range of expected true effects in prospective observations. Between-study heterogeneity was estimated using the Restricted Maximum Likelihood (REML) and adjusted with the method suggested by Knapp and Hartung (2003). We assessed between-study heterogeneity using Cochran's Q and Higgins' I2 statistics (Higgins, Thompson, Deeks, & Altman, 2003). Publication bias was visually inspected using forest plots and furthermore examined using Egger's test and the trim and fill method for all analyses including at least 10 studies (Duval & Tweedie, 2000; Egger, Smith, Schneider, & Minder, 1997). Sensitivity analyses were conducted on different levels to explore heterogeneity (Patsopoulos, Evangelou, & Ioannidis, 2008). First, we investigated influential studies on a case-by-case basis using the leave-one-out method. Second, we considered groups of studies based on quality (i.e. validation of guilt measure, inclusion of clinical samples) or outlying effect sizes. Outliers were defined as studies which 95% CI did not overlap with the 95% CI of the pooled effect. Mixed-effect models and meta-regressions were employed to examine whether the observed heterogeneity may be explained by variables of interest (e.g. trauma type, time since trauma).
Results
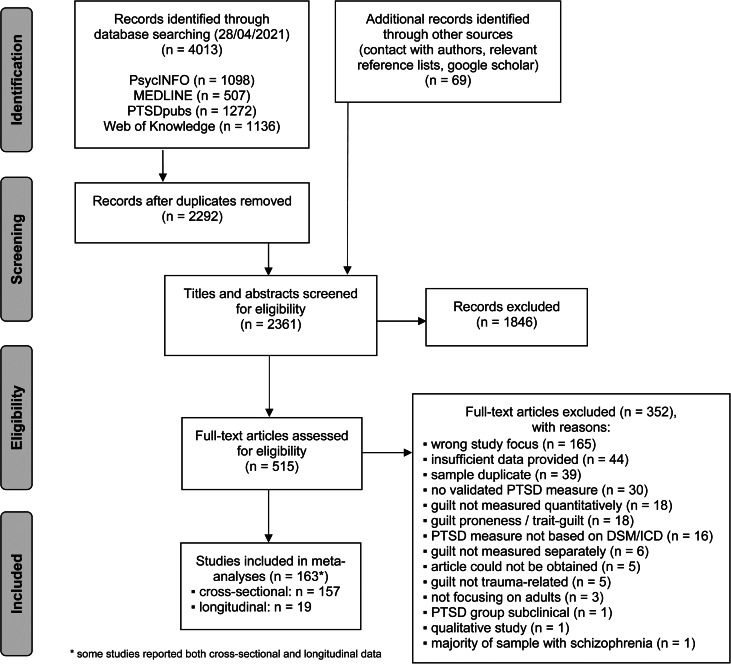
Our database search yielded 2292 unique studies, which were supplemented by 69 studies from other sources (see Fig. 1). After screening of titles and abstracts, we reviewed 515 publications in full text. A list of all excluded publications after full-text review with reasons for exclusion is provided in the online Supplementary Appendix C. Overall, 163 studies including 35 020 participants and 286 effect sizes were considered in our analyses. The included studies were published between 1995 and 2021. The sample size ranged from 22 to 1679. The mean age was 35.23 and 46.36% were female.
Fig. 1.
Flow chart of study selection process.
Characteristics of included studies
Detailed characteristics of all included studies in the meta-analysis, including funding sources, are provided in online Supplementary Appendices D–F. We included 25 dissertation theses, 135 peer-reviewed articles, two master theses and one book chapter. Unpublished data were obtained from Bovin et al. (2014). Trauma-related guilt and self-blame were most frequently measured using the PTCI (48.2%) and the TRGI (15.5%), followed by the Brief Coping Orientation to Problems Experienced Inventory (Brief COPE; 6.0%; Carver, 1997) and the Rape Attribution Questionnaire (RAQ; 4.2%; Frazier, 2003). The majority of studies included individuals with mixed traumatic experiences; specific traumas most frequently reported were war-related (22.0%) and sexual assault-related (12.5%). PTSD symptoms were most commonly assessed using the Posttraumatic Diagnostic Scale (PDS; 20.8%; Foa, Cashman, Jaycox, & Perry, 1997), the PTSD checklist for DSM-5 (PCL-5; 13.7%; Weathers et al., 2013) and the CAPS (11.3%; Blake et al., 1995).
Association between guilt and PTSD symptoms
The overall cross-sectional correlation between guilt and PTSD symptoms, based on 157 studies and including 30 389 trauma survivors, was r = 0.38 (95% CI 0.35–0.42, p < 0.001). Forest plots of main analyses are presented in the online Supplementary Appendices G–H. The heterogeneity was considerable between studies with I2 = 90.3%, the 95% prediction interval ranged from −0.04 to 0.69. A total of 44 studies were identified as statistical outliers and omitted from additional sensitivity analyses. This resulted in a coefficient of r = 0.36 (95% CI 0.34–0.37, p < 0.001) and a heterogeneity of I2 = 39.8%. Detailed results are presented in Table 1. The leave-one-out analysis on putative influential cases revealed no changes in the overall effect size (see online Supplementary Appendix I).
Table 1.
Results from the main meta-analyses, sensitivity and subgroup analyses
| Comparison | k | N | r (95% CI) | p | I2 | 95% PI | Egger's test | Trim and fill | Qbetween | pQ |
|---|---|---|---|---|---|---|---|---|---|---|
| Main meta-analysis | 157 | 30 389 | 0.38 (0.35–0.42) | <0.001 | 90.3 | −0.04 to 0.69 |
t = −1.46 p = 0.146 |
31 studies added, radj = 0.44, 95% CI 0.41–0.47 | ||
| Outliers omitted | 113 | 21 452 | 0.36 (0.34–0.37) | <0.001 | 39.8 | 0.24–0.46 | n.a. | n.a. | ||
| Prediction of PTSD | 19 | 2760 | 0.21 (0.13–0.29) | <0.001 | 66.7 | −0.09 to 0.47 |
t = 0.62 p = 0.545 |
2 studies added, radj = 0.18, 95% CI 0.08–0.27 | ||
| Cluster | ||||||||||
| Intrusion/re-experience | 26 | 5718 | 0.28 (0.19–0.37) | <0.001 | 83.9 | −0.16 to 0.63 |
t = 0.79 p = 0.439 |
1 study added, radj = 0.26, 95% CI 0.16–0.36 | ||
| Avoidance | 25 | 5638 | 0.31 (0.24–0.38) | <0.001 | 79.7 | −0.03 to 0.58 |
t = 0.71 p = 0.483 |
2 studies added, radj = 0.29, 95% CI 0.20–0.36 | ||
| Hyperarousal | 26 | 5702 | 0.30 (0.22–0.37) | <0.001 | 82.8 | −0.07 to 0.60 |
t = 0.55 p = 0.588 |
1 study added, radj = 0.29, 95% CI 0.20–0.37 | ||
| Omnibus test of subgroup differences | 0.26 | 0.878 | ||||||||
| Negative alterations in cognitions/mood | 6 | 1636 | 0.56 (0.42–0.68) | <0.001 | 77.4 | 0.16–0.80 | n.a. | n.a. | ||
| Sample-specific moderators | ||||||||||
| Clinical sample | 31 | 5672 | 0.36 (0.29–0.43) | <0.001 | 79.2 | −0.01 to 0.64 |
t = 0.42 p = 0.677 |
0 studies added | ||
| Compared to non-clinical sample | 0.25 | 0.620 | ||||||||
| Population | ||||||||||
| Military | 38 | 10 246 | 0.43 (0.35–0.50) | <0.001 | 95.4 | −0.10 to 0.77 |
t = −0.43 p = 0.671 |
6 studies added, radj = 0.47, 95% CI 0.40–0.54 | ||
| Civilians | 118 | 20 063 | 0.37 (0.33–0.40) | <0.001 | 84.7 | −0.01 to 0.65 |
t = −0.92 p = 0.361 |
22 studies added, radj = 0.42, 95% CI 0.39–0.46 | ||
| Subgroup analysis | 2.40 | 0.121 | ||||||||
| Trauma type | ||||||||||
| Sexual assault | 19 | 3857 | 0.40 (0.29–0.50) | <0.001 | 86.3 | −0.08 to 0.73 |
t = 0.58 p = 0.571 |
2 studies added, radj = 0.36, 95% CI 0.24–0.47 | ||
| War-related | 37 | 10 029 | 0.44 (0.36–0.51) | <0.001 | 95.4 | −0.09 to 0.77 |
t = −0.31 p = 0.756 |
5 studies added, radj = 0.47, 95% CI 0.40–0.54 | ||
| IPV | 11 | 1138 | 0.42 (0.33–0.51) | <0.001 | 64.9 | 0.15–0.64 |
t = −0.45 p = 0.665 |
0 studies added | ||
| Childhood sexual abuse | 10 | 1467 | 0.21 (0.04–0.37) | 0.020 | 75.1 | −0.26 to 0.60 |
t = −0.59 p = 0.569 |
0 studies added | ||
| MVA | 5 | 1044 | 0.18 (0.02–0.33) | 0.035 | 71.7 | −0.21 to 0.52 | n.a. | n.a. | ||
| Medical condition | 4 | 272 | 0.44 (0.13–0.67) | 0.021 | 63.1 | −0.36 to 0.87 | n.a. | n.a. | ||
| Omnibus test of subgroup differences | 23.35 | <0.001 | ||||||||
| Sexual assault: v. war-related p = 0.525; v. IPV p = 0.745; v. childhood sexual abuse p = 0.021; v. MVA p = 0.004; v. medical condition p = 0.692 | ||||||||||
| War-related: v. IPV p = 0.746; v. childhood sexual abuse p = 0.002; v. MVA p = 0.000; v. medical condition p = 0.998 | ||||||||||
| IPV: v. childhood sexual abuse p = 0.006; v. MVA p = 0.001; v. medical condition p = 0.849 | ||||||||||
| Childhood sexual abuse: v. MVA p = 0.747; v. medical condition p = 0.040 | ||||||||||
| MVA: v. medical condition p = 0.017 | ||||||||||
| Time since trauma | ||||||||||
| <1 year | 21 | 3020 | 0.37 (0.30–0.45) | <0.001 | 86.1 | 0.00–0.66 |
t = −0.56 p = 0.585 |
7 studies added, radj = 0.47, 95% CI 0.39–0.54 | ||
| 1–5 years | 13 | 1983 | 0.34 (0.22–0.45) | <0.001 | 84.6 | −0.14 to 0.69 |
t = 0.89 p = 0.391 |
2 studies added, radj = 0.28, 95% CI 0.14–0.41 | ||
| >5 years | 22 | 4109 | 0.30 (0.20–0.40) | <0.001 | 95.3 | −0.21 to 0.68 |
t = −4.85 p = <0.001 |
11 studies added, radj = 0.54, 95% CI 0.41–0.65 | ||
| Omnibus test of subgroup differences | 1.42 | 0.492 | ||||||||
| Methodological moderators | ||||||||||
| Only DSM-IV | 112 | 21 246 | 0.35 (0.31–0.39) | <0.001 | 91.4 | −0.07 to 0.66 |
t = −1.69 p = 0.094 |
31 studies added, radj = 0.43, 95% CI 0.39–0.47 | ||
| Only DSM-5 | 27 | 6144 | 0.51 (0.44–0.57) | <0.001 | 84.8 | 0.14–0.75 |
t = 1.15 p = 0.262 |
4 studies added, radj = 0.46, 95% CI 0.38–0.54 | ||
| Subgroup analysis | 16.83 | <0.001 | ||||||||
| Validated guilt measures | 125 | 23 880 | 0.37 (0.34–0.41) | <0.001 | 85.7 | −0.00 to 0.66 |
t = 0.05 p = 0.959 |
0 studies added | ||
| Compared to unvalidated guilt measures | 0.74 | 0.391 | ||||||||
| Guilt measure | ||||||||||
| PTCI | 73 | 12 678 | 0.33 (0.28–0.37) | <0.001 | 84.4 | −0.04 to 0.62 |
t = −0.84 p = 0.405 |
18 studies added, radj = 0.40, 95% CI 0.35–0.44 | ||
| TRGI | 26 | 4579 | 0.37 (0.32–0.43) | <0.001 | 66.9 | 0.12–0.58 |
t = 0.10 p = 0.925 |
1 study added, radj = 0.36, 95% CI 0.31–0.42 | ||
| Brief COPE | 9 | 3505 | 0.45 (0.32–0.56) | <0.001 | 92.1 | 0.01–0.74 | n.a. | n.a. | ||
| RAQ | 7 | 2295 | 0.50 (0.36–0.63) | <0.001 | 84.2 | 0.07–0.78 | n.a. | n.a. | ||
| Omnibus test of subgroup differences | 10.24 | 0.017 | ||||||||
| PTCI: v. TRGI p = 0.225; v. Brief COPE p = 0.049; v. RAQ p = 0.007 | ||||||||||
| TRGI: v. Brief COPE p = 0.207; v. RAQ p = 0.042 | ||||||||||
| Brief COPE: v. RAQ p = 0.496 | ||||||||||
| Only high-quality studies | 21 | 3614 | 0.30 (0.24–0.36) | <0.001 | 65.8 | 0.08–0.50 |
t = −1.13 p = 0.274 |
6 studies added, radj = 0.36, 95% CI 0.30–0.42 | ||
| Compared to others | 7.89 | 0.005 | ||||||||
Note: For significant omnibus tests of subgroup differences, detailed comparisons of each subgroup are presented. CI, confidence interval; Brief COPE, Coping Orientation to Problems Experienced – brief version; IPV, intimate partner violence; MVA, motor-vehicle accident; PI, prediction interval; PTCI, Posttraumatic Cognitions Inventory; PTSD, posttraumatic stress disorder; RAQ, Rape Attribution Questionnaire; TRGI, Trauma-Related Guilt Inventory.
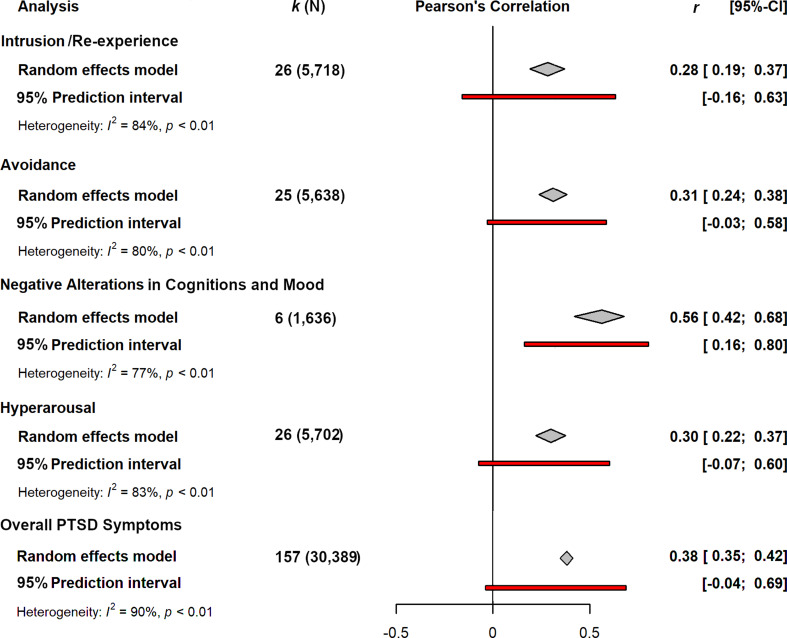
The association between guilt and individual PTSD symptom clusters was investigated in 27 studies, 20 of them based on DSM-IV and seven on DSM-5 criteria for PTSD. Moderate significant (all p < 0.001) associations were found for the intrusion/re-experience (r = 0.28, k = 26), avoidance (r = 0.31, k = 25) and hyperarousal cluster (r = 0.30, k = 26; Fig. 2). Omitting outliers changed the coefficients to r = 0.26 (k = 23), r = 0.32 (k = 20) and r = 0.25 (k = 19), respectively. The differences between the symptom clusters were not significant (p = 0.878).
Fig. 2.
Cross-sectional association between trauma-related guilt and PTSD symptoms.
Finally, the DSM-5 cluster of negative alterations in cognitions and mood yielded a strong association with guilt measures (r = 0.56, k = 6). This cluster was addressed separately as it includes guilt itself.
Predictive effect of guilt on PTSD symptoms
A total of 19 longitudinal studies including 2760 trauma survivors reported correlations or univariate regressions between guilt at baseline and PTSD symptoms at follow-up. Guilt was assessed between 7 days and 2 years post-trauma, PTSD symptoms between 3 months and 3 years post-trauma. Guilt significantly predicted PTSD symptoms yielding a small to moderate effect (r = 0.21; p < 0.001). There was substantial heterogeneity between studies (I2 = 66.7%), resulting in a wide prediction interval covering the null value. Three studies were identified as outliers, omitting them from analyses resulted in a marginally smaller association (r = 0.19; p < 0.001). Heterogeneity decreased (I2 = 36.0%), resulting in a significant 95% prediction interval ranging from 0.14 to 0.25.
Study quality
The Intraclass Correlation Coefficient (ICC) for all ratings and studies combined among the two raters was 0.93, indicating excellent inter-rater reliability. In total, 32.7% of studies included trauma survivors without indicating diagnostic status. Of those studies including a clinical sample (24.4%), the majority of diagnoses were established using a validated questionnaire or via referral from a psychiatric treatment unit (63.5%). In total, 22.6% used an unvalidated measure to assess guilt, i.e. an existing unvalidated questionnaire, a combination of items from existing questionnaires or items specifically developed for the purpose of the study. Single-item assessments were used in seven studies. The majority of studies did not report an a priori guilt-related power analysis (89.3%). Detailed quality ratings are presented in the online Supplementary Appendix J.
Sample-specific and methodological moderators
Results of subgroup analyses are presented in Table 1. Several significant sources of heterogeneity were detected. The relationship between guilt and PTSD symptoms was significantly influenced by trauma type. The largest effects were found for war-related trauma and trauma related to medical conditions (both r = 0.44) such as injuries or severe illnesses, the smallest effects regarding childhood sexual abuse and motor vehicle accidents (r = 0.21 and r = 0.18, respectively). Military samples, however, showed no different associations compared to civilians. Effect sizes for clinical samples with PTSD diagnoses established by validated interviews did not differ significantly from non-clinical samples. Finally, no heterogeneity was accounted by time since trauma. Percentage of females was entered in a meta-regression and showed no significant impact (p = 0.255).
Regarding methodological moderators, we found a significantly larger effect for DSM-5-based PTSD instruments. High-quality studies showed significantly smaller associations compared to the remaining studies. Given that the vast majority of studies did not report on relevant power analyses, this criterion was omitted from quality analyses. The validity of applied guilt measures alone explained no heterogeneity. Comparison of the four most frequently used guilt measures showed that type of guilt measure was a significant moderator (see Table 1).
Discussion
We aimed at providing a comprehensive meta-analytic review on the cross-sectional as well as longitudinal relationship between guilt and PTSD symptoms, while also investigating putative sample-specific and methodological moderators. Results from 157 cross-sectional studies including 30 389 trauma survivors yielded a moderate effect size, which was robust to sensitivity analyses. Associations with individual symptom clusters were all significant. There were no significant differences across the symptom clusters except for the DSM-5 cluster of negative alterations in cognitions and mood. Significant moderators of the overall relationship were trauma type and PTSD measures based on DSM-IV v. DSM-5. In addition, 19 studies with 2760 trauma survivors showed a moderate predictive relationship between guilt and PTSD symptoms, which was also robust to sensitivity analyses.
Overall effects
Our finding that increased guilt is positively associated with PTSD symptoms is in line with previous literature. Previous meta-analyses yielded a moderate association between self-blame appraisals and PTSD symptoms (r = 0.28; 95% CI 0.24–0.32; k = 57; Gómez de La Cuesta et al., 2019) and a moderate to strong association between trauma-related guilt and PTSD symptoms (r = 0.43; 95% CI 0.38–0.48; k = 45; Shi et al., 2021). Compared to Shi et al. (2021), our meta-analysis overlaps by only 14% of studies and included 135 additional ones. The significantly larger number of studies in our meta-analysis provides a strong explanatory power. In addition, our approach extends the reliability of previous findings on several accounts: First, we excluded effect sizes on guilt distress (i.e. severe emotional distress and strong physical sensations when thinking about what happened; Kubany et al., 1996) given its strong conceptual overlap with PTSD symptomatology. Second, we examined putative sample duplicates under consideration of involved research groups, recruitment place, methods, and time, grant numbers and contact with authors. Consequently, we excluded a total of 39 studies because of sample overlap. Third, we excluded studies on acute stress disorder and posttraumatic stress symptoms within one month following the traumatic event and focused on studies that assessed PTSD symptoms with validated measures based on DSM/ICD. Fourth, we differentiated between DSM-IV v. DSM-5 assessment of PTSD. Results suggest that, although the association is inflated by DSM-5 instruments, the effect remains significant when focusing on DSM-IV symptoms. Finally, we did not apply search restrictions and assessed studies irrespective of language. Our analyses on self-blame appraisals, as assessed with the PTCI, and PTSD symptoms yielded a larger effect compared to Gómez de La Cuesta et al. (2019). While our analysis included more studies (k = 57 v. k = 81), we excluded studies that involved individuals with schizophrenia as delusional guilt may be an associated feature of this disease (Gelkopf et al., 2013; O'Hare, Shen, & Sherrer, 2015). Furthermore, Gómez de La Cuesta et al. (2019) included and counted eight studies as separate data points although they had reported on the same three samples.
Theoretical considerations as well as empirical path analyses suggest that guilt may be linked to PTSD through avoidant coping strategies, implying that the association between guilt and the DSM avoidance cluster might be the strongest (Ehlers & Clark, 2000; Held, Owens, Schumm, Chard, & Hansel, 2011; Kubany, 1998; Norman, 2022; Pugh et al., 2015; Street, Gibson, & Holohan, 2005). While our findings show that guilt is significantly associated with avoidance symptoms, the degree of this association was not significantly stronger relative to the association with the other PTSD clusters. In fact, the DSM-5 cluster of negative alterations in cognitions and mood showed a significantly stronger correlation with guilt. This finding may, however, be explained by the fact that guilt and self-blame are part of this DSM-5 symptom cluster.
Altogether, the relationship between guilt and PTSD symptoms appeared smaller relative to other related constructs such as shame, anger or rumination (López-Castro, Saraiya, Zumberg-Smith, & Dambreville, 2019; Orth & Wieland, 2006; Shi et al., 2021; Szabo, Warnecke, Newton, & Valentine, 2017). Whereas guilt was not particularly linked to intrusion, avoidance or hyperarousal symptoms, findings on rumination suggest a particularly strong association with intrusive re-experiencing (Szabo et al., 2017). No such data exist for anger yet, however, it is assumed that anger might be particularly linked to hyperarousal by means of a physiological pathway (Orth & Wieland, 2006). The smaller correlation detected in the relationship between guilt and PTSD symptoms may reflect true differences among guilt and similar constructs. Yet, future research needs to investigate the extent to which methodological factors (e.g. trait v. state measures of these constructs, psychometric properties of PTSD measures or age of participants) may also be responsible for the reported differences. In addition, the conceptual overlap between guilt, shame, anger and rumination needs to be considered when interpreting results (e.g. angry rumination; Denson, 2013).
In their systematic review, Pugh et al. (2015) considered guilt and PTSD to be co-occurring, yet causally unrelated products of trauma. Our findings on the predictive association indicate that guilt may play a causal role in the development of PTSD. Yet, this interpretation requires caution since we did not calculate extensive mediation models to examine whether guilt mediates the relationship between trauma exposure and PTSD symptoms.
The quality of evidence based on our self-developed quality appraisal tool was mixed. With regard to psychopathology, only a quarter of studies included clinical samples while a third of studies focused on trauma survivors regardless of their diagnostic status. However, we did not detect a significant difference in effect sizes for clinical v. non-clinical samples, suggesting that the association between guilt and PTSD might be similar for both clinical and subclinical PTSD. Given that the use of a validated PTSD instrument was required for inclusion in the meta-analysis, quality of the assessment of PTSD symptoms was high with almost all instruments having been validated in clinical samples. The quality of the assessment of guilt was sufficient with three-quarters of used instruments having been validated in trauma populations. In addition, while the vast majority of studies did not report adequate power analyses, the high number of included studies suggests that the overall power of the meta-analysis is rather sufficient.
Moderator effects
As opposed to Shi et al. (2021), we did not find military populations to display a stronger relationship between guilt and PTSD. Type of trauma, however, explained a significant amount of heterogeneity with war-related trauma (i.e. not limited to combat) yielding the largest effects. Trauma related to motor-vehicle accidents yielded the smallest association. Research suggests that women display both a higher prevalence of PTSD (Olff, Langeland, Draijer, & Gersons, 2007; Tolin & Foa, 2006) as well as higher guilt scores relative to men (Cohen, Panter, & Turan, 2012). Yet, we did not detect a significant gender effect with respect to the relationship between guilt and PTSD symptoms. One potential explanation for this finding might relate to the different definitions and measurements of guilt. Women may display higher dispositional guilt, yet meta-analytic results suggest no such gender differences in situation-specific self-blame coping (Tamres, Janicki, & Helgeson, 2002). The latter relates more to trauma-related guilt as investigated in the studies included in our meta-analysis. Time since trauma was not a significant moderator, suggesting a stable association over time. The results, however, require caution as they might be subject to publication bias. Type of guilt measure had a significant influence on effect sizes with largest associations for studies including the RAQ and smallest associations for studies including the PTCI. These results may suggest a bias given that the RAQ is insufficiently validated, whereas the PTCI has been extensively validated in many languages. Yet, we could not find a general difference between validated v. unvalidated guilt measures. Use of a validated guilt measure and inclusion of a clinical sample did not appear to have a stand-alone influence on results and studies were very homogeneous regarding validation of the PTSD measure. Yet, it is important to notice that the overall quality of studies accounted for a significant amount of heterogeneity with high-quality studies displaying smaller associations.
Clinical implications
Our results emphasise the necessity to consider associated features of PTSD within treatment, including guilt. The finding that guilt predicts PTSD when assessed both within days and after several months following the traumatic event, suggests that guilt plays a significant role in the onset and maintenance of PTSD. As the association appears to be stable over time, one's role in a traumatic event should be considered when elaborating the event, irrespective of time since the traumatic event. This may be especially important regarding specific types of traumatic events including war-related trauma. Findings with veteran samples indicate that direct personal involvement during the traumatic event is associated with greater guilt, potentially by inducing a stronger perceived responsibility and sense of wrongdoing (Pugh et al., 2015). Yet, our findings suggest that appraisals of having personally done something wrong are not to be limited to such traumatic events. Guilt related to severe medical conditions including strokes or severe illnesses also showed a significant association with PTSD symptoms. Thus, our findings suggest that treatment of PTSD may benefit from addressing guilt regardless of the nature of the patient's traumatic history.
Limitations and future research
To better understand the predictive relationship between guilt and PTSD, meta-analytic mediation analyses are needed, which were impeded by the limited number of studies providing eligible data. Furthermore, we conducted one-sided predictive analyses and did not assess to what extent PTSD symptoms, or their consequences, may lead to guilt. We considered bias in sensitivity analyses both on individual study level as well as on group level and tried to limit publication bias by including both published and unpublished studies. Regarding our main effects, trim and fill analyses suggested missing studies with large effect sizes, resulting in a larger adjusted association of r = 0.44. On the other hand, we observed a contrary file drawer problem within reviewed studies. Several studies reported insignificant associations between guilt and PTSD without specifying coefficients. These studies could not be included or only included in limited analyses, because we were not able to obtain further data from the authors (Feinstein, Pavisian, & Storm, 2018; Hiskey, Ayres, Andrews, & Troop, 2015; Hu, Liang, Hu, Long, & Ge, 2000; Merecz-Kot, Wężyk, Waszkowska, & Andysz, 2020; Wenninger & Ehlers, 1998). Although our subgroup analyses detected several significant moderators, other recommended putative variables did not appear to have an influence on our results. Heterogeneity remained large in all analyses suggesting that sources of heterogeneity remained unknown. The large heterogeneity in results furthermore involves a large number of statistical outliers based on our criteria. We aimed at limiting inflated effect sizes by conducting separate analyses for DSM-IV v. DSM-5 PTSD instruments. However, some of the included measures of PTSD that were based on DSM-IV include guilt-related items as well (e.g. the CAPS; Blake et al., 1995). The provided data did not allow for removal of the guilt-related items from the mean scores of the respective PTSD instrument. Combining studies on guilt and self-blame appraisals is in line with previous meta-analyses and theoretical models of guilt. Yet, more research is needed to increase our knowledge on the role of self-blame as the cognitive component of guilt in trauma survivors. Finally, in order to enhance PTSD treatment, further treatment studies are essential to understand the relationship between changes in trauma-related guilt and PTSD symptoms as well as the mechanisms of change within treatment.
Conclusion
This meta-analysis found a moderate cross-sectional association between trauma-related guilt and PTSD in adult trauma survivors. This relationship was robust to sensitivity analyses and varied significantly by trauma type, study quality, guilt measure and DSM version underlying the PTSD measure. Longitudinal studies, although limited in number, also suggest that guilt plays a significant role in the onset and maintenance of PTSD. Apart from negative alterations in cognitions and mood, guilt was not specifically related to individual PTSD symptom clusters. While these findings have important clinical implications, more studies are needed to examine the change interactions during treatment.
Acknowledgements
We thank Michelle Bovin and Suzanne Pineles for sharing unpublished data with us. We furthermore thank all contacted authors who provided additional information regarding coefficients or sample overlaps. Finally, we thank Lena Polmann for assisting in quality ratings.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291722001866.
click here to view supplementary material
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
References
- Allard, C. B., Norman, S. B., Thorp, S. R., Browne, K. C., & Stein, M. B. (2018). Mid-treatment reduction in trauma-related guilt predicts PTSD and functioning following cognitive trauma therapy for survivors of intimate partner violence. Journal of Interpersonal Violence, 33(23), 3610–3629. doi: 10.1177/0886260516636068. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (1987). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. Retrieved from doi: 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. The Cochrane Database of Systematic Reviews, 2013(12), CD003388. doi: 10.1002/14651858.CD003388.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8(1), 75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bland, J. M., & Altman, D. G. (1997). Cronbach's alpha. BMJ, 314, 572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin, M. J., Dodson, T. S., Smith, B. N., Gregor, K., Marx, B. P., & Pineles, S. L. (2014). Does guilt mediate the association between tonic immobility and posttraumatic stress disorder symptoms in female trauma survivors? Journal of Traumatic Stress, 27(6), 721–724. doi: 10.1002/jts.21963. [DOI] [PubMed] [Google Scholar]
- Brewin, C. R., Dalgleish, T., & Joseph, S. (1996). A dual representation theory of posttraumatic stress disorder. Psychological Review, 103(4), 670–686. doi: 10.1037/0033-295X.103.4.670. [DOI] [PubMed] [Google Scholar]
- Browne, K. C., Trim, R. S., Myers, U. S., & Norman, S. B. (2015). Trauma-related guilt: Conceptual development and relationship with posttraumatic stress and depressive symptoms. Journal of Traumatic Stress, 28(2), 134–141. doi: 10.1002/jts.21999. [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Morrow, C. E., Etienne, N., & Ray-Sannerud, B. (2013). Guilt, shame, and suicidal ideation in a military outpatient clinical sample. Depression and Anxiety, 30(1), 55–60. doi: 10.1002/da.22002. [DOI] [PubMed] [Google Scholar]
- Carver, C. S. (1997). You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4(1), 220–223. doi: 10.7560/734166-019. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). New York, NY: Erlbaum. [Google Scholar]
- Cohen, T. R., Panter, A. T., & Turan, N. (2012). Guilt proneness and moral character. Current Directions in Psychological Science, 21(5), 355–359. doi: 10.1177/0963721412454874. [DOI] [Google Scholar]
- Cunningham, K. C., Davis, J. L., Wilson, S. M., & Resick, P. A. (2018). A relative weights comparison of trauma-related shame and guilt as predictors of DSM-5 posttraumatic stress disorder symptom severity among US veterans and military members. The British Journal of Clinical Psychology, 57(2), 163–176. 10.1111/bjc.12163 . [DOI] [PubMed] [Google Scholar]
- Denson, T. F. (2013). The multiple systems model of angry rumination. Personality and Social Psychology Review, 17(2), 103–123. doi: 10.1177/1088868312467086. [DOI] [PubMed] [Google Scholar]
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Feinstein, A., Pavisian, B., & Storm, H. (2018). Journalists covering the refugee and migration crisis are affected by moral injury not PTSD. JRSM Open, 9(3), 1–7. doi: 10.1177/2054270418759010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa, E. B., Cashman, L., Jaycox, L., & Perry, K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9(4), 445–451. doi: 10.1037/1040-3590.9.4.445. [DOI] [Google Scholar]
- Foa, E. B., Ehlers, A., Clark, D. M., Tolin, D. F., & Orsillo, S. M. (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. doi: 10.1037/1040-3590.11.3.303. [DOI] [Google Scholar]
- Frazier, P. A. (2003). Perceived control and distress following sexual assault: A longitudinal test of a new model. Journal of Personality and Social Psychology, 84(6), 1257–1269. doi: 10.1037/0022-3514.84.6.1257. [DOI] [PubMed] [Google Scholar]
- Gelkopf, M., Roe, D., Werbeloff, N., Hasson-Ohayon, I., Mueser, K. T., Caspi, A., & Weiser, M. (2013). The prevalence of full and partial posttraumatic stress disorder among people with severe mental illness in Israel. The Journal of Nervous and Mental Disease, 201(3), 244–250. doi: 10.1097/NMD.0b013e3182848d1e. [DOI] [PubMed] [Google Scholar]
- Gómez de La Cuesta, G., Schweizer, S., Diehle, J., Young, J., & Meiser-Stedman, R. (2019). The relationship between maladaptive appraisals and posttraumatic stress disorder: A meta-analysis. European Journal of Psychotraumatology, 10(1), 1–15. doi: 10.1080/20008198.2019.1620084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer, M., Cuijpers, P., Toshi, A., Furukawa, D., & Ebert, D. (2021). Doing meta-analysis in R: A hands-on guide. Boca Raton, FL; London: Chapman & Hall/CRC Press. [Google Scholar]
- Held, P., Owens, G. P., Schumm, J. A., Chard, K. M., & Hansel, J. E. (2011). Disengagement coping as a mediator between trauma-related guilt and PTSD severity. Journal of Traumatic Stress, 24(6), 708–715. doi: 10.1002/jts.20689. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiskey, S., Ayres, R., Andrews, L., & Troop, N. (2015). Support for the location of negative posttraumatic cognitions in the diagnosis of posttraumatic stress disorder. Personality and Individual Differences, 74, 192–195. doi: 10.1016/j.paid.2014.10.021. [DOI] [Google Scholar]
- Hu, B. S., Liang, Y. X., Hu, X. Y., Long, Y. F., & Ge, L. N. (2000). Posttraumatic stress disorder in co-workers following exposure to a fatal construction accident in China. International Journal of Occupational and Environmental Health, 6(3), 203–207. doi: 10.1179/oeh.2000.6.3.203. [DOI] [PubMed] [Google Scholar]
- Jellestad, L., Vital, N. A., Malamud, J., Taeymans, J., & Mueller-Pfeiffer, C. (2021). Functional impairment in posttraumatic stress disorder: A systematic review and meta-analysis. Journal of Psychiatric Research, 136, 14–22. doi: 10.1016/j.jpsychires.2021.01.039. [DOI] [PubMed] [Google Scholar]
- Knapp, G., & Hartung, J. (2003). Improved tests for a random effects meta-regression with a single covariate. Statistics in Medicine, 22, 2693–2710. doi: 10.1002/sim.1482. [DOI] [PubMed] [Google Scholar]
- Kubany, E. S. (1998). Cognitive therapy for trauma-related guilt. In Follette V. M. & Ruzek J. I. (Eds.), Cognitive-behavioral therapies for trauma (pp. 124–161). New York, NY: The Guilford Press. [Google Scholar]
- Kubany, E. S., Haynes, S. N., Abueg, F. R., Manke, F. P., Brennan, J. M., & Stahura, C. (1996). Development and validation of the trauma-related guilt inventory (TRGI). Psychological Assessment, 8(4), 428–444. [Google Scholar]
- Kubany, E. S., & Manke, F. P. (1995). Cognitive therapy for trauma-related guilt: Conceptual bases and treatment outlines. Cognitive and Behavioral Practice, 2(1), 27–61. doi: 10.1016/S1077-7229(05)80004-5. [DOI] [Google Scholar]
- Kubany, E. S., & Watson, S. B. (2003). Guilt: Elaboration of a multidimensional model. The Psychological Record, 53(1), 51–90. [Google Scholar]
- Larsen, S. E., Fleming, C. J. E., & Resick, P. A. (2019). Residual symptoms following empirically supported treatment for PTSD. Psychological Trauma, 11(2), 207–2015. doi: 10.1037/tra0000384. [DOI] [PubMed] [Google Scholar]
- Lee, D. A., Scragg, P., & Turner, S. (2001). The role of shame and guilt in traumatic events: A clinical model of shame-based and guilt-based PTSD. British Journal of Medical Psychology, 74(4), 451–466. doi: 10.1348/000711201161109. [DOI] [PubMed] [Google Scholar]
- Lewis, H. B. (1971). Shame and guilt in neurosis. Psychoanalytic Review, 58(3), 419–438. [PubMed] [Google Scholar]
- Lewis, M. (2008). Self-conscious emotions: Embarrassment, pride, shame, and guilt. In Lewis M., Haviland-Jones J. M. & Barrett L. F. (Eds.), Handbook of emotions (pp. 742–756). New York, NY: Guilford Press. [Google Scholar]
- Lewis, M. (2014). The rise of consciousness and the development of emotional life. New York, NY: Guilford Press. [Google Scholar]
- López-Castro, T., Saraiya, T., Zumberg-Smith, K., & Dambreville, N. (2019). Association between shame and posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 32(4), 484–495. doi: 10.1002/jts.22411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy, P. A., & Morina, N. (2020). Exploring the association of social comparison with depression and anxiety: A systematic review and meta-analysis. Clinical Psychology & Psychotherapy, 27(5), 640–671. doi: 10.1002/cpp.2452. [DOI] [PubMed] [Google Scholar]
- Merecz-Kot, D., Wężyk, A., Waszkowska, M., & Andysz, A. (2020). Wstyd, poczucie winy, perspektywa czasowa, czas odbywania kary pozbawienia wolności i objawy PTSD u skazanych sprawców wypadków drogowych – doniesienie wstępne [Shame, guilt, time perspective, time of imprisonment and PTSD symptoms in sentenced motor vehicle accidents perpetrators – a preliminary report]. Psychiatria Polska, 54(6), 1163–1180. doi: 10.12740/PP/113555. [DOI] [PubMed] [Google Scholar]
- Miller, M. W., Wolf, E. J., Kilpatrick, D., Resnick, H., Marx, B. P., Holowka, D. W., … Friedman, M. J. (2013). The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychological Trauma, 5(6), 501–512. doi: 10.1037/a0029730. [DOI] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), 1–6. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morina, N., Hoppen, T. H., & Kip, A. (2021). Study quality and efficacy of psychological interventions for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Psychological Medicine, 51(8), 1260–1270. doi: 10.1017/S0033291721001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, H. L. (2018). Survivor guilt in a posttraumatic stress disorder clinic sample. Journal of Loss and Trauma, 23(7), 600–607. doi: 10.1080/15325024.2018.1507965. [DOI] [Google Scholar]
- Norman, S. (2022). Trauma-informed guilt reduction therapy: Overview of the treatment and research. Current Treatment Options in Psychiatry, Advance online publication. doi: 10.1007/s40501-022-00261-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman, S. B., Haller, M., Kim, H. M., Allard, C. B., Porter, K. E., Stein, M. B., … Rauch, S. A. M. (2018). Trauma related guilt cognitions partially mediate the relationship between PTSD symptom severity and functioning among returning combat veterans. Journal of Psychiatric Research, 100, 56–62. doi: 10.1016/j.jpsychires.2018.02.003. [DOI] [PubMed] [Google Scholar]
- Norman, S. B., Wilkins, K. C., Myers, U. S., & Allard, C. B. (2014). Trauma informed guilt reduction therapy with combat veterans. Cognitive and Behavioral Practice, 21(1), 78–88. doi: 10.1016/j.cbpra.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally, J., & Bernstein, L. (1994). Psychometric theory. New York, NY: McGraw-Hill. [Google Scholar]
- O'Hare, T., Shen, C., & Sherrer, M. V. (2015). Lifetime abuse and self-harm in people with severe mental illness: A structural equation model. Psychological Trauma: Theory, Research, Practice and Policy, 7(4), 348–355. doi: 10.1037/tra0000016. [DOI] [PubMed] [Google Scholar]
- Øktedalen, T., Hoffart, A., & Langkaas, T. F. (2015). Trauma-related shame and guilt as time-varying predictors of posttraumatic stress disorder symptoms during imagery exposure and imagery rescripting – a randomized controlled trial. Psychotherapy Research, 25(5), 518–532. doi: 10.1080/10503307.2014.917217. [DOI] [PubMed] [Google Scholar]
- Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. R. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Orth, U., & Wieland, E. (2006). Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology, 74(4), 698–706. doi: 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan – a web and mobile app for systematic reviews. Systematic Reviews, 5(210), 1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsopoulos, N. A., Evangelou, E., & Ioannidis, J. P. A. (2008). Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. International Journal of Epidemiology, 37(5), 1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh, L. R., Taylor, P. J., & Berry, K. (2015). The role of guilt in the development of post-traumatic stress disorder: A systematic review. Journal of Affective Disorders, 182, 138–150. doi: 10.1016/j.jad.2015.04.026. [DOI] [PubMed] [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Rosenthal, R., & Rubin, D. B. (1986). Meta-analytic procedures for combining studies with multiple effect sizes. Psychological Bulletin, 99(3), 400–406. doi: 10.1037/0033-2909.99.3.400. [DOI] [Google Scholar]
- Shi, C., Ren, Z., Zhao, C., Zhang, T., & Chan, S. H.-W. (2021). Shame, guilt, and posttraumatic stress symptoms: A three-level meta-analysis. Journal of Anxiety Disorders, 82, 102443. doi: 10.1016/j.janxdis.2021.102443. [DOI] [PubMed] [Google Scholar]
- Street, A. E., Gibson, L. E., & Holohan, D. R. (2005). Impact of childhood traumatic events, trauma-related guilt, and avoidant coping strategies on PTSD symptoms in female survivors of domestic violence. Journal of Traumatic Stress, 18(3), 245–252. doi: 10.1002/jts.20026. [DOI] [PubMed] [Google Scholar]
- Szabo, Y. Z., Warnecke, A. J., Newton, T. L., & Valentine, J. C. (2017). Rumination and posttraumatic stress symptoms in trauma-exposed adults: A systematic review and meta-analysis. Anxiety, Stress, and Coping, 30(4), 396–414. doi: 10.1080/10615806.2017.1313835. [DOI] [PubMed] [Google Scholar]
- Tamres, L. K., Janicki, D., & Helgeson, V. S. (2002). Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personality and Social Psychology Review, 6(1), 2–30. doi: 10.1207/S15327957PSPR0601_1. [DOI] [Google Scholar]
- Tangney, J. P., & Dearing, R. L. (2002). Shame and guilt. New York, NY: Guilford Press. [Google Scholar]
- Tilghman-Osborne, C., Cole, D. A., & Felton, J. W. (2010). Definition and measurement of guilt: Implications for clinical research and practice. Clinical Psychology Review, 30(5), 536–546. doi: 10.1016/j.cpr.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Retrieved from https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp#obtain.
- Wenninger, K., & Ehlers, A. (1998). Dysfunctional cognitions and adult psychological functioning in child sexual abuse survivors. Journal of Traumatic Stress, 11(2), 281–300. doi: 10.1023/A:1024451103931. [DOI] [PubMed] [Google Scholar]
- Wilson, J. P., Drozdek, B., & Turkovic, S. (2006). Posttraumatic shame and guilt. Trauma, Violence & Abuse, 7(2), 122–141. doi: 10.1177/1524838005285914. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291722001866.
click here to view supplementary material