Abstract
Demodex mites are common ectoparasites of the human pilosebaceous units. Most adults are infested with Demodex mites without clinical symptoms. Demodex mite will only become a pathogenic organism when there is an abnormal increase in the number of Demodex mite density. This situation happens when the equilibrium between Demodex mites, skin microenvironment and human immunity system changes. Demodex infestation can cause multiple skin disorders, which are grouped under the term demodicosis or demodicidosis. Clinical manifestations of demodicosis can mimic other known skin diseases such as folliculitis, rosacea, perioral dermatitis, which is why it is often misdiagnosed. Diagnosis criteria consists of relevant correlation of suspected clinical skin lesions, confirmed by the presence of abnormal proliferation of Demodex mites and by clinical cure after acaricidal treatment together with normalization of Demodex mite density. Dermatologists should be aware that demodicosis is not an uncommon skin disease, and there are still many unknowns about it that should be researched further.
Key words: Demodex mite, Demodicosis, Demodex
Introduction
Humans do not live alone on this planet, as there are many types of microorganisms living together with humans. Some of these microorganisms have been associated with the skin and mucous membrane of humans since birth, much like a close friend. Most of these are bacteria, but there are also fungi, intestinal worm and mite. Demodex mites are common ectoparasites of the human hair follicles and usually do not cause any clinical symptoms. However, on some occasions, Demodex mite may be the main cause of many skin disorders, turning it from a close friend into the worst enemy.
Demodex mite
Demodex is a genus of mites that live in the pilosebaceous unit of mammals. They are highly host specific and obligate commensals. Different species of animal hosts has different species of Demodex mites. Only two species of Demodex mite lives on the human skin, D. folliculorum is found in hair follicle and D. brevis lives in sebaceous gland connected to hair follicles (Figure1). Demodex mites have a tendency to reside in vellus sebaceous follicles that have more sebum producing cells. Both species are primarily found in the face, paranasal area, eyelashes, or eyebrows, but D. brevis has a wider distribution on other parts of the body.1 Demodex mites cannot be found in newborn skin. Sebaceous follicles will colonize during the late childhood and early adulthood via transmission from adult family members. The adult mites are only 0.3-0.4 mm in length, with D. folliculorum being slightly longer than D. brevis. Demodex mite has semitransparent elongated body composing of two segments, short eight legs protruding from the upper segment and the lower segment which addresses genital organs and gastrointestinal organs (without anus). Its body surface is covered with scales for anchoring itself in hair follicle or sebaceous gland. The mite has pin-like mouth part for eating oils in hair follicle and using lipase enzymes for digestion.2 There are also a lot of bacteria on the surface of Demodex mite that can stimulate an inflammatory response in patients.3 Female mites are larger and rounder than males. Mating takes place in the hair follicle opening, and eggs are laid inside the hair follicle. The six-legged larvae hatch after 3-4 days, and develop into adults in about 7 days. Spickett studied about Demodex mite and presented that the life cycle of D. folliculorum was about 14.5 days.4 The dead mites decompose inside the hair follicles or sebaceous glands. The total lifespan of a Demodex mite is several weeks (Figure 2).
Demodex mites can be transmitted from one person to another via direct skin contact. Makeup cosmetics used by different persons at short intervals (from several hours to several days) can also be a source of transmission of Demodex mites.5
Prevalence
Demodex mites are common ectoparasites in human skin, the number of mites increases with age. Demodex mites are found in about one third of children and young adults, half of adults, and two-thirds of elderly people.6 The lower rate in children is probably caused by immature sebaceous glands. Demodex mites is found to be significantly more prominent in obese, high blood sugar levels, end stage chronic renal failure and immunocompromised patients.7-9 Increased numbers of Demodex mites have been reported following repeated facial application of topical steroids and other immunomodulators.10 Facial skin microenvironment, moisture, pH levels, types and quantities of skin surface lipids and epidermal barrier function may facilitate Demodex mite proliferation.11 Study by Thoemmes in 2014, using DNA-detection method for Demodex mite detection, found that 100% of adults (over 18 years of age) and 70% of children and young adults carried Demodex mites.12 Surprisingly, human cadaver study has found Demodex mites on facial skin up to 100% of all findings except for newborns.13 This study suggested that previous studies might have underestimated the prevalence of Demodex mites. Demodex mites are transmitted between hosts with high host specificity. There are few reports showing transmission of dog mites to their owners, but non definite evidence has confirmed that the Demodex mite species was D. canis.14 Differentiation of Demodex mite species is usually based on morphology, but within the same species, different morphologies can occur. DNA polymerase chain reaction has been used as a definite method to identify and differentiate Demodex mite species.15 In addition, the research study also found that D. canis can survive and reproduce in dog skin engrafted onto SCID mice but did not spread to the surrounding mouse skin.16
Immune response
There is a correlation between the frequency of HLA Cw2 and Cw4 haplotypes and the incidence of demodicosis. The risk of developing clinical symptoms of this disease is 5 times higher for people with the Cw2 phenotype and 3 times higher for those with the Cw4 haplotype. This study also found an association between Cw2 and Cw4 alleles in the phenotype of patients with demodicosis and a decrease in the number of natural killer cells.17 From another research study, it was found that the absolute number of CD3+, CD4+, CD8+ and CD16+ cells, the ratio CD3+/CD20+ and the functional activity of leukocytes were significantly lower in individuals infested with Demodex mites. On the contrary, no significant differences were found in the percentage and absolute number of CD20+ cells, circulating immune complexes, activity and index of phagocytosis and the levels of IgA, IgM and IgG antibodies between individuals infested with Demodex mites and the control group.18
Genetic and human cellular immunity played a major role in protection against demodicosis. Demodex mites have the ability to modify human immunity so that they can survive and live on the human skin without being destroyed by human immunity system.17-19
Pathogenesis
Pathogenesis of demodicosis is not well established and is still a controversial topic. Demodex mites live in balance with the human immune system in the appropriate microenvironment. Human immune system has an inhibitory effect on Demodex mite proliferation, keeping numbers under control without inducing an inflammatory reaction or any clinical symptoms. On the contrary, Demodex mites can also cause local immunosuppression, which allows them to survive in human skin.18 This balancing system consists of microenvironment, Demodex mites and human immunity system. Whenever this equilibrium changes, it can cause clinical symptoms of demodicosis. Reduction of local immune system as previously reported in patients who have been repeating facial application of topical steroids and other immunomodulators resulted in an increased number of Demodex mites on their faces.19,20 Changes in microenvironment of the facial skin can also change the number of Demodex mites. Studies have shown that rosacea patients have an increase in facial pH and a decrease in skin surface hydration levels, together with an abnormal fatty acid composition of their skin surface lipid layer.21,22 All of these reasons could be the cause of why rosacea patients have high density of Demodex mites on their facial skin.23 Balancing between Demodex mites and another commensal microorganism inhabiting the pilosebaceous unit such as Malassezia yeast and Propionibacterium acnes may change sebum components in hair follicle and affect the proliferation of Demodex mites.22 The abnormal proliferation of demodex mites can cause inflammation. Demodex mites use lipase enzymes to digest lipid material from sebum. This lipase enzymes also play a role in digesting bacteria or other microorganisms in hair follicles.24 This process can cause degradation of the follicular epithelium, elevated numbers of Demodex mites which cause greater hair follicular destruction and perifollicular inflammation.25 Demodex mites act as a carrier of Bacillus oleronius bacteria, which probably functions as a co-pathogen in the development of inflammatory process in rosacea by neutrophil induction and activation. 18,26 It was also found that Demodex mites can cause mechanical blockage of hair follicles and sebaceous glands by an increased number of mites, resulting in cutaneous barrier disruption and tissue damage. Dying mites release chitinous exoskeletons and internal mite contents, including bacterial antigens cause an increase in TLR-2 expression, trigger an inflammatory reaction27-29 resulting in an immune response followed by neutrophil and macrophage activation.30-32 During this time, Demodex mite acts as a pathogenic organism. This situation will start the inflammatory process, cytokine secretion may initiate a humoral immune inflammatory response that causes demodicosis.33 The clinical symptoms and severity of demodicosis can vary from nonspecific dry sensitive skin, papulopustular lesions, nodular lesions to granulomatous lesions, depending on number of demodex mites, skin microenvironment and immunity response of the patients.
Figure 1.
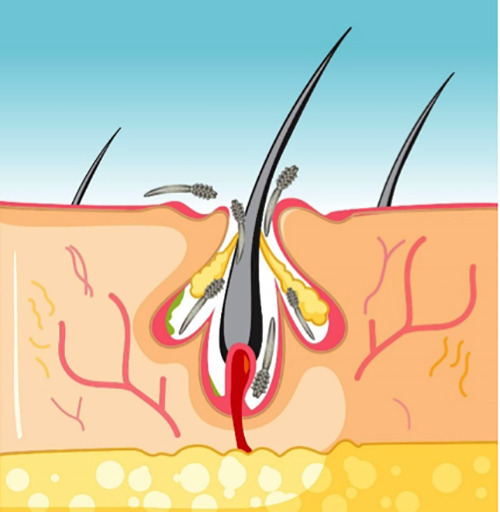
Demodex mites.
Figure 2.
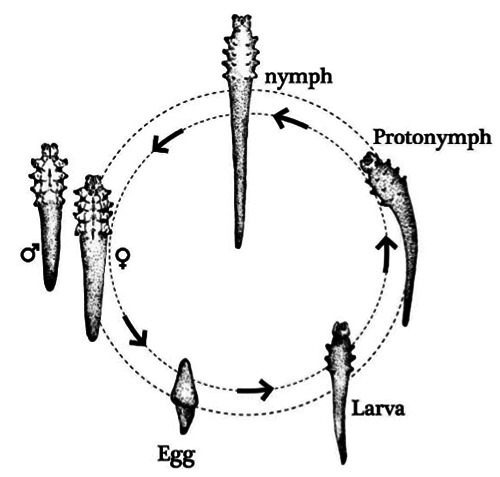
Life cycle of Demodex mite.
Figure 3.
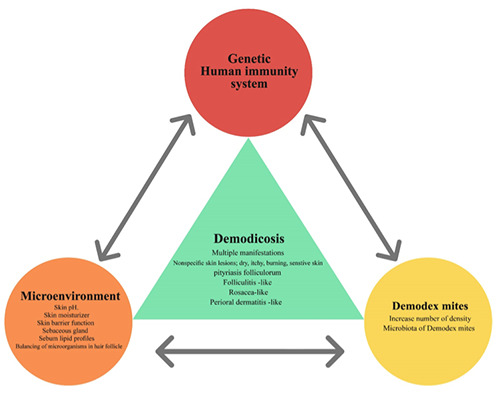
Pathogenesis of Demodicosis.
Pathogenesis diagram of demodicosis is presented in Figure 3.
Clinical presentation
Demodex infestation can cause multiple skin disorders, which are grouped under the term demodicosis or demodicidosis. Demodicosis has various clinical features based on the literature. Pityriasis folliculorum type (Figure 4) manifests as erythematous patch with dry, rough skin due to the increased scale within hair follicle on the face.34,45 Rosacea-like type (Figure 5) consists of dry, itchy, burning erythematous skin with papulopustular lesions involving the face of patients with or without pre-existing rosacea.36 Folliculitis-like type (Figure 6) is described as localized follicular pustules clinically mimicking acne or folliculitis.35,37 Perioral dermatitis-like type (Figure 7) showed the appearance of papulopustular lesions involving the perioral area like perioral dermatitis.38 The most common clinical type was pityriasis folliculorum, followed by rosacea-like type and perioral dermatitis- like type.38 Demodicosis can also be presented with dry scaly, itchy, hypersensitivity skin,39 burning sensation, unexplained eczema, papulopustular lesions,34,40 scalp pruritus, dandruff, scalp folliculitis,41,42 seborrheic dermatitis-like lesion,35 Demodex folliculitis,43 Demodex abscess,44 granulomatous rosacea- like lesion,45 eosinophilic folliculitis-like lesion46, otitis externa- auricular demodex47 and vulvar democidosis48. It was also found that there is a significant correlation between demodicosis and long-term inappropriate usage of topical steroid on the face.49,50 Demodex mites play a major role in many eye diseases such as, blepharitis, eyelid dermatitis, madarosis (loss of eyelashes), dry eye, meibomian gland dysfunction and chalazion.51-53 Demodicosis patients have higher numbers of eyelash mites, and significantly higher rates of blepharitis than the control group. Therefore, all demodicosis patients should also be examined for eyelash mites to prevent possible chronic blepharitis.21 Demodicosis is a common skin disease with multiple clinical presentations but is usually underdiagnosed.49,54 The definition and classification of demodicosis are still being debated.55,56 In particular, patients with a history of long-term inappropriate usage of topical steroid on their face, shows clinical symptoms as steroid-induced dermatitis or steroid addiction dermatitis should be evaluated for demodicosis.49,50
Figure 4.

Pityriasis folliculorum type.
Figure 5.

Rosacea-like type.
Figure 6.

Folliculitis-like type.
Figure 7.

Perioral dermatitis-like type.
Figure 8.

Superficial needle-scraping method with Gram stain.
Diagnosis
High density of Demodex mites is considered to play a pathogenic role in demodicosis. Therefore, the method used to determine the mite density per square centimeter is important for diagnosing demodicosis. Standardized skin surface biopsy (SSSB) and direct microscopic examination (DME) are commonly used to determine Demodex mite density. Standardized Skin Surface Biopsy is the most widely used method, starting with drawing a square shape measuring 1 cm2 area on one side of slide, dropping cyanoacrylic glue on the other side of the slide and then applying adhesive-bearing surface to the lesional skin. After allowing the adhesive to dry, the slide is removed, add one drop of oil and covered with a cover slip.23,38 Direct microscopic examination (DME) will be performed by selecting 1 cm2 sized lesional skin area and squeezing with a comedone extractor. The sample obtained is then transferred to a 10% potassium hydroxide drop and covered with a cover slip.38 Samples obtained from both methods will be studied under an optical microscope for Demodex mite counting. Demodicosis is diagnosed when there is a high density of demodex mites (> 5D/cm2).23 Forton suggested a new method for facial Demodex mite density detection by 2 consecutive standardized skin surface biopsies. The cut-off value of 2 consecutive SSSB is >10 D/cm2 and >15 D/ cm2 for combination single SSSB and 2 consecutive SSSB. The depth of 2 consecutive SSSB method is deeper than SSSB method. This also explains why Demodex mite density from this method were much higher than those detected with only one SSSB, suggesting that the majority of the D. folliculorum are located deep in the hair follicles.57 Huang proposed a method for assessing Demodex mite density in papulopustular rosacea (PPR) called “superficial needlescraping” (SNS) method, performed by gently scraping off 5 small pustules with the convex surface of the tip of number 18 needle for examination. Demodex density was reported as “mites per 5 pustules” for SNS. Demodicosis is diagnosed when there is a high density of demodex mites ≥3 Demodex mites per 5 pustules.58 The author proposes to use superficial needle-scraping method with Gram stain combine with Standardized Skin Surface Biopsy for evaluation of Demodex-associated facial papulopustular eruptions. This combined method can increase the ability of Demodex mite detection and rule out other causative organisms at the same time (Figure 8).
There are also two new Demodex mite detection and quantification methods. Dermoscopy is a non-invasive real time method which directly contacts with lesional skin, typically shows gelatinous filaments protruding out of follicular openings known as “Demodex tails” and “Demodex follicular openings” identified as dilated follicular openings containing round, amorphic, grayish plugs surrounded by erythematous halo.59 Confocal laser scanning microscope (CLSM) is an efficient method for detecting facial Demodex, and is advantageous as it is a noninvasive, realtime detection.60 Both methods can be useful in diagnosing and monitoring treatment of Demodicosis. Demodicosis is a multifactorial disease, it is not only the abnormal proliferation of Demodex mites, but also changes in skin microenvironment and host immunity. In general, demodicosis patients will have more severity of clinical symptoms when the number of Demodex mite density is high, but does not happen in all severe cases.38 In contrast, persons with normal skin may have a high number of Demodex mite density without any clinical symptoms of Demodicosis.6 From research study, a significant clinical healing of demodicosis and density of D. folliculorum at <5 D/cm2 was not determined in all patients after treatment.34 All of these happened primarily by host immunity response of the patients.
Erbagci and Ozgoztasi suggested that a certain density might not be an appropriate criterion in the diagnosis of rosacea; nevertheless, large numbers of D. folliculorum may have an important role in the pathogenesis of rosacea, together with other stimulating factors.33
The specific number of Demodex mite density should not be a determinant, because Demodex mites can leave the hair follicles and walk around on the skin surface at the speed of 8-16 cm per hour,61 and most of Demodex mites are located deep in the hair follicles, but SSSB can only detect demodex mites on the skin surface.57 This could give rise to false negative results regarding the measurement of Demodex mites.62 Many studies have shown that there were also differences in the number of Demodex mites found from different testing methods.38,63
Diagnosis criteria should therefore consist of relevant correlation of suspected clinical skin lesions, confirmed by the presence of abnormal proliferation of Demodex mites and by clinical cure after acaricidal treatment, together with normalization of Demodex mite density.
Treatment
Treatment with acaricides for demodicosis is aimed at reducing the excessive number of Demodex mites, and in order for patients to recover from the clinical symptoms. These treatments include topical metronidazole, permethrin, benzoyl benzoate, crotamiton, lindane, and sulfur.54,65 Tea tree oil are also found to be effective in Demodicosis, possible effects include lowering Demodex mite counts, relieving clinical symptoms, and modulating the immune system.66 Topical ivermectin 1%, showed excellent clinical improvement and none of the patients were still positive for demodex SSSB after 16 weeks of treatment.67 Topical metronidazole 2% have been recommended for demodicosis blepharitis and conjunctivitis. 68 Permethrin cream 5% was also effective in reducing the number of demodex mites and blepharitis symptoms.69 All of topical treatments should be used with caution, because of sensitive skin in demodicosis patients and many topical therapies were associated with mild to moderate irritation. 64,65 In severe cases or immunocompromised host such as those with HIV infection, treatment with oral medication should be considered. Oral metronidazole has shown efficacy in reducing Demodex mite density and improving clinical symptom of demodicosis.70 Ivermectin and fluralaner can inhibit overlapping molecule pathways regulating neuron activity, causing paralysis, lack of feeding and indirect killing effect on Demodex mite.71,72
Conclusions
Demodex mites can be found in healthy humans without causing any clinical symptoms. Under appropriate circumstances, when there is an increase in the number of Demodex mite density, it can cause demodicosis. Nevertheless, its role as the primary causative agent of the pathogenic conditions in humans is still being debated. Demodex mites, like other cutaneous microflora,73 may change to opportunistic pathogens. They have the potential to change status from commensals if the host immunity and cutaneous environment facilitates their proliferation.73-75 Clinical symptoms and severity of Demodicosis depends on these circumstances as well. In addition to the well-known symptoms of demodicosis such as, pityriasis folliculorum, rosacealike, folliculitis-like, perioral dermatosislike, there are also many other clinical symptoms that have been reported.39,49 Demodicosis can be presented with nonspecific facial symptoms such as unexplained itching, dry patchy skin, hypersensitive skin, non-specific papulopustular and nodular lesions. All of these symptoms were found to be strongly associated with abnormal proliferation of Demodex mites.34,40 Demodicosis is a challenging disease, which can be presented as a variety of symptoms mimicking many other dermatoses. It will be greatly beneficial to the patients if dermatologists became more aware of this disease. In addition, there are many unknowns about demodicosis that should be researched further.
Funding Statement
Funding: None.
References
- 1.Aylesworth R, Vance JC. Demodex folliculorum and Demodex brevis in cutaneous biopsies. J Am Acad Dermatol 1982;7:583-9. [DOI] [PubMed] [Google Scholar]
- 2.Acosta FJ, Planas L, Penneys N. Demodex mites contain immunoreactive lipase. Arch Dermatol. 1989;125:1436-7. [DOI] [PubMed] [Google Scholar]
- 3.Lacey N, Delaney S, Kavanagh K, Powell FC. Mite-related bacterial antigens stimulate inflammatory cells in rosacea. Br J Dermatol 2007;157:474-81. [DOI] [PubMed] [Google Scholar]
- 4.Spickett SG. Studies on Demodex folliculorum Simon. Parasitology 1961;51:181–92. [Google Scholar]
- 5.Sędzikowska A, Bartosik K, Przydatek-Tyrajska R, Dybicz M. Shared Makeup Cosmetics as a Route of Demodex folliculorum Infections. Acta Parasitol 2021;66:631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sengbusch HG, Hauswirth JM. Prevalence of hair follicle mites, Demodex folliculorum and Demodex brevis, in a selected human population in Western New York, USA. J Med Entomol 1986;23:384-8. [DOI] [PubMed] [Google Scholar]
- 7.Özer TT, Akyürek Ö, Durmaz S. Association between Demodex folliculorum and Metabolic syndrome. J Cosmet Dermatol 2020;19:3145-9. [DOI] [PubMed] [Google Scholar]
- 8.Karincaoglu Y, Seyhan ME, Bayram N, et al. Incidence of Demodex folliculorum in patients with end stage chronic renal failure. Ren Fail 2005;27:495-9. [DOI] [PubMed] [Google Scholar]
- 9.Ivy SP, Mackall CL, Gore L, et al. Demodicidosis in childhood acute lymphoblastic leukemia: an opportunistic infection occurring with immunosuppression. J Pediatr 1995;127:751-4. [DOI] [PubMed] [Google Scholar]
- 10.Fujiwara S, Okubo Y, Irisawa R, Tsuboi R. Rosaceiform dermatitis associated with topical tacrolimus treatment. J Am Acad Dermatol 2010;62:1050-2. [DOI] [PubMed] [Google Scholar]
- 11.Demirdağ HG, Özcan H, Gürsoy Ş, et al. The effects of sebum configuration on Demodex spp. Density. Turk J Med Sci 2016;46:1415-21. [DOI] [PubMed] [Google Scholar]
- 12.Thoemmes MS, Fergus DJ, Urban J, Tautwein M, Dunn RR. Ubiquity and diversity of human-associated Demodex mite. PLoS One 2014;9: e106265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Desch CE. Human hair follicle mites and forensic acarology. Exp Appl Acarol 2009;49:143-6. [DOI] [PubMed] [Google Scholar]
- 14.Esenkaya Taşbent F, Dik B. A dog related Demodex spp. infestation in a student: a rare Demodex case. Mikrobiyol Bul 2018;52:214-20. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira D, Sastre N, Ravera I, Altet L, et al. Identification of a third feline Demodex species through partial sequencing of the 16S rDNA and frequency of Demodex species in 74 cats using a PCR assay. Vet Dermatol 2015;26:239. [DOI] [PubMed] [Google Scholar]
- 16.Tani K, Une S, Hasegawa A, et al. Infestivity of Demodex canis to hamster skin engrafted onto SCID mice. J Vet Med Sci 2005;67:445-8. [DOI] [PubMed] [Google Scholar]
- 17.Akilov OE, KY. Association between human demodicosis and HLA class I. Clin Exp Dermatol. 2003;28:70-3. [DOI] [PubMed] [Google Scholar]
- 18.Akilov OE, Mumcuoglu KY. Immune response in demodicosis. J Eur Acad Dermatol Venereol 2004;18:440-4. [DOI] [PubMed] [Google Scholar]
- 19.Gazi U, Taylan-Ozkan A, Mumcuoglu KY. Immune mechanisms in human and canine demodicosis: A review. Parasite Immunol 2019;41:e12673. [DOI] [PubMed] [Google Scholar]
- 20.Kalincaoglu Y, Tepe B, Kalayci B, Seyhan M. Pseudozoster clinical presentation of Demodex infestation after prolonged topical steroid use. Clin Exp Dermatol 2008;33:740-2. [DOI] [PubMed] [Google Scholar]
- 21.Ní Raghallaigh S, Powell FC: The cutaneous microenvironment in papulopustular rosacea. Br J Dermatol 2009;161:25. [Google Scholar]
- 22.Ní Raghallaigh S, Bender K, Lacey N, et al. The fatty acid profile of the skin surface lipid layer in patients with papulopustular rosacea. Br J Dermatol 2012;166:279-87. [DOI] [PubMed] [Google Scholar]
- 23.Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol 1993;128:650-9. [DOI] [PubMed] [Google Scholar]
- 24.Jimenez-Acosta F, Planas L, Penneys N. Demodex mites contain immunoreactive lipase. Arch Dermatol 1989;125:1436-7. [DOI] [PubMed] [Google Scholar]
- 25.Moran EM, Foley R, Powell FC. Demodex and rosacea revisited. Clin Dermatol 2017;35:195-200. [DOI] [PubMed] [Google Scholar]
- 26.Jarmuda S, O’Reilly N, Żaba R, et al. Potential role of Demodex mites and bacteria in the induction of rosacea. J Med Microbiol 2012;61:1504-10. [DOI] [PubMed] [Google Scholar]
- 27.Fischer K, Walton S. Parasitic mites of medical and veterinary importance—is there a common research agenda? Int J Parasitol 2014;44:955-67. [DOI] [PubMed] [Google Scholar]
- 28.O’Reilly N, Menezes N, Kavanagh K. Positive correlation between serum immunoreactivity to Demodex-associated Bacillus proteins and erythematotelangiectatic rosacea. Br J Dermatol 2012;167:1032-6. [DOI] [PubMed] [Google Scholar]
- 29.Ionescu MA, Joly F, Bombard E, et al. TLR-2, cathelicidin-LL37 and kallikrein- 5 targeting in rosacea: In tubo, ex vivo and in vivo studies. J Am Acad Dermatol 2015;72:65. [Google Scholar]
- 30.Koller B, Muller Wiefel AS, Rupec R, et al. Chitin modulates innate immune responses of keratinocytes. PLoS One 2011;6:e16594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamasaki K, Kanada K, Macleod DT, et al. TLR2 expression is increased in rosacea and stimulates enhanced serine protease production by keratinocytes. J Invest Dermatol 2011;131:688-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Casas C, Paul C, Lahfa M, et al. Quantification of Demodex folliculorum by PCR in rosacea and its relationship to skin innate immune activation. Exp Dermatol 2012;21:906-10. [DOI] [PubMed] [Google Scholar]
- 33.Erbagci Z, Ozgoztasi O. The significance of Demodex folliculorum density in rosacea. Int J Dermatol 1998;37:421-5. [DOI] [PubMed] [Google Scholar]
- 34.Karincaoglu Y, Bayram N, Aycan O, Esrefoglu M. The clinical importance of demodex folliculorum presenting with nonspecific facial signs and symptoms. J Dermatol 2004;31:618-26. [DOI] [PubMed] [Google Scholar]
- 35.Aktaş Karabay E, Aksu Çerman A. Demodex folliculorum infestations in common facial dermatoses: acne vulgaris, rosacea, seborrheic dermatitis. An Bras Dermatol 2020;95:187-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Forton F, De Maertelaer V. Rosacea-like demodicosis and papulopustular rosacea may be two phenotypes of the same disease, and pityriasis folliculorum may be their precursor: response to the comment of Tatu. J Eur Acad Dermatol Venereol 2019;33:e47-8. [DOI] [PubMed] [Google Scholar]
- 37.Akçınar UG, Ünal E, Doğruman Al F. Demodex spp. as a possible aetiopathogenic factor of acne and relation with acne severity and type. Postepy Dermatol Alergol 2018;35:174-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yun CH, Yun JH, Baek JO, et al. Demodex Mite Density Determinations by Standardized Skin Surface Biopsy and Direct Microscopic Examination and Their Relations with Clinical Types and Distribution Patterns. Ann Dermatol 2017;29:137-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yasak Guner R, Tosun M, Akyol M, Hayta SB. Demodex infestation as a cause of sensitive skin in a dermatology outpatient clinic. J Cosmet Dermatol. 2021. May 22. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 40.Douglas A, Zaenglein AL. A case series of demodicosis in children. Pediatr Dermatol 2019;36:651-4. [DOI] [PubMed] [Google Scholar]
- 41.Forton FMN, De Maertelaer V. Rosacea and Demodicosis: Little-known Diagnostic Signs and Symptoms. Acta Derm Venereol 2019;99:47-52. [DOI] [PubMed] [Google Scholar]
- 42.Helou W, Avitan-Hersh E, Bergman R. Demodex Folliculitis of the Scalp:Clinicopathological Study of an Uncommon Entity. Am J Dermatopathol 2016;38:658-63. [DOI] [PubMed] [Google Scholar]
- 43.Bachmeyer C, Moreno-Sabater A. Demodex folliculitis. CMAJ 2017;189:E865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schaller M, Sander CA, Plewig G. Demodex abscesses: clinical and therapeutic challenges. J Am Acad Dermatol 2003;49:S272-274. [DOI] [PubMed] [Google Scholar]
- 45.Lee JY, Hsu CH. Granulomatous rosacea- like demodicidosis. Dermatol Online J 2007;13:9. [PubMed] [Google Scholar]
- 46.Sabater-Marco V, Escutia-Munoz B, Botella-Estrada R. Eosinophilic follicular reaction induced by Demodex folliculorum mite: a different disease from eosinophilic folliculitis. Clin Exp Dermatol 2015;40:413-5. [DOI] [PubMed] [Google Scholar]
- 47.Klemm E, Haroske G, Wollina U. Otitis externa and myringitis due to demodicidosis. Acta Dermatovenerol Alp Pannonica Adriat 2009;18:73-6. [PubMed] [Google Scholar]
- 48.Hedberg ML, Chibnall RJ, Compton LA. Symptomatic vulvar demodicosis: A case report and review of the literature. J Cutan Patho 2020;47:1063-6. [DOI] [PubMed] [Google Scholar]
- 49.Zhao YE, Peng Y, Wang XL, et al. Facial dermatosis associated with Demodex: a case-control study. J Zhejiang Univ Sci B 2011;12:1008-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sakuntabhai A, Timpatanapong P. Topical steroid induced chronic demodicidosis. J Med Assoc Thai 1991;74:116-9. [PubMed] [Google Scholar]
- 51.Sarac G, Cankaya C, Ozcan KN, et al. Increased frequency of Demodex blepharitis in rosacea and facial demodicosis patients. J Cosmet Dermatol 2020;19:1260-5. [DOI] [PubMed] [Google Scholar]
- 52.Zhang AC, Muntz A, Wang MTM, et al. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt 2020;40:389-432. [DOI] [PubMed] [Google Scholar]
- 53.Moris García V, Valenzuela Vargas G, Marín Cornuy M, Aguila Torres P. Ocular demodicosis: A review. Arch Soc Esp Oftalmol (Engl Ed) 2019;94:316-22. [DOI] [PubMed] [Google Scholar]
- 54.Zhao YE, Hu L, Wu LP, Ma JX. A metaanalysis of association between acne vulgaris and Demodex infestation. J Zhejiang Univ Sci B 2012;13:192-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen W, Plewig G. Human demodicosis: revisit and a proposed classification. Br J Dermatol 2014;170:1219-25. [DOI] [PubMed] [Google Scholar]
- 56.Forton FM, Germaux M-AE, Thibaut SC, et al. Demodicosis: descriptive classification and status of rosacea, in response to prior classification proposed. J Eur Acad Dermatol Venereol 2015;29:829-32. [DOI] [PubMed] [Google Scholar]
- 57.Forton FM, De Maertelaer V. Two Consecutive Standardized Skin Surface Biopsies: An Improved Sampling Method to Evaluate Demodex Density as a Diagnostic Tool for Rosacea and Demodicosis. Acta Derm Venereol 2017;97:242-8. [DOI] [PubMed] [Google Scholar]
- 58.Huang HP, Hsu CK, Lee JY. A new superficial needle-scraping method for assessing Demodex density in papulopustular rosacea. J Cosmet Dermatol 2020;19:896-900. [DOI] [PubMed] [Google Scholar]
- 59.Friedman P., Sabban EC., Cabo H. Usefulness of dermoscopy in the diagnosis and monitoring treatment of demodicidosis. Dermatol Pract Concept 2017;7:35-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sattler EC, Maier T, Hoffmann VS, et al. Noninvasive in vivo detection and quantification of Demodex mites by confocal laser scanning microscopy: reply from the authors. Br J Dermatol 2013;169:213-5. [DOI] [PubMed] [Google Scholar]
- 61.Rufli T, Mumcluoglu Y. The hair follicle mite demodex folliculorum and demodex brevis: biology and medical important. A review. Dermatologica 1981;162:1-11. [DOI] [PubMed] [Google Scholar]
- 62.Forton F, Song M. Limitations of standardized skin surface biopsy in measurement of the density of Demodex folliculorum. A case report. Br J Dermatol 1998;139:697-700. [DOI] [PubMed] [Google Scholar]
- 63.Aşkin U, Seçkin D. Comparison of the two techniques for measurement of the density of Demodex folliculorum: standardized skin surface biopsy and direct microscopic examination. Br J Dermatol 2010;162:1124-6. [DOI] [PubMed] [Google Scholar]
- 64.Jacob S, VanDaele MA, Brown JN. Treatment of Demodex-associated inflammatory skin conditions: A systematic review. Dermatol Ther 2019;32:e13103. [DOI] [PubMed] [Google Scholar]
- 65.Sarac G. A comparison of the efficacy and tolerability of topical agents used in facial Demodex treatment. J Cosmet Dermatol 2019;18:1784-7. [DOI] [PubMed] [Google Scholar]
- 66.Lam NSK, Long XX, Li X, et al. Comparison of the efficacy of tea tree (Melaleuca alternifolia) oil with other current pharmacological management in human demodicosis: A Systematic Review. Parasitology 2020;147:1587-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trave I, Merlo G, Cozzani E, Parodi A. Real-life experience on effectiveness and tolerability of topical ivermectin in papulopustular rosacea and antiparasitic effect on Demodex mites. Dermatol Ther 2019;32:e13093. [DOI] [PubMed] [Google Scholar]
- 68.Baima B, Sticherling M. Demodicidosis revisited. Acta Derm Venereol 2002;82:3-6. [DOI] [PubMed] [Google Scholar]
- 69.Hecht I, Melzer-Golik A, Sadi Szyper N, Kaiserman I. Permethrin Cream for the Treatment of Demodex Blepharitis. Cornea 2019;38:1513-8. [DOI] [PubMed] [Google Scholar]
- 70.Salem DA, El-Shazly A, Nabih N, et al. Evaluation of the efficacy of oral ivermectin in comparison with ivermectinmetronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis 2013;17:e343-7. [DOI] [PubMed] [Google Scholar]
- 71.da Rocha MC, Travassos AR, Uva L, et al. Demodicosis Treatment with Systemic Ivermectin. Skinmed 2017;15:293-5. [PubMed] [Google Scholar]
- 72.Nakata Y, Fuse T, Yamato K, et al. A Single Amino Acid Substitution in the Third Transmembrane Region Has Opposite Impacts on the Selectivity of the Parasiticides Fluralaner and Ivermectin for Ligand-Gated Chloride Channels. Mol Pharmacol 2017;92:546-55. [DOI] [PubMed] [Google Scholar]
- 73.Cogen AL, Nizet V, Gallo RL. Skin microbiota: a source of disease or defence? Br J Dermatol 2008;158:442-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dahl MV, Ross AJ, Schlievert PM. Temperature regulates bacterial protein production: possible role in rosacea. J Am Acad Dermatol 2004;50:266-72. [DOI] [PubMed] [Google Scholar]
- 75.Lacey N, Ní Raghallaigh S, Powell FC. Demodex mites—commensals, parasites or mutualistic organisms? Dermatology 2011;222:128-30. [DOI] [PubMed] [Google Scholar]


