Abstract
Background:
Running is a popular sport with widely recognized health benefits. Given the high rates of knee injury in runners and the growing prevalence of knee osteoarthritis (KOA), it may be useful to assess perceptions about running and knee joint health.
Purpose:
The objectives of this study were to (1) explore and compare the perceptions of the general public (PUB) and health care professionals (HCPs) on the topic of running and knee health and (2) explore recommendations about running and knee health provided by HCPs.
Study Design:
Cross-sectional study.
Methods:
We conducted an online survey between June 18 and October 1, 2020. The questionnaire included questions on running and knee health, and HCPs were asked about their typical recommendations and level of confidence in providing recommendations on the topic. Perceptions (proportions) were compared between the PUB and HCPs using the chi-square test.
Results:
In total, 4521 responses (PUB, n = 2514; HCPs, n = 2007) were analyzed. A greater proportion of HCPs perceived regular running as healthy for knees (86% vs 68%; P < .001). More of the PUB than HCPs (P < .001) believed that running frequently (29% vs 13%), long distances (54% vs 45%), and on hard surfaces (60% vs 36%) increased the risk of developing KOA. Running for those with KOA was perceived by the PUB as posing an increased risk of getting more knee pain (48%) and needing joint replacement surgery (38%), more so than by HCPs (26% and 17%, respectively). The majority of HCPs reported being relatively confident in providing evidence-based recommendations about running and knee health and mostly recommended that runners with KOA modify training parameters instead of quit.
Conclusion:
More HCPs perceived running as healthy for knees when compared with the PUB. Most HCPs felt confident in providing evidence-based recommendations about running and knee health.
Keywords: osteoarthritis, physical activity, questionnaire, joint
The World Health Organization recommends that all adults engage in regular physical activity, 7 a behavior that can reduce the risk of at least 35 chronic diseases. 5 Running represents an easy and accessible form of physical activity for adults worldwide and is known to provide many physical 17,23 and psychological 27,30 health benefits. Given that running is associated with high knee joint forces 28 and injury rates, 16 it is often perceived as detrimental to knee joint health. 14
A growing number of people see their quality of life and physical function negatively affected by knee osteoarthritis (KOA). 4,9 Several risk factors for the development of KOA have been identified, including participation in certain sports (eg, soccer and wrestling), 12 as well as genetics, older age, female sex, previous knee injury, and greater body mass. 29 However, the current state of research does not identify recreational running as a risk factor for the development of cartilage lesions or symptomatic KOA. 19 Indeed, despite the presence of confounding factors, the prevalence of knee and hip osteoarthritis in recreational runners is 3 times less than in sedentary nonrunners and 4 times less than in competitive runners. 2 A history of running has also been associated with a 54% lower risk of requiring surgery later in life owing to KOA. 31 In other studies, novice runners exhibited positive chondroprotective effects (ie, estimated greater glycosaminoglycan content) after completing a 10-week running intervention, 32 and established runners exhibited an acute decrease of inflammatory markers in the knee joint after a 30-minute running bout. 18 In people with KOA, maintaining a running program does not appear to lead to the progression of symptoms or structural features. 14 Even though knee cartilage in those with KOA may react differently to running, 13 current evidence suggests that physical activity is helpful 21 and that moderate-impact loading is not harmful to cartilage health or function. 6
Perceived benefits or harms potentially influence how people select physical activities in which they will participate. In a previous survey completed by the general public (PUB) and health care professionals (HCPs) in Canada, as much as 26%, 34%, and 44% of respondents were uncertain if running in general, running often, or running long distances was detrimental for knee health, respectively. 14 Nearly half of respondents from the PUB believed that running with KOA would lead to faster structural disease progression, as well as a premature need for knee arthroplasty. Recommendations issued to the public by HCPs can also influence the choice of activities and are more likely to be evidence based. Indeed, half of surveyed HCPs reported that their recommendations have changed over time, with a growing number advising continuation of running among runners with KOA. 14
Presently, it remains unknown if the aforementioned survey data from Canada are representative of global views about running and KOA. Perceptions need to be explored and documented to evaluate the pertinence of global knowledge translation strategies to increase awareness on current evidence about running and knee health. Therefore, the first objective of this study was to explore and compare, using an online survey in 7 languages, the perceptions of runners and nonrunners from the PUB and HCPs on the topic of running and knee joint health. The second objective was to explore HCPs’ typical recommendations about running and knee joint health.
Methods
Participants
The protocol for this study was approved by our institution. This study was guided by the Checklist for Reporting Results of Internet E-surveys. 15 We conducted an online survey between June 18 and October 1, 2020, using a convenience sample. To be included, participants had to self-report being ≥18 years old; have access to the internet; and understand English, Spanish, French, Portuguese, Italian, Danish, or Dutch. Participants were recruited by posting about the survey through social media (paid advertisements, accounts of the coauthors and their collaborators, groups of HCPs and runners) (Supplemental Figure S1, available online), sports and arthritis interest groups, and email lists from previous studies on running and KOA. No incentives were offered for participation.
Study Design
This was a single-round online open survey. After selecting their preferred language, participants were informed about the study objectives, the length of the survey, and the members of the research team. They provided informed consent electronically and then self-identified as a member of the PUB or an HCP; after which, they were directed to the corresponding set of questions on demographics and perceptions about the association between running and knee joint health. No personal information was collected. Individuals were permitted to close the browser without starting the survey or at any time during the survey, even after providing consent. The design and administration of the survey consisted of the following 4 steps, per previous work. 11
Step 1: Designing the First Version of the English-Language Survey. We designed a first set of questions about demographics based on previous survey studies. 11,14 We also built a series of statements evaluating perceptions on running and knee joint health. To minimize response bias, statements were constructed as “fill in the blank” sentences with choices corresponding to beliefs. Questions targeted 3 main themes: (1) whether or not running habits are a risk factor in the development of KOA in people with healthy knees, (2) whether or not running habits are detrimental in people with KOA, and (3) whether or not respondents had received previous information regarding running and knee joint health. Thereafter, additional questions specific to those of the PUB who declared that they were runners were developed to explore what they would do in the event of future knee pain or a diagnosis of KOA. Finally, questions specific for HCPs were added to explore their professional experience as it related to running and knee joint health and about typical recommendations that they provided to patients.
Step 2: Feedback on Survey Questions and Reaching the Final Version. The first version of the survey was sent out for review to individuals external to the research team. A total of 6 (2 runners, 2 nonrunners with KOA, 2 HCPs) provided feedback on the questions and choices of responses (relevance, clarity, interpretation, wording). Following feedback, we modified the wording of 3 survey questions and added multiple-choice options to 2 questions to reach the final version of the survey. In addition to questions on demographics, there were 11 core questions that were relevant to all participants that permitted us to explore and compare perceptions on the topic of running and knee joint health. The subgroup of HCPs had 6 additional questions specific to recommendations that they provided to their patients about running and knee joint health plus another one on whether or not they had received training in this topic. The exact wording of these questions in English is summarized in Appendix Table A1. The final version of the survey included 37 questions (6 pages) for the PUB respondents who were runners, 30 questions for PUB respondents who were not runners (5 pages), and 36 questions for HCPs (8 pages).
Step 3: Translating the Survey and Getting Feedback on the Translated Versions. Members of the research team translated the final version of the English survey into Spanish (M.B.), French (J.-F.E.), Portuguese (D.O.S.), Italian (S.P.), Danish (M.S.R.), and Dutch (M.V.M.). Each translated version was reviewed independently by another bilingual researcher in each language to verify its accuracy against the original English version. Thereafter, each translated survey was sent out for additional language review to 1 runner, 1 person with KOA, and 1 HCP who had that language as their first language. Minor modifications to wording were made before reaching the final version in all languages.
Step 4: Administering the Survey. The online survey in all 7 languages was input into the XM Qualtrics (SAP America) survey system. After selecting their language and reading an overview of the study objectives and inclusion criteria, participants provided consent electronically and self-identified as PUB or HCP. They were then directed to the corresponding set of survey questions. The order of questions was not randomized, and adaptive questioning was used when required. All questions were mandatory and automatically checked by the online system. Participants were allowed to go back to review and change their responses.
Data Analysis
Data for all 7 languages were exported from Qualtrics and merged into a single Microsoft Excel spreadsheet, before being transferred to the Statistical Package for Social Sciences Version 27 (IBM) for statistical analysis. Given the possibility that multiple HCPs from the same workplace would participate, we did not exclude responses based on an IP address check. The primary comparisons were between the PUB and HCP groups. To be included in analyses, survey responses had to have all 11 core questions completed. Descriptive statistics (frequencies and proportions) were generated for each question. For the purpose of statistical analyses (but not figures), some responses were combined to provide a better overview of global perceptions (eg, “very appropriate” combined with “somewhat appropriate”; “somewhat decreased” combined with “greatly decreased”). This resulted in 4 response categories: “favorable,” “neutral,” “unfavorable,” and “don’t know.” Response proportions across these 4 categories were compared between the PUB and HCPs using the chi-square test for all 11 core questions on perceptions (2 × 4 contingency tables). Effect sizes were calculated using Cramer V and were categorized by 3 levels of freedom as negligible (<0.06), small (≥0.06), moderate (≥0.17), or large (≥0.29). 8,20 Since perceptions could be affected by personal running habits, 14 we also compared responses of runners and nonrunners, irrespective of PUB or HCP group membership. An alpha level of .05 was used for the chi-square test. The level of post hoc significance was Bonferroni adjusted (P < .0125) to account for the 4 response categories per analysis between the PUB and HCPs. 3
Results
Sample
A total of 8843 individuals showed interest in the survey and accessed the Qualtrics website. Of these, 4521 responses (51%) were complete and considered in analyses (1747 in English, 672 in Spanish, 593 in French, 568 in Portuguese, 495 in Italian, 345 in Danish, and 101 in Dutch). Demographics for the PUB (n = 2514) and HCPs (n = 2007) are provided in Appendix Table A2, and demographics by language are provided in Supplemental Table S1 (available online).
Perceptions About Running Habits and KOA in People With Healthy Knees
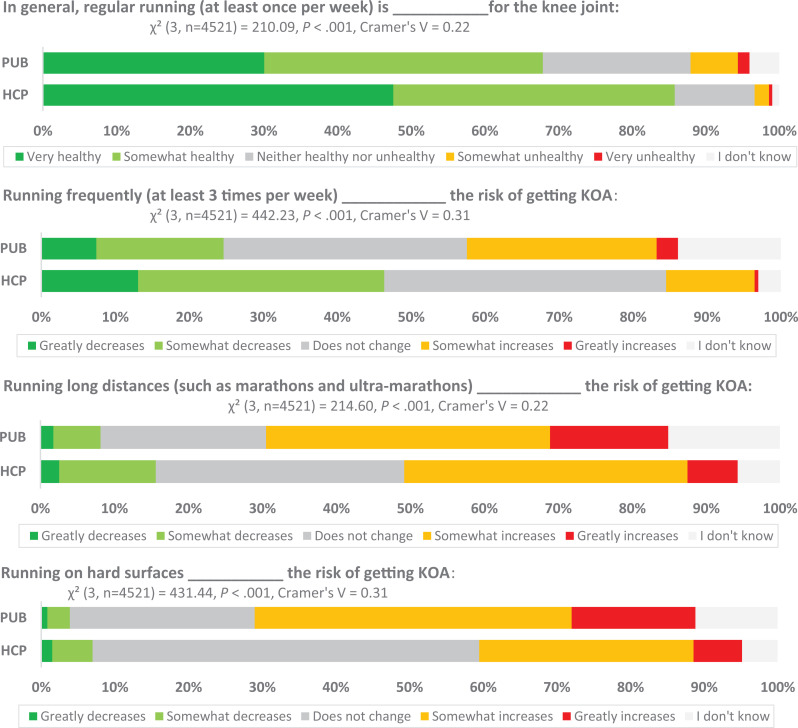
Among the 11 core questions, perceptions about the effects of regular running, frequent running, running long distances, and running on hard surfaces on knee health were all different between the PUB and HCP groups (P < .001) (Figure 1), with moderate to large effect sizes (Cramer V = 0.22-0.31). Specifically, a greater proportion of HCPs (86%) perceived regular running as healthy for knees as compared with the PUB (68%). Runners and nonrunners had similar perceptions on those topics (χ2 [df = 3; n = 4521] = 0.95; P = .813; Cramer V = 0.02). Significantly more PUB respondents than HCPs (P < .001) believed that running frequently (29% vs 13%), running for long distances (54% vs 45%), or running on hard surfaces (60% vs 36%) increased the risk of developing KOA. Perceptions were also different about the effects of shoe cushioning (χ2 [df = 3; n = 4521] = 327.69; P < .001; Cramer V = 0.27), with more PUB respondents (50%) believing that greater cushioning and support decreased the risk of KOA as compared with HCPs (39%). The running status of respondents had a significant but small influence on perceptions about the influence of running frequency, distances, surface, and shoe cushioning on the risk of developing KOA (χ2 [df = 3; n = 4521] = 9.07-32.30; P ≤ .028; Cramer V = 0.05-0.09). For example, 6% of nonrunners reported being uncertain about the influence of shoe cushioning on the risk of KOA as compared with 9% of runners (P = .0009). All proportions and comparisons between the PUB and HCP groups, as well as between runners and nonrunners, are provided in Supplemental Table S2 (available online).
Figure 1.
Perceptions about the effects of running and knee health in healthy individuals. KOA, knee osteoarthritis. HCP, health care professionals; PUB, general public. The first value in parentheses indicates the degrees of freedom for the chi-square test.
Perceptions About Running Habits and Knee Joint Health in People With KOA
Perceptions about running in individuals with KOA were different between the PUB and HCPs (all P < .001) (Figure 2). Significantly more HCPs (P < .001) perceived that it was appropriate or very appropriate for nonrunners with KOA to start running (74%) or for runners with KOA to keep running (86%) if they had no symptoms before or after they went running, in comparison with the PUB (49% and 59%, respectively). When compared with HCPs, significantly more of the PUB (P < .001) perceived that people with KOA who maintained running could increase their risk of getting more knee pain (48% vs 26%) or needing joint replacement surgery (38% vs 17%). Detailed frequencies and proportions are provided in Supplemental Table S2 (available online). Despite response proportions on this topic being slightly different between individuals who reported being runners and nonrunners (Cramer V = 0.05-0.12; negligible to small effect sizes), differences in perceptions were much greater when comparing PUB and HCP respondents (Cramer V = 0.24-0.38; moderate to large effect sizes).
Figure 2.
Perceptions about running and knee health in people with knee osteoarthritis (KOA). HCP, health care professionals; PUB, general public. The first value in parentheses indicates the degrees of freedom for the chi-square test.
Current runners from the PUB who had not been diagnosed with KOA (n = 1759) mostly reported that in the event that they would go on to develop knee pain without a diagnosis of KOA, they would reduce distance (43%), decrease frequency (40%), stop temporarily (34%), or lower speed (25%). Only 1% would stop running completely, while 10% would not change anything. If they were diagnosed with KOA, they would also reduce distance (39%), decrease frequency (35%), stop temporarily (20%), or lower speed (19%). Stopping running completely after a diagnosis of KOA would be considered by just 3%, while 20% would not change anything in their training.
Recommendations About Running and Knee Joint Health
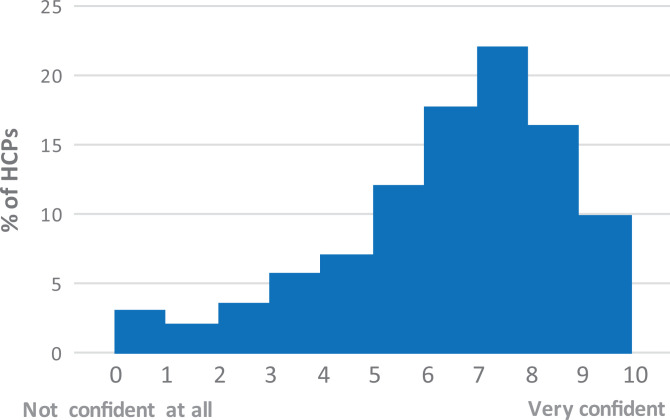
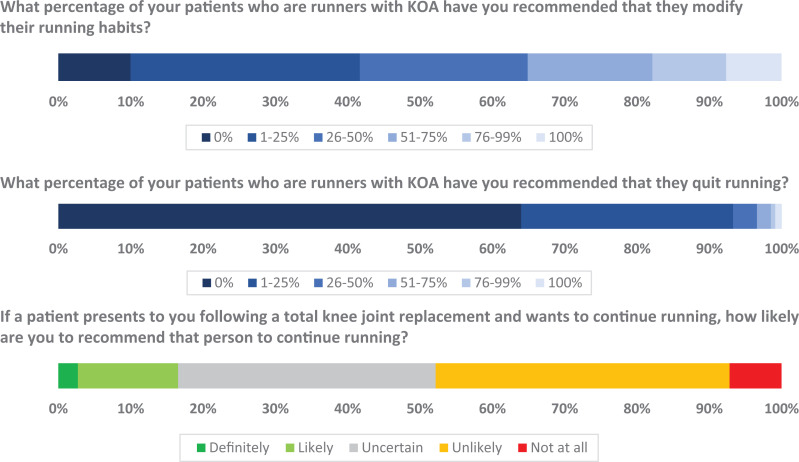
Among the PUB, 25% reported having received information about running and knee joint health, as opposed to 74% of HCPs. On a scale from 0 (not confident at all) to 10 (very confident), the median level of confidence of HCPs in providing evidence-based recommendations on the topic was 6.8 (interquartile range = 3.0) (Figure 3). The majority of HCPs (73%) indicated having discussed running and knee joint health with their patients, mostly recommending modifications to their running habits instead of quitting running (Figure 4). Over three-quarters (78%) stated that their recommendations had changed over the years, with the majority (96%) now recommending that more runners with KOA maintain running. Finally, only 17% of HCPs said that they would likely or definitely recommend that runners maintain running after getting total knee joint replacement surgery, while 48% would be unlikely or would not recommend it at all (Figure 4). Over one-third of HCPs (36%) were uncertain about what they would recommend.
Figure 3.
Level of confidence of health care professionals (HCPs) in providing evidence-based recommendations on running and knee health.
Figure 4.
Typical recommendations from health care professionals. KOA, knee osteoarthritis.
Discussion
We compared the perceptions of the PUB (runners and nonrunners) and HCPs on the topic of running and knee joint health and explored HCPs’ typical practice recommendations across multiple countries and in 7 languages. Overall, running was perceived in our sample as healthy for the knee joint with some exceptions: running often, over long distances, or on hard surfaces. A significant number of respondents perceived that running with KOA could lead to more pain and an increased need for joint replacement surgery. HCPs had more positive perceptions than the PUB with regard to running for people with healthy knees and those with KOA. HCPs mostly recommended that runners with KOA modify their training parameters instead of quit, and they were generally confident with providing evidence-based recommendations. In contrast, most HCPs were not in favor of or were uncertain about running after total knee joint replacement surgery.
To our knowledge, this is the first study to document perceptions about running and knee health in a large international sample of individuals. A previous study conducted in Canadians noted much higher rates of uncertainty than the current sample, especially in the general public. 14 Just one-quarter of our international sample reported having received information about running and knee joint health, as opposed to two-thirds of the sample in the Canadian study. It must be noted that the current sample included individuals from the PUB aged ≥18 years (mean, 41 years), while the Canadian study surveyed those aged at least 40 years (mean age for runners, 51 years; nonrunners, 61 years). While cultural differences, age, and recruitment methods might explain the differences between studies, a greater proportion of our international sample indicated having a university education. It is also possible that more information, whether favorable or not to running for knee joint health, has been freely accessible in the interval between studies. Nonetheless, lower rates of uncertainty do not mean that perceptions are in line with the current literature. Over half of the PUB perceived long distances and hard surfaces as factors that increase the risk of developing KOA, although the current evidence links only “elite”-level running with greater rates of KOA. 2 Similarly, almost half of the PUB respondents perceived running with KOA as potentially hazardous to knee health because they believed that it would increase the risk of worsening pain and the need for joint replacement surgery. In contrast and despite many limitations, the current state of literature suggests that recreational running has a protective effect on surgery 31 and may not affect the progression of KOA. 22
In comparison, 74% of HCPs reported having received information on running and knee joint health, and most were fairly confident in providing evidence-based recommendations to their patients. This might explain why their perceptions were more in line with the latest scientific literature outlined here. While we aimed for several sources of recruitment, a large proportion of participants were recruited from social media, which could have biased our sample to those HCPs who show interest in the latest research and are trying to stay up-to-date. However, a large proportion of HCPs were unlikely to recommend running after a total joint replacement or were simply uncertain. This is not surprising given the scarce evidence on the topic. To date, only observational studies and case series providing very little guidance have been published, mostly after hip joint replacement. 1,24 –26 Although these studies suggest that running might be relatively safe and competing in ultraendurance events might even possible be after a joint replacement, just a single recent study has specifically reported on the knee joint. 26 This low level of evidence is likely related to the uncertainty expressed by HCPs in our survey.
Taken together, our findings highlight 2 main points. The first is the need to translate and transfer the latest scientific knowledge to the PUB and HCPs to help make evidence-informed decisions about physical activity. One way of reaching large numbers of the PUB and HCPs would be by means of digital resources, such as an online educational module, and integration into health professional teaching curricula. 11 Second, there is a need for high-quality and better-controlled studies regarding running and knee joint health. Although the body of literature is growing, there is a lack of prospective studies that clearly document running parameters with the intent of studying knee health and a surgical endpoint. Despite emerging evidence, research is needed to provide practical recommendations to runners and HCPs on optimal training parameters, for runners with healthy knees and those with KOA. To support these efforts to be successful, it will be imperative to utilize evidence and best practice from the fields of knowledge dissemination and implementation as well as from the discipline of behavior change. Studies using qualitative designs would also be relevant to better understand perceptions in these different populations.
The 7 languages used to collect data for this study, as well as the sample size, represent its biggest strengths because we can generalize the results to a broader population. However, since it was an online survey and our languages did not apply to the entire world, we cannot assume that our findings are fully representative of the global population. The process that we used to develop the survey represents another strength. Questions were designed with the help of the PUB and HCPs and reviewed for accuracy and wording in all languages after being translated.
Limitations
Even if the overall sample size was appropriate to perform well-powered comparisons between HCPs and the PUB, the varying numbers among languages does not guarantee that our results are representative of the population speaking each of these languages. Given the nature of an online survey, there are obvious limitations to using this method, such as recall bias or the inability to confirm that respondents were indeed HCPs or members of the PUB who had received a diagnosis of KOA. Recruiting respondents online bears the risk of involuntarily targeting individuals who might have been in contact with information circulating on social media, for example, leading to a selection bias. There is no guarantee, however, that information circulating online would be in accordance with the current state of literature. 10 Thus, sources of recruitment must be kept in mind when interpreting results, although they do not compromise the validity of results. Finally, it could be argued that perceptions and beliefs about health might be better studied with qualitative or mixed-method designs. We feel that our data provide a necessary step to inform future research, which could include qualitative research as well as educational interventions.
Conclusion
Findings from our international survey suggest that the PUB and HCPs generally perceive running as being healthy for knee joint health—except for perceptions about running frequently, for long distances, or on hard surfaces. For people with KOA, members of the PUB often perceived running as an activity that could increase the risk of worsening pain and joint replacement surgery. Overall, HCPs had more positive perceptions about running in people with healthy knees and those with KOA. They were mostly confident in providing evidence-based recommendations about running and knee joint health and mostly reported recommending that runners with KOA modify their training parameters instead of quit. Running after a joint replacement is a topic that most HCPs were not in favor of or were uncertain about. Results from this study can inform knowledge translation initiatives to educate the PUB and HCPs about the current literature on running and knee joint health.
Supplemental Material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671221124141
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221124141 for Do the General Public and Health Care Professionals Think That Running Is Bad for the Knees? A Cross-sectional International Multilanguage Online Survey by Jean-Francois Esculier, Manuela Besomi, Danilo de Oliveira Silva, Samuele Passigli, Michael Skovdal Rathleff, Marienke Van Middelkoop, Christian Barton, Michael J. Callaghan, Matthew S. Harkey, Alison M. Hoens, Natasha M. Krowchuk, Anthony Teoli, Bill Vicenzino, Richard W. Willy and Michael A. Hunt in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors thank all members of the public and health care professionals who gave their feedback and helped to translate the survey and educational module, as well as all those who participated in this study.
APPENDIX
Appendix Table A1.
Survey Questions About Perceptions (PUB and HCPs) and Recommendations (HCPs) on Running and Knee Joint Health a
| Core questions on running and knee health for PUB and HCP |
| In general, regular running (at least once per week) is ___________ for the knee joint. |
| Running frequently (at least 3 times per week) ____________ the risk of getting KOA. |
| Running long distances (such as marathons and ultra-marathons) ____________ the risk of getting KOA. |
| Running on hard surfaces ___________ the risk of getting KOA. |
| Running with shoes that have more cushioning and support ___________ the risk of getting KOA. |
| It is _________ for a nonrunner with KOA to start a running program if they don’t have symptoms before or after they go running. |
| People with KOA who continue to run will __________ their risk of getting more knee pain. |
| People with KOA who keep running regularly will ____________ the need for joint replacement surgery. |
| It is _________ for runners who have KOA to continue if they don’t have symptoms before or after they go running. |
| People with KOA who continue to run should choose shoes with ____________. |
| People with KOA who continue to run should _____________. |
| Additional question for PUB |
| Have you ever received information on running and knee health? |
| Additional questions for PUB who identified as runners |
| If I were to develop knee pain (but without a diagnosis of KOA), I would __________ |
| If I was diagnosed with KOA by a doctor, I would __________ |
| Additional questions for HCP |
| Have you ever received training on running and knee health? |
| Have you ever discussed running and KOA with your patients? |
| What percentage of your patients who are runners with KOA have you recommended that they modify their running habits? |
| What percentage of your patients who are runners with KOA have you recommended that they quit running? |
| Have your recommendations about running and KOA changed over the course of your career? |
| If a patient presents to you following a total knee joint replacement and wants to continue running, how likely are you to recommend that person to continue running? |
| How confident do you feel about providing evidence-based recommendations on running and knee health? |
a HCP, health care professional; KOA, knee osteoarthritis; PUB, general public.
Appendix Table A2.
Demographics of Respondents a
| PUB (n = 2514) | HCPs (n = 2007) | |
|---|---|---|
| Age, y, mean ± SD | 41.2 ± 2.8 | 36.5 ± 10.3 |
| Gender | ||
| Woman | 1267 (50.4) | 960 (47.8) |
| Man | 1233 (49.0) | 1044 (52.0) |
| Gender-fluid | 4 (0.2) | 0 (0) |
| Nonbinary | 5 (0.2) | 0 (0) |
| Two-spirit | 1 (0) | 2 (0.1) |
| Prefer not to answer | 4 (0.2) | 1 (0) |
| Level of education | ||
| Below high school | 46 (1.8) | 0 (0) |
| High school | 263 (10.5) | 18 (0.9) |
| Nonuniversity | 337 (13.4) | 56 (2.8) |
| University | 1868 (74.3) | 1933 (96.3) |
| General health status | ||
| Excellent | 723 (28.8) | 725 (38.0) |
| Very good | 1172 (46.6) | 956 (47.6) |
| Good | 542 (21.6) | 292 (14.5) |
| Fair | 71 (2.8) | 31 (1.5) |
| Poor | 6 (0.2) | 3 (0.1) |
| Currently a runner | 2031 (80.8) | 1037 (51.7) |
| Diagnosed with KOA | 356 (14.2) | 194 (9.7) |
| History of knee injury | ||
| No | 997 (39.7) | 762 (38.0) |
| Yes, without surgery | 1146 (45.6) | 949 (47.3) |
| Yes, with surgery | 371 (14.8) | 296 (14.7) |
| Experience, y, mean ± SD | 11.5 ± 9.9 | |
| Profession b | ||
| Physiotherapist | — | 1583 (78.9) |
| Athletic therapist | — | 125 (6.2) |
| Medical doctor | — | 114 (5.7) |
| Chiropractor | — | 86 (4.3) |
| Nurse | — | 40 (2.0) |
| Osteopath | — | 35 (1.7) |
| Podiatrist, pedorthist | — | 17 (0.8) |
| Other | — | 112 (5.6) |
| Primary area of practice | ||
| Orthopedics | — | 666 (33.2) |
| Physical medicine and rehabilitation | — | 345 (17.2) |
| Sports medicine | — | 297 (14.8) |
| General practice | — | 264 (13.2) |
| Rheumatology | — | 33 (1.6) |
| Other | — | 383 (19.1) |
a Data are reported as No. (%) unless otherwise indicated. Dashes indicate areas not applicable. HCP, health care professional; KOA, knee osteoarthritis; PUB, general public.
b Total adds to >100% because some respondents reported multiple health professions.
Footnotes
Final revision submitted June 24, 2022; accepted July 12, 2022.
All authors are listed in the Authors section at the end of this article.
One or more of the authors has declared the following potential conflict of interest or source of funding: Salary support was provided by the Canadian Institutes for Health Research to J.-F.E. and the Michael Smith Foundation for Health Research to M.A.H. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of British Columbia (H19-03859).
Authors: Jean-Francois Esculier, PT, PhD (Department of Physical Therapy, University of British Columbia, Vancouver, Canada; Motion Analysis and Biofeedback Laboratory, University of British Columbia, Vancouver, Canada; The Running Clinic, Lac Beauport, Canada); Manuela Besomi, PT, PhD (School of Health and Rehabilitation Sciences, The University of Queensland, Brisbane, Australia; School of Physical Therapy, Universidad del Desarrollo, Santiago, Chile); Danilo de Oliveira Silva (La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, La Trobe University, Melbourne, Australia); Samuele Passigli, BSc, PT (University of Rome “Tor Vergata,” Rome, Italy); Michael Skovdal Rathleff, PT, PhD (Research Unit for General Practice in Aalborg, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark; Department of Occupational Therapy and Physiotherapy, Aalborg University Hospital, Aalborg, Denmark); Marienke Van Middelkoop, PhD (Department of General Practice, Erasmus MC Medical University, Rotterdam, the Netherlands); Christian Barton, PT, PhD (La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, La Trobe University, Melbourne, Australia); Michael J. Callaghan, PT, PhD (Department of Health Professions, Manchester Metropolitan University, Manchester, UK; Manchester University Foundation NHS Trust, Manchester, UK); Matthew S. Harkey, PhD, ATC (Department of Kinesiology, Michigan State University, East Lansing, Michigan, USA); Alison M. Hoens, BSc, PT (Department of Physical Therapy, University of British Columbia, Vancouver, Canada; Arthritis Research Canada, Vancouver, Canada; Centre for Health Evaluation and Outcome Sciences, University of British Columbia, Vancouver, Canada); Natasha M. Krowchuk, BSc (Motion Analysis and Biofeedback Laboratory, University of British Columbia, Vancouver, Canada); Anthony Teoli, MScPT (School of Physical and Occupational Therapy, McGill University, Montreal, Canada; Lethbridge Layton Mackay Rehabilitation Center, Montreal, Canada; InfoPhysiotherapy, Montreal, Canada); Bill Vicenzino, PT, PhD (School of Health and Rehabilitation Sciences, The University of Queensland, Brisbane, Australia); Richard W. Willy, PT, PhD (School of Physical Therapy, University of Montana, Missoula, Montana, USA); and Michael A. Hunt, PT, PhD (Department of Physical Therapy, University of British Columbia, Vancouver, Canada; Motion Analysis and Biofeedback Laboratory, University of British Columbia, Vancouver, Canada).
References
- 1. Abe H, Sakai T, Nishii T, et al. Jogging after total hip arthroplasty. Am J Sports Med. 2014;42:131–137. [DOI] [PubMed] [Google Scholar]
- 2. Alentorn-Geli E, Samuelsson K, Musahl V, et al. The association of recreational and competitive running with hip and knee osteoarthritis: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47:373–390. [DOI] [PubMed] [Google Scholar]
- 3. Beasley MT, Schumacker RE. Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. J Exp Educ. 1995;64:79–93. [Google Scholar]
- 4. Bombardier C, Hawker G, Mosher D. The Impact of Arthritis in Canada: Today and Over the Next 30 Years. Arthritis Alliance of Canada; 2011. [Google Scholar]
- 5. Booth FW, Robert CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2:1143–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bricca A, Juhl CB, Steultjens M, et al. Impact of exercise on articular cartilage in people at risk of, or with established, knee osteoarthritis: a systematic review of randomised controlled trials. Br J Sports Med. 2019;53:940–947. [DOI] [PubMed] [Google Scholar]
- 7. Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Routledge Academic; 1988. [Google Scholar]
- 9. Cui A, Li H, Wang D, et al. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Oliveira Silva D, Rathleff MS, Holden S, et al. Patients and clinicians managing patellofemoral pain should not rely on general web-based information. Phys Ther Sport. 2020;45:176–180. [DOI] [PubMed] [Google Scholar]
- 11. Dhillon G, Hunt MA, Reid A, et al. What are the perceptions on footwear and running injury, and are these perceptions modifiable? BMJ Open SEM. 2020;6:e000767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Driban JB, Hootman JM, Sitler MR, et al. Is participation in certain sports associated with knee osteoarthritis? A systematic review. J Athl Train. 2017;52:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Esculier JF, Jarrett M, Krowchuk NM, et al. Cartilage recovery in runners with and without knee osteoarthritis: a pilot study. Knee. 2019;26:1049–1057. [DOI] [PubMed] [Google Scholar]
- 14. Esculier JF, Krowchuk NM, Li LC, et al. What are the perceptions about running and knee joint health among the public and healthcare practitioners in Canada? PLoS One. 2018;13:e0204872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-surveys (CHERRIES). J Med Internet Res. 2004;6:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fredette A, Roy JS, Perreault K, et al. The association between running injuries and training parameters: a systematic review. J Athl Train. Published online September 3, 2021. doi:10.4085/1062-6050-0195.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hespanhol Junior LC, Pillay JD, van Mechelen W, et al. Meta-analyses of the effects of habitual running on indices of health in physically inactive adults. Sports Med. 2015;45:1455–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hyldahl RD, Evans A, Kwon S, et al. Running decreases knee intra-articular cytokine and cartilage oligomeric matrix concentrations: a pilot study. Eur J Appl Physiol. 2016;116:2305–2314. [DOI] [PubMed] [Google Scholar]
- 19. Khan MCM, O’Donovan J, Charlton JM, et al. The influence of running on lower limb cartilage: a systematic review and meta-analysis. Sports Med. 2022;52(1):55–74. doi:10.1007/s40279-021-01533-7 [DOI] [PubMed] [Google Scholar]
- 20. Kim HY. Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017;42:152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kraus VB, Sprow K, Powell KE, et al. Effects of physical activity in knee and hip osteoarthritis: a systematic umbrella review. Med Sci Sports Exerc. 2019;51:1324–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lo GH, Musa SM, Driban JB, et al. Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37:2497–2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pedisic Z, Shrestha N, Kovalchik S, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med. 2020;54:898–905. [DOI] [PubMed] [Google Scholar]
- 24. Pozzi F, Madara K, Zeni JAJ. A six-week supervised exercise and educational intervention after total hip arthroplasty: a case series. Int J Sports Phys Ther. 2017;12:259–272. [PMC free article] [PubMed] [Google Scholar]
- 25. Raguet M, Pierson C, Pierson A. La course à pied hors norme est-elle possible avec une prothèse totale de hanche? J Traumatol du Sport. 2015;32:3–14. [Google Scholar]
- 26. Rochoy M, Six J, Favre J, et al. Does hip or knee joint replacement decrease chances to complete an ultra-trail race? Study in participants at the Ultra-Trail du Mont Blanc. Orthop Traumatol Surg Res. 2020;106:1539–1544. [DOI] [PubMed] [Google Scholar]
- 27. Roeh A, Lembeck M, Papazova I, et al. Marathon running improves mood and negative affect. J Psychiatr Res. 2020;130:254–259. [DOI] [PubMed] [Google Scholar]
- 28. Saxby DJ, Modenese L, Bryant AL, et al. Tibiofemoral contact forces during walking, running and sidestepping. Gait Posture. 2016;49:78–85. [DOI] [PubMed] [Google Scholar]
- 29. Silverwood V, Blagojevic-Bucknall M, Jinks C, et al. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta analysis. Osteoarthritis Cartilage. 2015;23:507–515. [DOI] [PubMed] [Google Scholar]
- 30. Szabo A, Abraham J. The psychological benefits of recreational running: a field study. Psychol Health Med. 2013;18:251–261. [DOI] [PubMed] [Google Scholar]
- 31. Timmins KA, Leech RD, Batt ME, et al. Running and knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2017;45:1447–1457. [DOI] [PubMed] [Google Scholar]
- 32. Van Ginckel A, Baelde N, Almqvist KF, et al. Functional adaptation of knee cartilage in asymptomatic female novice runners. Osteoarthritis Cartilage. 2010;18:1564–1569. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221124141 for Do the General Public and Health Care Professionals Think That Running Is Bad for the Knees? A Cross-sectional International Multilanguage Online Survey by Jean-Francois Esculier, Manuela Besomi, Danilo de Oliveira Silva, Samuele Passigli, Michael Skovdal Rathleff, Marienke Van Middelkoop, Christian Barton, Michael J. Callaghan, Matthew S. Harkey, Alison M. Hoens, Natasha M. Krowchuk, Anthony Teoli, Bill Vicenzino, Richard W. Willy and Michael A. Hunt in Orthopaedic Journal of Sports Medicine