Abstract
Macrophages are influential members of the innate immune system that can be reversibly polarized by different microenvironment signals. Cell polarization leads to a wide range of features, involving the migration, development, and organization of the cells. There is mounting evidence that macrophage polarization plays a key role in the initiation and development of a wide range of diseases. This study aims to give an overview of macrophage polarization, their different subtypes, and the importance of alternatively activated M2 macrophage and classically activated M1 macrophage in immune responses and pathological conditions. This review provides insight on the role of exosomes in M1/M2-like macrophage polarization and their potential as a promising therapeutic candidate.
Keywords: Exosomes, Inflammation, Macrophages, Macrophage polarization
Introduction
Macrophages and their phagocytosis activity were first discovered by Elie Metchnikoff and Paul Ehrlich in 1908 [1–3]. The mononuclear phagocyte system (MPS) is a professional phagocyte that comprises dendritic cells (DCs), blood monocytes, and tissue macrophages [4]. Macrophages are mononuclear cells that are the most plenteous and widespread immune cells and are involved in phagocytosis, homeostasis, and remodeling after injury and are necessary during organ development [5–7]. Macrophages can originate from local tissue-resident macrophages with a self-renewed ability or blood monocytes. Bone marrow progenitor-derived monocytes migrate to tissue by receiving stimuli signals and then become macrophages [4, 8]. Macrophages have plastic characteristics. These characteristics enable them to switch their phenotypes and functions in connection with various microenvironmental signals [9].
Macrophages have been observed in many tissues. They are categorized on the basis of their location and function, for instance, microglial cells in the central nervous system (CNS) with the ability to clear defective neurons; alveolar macrophages in the lung, which are needed for lung homeostasis; osteoclasts in bone with bone remodeling activity [10–12]; and Kupffer cells, which are the most lavish macrophages present in liver [13–15]. Macrophages are innate immune cells that can affect a variety of processes, including tissue repair, angiogenesis, and immunomodulation [16, 17]. Macrophages gain different phenotypes and functions under normal condition or during disease. Macrophages’ ability to change their functions in response to different signals is known as polarization, which is a multifactorial process [18]. This is a key mediator of different diseases, including autoimmune diseases [19], glycolipid metabolic disorders [20], neurology disorders [21], cardiovascular diseases [3], and cancers [22]. Different polarized macrophages, M1 (classically activated macrophages) and M2 (alternatively activated macrophages), express diverse cell surface markers and factors (Table 1) [23].
Table 1.
Macrophage subtypes and their characteristic markers and stimuli
| Macrophage types | Suggested roles | Markers | Different stimulator factors | References |
|---|---|---|---|---|
| M1 | Pro-inflammation, microbicidal effect, tumor resistance | IL-6, IL-10 (low), IL-12 (high), iNOS, CD80, CD86, CXCL9, CXCL10, CXCL11, CCL15, CCL20, CCL22, TLR2, TLR4, MHCII, TNF-α | IL-1, IL-6, IL-12, CXCL1-3, CXCL-5, CXCL8-10, CCL2, Type I IFN, IFN-γ, TNF-α, STAT1, iNOS, LPS, M-CSF, NF-κB, IRF5 miR-155, miR-125b, DNMT1, DNMT3b, HDAC3 | [19, 28–31] |
| M2a | Allergy, profibrotic, anti-inflammatory, wound healing | IL-10, IL-1R, IL-27Rα, CCL1, CCL17, CCL18, CCL22, CD11b, CD45, CD206, YM1, RELMα, IGF1, DCIR, Stabilin 1, Factor XIII-A, Ly6C, TREM-2, DC-SIGN | IL-4, IL-10, IL-13, (PPAR-γ) | [19, 28, 32–35] |
| M2b | Th2 activation, immune regulation, promoting infection, tumor progression | IL-6, TNF-α, CD86, SPHK1 | IL-1β, LPS | [28, 31, 36] |
| M2c | Immunosuppression, phagocytosis, tissue repair, matrix remodeling | IL-10, CXCL13, CD163, CD206, CXCR4, TGF-β, MerTK, |
IL-10, glucocorticoids IL-6, IL-10, TNF-α, TLR, |
[28, 36, 37] |
| M2d | Tumor progression, angiogenesis, clearance of apoptotic tissue | IL-10, VEGF, TGF-β, | LPS | [28, 36, 38] |
CCL, C–C chemokine ligand; CXCL, C–X–C chemokine ligand; CXCR, C–X–C chemokine receptor; DCIR, dendritic cell immunoreceptor; IFN, interferon; IFNγ, interferon-γ; IL, interleukin; IL-1R, IL-1 receptor; IL-27Rα, IL-27 receptor α-chain; iNOS, inducible nitric-oxide synthase; RELMα, resistin-like molecule-α; SPHK1, sphingosine kinase 1; TLR, Toll-like receptor; CD, cluster of differentiation; TGF-β, transforming growth factor-β; STATs, signal transducer and activator of transcription; PPAR-γ, peroxisome proliferator-activated receptor gamma; TNF-α, tumor necrotic factor-α; YM1, chitinase-like protein 3; LPS, lipopolysaccharides; VEGF, vascular endothelial growth factor; ICAM, intercellular adhesion molecule; DC-SIGN, dendritic cell-specific ICAM-grabbing non integrin; IRF5, interferon regulatory factor 5; HDAC3, histone deacetylase 3; MerTK, myeloid epithelial reproductive tyrosine kinase; M-CSF, macrophage-colony-stimulating factor; DNMT, DNA methyl transferase; miRs, microRNAs; NF-κB, nuclear factor-κB; MHCII, major histocompatibility complex II; IGF, insulin-like growth factor; Ly6C, lymphocyte antigen 6 complex; TREM-2, triggering receptor expressed on myeloid cells 2
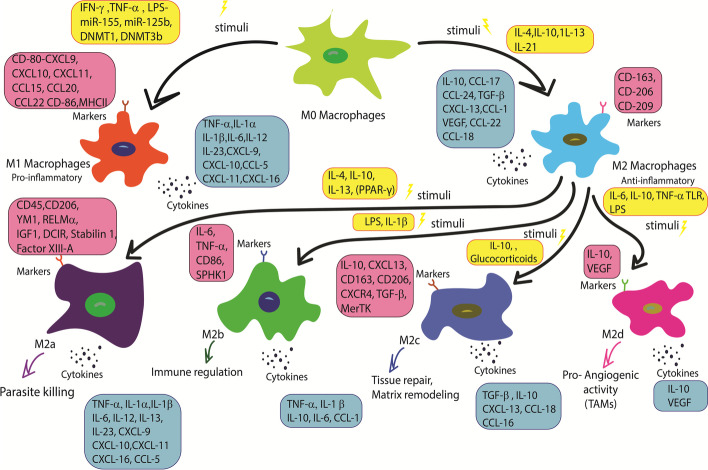
The polarization of macrophages is a dynamic process, so it can be reversed by different microenvironment conditions in different biological conditions and diseases. Macrophages can polarize with more than two forms [24]. M2 macrophage, also called activated or healing macrophage, was first described in the 1990s [25]. Subsets of M2 macrophages include M2a, M2b, M2c, and M2d, with different properties such as cell markers, cytokines, and functions, i.e., M2a enhances cell growth and tissue repair while M2b, M2c, and M2d play crucial roles in inflammation, phagocytosis, and tumor progression, respectively [16, 26]. M2d macrophages are the main element of tumor microenvironment and are generally called tumor-associated macrophage (TAM). They could promote cancer-related processes such as progression and invasion of cancerous cells (Fig. 1) [27, 28]. There is a dynamic balance between different types of macrophages that could cause a variety of diseases when it is disturbed. The number of tissue-resident macrophages is regulated by colony-stimulating factor-1 (CSF-1) or macrophage-colony-stimulating factor (M-CSF), interleukin-34 (IL-34), and colony-stimulating factor-1 receptor (CSF-1R) [4]. M1 macrophages are the first agents of protection in blocking the intracellular pathogens, and their activation can promote T-helper lymphocytes type 1 (Th1) polarization. M1 macrophages release great amounts of some cytokines that have pro-inflammatory roles, including tumor necrotic factor-α (TNF-α), monocyte chemo attractant protein-1 (MCP-1), IL-6, IL-1, IL-12, type 1 interferons (IFNs), inducible nitric oxide synthase (iNOS), and C–X–C motif chemokine ligands (CXCLs) such as CXCL1-3, CXCL5, and CXCL8-10.
Fig. 1.
Macrophage polarization phenotypes and subtypes according to their different characteristics have many roles in immune responses. M1 macrophages have a pro-inflammatory role by their cytokines, but M2 macrophages, which are divided into four subtypes, have many different roles. For example, M2a macrophages play an important role in parasite killing, M2b macrophages function as immune system regulators, M2c macrophages assist in the wound healing process, and M2d macrophages have a pro-angiogenic role and are very important in tumor progression. CCL, C–C chemokine ligand; CXCL, C–X–C chemokine ligand; CXCR, C–X–C chemokine receptor; DCIR, dendritic cell immunoreceptor; IFN, interferon; IFNγ, interferon-γ; IL, interleukin; RELMα, resistin-like molecule-α; SPHK1, sphingosine kinase 1; TLR, Toll-like receptor; CD, cluster of differentiation; TGF-β, transforming growth factor-β; PPAR-γ, peroxisome proliferator-activated receptor gamma; TNF-α, tumor necrotic factor-α; YM1, chitinase-like protein 3; LPS, lipopolysaccharides; VEGF, vascular endothelial growth factor; MerTK, myeloid epithelial reproductive tyrosine kinase; DNMT, DNA methyl transferase; miRs, microRNAs; MHCII, major histocompatibility complex II; IGF, insulin-like growth factor
M2 macrophages are involved in infections caused by fungal, parasitic, or helminthic pathogens and conversely express high level of dectin-1, DC-SIGN (CD209), mannose receptor (CD206), CD163, scavenger receptor A and B-1, C–C chemokine receptor 2 (CCR2), C–X–C motif chemokine receptor 1 (CXCR1), and CXCR2. M2 macrophages produce materials that play a role in tissue remodeling and repair, such as IL-10, chitinase-like protein 3 (YM1), macrophage and granulocyte inducer-form 1 (MgI1), and arginase-1 [4, 16]. Arginine metabolism pathways play a central role in macrophage polarization (Fig. 2) [29, 30]. Macrophage polarization is governed by the surrounding microenvironment, including cytokines and other components such as oligosaccharides, or by exosomes [22, 31]. On the other hand, epigenetic mechanisms such as chromatin remodeling, DNA methylation (DNAm), and histone modifications can control this process in connection with different factors. It was demonstrated that different levels of DNA methyl transferase 1 (DNMT 1), 3a and b, are expressed in M1 and M2 macrophages [4].
Fig. 2.
Mammalian arginine metabolism pathways and M1 and M2 macrophage polarization. Arginine metabolism can be derived via NOS or arginase. NOS, which is expressed in M1 macrophages, causes arginine metabolism to release NO and citrulline, and M2 macrophages synthesize arginase, which causes arginine metabolism to release ornithine and urea. Downstream pathways of ornithine include putrescine, spermidine, and spermine, which hydrolyze products of ODC, SRM, and spermine synthase, respectively. Spermine can be resynthesized to spermidine by SMOX. As shown in the figure, putrescine and spermine downregulate the polarization of the M1 macrophages. Spermidine upregulates M1 macrophage polarization. In the case of M2 macrophage polarization, spermidine and spermine have inhibitor and enhancer effects, respectively. M1 macrophages increase NOS, but M2 macrophages upregulate arginase and ODC. Both arginine metabolic pathways arrest each other. Enzymes are shown by blue boxes and metabolites by yellow boxes, respectively. NOS, nitric oxide synthase; NO, nitric oxide; ODC, ornithine decarboxylase; SRM, spermidine synthase; SMOX, spermine oxidase
The importance of macrophage polarization balance
Macrophage activation is necessary for the appropriate response against pathogen spreading in infected tissue. The process begins with pathogen-associated molecules releasing active danger signals that induce most tissue-resident macrophages to M1 polarization with nitrogen/oxygen-reactive agents and pro-inflammatory cytokine production ability. The next step is clearing cellular debris, then wound-healing signals commence M2 polarization with anti-inflammatory activity [26, 32–34]. Data validate the association between various diseases and the balance of M1/M2 macrophage polarization [35]. M1/M2 ratio and the regulation of macrophage polarization are very important. This ratio can signal progression of many inflammation-related diseases, for example, in psoriasis, which is a chronic inflammatory skin disorder. M1 macrophage markers are more abundant than M2 macrophage markers in psoriatic tissues [36]. Some pathogens and even tumors are able to reduce the M1/M2 ratio to avoid inflammation response [37–39]. For instance, some Lactobacillus are able to inhibit the formation of foam cells, which are a type of macrophage with lipoprotein ingestion activity [40]. Macrophage polarization is linked with some clinical conditions, including diabetes and obesity [3, 41], rheumatoid arthritis (RA) [42–44], chronic obstructive pulmonary disease [45], atherosclerosis [46, 47], non-alcoholic fatty liver disease (NAFLD) [48], osteoclastogenesis [49, 50], asthma [51], hypertension, and cardiovascular disease [52].
Balanced M1/M2 ratios are necessary for appropriate inflammatory response [16, 53]. Different stimuli factors or pathways involved in macrophage polarization can be promising candidates for therapeutic targets (Table 2) [4, 8, 54]. For instance, thiazolidinediones (TZDs), which target a member of the M2-like macrophage pathway, peroxisome proliferator-activated receptor gamma (PPAR-γ), are used for patients with type 2 diabetes (T2D) [55]. In a clinical study, it was observed that reducing the ratio of M1/M2 macrophages by blocking T-cell death-associated gene 8 (TDAG8), which has pro-inflammatory role, can attenuate RA progression (NSC745885) [56].
Table 2.
Immunomodulatory drugs that target macrophage polarization
| immunomodulatory drugs | Functions | References |
|---|---|---|
| Thapsigargin | Promote M2 polarization | [95] |
| Glucocorticoids |
Trigger M2 polarization |
[96] |
| Azithromycin | Promotes polarization from M1 to M2 | [97] |
| 5-Aminosalicylates (5-ASAs) | Inhibitory role in macrophage activation and inflammation suppressor | [98] |
| [6-(1-Methyl-4-nitroimidazol-5-yl)thiopurine] | Repressed nitric oxide synthase (iNOS) expression | [99] |
| Imiquimod | Restore pro-inflammatory of TAMs | [100] |
|
PLX3397, PLX108-01 (pexidartinib) |
Deplete macrophages | [101–103] |
| Trabectedin | Deplete macrophages | [104] |
|
CP-690,550 (tofacitinib) |
Inhibit modulate gene expression in macrophages | [105] |
|
Hyaluronic acid oligosaccharides |
Modulate macrophage polarity |
[106] |
| Tocilizumab |
M1 macrophage suppression |
[107, 108] |
Macrophages possess phagocytosis activity, which makes them able to capture nanoscale particles, and thus are appropriate candidates for targeting macrophages [57–61]. In a study, a bioactive nanodevice was designed to convert the M1 phenotype to the M2 phenotype. A nanodevice is a peptide-coated gold nanoparticle (GNP) that promotes inflammation resolution. It also can be used as a novel therapeutic agent for patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) [62]. It has been shown that nanoparticles, including designed miRNAs or siRNAs, switch macrophage polarization in some disease conditions [63, 64]. Clinical and experimental data have shown that M2 macrophages, which are TAMs, improve the growth, migration, invasion, and immunosuppressive activities of tumor cells [65–67]. Various therapeutic strategies targeting TAMs, depletion of the M2 macrophage ratio, or converting M2 macrophages to M1 macrophages are highlighted as potential strategies for suppressing tumor progression [65, 68–70]. TAMs can be used as novel targets in cancer therapy. For instance, a saponin component isolated from Astragali radix, called astragaloside IV (AS-IV), is reported to reduce tumor growth and metastasis by arresting the polarization of M2 macrophages through the adenosine monophosphate-activated protein kinase (AMPK) signaling pathway [65, 71].
Another study has demonstrated that M1 macrophage induction can increase cellular apoptosis and decrease tumor metastasis and chemotherapy resistance in mice with hepatocellular carcinoma (HCC) [72]. Macrophage targeting strategies in combination with chemotherapies exhibit more antitumor activity [73]. Among the autoimmune diseases caused by imbalanced M1/M2 ratio are systemic lupus erythematosus (SLE) [74], inflammatory bowel diseases (IBD) [75], autoimmune myocarditis [76], and autoimmune neuritis [77, 78]. Chronic inflammation is associated with age-related diseases such as cardiovascular disease, diabetes, and Alzheimer’s disease [5]. Much research has revealed that macrophages participate in the process of pregnancy [79] and could have important effects on preeclampsia, miscarriage, and preterm birth [32]. Different phenotypes and functions of macrophages are essential for each phase of pregnancy to establish and maintain pregnancy. Decidual macrophages participate in implantation, spiral artery remodeling, and angiogenesis of embryo, and they also protect the embryo from pathogens and maternal immune responses [80].
According to various studies, different polarized states of macrophages have been associated with diseases, including cystic fibrosis (CF) and asthma; high level of M2-polarized macrophages is correlated with higher-severity asthma [81]. Accumulating data have shown indispensable roles for M2b macrophages in cardiovascular diseases [82]. In addition to M1 and M2 macrophages, a “chimeric” M1–M2 type with mixed biological function and phenotype that can cause impaired inflammation conditions is described in some cases such as rheumatoid arthritis [83]. In fact, recent evidence shows a continuum of different macrophages with different markers and phenotypes that strongly depend on their microenvironment. Therefore, they can be considered as a spectrum [84–86], although simplified macrophage classification (M1/M2) is used for better understanding. M1 and M2 macrophages can be reprogrammed by different stimuli signals. These reversible changes are essential during inflammation and its resolution phases [87, 88]. Of note, the tumor microenvironment (TME) has a vital effect on cancer progression [89, 90]. Macrophages are able to alter their features according to the TME. Therefore, macrophage polarization can be considered as a therapeutic strategy for cancer treatment [66].
Inflammation and the role of macrophage polarization in this process
Inflammation is a physiological condition that occurs in response to various situations, such as injury and infection. Acute inflammation is the first mechanism in responding to these conditions [91]. Uncontrolled acute inflammation may lead to chronic inflammation, which has been related to many diseases [92]. Sterile inflammation (SI) occurs by nonmicrobial factors such as chemical, physical, or metabolic stimuli, while nonsterile inflammation occurs by infection [93, 94]. Regenerative inflammation takes place in cases of low-grade damage or in highly regenerative tissues, such as the liver, and this type of inflammation plays a critical role in regeneration and repair [95]. Fibrotic inflammation occurs as a response to extensive damage or in poorly regenerative tissues, such as the myocardium. Macrophages play a crucial role in fibrotic inflammation [96]. Inflammation can lead to different immune responses via releasing molecular mediators. These mediators have roles in the direction of vascular responses, immune cell recruitment, macrophage polarization, pathogen clearance, repair of damaged tissue, and restoration of homeostasis. The balance of signal transducer and activator of transcription (STATs) activation has a very important role in macrophage polarization. The activation of STAT1 can lead to M1 macrophage polarization. This is important in the process of cytotoxicity and pro-inflammatory functions. On the contrary, some cytokines such as IL-4/IL-13 and IL-10 and activation of STAT3 and STAT6 can increase M2 polarization. Some other factors such as DNA methylation, chromatin remodeling, histone modification, and meta-inflammation, caused by chronic overnutrition and obesity, are involved in macrophage polarization. There are many clinical trials on macrophage polarization and inflammation (Table 3) [16, 97, 98]. Cardiac macrophages (CMs) are tissue-resident macrophages that are critical agents in the generation and development of cardiac inflammation, tissue remodeling, and repair. CMs are activated by the recognition of DAMPs or PAMPs. via cytokines released from inflammatory cells in the myocardium. An example of this is a promotion of M2 phenotype in dead cell clearance processes and an increase in the level of IL-10 and transforming growth factor-β (TGF-β), but pro-inflammatory cytokines such as TNF-α promote the M1 phenotype [99]. Unregulated immune responses mediated by macrophages may lead to chronic kidney disease (CKD). The balance of macrophage polarization between M1 phenotype and M2 phenotype is important in tissue injury.
Table 3.
Clinical trials on macrophage polarization and inflammation
| Status | Study title | Intervention | ClinicalTrials.gov identifier |
|---|---|---|---|
| Recruiting | Treatment of macrophage activation syndrome (MAS) with anakinra |
•Drug: kineret •Drug: placebo |
NCT02780583 |
| Completed | Effect of liraglutide (Victoza) on inflammation in human adipose tissue and blood |
•Drug: Victoza (liraglutide) with dietician monitoring •Other: placebo with dietician monitoring |
NCT02650206 |
| Completed | The effect of gut sterilization on macrophage activation in patients with alcoholic hepatitis |
•Drug: combined vancomycin and gentamycin and meropenem |
NCT03157388 |
| Completed | Macrophage activation markers during sofosbuvir-based treatment regimens of chronic hepatitis C |
•Drug: galactose •Procedure: gastroscopy •Procedure: liver biopsy •Procedure: FibroScan •Procedure: liver vein catheterization •Drug: sofosbuvir |
NCT02528461 |
| Unknown status | New candidate criteria for diagnosis of macrophage activation syndrome | – | NCT01095146 |
| Completed | Exploration of immunity in Gaucher disease | – | NCT01358188 |
| Completed | A study to investigate the safety and efficacy of emapalumab, an anti-IFN-gamma mAb in patients with systemic juvenile idiopathic arthritis (sJIA) or adult-onset Still’s disease (AOSD) developing macrophage activation syndrome/secondary HLH (MAS/sHLH) | •Drug: emapalumab | NCT03311854 |
| Recruiting | sCD163 in patients with PBC—assessment of disease severity and prognosis | •Other: blood samples, FibroScan, and questionnaires | NCT02924701 |
| Completed | A role for RAGE/TXNIP/inflammasome axis in alveolar macrophage activation during ARDS (RIAMA): a proof-of concept clinical study | •Other: RAGE/TXNIP/inflammasome axis | NCT02545621 |
| Recruiting |
sCD163 in patients with PBC—assessment of treatment response |
•Other: blood samples •Device: FibroScan •Other: questionnaires •Biological: liver biopsy |
NCT02931513 |
| Completed | Downmodulating monocyte activation for HIV-1-associated neurocognitive disorders (HAND) |
•Drug: atorvastatin (Lipitor) •Drug: placebo |
NCT01600170 |
| Completed | A trial of validation and restoration of immune dysfunction in severe infections and sepsis |
•Drug: anakinra •Drug: recombinant human interferon gamma •Drug: placebo |
NCT03332225 |
M1 macrophages play a key role in CKD. These macrophages increase plasma pro-inflammatory biomarkers such as TNF-α in patients, which may lead to chronic renal insufficiency. Furthermore, M2 macrophages are involved in chronic renal inflammation, especially in the repair phase, where M1 macrophages switch to M2 macrophages and secrete anti-inflammatory cytokines such as IL-10, IL-22, and TGF-β. M2 macrophages are involved more in the progression of fibrosis than M1 macrophages because they secret profibrotic factors such as TGF-β [100]. Adipocytes can play an important role in the management of macrophage polarization in adipose tissue. In healthy conditions, adipocytes promote M2-like polarization, but in obesity, adipocytes may favor the prevalence of M1-like macrophage polarization [101, 102]. Imbalance of inflammatory responses can cause many inflammatory insufficiencies, like what happens in IBD. In this case, lamina propria macrophages from patients with IBD have M1 phenotype rather than M2 phenotype, and as mentioned previously, these macrophages can produce a large amount of pro-inflammatory cytokines [103]. The polarization of macrophages is tied to glycolytic changes and oxidative phosphorylation (OXPHOS) metabolism. Indeed, M1 macrophages rely on glycolytic changes but M2 macrophages rely on fatty-acid-fueled OXPHOS. Many risk factors change macrophage polarization, including obesity and hypertension. These factors can lead to chronic and systemic inflammation by M1 macrophage activation. Obesity and hypertension can change target-organ damage by hormones, local inflammatory signals, and hypoxia-induced signaling or alteration in glycolytic- OXPHOS paradigm in macrophages [104]. Macrophage polarization processes and their regulation are very important for sufficient immune responses, and any skew in these processes may lead to some inflammation disorders [105].
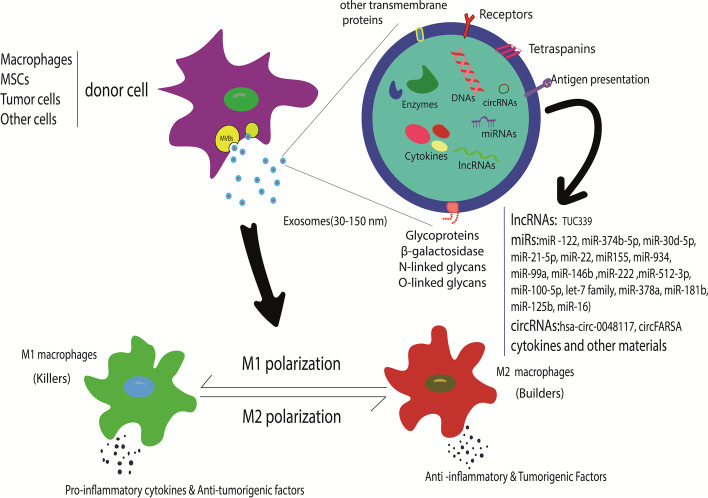
Exosomes involve in macrophage polarization
Exosomes are a subset of nanoscale (30–150 nm) extracellular vesicles (EVs) that are released from almost every eukaryotic cell. Exosomes carry and deliver biological material, including proteins, lipids, saccharides, and genetic signals such as messenger ribonucleic acid (mRNAs), microRNAs (miRs), long noncoding RNAs (lncRNAs), deoxyribonucleic acid (DNAs), and circular RNAs (circRNAs). They have a very important role in cell communication. Exosomes have various effects on immune cell responses, stromal cells, and extracellular matrix (ECM), and can even alter them and their behaviors [106–108]. Exosomes derived from different cells play a key role in macrophage polarization processes. They are also able to change macrophage polarization. Recently, a research study demonstrated that M2-Exo causes a reprogramming of the M1 phenotype to the M2 phenotype (Fig. 3) [109]. Mesenchymal stromal cells (MSCs) have great potential to differentiate into many cell types. Numerous studies have demonstrated that exosomes secreted by MSCs have an important role in macrophage polarization [110, 111]. Exosomes present in serum have demonstrated involvement in IBD. A study reported that pregnancy zone protein (PZP) can be used as a biomarker in IBD [78].
Fig. 3.
Exosomes are derived from different cells, including MSCs, tumor cells, or other cells that are present in the microenvironment such as macrophages. These exosomes can switch macrophage polarization according to their cargos. MSCs, mesenchymal stromal cells; lncRNA, long noncoding RNAs; miR, microRNAs; circRNA, circular RNA
Exosomes derived from MSCs of human bone marrow assist in the regulation of inflammatory responses. The systemic administration of these exosomes could substantially mitigate colitis in various models of IBD [112]. MSC exosomes have an important role in neuroinflammatory conditions. These exosomes can regulate macrophage polarization and change it toward an anti-inflammatory phenotype [113]. Also, MSC exosomes have a tumor-growth-suppressive effect by increasing inflammatory infiltration [111]. Pro-inflammatory bone-marrow-derived mesenchymal stem cells (BMMSCs) secrete exosomes that potentially promote macrophage M2 polarization. BMMSCs exosomes can reduce macrophage M1 polarization by regulation of the protein kinase B1/protein kinase B2 (AKT1/AKT2) signaling pathway and relieve myocardial injury [114, 115]. Fibronectin type III domain-containing protein 5 (FNDC5) is a transmembrane protein located in the cytoplasm that can increase BMMSC exosome secretion. This mechanism can promote M2 polarization by the nuclear factor-κB (NF-κB) signaling pathway [116, 117]. A study reported that administration of BMMSC-derived exosomes can induce macrophage M2 polarization, improve the inflammatory microenvironment, and promote fibrocartilage regeneration, especially at the tendon–bone interface [118].
Exosomes of adipose-derived stem cells (ADSCs) have an important role in obesity-associated inflammation and other metabolic disorders. They can induce anti-inflammation M2 macrophage polarization by carrying active STAT3 and inhibiting macrophage inflammatory responses [119]. ADSC exosomes have a critical role in myocardial repair after myocardial infection (MI). These exosomes can decrease lipopolysaccharides (LPS)-induced inflammation by activating sphingosine 1-phosphate (S1P), sphingosine kinase 1 (SphK1 or SK1), and sphingosine-1-phosphate receptor 1 (S1PR1) signaling, which leads to promotion of macrophage M2 polarization [120].
Exosomes derived from human umbilical cord mesenchymal stem cells (hUCMSCs) have involvement in regulation of macrophage polarization. They can inhibit M1 polarization and promote M2 polarization. These exosomes can inhibit the expression of tumor necrosis factor receptor-associated factor 1 (TRAF1), which has been shown to be involved in the macrophage M1 polarization mechanism and ameliorate steroid-resistant asthma (SSRA), an important clinical problem in asthma management [121]. Exosomes carry genetic signals such as miRs, which play a critical role in macrophage polarization. For example, mammary epithelial cells (MECs) can regulate immune system responses, secreting exosomes carrying exosomal miR-122. This miR can promote polarization of M1 macrophages by suppressing cytokine signaling 1 (SOCS1), STAT1, and STAT3 [122].
It has been demonstrated that exosomal miR-21-5p, originated from MSCs, can stimulate the polarization of M2 macrophages. It can reduce the inflammatory response and promote heart cell repair after myocardial ischemia–reperfusion injury [123]. It is reported that exosomal miR-21-5p released from MSCs has an important role in macrophage polarization. miR-21-5p induces M2 polarization by mediating phosphate and tensin homolog (PTEN) downregulation. This mechanism can support lung cancer cell growth and facilitate their invasion [110]. Upregulation of miR-374b-5p in exosomes, derived from hypoxic tubular epithelial cells (TECs), reduces SOCS1 expression and promotes M1 macrophage activation during renal ischemia–reperfusion injury (RIRI) conditions [124, 125]. Exosomes derived from polymorph nuclear neutrophils (PMNs) have an important role in sepsis-related ALI. These exosomes promote M1 macrophage activation by miR-30d-5p, which targets SOCS-1 and sirtuin 1 (SIRT1) in macrophages [126]. Atherosclerosis is an inflammatory disease that leads to clogging of blood vessels by the accumulation of lipids.
Exosomes, which originate from different cells, have a very important role in atherosclerosis. For example, exosomal miR-155 can enlarge inflammatory cytokines and M1 polarization markers such as cluster of differentiation 80 (CD80) and CD86, which are involved in the process of atherosclerosis through pro-inflammatory M1 polarization [127]. Some exosomal miRs such as miR-100-5p, miR-512-3p, let-7 family, and miR-21a-5p are derived from MSCs and have various properties. As these exosomal miRs can induce M2 macrophage polarization, they are capable of suppressing atherosclerosis [128, 129]. Bone-marrow-derived macrophages (BMDMs) can release exosomal miRs with anti-inflammatory properties, including miR-99a, miR-146b, and miR-378a, which are capable of promoting M2 polarization in BMDMs [127, 130]. Wu et al. generated exosomes with anti-inflammatory functions in atherosclerosis. These exosomes are derived from M2 macrophages and contain hexyl 5-aminolevulinate hydrochloride (HAL), which is FDA-approved and has an anti-inflammatory effect. This makes HALM2 exosomes a promising candidate for atherosclerosis therapy applying macrophage-derived exosomes [127, 131].
Exosomes can modulate immune responses in tumor cells. Tumor-derived exosomes (TEs) can change macrophage polarization, and could activate anti-inflammatory pro-tumorigenic M2 macrophage phenotypes or pro-inflammatory anti-tumorigenic M1 macrophage phenotypes, change the M1/M2 ratio in the TME, and promote tumor growth [132]. Melanoma-derived exosomes can upregulate specific macrophage polarization factors and promote mixed M1 and M2 macrophage phenotypes (128) Lung tumor cell-derived exosomes can reprogram macrophage metabolism and promote M2 macrophage polarization [133]. Exosomal miR-222 derived from adriamycin-resistant breast cancer cells can target phosphatases and PTEN gene, and activate the Akt pathway, so it can switch macrophage polarization to M2 phenotype and stimulate tumor growth [134, 135]. Exosomal miR-222 derived from adriamycin-resistant breast cancer cells can directly target phosphatase and the PTEN gene, activate the Akt pathway, convert macrophage polarization to M2 phenotype, and stimulate tumor growth by M2 macrophage polarization [136]. It has been reported that exosomes derived from hypoxic tumor cells can elevate oxidative phosphorylation in macrophages that originate from bone marrow by let-7a exosomal miR, which suppresses insulin-Akt-mammalian target of rapamycin (mTOR) signaling pathway and promotes M2-like macrophages [137].
Exosomal lncRNAs participate in macrophage polarization. For example, HCC-derived exosomes contain different levels of exosomal lncRNA TUC339 that regulate macrophage polarization [138]. It has been identified that circRNA, which is carried by exosomes, has important regulatory roles in different pathophysiological processes. For example, exosomal hsa-circ-0048117 has been upregulated in esophageal squamous cell carcinoma (ESCC). Upregulation of hsa-circ0048117 can promote M2 macrophage polarization and regulate ESCC progression. Another exosomal circRNA is circFARSA, which is highly expressed in tumor cells and is capable of inducing the promotion of M2 phenotypes and facilitating metastasis in non-small cell lung cancer (NSCLC) cells [139]. M1 macrophage-derived exosomes can be used as paclitaxel (PTX) nanocarriers and enhance antitumor activity of PTX [140]. These can also be tumor biomarkers such as exosomal miR-16, which are received by macrophages. These act as metastasis biomarkers in breast cancer [141], showing that exosomes can be employed for the treatment of cancer [59].
Conclusion
Recently, it was confirmed that inflammation is a sign of chronic disease such as cancers, diabetes, cardiovascular, and neurologic system disorders. This review points out that the plasticity features of macrophages give them a critical role in inflammatory conditions. Macrophage polarization can be switched from pro-inflammatory with anti-tumorigenic macrophages (M1-like) phenotype to anti-inflammatory with pro-tumorigenic (M2-like) phenotype. In addition. The balance between different types of macrophages plays a key role in immune system dysfunctions. Exosomes as vehicles in cell communication have serious involvement in macrophage polarization. Cancerous cells can modulate immune cell responses by their secreted exosomes. There are many immune-based strategies that have been established for cancer therapy such as cancer vaccines. Various agents have been used for delivering of medicines.
Exosomes can change macrophage polarization and promote or prevent different subtypes of macrophage population via their cargos, such as miRs, cricRNAs, and lncRNAs. Numerous studies have reported that these nano-sized vesicles could be engineered for medical aims and developed as delivery systems for immune system modulation. However, there are several unsolved problems in the clinical application of exosomes as biologically derived nanovesicles. Examples of this are selecting the appropriate exosome isolation method, ensuring purity of exosomes, and identifying an efficient method for exosome modification. In conclusion, further studies on macrophage polarization mechanisms and its related pathways are needed to elucidate exosomes’ roles in these pathways and their therapeutic potential in the development of immunotherapies for various medical aims.
Acknowledgements
Not applicable.
Abbreviations
- MPS
Mononuclear phagocyte system
- DCs
Dendritic cells
- CNS
Central nervous system
- TAM
Tumor-associated macrophages
- CSF-1
Colony-stimulating factor-1
- M-CSF
Macrophage-colony-stimulating factor
- CSF-1R
Colony-stimulating factor-1 receptor
- Th1
T-helper lymphocytes type 1
- TNF-α
Tumor necrotic factor-α
- MCP-1
Monocyte chemo attractant protein-1
- IL
Interleukin
- IFNs
Interferons
- iNOS
Inducible nitric oxide synthase
- CXCLs
C–X–C motif chemokine ligands
- CCR
C–C chemokine receptor
- CXCR
C–X–C motif chemokine receptor
- YM1
Chitinase-like protein 3
- MgI1
Macrophage and granulocyte inducer-form 1
- DNMT
DNA methyl transferase
- DNAm
DNA methylation
- RA
Rheumatoid arthritis
- NAFLD
Non-alcoholic fatty liver disease
- TZDs
Thiazolidinediones
- PPAR-γ
Peroxisome proliferator-activated receptor gamma
- T2D
Type 2 diabetes
- TDAG8
T-cell death-associated gene 8
- GNP
Gold nanoparticle
- ALI
Acute lung injury
- ARDS
Acute respiratory distress syndrome
- AS-IV
Astragaloside IV
- AMPK
Adenosine monophosphate-activated protein kinase
- HCC
Hepatocellular carcinoma
- SLE
Systemic lupus erythematosus
- IBD
Inflammatory bowel diseases
- CF
Cystic fibrosis
- TME
Tumor microenvironment
- STATs
Signal transducer and activator of transcription
- CMs
Cardiac macrophages
- TGF-β
Transforming growth factor-β
- CKD
Chronic kidney disease
- OXPHOS
Oxidative phosphorylation
- EVs
Extracellular vesicles
- DNA
Deoxyribonucleic acid
- miRs
MicroRNAs
- lncRNA
Long noncoding RNAs
- circRNAs
Circular RNAs
- mRNA
Messenger ribonucleic acid
- ECM
Extracellular matrix
- MSCs
Mesenchymal stromal cells
- BMMSCs
Bone marrow-derived mesenchymal stem cells
- AKT
Protein kinase B
- FNDC5
Fibronectin type III domain-containing protein 5
- NF-κB
Nuclear factor-κB
- ADSCs
Adipose derived stem cells
- MI
Myocardial infection
- LPS
Lipopolysaccharides
- S1P
Sphingosine 1-phosphate
- SI
Sterile inflammation
- SphK1 or SK1
Sphingosine kinase 1
- S1PR1
Sphingosine-1-phosphate receptor 1
- hUCMSCs
Human umbilical cord mesenchymal stem cells
- TRAF1
Tumor necrosis factor receptor-associated factor 1
- SSRA
Steroid-resistant asthma
- MECs
Mammary epithelial cells
- SOCS1
Suppressor of cytokine signaling 1
- PMNs
Polymorph nuclear neutrophils
- PTEN
Phosphate and tensin homolog
- PZP
Pregnancy zone protein
- TECs
Tubular epithelial cells
- RIRI
Renal ischemia–reperfusion injury
- SIRT1
Sirtuin 1
- BMDMs
Bone-marrow-derived macrophages
- CD
Cluster of differentiation
- HAL
Hexyl 5-aminolevulinate hydrochloride
- TEs
Tumor-derived exosomes
- mTOR
Mammalian target of rapamycin
- ESCC
Esophageal squamous cell carcinoma
- NSCLC
Non-small cell lung cancer
- PTX
Paclitaxel
- CCL
Chemokine (C–C motif) ligand
- TLR
Toll-like receptor
- VEGF
Vascular endothelial growth factor
- ICAM
Intercellular adhesion molecule
- DC-SIGN
Dendritic cell-specific ICAM-grabbing non integrin
- IRF5
Interferon regulatory factor 5
- HDAC3
Histone deacetylase 3
- MerTK
Myeloid epithelial reproductive tyrosine kinase
- NOS
Nitric oxide synthase
- NO
Nitric oxide
- ODC
Ornithine decarboxylase
- SRM
Spermidine synthase
- SMOX
Spermine oxidase
- siRNA
Small interfering RNA
- DAMP
Danger-associated molecular patterns
- PAMP
Pathogen-associated molecular patterns
- M2-Exo
M2-derived exosomes
- FDA
US Food and Drug Administration
Author contributions
A.T.G.: writing—review and editing and figure drawing. N.A.H.: writing—review and editing. E.M.: editing. M.D.: supervision and editing. All authors read and approved the final manuscript.
Funding
This study received no external founding.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abdulwahab Teflischi Gharavi and Niloofar Asadi Hanjani contributed equally to this work.
References
- 1.Nathan C. Metchnikoff's legacy in 2008. Nat Immunol. 2008;9(7):695–698. doi: 10.1038/ni0708-695. [DOI] [PubMed] [Google Scholar]
- 2.Kaufmann SH. Immunology's foundation: the 100-year anniversary of the Nobel Prize to Paul Ehrlich and Elie Metchnikoff. Nat Immunol. 2008;9(7):705–712. doi: 10.1038/ni0708-705. [DOI] [PubMed] [Google Scholar]
- 3.Chylikova J, Dvorackova J, Tauber Z, Kamarad V. M1/M2 macrophage polarization in human obese adipose tissue. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018;162(2):79–82. doi: 10.5507/bp.2018.015. [DOI] [PubMed] [Google Scholar]
- 4.Parisi L, Gini E, Baci D, Tremolati M, Fanuli M, Bassani B, et al. Macrophage polarization in chronic inflammatory diseases: killers or builders? J Immunol Res. 2018;2018:9. doi: 10.1155/2018/8917804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oishi Y, Manabe I. Macrophages in age-related chronic inflammatory diseases. NPJ Aging Mech Dis. 2016;2(1):1–8. doi: 10.1038/npjamd.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dzik JM. The ancestry and cumulative evolution of immune reactions. Acta Biochim Pol. 2010;57:4. doi: 10.18388/abp.2010_2431. [DOI] [PubMed] [Google Scholar]
- 7.Guo F, Zhang H, Chen C, Hu S, Wang Y, Qiao J, et al. Autophagy favors Brucella melitensis survival in infected macrophages. Cell Mol Biol Lett. 2012;17(2):249–257. doi: 10.2478/s11658-012-0009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vannella KM, Wynn TA. Mechanisms of organ injury and repair by macrophages. Annu Rev Physiol. 2017;79:593–617. doi: 10.1146/annurev-physiol-022516-034356. [DOI] [PubMed] [Google Scholar]
- 9.Peter J. Macrophage polarization. Annu Rev Physiol. 2017;79(1):541–566. doi: 10.1146/annurev-physiol-022516-034339. [DOI] [PubMed] [Google Scholar]
- 10.Xie J, Huang Z, Yu X, Zhou L, Pei F. Clinical implications of macrophage dysfunction in the development of osteoarthritis of the knee. Cytokine Growth Factor Rev. 2019;46:36–44. doi: 10.1016/j.cytogfr.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Liang Y, Yang N, Pan G, Jin B, Wang S, Ji W. Elevated IL-33 promotes expression of MMP2 and MMP9 via activating STAT3 in alveolar macrophages during LPS-induced acute lung injury. Cell Mol Biol Lett. 2018;23(1):52. doi: 10.1186/s11658-018-0117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asaga H, Ishigami A. Microglial expression of peptidylarginine deiminase 2 in the prenatal rat brain. Cell Mol Biol Lett. 2007;12(4):536–544. doi: 10.2478/s11658-007-0025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496(7446):445–455. doi: 10.1038/nature12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X, Chang Y, Wei W. Emerging role of targeting macrophages in rheumatoid arthritis: focus on polarization, metabolism and apoptosis. Cell Prolif. 2020;53(7):e12854. doi: 10.1111/cpr.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Li M, Huang S, Qiao S, Qin Z, Kang C, et al. The effect of buffalo CD14 shRNA on the gene expression of TLR4 signal pathway in buffalo monocyte/macrophages. Cell Mol Biol Lett. 2014;19(4):623–637. doi: 10.2478/s11658-014-0217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atri C, Guerfali FZ, Laouini D. Role of human macrophage polarization in inflammation during infectious diseases. Int J Mol Sci. 2018;19(6):1801. doi: 10.3390/ijms19061801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Reilly C, Doroudian M, Mawhinney L, Donnelly SC. Targeting MIF in cancer: therapeutic strategies, current developments, and future opportunities. Med Res Rev. 2016;36(3):440–460. doi: 10.1002/med.21385. [DOI] [PubMed] [Google Scholar]
- 18.Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41(1):14–20. doi: 10.1016/j.immuni.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li F, Yang Y, Zhu X, Huang L, Xu J. Macrophage polarization modulates development of systemic lupus erythematosus. Cell Physiol Biochem. 2015;37(4):1279–1288. doi: 10.1159/000430251. [DOI] [PubMed] [Google Scholar]
- 20.Lee B-C, Lee J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochem Biophys Acta. 2014;1842(3):446–462. doi: 10.1016/j.bbadis.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly DJ, Popovich PG. Inflammation and its role in neuroprotection, axonal regeneration and functional recovery after spinal cord injury. Exp Neurol. 2008;209(2):378–388. doi: 10.1016/j.expneurol.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, et al. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233(9):6425–6440. doi: 10.1002/jcp.26429. [DOI] [PubMed] [Google Scholar]
- 23.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25(12):677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Linton MF, Moslehi JJ, Babaev VR. Akt signaling in macrophage polarization, survival, and atherosclerosis. Int J Mol Sci. 2019;20(11):2703. doi: 10.3390/ijms20112703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stein M, Keshav S, Harris N, Gordon S. Interleukin 4 potently enhances murine macrophage mannose receptor activity: a marker of alternative immunologic macrophage activation. J Exp Med. 1992;176(1):287–292. doi: 10.1084/jem.176.1.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Funes SC, Rios M, Escobar-Vera J, Kalergis AM. Implications of macrophage polarization in autoimmunity. Immunology. 2018;154(2):186–195. doi: 10.1111/imm.12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu H, Xu JB, He YL, Peng JJ, Zhang XH, Chen CQ, et al. Tumor-associated macrophages promote angiogenesis and lymphangiogenesis of gastric cancer. J Surg Oncol. 2012;106(4):462–468. doi: 10.1002/jso.23110. [DOI] [PubMed] [Google Scholar]
- 28.Tamura R, Tanaka T, Yamamoto Y, Akasaki Y, Sasaki H. Dual role of macrophage in tumor immunity. Immunotherapy. 2018;10(10):899–909. doi: 10.2217/imt-2018-0006. [DOI] [PubMed] [Google Scholar]
- 29.Latour YL, Gobert AP, Wilson KT. The role of polyamines in the regulation of macrophage polarization and function. Amino Acids. 2020;52(2):151–160. doi: 10.1007/s00726-019-02719-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rath T, Baker K, Pyzik M, Blumberg RS. Regulation of immune responses by the neonatal Fc receptor and its therapeutic implications. Front Immunol. 2015;5:664. doi: 10.3389/fimmu.2014.00664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arabpour M, Saghazadeh A, Rezaei N. Anti-inflammatory and M2 macrophage polarization-promoting effect of mesenchymal stem cell-derived exosomes. Int Immunopharmacol. 2021;97:107823. doi: 10.1016/j.intimp.2021.107823. [DOI] [PubMed] [Google Scholar]
- 32.Porta C, Riboldi E, Ippolito A, Sica A, editors. Molecular and epigenetic basis of macrophage polarized activation. In: Seminars in immunology; 2015: Elsevier. [DOI] [PubMed]
- 33.Zhang X, Mosser D. Macrophage activation by endogenous danger signals. J Pathol. 2008;214(2):161–178. doi: 10.1002/path.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Neill A, Tynan A, Mawhinney L, Kennedy S, Caraher E, Poynton F, et al., editors. Macrophage migration inhibitory factor enhances Pseudomonas aeruginosa biofilms, a potential novel therapeutic for cystic fibrosis patients. Irish J Med Sci; 2017: Springer London ltd 236 grays inn rd, 6th floor, London wc1x 8hl, England.
- 35.Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12(4):253–268. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu C-H, Lai C-Y, Yeh D-W, Liu Y-L, Su Y-W, Hsu L-C, et al. Involvement of M1 macrophage polarization in endosomal toll-like receptors activated psoriatic inflammation. Mediat Inflam. 2018;2018:9. doi: 10.1155/2018/3523642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benoit M, Desnues B, Mege J-L. Macrophage polarization in bacterial infections. J Immunol. 2008;181(6):3733–3739. doi: 10.4049/jimmunol.181.6.3733. [DOI] [PubMed] [Google Scholar]
- 38.Domínguez-Soto Á, Usategui A, Casas-Engel M, Simón-Fuentes M, Nieto C, Cuevas VD, et al. Serotonin drives the acquisition of a profibrotic and anti-inflammatory gene profile through the 5-HT7R-PKA signaling axis. Sci Rep. 2017;7(1):1–15. doi: 10.1038/s41598-017-15348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mostafaei S, Kazemnejad A, Azimzadeh Jamalkandi S, Amirhashchi S, Donnelly SC, Armstrong ME, et al. Identification of novel genes in human airway epithelial cells associated with chronic obstructive pulmonary disease (COPD) using machine-based learning algorithms. Sci Rep. 2018;8(1):1–20. doi: 10.1038/s41598-018-33986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ding Y-H, Qian L-Y, Pang J, Lin J-Y, Xu Q, Wang L-H, et al. The regulation of immune cells by Lactobacilli: a potential therapeutic target for anti-atherosclerosis therapy. Oncotarget. 2017;8(35):59915. doi: 10.18632/oncotarget.18346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Investig. 2007;117(1):175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y, Han C-C, Cui D, Li Y, Ma Y, Wei W. Is macrophage polarization important in rheumatoid arthritis? Int Immunopharmacol. 2017;50:345–352. doi: 10.1016/j.intimp.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 43.Kinne RW, Stuhlmüller B, Burmester G-R. Cells of the synovium in rheumatoid arthritis. Macrophages Arthritis Res Ther. 2007;9(6):1–16. doi: 10.1186/ar2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tardito S, Martinelli G, Soldano S, Paolino S, Pacini G, Patane M, et al. Macrophage M1/M2 polarization and rheumatoid arthritis: a systematic review. Autoimmun Rev. 2019;18(11):102397. doi: 10.1016/j.autrev.2019.102397. [DOI] [PubMed] [Google Scholar]
- 45.Shaykhiev R, Krause A, Salit J, Strulovici-Barel Y, Harvey B-G, O'Connor TP, et al. Smoking-dependent reprogramming of alveolar macrophage polarization: implication for pathogenesis of chronic obstructive pulmonary disease. J Immunol. 2009;183(4):2867–2883. doi: 10.4049/jimmunol.0900473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Gaetano M, Crean D, Barry M, Belton O. M1-and M2-type macrophage responses are predictive of adverse outcomes in human atherosclerosis. Front Immunol. 2016;7:275. doi: 10.3389/fimmu.2016.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stöger JL, Gijbels MJ, van der Velden S, Manca M, van der Loos CM, Biessen EA, et al. Distribution of macrophage polarization markers in human atherosclerosis. Atherosclerosis. 2012;225(2):461–468. doi: 10.1016/j.atherosclerosis.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 48.Kazankov K, Jørgensen SMD, Thomsen KL, Møller HJ, Vilstrup H, George J, et al. The role of macrophages in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Nat Rev Gastroenterol Hepatol. 2019;16(3):145–159. doi: 10.1038/s41575-018-0082-x. [DOI] [PubMed] [Google Scholar]
- 49.Fukui S, Iwamoto N, Takatani A, Igawa T, Shimizu T, Umeda M, et al. M1 and M2 monocytes in rheumatoid arthritis: a contribution of imbalance of M1/M2 monocytes to osteoclastogenesis. Front Immunol. 2018;8:1958. doi: 10.3389/fimmu.2017.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 51.Madore A-M, Perron S, Turmel V, Laviolette M, Bissonnette EY, Laprise C. Alveolar macrophages in allergic asthma: an expression signature characterized by heat shock protein pathways. Hum Immunol. 2010;71(2):144–150. doi: 10.1016/j.humimm.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harwani SC. Macrophages under pressure: the role of macrophage polarization in hypertension. Transl Res. 2018;191:45–63. doi: 10.1016/j.trsl.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dehbidi MY, Goodarzi N, Azhdari MH, Doroudian M. Mesenchymal stem cells and their derived exosomes to combat Covid–19. Rev Med Virol. 2021;34:2. doi: 10.1002/rmv.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galeotti C, Kaveri SV, Bayry J. IVIG-mediated effector functions in autoimmune and inflammatory diseases. Int Immunol. 2017;29(11):491–498. doi: 10.1093/intimm/dxx039. [DOI] [PubMed] [Google Scholar]
- 55.Consoli A, Formoso G. Do thiazolidinediones still have a role in treatment of type 2 diabetes mellitus? Diabetes Obes Metab. 2013;15(11):967–977. doi: 10.1111/dom.12101. [DOI] [PubMed] [Google Scholar]
- 56.Kung C-C, Dai S-P, Chiang H, Huang H-S, Sun W-H. Temporal expression patterns of distinct cytokines and M1/M2 macrophage polarization regulate rheumatoid arthritis progression. Mol Biol Rep. 2020;47(5):3423–3437. doi: 10.1007/s11033-020-05422-6. [DOI] [PubMed] [Google Scholar]
- 57.Parayath NN, Parikh A, Amiji MM. Repolarization of tumor-associated macrophages in a genetically engineered nonsmall cell lung cancer model by intraperitoneal administration of hyaluronic acid-based nanoparticles encapsulating microRNA-125b. Nano Lett. 2018;18(6):3571–3579. doi: 10.1021/acs.nanolett.8b00689. [DOI] [PubMed] [Google Scholar]
- 58.Mehanna MM, Mohyeldin SM, Elgindy NA. Respirable nanocarriers as a promising strategy for antitubercular drug delivery. J Control Release. 2014;187:183–197. doi: 10.1016/j.jconrel.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 59.Hanjani NA, Esmaelizad N, Zanganeh S, Gharavi AT, Heidarizadeh P, Radfar M, et al. Emerging role of exosomes as biomarkers in cancer treatment and diagnosis. Crit Rev Oncol Hematol. 2022;169:103565. doi: 10.1016/j.critrevonc.2021.103565. [DOI] [PubMed] [Google Scholar]
- 60.Doroudian M, O'Neill A, O'Reilly C, Tynan A, Mawhinney L, McElroy A, et al. Aerosolized drug-loaded nanoparticles targeting migration inhibitory factors inhibit Pseudomonas aeruginosa-induced inflammation and biofilm formation. Nanomedicine. 2020;15(30):2933–2953. doi: 10.2217/nnm-2020-0344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Doroudian M, O'Reilly C, Crosbie-Staunton K, MacLoughlin R, Prina-Mello A, Volkov Y, et al., editors. Good things come in small packages: An aerosolized delivery system for small molecule inhibitors of macrophage migration inhibitory factor. Irish J Med Sci; 2016: springer London ltd 236 grays inn Rd, 6th floor, London wc1x 8hl, England.
- 62.Wang L, Zhang H, Sun L, Gao W, Xiong Y, Ma A, et al. Manipulation of macrophage polarization by peptide-coated gold nanoparticles and its protective effects on acute lung injury. J Nanobiotechnol. 2020;18(1):1–16. doi: 10.1186/s12951-020-00593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bejerano T, Etzion S, Elyagon S, Etzion Y, Cohen S. Nanoparticle delivery of miRNA-21 mimic to cardiac macrophages improves myocardial remodeling after myocardial infarction. Nano Lett. 2018;18(9):5885–5891. doi: 10.1021/acs.nanolett.8b02578. [DOI] [PubMed] [Google Scholar]
- 64.Kim B, Pang H-B, Kang J, Park J-H, Ruoslahti E, Sailor MJ. Immunogene therapy with fusogenic nanoparticles modulates macrophage response to Staphylococcus aureus. Nat Commun. 2018;9(1):1–13. doi: 10.1038/s41467-018-04390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xu F, Cui W-Q, Wei Y, Cui J, Qiu J, Hu L-L, et al. Astragaloside IV inhibits lung cancer progression and metastasis by modulating macrophage polarization through AMPK signaling. J Exp Clin Cancer Res. 2018;37(1):1–16. doi: 10.1186/s13046-018-0878-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kimura YN, Watari K, Fotovati A, Hosoi F, Yasumoto K, Izumi H, et al. Inflammatory stimuli from macrophages and cancer cells synergistically promote tumor growth and angiogenesis. Cancer Sci. 2007;98(12):2009–2018. doi: 10.1111/j.1349-7006.2007.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mu X, Shi W, Xu Y, Xu C, Zhao T, Geng B, et al. Tumor-derived lactate induces M2 macrophage polarization via the activation of the ERK/STAT3 signaling pathway in breast cancer. Cell Cycle. 2018;17(4):428–438. doi: 10.1080/15384101.2018.1444305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ostuni R, Kratochvill F, Murray PJ, Natoli G. Macrophages and cancer: from mechanisms to therapeutic implications. Trends Immunol. 2015;36(4):229–239. doi: 10.1016/j.it.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 69.Sica A, Schioppa T, Mantovani A, Allavena P. Tumour-associated macrophages are a distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eur J Cancer. 2006;42(6):717–727. doi: 10.1016/j.ejca.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 70.Yu H, Yin S, Zhou S, Shao Y, Sun J, Pang X, et al. Magnolin promotes autophagy and cell cycle arrest via blocking LIF/Stat3/Mcl-1 axis in human colorectal cancers. Cell Death Dis. 2018;9(6):1–13. doi: 10.1038/s41419-018-0660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Singh Y, Pawar VK, Meher JG, Raval K, Kumar A, Shrivastava R, et al. Targeting tumor associated macrophages (TAMs) via nanocarriers. J Control Release. 2017;254:92–106. doi: 10.1016/j.jconrel.2017.03.395. [DOI] [PubMed] [Google Scholar]
- 72.Hu X, Wang H, Han C, Cao X. Src promotes anti-inflammatory (M2) macrophage generation via the IL-4/STAT6 pathway. Cytokine. 2018;111:209–215. doi: 10.1016/j.cyto.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 73.Mehla K, Singh P. Metabolic regulation of macrophage polarization in cancer. Trends Cancer. 2019;5:822–834. doi: 10.1016/j.trecan.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Triantafyllopoulou A, Franzke C-W, Seshan SV, Perino G, Kalliolias GD, Ramanujam M, et al. Proliferative lesions and metalloproteinase activity in murine lupus nephritis mediated by type I interferons and macrophages. Proc Natl Acad Sci USA. 2010;107(7):3012–3017. doi: 10.1073/pnas.0914902107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Steinbach EC, Plevy SE. The role of macrophages and dendritic cells in the initiation of inflammation in IBD. Inflamm Bowel Dis. 2014;20(1):166–175. doi: 10.1097/MIB.0b013e3182a69dca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Su Z, Zhang P, Yu Y, Lu H, Liu Y, Ni P, et al. HMGB1 facilitated macrophage reprogramming towards a proinflammatory M1-like phenotype in experimental autoimmune myocarditis development. Sci Rep. 2016;6:8. doi: 10.1038/srep21884. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 77.Han R, Xiao J, Zhai H, Hao J. Dimethyl fumarate attenuates experimental autoimmune neuritis through the nuclear factor erythroid-derived 2-related factor 2/hemoxygenase-1 pathway by altering the balance of M1/M2 macrophages. J Neuroinflam. 2016;13(1):1–14. doi: 10.1186/s12974-016-0559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shao J, Jin Y, Shao C, Fan H, Wang X, Yang G. Serum exosomal pregnancy zone protein as a promising biomarker in inflammatory bowel disease. Cell Mol Biol Lett. 2021;26(1):36. doi: 10.1186/s11658-021-00280-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hazan AD, Smith SD, Jones RL, Whittle W, Lye SJ, Dunk CE. Vascular-leukocyte interactions: mechanisms of human decidual spiral artery remodeling in vitro. Am J Pathol. 2010;177(2):1017–1030. doi: 10.2353/ajpath.2010.091105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang L-L, Li Z-H, Wang H, Kwak-Kim J, Liao A-H. Cutting edge: the regulatory mechanisms of macrophage polarization and function during pregnancy. J Reprod Immunol. 2022;151:103627. doi: 10.1016/j.jri.2022.103627. [DOI] [PubMed] [Google Scholar]
- 81.Gharib SA, McMahan RS, Eddy WE, Long ME, Parks WC, Aitken ML, et al. Transcriptional and functional diversity of human macrophage repolarization. J Allergy Clin Immunol. 2019;143(4):1536–1548. doi: 10.1016/j.jaci.2018.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang L, Zhang S, Wu H, Rong X, Guo J. M2b macrophage polarization and its roles in diseases. J Leukocyte Biol. 2019;106(2):345–358. doi: 10.1002/JLB.3RU1018-378RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Quero L, Hanser E, Manigold T, Tiaden AN, Kyburz D. TLR2 stimulation impairs anti-inflammatory activity of M2-like macrophages, generating a chimeric M1/M2 phenotype. Arthritis Res Ther. 2017;19(1):1–13. doi: 10.1186/s13075-017-1447-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Palma A, Jarrah AS, Tieri P, Cesareni G, Castiglione F. Gene regulatory network modeling of macrophage differentiation corroborates the continuum hypothesis of polarization states. Front Physiol. 2018;9:1659. doi: 10.3389/fphys.2018.01659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gao T, Huang F, Wang W, Xie Y, Wang B. Interleukin-10 genetically modified clinical-grade mesenchymal stromal cells markedly reinforced functional recovery after spinal cord injury via directing alternative activation of macrophages. Cell Mol Biol Lett. 2022;27(1):1–27. doi: 10.1186/s11658-022-00325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Babazadeh S, Nassiri SM, Siavashi V, Sahlabadi M, Hajinasrollah M, Zamani-Ahmadmahmudi M. Macrophage polarization by MSC-derived CXCL12 determines tumor growth. Cell Mol Biol Lett. 2021;26(1):1–15. doi: 10.1186/s11658-021-00273-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tarique AA, Logan J, Thomas E, Holt PG, Sly PD, Fantino E. Phenotypic, functional, and plasticity features of classical and alternatively activated human macrophages. Am J Respir Cell Mol Biol. 2015;53(5):676–688. doi: 10.1165/rcmb.2015-0012OC. [DOI] [PubMed] [Google Scholar]
- 88.Xu W, Zhao X, Daha MR, van Kooten C. Reversible differentiation of pro-and anti-inflammatory macrophages. Mol Immunol. 2013;53(3):179–186. doi: 10.1016/j.molimm.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 89.Korniluk A, Koper O, Kemona H, Dymicka-Piekarska V. From inflammation to cancer. Irish J Med Sci. 2017;186(1):57–62. doi: 10.1007/s11845-016-1464-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mostafavi S, Zalpoor H, Hassan ZM. The promising therapeutic effects of metformin on metabolic reprogramming of cancer-associated fibroblasts in solid tumors. Cell Mol Biol Lett. 2022;27(1):58. doi: 10.1186/s11658-022-00356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chimenti I, Sattler S, Del Monte-Nieto G, Forte E. Editorial: fibrosis and inflammation in tissue pathophysiology. Front Physiol. 2021;12:830683. doi: 10.3389/fphys.2021.830683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2018;9(6):7204–7218. doi: 10.18632/oncotarget.23208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rubartelli A, Lotze MT, Latz E, Manfredi A. Mechanisms of sterile inflammation. Front Immunol. 2013;4:398. doi: 10.3389/fimmu.2013.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zindel J, Kubes P. DAMPs, PAMPs, and LAMPs in immunity and sterile inflammation. Annu Rev Pathol. 2020;15(1):493–518. doi: 10.1146/annurev-pathmechdis-012419-032847. [DOI] [PubMed] [Google Scholar]
- 95.Cooke JP. Inflammation and its role in regeneration and repair. Circ Res. 2019;124(8):1166–1168. doi: 10.1161/CIRCRESAHA.118.314669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mack M. Inflammation and fibrosis. Matrix Biol. 2018;68–69:106–121. doi: 10.1016/j.matbio.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 97.Li C, Xu MM, Wang K, Adler AJ, Vella AT, Zhou B. Macrophage polarization and meta-inflammation. Transl Res. 2018;191:29–44. doi: 10.1016/j.trsl.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Parisi L, Gini E, Baci D, Tremolati M, Fanuli M, Bassani B, et al. Macrophage polarization in chronic inflammatory diseases: killers or builders? J Immunol Res. 2018;2018:8917804. doi: 10.1155/2018/8917804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lafuse WP, Wozniak DJ, Rajaram MVS. Role of cardiac macrophages on cardiac inflammation, fibrosis and tissue repair. Cells. 2021;10(1):51. doi: 10.3390/cells10010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lee H, Fessler MB, Qu P, Heymann J, Kopp JB. Macrophage polarization in innate immune responses contributing to pathogenesis of chronic kidney disease. BMC Nephrol. 2020;21(1):270. doi: 10.1186/s12882-020-01921-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Liu X, Chu H, Ji Y, Bosnjak Z, Ao H, Li T. Which BMI for diabetes patients is better? from the view of the adipose tissue macrophage-derived exosome. Diabetes Metab Syndr Obes. 2022;15:141–153. doi: 10.2147/DMSO.S345890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang J, Liu Y, Yin W, Hu X. Adipose-derived stromal cells in regulation of hematopoiesis. Cell Mol Biol Lett. 2020;25(1):16. doi: 10.1186/s11658-020-00209-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moreira Lopes TC, Mosser DM, Gonçalves R. Macrophage polarization in intestinal inflammation and gut homeostasis. Inflamm Res. 2020;69(12):1163–1172. doi: 10.1007/s00011-020-01398-y. [DOI] [PubMed] [Google Scholar]
- 104.Mouton AJ, Li X, Hall ME, Hall JE. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation. Circ Res. 2020;126(6):789–806. doi: 10.1161/CIRCRESAHA.119.312321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Liu W, Yu M, Chen F, Wang L, Ye C, Chen Q, et al. A novel delivery nanobiotechnology: engineered miR-181b exosomes improved osteointegration by regulating macrophage polarization. J Nanobiotechnology. 2021;19(1):269. doi: 10.1186/s12951-021-01015-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tai Y-L, Chen K-C, Hsieh J-T, Shen T-L. Exosomes in cancer development and clinical applications. Cancer Sci. 2018;109(8):2364–2374. doi: 10.1111/cas.13697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Letafati A, Najafi S, Mottahedi M, Karimzadeh M, Shahini A, Garousi S, et al. MicroRNA let-7 and viral infections: focus on mechanisms of action. Cell Mol Biol Lett. 2022;27(1):14. doi: 10.1186/s11658-022-00317-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.He X-Y, Yu H-M, Lin S, Li Y-Z. Advances in the application of mesenchymal stem cells, exosomes, biomimetic materials, and 3D printing in osteoporosis treatment. Cell Mol Biol Lett. 2021;26(1):47. doi: 10.1186/s11658-021-00291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim H, Wang SY, Kwak G, Yang Y, Kwon IC, Kim SH. Exosome-guided phenotypic switch of M1 to M2 macrophages for cutaneous wound healing. Adv Sci (Weinh) 2019;6(20):1900513. doi: 10.1002/advs.201900513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang F, Guo J, Zhang Z, Qian Y, Wang G, Duan M, et al. Mesenchymal stem cell-derived exosome: a tumor regulator and carrier for targeted tumor therapy. Cancer Lett. 2022;526:29–40. doi: 10.1016/j.canlet.2021.11.015. [DOI] [PubMed] [Google Scholar]
- 111.Liang W, Chen X, Zhang S, Fang J, Chen M, Xu Y, et al. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol Biol Lett. 2021;26(1):3. doi: 10.1186/s11658-020-00246-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu H, Liang Z, Wang F, Zhou C, Zheng X, Hu T, et al. Exosomes from mesenchymal stromal cells reduce murine colonic inflammation via a macrophage-dependent mechanism. JCI Insight. 2019;4:24. doi: 10.1172/jci.insight.131273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bischoff JP, Schulz A, Morrison H. The role of exosomes in intercellular and inter-organ communication of the peripheral nervous system. FEBS Lett. 2022;8:56. doi: 10.1002/1873-3468.14274. [DOI] [PubMed] [Google Scholar]
- 114.Xu R, Zhang F, Chai R, Zhou W, Hu M, Liu B, et al. Exosomes derived from pro-inflammatory bone marrow-derived mesenchymal stem cells reduce inflammation and myocardial injury via mediating macrophage polarization. J Cell Mol Med. 2019;23(11):7617–7631. doi: 10.1111/jcmm.14635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Li Q, Yu P, Wang W, Zhang P, Yang H, Li S, et al. Gene expression profiles of various cytokines in mesenchymal stem cells derived from umbilical cord tissue and bone marrow following infection with human cytomegalovirus. Cell Mol Biol Lett. 2014;19(1):140–157. doi: 10.2478/s11658-014-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ning H, Chen H, Deng J, Xiao C, Xu M, Shan L, et al. Exosomes secreted by FNDC5-BMMSCs protect myocardial infarction by anti-inflammation and macrophage polarization via NF-κB signaling pathway and Nrf2/HO-1 axis. Stem Cell Res Ther. 2021;12(1):519. doi: 10.1186/s13287-021-02591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ghashghaeinia M, Toulany M, Saki M, Rodemann HP, Mrowietz U, Lang F, et al. Roles of the NFκB and glutathione pathways in mature human erythrocytes. Cell Mol Biol Lett. 2012;17(1):11–20. doi: 10.2478/s11658-011-0032-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shi Y, Kang X, Wang Y, Bian X, He G, Zhou M, et al. Exosomes derived from bone marrow stromal cells (BMSCs) enhance tendon–bone healing by regulating macrophage polarization. Med Sci Monit. 2020;26:e923328. doi: 10.12659/MSM.923328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhao H, Shang Q, Pan Z, Bai Y, Li Z, Zhang H, et al. Exosomes from adipose-derived stem cells attenuate adipose inflammation and obesity through polarizing m2 macrophages and beiging in white adipose tissue. Diabetes. 2018;67(2):235–247. doi: 10.2337/db17-0356. [DOI] [PubMed] [Google Scholar]
- 120.Deng S, Zhou X, Ge Z, Song Y, Wang H, Liu X, et al. Exosomes from adipose-derived mesenchymal stem cells ameliorate cardiac damage after myocardial infarction by activating S1P/SK1/S1PR1 signaling and promoting macrophage M2 polarization. Int J Biochem Cell Biol. 2019;114:105564. doi: 10.1016/j.biocel.2019.105564. [DOI] [PubMed] [Google Scholar]
- 121.Dong B, Wang C, Zhang J, Zhang J, Gu Y, Guo X, et al. Exosomes from human umbilical cord mesenchymal stem cells attenuate the inflammation of severe steroid-resistant asthma by reshaping macrophage polarization. Stem Cell Res Ther. 2021;12(1):204. doi: 10.1186/s13287-021-02244-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cai M, Shi Y, Zheng T, Hu S, Du K, Ren A, et al. Mammary epithelial cell derived exosomal MiR-221 mediates M1 macrophage polarization via SOCS1/STATs to promote inflammatory response. Int Immunopharmacol. 2020;83:106493. doi: 10.1016/j.intimp.2020.106493. [DOI] [PubMed] [Google Scholar]
- 123.Shen D, He Z. Mesenchymal stem cell-derived exosomes regulate the polarization and inflammatory response of macrophages via miR-21-5p to promote repair after myocardial reperfusion injury. Ann Transl Med. 2021;9(16):1323. doi: 10.21037/atm-21-3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ding C, Zheng J, Wang B, Li Y, Xiang H, Dou M, et al. Exosomal MicroRNA-374b-5p from tubular epithelial cells promoted m1 macrophages activation and worsened renal ischemia/reperfusion injury. Front Cell Dev Biol. 2020;8:587693. doi: 10.3389/fcell.2020.587693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao S, Wu W, Liao J, Zhang X, Shen M, Li X, et al. Molecular mechanisms underlying the renal protective effects of coenzyme Q10 in acute kidney injury. Cell Mol Biol Lett. 2022;27(1):57. doi: 10.1186/s11658-022-00361-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jiao Y, Zhang T, Zhang C, Ji H, Tong X, Xia R, et al. Exosomal miR-30d-5p of neutrophils induces M1 macrophage polarization and primes macrophage pyroptosis in sepsis-related acute lung injury. Crit Care. 2021;25(1):356. doi: 10.1186/s13054-021-03775-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Heo J, Kang H. Exosome-dosis. Int J Mol Sci. 2022;23(2):1002. doi: 10.3390/ijms23021002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Li J, Xue H, Li T, Chu X, Xin D, Xiong Y, et al. Exosomes derived from mesenchymal stem cells attenuate the progression of atherosclerosis in ApoE−/-mice via miR-let7 mediated infiltration and polarization of M2 macrophage. Biochem Biophys Res Commun. 2019;510(4):565–572. doi: 10.1016/j.bbrc.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 129.Ma J, Chen L, Zhu X, Li Q, Hu L, Li H. Mesenchymal stem cell-derived exosomal miR-21a-5p promotes M2 macrophage polarization and reduces macrophage infiltration to attenuate atherosclerosis. Acta Biochim Biophys Sin. 2021;53(9):1227–1236. doi: 10.1093/abbs/gmab102. [DOI] [PubMed] [Google Scholar]
- 130.Bouchareychas L, Duong P, Covarrubias S, Alsop E, Phu TA, Chung A, et al. Macrophage exosomes resolve atherosclerosis by regulating hematopoiesis and inflammation via MicroRNA cargo. Cell Rep. 2020;32(2):107881. doi: 10.1016/j.celrep.2020.107881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu G, Zhang J, Zhao Q, Zhuang W, Ding J, Zhang C, et al. Molecularly engineered macrophage-derived exosomes with inflammation tropism and intrinsic heme biosynthesis for atherosclerosis treatment. Angew Chem. 2020;132(10):4097–4103. doi: 10.1002/ange.201913700. [DOI] [PubMed] [Google Scholar]
- 132.Baig MS, Roy A, Rajpoot S, Liu D, Savai R, Banerjee S, et al. Tumor-derived exosomes in the regulation of macrophage polarization. Inflamm Res. 2020;69(5):435–451. doi: 10.1007/s00011-020-01318-0. [DOI] [PubMed] [Google Scholar]
- 133.Bardi GT, Smith MA, Hood JL. Melanoma exosomes promote mixed M1 and M2 macrophage polarization. Cytokine. 2018;105:63–72. doi: 10.1016/j.cyto.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pritchard A, Tousif S, Wang Y, Hough K, Khan S, Strenkowski J, et al. Lung tumor cell-derived exosomes promote M2 macrophage polarization. Cells. 2020;9:5. doi: 10.3390/cells9051303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nahand JS, Vandchali NR, Darabi H, Doroudian M, Banafshe HR, Moghoofei M, et al. Exosomal microRNAs: novel players in cervical cancer. Epigenomics. 2020;12(18):1651–1660. doi: 10.2217/epi-2020-0026. [DOI] [PubMed] [Google Scholar]
- 136.Chen WX, Wang DD, Zhu B, Zhu YZ, Zheng L, Feng ZQ, et al. Exosomal miR-222 from adriamycin-resistant MCF-7 breast cancer cells promote macrophages M2 polarization via PTEN/Akt to induce tumor progression. Aging (Albany NY) 2021;13(7):10415–10430. doi: 10.18632/aging.202802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Park JE, Dutta B, Tse SW, Gupta N, Tan CF, Low JK, et al. Hypoxia-induced tumor exosomes promote M2-like macrophage polarization of infiltrating myeloid cells and microRNA-mediated metabolic shift. Oncogene. 2019;38(26):5158–5173. doi: 10.1038/s41388-019-0782-x. [DOI] [PubMed] [Google Scholar]
- 138.Li X, Lei Y, Wu M, Li N. Regulation of macrophage activation and polarization by HCC-derived exosomal lncRNA TUC339. Int J Mol Sci. 2018;19(10):2958. doi: 10.3390/ijms19102958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Li J, Zhang G, Liu C-G, Xiang X, Le MT, Sethi G, et al. The potential role of exosomal circRNAs in the tumor microenvironment: insights into cancer diagnosis and therapy. Theranostics. 2022;12(1):87. doi: 10.7150/thno.64096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang P, Wang H, Huang Q, Peng C, Yao L, Chen H, et al. Exosomes from M1-polarized macrophages enhance paclitaxel antitumor activity by activating macrophages-mediated inflammation. Theranostics. 2019;9(6):1714–1727. doi: 10.7150/thno.30716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Vannini I, Fanini F, Fabbri M. Emerging roles of microRNAs in cancer. Curr Opin Genet Dev. 2018;48:128–133. doi: 10.1016/j.gde.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.