Abstract
How maintenance dialysis modality, dialysis setting, and residence in a nursing facility have jointly associated with coronavirus disease 2019 (COVID-19)-related outcomes in the United States is relevant to future viral outbreaks. Using Medicare claims, we determined the incidence of COVID-19–related infection, hospitalization, and death between March 15, 2020 and June 5, 2021. The exposure was one of five combinations of dialysis modality and care setting: in-facility hemodialysis without a recent history of skilled nursing facility care, in-facility hemodialysis with a recent history of skilled nursing facility care, hemodialysis in a skilled nursing facility, home hemodialysis, and (home) peritoneal dialysis. Patient-weeks were pooled to estimate the adjusted associations of event incidence with each dialysis modality/setting during four intervals in 2020–2021. Relative to in-facility hemodialysis without a recent history of skilled nursing facility care, home dialysis was associated with 36%–60% lower odds of all events during weeks 12–23 of 2020; 24%–37% lower odds of all events during weeks 24–37 of 2020; 20%–33% lower odds of infection and hospitalization during the winter of 2020–2021; and similar odds of all events thereafter. In contrast, exposure to skilled nursing facilities was associated with 570%–1140% higher odds of all events during spring of 2020, although excess risk attenuated as the pandemic transpired, especially among patients who received hemodialysis in skilled nursing facilities. In conclusion, home dialysis was associated with lower risks of COVID-19 diagnosis, hospitalization, and death until vaccines were available, whereas care in skilled nursing facilities was associated with higher risks.
Keywords: United States Renal Data System, COVID-19, ESRD
Introduction
The effect of the coronavirus disease 2019 (COVID-19) pandemic on people undergoing maintenance dialysis in the United States has been enormous; excess mortality during the pandemic led to an unprecedented shrinkage of the dialysis population (1–4). More than 85% of patients on dialysis undergo in-facility hemodialysis (HD) (4). The nature of this modality confers inherent risks of viral transmission, as patients are exposed to nursing staff and other patients three times per week. In addition, many patients use public or medical transportation (5). Some patients reside in skilled nursing facilities (SNFs) and may carry viral infections from SNFs to dialysis centers, thereby indirectly exposing patients who live in private residences to viral outbreaks in SNFs (6).
In principle, dialysis in the home setting mitigates these concerns. Data from Ontario (Canada) and a US dialysis provider operating >200 facilities indicate that home dialysis was associated with lower risk of COVID-19 diagnosis and its sequelae than in-facility HD during much of 2020 and that exposure to SNFs was associated with higher risk (7,8). However, there are no multiprovider studies assessing the associations of dialysis modality, dialysis setting, and SNF residency with COVID-19 outcomes in the United States. We analyzed Medicare fee-for-service claims to assess the associations of dialysis modality and setting with risks of COVID-19 diagnosis, COVID-19 hospitalization, and COVID-19 death (Figure 1).
Figure 1.
Overview of the study. COVID-19, coronavirus disease 2019; HD, hemodialysis; SNF, skilled nursing facility; USRDS, United States Renal Data System.
Materials and Methods
We analyzed quarterly extracts of Medicare Parts A and B claims in 2020 and the first half of 2021. The Centers for Medicare & Medicaid Services (CMS) extracted all such claims among patients with documented kidney failure, according to the CMS End Stage Renal Disease Quality Reporting System. We also analyzed submissions of forms CMS-2728 (“ESRD Medical Evidence Report”) and CMS-2746 (“ESRD Death Notification”) in the CMS End Stage Renal Disease Quality Reporting System as of February 2022.
We analyzed incidence of COVID-19 diagnosis, COVID-19 hospitalization, and COVID-19 death between epidemiologic week 12 of 2020 and week 22 of 2021 (March 15, 2020 to June 5, 2021); each week begins on Sunday and ends on Saturday (1). For each week, we identified patients who underwent one or more outpatient dialysis treatments during the 7 days (for analyses of COVID-19 diagnosis and hospitalization) or 28 days (for analyses of death) that preceded the first day of the week. Outpatient dialysis was ascertained from claims with qualifying revenue centers, Healthcare Common Procedure Coding System codes, and condition codes indicating HD or peritoneal dialysis (PD) in a dialysis facility, home, or SNF (Supplemental Table 1). For each patient-week, we ascertained age and kidney failure duration at the beginning of the week; sex and race and ethnicity as recorded in the Medicare Enrollment Database; state/territory of the current dialysis facility; any hospitalization during the preceding 28 days; and diabetes mellitus and heart failure ascertained from form CMS-2728. The 28-day period regarding hospitalization was specified to address confounding due to potential exposure to COVID-19 in the hospital. For analysis, we retained Medicare fee-for-service beneficiaries with age ≥18 years, nonmissing sex, and dialysis treatment in the 50 states, the District of Columbia, and Puerto Rico.
The exposure was dialysis modality and setting summarized in five categories: in-facility HD without recent history of SNF care, in-facility HD with recent history of SNF care, HD in an SNF, home HD, and home PD. Recent history of SNF care was defined by physician claims with qualifying place of service or Current Procedural Terminology codes indicating nursing facility care during the 13 weeks that preceded the first day of the epidemiologic week (Supplemental Table 2). HD in an SNF was defined by multiple criteria involving condition codes and characteristics of the current dialysis facility (Supplemental Tables 1 and 3). From one week to the next, patients could change exposure categories.
In each epidemiologic week, we measured the incidence of COVID-19 diagnosis, COVID-19 hospitalization, and COVID-19 death. A COVID-19 diagnosis was established by a physician claim with qualifying place of service codes (Supplemental Table 4) and International Classification of Diseases, 10th Edition, Clinical Modification diagnosis codes B97.29 (other coronavirus as the cause of diseases classified elsewhere) or U07.1 (COVID-19, virus identified). A COVID-19 hospitalization was defined by admission to a short-term hospital or critical access hospital and discharge diagnosis codes B97.29 or U07.1. Patients could be recurrently admitted to the hospital with COVID-19, but a hospitalization spanning multiple weeks contributed an event only to the first week. COVID-19 death was defined by submission of the ESRD Death Notification with primary cause of death code 105 (COVID-19, virus identified), 106 (COVID-19, virus not identified), or 98 (other cause of death) in tandem with a text string including “COVID.”
We summarized demographic characteristics in epidemiologic week 12 of 2020. For each event, we calculated crude weekly incidence in each category of dialysis modality/setting and used loess regression to estimate smoothed trends. We pooled all patient-weeks and used a generalized estimating equation with a binomial distributed response to estimate adjusted associations of event incidence with dialysis modality setting during four “periods”: from epidemiologic week 12 to week 23 of 2020 (March 15 to June 6), from week 24 to week 37 of 2020 (June 7 to September 12), from week 38 of 2020 to week 8 of 2021 (September 13 to February 27), and from week 9 to week 22 of 2021 (February 28 to June 5). For the analysis of COVID-19 diagnosis, patients were followed only until the first week with a diagnosis. To assess regional variability, we repeated analyses of COVID-19 diagnosis and hospitalization incidence in the ten states with the largest numbers of patients; because of limited sample sizes per state, we pooled the SNF-related and home dialysis–related exposure categories.
Data were accessed under the auspices of a data use agreement with CMS, and research was approved by the Advarra Institutional Review Board. All analyses were executed in SAS, version 9.4 (Cary, NC).
Results
The cohort included 381,091 patients with ≥1 follow-up week. In 2020, mean weekly sample sizes were 225,794 for in-facility HD without a recent history of SNF care; 14,929 for in-facility HD with a recent history of SNF care; 2708 for HD in an SNF; 6058 for home HD; and 28,530 for home PD. Compared with patients undergoing in-facility HD without a recent history of SNF care, patients with any exposure to an SNF were older, more likely to be women, and in poorer health, whereas patients on home dialysis were younger, more likely White, and less likely to have diabetes and heart failure (Table 1).
Table 1.
Patient characteristics by dialysis modality and setting in epidemiologic week 12 of 2020 (beginning March 15)
| Characteristic | In-Facility Hemodialysisa | Hemodialysis and Skilled Nursing Facility Care | Home Dialysis | ||
|---|---|---|---|---|---|
| In-Facility Hemodialysisb | Hemodialysis in a Skilled Nursing Facility Care | Home Hemodialysis | Home Peritoneal Dialysis | ||
| Sample size, N | 230,223 | 19,217 | 2902 | 5589 | 28,500 |
| Age, yr | |||||
| Mean (SD) | 63 (14) | 70 (11) | 69 (13) | 56 (14) | 61 (15) |
| Median (IQR) | 65 (54–73) | 70 (63–78) | 70 (62–78) | 56 (46–66) | 63 (51–72) |
| Sex, N (%) | |||||
| Women | 98,502 (43) | 9666 (50) | 1362 (47) | 2142 (38) | 12,849 (45) |
| Men | 131,721 (57) | 9551 (50) | 1540 (53) | 3447 (62) | 15,651 (55) |
| Race and ethnicity, N (%) | |||||
| White | 98,436 (43) | 9999 (52) | 977 (34) | 3114 (56) | 15,901 (56) |
| Black | 86,754 (38) | 6971 (36) | 1546 (53) | 1769 (32) | 6957 (24) |
| Hispanic | 20,941 (9) | 907 (5) | 151 (5) | 271 (5) | 2152 (8) |
| Asian | 9400 (4) | 517 (3) | 66 (2) | 160 (3) | 1385 (5) |
| Other | 4424 (2) | 243 (1) | 4 (0.1) | 44 (1) | 392 (1) |
| Unknown | 10,268 (4) | 580 (3) | 158 (5) | 231 (4) | 1713 (6) |
| Kidney failure duration, yr | |||||
| Mean (SD) | 5.6 (5.2) | 4.9 (4.4) | 5.0 (4.5) | 7.4 (6.7) | 3.8 (4.2) |
| Median (IQR) | 4.1 (2.0–7.4) | 3.9 (1.7–6.8) | 4.0 (1.8–6.7) | 5.0 (2.9–9.8) | 2.6 (1.2–4.5) |
| Diabetes mellitus, N (%) | 127,878 (56) | 12,870 (67) | 1684 (58) | 2401 (43) | 13,752 (48) |
| Heart failure, N (%) | 54,183 (24) | 6138 (32) | 777 (27) | 842 (15) | 4449 (16) |
| Recent hospitalization,c N (%) | 20,910 (9) | 5565 (29) | 698 (24) | 448 (8) | 2187 (8) |
IQR, interquartile range.
In-facility hemodialysis without a recent history of skilled nursing facility care.
In-facility hemodialysis with a recent history of skilled nursing facility care.
During the 4 weeks that preceded the first day of the epidemiologic week.
There were 52,541 COVID-19 diagnoses (crude weekly incidence, 0.33%), 43,205 COVID-19 hospitalizations (0.26%), and 4936 COVID-19 deaths (0.03%). The largest weekly counts of COVID-19 diagnoses and hospitalizations occurred in December 2020 and January 2021. Smoothed trends in crude weekly incidence of COVID-19 diagnosis, hospitalization, and death, stratified by dialysis modality and setting, are displayed in Figures 2–4, respectively, and period-specific incidence estimates are displayed in Supplemental Table 4. Relative to in-facility HD without recent history of SNF care, both home dialysis modalities exhibited consistently lower incidence until the spring of 2021. Conversely, exposure to the SNF was associated with higher incidence. Death patterns were congruous, although home dialysis was associated with only a modest difference in absolute risk.
Figure 2.
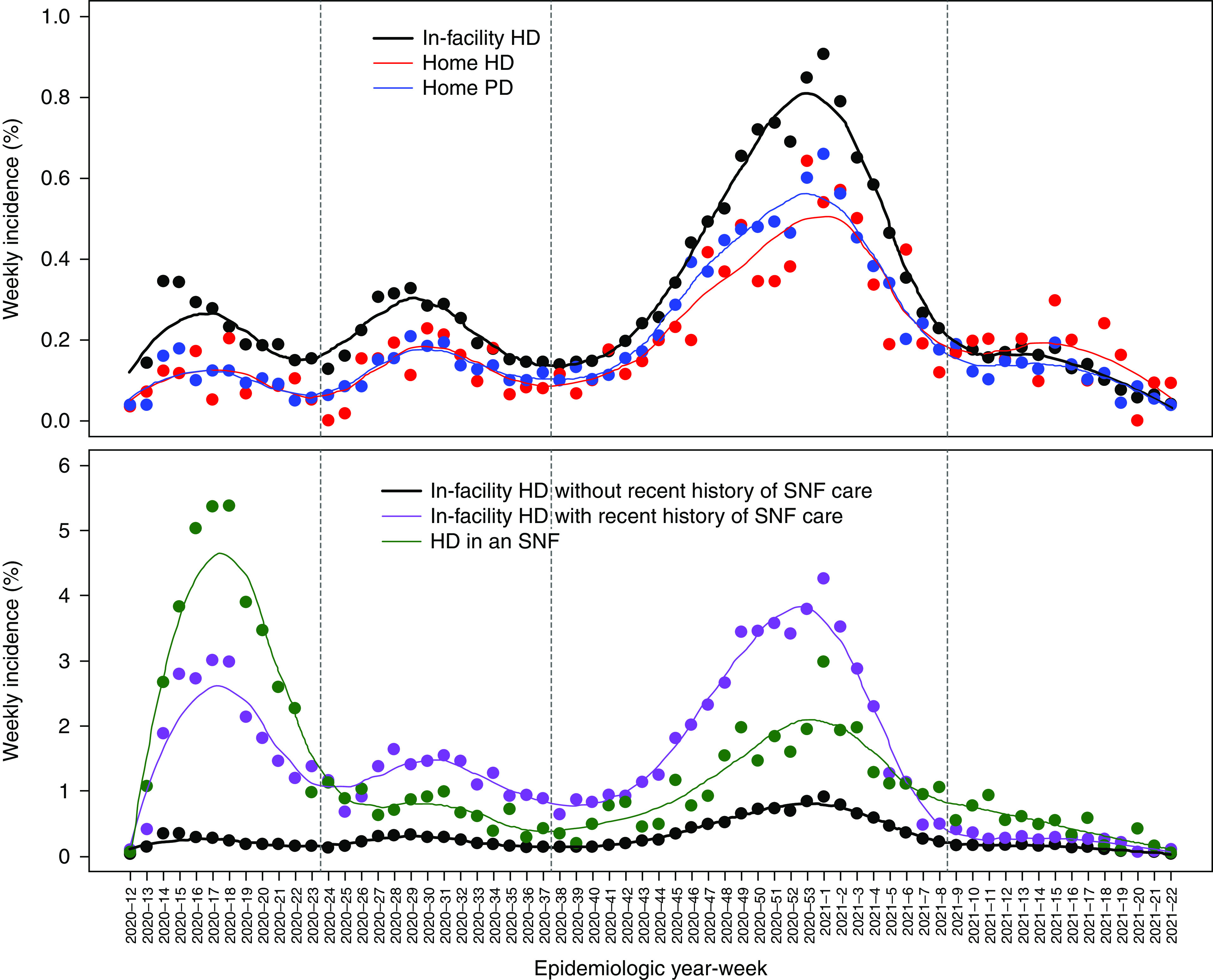
Weekly incidence of COVID-19 diagnosis from epidemiologic week 12 of 2020 to week 22 of 2021 (March 15, 2020 to June 5, 2021). Patients undergoing in-facility HD without a recent history of SNF care are shown in black in both panels, patients on home HD are shown in red in the upper panel, patients performing home peritoneal dialysis (PD) are shown in blue in the upper panel, patients receiving in-facility HD with a recent history of SNF care are shown in purple in the lower panel, and patients receiving HD in an SNF are shown in green in the lower panel. Vertical lines separate the four intervals specified in risk models.
Figure 4.
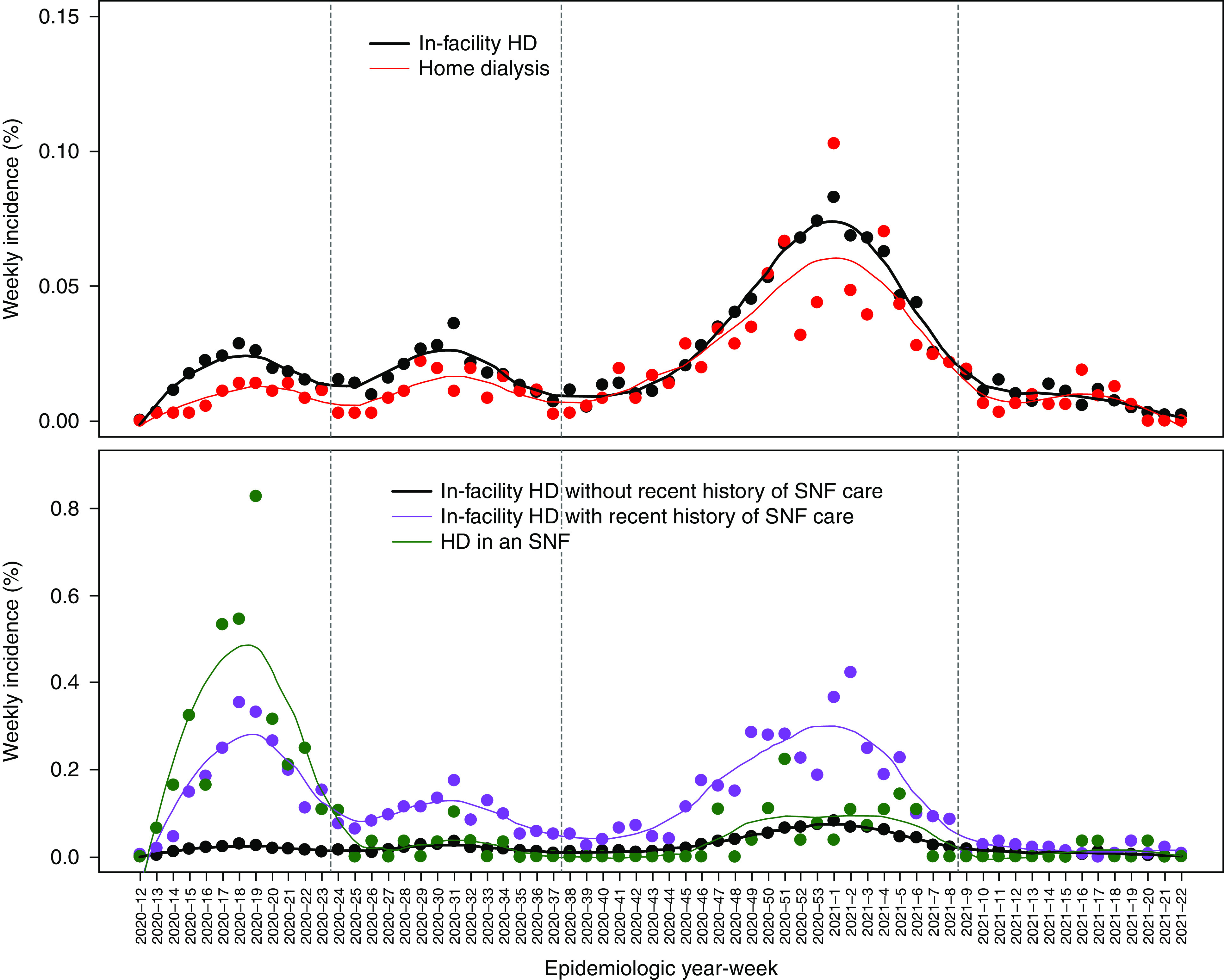
Weekly incidence of COVID-19 death among patients undergoing in-facility HD without a recent history of SNF care (both panels), home dialysis (upper panel), in-facility HD with a recent history of SNF care (lower panel), or HD in an SNF (lower panel) from epidemiologic week 12 of 2020 to week 22 of 2021 (March 15, 2020 to June 5, 2021). Vertical lines separate the four intervals specified in risk models.
Figure 3.
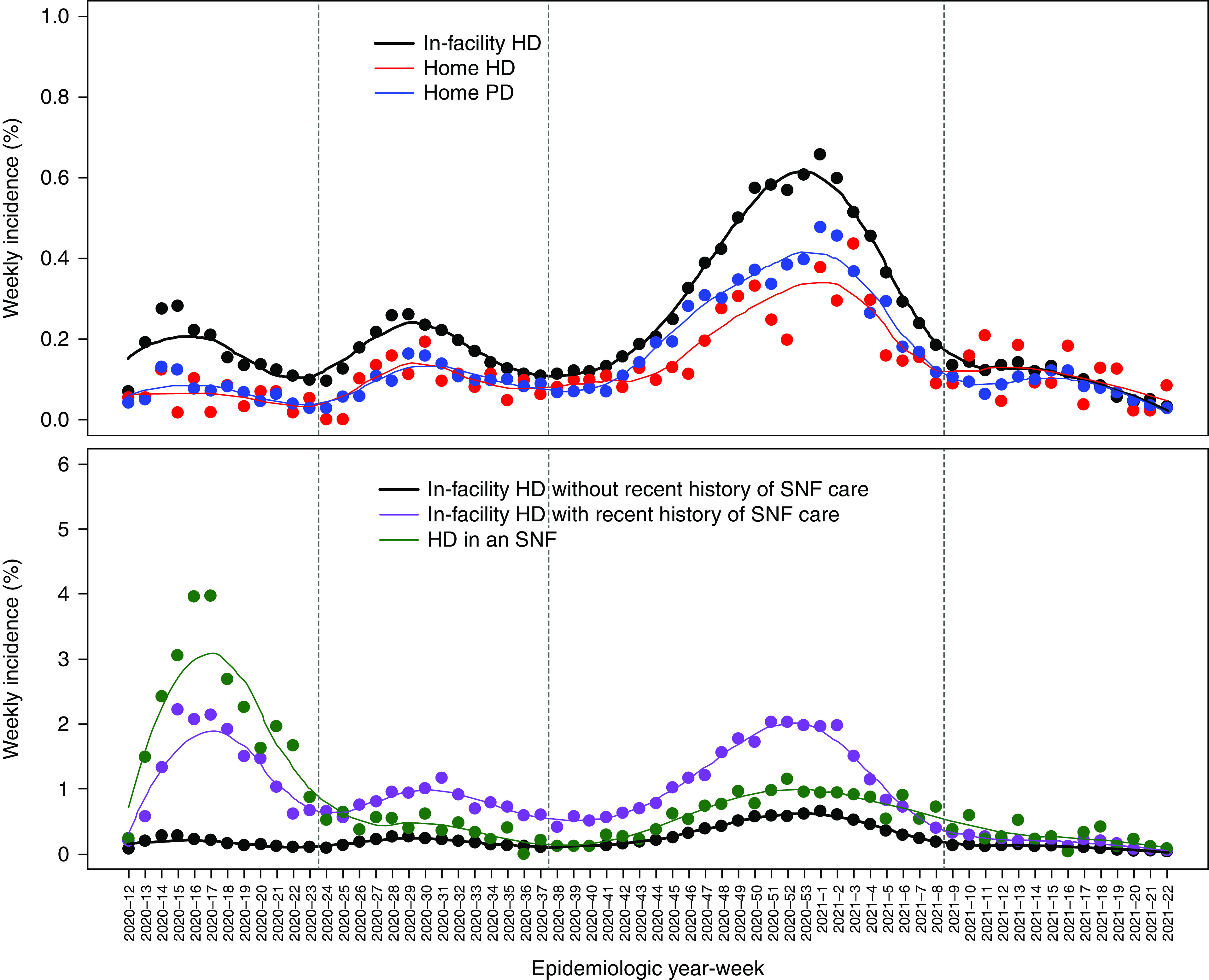
Weekly incidence of COVID-19 hospitalization among patients undergoing in-facility HD without a recent history of SNF care (both panels), home HD (upper panel), home PD (upper panel), in-facility HD with a recent history of SNF care (lower panel), or HD in an SNF (lower panel) from epidemiologic week 12 of 2020 to week 22 of 2021 (March 15, 2020 to June 5, 2021). Vertical lines separate the four intervals specified in risk models.
Adjusted odds ratios of COVID-19 diagnosis, hospitalization, and death are displayed in Table 2. Relative to in-facility HD without recent history of SNF care, home dialysis was associated with 36%–60% lower odds of all events during weeks 12–23 of 2020 and with 24%–37% lower odds of all events during weeks 24–37 of 2020. During the winter of 2020–2021, home dialysis was associated with 20%–33% lower odds of infection and hospitalization, but it was associated with similar odds of COVID-19 death as in-facility HD without recent history of SNF care. During the spring of 2021, in-facility HD without recent history of SNF care and home dialysis exhibited similar odds of all events.
Table 2.
Adjusted odds ratios of coronavirus disease 2019 diagnosis, coronavirus disease 2019 hospitalization, and coronavirus disease 2019 death from epidemiologic week 12 to week 23 of 2020 (March 15 to June 6), from week 24 of 2020 to week 37 of 2020 (June 7 to September 12), from week 38 of 2020 to week 8 of 2021 (September 13 to February 27), and from week 9 of 2021 to week 22 of 2021 (February 28 to June 5) among Medicare fee-for-service beneficiaries undergoing maintenance dialysis
| Week 12 of 2020 to Week 23 of 2020 | Week 24 of 2020 to Week 37 of 2020 | Week 38 of 2020 to Week 8 of 2021 | Week 9 of 2021 to Week 22 of 2021 | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted Odds Ratio | 95% Confidence Interval | Adjusted Odds Ratio | 95% Confidence Interval | Adjusted Odds Ratio | 95% Confidence Interval | Adjusted Odds Ratio | 95% Confidence Interval | |
| COVID-19 diagnosis | ||||||||
| In-facility HD without recent history of SNF care | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| In-facility HD with recent history of SNF care | 7.8 | 7.4 to 8.1 | 5.0 | 4.7 to 5.2 | 3.9 | 3.8 to 4.1 | 1.7 | 1.5 to 1.9 |
| HD in an SNF | 12.4 | 11.5 to 13.3 | 2.8 | 2.4 to 3.2 | 2.2 | 2.0 to 2.4 | 2.8 | 2.4 to 3.4 |
| Home HD | 0.52 | 0.41 to 0.66 | 0.63 | 0.52 to 0.76 | 0.74 | 0.67 to 0.81 | 1.4 | 1.1 to 1.7 |
| Home PD | 0.50 | 0.45 to 0.56 | 0.65 | 0.59 to 0.71 | 0.80 | 0.76 to 0.84 | 0.96 | 0.86 to 1.1 |
| COVID-19 hospitalization | ||||||||
| In-facility HD without recent history of SNF care | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| In-facility HD with recent history of SNF care | 5.9 | 5.6 to 6.3 | 3.5 | 3.3 to 3.7 | 2.4 | 2.3 to 2.5 | 1.4 | 1.2 to 1.6 |
| HD in an SNF | 9.5 | 8.8 to 10.4 | 1.7 | 1.4 to 2.0 | 1.3 | 1.2 to 1.5 | 1.9 | 1.5 to 2.3 |
| Home HD | 0.40 | 0.29 to 0.55 | 0.63 | 0.48 to 0.81 | 0.67 | 0.59 to 0.76 | 1.2 | 0.93 to 1.6 |
| Home PD | 0.47 | 0.40 to 0.54 | 0.64 | 0.57 to 0.72 | 0.80 | 0.76 to 0.85 | 0.92 | 0.81 to 1.1 |
| COVID-19 death | ||||||||
| In-facility HD without recent history of SNF care | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| In-facility HD with recent history of SNF care | 6.7 | 5.8 to 7.7 | 3.5 | 3.0 to 4.2 | 2.8 | 2.6 to 3.1 | 1.3 | 0.91 to 1.9 |
| HD in an SNF | 12.3 | 9.9 to 15.5 | 1.1 | 0.58 to 1.9 | 0.91 | 0.64 to 1.3 | 0.60 | 0.19 to 1.9 |
| Home dialysisa | 0.64 | 0.45 to 0.90 | 0.76 | 0.58 to 1.0 | 1.1 | 0.98 to 1.3 | 1.1 | 0.76 to 1.6 |
Adjustment factors were age, sex, race and ethnicity, state/territory of dialysis treatment, duration of kidney failure, diabetes mellitus, heart failure, and recent hospitalization. COVID-19, coronavirus disease 2019; HD, hemodialysis; SNF, skilled nursing facility; PD, peritoneal dialysis.
Home HD and home PD are pooled due to the small number of COVID-19 deaths among patients on home HD.
During weeks 12–23 of 2020, in-facility HD with a recent history of SNF care was associated with 5.9- to 7.8-times higher odds of events, whereas HD in an SNF was associated with 9.5- to 12.4-times higher odds of events relative to in-facility HD without a recent history of SNF care. During weeks 24–37 of 2020 and again during the winter of 2020–2021, all associations attenuated. In contrast to the first period, odds of all events were 40%–70% lower among patients receiving HD in an SNF versus in-facility HD with recent history of SNF care. During the spring of 2021, in-facility HD with a recent history of SNF care exhibited modestly higher odds of infection and hospitalization relative to in-facility HD without recent history of SNF care and similar odds of COVID-19 death.
The evolution of associations of home dialysis and SNF exposure with odds of COVID-19 events was qualitatively similar among ten diverse states (Supplemental Tables 5 and 6).
Discussion
In this study of Medicare beneficiaries undergoing dialysis between March 2020 and February 2021, we observed that patients performing home dialysis exhibited markedly lower risks of COVID-19 diagnosis and COVID-19 hospitalization relative to patients on in-facility HD without direct exposure to an SNF. During the spring and summer of 2020 but not the winter of 2020–2021, patients on home dialysis also exhibited lower risk of COVID-19 death. In contrast, patients with any exposure to an SNF exhibited much higher risk of COVID-19–related morbidity and mortality than patients on in-facility HD without SNF exposure.
The COVID-19 pandemic has exposed numerous weaknesses in the public health and medical care systems in the United States. In-facility HD may be one of the more glaring examples. Amid shelter-in-place orders, vulnerable patients were required to congregate for hours at a time three times per week to undergo HD. Moreover, a majority population that lives in private residences mixed with a minority population that lives in SNFs, despite widespread outbreaks of COVID-19 in SNFs across the country (9).
Several studies have already investigated whether home dialysis offered protection from COVID-19. Weinhandl et al. (1) reported that adjusted relative rates of COVID-19 hospitalization during weeks 13–27 of 2020 were approximately 65% lower among patients undergoing PD versus HD. In facilities operated by Dialysis Clinic, Inc. between February 22 and September 30, 2020, the incidence of COVID-19 diagnosis was 6.5 cases per 1000 patient-months with home dialysis but 14.0 cases per 1000 patient-months with in-facility HD (8). However, during the fourth quarter of 2020, the incidence of COVID-19 diagnosis was only 10% lower with home dialysis versus in-facility HD. Among patients undergoing dialysis in Ontario between March 12 and August 20, 2020, adjusted odds ratios of COVID-19 diagnosis were 0.39 with home dialysis versus in-facility HD and 7.7 with long-term care residency versus not (7). In another study from Ontario, with follow-up through November 20, 2020, the adjusted rate ratio of COVID-19 hospitalization was 0.57 with home dialysis versus in-facility HD (10). We found that home HD and PD exhibited identical outcomes, despite the fact that patients on home HD could draw blood samples at home; single-patient rooms in many home therapy units may have afforded protection from COVID-19 transmission during periodic clinic visits.
This study also showed that patients on dialysis who were exposed to SNFs exhibited sharply higher risks of COVID-19–related morbidity and mortality. The number of patients on dialysis who reside in SNFs is not clear. The United States Renal Data System reports that 6% of all patients with incident kidney failure in 2017–2019 resided in a nursing home, with a higher prevalence among patients aged ≥70 years (4). Aggregated data from Dialysis Facility Reports indicate that nearly 15% of all patients on dialysis resided in an SNF at some point during 2019 (11). It is possible that patients carried infection from SNFs to dialysis facilities, considering the frequency of COVID-19 outbreaks in SNFs during 2020—especially during the spring. It is also possible that the higher risk of COVID-19 diagnosis among patients with SNF exposure was driven by more frequent testing for COVID-19 in nursing homes. However, the correspondingly higher risks of COVID-19 hospitalization and death would seem to indicate that the higher risk was not merely attributable to detection of asymptomatic cases.
One way to limit the spread of viral infections as well as limit exposure to medical transportation is to render on-site dialysis in SNFs. Although HD in an SNF was associated with the highest risks of COVID-19 diagnosis and hospitalization during spring of 2020, the therapy was associated with significantly lower risks than in-facility HD with a recent history of SNF care from June 2020 to February 2021. This pattern of rapid reduction in relative risk may suggest that infection control practices within SNFs or by providers of dialysis within SNFs improved after spring of 2020. At the same time, risks of COVID-19–related events being highest among patients receiving in-facility HD with recent SNF exposure after the spring of 2020 may indicate that risks conferred by SNF exposure and medical transportation both contributed substantially to the overall risk during the second half of 2020. Rates of COVID-19 events were much lower in the spring of 2021, and associations of dialysis modality with risk of events were less remarkable, likely reflecting increasing vaccine coverage in both SNFs and dialysis facilities, especially after the federal government began to allocate vaccine supply to dialysis providers in March 2021.
This study has several limitations. First, nonrandomized cohort studies may be subject to unmeasured confounding. Patients on home dialysis are younger and carry less comorbidity than patients on in-facility HD. We adjusted for age, kidney failure duration, diabetes, and heart failure, but other differences, including differences in health-seeking behaviors and frailty, likely persisted. Furthermore, adjustment for diabetes and heart failure was incomplete due to misclassification error on form CMS-2728 (12,13). Some of the attenuation in associations during 2020 may reflect a “depletion-of-susceptibles” bias. Nonetheless, whether these issues influence the risk of COVID-19 diagnosis is not obvious. Second, Medicare claims lack the certainty of laboratory confirmation of COVID-19, although the use of diagnosis code U07.1 should be supported by documentation of a positive test. We extracted COVID-19 diagnosis and hospitalization from mutually exclusive sets of claims and reported similar associations. Third, we could not assess the patient-level association of COVID-19 vaccination with events due to incomplete recording of vaccination in claims (14). Finally, the cohort was restricted to Medicare beneficiaries. Among patients with private insurance, in whom employment is more likely, the dialysis setting may not be associated with COVID-19 events.
The COVID-19 pandemic imparted unprecedented adversity upon patients undergoing dialysis. However, this study, and others like it, suggest that risks of COVID-19– related morbidity and mortality may be partly mitigated by dialysis modalities and settings other than in-facility HD. As the United States continues to grow home dialysis, dialysis providers and nephrologists may consider presenting the possibility that dialyzing at home offers protection from viral illnesses, including not only COVID-19 but also seasonal influenza (15). Additionally, the nephrology community must focus more on addressing outcomes among patients on dialysis who reside in SNFs, as well as preventing the spread of communicable disease between nursing facilities and dialysis centers.
Disclosures
D.T. Gilbertson reports employment with the Chronic Disease Research Group; consultancy agreements with Amgen (providing general input in epidemiologic and biostatistical research); and research funding from Acadia, Amgen, AstraZeneca, DaVita, Genentech, Gilead, Health Resources and Services Administration, Merck, the National Institutes of Health, and OPKO Renal. K.L. Johansen reports employment with Hennepin Healthcare; reports consultancy agreements with Akebia; serves on the Akebia Advisory Board and as a member of the steering committee for the GlaxoSmithKline prolyl hydroxylase inhibitor clinical trials program; and serves as an associate editor of JASN. J. Liu reports employment with the Hennepin Healthcare Research Institute and research funding from Amgen Inc. and the GlaxoSmithKline group of companies. E.D. Weinhandl reports employment with Satellite Healthcare; reports consultancy agreements with Fresenius Medical Care North America, NxStage Medical, Outset Medical, and Quanta Dialysis Technologies; reports research funding from Dialyze Direct and Outset Medical; serves on the board of directors of Home Dialyzors United and on the board of directors of Medical Education Institute; and reports other interests or relationships with the University of Minnesota. J.B. Wetmore reports employment with Hennepin County Medical Center; ad hoc consulting for the BMS-Pfizer Alliance; research funding from Amgen, AstraZeneca, Bristol Myers Squibb/Pfizer, Genentech, GlaxoSmithKline, Merck, the National Institutes of Health (the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases), and OPKO Health; honoraria from Bristol Myers Squibb/Pfizer Alliance(for advisory board activities), Reata, and Vifor; and honoraria for academic continuing medical education from Healio and the Nephrology Self-Assessment Program.
Funding
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases grant 75N94019C00006.
Supplementary Material
Acknowledgments
The data reported here have been supplied by the United States Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Author Contributions
K.L. Johansen, E.D. Weinhandl, and J.B. Wetmore conceptualized the study; D.T. Gilbertson, K.L. Johansen, J. Liu, and J.B. Wetmore were responsible for investigation; E.D. Weinhandl was responsible for formal analysis; E.D. Weinhandl was responsible for methodology; D. T. Gilbertson, K.L. Johansen, and J.B. Wetmore were responsible for funding acquisition; E.D. Weinhandl wrote the original draft; and D.T. Gilbertson, K.L. Johansen, J. Liu, E.D. Weinhandl, and J.B. Wetmore reviewed and edited the manuscript.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03400322/-/DCSupplemental.
Supplemental Table 1. Qualifying condition codes, revenue centers, and Healthcare Common Procedure Coding System codes indicating hemodialysis or peritoneal dialysis in a dialysis facility, home, or skilled nursing facility.
Supplemental Table 2. Qualifying place of service or Current Procedural Terminology codes indicating nursing facility care.
Supplemental Table 3. Qualifying place of service codes on physician claims indicating COVID-19 diagnosis.
Supplemental Table 4. Unadjusted rates of COVID-19 diagnosis, COVID-19 hospitalization, and COVID-19 death from epidemiologic week 12 to week 23 of 2020 (March 15 to June 6), from week 24 of 2020 to week 37 of 2020 (June 7 to September 12), from week 38 of 2020 to week 8 of 2021 (September 13 to February 27), and from week 9 of 2021 to week 22 of 2021 (February 28 to June 5) among Medicare fee-for-service beneficiaries undergoing maintenance dialysis.
Supplemental Table 5. Adjusted odds ratios of COVID-19 diagnosis from epidemiologic week 12 to week 23 of 2020 (March 15 to June 6), from week 24 of 2020 to week 37 of 2020 (June 7 to September 12), from week 38 of 2020 to week 8 of 2021 (September 13 to February 27), and from week 9 of 2021 to week 22 of 2021 (February 28 to June 5) among Medicare fee-for-service beneficiaries undergoing maintenance dialysis.
Supplemental Table 6. Adjusted odds ratios of COVID-19 hospitalization from epidemiologic week 12 to week 23 of 2020 (March 15 to June 6), from week 24 of 2020 to week 37 of 2020 (June 7 to September 12), from week 38 of 2020 to week 8 of 2021 (September 13 to February 27), and from week 9 of 2021 to week 22 of 2021 (February 28 to June 5) among Medicare fee-for-service beneficiaries undergoing maintenance dialysis.
References
- 1.Weinhandl ED, Wetmore JB, Peng Y, Liu J, Gilbertson DT, Johansen KL: Initial effects of COVID-19 on patients with ESKD. J Am Soc Nephrol 32: 1444–1453, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wetmore JB, Johansen KL, Liu J, Peng Y, Gilbertson DT, Weinhandl ED: Changes in treatment of patients with incident ESKD during the novel coronavirus disease 2019 pandemic. J Am Soc Nephrol 32: 2948–2957, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinhandl ED, Gilbertson DT, Wetmore JB, Johansen KL: COVID-19-associated decline in the size of the end-stage kidney disease population in the United States. Kidney Int Rep 6: 2698–2701, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United States Renal Data System : USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2021 [Google Scholar]
- 5.Park S, Kear TM: Current state-of-practice: Transportation for patients with end stage renal disease. Nephrol Nurs J 44: 309–315, 2017 [PubMed] [Google Scholar]
- 6.Montoya A, Cassone M, Mody L: Infections in nursing homes: Epidemiology and prevention programs. Clin Geriatr Med 32: 585–607, 2016 [DOI] [PubMed] [Google Scholar]
- 7.Taji L, Thomas D, Oliver MJ, Ip J, Tang Y, Yeung A, Cooper R, House AA, McFarlane P, Blake PG: COVID-19 in patients undergoing long-term dialysis in Ontario. CMAJ 193: E278–E284, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu CM, Weiner DE, Aweh G, Salenger P, Johnson DS, Lacson E Jr: Epidemiology and outcomes of COVID-19 in home dialysis patients compared with in-center dialysis patients. J Am Soc Nephrol 32: 1569–1573, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ouslander JG, Grabowski DC: COVID-19 in nursing homes: Calming the perfect storm. J Am Geriatr Soc 68: 2153–2162, 2020 [DOI] [PubMed] [Google Scholar]
- 10.Perl J, Thomas D, Tang Y, Yeung A, Ip J, Oliver MJ, Blake PG: COVID-19 among adults receiving home versus in-center dialysis. Clin J Am Soc Nephrol 16: 1410–1412, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare and Medicaid Services : Dialysis Facility Reports for Fiscal Year 2020, 2020. Available at: https://data.cms.gov/quality-of-care/medicare-dialysis-facilities/data/2020. Accessed March 10, 2022
- 12.Longenecker JC, Coresh J, Klag MJ, Levey AS, Martin AA, Fink NE, Powe NR: Validation of comorbid conditions on the end-stage renal disease medical evidence report: The CHOICE study. J Am Soc Nephrol 11: 520–529, 2000 [DOI] [PubMed] [Google Scholar]
- 13.Krishnan M, Weinhandl ED, Jackson S, Gilbertson DT, Lacson E Jr: Comorbidity ascertainment from the ESRD Medical Evidence Report and Medicare claims around dialysis initiation: A comparison using US Renal Data System data. Am J Kidney Dis 66: 802–812, 2015 [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services : Medicare COVID-19 Vaccine Analysis, 2022. Available at: https://www.cms.gov/medicare-covid-19-vaccine-analysis. Accessed March 10, 2022
- 15.Gilbertson DT, Rothman KJ, Chertow GM, Bradbury BD, Brookhart MA, Liu J, Winkelmayer WC, Stürmer T, Monda KL, Herzog CA, Ashfaq A, Collins AJ, Wetmore JB: Excess deaths attributable to influenza-like illness in the ESRD population. J Am Soc Nephrol 30: 346–353, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.