Introduction
Despite the high prevalence of ESKD in Nigeria, only 2% of these patients receive hemodialysis, which is the most widely available form of RRT in Nigeria (1–3). The overarching reason behind this devastatingly low hemodialysis uptake is out-of-pocket payment for health services in the country (1–3). Reports from 2018 revealed that only 3000 patients were receiving hemodialysis nationwide (3), and 80% of these patients do not sustain treatment beyond 3 months, resulting in repeated hospitalization of ESKD patients, poor quality of life, high morbidity, and premature deaths (4).
Patient advocacy efforts by nephrology health care professionals under the auspices of the Nigeria Association of Nephrology has not yielded a significant government response. The National Health Insurance Scheme (NHIS) does not fund hemodialysis for patients with CKD, and erythropoietin stimulating agents are not included in the NHIS medicines list (5); furthermore, <5% of Nigerians utilize the NHIS, mainly due to the elemental benefit packages and general poor health-seeking behavior of Nigerians (6). Consequently, a diagnosis of ESKD in Nigeria spells doom for the majority.
This paper aims to describe the status of hemodialysis service delivery in Nigeria, reviewing the barriers to effective dialysis management and highlighting opportunities for improvement. Data presented are based on an online survey completed by nephrology care professionals from April to May 2022 and relevant existing literature.
History of Hemodialysis in Nigeria
Hemodialysis services in Nigeria have evolved over the years, providing relatively improved care for the growing population with ESKD. The first public hemodialysis center in Nigeria was at the Lagos University Teaching Hospital, which became operational in November 1981 (1), while the first private center, also situated in Lagos, started in 1987 (1). The number of centers increased from 27 in 2006 (1) to 186 in 2021 (3), while the dialysis population grew from 300 in 2000 to more than 3000 in 2018 (1,3).
The average cost of hemodialysis has increased steadily over the years from N25,000 (US$125) in 2005 (2) to N36,000–N70,000 (US$100–US$200) in 2018 (3). The dialysate used was mainly acetate, with a few centers (25%) practicing dialyzer reuse, and no center offered hemodiafiltration treatment in 2000 (3). Femoral catheters were typically used for vascular access in most units because there were few trained experts in central venous catheters insertion and arteriovenous fistulae (AVF) creation in 2000. Although trained nephrologists, specialist nurses, and dialysis technicians were initially scarce, there has been an increase in the number of nephrologists, dialysis nurses, and technicians (3). However, this positive change is threatened by the rising brain drain.
Current Status of Hemodialysis Services in Nigeria
Nigeria comprises 36 states and the Federal Capital Territory, with an estimated population of 200 million (7). Although the Nigerian renal registry is still a work in progress, and there are no conclusive figures for the ESKD population in Nigeria, several studies have shown that approximately 20 million Nigerians are living with CKD (1). Assuming a modest 1% (200,000) of people living with CKD population are likely to progress to ESKD, then only 2% (3000) of Nigerian ESKD patients were receiving hemodialysis in 2018; this situation has not changed much in 2022. Furthermore, there are only 240 nephrologists, 697 registered dialysis nurses (145 of these migrated to Western countries), and 120 dialysis technologists/technicians delivering care to the large population of CKD patients in Nigeria.
The financial cost of hemodialysis is still prohibitive for most Nigerians, considering the minimum wage of N30,000 (US$72). The average cost of a session of hemodialysis is N40,000 (US$96) compared with N30,000 (US$150) about 10 years ago; and the cost is usually higher in private facilities. A tunnel catheter costs N80,000 (US$192), temporary central catheter N25,000 (US$60), and a femoral catheter N10,000 (US$24), and AVF surgery costs N150,000–N300,000 (US$316–US$722).
A researcher-structured online survey aimed at determining the current status of hemodialysis in the country was completed by nephrology care professionals across Nigeria from April to May 2022. The authors (one of whom is an executive of the Nigerian Association of Nephrology) purposively disseminated the survey to nephrologists, dialysis nurses, and technicians using their contacts on the Nigerian Association of Nephrology WhatsApp messenger platform. The survey included 19 questions to ascertain the name of the hemodialysis center and whether private or public owned, the number of patients, the number of hemodialysis machines, the presence of support facilities, the staffing and patient/nurse ratio, and the use of vascular access. A total of 103 responses were received, each representing their hemodialysis unit; however, after removing duplicate reports for some centers, the final number of units was 80, spanning all regions of the country.
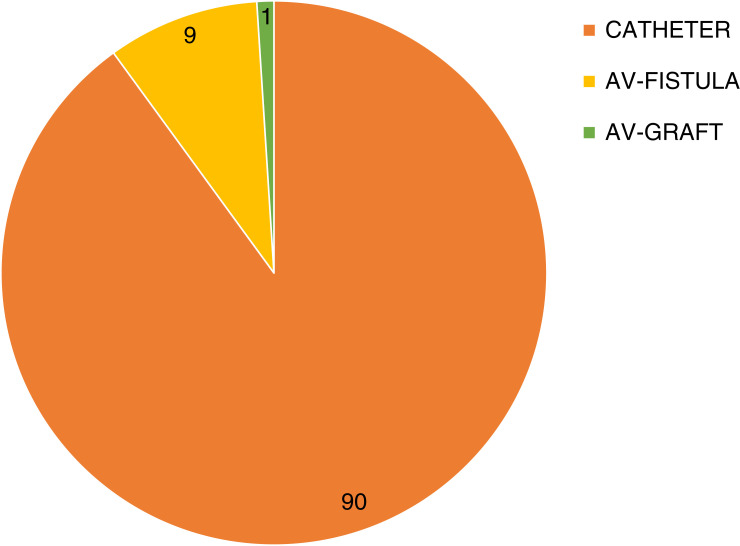
The survey revealed a total hemodialysis population of 3050 spread across 80 actively functioning centers in Nigeria, with the majority of units having 5–30 patients each. Unfortunately, the few centers in the country having more than 200 hemodialysis patients are supported by philanthropists or located in high-rise areas with relatively wealthier clientele. The median dialysis vintage is 1 month (interquartile range 0.6) but ranged from 0.5 to 120 months with the wealthier patients and those supported by philanthropists and cooperate bodies representing a minority who have longer mean dialysis vintage. The 80 hemodialysis units mainly cater for adult patients, with the majority lacking the appropriate size of consumables for the pediatric age group. Regarding vascular access, >90% of patients dialyze using central venous catheters, with the majority being temporary femoral catheters, which are the cheapest; <10% of patients dialyze using an AVF or arteriovenous graft in most of the centers (Figure 1). Table 1 shows an overview of the status of hemodialysis in Nigeria as of April 2022.
Figure 1.
Percentage of hemodialysis patients using types of vascular access across 80 hemodialysis centers.
Table 1.
Overview of hemodialysis status in Nigeria (April 2022)
| Description | Data |
|---|---|
| Number of hemodialysis patients | 17 per million people (N=3050) |
| Percent of patients on home hemodialysis dialysis | 0.62% |
| Out-of-pocket payment for dialysis | 98% |
| Number of hemodialysis centers | 80 |
| Hemodialysis vintage | |
| Median (months) | 1 (0.3) |
| Range (months) | 0.5–60 |
| Unit characteristics, % of units (N=80) | |
| Hospital-based units | 90 |
| Freestanding units | 10 |
| Public-owned units | 65 |
| Private-owned units | 24 |
| Public-private owned | 11 |
| For-profit | 64 |
| Nonprofit | 36 |
| Number of hemodialysis machines per center | |
| Mean | 4±1 |
| Range | 1–15 |
| Units with functioning continuous RRT machines (%) | |
| Yes | 16 |
| No | 84 |
| Staff offering dialysis in units (%) | |
| Nurses only | 55 |
| Nurses and other staffa | 45 |
| Patient/nurse ratio (%) | |
| ≥4:1 | 19 |
| 3:1 | 29 |
| 2:1 | 36 |
| 1:1 | 16 |
| Nephrologists’ review of dialysis patients per month | |
| 0–1 | 23 |
| 2–4 | 53 |
| 5–8 | 14 |
| >8 | 11 |
| Pharmacy located within the unit? | |
| Yes | 28 |
| No | 73 |
| Laboratory located within the unit? | |
| Yes | 38 |
| No | 63 |
Doctors, technicians, health assistants, student nurses, or biomedical engineers.
Barriers to Quality Hemodialysis in Nigeria
With a fast-growing population and an increasing disease burden, tremendous progress has been made by collective efforts of stakeholders to improve hemodialysis in Nigeria. Yet, challenges persist. Several factors threaten the availability, affordability, and accessibility of hemodialysis services, including those that are economic, political, manpower related, infrastructure and equipment related, and behavioral.
Economic Factors
Dialysis is expensive and unaffordable for most patients in Nigeria. Although Nigeria has the largest economy in Africa, 40% of the population live below the poverty line—a situation worsened by the deep recession experienced in 2020 following the pandemic (8). The cost of a session of hemodialysis is presently more than the official minimum wage (N30,000) in Nigeria, and many people earn below this figure. The implication of this meager income is that a large proportion of ESKD patients will either not subscribe to hemodialysis or exhaust their earnings and savings and still not be able to sustain hemodialysis beyond 1–3 months.
The resource allocated to health is poor, and there is no meaningful government support for hemodialysis. Consequently, the majority of patients pay out-of-pocket for hemodialysis and most essential medications such as erythropoiesis-stimulating agents. Only a negligible number of patients benefit from corporate bodies and philanthropists.
Political Factors
The government lacks the political will regarding improved care for ESKD patients, and this is despite advocacy efforts of nephrology associations and other nongovernmental organizations. Unfortunately, accurate data on the burden of ESKD in Nigeria are still lacking, and this crucial information is needed for more effective advocacy. Nevertheless, the devastating outcomes of ESKD are evident to Nigerians and the government, but this has not motivated any appreciable response. Politicians are among the wealthy class who often do not experience the hardships described above and hardly utilize public health institutions, possibly explaining their apathy. Another reason is competing financial demands, where health is hardly considered a priority. A few states have attempted to provide subsidized hemodialysis for their indigenes, but this was not sustainable in some states due to the high associated costs and corrupt practices.
Manpower Factors
Manpower-related challenges include manpower shortage, poor staff motivation, brain drain, and inadequate training. Other factors are unavailability of staff due to incessant strikes, especially in the public sector to protest against unfavorable remuneration, poor work environment, and embargo on employment, among others. Furthermore, Nigeria, like other Sub-Saharan African countries, is experiencing a disproportionately higher disease burden that overwhelms the available nephrology workforce, resulting in suboptimal patient care and outcomes in underserved areas.
Training and education of dialysis staff is inadequate, and training centers are scarce and very competitive. Hemodialysis nurses who are motivated to learn new skills and advance their career cannot afford the opportunities available, and minimal support is provided by their training institutions in terms of financing and protected training time. Several centers are manned by nurses without nephrology certification assisted by other health workers. Staff motivation is low due to poor remuneration when compared with developed countries, and this is a push factor for brain drain, which has further reduced the available staff in many centers and closure of hemodialysis units in extreme situations.
Infrastructure and Equipment
Compared with hemodialysis units in developed countries, the hemodialysis infrastructure in Nigeria is inadequate, with centers lacking basic utilities and support services such as side laboratories, pharmacy units, or drug dispensaries. Most centers are in-hospital and thus shared by in- and outpatients—a situation that often results in long waiting times. The availability of hemodialysis centers is disparate, with none in rural areas, few in most urban areas, and several in the megacities. This disparity is because hemodialysis centers are mainly for-profit and so the profit drives location. The implication of this is that many patients have to travel long distances to access hemodialysis, thereby increasing the financial burden in addition to travel safety issues.
Equipment downtime in many centers is a common challenge; machines are old and often poorly maintained, and spare parts are imported, scarce, and costly. The high costs and resultant scarcity stem from the uncertainties in the Nigerian economy since the coronavirus disease 2019 crisis. In addition, there is a dearth of trained technicians to maintain machines. Other problems are frequent power interruptions, with poor and expensive backups.
Behavioral Factors
A good number of ESKD patients in Nigeria will resort to alternative practices aimed at treating or curing CKD because the cost of orthodox treatment is prohibitive. These alternatives include buying medicines over the counter for symptom relief, purchasing alternative medicines that are marketed as curative sometimes by health professionals themselves, seeking miracles in prayer houses, and resorting to diabolic means to rid themselves of the perceived curse. The result of this trend is late presentation to the nephrologist with advanced disease and severe clinical features, contributing to increased morbidity, repeated hospitalizations, and mortality.
Conclusions
Access to hemodialysis services in Nigeria remains poor and concerning. The available dialysis units are insufficient, with a number of areas lacking any functional dialysis unit. Out-of-pocket payment is an enormous barrier to equitable dialysis access, and it will require efforts from all stakeholders. The nephrology community needs to continue steadfastly with public education, preventive programs, and advocacy efforts in partnership with other stakeholders to find sustainable solutions to the devasting outcomes of ESKD treatment in Nigeria. Universal NHIS coverage to include kidney care and improved remuneration, incentives, and training for health care workers is strongly recommended to limit the brain drain.
Disclosures
O. Okoye reports being the founder of St. Linus Renal Care Initiative, a nonprofit organization focused on preventing CKD and on improving the lives of Nigerians living with CKD. The remaining author has nothing to disclose.
Funding
None.
Acknowledgments
The content of this article reflects the personal experience and views of the authors and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the authors. The authors wish to appreciate members of Nigerian Association of Nephrology who completed the online survey and provided useful information.
Author Contributions
O. Okoye was responsible for the conceptualization, data curation, and formal analysis, and both authors wrote the original draft of the manuscript and reviewed and edited the manuscript.
References
- 1.Bamgboye EL: Hemodialysis: Management problems in developing countries, with Nigeria as a surrogate. Kidney Int Suppl 63: S93–S95, 2003. 10.1046/j.1523-1755.63.s83.19.x [DOI] [PubMed] [Google Scholar]
- 2.Ajayi S, Raji Y, Bello T, Jinadu L, Salako B: Unaffordability of renal replacement therapy in Nigeria. Hong Kong J Nephrol 18: 15–19, 2016. 10.1016/j.hkjn.2015.11.002 [DOI] [Google Scholar]
- 3.Arogundade FA, Esezobor CI, Okafor HU, Abdu A, Balogun RA, Effa EE, Popoola J, Bamgboye EL: Nephrology in Nigeria. In: Nephrology Worldwide, edited by Moura-Neto JA, Divino-Filho JC, Ronco C, Cham, Springer, 2021, pp 41–54 10.1007/978-3-030-56890-0_5 [DOI] [Google Scholar]
- 4.Salako BL: Managing chronic renal disease in Nigeria. Niger Med J 40: 75e7, 2001 [Google Scholar]
- 5.National Health Insurance Scheme (NHIS) : Benefits Package. Available at: https://www.nhis.gov.gh/benefits.aspx. Accessed June 2, 2022
- 6.Adeniji F: National Health Insurance Scheme in Nigeria: Progress towards universal coverage. Asian J Med Health 3: 1–2, 2017. 10.9734/AJMAH/2017/31975 [DOI] [Google Scholar]
- 7.The World Bank : Population, Total—Nigeria. Available at: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=NG. Accessed June 10, 2022
- 8.The World Bank : The World Bank in Nigeria. Available at: https://www.worldbank.org/en/country/nigeria. Accessed June 10, 2020