Abstract
Background
Falls are a leading cause of injury-related hospitalizations among adults aged 65 years and older and may result in social isolation.
Objective
To summarise evidence on falls and subsequent social isolation and/or loneliness in older adults through a scoping review.
Eligibility criteria
Studies were eligible for inclusion if the population had a mean age of 60 years or older, they examined falls and subsequent social isolation, loneliness, fear of falling or risk factors and were primary studies (eg, experimental, quasi-experimental, observational and qualitative).
Sources of evidence
MEDLINE, CINAHL, Embase, Ageline and grey literature from inception until 11 January 2021.
Charting methods
A screening and charting form was developed and pilot-tested. Subsequently, two reviewers screened citations and full-text articles, and charted the evidence.
Results
After screening 4993 citations and 304 full-text articles, 39 studies were included in this review. Participants had a history of falling (range: 11% to 100%). Most studies were conducted in Europe (44%) and North America (33%) and were of the cross-sectional study design (66.7%), in the community (79%). Studies utilised 15 different scales. Six studies examined risk factors for social isolation and activity restriction associated with fear of falling. Six studies reported mental health outcomes related to falls and subsequent social isolation.
Conclusions
Consistency in outcome measurement is recommended, as multiple outcomes were used across the included studies. Further research is warranted in this area, given the ageing population and the importance of falls and social isolation to the health of older adults.
Scoping review registration number
10.17605/OSF.IO/2R8HM.
Keywords: rehabilitation medicine, geriatric medicine, preventive medicine
Strengths and limitations of this study.
A robust methodology including a thorough and extensive literature search was used to review the literature in the area.
There were no date or language limits for studies eligible for inclusion in this scoping review.
Scoping reviews do not assess the quality of included studies and we cannot confirm the directional causality between falls and social isolation.
Introduction
Addressing social isolation in older adults is a growing priority in Canada, as over 30% of older adults are at risk of social isolation.1 Social isolation among older adults is associated with adverse health outcomes including cognitive decline, depression, anxiety and dementia.2
Globally, falls are the second leading cause of unintentional injury death, making falls a major public health concern.3 In Canada, falls are the leading cause of injury-related hospitalisations among adults aged 65 years and older, and 20%–30% of older adults experience at least one fall each year.4 Falls may result in serious health-related consequences including physical (eg, fractures), physiological (eg, cognitive decline) and psychological (eg, anxiety, depressive symptoms, fear of falling and social isolation) outcomes.5
Given the detrimental outcomes associated with both falls and social isolation, there is a need to understand the relationship between falls and subsequent social isolation in older adults. The current scoping review is focused on falling and the subsequent experience of social isolation and/or loneliness and to ascertain whether the COVID-19 context affected the relationship between falls and subsequent social isolation.
Methods
Protocol and registration
The protocol for this scoping review was developed in accordance with the JBI (formerly Joanna Briggs Institute) guidance for scoping reviews and registered with Open Science Framework.6 An integrated knowledge translation approach was used,7 whereby colleagues from the Public Health Agency of Canada (YJ, KA, MD and AG-B) co-developed the review. The results are reported using the Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) extension to scoping reviews8 supplemented by PRISMA 2020.9
Patient and public involvement
Through the Strategy for Patient-Oriented Research (SPOR) Evidence Alliance, we collaborated closely with a patient partner who provided feedback on our protocol, participated in full-text screening piloting and provided input on the manuscript (JB).
Search strategy
An experienced librarian developed our comprehensive literature search strategy, which was peer-reviewed by a second information specialist using the Peer Review of Electronic Search Strategies (PRESS) checklist.10 MEDLINE, CINAHL, Embase and Ageline were searched from inception until 11 January 2021 (online supplemental appendix 1). References of included studies and relevant reviews were scanned. Grey literature (ie, unpublished or difficult to locate studies) was searched using the Canadian Agency for Drugs and Technologies in Health’s Grey Matters checklist.11
bmjopen-2022-062124supp001.pdf (365.5KB, pdf)
Eligibility criteria
The population of interest were older adults with a mean age of 60 years or older. The concept was the relationship between falls and subsequent social isolation or loneliness. As mentioned in our related systematic review on interventions for social isolation after falling, social isolation and loneliness are distinct concepts.12 Social isolation included a decrease in any of the following: number of social contacts, feeling of belonging, fulfilling relationships, engagement with others and quality of their personal network.12 We defined loneliness as ‘the unpleasant experience that occurs when a person’s network of social relations is deficient in some way, either quantitatively or qualitatively’.13 For our primary objective, the context included any community or institutional setting. For our secondary objective, we limited the context to include studies that specified their consideration of the COVID-19 pandemic. Studies including participants reporting a history of falling (ie, regardless of the proportion of the sample who fell), the role of fear of falling in this relationship, as well as any risk (eg, medication use, frailty) or protective (eg, exercise, gait or balance training) factors were considered eligible for inclusion.
Eligible study designs included primary research studies of experimental (e.g., randomised controlled trials), quasi-experimental (e.g., non-randomised controlled trials, controlled before and after studies and interrupted time series), observational (e.g., cohort studies, case–control studies and cross-sectional studies), qualitative (phenomenological, ethnography, qualitative interview, etc.) and mixed-method (e.g., convergent parallel, embedded and explanatory sequential) design. No restrictions based on study year, language of publication or study duration were applied.
Study selection
A screening form was developed and a pilot-test using 50 citations was completed with 80% agreement, and subsequently, all remaining titles and abstracts were screened independently by pairs of reviewers (SMT, AP, JF, GM and AH). Discrepancies were resolved by a third reviewer.
Similarly, two pilot-tests were completed for full-text article screening (achieving 27% and 40% agreement, respectively), screening criteria were revised, and subsequently, full-text articles were assigned to independent pairs of reviewers. Discrepancies were resolved by a third reviewer.
Data charting
A charting form was developed to capture data on study characteristics, population characteristics and outcomes of interest. Relevant outcomes included any data illustrating the relationship between falls and subsequent social isolation, including the role of fear of falling, and other risk factors or protective factors. A pilot-test was conducted using five studies, sufficient agreement was achieved, and subsequently, full data charting was completed by independent pairs of reviewers. Discrepancies were resolved by a third reviewer.
Analysis and presentation of results
The review findings were summarised descriptively using summary tables.
Results
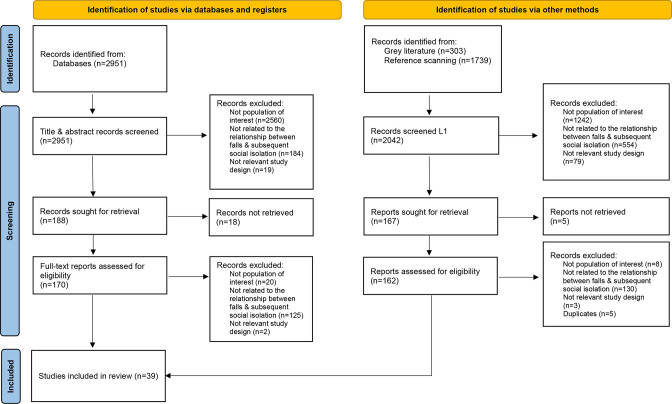
After screening 4993 citations and 304 full-text articles against our eligibility criteria, 39 studies were identified as eligible for inclusion based on our primary objective for this review (figure 1). No studies were identified when limiting to the COVID-19 context for our secondary objective. Study and patient characteristics have been summarised in table 1 and detailed data are reported in online supplemental appendices 2 and 3.
Figure 1.
PRISMA 2020 study flow diagram. PRISMA, Preferred Reporting Items for Systematic reviews and Meta-analysis.
Table 1.
Summary of study and patient characteristics
| Characteristics | Number (%) |
| Study characteristics (n=39) | |
| Geographical region | |
| Asia | 5 (12.8) |
| Australia | 1 (2.5) |
| Europe | 17 (43.6) |
| North America | 13 (33.3) |
| South America | 3 (7.7) |
| Study design | |
| Cohort | 6 (13.8) |
| Cross-sectional | 26 (66.7) |
| Qualitative | 7 (19.4) |
| Study duration | |
| Not applicable | 29 (74.3) |
| ≤ 1 year | 5 (12.8) |
| ≥ 1 year | 5 (12.8) |
| Patient characteristics | |
| Mean age | 74.9 (range, 65.0 to 95.0) |
| Not reported | 11 (28.2) |
| 65.0–69.9 years | 4 (10.2) |
| 70.0–74.9 years | 8 (20.5) |
| 75.0–79.9 years | 14 (35.9) |
| ≥80.0 years | 2 (5.1) |
| Proportion of female participants | Mean: 65.3% (range, 42.5 to 88.9) |
| Sample size | Mean: 3043.6 (9 to 43487) |
| <100 | 11 (28.2) |
| 100–499 | 11 (28.2) |
| 500–999 | 3 (7.7) |
| 1000–1999 | 4 (10.2) |
| 2000–5000 | 4 (10.2) |
| >5000 | 6 (15.4) |
| Study setting | |
| Community | 31 (79.4) |
| Medical | 6 (15.4) |
| Nursing home | 1 (2.5) |
| Multisite | 1 (2.5) |
| Participants living alone | 44.1% (range, 0 to 100) |
| Participants with a history of falling | Mean: 50.8% (range, 11.2 to 100) |
| Not reported* | 11 (28.2) |
| ≤25% | 6 (15.4) |
| 25–40% | 10 (25.6) |
| 40–85% | 5 (12.8) |
| >85% | 7 (17.9) |
*Not reported for the overall sample.
Study characteristics
The publication year for included studies ranged from 1987 to 2020, with more than half published since 2010. Most studies were conducted in Europe (17/39, 44%) and North America (13/39, 33%). More than half of the studies were cross-sectional study design (66.7%) and seven qualitative studies were included. Most were conducted in the community (79%). Studies utilised 15 different scales and a variety of self reported responses to assess variables such as social isolation and loneliness (eg, 18-item Lubben Social Network Scale, 6-item de Jong-Gierveld Loneliness Scale). Six studies identified risk factors for social isolation and for activity restriction due to fear of falling (table 2). Six studies reported mental health outcomes (online supplemental appendix 4).
Table 2.
Potential risk factors for social isolation and activity restriction associated with fear of falling
| Author, year | Risk factor | Associated evidence |
| Social isolation after injurious fall | ||
| Nicholson, 200525 | Sex (female) | The authors noted a strong positive correlation between injurious falls and social isolation for women (ρ=−0.5; p=0.01), but this was not significant for men. |
| Activity restriction due to fear of falling | ||
| Zijlstra, 2007 | Aged 80 years or older | OR: 1.56 (95% CI, 1.24 to 1.95) |
| Fair perceived general health | OR: 2.92 (95% CI, 2.43 to 3.52) | |
| Poor perceived general health | OR: 5.7 (95% CI, 3.57 to 9.12) | |
| Curcio et al, 200932 | Poor perceived health | OR: 1.38 (95% CI, 1.06 to 1.79) |
| Depression | OR: 1.76 (95% CI, 1.38 to 2.24) | |
| Low social participation | OR: 1.52 (95% CI, 1.20 to 1.92) | |
| Difficulties in activities of daily living | OR: 1.65 (95% CI, 1.16 to 2.32) | |
| Decreased physical activity | OR: 1.35 (95% CI, 1.06 to 1.70) | |
| Polypharmacy | OR: 1.56 (95% CI, 1.14 to 2.14) | |
| Below poverty level | OR: 1.32 (95% CI, 1.05 to 1.65) | |
| Dias, 2011 | Depression | χ2=15.2, p=0.004 |
| Exhaustion (frailty) | χ2=9.2, p=0.01 | |
| Participation in social activities | χ2=10.4, p=0.016 | |
| Murphy et al, 200240 | Two or more chronic conditions | ARR: 1.34 (95% CI, 1.08 to 1.65) |
| Slow-timed physical performance | ARR: 1.44 (95% CI, 1.18 to 1.75) | |
| Merchant et al, 202034 | Sarcopenia | OR, 8.13 (95% CI, 1.52 to 43.41) |
ARR, adjusted risk ratio; OR, odds ratio.
Patient characteristics
Across all studies, the number of included patients was 118 702, with an average of 3043 patients per study. Their mean age ranged from 65 to 95 years. Approximately 65% of patients were female. Most studies included participants with a history of falling, ranging from 11% to 100% of the study population.
Cohort studies
Among the 39 included studies, six were cohort studies (online supplemental appendix 5). Tinetti and Williams14 demonstrated a significant relationship between multiple non-injurious falls and a decline in social functioning (regression coefficient=−0.538 (p<0.05)), measured using the Social Activity Scale, in a sample of 770 older adults after 3 years of follow-up.14 Similarly, Pin and Spini15 found that in their cohort of 16 583 participants, those who fell showed decreased social participation after falling (p<0.001), which was no longer statistically significant when frailty was added in the model.15
Vellas et al16 compared people who fall versus those who did not in two populations: a retirement home (n=118) and older adults living at home (n=60).16 Among the older adults who lived at home, they noted that fewer fallers were able to maintain the same level of activity after 6 months of follow-up when compared with non-fallers (p<0.02).
van der Meulen et al17 assessed social participation (using the Frenchay Activities Index) in 260 older adults with low and high levels of concern about falling over 14 months.17 They reported significant differences (specific results not reported) between the groups, with lower social participation scores in those who had a higher level of concern about falling.
In 4680 older adults, Yu et al18 reported a significant relationship between the number of falls and loneliness scores (measured using the three-item University of California, Los Angeles (UCLA) Loneliness Scale) across three time points over 4 years (B=0.008, p<0.05).18 A cohort study by Hajek and König19 looked at loneliness (as measured using the Bude and Lantermann scale) and social isolation (measured using the De Jong Gierveld Loneliness Scale) and their link to fear of falling 669 older adults.19 They compared older adults with an onset of fear of falling, to those who had no fear. Their findings revealed that the end of fear of falling was associated with lower loneliness scores (β = −0.06, p<0.05) and other negative psychosocial outcomes (eg, increased depressive symptoms).
Cross-sectional studies related to falls and social isolation
Of the 26 cross-sectional studies included in this review, 11 reported on the relationship between falls and social isolation or loneliness (online supplemental appendix 6).
Quach20 examined the relationship between falls and scores on the Social Relationship Index including 8464 participants. He noted that participants who reported experiencing a fall or multiple falls had a lower social relationship index score (mean, 3.24 and 3.08 respectively) compared with those who had not fallen (mean, 3.34; p<0.0001).
Hajek and König21 examined variables associated with a history of falling in 7808 participants. They found those reporting a fall in the previous 12 months had higher loneliness scores (De Jong Gierveld Loneliness Scale; β=0.08, p<0.001) and social exclusion scores (Bude and Lantermann scale; β=0.08, p<0.001) compared with those who had not fallen.
Schnittger et al22 conducted a study in 579 older adults identifying risk factors for different pathways of loneliness—emotional loneliness, social loneliness (both measured using the De Jong Gierveld Loneliness Scale) and social support (measured using the Lubben Social Network Scale). A history of falls was the only biological variable that was identified as a statistically significant risk factor for inclusion in the model for social support (correlation coefficient=−0.247; p<0.003).
Stel et al23 reported a statistically significant decline in social activities in 204 older adults who experienced a fall inside their home (OR: 2.6 (95% CI: 1.1 to 6.5); p<0.05), and Vanden Wyngaert et al24 reported an association between risk of falls and participation in social roles and activities in 154 older adult haemodialysis patients (PROMIS questionnaire; R2=0.11; p=0.01). Finally, Nicholson25 reported a strong positive relationship between experiencing an injurious fall and increasing social isolation in a sample of 68 older adults (Lubben Social Network Scale; ρ=−0.4; p<0.05), and highlighted that this relationship was stronger in women (ρ=−0.5; p=0.01). Additionally, they assessed this relationship using both the Family and Friends subscales of the Lubben Social Network Scale and found that the correlation was specific to the Friends subscale (ρ=−0.43; p<0.05).
Iliffe et al26 and Robins et al27 found no statistically significant associations between falls and social isolation using the Lubben Social Network Scale in a sample of 3139 older adults and the Friendship Scale for social isolation in a sample of 245 older adults, respectively. Similarly, van Lankveld et al28 and Faria et al29 found no correlation between falls and loneliness, using the De Jong Gierveld Loneliness Scale in a sample of 579 older adults, and the UCLA Scale in a sample of 48 older adults, respectively. Additionally, Finn 30 noted no difference in scores for the Older Americans Resources and Services (OARS) social support scale when comparing fallers to non-fallers in a nursing home setting (n=49).
Cross-sectional studies related to fear of falling and social isolation
Seven studies examined fear of falling linked to falls and social isolation (online supplemental appendix 7). Gagnon et al31 reported a statistically significant positive relationship between fear of falling and social support in a sample of 105 older adults (measured using the confiding-relationships component of the Bedford Life Events and Difficulties Schedule modified for elderly subjects; Wald χ2=3.77; p=0.05). Curcio et al32 reported a strong relationship between fear of falling and low social participation in 1668 older adults (OR, 1.52; 95% CI, 1.20 to 1.92; p<0.01). Petrinec et al33 (2020) identified fear of falling as an independent predictor of social functioning (as measured by the Medical Outcomes Study 36-item Short-Form General Health Survey; β=−0.29) in 108 older adults.
Merchant et al34 and Iliffe et al26 showed no statistically significant relationship between fear of falling and social isolation in 493 older adults and 3139 older adults, respectively. Ferreira et al35 and Kara et al36 showed no association between fear of falling and social participation (n=7935) or fear of falling and loneliness (n=47), respectively.35 36
Cross-sectional studies related to falls and activity restriction due to fear of falling
Eight studies examined the relationship between falls and activity restriction due to fear of falling (online supplemental appendix 7). Tinetti et al37 and Apikomonkon38 both reported a statistically significant decrease in activity due to fear of falling in individuals who experienced a fall compared with those who had not (n=1103, χ2=13.1, p<0.001; and n=546, χ2=5.49, p<0.05, respectively).37 38 Similarly, in 1668 older adults, Curcio et al32 demonstrated that those who restricted activity due to fear of falling were more likely to have experienced a fall in the year prior (OR: 1.48 (95% CI, 1.18 to 1.86); p=0.001), and Mendes da Costa et al39 demonstrated that activity restriction increased in those with multiple falls over the past year (OR, 3.04; 95% CI, 1.70 to 5.42). Murphy et al40 and Choi and Ko41 showed that a history of injurious falls was independently associated with activity restriction due to fear of falling (n=1064, adjusted risk ratio: 1.36; 95% CI, 1.11 to 1.66; p=0.003; and n=4247, OR, 3.03; 95% CI, 1.21 to 7.54, p=0.008, respectively).
Howland et al42 reported no relationship between the experience of a fall and activity restriction in a sample of 266 older adults (OR: 1.094; 95% CI, 0.376 to 3.177; p=0.869), as did Choi and Ko41 (OR, 2.12; 95% CI, 0.96 to 4.67; p=0.062) among 4247 older adults. Similarly, Merchant et al34 (2020) also reported no significant relationship between the number of falls and fear-based activity restriction in 493 older adults (OR, 1.4; 95% CI, 0.94 to 2.20).
Qualitative studies
Seven qualitative studies were included (online supplemental appendix 8). All participants interviewed were older adults (n=124), including 51 stroke survivors43 44 and 10 experiencing frailty.45 Common categories identified across these studies were activity restriction to manage fear of falling, changing behaviours to avoid falling,43 45–47 feeling restricted due to reduced mobility after falling,43 44 48 increasing dependence on caregivers,43 45 developing fear of falling,43 45 feelings of loneliness or isolation43 48 and a negative impact on identity or autonomy.47
Discussion
We conducted a comprehensive scoping review including 39 studies examining the relationship between falls and subsequent social isolation. We limited the scoping review to studies that identified social isolation after a fall, this was due to the request of the commissioning knowledge user. More than half of the studies were published since 2010, suggesting increased interest in the relationship between falls and social isolation in older adults. Social isolation and loneliness were measured using a variety of outcome measures across studies, such as degree of activity, varying scales for loneliness, social isolation, social participation and social support. This highlights the growing need for consistency in the measurement of social isolation and loneliness to allow for meaningful comparison across studies. Cornwall and Waite49 highlight previous efforts to consolidate different measures of social isolation and build off this work. They combined multiple measures of social isolation to develop two scales that measure distinct dimensions of social isolation—social disconnectedness and perceived isolation.
Only a few studies examined risk factors and mental health outcomes related to falls and subsequent social isolation. Risk factors linked to social isolation and activity restriction included age, sex/gender, poor perceived health, poverty, frailty and comorbidity. Few studies also documented an association between activity restriction due to fear of falling and depression. Our findings suggest the presence of gaps in the literature for these important outcomes, highlighting the need for further research. No randomised trials exploring interventions for social isolation after a fall were identified in our scoping review, highlighting another gap in the literature and an area for future research to explore.
We did not identify any studies on falls and subsequent social isolation that were specific to the COVID-19 context, highlighting another gap in the evidence base. A scoping review by Kasar and Karaman50 suggest that older adults face increased social isolation as a result of pandemic-related restrictions, which can result in increased loneliness and reduced quality of life. They also highlighted how technology can be used to deliver virtual or tele-health support services, and to allow older adults stay connected with their social networks.50 A systematic review by Larson et al assessed the impact of COVID-19 lockdowns on physical activity in older adults and reported that most studies demonstrated a decline in physical activity or an increase in sedentary behaviours in this population. The effectiveness of physical activity and exercise in preventing falls and fractures in older adults is well established in the literature.51–53 A decline in physical activity in older adults could lead to sarcopenia, and an increased risk of falls or fractures.53
There are several strengths to our scoping review, such as the use of the JBI guide, and the PRISMA-extension for scoping reviews. A comprehensive literature search was conduced and several different types of study designs were included. However, limitations include that all studies were conducted in middle–high-income or high-income economy countries. This suggests that our results may not be generalisable to low-income and middle-income countries, highlighting a gap in the literature. Many of the included studies were cross-sectional and we cannot confirm the directional causality between falls and social isolation without more robust research. Furthermore, none of the included studies specifically focused on culturally and linguistically diverse backgrounds, who might be at greater risk of social isolation after experiencing a fall. Additional research is warranted in this area.54 In addition, we were unable to update the literature search due to lack of capacity and funding.
In summary, we found a dearth of research, particularly examining risk factors and mental health outcomes related to social isolation and falling in older adults. Further research is warranted in this area, given the importance of falls and social isolation to the health of older adults.
Supplementary Material
Acknowledgments
We thank Alissa Epworth for running the searches, deduplicating results and obtaining full-text articles. We also thank Katrina Chiu and Faryal Khan for their support with formatting the manuscript and creating tables and appendices.
Footnotes
Twitter: @GaryMitchellRN, @ameliegbeaupre
Contributors: ACT obtained funding for this study. SMT, ACT, YJ, MdG, and KA conceptualized the study. SMT drafted the protocol, with input from ACT, YJ, MdG, KA, JB, JW, and SES. SMT, AP, JF, GM, AH, and JB screened citations and full text articles, abstracted and verified data. SMT and ACT interpreted results, and SMT, AP, and ACT drafted the manuscript and revised the final version of the manuscript. All authors critically reviewed the manuscript and approved of the final version. ACT is acting as guarantor.
Funding: This project was commissioned and funded by the Public Health Agency of Canada (4500415303) through the query services of the Strategy for Patient-Oriented Research (SPOR) Evidence Alliance. The SPOR Evidence Alliance is supported by the Canadian Institutes of Health Research (CIHR) under Canada’s SPOR initiative, and the generosity of partners from 41 public agencies and organisations across Canada who have made cash or in-kind contributions. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis (17-0126-AWA), and SES is funded by a Tier 1 Canada Research Chair in Knowledge Translation (17-0245-SUB). GM and JF were in part supported by the Health Research Board (Ireland) and the HSC Public Health Agency (Grant number CBES-2018–001) through Evidence Synthesis Ireland and Cochrane Ireland.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The full dataset is available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not required.
References
- 1.Keefe J, Andrew M, Fancey P. A profile of social isolation in Canada. Report submitted to the F/P/T Working group on social isolation Province of British Columbia and Mount Saint Vincent university, 2006. [Google Scholar]
- 2.Government of Canada . Report on the social isolation of seniors, 2016. [Google Scholar]
- 3.World Health Organization . Falls, 2021. Available: https://www.who.int/news-room/fact-sheets/detail/falls
- 4.Public Health Agency of Canada . Seniors’ Falls in Canada: Second Report, 2014. [Google Scholar]
- 5.Terroso M, Rosa N, Torres Marques A, et al. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act 2014;11:51–9. 10.1007/s11556-013-0134-8 [DOI] [Google Scholar]
- 6.Tricco A, Thomas SM, Ramkissoon N, et al. Falls and social isolation in older adults, 2021. Available: https://osf.io/2r8hm
- 7.Kothari A, McCutcheon C, Graham ID. Defining integrated knowledge translation and moving forward: a response to recent commentaries. Int J Health Policy Manag 2017;6:299. 10.15171/ijhpm.2017.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGowan J, Sampson M, Salzwedel DM, et al. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 11.Canadian Agency for Drugs Technologies in Health . Grey matters: a practical tool for searching health-related grey literature (Internet, 2018. [Google Scholar]
- 12.Tricco AC, Thomas SM, Radhakrishnan A, et al. Interventions for social isolation in older adults who have experienced a fall: a systematic review. BMJ Open 2022;12:e056540. 10.1136/bmjopen-2021-056540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perlman D, Peplau LA. Toward a social psychology of loneliness. Pers Relationsh 1981;3:31–56. [Google Scholar]
- 14.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci 1998;53:M112–9. 10.1093/gerona/53a.2.m112 [DOI] [PubMed] [Google Scholar]
- 15.Pin S, Spini D. Impact of falling on social participation and social support trajectories in a middle-aged and elderly European sample. SSM Popul Health 2016;2:382–9. 10.1016/j.ssmph.2016.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vellas B, Cayla F, Bocquet H, et al. Prospective study of restriction of activity in old people after falls. Age Ageing 1987;16:189–93. 10.1093/ageing/16.3.189 [DOI] [PubMed] [Google Scholar]
- 17.van der Meulen E, Zijlstra GAR, Ambergen T, et al. Effect of fall-related concerns on physical, mental, and social function in community-dwelling older adults: a prospective cohort study. J Am Geriatr Soc 2014;62:2333–8. 10.1111/jgs.13083 [DOI] [PubMed] [Google Scholar]
- 18.Yu K, Wu S, Jang Y, et al. Longitudinal assessment of the relationships between geriatric conditions and loneliness. J Am Med Dir Assoc 2021;22:1107–13. 10.1016/j.jamda.2020.09.002 [DOI] [PubMed] [Google Scholar]
- 19.Hajek A, König H-H. What are the psychosocial consequences when fear of falling starts or ends? Evidence from an asymmetric fixed effects analysis based on longitudinal data from the general population. Int J Geriatr Psychiatry 2020;35:1028–35. 10.1002/gps.5325 [DOI] [PubMed] [Google Scholar]
- 20.Quach LT. Social determinants of falls: the role of social support and depression among community-dwelling older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering 2016;2018:78. [Google Scholar]
- 21.Hajek A, König H-H. The association of falls with loneliness and social exclusion: evidence from the DEAS German ageing survey. BMC Geriatr 2017;17:204. 10.1186/s12877-017-0602-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schnittger RIB, Wherton J, Prendergast D, et al. Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging Ment Health 2012;16:335–46. 10.1080/13607863.2011.629092 [DOI] [PubMed] [Google Scholar]
- 23.Stel VS, Smit JH, Pluijm SMF, et al. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing 2004;33:58–65. 10.1093/ageing/afh028 [DOI] [PubMed] [Google Scholar]
- 24.Vanden Wyngaert K, Van Craenenbroeck AH, Eloot S, et al. Associations between the measures of physical function, risk of falls and the quality of life in haemodialysis patients: a cross-sectional study. BMC Nephrol 2020;21:7. 10.1186/s12882-019-1671-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholson NR. The relationship between injurious falls, fear of falling, social isolation and depression, 2005. [Google Scholar]
- 26.Iliffe S, Kharicha K, Harari D, et al. Health risk appraisal in older people 2: the implications for clinicians and commissioners of social isolation risk in older people. Br J Gen Pract 2007;57:277. [PMC free article] [PubMed] [Google Scholar]
- 27.Robins LM, Hill KD, Finch CF, et al. The association between physical activity and social isolation in community-dwelling older adults. Aging Ment Health 2018;22:175–82. 10.1080/13607863.2016.1242116 [DOI] [PubMed] [Google Scholar]
- 28.van Lankveld W, Fransen M, van den Hoogen F, et al. Age-Related health hazards in old patients with first-time referral to a rheumatologist: a descriptive study. Arthritis 2011;2011:823527. 10.1155/2011/823527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faria AdaCA, Martins MMFPdaS, Ribeiro OMPL, et al. Elderly residents in the community: gaining knowledge to support a rehabilitation nursing program. Rev Bras Enferm 2020;73Suppl 3:e20200194. 10.1590/0034-7167-2020-0194 [DOI] [PubMed] [Google Scholar]
- 30.Finn JM. The relationship between falls and fall-related efficacy, depression, and social resources: Adler school of professional psychology, 2001. [Google Scholar]
- 31.Gagnon N, Flint AJ, Naglie G, et al. Affective correlates of fear of falling in elderly persons. Am J Geriatr Psychiatry 2005;13:7–14. 10.1176/appi.ajgp.13.1.7 [DOI] [PubMed] [Google Scholar]
- 32.Curcio C-L, Gomez F, Reyes-Ortiz CA. Activity restriction related to fear of falling among older people in the Colombian Andes mountains: are functional or psychosocial risk factors more important? J Aging Health 2009;21:460–79. 10.1177/0898264308329024 [DOI] [PubMed] [Google Scholar]
- 33.Petrinec AB, Crowe ML, Flanagan SK, et al. Health-Related quality of life of older women religious: negative influence of frailty. West J Nurs Res 2020;42:1088–96. 10.1177/0193945920936171 [DOI] [PubMed] [Google Scholar]
- 34.Merchant RA, Chen MZ, Wong BLL, et al. Relationship between fear of falling, Fear-Related activity restriction, frailty, and sarcopenia. J Am Geriatr Soc 2020;68:2602–8. 10.1111/jgs.16719 [DOI] [PubMed] [Google Scholar]
- 35.Ferreira FR, César CC, Andrade FBde, et al. Aspects of social participation and neighborhood perception: ELSI-Brazil. Rev Saude Publica 2018;52Suppl 2:18s. 10.11606/S1518-8787.2018052000647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kara B, Yildirim Y, Genc A. Assessment of home environment and life satisfaction in geriatrics and relation to fear of falling. Turk J Physiother Rehabil 2009;20:190–200. [Google Scholar]
- 37.Tinetti ME, Mendes de Leon CF, Doucette JT, et al. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol 1994;49:M140–7. 10.1093/geronj/49.3.m140 [DOI] [PubMed] [Google Scholar]
- 38.Apikomonkon H. Fear of falling and fall circumstances in Thailand. Curtin University, 2003. [Google Scholar]
- 39.Mendes da Costa E, Pepersack T, Godin I, et al. Fear of falling and associated activity restriction in older people. Results of a cross-sectional study conducted in a Belgian town. Arch Public Health 2012;70:1. 10.1186/0778-7367-70-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. J Am Geriatr Soc 2002;50:516–20. 10.1046/j.1532-5415.2002.50119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi K, Ko Y. Characteristics associated with fear of falling and activity restriction in South Korean older adults. J Aging Health 2015;27:1066–83. 10.1177/0898264315573519 [DOI] [PubMed] [Google Scholar]
- 42.Howland J, Lachman ME, Peterson EW, et al. Covariates of fear of falling and associated activity curtailment. Gerontologist 1998;38:549–55. 10.1093/geront/38.5.549 [DOI] [PubMed] [Google Scholar]
- 43.Schmid AA, Rittman M. Consequences of poststroke falls: activity limitation, increased dependence, and the development of fear of falling. Am J Occup Ther 2009;63:310–6. 10.5014/ajot.63.3.310 [DOI] [PubMed] [Google Scholar]
- 44.Xu T, O'Loughlin K, Clemson L, et al. Developing a falls prevention program for community-dwelling stroke survivors in Singapore: client and caregiver perspectives. Disabil Rehabil 2019;41:1044–54. 10.1080/09638288.2017.1419293 [DOI] [PubMed] [Google Scholar]
- 45.Faes MC, Reelick MF, Joosten-Weyn Banningh LW, et al. Qualitative study on the impact of falling in frail older persons and family caregivers: foundations for an intervention to prevent falls. Aging Ment Health 2010;14:834–42. 10.1080/13607861003781825 [DOI] [PubMed] [Google Scholar]
- 46.Meltem M, Oflaz Ç Fahriye. A Qualitative Study on the Perception of Elderly about fear of falling and it’s impact on daily life. Turk Geriatri Derg 2007;10:19–23. [Google Scholar]
- 47.Høst D, Hendriksen C, Borup I. Older people's perception of and coping with falling, and their motivation for fall-prevention programmes. Scand J Public Health 2011;39:742–8. 10.1177/1403494811421639 [DOI] [PubMed] [Google Scholar]
- 48.Chiu MW-Y. Psychosocial responses to falling in older Chinese immigrants living in the community [Doctoral Dissertation], 2010. [Google Scholar]
- 49.Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci 2009;64 Suppl 1:i38–46. 10.1093/geronb/gbp037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sayin Kasar K, Karaman E. Life in lockdown: social isolation, loneliness and quality of life in the elderly during the COVID-19 pandemic: a scoping review. Geriatr Nurs 2021;42:1222–9. 10.1016/j.gerinurse.2021.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 2017;318:1687–99. 10.1001/jama.2017.15006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Langhammer B, Bergland A, Rydwik E. The importance of physical activity exercise among older people. Biomed Res Int 2018;2018:1–3. 10.1155/2018/7856823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elisabeth AL, Karlen SB-L, Magkos F. The effect of COVID-19-related lockdowns on diet and physical activity in older adults: a systematic review. Aging Dis 2021;12:1935. 10.14336/AD.2021.0606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jang H, Lovarini M, Clemson L, et al. Fall prevention programs for culturally and linguistically diverse groups: program provider perspectives. Ethn Health 2021;26:299–317. 10.1080/13557858.2018.1493436 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-062124supp001.pdf (365.5KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The full dataset is available from the corresponding author upon reasonable request.