Abstract
Objectives. To evaluate lead levels in tap water at licensed North Carolina child care facilities.
Methods. Between July 2020 and October 2021, we enrolled 4005 facilities in a grant-funded, participatory science testing program. We identified risk factors associated with elevated first-draw lead levels using multiple logistic regression analysis.
Results. By sample (n = 22 943), 3% of tap water sources exceeded the 10 parts per billion (ppb) North Carolina hazard level, whereas 25% of tap water sources exceeded 1 ppb, the American Academy of Pediatrics’ reference level. By facility, at least 1 tap water source exceeded 1 ppb and 10 ppb at 56% and 12% of facilities, respectively. Well water reliance was the largest risk factor, followed by participation in Head Start programs and building age. We observed large variability between tap water sources within the same facility.
Conclusions. Tap water in child care facilities is a potential lead exposure source for children. Given variability among tap water sources, it is imperative to test every source used for drinking and cooking so appropriate action can be taken to protect children’s health. (Am J Public Health. 2022;112(S7):S695–S705. https://doi.org/10.2105/AJPH.2022.307003)
US regulations to control lead sources, including gasoline, paint, and plumbing, have led to significant declines in children’s blood lead levels since the 1970s.1 The continued presence of lead in drinking water from lead-bearing water infrastructure, including pipes, fixtures, solder, and service lines, still poses an ongoing health risk, however. Even low-level lead exposures in early childhood can result in irreversible developmental deficits, IQ loss, and behavioral issues.2,3 Lead exposure also affects other critical systems in the body, including the renal, cardiovascular, hematologic, and immunological systems.4 No safe lead exposure thresholds exist for any organ systems studied.4
Younger children may be exposed to lead by ingesting water at home, schools, and child care facilities, including those providing prekindergarten or Head Start programs. Nevertheless, tap water sources (herein called taps) at most US schools and child care centers are not currently tested for lead. The US Environmental Protection Agency (EPA) previously estimated that approximately 500 000 US child care facilities are not required to test for lead under current drinking water legislation.5 Child care centers and schools using well water serving at least 25 people for at least half the year (i.e., nontransient noncommunity water systems) are required to perform lead testing at the tap under the Lead and Copper Rule, but this applies to relatively few facilities and uses a different sampling approach. In North Carolina, there are only 180 such child care facilities, although there are more than 4300 facilities overall.6,7
The latest Lead and Copper Rule revisions include lead-testing requirements for centers and schools but would require only minimal testing (5 taps per school and 2 taps per center every 5 years) starting in 2024 at the earliest.8 Some limited studies have been conducted to estimate lead levels in US child care facilities, including among 56 primary schools and preschools in Kansas,9 206 centers across North Carolina,10 and 11 centers across 4 additional US states (i.e., Illinois, Michigan, Ohio, and Mississippi),11 but lead levels in drinking and cooking water at most US child care facilities is still unknown.
In response to these concerns, researchers from RTI International piloted a participatory science sampling program in 2017 with 86 licensed North Carolina child care centers and facilities with elementary schools with licensed prekindergarten or Head Start programs.12 The study revealed a high prevalence and variability of lead in tap water at facilities: 16% had at least 1 tap water source above 15 micrograms per liter (µg/L) or parts per billion (ppb), 60% had at least 1 tap water source above 1 ppb, and 83% had at least 1 tap water source above the laboratory reporting limit of 0.1 ppb. Furthermore, the study demonstrated the feasibility of a participatory science sampling approach. Based on this pilot study, in October 2019, the North Carolina Commission for Public Health adopted an amendment to an existing child care sanitation rule that requires licensed North Carolina child care centers, including pre-Kindergarten and Head Start programs within elementary school facilities, to test all drinking and food preparation taps for lead.13 As many child care facilities have older water infrastructure and even new “lead-free” plumbing contains allowable lead that may leach into tap water under corrosive conditions,14 all facilities were required to participate in the program regardless of building age. The initial round of statewide testing was free for child care facilities with a grant from the EPA’s Water Infrastructure for Improvements to the Nation (WIIN) Act.
We evaluated the results of first-draw testing from child care facilities across North Carolina to identify socioeconomic, demographic, and infrastructure-related factors associated with the risk of elevated lead in water in child care settings. To our knowledge, this study is the largest analysis of lead levels in child care facilities in the United States to date. The study provides critical new insight for facility staff and policymakers to make evidence-based decisions to improve the process of identifying, communicating, and eliminating water-related lead exposures where children learn and play.
METHODS
Licensed child care facilities enrolled in a participatory science sampling program to facilitate compliance with the amended 2019 North Carolina child care sanitation rule.13 After a preenrollment training webinar, child care staff filled out an online enrollment survey at www.cleanwaterforcarolinakids.org. Participants provided information on the building, water source, tap water source locations, filter use, and attending children’s demographics, including total enrollment, student race/ethnicity, number of children receiving free or reduced cost lunch, and number of children receiving subsidized tuition. After enrollment, we shipped a sampling kit to the facility. We enrolled and tested 4005 North Carolina child care facilities between July 2020 and October 2021, representing approximately 92% of all licensed facilities in the state at the time of this analysis.7 Only facilities confirmed to be currently operating under normal or reduced operating conditions despite the COVID-19 pandemic were eligible to participate. We did not include additional facilities that were tested after our required testing time frame in this analysis.
Testing and Laboratory Analysis
Child care facility staff collected first-draw samples in 250-milliliter (mL) high-density polyethylene bottles at each drinking and cooking tap water source. The protocol was based on the EPA’s training, testing, and taking action approach,15 with the exception that participants typically collected samples on Monday mornings after a weekend-long stagnation time because most child care facilities are closed during weekends and thus routinely experience stagnation periods greater than 8 to 18 hours.12 Participants returned samples to RTI International using prepaid return shipping labels. We analyzed water samples according to EPA method 200.8 (reporting limit = 0.1 ppb) following robust quality assurance and quality control protocols (details provided in the Appendix). In total, samples from 22 943 separate taps were collected and analyzed.
Data Analysis
We merged lead results with the corresponding socioeconomic, demographic, and building variables from the enrollment survey (Table 1). As there is no federally enforceable, health-based maximum contaminant level for lead at the tap water source, we categorized the lead results according to whether the first-draw lead concentration equaled or exceeded each of 3 different reference levels: (1) the American Academy of Pediatrics (AAP) reference level of 1 ppb, which most closely approximates a nonzero health-based reference level;17 (2) the revised North Carolina lead hazard level of 10 ppb (effective December 2021);18 and (3) the Lead and Copper Rule treatment-based action level for public utilities of 15 ppb, which many states use to document elevated lead, even though it is not a health-based threshold.19 We did not use the reporting limit of 0.1 ppb as a reference level for data analysis, as our goal in this analysis was to characterize factors associated with high-risk taps, and with the low reporting limit, most samples and child care facilities contained detectable lead at the tap water source.
TABLE 1—
Building, Water, and Program Characteristics and Child Demographics of Child Care Facilities Tested for Tap Water Lead Levels: North Carolina, July 2020–October 2021
| No. (%) or Mean ±SD (Range) | |
| Facility type | |
| Total | 4005 (100) |
| Home baseda | 192 (5) |
| School based | 743 (19) |
| Stand-alone, franchised | 205 (5) |
| Stand-alone, not franchised | 2865 (72) |
| Year built | |
| Before 1988 | 1944 (49) |
| 1988–2014 | 1876 (47) |
| After 2014 | 185 (5) |
| Building ownership | |
| Own | 2776 (69) |
| Lease | 1229 (31) |
| Water source | |
| Community water systemb | 3453 (86) |
| Well water | 196 (5) |
| Not reported | 356 (9) |
| Wastewater connection | |
| Community sewer system | 2581 (64) |
| Onsite waste system | 535 (13) |
| Not reported | 889 (22) |
| Located in HUD opportunity zone? | |
| Yes | 570 (14) |
| No | 3435 (86) |
| Houses Head Start program? | |
| Yes | 521 (13) |
| No | 3484 (87) |
| Number of samples collected | 6 ±6 (1–51) |
| Total student enrollment | 51 ±45 (1–651) |
| Child demographics, % | |
| Receiving free/reduced cost lunch | 55 ±42 (0–100) |
| Receiving subsidized tuition | 38 ±36 (0–100) |
| Non-White | 52 ±34 (0–100) |
Note. HUD = Department of Housing and Urban Development. We enrolled and tested 4005 North Carolina child care facilities.
Home-based licensed centers are different from family child care homes, which have a different license type and lower student number. Family child care homes were excluded from the North Carolina statewide lead-testing rule and did not participate in the initial round of grant-funded testing. They are included in the second round of testing currently in progress.
The Environmental Protection Agency defines a community water system as a public water utility that serves the same population year-round.16
We used the 3 resulting binary outcomes in mixed-effects multiple logistic regression models to evaluate potential risk factors from Table 1 associated with the odds of exceeding each reference level. Future analyses responding to changing regulatory limits may consider multinomial or continuous outcomes, but the 3 reference levels we chose provided insight into the most current policy and regulatory triggers in the United States. We also calculated the coefficient of variation (CV) to assess variability in lead concentrations across taps within each facility (facility-wide CV) and taps across the state. Additional details are available in the Appendix (available as a supplement to the online version of this article at https://www.ajph.org).
RESULTS
Most child care facilities (95%) were built before 2014 when the Reduction of Lead in Drinking Water Act took effect, which restricted the amount of lead in plumbing used for drinking water to 0.25% in wetted surfaces and 0.2% in solder (Table 1).16 Almost half of all facilities (49%) were also built before 1988, when the 1986 amendments to the Safe Drinking Water Act first restricted the allowable amount of lead in plumbing (8.0%) and solder (0.2%). Most facilities (86%) were connected to a community water system (i.e., a regulated public water utility) for their water supply, although 5% (196 facilities) reported well water usage (9% did not report water supply).
A total of 570 facilities (14%) were in economically distressed “opportunity zones” identified by the US Department of Housing and Urban Development, and 521 facilities (13%) ran federally funded Head Start programs for children from low-income families. Most Head Start programs were school based (57%). On average, Head Start programs served a significantly higher proportion of children receiving free and reduced cost lunch (91% among Head Start facilities compared with 49% among non–Head Start facilities; Wilcoxon P < .001) and non-White children (62% among Head Start facilities compared with 51% among non–Head Start facilities; Wilcoxon P < .001; Figure A [available as a supplement to the online version of this article at https://www.ajph.org]).
Summary of Lead Concentrations
The average first-draw lead level across all samples was 2.6 ppb and ranged from less than 0.1 ppb to 3930 ppb (Table 2; Figure B [available as a supplement to the online version of this article at https://www.ajph.org]). Overall, we detected lead above the laboratory reporting limit (0.1 ppb) in 76% of samples, whereas 25% of samples exceeded the AAP reference level of 1 ppb, 3% exceeded the North Carolina lead hazard level of 10 ppb, and 2% exceeded the EPA action level of 15 ppb.
TABLE 2—
Summary of First-Draw Lead Level Results by Sample Location for 4005 Child Care Facilities: North Carolina, July 2020–October 2021
| Tap Water Source Type | Median | Mean | Minimum | Maximum | 90th Percentile | CV | Parts per Billion | No. Samples | ||
| % > 1 | % > 10 | % > 15 | ||||||||
| Kitchen/cafeteria/food preparation sink | 0.4 | 2.8 | < 0.1 | 3 930.0 | 3.4 | 15.9 | 30 | 4 | 2 | 9 685 |
| Water fountain | 0.2 | 2.3 | < 0.1 | 1 503.0 | 2.1 | 11.0 | 19 | 3 | 2 | 5 321 |
| Classroom sink (no food preparation) | 0.3 | 1.7 | < 0.1 | 929.4 | 2.8 | 8.6 | 23 | 3 | 2 | 5 062 |
| Bathroom sink | 0.3 | 1.8 | < 0.1 | 94.0 | 2.9 | 3.6 | 25 | 4 | 2 | 1 690 |
| Playground/outside spigot | 0.2 | 8.4 | < 0.1 | 2 717.0 | 6.9 | 12.5 | 26 | 8 | 5 | 792 |
| Miscellaneous/unidentified | 0.3 | 2.4 | < 0.1 | 94.3 | 3.1 | 4.1 | 27 | 4 | 2 | 203 |
| Water bottle filler | 0.1 | 0.2 | < 0.1 | 3.3 | 0.6 | 2.0 | 7 | 0 | 0 | 71 |
| Staff/lounge sink | 0.6 | 1.3 | < 0.1 | 15.1 | 3.7 | 1.7 | 31 | 2 | 2 | 62 |
| Laundry/janitorial/utility sink | 0.6 | 10.1 | < 0.1 | 247.8 | 9.6 | 4.4 | 32 | 10 | 6 | 31 |
| Ice maker | 0.8 | 2.8 | < 0.1 | 22.0 | 7.7 | 1.9 | 47 | 5 | 5 | 19 |
| Bottled water | 0.1 | 0.1 | < 0.1 | 0.5 | 0.3 | 1.3 | 0 | 0 | 0 | 7 |
| Filtered samplesa | 0.2 | 1.8 | < 0.1 | 620 | 2.7 | 8.0 | 22 | 3 | 2 | 2 214 |
| Unfiltered samplesa | 0.3 | 2.7 | < 0.1 | 3 930 | 3.1 | 14.9 | 26 | 3 | 2 | 20 240 |
| All samples | 0.3 | 2.6 | < 0.1 | 3 930 | 3.0 | 14.7 | 25 | 3 | 2 | 22 943 |
Note. CV = coefficient of variation. Concentrations are shown in ppb. We instructed participants to list only drinking or cooking taps in the enrollment survey. If they listed taps that seemed unlikely to be used for consumption, we still analyzed the samples to err on the side of caution. When first-draw samples exceeded the North Carolina hazard level, a local or state health official collected follow-up samples. We did not include these follow-up samples in our analysis, which focused on the initial statewide testing using Environmental Protection Agency’s training, testing, and taking action guidance.
489 samples were missing designation as filtered or unfiltered.
Most facilities (93%) had at least 1 tap water source with detectable lead (n = 3712). More than half of the facilities (56%) had at least 1 sample above 1 ppb (n = 2232), 12% (n = 489) had at least 1 sample above 10 ppb, and 9% (n = 349) had at least 1 sample that exceeded 15 ppb. Median lead levels were less than 1 ppb across all sample locations (Table 2; Figure C [available as a supplement to the online version of this article at https://www.ajph.org]). Average lead levels were highest in laundry, janitorial, and utility sinks (mean = 10.1 ppb) and playground and outdoor spigots (mean = 8.4 ppb), potentially because of less frequent use of these taps.
Notably, median first-draw lead levels from kitchen, cafeteria, and food preparation sinks were greater than outdoor taps (0.4 ppb vs 0.1 ppb; Wilcoxon P ≤ .001; Figure C; Table A [available as a supplement to the online version of this article at https://www.ajph.org]) and exceeded 1 ppb at a higher rate (30% vs 26%; Table 2). Elevated lead levels were also detected in drinking water fountains, with first-draw concentrations up to 1503 ppb and 19% of fountain samples exceeding 1 ppb. Ice collected from ice makers showed the highest prevalence of lead of greater than 1 ppb (47%), although samples from ice makers were few (n = 19).
Water bottle–filling stations showed the lowest lead levels; average bottle filler concentrations were significantly lower than traditional water fountains (mean = 0.2 ppb vs 2.3 ppb; Wilcoxon P < .001; Figure D [available as a supplement to the online version of this article at https://www.ajph.org]). Filtered samples, including from all filter types, had slightly lower lead levels than did unfiltered samples on average (1.8 ppb vs 2.7 ppb; Wilcoxon P < .001; Figure E [available as a supplement to the online version of this article at https://www.ajph.org]) but were not significantly different when comparing exceedances (both filtered and unfiltered samples exceeded 10 ppb 3% of the time and 15 ppb 2% of the time).
There was high variation in first-draw lead levels across taps within facilities (median facility-wide CV for all tap types = 1; i.e., SD = mean; Table B [available as a supplement to the online version of this article at https://www.ajph.org]). Some facilities showed extreme variability across tap water sources (facility-wide CV up to 5.2; ±520% from the mean). Among specific fixture types within facilities, kitchen, cafeteria, and food preparation sinks exhibited the widest range of variability (CV median = 0.8, maximum = 4.0), followed by classroom sinks (CV median = 0.76, maximum = 3.5) and bathroom sinks (CV median = 0.68, maximum = 2.8), all of which demonstrated significantly higher median CV values than did water fountains and outdoor taps (Figure F [available as a supplement to the online version of this article at https://www.ajph.org]). Statewide, kitchen, cafeteria, and food preparation sinks exhibited the highest variability (CV value = 15.9), followed by outdoor taps (12.5) and water fountains (11.0; Table 2).
Lead Risk Across Child Care Facilities
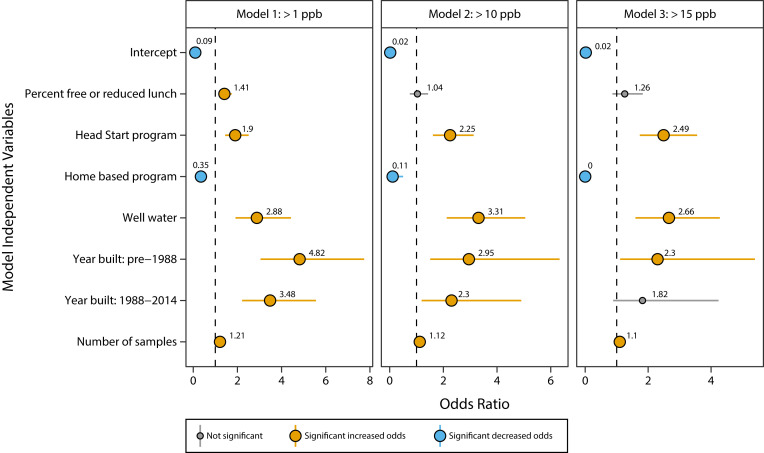
Child care facilities using well water (i.e., not connected to a public community water system) had approximately 3 times the odds of at least 1 sample exceeding all 3 lead reference levels (odds ratio [OR]1 ppb, Model 1 = 2.9; 95% confidence interval [CI] = 1.9, 4.4; OR10 ppb, Model 2 = 3.3; 95% CI = 2.1, 5.1; OR15 ppb, Model 3 = 2.7; 95% CI = 1.6, 4.3; Figure 1). Facilities built before 1988 also had significantly higher odds of at least 1 sample exceeding each reference level compared with facilities built after 2014—almost 5 times the odds of a sample exceeding 1 ppb (OR1 ppb, Model 1 = 4.8; 95% CI = 3.0, 7.7); 3 times the odds of exceeding 10 ppb (OR10 ppb, Model 2 = 3.0; 95% CI = 1.5, 6.3); and more than 2 times the odds of exceeding 15 ppb (OR15 ppb, Model 3 = 2.3; 95% CI = 1.1, 5.4). Facilities built between 1988 and 2014 exhibited slightly lower odds of lead exceedances (and lower lead concentrations overall) compared with facilities built before 1988 but were still significantly higher than those built after 2014 (Figure 1; Figure G [available as a supplement to the online version of this article at https://www.ajph.org]).
FIGURE 1—
Models of Child Care Facility Characteristics of Samples Exceeding Lead Reference Levels: North Carolina, July 2020–October 2021
Note. ppb = parts per billion. Bars indicate the 95% confidence intervals of the odds ratios.
Facilities housing Head Start programs showed significantly higher odds of at least 1 sample exceeding all 3 reference levels compared with non–Head Start program facilities, with 90% higher odds of at least 1 sample exceeding 1 ppb (OR1 ppb, Model 1 = 1.9; 95% CI = 1.4, 2.5), 2.2 times the odds of at least 1 sample exceeding 10 ppb (OR10 ppb, Model 2 = 2.2; 95% CI = 1.6, 3.1), and 2.5 times the odds of at least 1 sample exceeding 15 ppb (OR15 ppb, Model 3 = 2.5; 95% CI = 1.7, 3.6). First-draw lead concentrations were also significantly higher in Head Start program facilities than in non–Head Start program facilities (Figures G and H [available as a supplement to the online version of this article at https://www.ajph.org]). Additionally, the percentage of children receiving free and reduced cost lunch was associated with the odds of exceeding 1 ppb in at least 1 sample; facilities with 100% of children receiving free and reduced cost lunch had 41% higher odds compared with facilities with no children receiving free or reduced cost lunch (OR1 ppb, Model 1 = 1.41; 95% CI = 1.1, 1.7).
Conversely, the 192 licensed home-based facilities had significantly lower odds of any sample exceeding each reference level compared with non–home-based facilities, even after controlling for lower sample numbers, with a 65% decrease in the odds of lead above 1 ppb (OR1 ppb, Model 1 = 0.35; 95% CI = 0.21, 0.55), 89% lower odds of lead above 10 ppb (OR10 ppb, Model 2 = 0.11; 95% CI = 0.006, 0.5), and almost 100% lower odds of any samples above 15 ppb (OR15 ppb, Model 3 = 4.3 × 10−7; 95% CI = 0, 2 × 10−8). Each additional sample collected per facility increased the odds of a lead exceedance above any reference level by 10% to 20%.
Meanwhile, the proportions of non-White and subsidized children in each facility, the facility’s location in US Department of Housing and Urban Development opportunity zones, building ownership, and whether the center was located in a school building were not significant factors in any models.
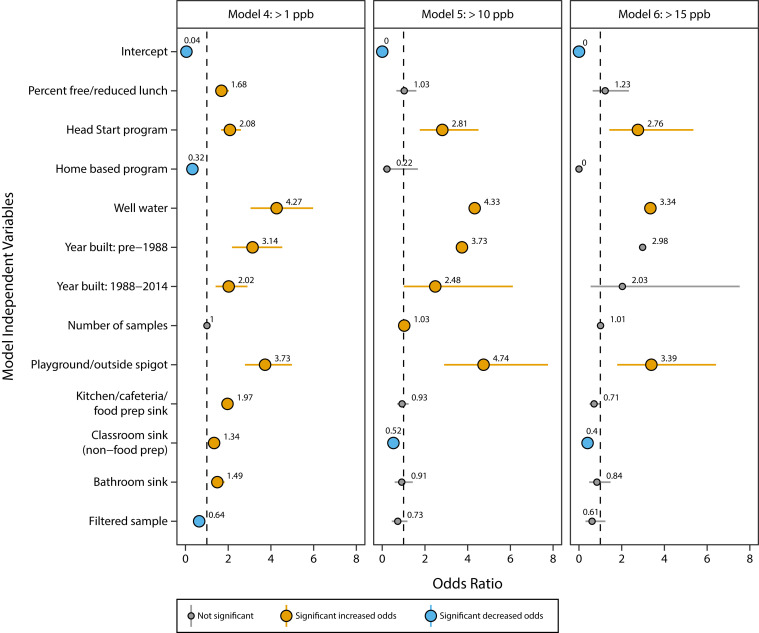
Lead Risk Among Individual Taps
Outside or playground samples exhibited the greatest risk of exceeding all 3 reference levels, with 3.7 times the odds of exceeding 1 ppb (OR1 ppb, Model 4 = 3.7; 95% CI = 2.8, 5.0), 4.7 times the odds of exceeding 10 ppb (OR10 ppb, Model 5 = 4.7; 95% CI = 2.9, 7.8), and 3.4 times the odds of exceeding 15 ppb (OR15 ppb, Model 6 = 3.4; 95% CI = 1.8, 6.4) compared with drinking fountains (Figure 2). Kitchen and other food preparation sinks, classroom sinks, and bathroom sinks were also all associated with significantly higher odds of exceeding 1 ppb compared with fountains (kitchen, cafeteria, and food preparation: OR1 ppb, Model 4 = 2.0; 95% CI = 1.7, 2.2; classrooms: OR1 ppb, Model 4 = 1.3; 95% CI = 1.1, 1.6; bathrooms: OR1 ppb, Model 4 = 1.5; 95% CI = 1.2, 1.8) but showed lower odds of exceeding 10 ppb or 15 ppb. Samples from filtered fountains or faucets had 36% lower odds of exceeding 1 ppb (OR1 ppb, Model 4 = 0.64; 95% CI = 0.52, 0.78) but were not significantly different from unfiltered samples in the odds of exceeding 10 ppb and 15 ppb.
FIGURE 2—
Models of Tap Water Source Characteristics of Samples Exceeding Lead Reference Levels: North Carolina, July 2020–October 2021
Note. Bars indicate the 95% confidence intervals of the odds ratios.
DISCUSSION
Our statewide lead-testing program reveals that detectable lead in drinking and cooking water is common in licensed child care facilities across North Carolina and varies in concentration among taps. One of every 4 taps exceeded the 1 ppb AAP reference level, 3 of every 100 taps exceeded the 10 ppb North Carolina lead hazard level, and 2 of every 100 taps exceeded the 15 ppb Lead and Copper Rule treatment–based action level. As there is no safe level of lead exposure, it is important to note that all participants received recommendations to practice “no-cost clean water habits” or low-cost solutions to take action even when findings were nondetectable or below the 1 ppb AAP reference level.
Facility-Level Lead Risk Factors
The child care facility-level factors associated with the highest lead risk in this study (i.e., any sample exceeding 10 ppb or 15 ppb) were reliance on well water, the year the facility was built, and status as a Head Start program. Facilities that collected more drinking and cooking samples (a possible proxy for building size) also had a slightly higher risk.
Well water may be an important factor because of corrosive groundwater conditions and facilities’ lack of corrosion control treatment or poorly optimized corrosion control of wells.20 Facilities relying on well water may be connected to unregulated private wells or classified as nontransient, noncommunity water systems.21 The latter are required to perform periodic lead testing under the Lead and Copper Rule and to implement corrosion control treatment when levels are elevated. However, these treatment processes can be difficult to optimize and maintain for very small systems,22 and research shows that elevated lead levels can still occur in schools and facilities with building-wide corrosion control.10 For facilities with private wells, no regular testing or treatment requirements exist, meaning that lead risks from the combination of legacy plumbing and corrosive groundwater may not be identified. Previous research showing that private well water is also an important risk factor for childhood lead exposure in household settings supports this finding.23
Building age is also a known risk factor for elevated water lead levels because of legacy lead-bearing plumbing components in older buildings.24 In our study, first-draw lead concentrations were significantly greater in facilities built before 2014, with facilities built before 1988 exhibiting the highest risk. Carter et al. have also observed the effect of building age on lead concentrations, with newer facilities demonstrating lower risk.10 These results highlight the incremental effect of legislation to control lead in drinking water and the need for facilities to update old faucets and fixtures to comply with more stringent plumbing requirements.19 Under corrosive conditions, however, even new “lead-free” components may still leach some lead.14
Head Start facilities, federally funded programs that are free to low-income families, also had significantly higher risk of at least 1 drinking or cooking tap water source exceeding each of the tested reference levels (1 ppb, 10 ppb, or 15 ppb). The reasons for this finding merit further investigation, but these facilities may be disproportionately located in underserved communities with fewer resources to make facility improvements. Indeed, Head Start facilities were significantly associated with opportunity zones in our data set (χ2 = 123.19; P ≤ .001), with 20% of all Head Start facilities versus only 11% of non–Head Start facilities located in opportunity zones. Head Start facilities also served significantly higher proportions of children receiving free and reduced cost lunch and of non-White children (Figure A), which may represent the communities where they are located. Given that many child care facilities already struggle to make ends meet, with 21% of North Carolina facilities recently reporting a risk of closing in 6 months,25 Head Start facilities may not have the resources to effectively identify or mitigate potential lead risks, highlighting persistent environmental justice and racial equity concerns associated with potential early childhood lead exposure.26,27
Meanwhile, home-based facilities had a lower risk of lead exceeding each of the reference levels. The lower risk at home-based facilities was also observed in our pilot study12 and may be associated with fewer lead sources in piping and plumbing (and fewer taps in general) compared with larger buildings such as schools, churches, and other commercial buildings, where facilities may lease space.28 Additionally, home-based facilities may have lower lead levels because of more frequent water use and shorter stagnation times, thus reducing the amount of lead that may accumulate in water from pipes and fixtures.
Tap Water Source–Level Lead Risk Factors
As in our pilot study, we found that different taps within the same child care facility may exhibit highly variable lead results.12 Although facility-wide variation (median CV = 1.0; range = 0–5.2) was slightly lower than that reported for 1094 Massachusetts schools (median CV = 1.5; range = 0–12)29—indicating that child care facilities may have lower variation in first-draw lead results than do schools because of smaller building size and fewer taps—we still identified wide variability between taps. Kitchen, cafeteria, and food preparation sinks, which had lead levels of up to 3930 ppb, exhibited the highest facility-wide and statewide variability of any taps. Additionally, although water fountains had lower facility-wide variability, they had extremely high variability across the state. Fountains were also significantly less likely to exceed 1 ppb than were kitchen, cafeteria, and food preparation; classroom; and bathroom sinks but more likely to exceed 10 ppb and 15 ppb. The inconsistent presence of leaded water coolers (banned in 1988) in some buildings may account for some variability among fountains.
Our results overall indicate that testing all drinking and cooking taps is necessary. The proposed Lead and Copper Rule revisions mandate sampling only 5 locations in schools and 2 locations in child care centers8 and may lead to misclassifications of buildings as “low-risk” overall while failing to detect individual high-risk faucets. A recent analysis of the 5-sample approach for assessing lead risk in schools successfully classified schools as having a 90th percentile lead level above or below 10 ppb overall,29 but policies designed to classify risk at the building level rather than the tap water source level are unlikely to eliminate lead exposure in school and child care settings, given such wide variability between taps. Research suggests that exposures from critical taps in schools and child care facilities could pose a health risk for children, even when building-wide levels are low.12,28,30 Other states and lead-sampling programs should test every drinking and cooking tap water source in child care and school settings.
Finally, although there was a significant difference in first-draw lead concentrations between filtered and unfiltered taps (Wilcoxon test P ≤ .001; Figure E), the small effect size (only a 0.1 ppb difference in median concentrations; Table 2) demonstrates that many filter systems and maintenance regimens currently in place are not adequate for removing lead risks. We detected lead levels of up to 620 ppb in filtered samples, with 22% exceeding 1 ppb. Point-of-use filters certified for lead removal according to protocols set by NSF International and the American National Standards Institute have been shown to be highly effective when properly maintained,31–33 but facilities may rely on a wide range of filter types, which may not be certified to reduce lead and may have highly variable maintenance routines. If filter programs are to be effective for child care facilities at home-based centers, stand-alone centers, and schools, strict protocols and policies need to be enforced for certified filter products and routine maintenance.
Public Health Implications
Our findings indicate that children enrolled in US child care facilities may be at risk for lead exposure from tap water. The complex nature of lead release from piping and plumbing, including both “near” (e.g., faucet fixtures) and “distant” (e.g., lead service lines) sources, prevents precise lead exposure estimates from first-draw samples alone;34 however, as a conservative estimate, the prevalence of facilities with first-draw lead levels above the 10 ppb North Carolina lead hazard level (12%) in our study suggests that, without appropriate mitigation, up to 25 000 of approximately 213 000 children could be exposed to lead from higher-risk taps (e.g., at or above the North Carolina hazard level) while learning and playing at licensed North Carolina child care facilities.7
Our Clean Water for Carolina Kids program aims to identify, communicate, and facilitate actions to eliminate water-related lead risks across North Carolina. Much needed resources to help child care centers and schools expand lead testing and conduct mitigation are also pending.15,35 Additionally, targeted educational training that overviews the importance of lead in water testing and mitigation is planned. These efforts ensure that infrastructure improvements are made in conjunction with updated protocols (e.g., designating specific taps for drinking) and behavioral modifications (e.g., regularly flushing water, maintaining filters, and using cold water for formula preparation). To continue reducing early childhood exposure to lead across the United States, scientifically rigorous and successful testing initiatives, comprehensive water infrastructure improvements, and integrated educational investments are necessary to mitigate lead at the tap water source.
ACKNOWLEDGMENTS
The authors would like to thank the US Environmental Protection Agency for providing a federal WIIN grant to conduct this statewide program. Funding for the initial round of statewide testing was provided by the North Carolina Department of Health and Human Services and its contractor for this work, RTI International (North Carolina requisition no. RQ22590792). The Clean Water for Carolina Kids pilot study and program was developed with an RTI International internal research and development grant.
The effectiveness and success of this program is a testament to the power of partnerships and possibilities when we unite in the effort to protect children’s health. The authors acknowledge the invaluable contributions of the North Carolina Department of Health and Human Services (DHHS) regional environmental health specialists W. David Brown, Brenda Bass, Kimly Blount, Robert Hunt, Tonya Zimmerman, Robert Pearsall, Alan Huneycutt, Barrette Gregory, Carissa Moore, and Donna Gilbird, who conducted follow-up onsite visits and sample collection at child care facilities that had 1 or more taps exceeding the applicable North Carolina hazard level. We would also like to thank the leadership at North Carolina DHHS, including Larry Michael and Mark Benton, for supporting this statewide partnership. The North Carolina Division of Child Development and Early Education provided timely and critical communication and notification support, including Ariel Ford, Arlette Lambert, Lorie Pugh, Andrea Lewis, Mandy Holland, and Kristi Snuggs. NC Child, North Carolina’s nonprofit dedicated to children, including Vikki Crouse, Fawn Pattinson, and Tom Vitaglione, also provided useful education about the importance of lead testing to child care groups and parents. Nancy Lauer and Michelle Nowlin at the Duke Environmental Law and Policy Clinic, along with their clinic students, provided legal context and research to support the statewide lead-testing rule and reduction of the North Carolina lead hazard level. We also acknowledge the following key RTI staff for their contributions to the project: Nunzio Landi (graphics), Lindsey Suggs (corporate communications), Culton Cobey (corporate communications), and Andrew Francis (programming). The extent of this effort would not have been possible without the thousands of child care center and school administrators who enrolled as participatory scientists and actively participated in training, testing, telling others, and taking action, as well as parents and staff who helped to support the program.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study did not include research on human participants. The Environmental Protection Agency approved the program work plan and all related quality documents and protocols before work initiation.
REFERENCES
- 1.Dignam T, Kaufmann RB, LeStourgeon L, Brown MJ. Control of lead sources in the United States, 1970–2017: public health progress and current challenges to eliminating lead exposure. J Public Health Manag Pract. 2019;25(suppl 1):S13–S22. doi: 10.1097/PHH.0000000000000889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canfield RL, Henderson CR, Jr, Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. Intellectual impairment in children with blood lead concentrations below 10 µg per deciliter. N Engl J Med. 2003;348(16):1517–1526. doi: 10.1056/NEJMoa022848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Agency for Toxic Substances and Disease Registry. Toxicological Profile for Lead. 2020. https://www.atsdr.cdc.gov/toxprofiles/tp13.pdf [PubMed]
- 5.Environmental Protection Agency. 2020. https://trumpadministration.archives.performance.gov/EPA/FY2020_september_Reduce_childhood_lead_exposures_and_associated_health_impacts.pdf
- 6.Environmental Protection Agency. SDWIS federal reports search. 2022. https://sdwis.epa.gov/ords/sfdw_pub/f?p=108:200
- 7.North Carolina Department of Health and Human Services, Division of Child Development and Early Education. 2022. https://ncchildcare.ncdhhs.gov/County/Child-Care-Snapshot/Child-Care-Statistical-Report
- 8.Environmental Protection Agency. National primary drinking water regulations: proposed Lead and Copper Rule revisions. Fed Regist. 2019;84(219):61684–61774. [Google Scholar]
- 9.Massey AR, Steele JE. Lead in drinking water: sampling in primary schools and preschools in south central Kansas. J Environ Health. 2012;74(7):16–20. [PubMed] [Google Scholar]
- 10.Carter JA, Erhardt RJ, Jones BT, Donati GL. Survey of lead in drinking water from schools and child care centers operating as public water suppliers in North Carolina, USA: implications for future legislation. Environ Sci Technol. 2020;54(22):14152–14160. doi: 10.1021/acs.est.0c04316. [DOI] [PubMed] [Google Scholar]
- 11.Stanbrough E, McCormick L, Barrett J, Barnett MO. A critical opportunity: detecting and reducing lead in drinking water at child care facilities. Environ Res. 2022;207:112140. doi: 10.1016/j.envres.2021.112140. [DOI] [PubMed] [Google Scholar]
- 12.Redmon JH, Levine KE, Aceituno AM, Litzenberger K, Gibson JM. Lead in drinking water at North Carolina childcare centers: piloting a citizen science-based testing strategy. Environ Res. 2020;183:109126. doi: 10.1016/j.envres.2020.109126. [DOI] [PubMed] [Google Scholar]
- 13.North Carolina Department of Health and Human Services. 2019. https://cph.dph.ncdhhs.gov/Rules/EnvHealth/15A_NCAC_18A.2816.htm#:∼:text=15A%20NCAC%2018A%20.-,2816%3A%20Lead%20Poisoning%20Hazards%20in%20Child%20Care%20Centers,above%20the%20lead%20hazard%20level
- 14.Parks J, Pieper KJ, Katner A, Tang M, Edwards M. Potential challenges meeting the American Academy of Pediatrics’ lead in school drinking water goal of 1 μg/L. Corrosion. 2018;74(8):914–917. doi: 10.5006/2770. [DOI] [Google Scholar]
- 15.Environmental Protection Agency. 3Ts for reducing lead in drinking water in schools: a training, testing, and taking action approach. 2022. https://www.epa.gov/ground-water-and-drinking-water/3ts-reducing-lead-drinking-water
- 16.Environmental Protection Agency. 2022. https://www.epa.gov/dwreginfo/information-about-public-water-systems
- 17.Council on Environmental Health. Prevention of childhood lead toxicity. Pediatrics. 2016;138(1):e20161493. doi: 10.1542/peds.2016-1493. [DOI] [PubMed] [Google Scholar]
- 18.North Carolina House Bill 272, Session Law 2021-69. 2021.
- 19.Redmon JH, Gibson JM, Woodward KP, Aceituno AM, Levine KE. Safeguarding children’s health: time to enact a health-based standard and comprehensive testing, mitigation, and communication protocol for lead in drinking water. N C Med J. 2018;79(5):313–317. doi: 10.18043/ncm.79.5.313. [DOI] [PubMed] [Google Scholar]
- 20.Reduction of Lead in Drinking Water Act, 124 Stat. 2011.
- 21.Pieper KJ, Krometis LA, Gallagher DL, Benham BL, Edwards M. Incidence of waterborne lead in private drinking water systems in Virginia. J Water Health. 2015;13(3):897–908. doi: 10.2166/wh.2015.275. [DOI] [PubMed] [Google Scholar]
- 22.Environmental Protection Agency. Optimal Corrosion Control Treatment Evaluation Technical Recommendations for Primacy Agencies and Public Water Systems. 2022. https://www.epa.gov/sites/default/files/2019-07/documents/occtmarch2016updated.pdf
- 23.Gibson JM, Fisher M, Clonch A, MacDonald JM, Cook PJ. Children drinking private well water have higher blood lead than those with city water. Proc Natl Acad Sci U S A. 2020;117(29):16898–16907. doi: 10.1073/pnas.2002729117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rabin R. The lead industry and lead water pipes “A Modest Campaign.”. Am J Public Health. 2008;98(9):1584–1592. doi: 10.2105/AJPH.2007.113555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bragg M.2022. https://www.wcnc.com/article/news/verify/verify-yes-child-care-facilities-north-carolina-struggling-stay-open/275-e767c9ce-bca3-4cc2-a48d-baf7a1e50c09
- 26.Yeter D, Banks EC, Aschner M. Disparity in risk factor severity for early childhood blood lead among predominantly African-American Black children: the 1999 to 2010 US NHANES. Int J Environ Res Public Health. 2020;17(5):1552. doi: 10.3390/ijerph17051552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitehead LS, Buchanan SD. Childhood lead poisoning: a perpetual environmental justice issue? J Public Health Manag Pract. 2019;25(suppl 1):S115–S120. doi: 10.1097/PHH.0000000000000891. [DOI] [PubMed] [Google Scholar]
- 28.Doré E, Deshommes E, Andrews RC, Nour S, Prévost M. Sampling in schools and large institutional buildings: implications for regulations, exposure and management of lead and copper. Water Res. 2018;140:110–122. doi: 10.1016/j.watres.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 29.Rome M, Estes-Smargiassi S, Masters SV, et al. Using the Lead and Copper Rule revisions five-sample approach to identify schools with increased lead in drinking water risks. Environ Sci Technol Lett. 2022;99(1):84–89. doi: 10.1021/acs.estlett.1c00845. [DOI] [Google Scholar]
- 30.Deshommes E, Andrews RC, Gagnon G, et al. Evaluation of exposure to lead from drinking water in large buildings. Water Res. 2016;99:46–55. doi: 10.1016/j.watres.2016.04.050. [DOI] [PubMed] [Google Scholar]
- 31.Mulhern R, MacDonald Gibson J. Under-Sink Activated Carbon Water Filters Effectively Remove Lead from Private Well Water for over Six Months. Water. 2020;12(12):3584. doi: 10.3390/w12123584. [DOI] [Google Scholar]
- 32.Deshommes E, Nour S, Richer B, Cartier C, Prévost M. POU devices in large buildings: Lead removal and water quality. J Am Water Works Assoc. 2012;104(4):E282–E297. [Google Scholar]
- 33.International RTI. 2022. https://www.rti.org/brochures/water-filters-certified-remove-lead-drinking-water-and-cooking-water-clean-water-carolina
- 34.Lytle DA, Formal C, Cahalan K, Muhlen C, Triantafyllidou S. The impact of sampling approach and daily water usage on lead levels measured at the tap. Water Res. 2021;197:117071. doi: 10.1016/j.watres.2021.117071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wagner A.2021.