Abstract
Objective
To synthesize the current evidence on the incidence of running-related injuries (RRIs) and their association with training parameters (distance, duration, frequency, intensity), as well as recent changes in training parameters.
Data Sources
Searches were conducted in MEDLINE/Ovid, CINAHL, Embase, and SPORTDiscus from their inception through July 7, 2020.
Study Selection
Included articles had to report prospective data on RRIs and training parameters or any changes in parameters and be published in English or French. Two reviewers independently screened the titles, abstracts, and full texts.
Data Extraction
Two independent raters performed data extraction and quality assessment using QualSyst, a quality appraisal tool.
Data Synthesis
A total of 36 articles that involved 23 047 runners were included. Overall, 6043 runners (26.2%) sustained an RRI (incidence range = 8.8%–91.3%). The incidence of RRI was 14.9% in novice runners (range = 9.4%–94.9%), 26.1% in recreational runners (range = 17.9%–79.3%), and 62.6% in competitive runners (range = 52.6%–91.3%). The 3 most frequently injured body parts were the knee (25.8%), foot/ankle (24.4%), and lower leg (24.4%). Overall, evidence about the association between weekly running distance, duration, frequency, intensity, or specific changes in training parameters and the onset of RRIs was conflicting.
Conclusions
Despite high rates of RRIs, current evidence does not consistently link RRIs with specific training parameters or recent changes in training parameters. Therefore, caution should be taken when recommending optimal parameters or progressions. Given the multifactorial nature of RRIs, future studies also need to consider the interactions between training parameters as well as psychosocial, hormonal, lifestyle, and recovery outcomes to better understand the onset of RRIs.
Keywords: sports medicine, prevention, incidence, exercise
Key Points
Evidence on the association between running distance, duration, frequency, or intensity or recent changes in these parameters and the onset of lower limb running-related injuries is conflicting.
No universal recommendations on training parameters or progressions can be issued based on the current evidence; the popular “10% rule” for increasing weekly distance is not justified.
The lack of reporting guidelines for running-related injuries contributes to high heterogeneity in the definition of injury, runner profiles, and follow-up periods.
Running is a popular activity due to the health and fitness benefits it provides. However, because running imposes forces of up to 3 times body weight at each step,1,2 it is commonly associated with lower limb overuse injuries.3 The yearly incidence of running-related injuries (RRIs) can affect 85% of all populations of runners (novice, recreational, competitive).4–6 In a consensus article published in 2015, an RRI was defined as “running-related (training or competition) musculoskeletal pain in the lower limbs that causes a restriction on or stoppage of running (distance, speed, duration, or training) for at least 7 days or 3 consecutive scheduled training sessions or that requires the runner to consult a physician or other health professional.”7 Running-related injuries may occur when repetitive stress is applied to a joint, muscle, tendon, or bone beyond its maximum tolerance to mechanical stress.2 Although mechanical (eg, biomechanics) and nonmechanical (eg, sleep) factors could play roles in the onset of an RRI,8 researchers2,8 have hypothesized that runners who sustain RRIs exceeded their limit of running distance or intensity (ie, training load) or both over 1 or more training sessions, resulting in injury instead of tissue adaptation.
The authors5,6,9,10 of previous literature reviews have investigated the role of training parameters such as distance, duration, frequency, and intensity, as well as recent changes in training parameters, in the onset of RRIs. Despite identifying greater weekly running distance as a risk factor for the onset of RRIs among male runners, van Gent et al6 found in their 2007 systematic review that a recent increase in weekly running distance was a protective factor against knee injuries. However, only limited evidence suggested that other training parameters, such as greater training frequency (males), greater training distance (females), a recent increase in training days per week, and a recent increase in distance per week, were risk factors for RRIs.6 In a 2012 review,5 conflicting results reflected the relationship between running distance, duration, frequency, and intensity and the onset of RRIs. Heterogeneity in the determinants of injuries among the included studies precluded the identification of any association between training parameters and RRIs. Finally, in 2018, Damsted et al11 observed very limited evidence (from only 4 articles) that sudden changes in training loads were associated with an increased risk of RRIs. Considering that new evidence has been published since these previous literature searches, an updated and more comprehensive review of RRI incidence and its association with training parameters is warranted. This could change the recommendations provided to sports medicine practitioners, exercise professionals, and runners regarding optimal training parameters to help reduce the injury risk.
The aim of our systematic review was to synthesize the current prospective evidence on the incidence of lower limb RRIs and explore the relationship between their onset and training parameters (distance, duration, frequency, intensity) as well as recent changes in training parameters.
METHODS
This systematic review was registered in PROSPERO (No. CRD42018112913) and is reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 guidelines.12
Literature Search
We conducted bibliographical searches in 4 databases (MEDLINE/Ovid, CINAHL, Embase, SPORTDiscus) in collaboration with experienced research librarians. All databases were searched from their inception to July 7, 2020, for 3 concepts: (1) running; (2) musculoskeletal lower limb injury, pain, or pathology; and (3) training parameters. The terminology used for the search strategy is presented in the Supplemental Table (see Supplemental Table, available online at http://dx.doi.org/10.4085/1062-6050-0195.21.S1). The search strategy was tailored for each database, using the appropriate truncation and medical subject heading.
Study Selection
To be included in the review, articles had to (1) be published in English or French, (2) involve humans engaging in running (defined by the authors as novice, recreational, competitive, or mixed cohorts), (3) include any running program (structured or unstructured), (4) report on prospective cohort studies or randomized clinical trials (RCTs), and (5) provide data on RRIs and training parameters (distance, duration, frequency, intensity) or any measure of change in training parameters. Systematic reviews, conference abstracts, and articles from the gray literature were excluded. No restrictions were placed on age, sex, or gender.
After conducting the database search, we removed duplicate articles. All articles were then independently screened for eligibility by 2 blinded reviewers. The same reviewers independently screened the publications' titles and abstracts to identify research eligible for full-text review. Thereafter, eligible articles were retrieved in full text, which was independently scrutinized by 2 raters (A.F., J.F.E.) to confirm inclusion. In case of disagreement about final inclusion, a third reviewer (J.S.R.) was available to make the decision. The bibliographical references of the retrieved studies were also searched to identify additional relevant publications.
Data Extraction
A first reader extracted the data from all included studies before a second reader corroborated and completed the extraction, if necessary. Data were extracted according to a predefined standardized form that consisted of authors, study design, population, methods, definition of RRI, running program, study variables (training parameters, changes in training parameters), outcomes (incidence of RRIs), results, and conclusions.
Critical Appraisal
We assessed the methodological quality and risk of bias of included studies using a structured and validated quality appraisal tool, the Quality Assessment for Evaluating Primary Research Studies (QualSyst).13 The evaluation checklist contains 14 items pertaining to the study question and design, outcome measurements, interventions, analyses, results, and conclusions. The items were scored depending on the degree to which the specific criteria were met (yes = 2, partial = 1, no = 0). Items not applicable to a particular study design were marked N/A (not applicable) and excluded from the total score.
To ensure consistency in scoring, all team members involved in critical appraisal (A.F., F.D., J.S.R.) met after independently assessing one of the included studies. Next, 2 raters (A.F., F.D.) independently evaluated each study using the QualSyst criteria checklist. A preconsensus, interrater reliability score using an intraclass correlation coefficient (ICC) with 95% CI was calculated for the total quality score. The ratings were then compared to determine the scoring consensus between raters. When consensus was not reached, a third rater (J.S.R.) was available to contribute to the final decision. The following classifications were used to categorize methodological quality: high quality (HQ) > 80.0%; good quality (GQ) = 65.0% to 80.0%; moderate quality (MQ) = 50.0% to 64.9%; and low quality (LQ) < 50.0%.14
Data Analysis
We conducted a qualitative review of the evidence. The level of evidence was adapted from the recommendations of the Cochrane Group Collaboration15 and classified as strong, moderate, limited, very limited, or conflicting (Table 1) after we considered the following domains: imprecision (number of studies and participants), risk of bias (methodological quality), indirectness (methodological and outcomes similarities), and inconsistency (direction of results). To obtain quantitative data about the incidence of RRIs, the total sample size and number of injured runners in each study were extracted. A weighted average (%) was calculated for each category of runners (novice, recreational, competitive, mixed) by dividing the number of injured runners by the total number of runners.
Table 1.
Level of Evidence
| Level of Evidence |
Definition |
| Strong evidence | Multiple HQ studies with consistent results, regardless of methodological heterogeneity |
| Moderate evidence | Multiple studies, including at least 1 HQ study or multiple MQ or GQ studies or multiple LQ studies, homogeneous methods; always providing consistent results |
| Limited evidence | Multiple studies, with heterogeneous methods or inconsistent results (or both) or a single GQ or higher study |
| Very limited evidence | Results from a single LQ or MQ study |
| Conflicting evidence | Multiple studies regardless of the methodological quality, with inconsistent results |
Abbreviations: GQ, good quality; HQ, high quality; LQ, low quality; MQ, moderate quality.
RESULTS
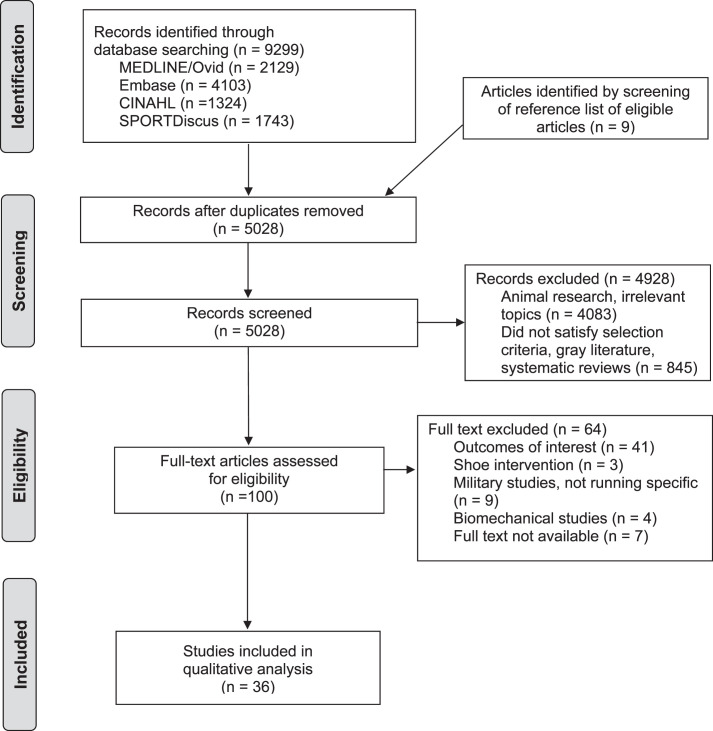
The search strategy identified a total of 9299 articles. After removing duplicates and screening the titles and abstracts, we identified 91 articles eligible for full-text review. Nine additional articles were included after the selected studies' reference lists were hand searched. After full-text screening, 36 studies were included in this review (Figure).
Figure.
Flow diagram of the article selection process presented according to 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.12
Characteristics of the Studies
Of the 36 included studies, 33 were prospective cohort studies and 3 were RCTs. In all, they involved 23 047 runners (44% females) aged 17 years and older. Seven studies were conducted specifically with novice runners (n = 3315 participants, 63% females),16–22 14 with recreational runners (n = 7905 participants, 44% females),23–35,50 5 with competitive runners (n = 414 participants, 48% females),36–40 and 10 with runners of mixed levels of ability and experience (n = 11 430 participants, 39% females; Table 2).4,41–49
Table 2.
Included Studies, Training Parameters, and Incidence of Injuries Continued on Next Page
| Authors |
Study Design |
Follow-Up |
Sample Size (% Females) |
Type of Runners |
Mean Age ± SD, y |
Age Range |
Running Program |
Reported RRI Incidence |
Association Between RRIs and Training Parameters |
Recent Changes in Training Parameters |
| Becker et al40 | Prospective | 24 mo | n = 24 (37.5%) | Competitive | 19 ± 1.2 | Usual training routine of the team | 75.0% of runners (18/24) reported RRIs | Running distance: No difference in weekly volume between injured (52 ± 21.8 km) and uninjured (54 ± 24.1 km; P = .684) runners | ||
| Begizew et al37 | Prospective | 10 mo | n = 229 (52.8%) | Competitive | Not available | 17–26 y: n = 205; >26 y: n = 24 | Self-selected running program | 62.4% (143/229); 3.54 RRIs/1000 h of running | Running distance: 40–50 km/wk = 99.7% ↓ risk of RRI than 60–70 km/wk (OR = 0.003, 95% CI = 0.000, 0.073; P ≤ .0001) 50–60 km/wk = 94.7% ↓ risk of RRI than 60–70 km/wk (OR = 0.053, 95% CI = 0.004, 0.728; P ≤ .028) | |
| Bovens et al16 | Prospective | 18 mo | n = 73 (13%) | Novice | Males = 35.2 ± 7.9; females = 33.5 ± 6.4 | Training program with 3 phases, each finishing with race (15, 25, and 42 km) Phase 1 = 28 wk (mean/wk = 2.7 h, 3.8 trainings, 24.1 km) Phase 2 = 23 wk (mean/wk = 3.2 h, 3.6 trainings, 34.9 km) Phase 3 = 30 wk (mean/wk = 4.0 h, 3.5 trainings, 43.6 km) | 84.9% (62/73); RRI incidence in phase 1 = 58%, phase 2 = 60%, phase 3 = 67% | Running distance: ↑ Distance related to more injuries during phases 1 (r2 = 0.36, P = .001) and 3 (r2 = 0.16, P = .015) Running duration and frequency: No analyses reported | Recent changes: Significant ↑ injury rates during phases 1–2 and 1–3. Training amount during last phase of marathon preparation ↑ injury risk (from mean distance/wk = 34.9 km to 43.6 km and mean duration = 3.2 h/wk to 4.0 h/wk) | |
| Buist et al18 | RCT | 8 or 13 wk | n = 532 (57.5%) | Novice | 39.8 ± 10.1 | GTG = <10% volume progression/wk (13 wk) STG = >10% volume progression/wk (8 wk) | GTG: 20.8% (52/250) STG: 20.3% (48/236) | Recent changes: No effect of graded “10% rule” on RRIs, compared with standard training program (P = .90) | ||
| Buist et al4 | Prospective | 8 wk | n = 629 (67.1%) | Novice, recreational | 43.7 ± 9.5 | 8-wk training program | 25.9% (163/629); 30.1 RRIs/1000 h of running | Running duration: Not associated with RRIs (P > .38) | Recent changes: Week-to-week changes in running frequency or duration were not associated with RRIs (P > .075) | |
| Buist et al17 | Prospective | 8 or 13 wk | n = 532; 486 followed running program (57.5%) | Novice | 39.8 ± 10.1 | GTG = <10% volume progression/wk (13 wk) STG = >10% volume progression/wk (8 wk) | 20.6% (100/486); 33.0 RRIs/1000 h of running | Running duration: Not associated with RRIs | ||
| Dallinga et al23 | Prospective | 3 mo | n = 706 (46.9%) | Recreational | 43.9 ± 11.6 | Usual training routine in preparation for 8- or 16-km run | 20.1% (142/706) in preparation for or during event | Running distance and duration: Not associated with RRIs Duration: OR = 1.00, 95% CI = 0.999, 1.002; Distance: OR = 1.24, 95% CI = 0.65, 2.38 | ||
| Damsted et al45 | Prospective | 14 wk | n = 508 (62.2%) | All abilities | 37 | 29–46 y | 1) Distance-based schedule 2) Pace-based schedule 3) Mixed schedule 4) Self-chosen running program (not analyzed) | 26.8% (136/508) across all running schedules: 24.2% (40/165), distance-based running schedule; 19.4% (14/72), pace-based running schedule; 30.3% (82/271), mixed running schedule | Running distance and intensity: Tendency (nonsignificant) for fewer injuries among runners with running distance >15 km/wk (RD = −11.3%, 95% CI = −27.2, 4.6), high pace (RD = −17.4%, 95% CI = −39.0%, 4.5%), or combination (RD = −8.1%, 95% CI = −22.3%, 6.1%) | |
| Damsted et al44 | Prospective | 14 wk | n = 261 (60.2%) | All abilities | 36 | 27–45 y | 1) Distance-based schedule 2) Pace-based schedule | 21.5% (56/261): 24.2% (40/165) distance-based running schedule; 16.7% (16/96) pace-based running schedule | Recent changes: More runners injured when weekly running distance ↑ 20%–60% compared with ↑ ≤20% (only at 21 d, not at 56 or 91 d): RD21 days = 22.6%, 95% CI = 0.9%, 44.3%; RD56 days = 19.0%, 95% CI = −11.9%, 50.0%; RD98 days = 4.2%, 95% CI = −26.2%, 34.7% No difference between runners ↑ distance >60%: RD21 days = 5.8%, 95% CI = −8.4%, 20.1%; RD56 days = 7.8%, 95% CI = −14.0%, 29.6%; RD98 days = −4.3%, 95% CI = −27.9%, 19.3% | |
| Dijkhuis et al38 | Prospective | 24 mo | n = 23 (30.4%) | Competitive | 22.5 ± 5.7 | Individualized program designed by running coach | 91.3% (21/23) | Running duration and intensity: No associations between acute workload, chronic workload, and risk of RRI (P > .05) | Recent changes: No associations between weekly acute:chronic workload ratio and RRI risk: wk 1–2, P > .451; wk 2–3, P > .494, except for “low increase'' (P = .013); wk 3–4, P > .125 | |
| Fields et al24 | Prospective | 12 mo | n = 40 (22.5%) | Recreational | 37 | 20–40 y (n = 25); 41–60 y (n = 15) | Self-selected running program | 42.5% (17/40) | Running distance: No significant association with RRIs, despite RRIs in 80% of those running <32.2 km/wk vs 50% of those running >64.4 km/wk | |
| Fokkema et al46 | Prospective | 3 mo | n = 997 (35.0%) | All abilities | 42.2 ± 11.7 | Online running program for half-marathon or a marathon | 51.3% (511/997) | Running distance, duration, and intensity: No associations with RRI risk Weekly distance (vs 20–32 km): <20 km: OR = 1.41, 95% CI = 0.86, 2.32; >32 km: OR = 0.97, 95% CI = 0.63, 1.50 Longest-run duration (vs 15–21 km): <15 km: OR = 1.19, 95% CI = 0.69, 2.04; >21 km: OR = 0.83, 95% CI = 0.52, 1.30 Intensity (vs 5.25–6.00 min/km): <5.25 min/km: OR = 0.68, 95% CI = 0.41, 1.11; >6.00 min/km: OR = 1.23, 95% CI = 0.77, 1.98 | ||
| Hamstra-Wright et al41 | Prospective | 18 wk | n = 113 (74.3%) | All abilities | 20–70 y | 18-wk marathon training program | 24.8% (28/113) | Running intensity: 96.4% (27/28) of runners injured in first 6 wk were doing tempo or interval runs 56.9% (37/65) of runners not injured during first 6 wk were doing tempo or interval runs; similar mileage as injured runners Tempo runs during first 6 wk ↑ RRI odds (OR = 3.96, 95% CI = 1.35, 11.61). Interval runs during first 6 wk tended to ↑ RRI odds (not significant; P = .06) | ||
| Hayes et al39 | Prospective | 3 mo | n = 97 (58.8%) | Competitive | Males = 19.0 ± 0.2, females = 19.2 ± 0.2 | Cross-country season training program from university coach | 52.6% (51/97) | Recent changes: Athletes with larger differences in running volume between regular and high-mileage weeks more likely to be injured but results not significant (P = .06) | ||
| Hespanhol Junior et al26 | Prospective | 12 wk | n = 200 (26%) | Recreational | 42.8 ± 10.5 | Self-selected running program | 31.4% (60/191): 10 RRIs per 1000 h of running | Running duration: ↑ Duration of training session associated with ↑ RRI risk (OR = 1.01, 95% CI = 1.00, 1.02) Running intensity: Inconclusive results; speed training associated with ↑ RRI risk (OR = 1.46, 95% CI = 1.02, 2.10) but interval training associated with ↓ RRI risk (OR = 0.61, 95% CI = 0.43, 0.88). | ||
| Hespanhol Junior et al25 | Prospective | 12 wk | n = 89 (23.6%) | Recreational | 44.2 ± 10.6 | Self-selected running program | 27.0% (24/89): 7.7 RRIs per 1000 h of running | Running distance, duration, frequency, intensity: No associations with RRI risk Distance: P = .51; Duration: P = .25; Frequency: P = .65; Intensity: P = .68 | ||
| Hootman et al47 | Prospective | 1–5 y | n = 3090 (19.7%) | Novice, Experienced | 20–85 y | Run/walk/jog program, 1–5 y | 39.1% (1207/3090) during 5-y recall period, 17.4% (481/2762) during 1-y recall period | Running distance: ↑ Run/walk/jog distance (>32.2 km/wk) associated with greater RRI risk during 5-y recall period; men's HR = 1.66, 95% CI = 1.43, 1.94; women's HR = 2.08, 95% CI = 1.45, 2.98; no association during 1-y recall period Running frequency: No associations with RRI risk during 5-y or 1-y recall periods Running intensity: No associations with RRI risk during 5-y recall period During 1-y recall period, ↓ intensity (15+ min/mile) associated with ↓ RRI risk only in men (OR = 0.51, 95% CI = 0.35, 0.74). | ||
| Jakobsen et al27 | Prospective | 12 mo | n = 41 (9.8%) | Recreational | 41.9 | Study group: endurance, hill and speed training, education; control group: no details provided | 85.7% (18/21) in study group, 65.0% (13/20) in control group RRIs/1000 h of running: study group = 7.4 during training, 30.7 during races; control group = 6.9 during training, 62.5 during races When adjusted for training time, RRI incidence similar in both groups | Running distance: ↑ RRIs in study group (P < .001), who ran more weekly distance at same pace Mean running distance (km/wk): Study group: 43.0, 95% CI = 41.6, 44.4 Control group: 33.4, 95% CI = 32.0, 34.9 | ||
| Kemler et al48 | Prospective | 3 mo | n = 4621 (41.8%) | Novice, Experienced | 34.2 | Usual training routine | 8.8% (405/4621) within 3-mo recall period: 9.5% (134/1405) of novice runners, 8.4% (271/3216) of experienced runners | Running duration: No association with injury incidence: novice mean = 14.6 h (IQR = 32.5) vs experienced mean = 30.0 h (IQR = 67.5) for similar injury rates | ||
| Kluitenberg et al19 | Prospective | 6 wk | n = 1696 (78.5%) | Novice | 43.3 ± 10.0 | 6-wk “Start to Run” program | 10.9% (159/1696) | Running duration: Running <60 min in previous 7 d protected against RRI (multivariate analysis: HR = 0.41, 95% CI = 0.20, 0.86) Running frequency: Not significantly associated with RRI but trend that running 3×/wk was more hazardous than 2×/wk (HR = 1.42, 95% CI = 0.97, 2.08). Running intensity: ↑ Intensity associated with RRI (multivariate analyses: HR = 1.28, 95% CI = 1.18, 1.40). | ||
| Lehmann et al50 | Prospective | 4 wk, 2 y in row | n = 17 (Unknown) | Experienced distance runners | 33.5 | Year 1: 103% ↑ in running volume (ITV; n = 8) Year 2: 152% ↑ in running intensity (ITI; n = 9; 7 had participated in year 1) | Only minor injuries that did not alter planned training; no details on number or type of injuries | Running distance: ITV: Average distance ↑ from 85.9 km to 174.6 km (week-to-week ↑ of 33.9%, 32.6%, and 36.8%, respectively); no more injuries than ITI, which ↑ from 61.7 km to 84.7 km (week-to-week ↑ of 1.9%, 20.0%, and 12.2%, respectively). Running intensity: ITI: Tempo pace and interval runs ↑ week-to-week from 14.7% of total training (9.0 km) to 23.7% (14.9 km), 24.6% (18.6 km), and 26.8% (22.9 km), respectively; no more injuries than ITV, which changed from 7.3% of total training (6.3 km) to 4.0% (4.6 km), 3.8% (5.4 km), and 2.0% (3.5 km), respectively | Recent changes: No change in RRI risk based on distance and intensity changes | |
| Lun et al28 | Prospective | 6 mo | n = 87 (49.4%) | Recreational | 38 | Usual training routine | 79.3% (69/87); RRI incidence/1000 h of running = 59% | Running distance: No difference in RRI incidence between uninjured (30.3 km) and injured (34.2 km) runners Running frequency: No difference between uninjured (3.8/wk) and injured (3.7/wk) runners | ||
| Lysholm et al36 | Prospective | 12 mo | n = 41; Sprinters excluded (9.8%) | Competitive | Middle-distance runners = 18.6 ± 2.4; long-distance runners = 34.5 ± 7.4 | Training with their athletic clubs | 76.9% (10/13) of middle-distance runners, 5.6 RRIs/1000 h; 57.1% (16/28) of long-distance runners, 2.5 RRIs/1000 h | Running distance: Significant correlation in long-distance runners between ↑ distance covered during given month and No. of injury days the next month (r = 0.59) | ||
| Malisoux et al34 | Prospective | 22 wk | n = 264 (26.1%) | Recreational | Single shoe (n = 116) = 40.5 ± 9.8; multiple shoes (n = 148) = 44.2 ± 8.8 | Usual training routine (at least 1x/wk) | 33.1% (87/264); 7.64 RRIs/1000 h of running | Running duration: ↑ Session duration associated with ↓ RRI risk in unadjusted model (HR = 0.963, P < .001) Running frequency: ↑ Frequency associated with ↓ RRI risk in unadjusted model (HR = 0.707, P = .002) Running intensity: ↑ Intensity not associated with RRI risk (HR = 0.873, P = .248) | ||
| Messier et al29 | Prospective | 24 mo | n = 300 (42.7%) | Recreational | Injured = 42.3 ± 9.7, uninjured = 40.0 ± 10.3 | Self-selected running program | 66.3% (199/300); 55.8% of injured runners (111/199) were injured >1x during 24-mo observation period | Running distance: No association with RRI risk (P = .16) Running intensity: No association with RRI risk (OR = 1.058; 95% CI = 0.727, 1.540; P = .20) | ||
| Nielsen et al20 | Prospective | 10 wk | n = 58 (48.3%) | Novice | 39.8 ± 9.2 | Not reported | 22.4% (13/58) | Running distance: No association with RRI risk (P = .23) | Recent changes: Not statistically significant (P = .07) but injured runners ↑ average weekly running distance by 31.6% ± 3.1%, compared with 22.1% ± 2.1% in uninjured runners Injured runners had higher weekly progression in running distance week before injury onset compared with other weeks (86% difference, 95% CI = 12.9%, 159.9%; P = .026). | |
| Nielsen et al21 | Prospective | 12 mo | n = 873 (49.5%) | Novice | 37.2 ± 10.2 | Self-selected running program | 23.1% (202/873) | Recent changes: No difference in RRI risk between different progressions in weekly distance (rolling average calculated after each running session, not cumulative average change in volume) <10%: HR = 1.00 (reference) 10%–30%: HR = 0.99, 95% CI = 0.55, 1.82 >30%: HR = 1.17, 95% CI = 0.84, 1.63 Those progressing >30% were more vulnerable to distance-related injuries compared with <10% (HR = 1.59, 95% CI = 0.96, 2.66; P = .07). | ||
| Pollock et al22 | RCT | 20 wk | Cohort 1: n = 87; 18 controls (0%) | Novice | N/A | Cohort 1, duration study: 3 d/wk for 15, 30, or 45 min; total = 20 wk | 26.0% (33/127) 33.3% (23/69); RRI reported in 20.0% (4/20), 24.0% (6/25), and 54.2% (13/24) of 15-, 30-, and 45-min groups, respectively | Running duration: ↑ Running duration (45 min/session) associated with ↑ RRI risk | ||
| Cohort 2: n = 71; 13 controls (0%) | Novice | N/A | Cohort 2, frequency study: 30-min runs 1, 3, or 5 d/wk; total = 20 wk | 17.2% (10/58); RRIs reported in 0% (0/15), 12.0% (3/25), and 38.9% (7/18) of 1, 3, and 5-d/wk groups, respectively | Running frequency: ↑ Running frequency (5×/wk) associated with ↑ RRI risk |
Table 2.
Continued From Previous Page
| Authors |
Study Design |
Follow-Up |
Sample Size (% Females) |
Type of Runners |
Mean Age ± SD, y |
Age Range |
Running Program |
Reported RRI Incidence |
Association Between RRIs and Training Parameters |
Recent Changes in Training Parameters |
| Ramskov et al30 | RCT | 24 wk | n = 839; 447 analyzed (62.1%) | Recreational | 39.1 ± 10.2 | 16-wk Running program based on progression of either running intensity (S-I) or volume (S-V); 3 runs/wk, 4-wk periodization cycle repeated ×6. Wk 1 in every cycle ↑ volume by 23% Wk 2–3: Adaptation, 0% progression Wk 4: Volume ↓ by 10% Progression/regression of running in S-I = % change in km/wk at intensity ≤88% maximal oxygen consumption | 17.9% (80/447) S-I group: 16.3% (36/221); 8/36 intensity related, 5/36 volume-related S-V group: 19.5% (44/226); 11/44 intensity related, 9/44 volume related No difference in risk of intensity or volume RRI between runners in S-I and S-V groups during 16-wk follow-up | Recent changes: No differences in overall RRI incidence between progression of distance or intensity or type of injuries sustained by each group (distance: P > .14, intensity: P > .32) | ||
| Taunton et al31 | Prospective | 13 wk | n = 844 (75.2%) | Recreational | Age by category: <30 y (16.8%), 31–49 y (59.8%), 50–55 y (13.2%), >56 y (8.8%) | 13-wk Program to complete 10-km race | 29.5% (249/844) | Running frequency: ↓ Running (only 1 d/wk) associated with ↑ RRI risk in overall cohort and female runners (OR = 3.6, 95% CI = 1.1, 12.3) but not in male runners | ||
| van der Worp et al35 | Prospective | 12 wk | n = 417 (100%) | Recreational | 38.7 ± 11.5 | Self-selected running program | 22.3% (93/417) | Running distance: Distance/wk >30 km associated with ↑RRI risk (HR = 3.28, 95% CI = 1.23, 8.75) <10 km: 28.3% (41/145) 10–20 km: 25.0% (30/120) 21–30 km: 34.8% (16/46) >30 km: 46.2% (6/13) | ||
| van Middelkoop et al32 | Prospective | 4 wk | n = 694 (0%) | Recreational | 44 ± 9.6 | Self-selected running program during 4 weeks leading up to marathon | 28.1% (195/694) | Running distance: Volume/wk <40 km protected against calf injuries (OR = 0.36, 95% CI = 0.17, 0.78) Running intensity: Consistent interval training protected against knee injuries (OR = 0.49, 95% CI = 0.26, 0.93) | ||
| van Poppel et al33 | Prospective | 12 mo | n = 3768 (39.2%) | Recreational | 42.8 ± 11.2 | Usual running routine | 21.5% of runners (811/3,768) reported RRIs: 17.5% of 5-km runners (67/250) reported RRIs; 18.7% of 10-km or 15-km runners (257/981) reported RRIs; 23.1% of half marathon runners (214/708) reported RRIs; 25.2% of marathon runners (266/762) reported RRIs | Running distance: A greater weekly distance was associated with ↓ risk of RRI (OR = 0.99, 95% CI = 0.98, 1.0) Running frequency: No association with risk of RRI (OR =1.3, 95% CI = 0.99, 1.7) Running intensity: No association with risk of RRI | ||
| Walter et al42 | Prospective | 12 mo | n = 1288 (23.5%) | Recreational, Competitive | Age by category: 14–19 y = 11.3%; 20–29 y = 21.2%; 30–39 y = 39.3%; 40–49 y = 21.0%; >50 y = 7.1% | Usual running routine | 48.1% of runners (620/1288) reported RRIs | Running distance: A greater weekly distance (over 64 km) was associated with ↑ risk of RRI (adjusted relative risk = 2.88). Relative risk in males = 2.22, 95% CI = 1.30, 3.68. Relative risk in females = 3.42, 95% CI = 1.42, 7.85. Running frequency: Running 7 d/wk was associated with significantly ↑ risk of RRI compared with 0–2 d/wk in both males (relative risk = 5.92, 95% CI = 2.49, 12.75) and females (relative risk = 5.50, 95% CI = 1.44, 17.39). Running intensity: No association with risk of RRI | ||
| Wen et al49 | Prospective | 32 wk | n = 108 (52.8%) | Novice, Recreational | 43.2 ± 9.8 | 32-wk Program leading up to marathon; organized sessions weekly; own program during week | 45.4% (49/108); 1.22 injuries/1609.3 km (95% CI = 0.97, 1.48) | Running distance: ↑ Distance associated with ↓ risk of knee RRI (relative risk = 0.901, 95% CI = 0.820, 0.991). Running duration: ↑ Training h/wk associated with ↓ overall RRIs (relative risk = 0.575, 95% CI = 0.451, 0.731), ↓ knee injuries (relative risk = 0.486, 95% CI = 0.297, 0.795), ↓ foot injuries (relative risk = 0.206, 95% CI = 0.096, 0.444) | ||
| Winter et al43 | Prospective | 12 mo | n = 76 (40.8%) | Recreational, Competitive | Injured = 40.7 ± 12.5; uninjured = 44.8 ± 12.5 | Self-selected running program | 51.3% (39/76) | Running distance: ↑ Average distance/wk in injured vs uninjured male runners (r = 0.32, P = .046); no difference in female runners | Recent changes: Injured male (n = 20; 91%) and female (n = 10; 59%) runners ↑ distance/wk by >10% between consecutive wk at least 1x in 4 wk before injury. Of 18 injured male runners who ↑ running distance by >10% 1x, 11 (61%) ↑ by >30%, and 5 (28%) ↑ by >50%. Of 9 injured female runners who ↑ running distance by >10% 1x, 5 (56%) ↑ by >30% and 3 (33%) ↑ by >50%. |
Abbreviations: GTG, graded training group; HR, hazard ratio; ITV, increased training volume; ITI, increased tempo pace and interval runs; IQR, interquartile range; OR, odds ratio; RCT, randomized clinical trial; RD, risk difference; RRI, running-related injury; STG, standard training group.
Methodological Quality
Methodological quality scores ranged from 27.3% to 96.2% (Table 3). On average, the studies were of high methodological quality, with a median score of 86.4% (interquartile range [IQR] = 19.3%). Twenty-two studies were classified as high quality, 5 as good quality, 5 as moderate quality, and 4 as low quality. The preconsensus, interrater reliability score for quality assessment was excellent with an ICC of 0.97 (95% CI = 0.95, 0.99).
Table 3.
Methodological Quality of Included Studies (Consensus Score)a
| Authors |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
11 |
12 |
13 |
14 |
Pointsb |
Total Score (%) |
Methodological Quality |
| Becker et al40 | Y | Y | P | Y | N/A | N/A | N/A | Y | N | Y | Y | P | P | P | 16/22 | 72.7 | GQ |
| Begizew et al37 | Y | P | Y | Y | N/A | N/A | N/A | P | P | Y | Y | Y | Y | Y | 19/22 | 86.4 | HQ |
| Bovens et al16 | Y | P | P | Y | N/A | N/A | N/A | P | N | P | N | N | Y | Y | 12/22 | 59.1 | MQ |
| Buist et al18 | Y | Y | Y | Y | Y | N | N/A | P | Y | Y | Y | Y | Y | Y | 23/26 | 88.5 | HQ |
| Buist et al4 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 21/22 | 95.5 | HQ |
| Buist et al17 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 21/22 | 95.5 | HQ |
| Dallinga et al23 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | P | Y | P | 19/22 | 86.4 | HQ |
| Damsted et al45 | Y | P | Y | Y | N/A | N/A | N/A | P | P | Y | Y | Y | Y | Y | 19/22 | 86.4 | HQ |
| Damsted et al44 | Y | Y | P | Y | N/A | N/A | N/A | P | P | Y | Y | Y | Y | Y | 19/22 | 86.4 | HQ |
| Dijkhuis et al38 | Y | Y | P | Y | N/A | N/A | N/A | P | N | Y | Y | N/A | Y | P | 15/20 | 75.0 | GQ |
| Fields et al24 | Y | P | P | P | N/A | N/A | N/A | P | P | P | N | N | P | Y | 11/22 | 50.0 | LQ |
| Fokkema et al46 | Y | P | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| Hamstra-Wright et al41 | Y | Y | P | P | N/A | N/A | N/A | Y | Y | N | N/A | Y | N | N | 14/22 | 63.6 | MQ |
| Hayes et al39 | Y | Y | Y | Y | N/A | N/A | N/A | P | P | P | Y | N | Y | Y | 17/22 | 77.3 | GQ |
| Hespanhol Junior et al26 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 21/22 | 95.5 | HQ |
| Hespanhol Junior et al25 | Y | Y | P | Y | N/A | N/A | N/A | P | N | P | Y | P | Y | Y | 16/22 | 72.7 | GQ |
| Hootman et al47 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | P | Y | 20/22 | 90.9 | HQ |
| Jakobsen et al27 | P | N | N | Y | N/A | N/A | N/A | P | P | N | N | N | P | N | 6/22 | 27.3 | LQ |
| Kemler et al48 | Y | P | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | P | Y | Y | 19/22 | 86.4 | HQ |
| Kluitenberg et al19 | Y | Y | P | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| Lehmann et al50 | P | N | N | P | N/A | N/A | N/A | P | N | Y | P | N | Y | Y | 10/22 | 45.5 | LQ |
| Lun et al28 | Y | Y | Y | Y | N/A | N/A | N/A | P | P | N | P | Y | P | P | 15/22 | 68.2 | MQ |
| Lysholm et al36 | N | P | N | P | N/A | N/A | N/A | P | P | Y | P | N | P | N | 8/22 | 36.5 | LQ |
| Malisoux et al34 | Y | Y | Y | Y | N/A | N/A | N/A | P | P | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| Messier et al29 | Y | Y | P | Y | N/A | N/A | N/A | Y | Y | P | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| Nielsen et al20 | Y | Y | P | Y | N/A | N/A | N/A | Y | Y | Y | Y | Y | Y | Y | 21/22 | 95.5 | HQ |
| Nielsen et al21 | Y | Y | P | Y | N/A | N/A | N/A | Y | P | Y | Y | Y | P | P | 18/22 | 81.8 | HQ |
| Pollock et al22 | Y | P | P | N | P | N | N/A | P | P | Y | P | N | Y | Y | 14/26 | 53.9 | MQ |
| Ramskov et al30 | Y | Y | Y | Y | Y | Y | N/A | Y | P | Y | Y | Y | Y | Y | 25/26 | 96.2 | HQ |
| Taunton et al31 | Y | Y | P | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| van der Worp et al35 | Y | Y | Y | Y | N/A | N/A | N/A | P | P | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| van Middelkoop et al32 | Y | Y | P | Y | N/A | N/A | N/A | P | Y | Y | Y | Y | Y | P | 19/22 | 86.4 | HQ |
| van Poppel et al33 | Y | Y | Y | Y | N/A | N/A | N/A | P | Y | Y | Y | N | P | P | 17/22 | 77.3 | GQ |
| Walter et al42 | Y | P | Y | Y | N/A | N/A | N/A | P | Y | P | Y | P | Y | Y | 18/22 | 81.8 | HQ |
| Wen et al49 | Y | Y | P | Y | N/A | N/A | N/A | Y | P | Y | Y | Y | Y | Y | 20/22 | 90.9 | HQ |
| Winter et al43 | Y | P | Y | Y | N/A | N/A | N/A | Y | P | N | Y | N | Y | P | 15/22 | 68.2 | MQ |
Abbreviations: GQ, good quality; HQ, high quality; LQ, low quality; MQ, moderate quality; N, no; N/A, not applicable; P, partial; Y, yes.
The Quality Assessment for Evaluating Primary Research Studies (QualSyst)13 contains the following items: Item 1, Description of study question/objective; Item 2, Appropriate study design for objective; Item 3, Description of subject selection strategy; Item 4, Description of subjects' characteristics; Item 5, Random allocation; Item 6, Blinding of investigators; Item 7, Blinding of participants; Item 8, Outcomes and exposures well-defined and robust; Item 9, Appropriate sample size; Item 10, Appropriate statistical analyses; Item 11, Estimates of variance; Item 12, Controlled for confounding; Item 13, Sufficiently reported results; Item 14, Results support conclusions. Scoring: Y = 2; P = 1; N = 0. The N/A items were excluded from the total score. Methodological quality: HQ = >80.0%; GQ = 65.0%–80.0%; MQ = 50.0%–64.9%; LQ = <50.0%.
Points scored/total possible points.
The most common reasons for deducting points on the methodological quality assessment were the outcomes being self-reported or not measured objectively (item 8, n = 28; see Table 3 for description of items), inappropriate or unjustified sample size (item 9, n = 20), not reporting the participants' selection methods or inclusion and exclusion criteria (item 3, n = 18), and inappropriate consideration of confounding variables (item 12, n = 14).
Description of RRIs
An overview of the incidence of injuries is presented in Table 2. Only 14 of 36 studies used definitions of RRI similar to the consensus definition developed by Yamato et al7 in terms of reducing or missing consecutive training sessions because of pain or the need to consult a health care professional. In total, 6043 (26.2%) runners sustained an injury among all 23 047 runners enrolled in the included studies. The incidence of RRI varied between 8.8% and 91.3% depending on the study population, length of follow-up, and definition of an RRI. More specifically, the incidence of RRI was 14.9% in novice runners (703 RRIs in 4720 runners; range = 9.4%–94.9%; follow-up = 6 weeks–18 months),16–22,48 26.1% in recreational runners (2057 RRIs in 7888 runners; range = 17.9%–79.3%; follow-up = 1–24 months),23–35 62.6% in competitive runners (259 RRIs in 414 runners; range = 52.6%–91.3%; follow-up = 3–24 months),36,40 and 27.6% in runners of mixed levels (3158 RRIs in 11 430 runners; range = 8.8%–51.3%; follow-up = 3–60 months).4,41–49
Based on diagnosis details, the most frequently injured body parts were the knee, foot/ankle, and lower leg with 25.8%, 24.4%, and 20.9% of all injuries, respectively. Novice runners sustained RRIs mostly to their knee (30.8%), lower leg (29.7%), and foot/ankle (18.1%).16–18,20,22,48 In recreational runners, the knee (26.5%), foot/ankle (20.5%), and lower leg (20.2%) were the most frequent sites injured,23,25–32,34,35,48 whereas competitive runners most often injured their foot/ankle (39.4%), knee (25.4%), and lower leg (20.8%).36,37,39 In cohorts of runners of mixed levels, the most commonly injured body parts were the foot/ankle (26.3%), knee (26.1%), and lower leg (23.1%).
Training Parameters
An overview of the running programs and of the variables of interest for this review is presented in Table 2. Overall, we found conflicting evidence about the association between RRIs and running distance (20 studies), duration (12 studies), frequency (10 studies), and intensity (14 studies). High heterogeneity among studies (definition of RRI, categories of runners, length of follow-up) prevented us from performing meta-analyses on the association between RRIs and training parameters.
Running Distance
Four HQ,32,35,37,42 2 MQ,16,43 and 2 LQ27,36 studies suggested that greater running distance could increase the injury risk. Three of the HQ studies reported that weekly distances of >30 km (hazard ratio [HR] = 3.28; 95% CI = 1.23, 8.75; P = .02),35 >64 km (adjusted relative risk = 2.88),42 or between 60 km and 70 km (99.7% and 94.7% increased risk versus 40 km to 50 km and 50 km to 60 km, respectively)37 increased the risk of RRI. Another HQ study stated that running <40 km per week was a strong protective factor against calf injuries in recreational runners.32 The incidence of RRI was linked with greater distance during the first (r2 = 0.36, P = .001) and third (r2 = 0.16, P = .015) phases of the running program for novice runners that was used in the first MQ study,16 whereas the second study reported a greater average weekly distance in injured compared with uninjured male recreational and competitive runners (effect size: r = 0.32, P = .046).43 The LQ studies demonstrated more RRIs in a study group that ran a greater weekly distance27 and a significant correlation between the injury rate during any 1 month and the distance covered by long-distance marathon runners during the preceding month (r = 0.59).36
On the other hand, 2 HQ studies,45,49 1 GQ study,33 and 1 LQ24 study described a tendency for a greater running distance to protect against RRIs. Specifically, the first HQ study showed a 10% reduced risk of knee injury (relative risk = 0.901, 95% CI = 0.820, 0.991) in novice and recreational athletes running greater distances,49 whereas the other observed fewer injuries in those running >15 km per week compared with those who ran less (risk difference [RD] = −11.3%, 95% CI = −27.2%, 4.6%).45 The authors of the GQ study concluded that overall, a greater weekly distance protected against RRIs (odds ratio [OR] = 0.99, β = 0.012).33 The LQ study24 indicated a trend for more injuries in those running <20 miles (32.2 km) per week (80% injury incidence) compared with >40 miles (64.4 km) per week (50% injury incidence).
Three HQ studies,20,29,46 2 GQ studies,25,40 1 MQ study,28 and 1 LQ50 study reported no association between weekly running distance and the risk of RRI in cohorts of novice,20 recreational,25,28,29,50 and competitive40 runners as well as runners at mixed levels.46 One HQ study47 noted conflicting results, associating a greater distance with an increased risk of RRI at the 5-year time point but not after 1 year.
Running Duration
One HQ study26 suggested that recreational runners were more at risk of RRI when running for sessions of longer duration (OR = 1.01, 95% CI = 1.00, 1.02), as did 1 MQ study,22 which revealed RRI incidences in novice runners of 22.0%, 24.0%, and 54.0% in the 15-, 30-, and 45-minute duration groups, respectively.
In contrast, 3 HQ studies19,34,49 demonstrated that longer running duration could lead to fewer injuries. Specifically, running >60 minutes in the previous 7 days was a protective factor against the occurrence of RRI (HR = 0.41, 95% CI = 0.20, 0.86).19 Greater mean session distance was also a significant protective factor among recreational runners (HR = 0.795, 95% CI = 0.725, 0.872),34 and more weekly training hours were associated with fewer injuries, especially to the knee and foot, in a mixed cohort of novice and recreational runners (relative risk = 0.575, 95% CI = 0.451, 0.731).49
Five HQ4,17,23,46,48 and 2 GQ25,38 studies found no association between running duration and the incidence of RRIs in cohorts of novice,17 recreational,23,25 and competitive38 runners as well as in runners at mixed levels.4,46,48
Running Frequency
Two HQ studies19,42 and 1 MQ22 study showed that more frequent running tended to yield more injuries. Among recreational and competitive runners, greater weekly frequency was linked with more RRIs (7 days versus 0–2 days).42 Running 3 times per week displayed a trend toward more injuries compared with 2 weekly sessions in novice runners (HR = 1.42, 95% CI = 0.97, 2.08), although it did not reach statistical significance.19 The investigators in the MQ research22 observed a 39% prevalence of injuries in those running 5 days per week, 12% in runners running 3 days per week, and 0% in those running 1 day per week.
However, in 2 HQ studies,31,34 running more often led to fewer injuries in recreational runners. In the first, compared with running 2 to 5 days per week, running only 1 day per week was a significant risk factor overall and in female runners (OR = 3.6, 95% CI = 1.1, 12.3), although the trend was not significant in males.31 In the second study, greater frequency was associated with a lower risk of RRI in the unadjusted statistical model (HR = 0.707, P = .002).34
Two HQ studies,46,47 2 GQ studies,25,33 and 1 MQ28 study described no association between running frequency and injury rates in cohorts of recreational runners25,28,33 and runners at various levels.46,47
Running Intensity
One HQ study19 indicated that greater running intensity in novice runners was more hazardous (HR = 1.28, 95% CI = 1.18, 1.40). One MQ study41 noticed more injuries in runners at mixed levels taking part in tempo runs during the first 6 weeks of a training program (OR = 3.96, 95% CI = 1.35, 11.61) and a trend toward more injuries in those practicing speed intervals (P = .06). The authors of the latter study reported that almost all runners who sustained RRIs (96.4%) performed tempo or interval runs as part of their marathon training.41
Investigators in 2 HQ32,45 studies suggested that greater running intensity could yield fewer RRIs. Performing speed intervals regularly was a protective factor against the occurrence of knee injuries among recreational marathon runners (OR = 0.49, 95% CI = 0.26, 0.93).32 In a cohort of runners of mixed abilities, there was a tendency toward fewer injuries among runners with a faster pace (>10 km/h, RD = –17.4%, 95% CI = −39.0%, 4.5%).45
Four HQ studies,29,34,42,46 3 GQ studies,25,33,38 and 1 LQ50 study found no association between running intensity and RRIs in cohorts involving mostly recreational runners25,29,33,34,50 but also competitive runners38 and mixed cohorts.42,46 Two HQ studies identified conflicting results.26,47 The first one found that speed training was associated with more injuries and interval training with fewer injuries.26 The other reported that greater intensity was linked with more injuries at the 1-year time point (only in men) but not after 5 years.47
Changes in Training Parameters
We found conflicting evidence about the association between RRIs and specific changes in training parameters based on 11 studies. Five16,20,21,39,43 stated that a recent increase in running distance was associated with an increased risk of RRIs. Specifically, 1 HQ study of 58 novice runners noted that over a 10-week follow-up, injured runners had a greater distance progression the week before the onset of injury compared with other weeks (86% difference, 95% CI = 12.9%, 159.9%; P = .026).20 Injured runners also had an average increase in weekly running distance of 31.6% ± 3.1%, compared with 22.1% ± 2.1% in uninjured runners, although the difference did not reach statistical difference (P = .07).20 According to another HQ study21 of 873 novice runners (12 months), those progressing weekly distance by >30% seemed more vulnerable to “distance-based injuries” than those who progressed <10% (HR = 1.59, 95% CI = 0.96, 2.66; P = .07). However, that same study found no association between overall incidence of injuries and distance progression. Another MQ study16 of 73 novice runners (over 18 months) associated a greater risk of RRI with a recent increase in distance between different training phases of a program leading to the completion of a marathon, especially when increasing from a mean weekly distance of 34.9 km to 43.6 km and duration from 3.2 hours to 4.0 hours. One GQ study39 described a trend for university-level competitive runners (n = 97) to sustain more injuries when they had larger differences in running distance between regular and high-mileage weeks during a 3-month cross-country season (P = .06). One MQ study43 with a mixed cohort of 76 recreational and competitive runners reported that, over the course of a 12-month follow-up, injured runners often increased their weekly distance by >30% and even >50% in the 4 weeks before sustaining an injury.
Five other studies (3 HQ,4,18,30 1 GQ,38 1 LQ50) showed no association between recent changes in training parameters and the incidence of RRIs. Week-to-week changes in frequency or duration of running were not linked with RRIs in a mixed cohort of novice and recreational runners.4 An RCT18 from the same research group revealed that a 10% average increase in weekly running distance had no preventive effect against RRIs in novice runners when compared with a weekly distance progression >10% (OR = 0.8, 95% CI = 0.6, 1.3).
Another RCT30 reported a similar incidence of injuries in 447 recreational runners whose schedules focused on increasing intensity or distance, although the average weekly increase in volume was only 3.25%. One more study in 17 recreational runners indicated no difference in RRIs after increasing running distance by 103% or intensity by 152% over a 4-week period.50 As for competitive runners, the acute-to-chronic workload ratio was not associated with the onset of RRIs in a small sample of 23 runners.38
One HQ study44 reported conflicting results in 261 runners of mixed levels. Indeed, more RRIs were recorded during the first 3 weeks of a 14-week training program in those increasing weekly running distance between 20% and 60% compared with those increasing their weekly distance by <20%. However, this association became nonsignificant after 7 weeks and 14 weeks, and those increasing by >60% did not sustain more injuries.44
DISCUSSION
Given the high volume of research on running injuries, this systematic review provided a much-needed update on the current state of the literature. Overall, the incidence of RRI across studies was 26.2%. Whereas previous data suggested greater injury rates in novice compared with recreational runners,51 our findings suggested the opposite, with a greater incidence in recreational (26.1%) than in novice runners (14.9%). In contrast with that previous review,51 we reported the number of events rather than the injuries per 1000 hours of running. Analyses based on exposure are interesting for putting numbers into perspective. However, we believe that considering injuries as events happening during a running program of any duration can better inform injury-prevention strategies, especially in novice and recreational runners. Almost half (48%) of novice runners who abandoned a running program did so because of an injury.4,52 Thus, avoiding RRIs appeared essential to maintaining participation in running and its associated health benefits.53 Yet it is possible that injuries per exposure time may better apply to the training reality of competitive runners, in whom the incidence was reported to be as high as 62.6% during follow-up periods of up to 24 months that likely included much more running than done by novice and recreational runners.
Overall, our findings showed conflicting evidence about the role of specific training parameters (distance, duration, frequency, intensity) as well as the influence of recent training changes in the onset of RRIs. In 2007, based on 17 studies (13 prospective, 4 retrospective), van Gent et al6 had already outlined the conflicting levels of evidence linking training parameters and RRIs. In 2012, based on 31 studies (13 prospective, 9 retrospective, 6 case-control series, and 3 RCTs), Nielsen et al5 also reported conflicting results between distance, duration, frequency of training, intensity, and RRIs. Finally, the authors of a more recent and smaller systematic review11 based on only 4 studies concluded that very limited evidence associated sudden changes in training loads with the onset of RRIs. In comparison, we reviewed 33 prospective cohort studies and 3 RCTs. The sole intervention in all studies was a running program and combined training parameters at large and recent changes in training. In our opinion, the persistence of conflicting results over the years speaks to a lack of consistent definitions and reporting guidelines in the field of RRIs. In addition, assessing the relationship between training parameters and RRIs is certainly more complex than looking at training parameters in isolation.
Running Programs Do Not Tell the Whole Story
Conflicting evidence for the association between running distance, duration, frequency, and intensity, as well as recent changes in training, and RRIs outlines the complexity of running injuries. Factors related to movement biomechanics, load capacity, and lifestyle factors8 are but a few elements that can contribute to RRIs. Importantly, these need to be measured and reported objectively to provide meaningful insights. Unfortunately, researchers in only 5 studies (14%) of the 36 included in this review collected global positioning system–based data to improve the accuracy of actual training loads.20,21,30,44,45 Moving forward, investigators should consider using wearable devices to provide a better picture of actual training parameters, instead of prescribed parameters, and to minimize reporting errors from participating runners.54 They should also consider describing multiple components of workload (eg, intensity and frequency)—not just distance55—as well as patterns of variation experienced during the running program and around the timing of injuries to provide a better picture of training loads. Recent examples of studies56,57 involving different running populations emphasized the substantial underestimation of changes in week-to-week training loads when only distance or duration was considered.
Attributing the cause of RRIs solely to training loads—or external loads—fails to address the plethora of factors related to the individual—or internal loads—which vary among individuals and even in the same individual over the course of a running program.58 The common advice to increase distance by 10% per week for all runners,59 in every situation, is too simplistic and should not be recommended based on our results. A 10% increase for a novice runner who runs 10 km per week is likely much safer than for a competitive runner who runs 150 km per week, including high-intensity workouts. In addition to experience and previous adaptations to exercise that involve impact, subjective measures of well-being, such as psychological stress, fatigue, and recovery, can all affect an athlete's response and adaptation to training.60 Only 10 studies in this review reported outcomes related to personality and mental health,17,24,26,29,41 diet,22,39,50 smoking habits,22,33,42 or alcohol intake.33,39 Only 2 studies22,39 asked questions about sleeping habits, and only one39 documented hormonal variations and the use of contraceptives in female runners. Monitoring and reporting these variables and measures of internal loads is crucial to gain a better understanding of the causes of RRIs in both females and males. These factors should be considered especially in competitive runners, among whom the interaction between training parameters and recovery could explain the higher rate of RRIs.
Limitations of This Review or Limitations of Included Articles?
The clinical applicability of this review was limited because of conflicting findings. However, the conflicting findings stemmed from the many limitations of the included studies. Results regarding the incidence of RRIs in different running populations were limited due to the heterogeneity of definitions used in the different articles. Findings about RRIs and training parameters or changes in these parameters were limited because of the lack of objective data about training loads and the lack of data on factors related to the individual. We understand that collecting all of these burdens research teams and might not always be feasible, depending on the budget. Still, unless these factors are addressed in future research, we predict that future reviews will still demonstrate conflicting findings about the causes of RRIs. It is also possible that the wide variability in factors affecting the capacity for adaptation in different runners precludes us from making specific recommendations for novice, recreational, or competitive runners about training parameters to reduce the risk of RRIs. Running biomechanics, footwear, and surface or changes in these variables should also be considered when possible.
Calling for Unity
Meaningful conclusions and recommendations are made possible with consensus definitions and reporting guidelines. Unfortunately, fewer than 40% (14/36) of included studies used RRI definitions that were in accordance with, or similar to, the consensus definition published by Yamato et al7 regarding reduced or missed consecutive training sessions because of pain or consultation of a health care professional. Our results also call for a better standardization of follow-up periods when monitoring injury incidence. Included studies varied between 1 month and 60 months, making the results too heterogeneous to generalize for the running population. A set of reporting guidelines could include, for example, details on injuries sustained during each 2-week period of a running program (eg, during weeks 1–2, 3–4, 5–6, and so on until the end of the study period). This could help to identify trends in injury incidence using a meta-analysis process, which was not possible in this review, and compare data in different levels of runners.
Novice, recreational, and competitive running populations should be more specifically defined. For the purpose of this review, we relied on information provided in the articles, although the details may not have been comparable. Despite a previous classification suggested based on the existing literature,61 a scientific process to determine consensus definitions could provide clear guidelines that experts in the field agree upon. This would make it easier to improve study designs, tailor research questions to the different populations,62 and unite multiple research teams in their efforts toward a common goal. Standardized guidelines could also translate to better research uptake by the running community, coaches, and health care professionals.
Despite high rates of RRIs, conflicting evidence described the associations between weekly running distance, duration, frequency, and intensity, or recent changes in these parameters, and the incidence of RRIs. Thus, at this time, no specific recommendations related to optimal training parameters or progressions can be issued to guide clinical decision making and program planning. This result was largely due to a lack of consistent definitions and reporting guidelines. Finally, RRIs are multifactorial and likely not explained solely by training parameters. Authors of future prospective studies on the incidence of RRIs should consider how variations in objectively measured training parameters interact with factors related to the individual using psychosocial, hormonal, lifestyle, and recovery outcomes.
Supplementary Material
SUPPLEMENTAL MATERIAL
Supplemental Table. Search strategy.
Found at DOI: http://dx.doi.org/10.4085/1062-6050-0195.21.S1
REFERENCES
- 1.Cavanagh PR, Lafortune MA. Ground reaction forces in distance running. J Biomech . 1980;13(5):397–406. doi: 10.1016/0021-9290(80)90033-0. [DOI] [PubMed] [Google Scholar]
- 2.Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc . 2004;36(5):845–849. doi: 10.1249/01.mss.0000126803.66636.dd. [DOI] [PubMed] [Google Scholar]
- 3.Hreljac A, Marshall RN, Hume PA. Evaluation of lower extremity overuse injury potential in runners. Med Sci Sports Exerc . 2000;32(9):1635–1641. doi: 10.1097/00005768-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Buist I, Bredeweg SW, Bessem B, van Mechelen W, Lemmink KAPM, Diercks RL. Incidence and risk factors of running-related injuries during preparation for a 4-mile recreational running event. Br J Sports Med . 2010;44(8):598–604. doi: 10.1136/bjsm.2007.044677. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen RO, Buist I, Sorensen H, Lind M, Rasmussen S. Training errors and running related injuries: a systematic review. Int J Sports Phys Ther . 2012;7(1):58–75. [PMC free article] [PubMed] [Google Scholar]
- 6.van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med . 2007;41(8):469–480. doi: 10.1136/bjsm.2006.033548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamato TP, Saragiotto BT, Lopes AL. A consensus definition of running-related injury in recreational runners: a modified Delphi approach. J Orthop Sports Phys Ther . 2015;45(5):375–380. doi: 10.2519/jospt.2015.5741. [DOI] [PubMed] [Google Scholar]
- 8.Hulme A, Salmon PM, Nielsen RO, Read GJM, Finch CF. From control to causation: validating a “complex systems model” of running-related injury development and prevention. Appl Ergon . 2017;65:345–354. doi: 10.1016/j.apergo.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Satterthwaite P, Norton R, Larmer P, Robinson E. Risk factors for injuries and other health problems sustained in a marathon. Br J Sports Med . 1999;33(1):22–26. doi: 10.1136/bjsm.33.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen DY. Risk factors for overuse injuries in runners. Curr Sports Med Rep . 2007;6(5):307–313. [PubMed] [Google Scholar]
- 11.Damsted C, Glad S, Nielsen RO, Sorensen H, Malisoux L. Is there evidence for an association between changes in training load and running-related injuries? A systematic review. Int J Sports Phys Ther . 2018;13(6):931–942. [PMC free article] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol . 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Kmet LM, Lee RC, Cook LS. Standard Quality Assessment Criteria for Evaluating Primary Research Papers From a Variety of Fields Alberta Heritage Foundation for Medical Research; 2004.
- 14.Bernard S, Ouellet MP, Moffet H, Roy JS, Dumoulin C. Effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area: a systematic review. J Cancer Surviv . 2016;10(2):351–362. doi: 10.1007/s11764-015-0481-8. [DOI] [PubMed] [Google Scholar]
- 15.van Tulder M, Furlan A, Bombardier C, Bouter L; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) . 2003;15(28):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 16.Bovens AM, Janssen GM, Vermeer HG, Hoeberigs JH, Janssen MP, Verstappen FT. Occurrence of running injuries in adults following a supervised training program. Int J Sports Med . 1989;10(suppl 3):S186–S190. doi: 10.1055/s-2007-1024970. [DOI] [PubMed] [Google Scholar]
- 17.Buist I, Bredeweg SW, Lemmink KAPM, van Mechelen W, Diercks RL. Predictors of running-related injuries in novice runners enrolled in a systematic training program: a prospective cohort study. Am J Sports Med . 2010;38(2):273–280. doi: 10.1177/0363546509347985. [DOI] [PubMed] [Google Scholar]
- 18.Buist I, Bredeweg SW, van Mechelen W, Lemmink KAPM, Pepping GJ, Diercks RL. No effect of a graded training program on the number of running-related injuries in novice runners: a randomized controlled trial. Am J Sports Med . 2008;36(1):33–39. doi: 10.1177/0363546507307505. [DOI] [PubMed] [Google Scholar]
- 19.Kluitenberg B, van der Worp H, Huisstede BM, et al. The NLstart2run study: training-related factors associated with running-related injuries in novice runners. J Sci Med Sport . 2016;19(8):642–646. doi: 10.1016/j.jsams.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Nielsen RO, Cederholm P, Buist I, Sorensen H, Lind M, Rasmussen S. Can GPS be used to detect deleterious progression in training volume among runners? J Strength Cond Res . 2013;27(6):1471–1478. doi: 10.1519/JSC.0b013e3182711e3c. [DOI] [PubMed] [Google Scholar]
- 21.Nielsen RO, Parner ET, Nohr EA, Sorensen H, Lind M, Rasmussen S. Excessive progression in weekly running distance and risk of running-related injuries: an association which varies according to type of injury. J Orthop Sports Phys Ther . 2014;44(10):739–747. doi: 10.2519/jospt.2014.5164. [DOI] [PubMed] [Google Scholar]
- 22.Pollock ML, Gettman LR, Milesis CA, Bah MD, Durstine L, Johnson RB. Effects of frequency and duration of training on attrition and incidence of injury. Med Sci Sports . 1977;9(1):31–36. [PubMed] [Google Scholar]
- 23.Dallinga J, Van Rijn R, Stubbe J, Deutekom M. Injury incidence and risk factors: a cohort study of 706 8-km or 16-km recreational runners. BMJ Open Sport Exerc Med . 2019;5(1):e000489. doi: 10.1136/bmjsem-2018-000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fields KB, Delaney M, Hinkle JS. A prospective study of type A behavior and running injuries. J Fam Pract . 1990;30(4):425–429. [PubMed] [Google Scholar]
- 25.Hespanhol LC, Junior, de Carvalho AC, Pena Costa LO, Lopes AD. Lower limb alignment characteristics are not associated with running injuries in runners: prospective cohort study. Eur J Sport Sci . 2016;16(8):1137–1144. doi: 10.1080/17461391.2016.1195878. [DOI] [PubMed] [Google Scholar]
- 26.Hespanhol LC, Junior, Pena Costa LO, Lopes AD. Previous injuries and some training characteristics predict running-related injuries in recreational runners: a prospective cohort study. J Physiother . 2013;59(4):263–269. doi: 10.1016/S1836-9553(13)70203-0. [DOI] [PubMed] [Google Scholar]
- 27.Jakobsen BW, Kroner K, Schmidt SA, Kjeldsen A. Prevention of injuries in long-distance runners. Knee Surg Sports Traumatol Arthrosc . 1994;2(4):245–249. doi: 10.1007/BF01845597. [DOI] [PubMed] [Google Scholar]
- 28.Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med . 2004;38(5):576–580. doi: 10.1136/bjsm.2003.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Messier SP, Martin DF, Mihalko SL, et al. A 2-year prospective cohort study of overuse running injuries: The Runners and Injury Longitudinal Study (TRAILS) Am J Sports Med . 2018;46(9):2211–2221. doi: 10.1177/0363546518773755. [DOI] [PubMed] [Google Scholar]
- 30.Ramskov D, Rasmussen S, Sorensen H, Parner ET, Lind M, Nielsen R. Progression in running intensity or running volume and the development of specific injuries in recreational runners: Run Clever, a randomized trial using competing risks. J Orthop Sports Phys Ther . 2018;48(10):740–748. doi: 10.2519/jospt.2018.8062. [DOI] [PubMed] [Google Scholar]
- 31.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A prospective study of running injuries: the Vancouver Sun Run “In Training” clinics. Br J Sports Med . 2003;37(3):239–244. doi: 10.1136/bjsm.37.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Middelkoop M, Kolkman J, van Ochten J, Bierma-Zeinstra SMA, Koes BW. Risk factors for lower extremity injuries among male marathon runners. Scand J Med Sci Sports . 2008;18(6):691–697. doi: 10.1111/j.1600-0838.2007.00768.x. [DOI] [PubMed] [Google Scholar]
- 33.van Poppel D, Scholten-Peeters GGM, van Middelkoop M, Koes BW, Verhagen AP. Risk models for lower extremity injuries among short- and long distance runners: a prospective cohort study. Musculoskelet Sci Pract . 2018;36:48–53. doi: 10.1016/j.msksp.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 34.Malisoux L, Ramesh J, Mann R, Seil R, Urhausen A, Theisen D. Can parallel use of different running shoes decrease running-related injury risk? Scand J Med Sci Sports . 2015;25(1):110–115. doi: 10.1111/sms.12154. [DOI] [PubMed] [Google Scholar]
- 35.van der Worp MP, de Wijer A, van Cingel R, Verbeek ALM, Nijhuis-van der Sanden MWG, Staal JB. The 5- or 10-km Marikenloop run: a prospective study of the etiology of running-related injuries in women. J Orthop Sports Phys Ther . 2016;46(6):462–470. doi: 10.2519/jospt.2016.6402. [DOI] [PubMed] [Google Scholar]
- 36.Lysholm J, Wiklander J. Injuries in runners. Am J Sports Med . 1987;15(2):168–171. doi: 10.1177/036354658701500213. [DOI] [PubMed] [Google Scholar]
- 37.Begizew DM, Grace JM, van Heerden HJ. Lower-extremity running-related injuries among 10 000-meter long distance runners in Ethiopia. J Hum Sport Sci . 2018;14(2):358–373. doi: 10.14198/jhse.2019.142.09. [DOI] [Google Scholar]
- 38.Dijkhuis TB, Otter R, Aiello M, Velthuijsen H, Lemmink K. Increase in the acute:chronic workload ratio relates to injury risk in competitive runners. Int J Sports Med . 2020;41(11):736–743. doi: 10.1055/a-1171-2331. [DOI] [PubMed] [Google Scholar]
- 39.Hayes LE, Boulos A, Cruz AI., Jr Risk factors for in-season injury in varsity collegiate cross-country athletes: an analysis of one season in 97 athletes. J Sports Med Phys Fitness . 2019;59(9):1536–1543. doi: 10.23736/S0022-4707.19.09221-1. [DOI] [PubMed] [Google Scholar]
- 40.Becker J, Nakajima M, Wu WFW. Factors contributing to medial tibial stress syndrome in runners: a prospective study. Med Sci Sports Exerc . 2018;50(10):2092–2100. doi: 10.1249/MSS.0000000000001674. [DOI] [PubMed] [Google Scholar]
- 41.Hamstra-Wright KL, Coumbe-Lilley JE, Kim H, McFarland JA, Huxel Bliven KC. The influence of training and mental skills preparation on injury incidence and performance in marathon runners. J Strength Cond Res . 2013;27(10):2828–2835. doi: 10.1519/JSC.0b013e31828a4733. [DOI] [PubMed] [Google Scholar]
- 42.Walter SD, Hart LE, McIntosh JM, Sutton JR. The Ontario cohort study of running-related injuries. Arch Intern Med . 1989;149(11):2561–2564. [PubMed] [Google Scholar]
- 43.Winter SC, Gordon S, Brice SM, Lindsay D, Barrs S. A multifactorial approach to overuse running injuries: a 1-year prospective study. Sports Health . 2020;12(3):296–303. doi: 10.1177/1941738119888504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Damsted C, Parner ET, Sorensen H, Malisoux L, Hulme A, Nielsen RO. The association between changes in weekly running distance and running-related injury: preparing for a half marathon. J Orthop Sports Phys Ther . 2019;49(4):230–238. doi: 10.2519/jospt.2019.8541. [DOI] [PubMed] [Google Scholar]
- 45.Damsted C, Parner ET, Sorensen H, Malisoux L, Nielsen RO. ProjectRun21: do running experience and running pace influence the risk of running injury? A 14-week prospective cohort study. J Sci Med Sport . 2019;22(3):281–287. doi: 10.1016/j.jsams.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 46.Fokkema T, van Damme AADN, Fornerod MWJ, de Vos RJ, Bierma-Zeinstra SMA, van Middelkoop M. Training for a (half-)marathon: training volume and longest endurance run related to performance and running injuries. Scand J Med Sci Sports . 2020;30(9):1692–1704. doi: 10.1111/sms.13725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hootman JM, Macera CA, Ainsworth BE, Martin M, Addy CL, Blair SN. Predictors of lower extremity injury among recreationally active adults. Clin J Sport Med . 2002;12(2):99–106. doi: 10.1097/00042752-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Kemler E, Blokland D, Backx F, Huisstede B. Differences in injury risk and characteristics of injuries between novice and experienced runners over a 4-year period. Phys Sportsmed . 2018;46(4):485–491. doi: 10.1080/00913847.2018.1507410. [DOI] [PubMed] [Google Scholar]
- 49.Wen DY, Puffer JC, Schmalzried TP. Injuries in runners: a prospective study of alignment. Clin J Sport Med . 1998;8(3):187–194. doi: 10.1097/00042752-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Lehmann M, Jakob E, Gastmann U, Steinacker JM, Keul J. Unaccustomed high mileage compared to intensity training-related neuromuscular excitability in distance runners. Eur J Appl Physiol Occup Physiol . 1995;70(5):457–461. doi: 10.1007/BF00618498. [DOI] [PubMed] [Google Scholar]
- 51.Videbæk S, Bueno AM, Nielsen RO, Rasmussen S. Incidence of running-related injuries per 1000 h of running in different types of runners: a systematic review and meta-analysis. Sports Med . 2015;45(7):1017–1026. doi: 10.1007/s40279-015-0333-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fokkema T, Hartgens F, Kluitenberg B, et al. Reasons and predictors of discontinuation of running after a running program for novice runners. J Sci Med Sport . 2019;22(1):106–111. doi: 10.1016/j.jsams.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 53.Pedisic Z, Shrestha N, Kovalchik S, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med . 2020;54(15):898–905. doi: 10.1136/bjsports-2018-100493. [DOI] [PubMed] [Google Scholar]
- 54.Napier C, Esculier JF, Hunt MA. Gait retraining: out of the lab and onto the streets with the benefit of wearables. Br J Sports Med . 2017;51(23):1642–1643. doi: 10.1136/bjsports-2017-098637. [DOI] [PubMed] [Google Scholar]
- 55.Paquette MR, Napier C, Willy RW, Stellingwerff T. Moving beyond weekly “distance”: optimizing quantification of training load in runners. J Orthop Sports Phys Ther . 2020;50(10):564–569. doi: 10.2519/jospt.2020.9533. [DOI] [PubMed] [Google Scholar]
- 56.Napier C, Ryan M, Menon C, Paquette MR. Session rating of perceived exertion combined with training volume for estimating training responses in runners. J Athl Train . 2020;55(12):1285–1291. doi: 10.4085/1062-6050-573-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ryan MR, Napier C, Greenwood D, Paquette MR. Comparison of different measures to monitor week-to-week changes in training load in high school runners. Int J Sports Sci Coach . 2020;16(2):370–379. doi: 10.1177/1747954120970305. [DOI] [Google Scholar]
- 58.Bertelsen ML, Hulme A, Petersen J, et al. A framework for the etiology of running-related injuries. Scand J Med Sci Sports . 2017;27(11):1170–1180. doi: 10.1111/sms.12883. [DOI] [PubMed] [Google Scholar]
- 59.Johnston CAM, Taunton JE, Lloyd-Smith DR, McKenzie DC. Preventing running injuries: practical approach for family doctors. Can Fam Physician . 2003;49:1101–1109. [PMC free article] [PubMed] [Google Scholar]
- 60.Saw AE, Main LC, Gastin PB. Monitoring the athlete training response: subjective self-360 reported measures trump commonly used objective measures. A systematic review. Br J Sports Med . 2016;50(5):281–291. doi: 10.1136/bjsports-2015-094758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kluitenberg B, van Middelkoop M, Diercks R, van der Worp H. What are the differences in injury proportions between different populations of runners? A systematic review and meta-analysis. Sports Med . 2015;45(8):1143–1161. doi: 10.1007/s40279-015-0331-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nielsen RO, Bertelsen ML, Møller M, et al. Methods matter: exploring the ‘too much, too soon' theory, part 1: causal questions in sports injury research. Br J Sports Med . 2020;54(18):1119–1122. doi: 10.1136/bjsports-2018-100245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.