Abstract
Patellar tendinopathy is a common yet misunderstood condition that afflicts a variety of patient populations. This lack of understanding affects the ability of clinicians to provide effective treatment interventions. Patients with tendinopathy often report long-term and low to moderate levels of pain, diminished flexibility, and reduced strength, as well as decreased physical function. Load-management strategies combined with exercise regimens focused on progressive tendon loading are the most effective treatment options for patients with patellar tendinopathy. This review will provide an evidence-based approach to patellar tendinopathy, including its pathoetiology, evaluation, and treatment strategies.
Keywords: tendinitis, tendon, tendinosis, load management, exercise, loading
Patellar tendinopathy accounts for approximately 10% of clinical knee diagnoses, making it one of the most common knee pathologies.1,2 Patellar tendinopathy occurs in physically active populations of all ages; the subsequent pain forces many athletes to limit or discontinue sport participation. Historically, patellar tendinitis, or “jumper's knee,” has been used colloquially to characterize anterior knee symptoms experienced in the quadriceps tendon, patellar tendon, or both, which suggests that this condition affects only those participating in jumping sports (eg, basketball and volleyball).3 However, any individuals who participate in activities that cause loading of the patellar tendon through rapid acceleration or deceleration, frequent change of direction, repetitive movements, or any combination of these are at risk for symptoms originating from the patellar tendon.4
Contemporary theory and histopathologic examinations suggest that the term tendinitis may be inaccurate, as the condition often presents with tissue degeneration rather than an acute inflammatory response.5 However, this is disputed in the literature, with some groups6,7 demonstrating active inflammation in chronic pathologic tendons. Nonetheless, tendinopathy is an umbrella term that encompasses tendon degeneration with failed healing due to tissue overload without adequate recovery.5 The term tendinopathy, as opposed to tendinitis or tendinosis, is recommended when discussing overuse conditions related to the patellar tendon unless histologically confirmed via tissue biopsy.5 The poor understanding of the underlying pathology contributing to patellar tendinopathy diminishes our ability to provide effective treatments.8 Therefore, the purpose of this current clinical concepts article is to present the practicing clinician with a comprehensive, evidence-based approach to the evaluation and treatment of patients with patellar tendinopathy. Interventions that bridge the gap from load-reduction management strategies to unrestricted sport participation are described. When possible, we used the Strength of Recommendation (SOR) Taxonomy to grade the strength of evidence (A, B, or C).9
EPIDEMIOLOGY
In a general practice adult population, lower extremity tendinopathies had a prevalence rate of 10.5 per 1000 person-years, with a patellar tendinopathy incidence of 1.6 per 1000 person-years.10 Injuries to the patella and patellar tendon account for almost 30% of knee structure injuries among high school athletes across a variety of sports, including soccer, running, volleyball, basketball, and ice hockey.11 Patellar tendinopathy reaches incidence proportions of 32% and 45% in elite basketball and volleyball athletes, respectively.12 Among recreational runners, patellar tendinopathy was the third most common condition behind patellofemoral pain syndrome and iliotibial band friction syndrome.13 Men may experience higher rates of patellar tendinopathy than women, despite anterior knee pain such as patellofemoral pain syndrome being more prevalent in women.4 Those who suffer from patellar tendinopathy are often younger (<20 years of age) and have a greater body mass index than those without the condition.4,11
PATHOPHYSIOLOGY
The pathologic sequence of patellar tendinopathy and factors contributing to resulting pain and disability remain poorly understood and are often disputed. Tendons generally have a poorer blood supply than muscles. The blood supply of the patellar tendon emanates directly from the infrapatellar fat pad and retinaculum.14,15 Notably, the patellar tendon has areas of reduced vascularity, especially at the proximal and distal attachments, which are frequently linked to degeneration and failure.15 Stress shielding and compression may also contribute to tendon strain during movement.16 Histopathologic findings typically suggest chronic, mucoid degeneration rather than an acute inflammatory response.5 Pathologic tendons demonstrate a higher concentration of type III collagen, in comparison with primarily type I collagen in healthy tendon tissue.7 When viewed both macroscopically and microscopically, the affected areas of the tendons' collagen fibers appear thinner and disorganized, with associated fibrosis.7 At the cellular level, changes include hypercellularity characterized by cell proliferation and increased fibroblast activity.7 Neovascularization, or abnormal vascular proliferation, along with an increased concentration of proteoglycans and water content, is also present.7 These pathologic responses suggest an attempt by the tendon to heal itself7 and lead to the often-observed increase in tendon thickness that typically characterizes patellar tendinopathy.7
A primary contributor to patellar tendinopathy is likely mechanical overloading of the quadriceps muscle, resulting in tensile failure of the collagen fibers within the patellar tendon.7 Repetitive tensile stresses within the patellar tendon without adequate recovery may cause microtrauma with insufficient opportunities for tissue adaptation and healing.7 The damage caused by excessive submaximal tensile strain weakens portions of the tendon and reduces its ability to transfer forces from the quadriceps muscle.17 This presents clinically as quadriceps muscle weakness.
RISK FACTORS
Repetitive activities that load the patellar tendon, often in combination with variations in training behavior, are a primary risk factor for the development of patellar tendinopathy.18 Patients with patellar tendinopathy demonstrate significantly higher total training volumes, previous training volumes, and match exposures compared with their healthy counterparts.18 Further, a recent meta-analysis18 indicated that higher body weight was associated with patellar tendinopathy (odds ratio = 1.92). However, despite speculation to the contrary, the type of playing surface was not a significant risk factor for patellar tendinopathy.18
The development and perpetuation of patellar tendinopathy has also been linked to alterations in muscle strength, range of motion, and static lower extremity alignment. Patients with patellar tendinopathy had decreased quadriceps strength and ankle-dorsiflexion range of motion.18,19 In a retrospective study, Taunton et al2 found that 27% of those with patellar tendinopathy displayed static genu valgum alignment, a potential mechanical contributor to tendinopathy. Quadriceps and hamstrings muscle strength and flexibility, pelvic tilt, and the Q-angle have all been associated with the level of self-reported disability in patients with patellar tendinopathy.20
From a biomechanical perspective, decreased sagittal-plane motion of the hip and knee during movement has been associated with the development and perpetuation of patellar tendinopathy.21 Individuals with patellar tendinopathy exhibited decreased external knee-extension moments compared with control participants during jump landings.22 However, whether these changes in biomechanics and movement patterns contribute to the onset of patellar tendinopathy or instead develop secondary to the onset of the condition is unclear.
SIGNS, SYMPTOMS, AND PHYSICAL EXAMINATION
Patients with patellar tendinopathy report localized anterior knee pain at the patellar tendon. The onset of pain is typically insidious and related to increases in both the frequency and intensity of patellar tendon–loading activity. In the early stages, patients may report pain at the beginning of exercise that diminishes with continued activity.7 In more advanced stages, anterior knee pain may be present throughout exercise and result in reduced activity.7 Further, patients may report pain during activities of daily living, including pain during long periods of sitting and stair ascent and descent.7
Focal point tenderness is the most prevalent finding on physical examination.23,24 Although the patellar tendon may be tender throughout, the inferior pole and distal insertion at the tibial tuberosity are the most common areas of tenderness.23 As part of a clinical assessment, palpation was statistically reliable both between and within raters; however, sensitivity was moderate and specificity was poor when compared with ultrasound imaging.23 Abnormal ultrasound findings in the patellar tendon are frequent in asymptomatic individuals and may contribute to the poor diagnostic accuracy of palpation.25 Similarly, providing the patient with an image on which to pinpoint the pain location (pain mapping) may assist clinical assessment.24 In particular, pain mapping during a single-legged squat in comparison with pain at rest may provide useful information regarding a variety of knee conditions, including the differentiation of patellar tendinopathy if pain is mapped to the patellar tendon.24 Pain may occur during resisted knee extension or other forms of high loading of the patellar tendon (eg, descending stairs, decline walking). SOR: A
Other useful functional performance tests for patients with patellar tendinopathy involve jumping and jump landing. The maximum vertical jump is the most assessed functional test in the literature related to patellar tendinopathy.18 However, the evidence is conflicting, with some authors18 reporting that those with patellar tendinopathy had better vertical jump performance than healthy control participants. The single-legged hop for distance and 6-m hop test may also be useful as part of a test battery to assess function and performance over time.26 Balance examinations may provide insight relating patient symptoms to function in patellar tendinopathy, as increases in pain are associated with worse dynamic postural stability.27 SOR: B
Symptoms associated with patellar tendinopathy have both short- and long-term outcomes. Symptom duration averages 19 months and can exceed 32 months in elite athletes.11 The most common outcome associated with patellar tendon injuries is loss of participation.28 In 1 long-term prospective study28 of male athletes, 53% of those with patellar tendinopathy indicated they ended their sports career because of the symptoms and their effects on physical function. Many of those athletes who continued to participate in their sports experienced mild but persistent symptoms that remained after their athletic careers ended.28
The main differential diagnosis of patellar tendinopathy is patellofemoral pain syndrome, defined as a form of nonspecific, nonstructural knee pain around or behind the patella.29 Patellofemoral pain syndrome is characterized by crepitus or “grinding” underneath the patella during knee flexion and tenderness along the patellar facets.29 Patellar tendinopathy can be differentiated from patellar tendon pain with palpation and tissue loading during resisted knee extension and functional activities; however, patellar tendinopathy and patellofemoral pain can coexist. Other differential diagnoses are fat-pad impingement syndrome, meniscal injury, cartilage degeneration, and bony abnormalities such as Osgood-Schlatter syndrome.30
IMAGING
Clinical assessment is the most appropriate means and criterion standard for diagnosing patellar tendinopathy. However, imaging may be used for confirmation and to assess other conditions that may coexist with patellar tendinopathy.30 Plain film radiographs, diagnostic ultrasound, and magnetic resonance imaging (MRI) can help assess the integrity of the patellar tendon and surrounding structures. Radiographs are typically the initial imaging modality for evaluating the bony structures of the knee, including enthesophytes, which can develop on the inferior pole of the patella. Conditions such as Osgood-Schlatter and intratendinous calcifications may also be investigated using plain radiographs.15
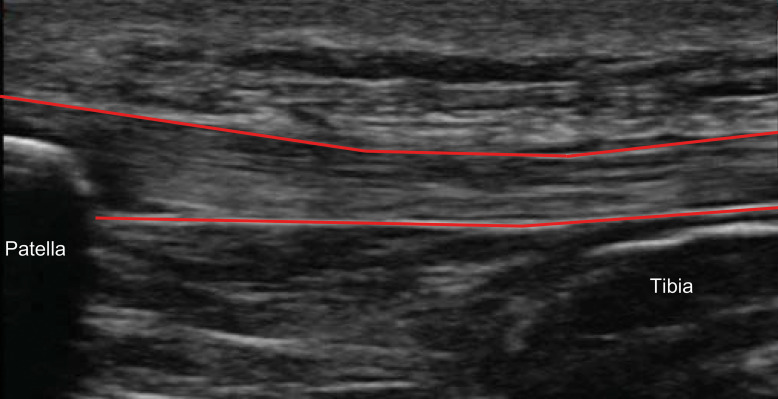
Diagnostic ultrasound (Figure 1) is 83% accurate in correctly identifying patellar tendinopathy with moderately high sensitivity (87%) and specificity (82%; positive likelihood ratio = 4.8, negative likelihood ratio = 0.2).30 The patellar tendon may show thickening and a greater cross-sectional area than normal.31,32 On average, the thickness and width of a healthy tendon range from 3 to 6 and 10 to 15 mm, respectively.15 Hypoechoic changes within the patellar tendon are pervasive in asymptomatic athletic populations, particularly as competition levels increase.33 Further, patellar tendon abnormality was more prevalent in male than in female athletes.33 These abnormal tendon changes result in a 5 times greater risk for tendinopathy compared with normal tendons.33 SOR: A
Figure 1.
Patellar tendon outlined on ultrasound image.
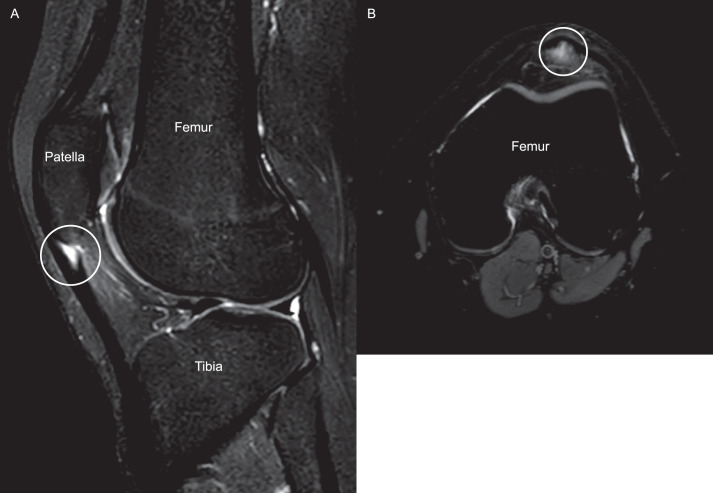
On MRI, increased T2 signal intensity within the patellar tendon corresponds with degenerative changes (Figure 2).34 Tendon thickening may also be prevalent on MRI.34 In more severe cases, calcification within the tendon may be present, portrayed as well-defined areas of low signal.15 Unlike diagnostic ultrasound, the accuracy of MRI in diagnosing patellar tendinopathy is only 70%, with a similar specificity (82%) as ultrasound but worse sensitivity (57%), positive likelihood ratio (3.1), and negative likelihood ratio (0.5).30 SOR: A
Figure 2.
A, Sagittal and, B, axial views of a T2-weighted magnetic resonance imaging scan of a patient with symptomatic patellar tendinopathy. Circles highlight focal regions of tendinopathy, which present as increased (white) signal in the substance of the tendon.
PATIENT-REPORTED OUTCOME MEASURES
The International Scientific Tendinopathy Symposium Consensus35 recently identified 9 core domains for tendinopathy to guide clinical research trials that can also provide a comprehensive road map for clinicians in their evaluation process (Table 1). Several disease-specific patient-reported outcomes for assessing patellar tendinopathy cover a significant portion of these domains, including symptom severity. The most widely used patient-reported outcome measure is the Victorian Institute of Sport Assessment–Patella (VISA-P).36 The VISA-P is scored with a maximum of 100 points; higher scores indicate better function, and the minimally clinically important difference is 13 points.37 A cutoff score of <80 is frequently used to characterize patellar tendinopathy and as an inclusion criterion for research. The VISA-P alone can differentiate individuals with and those without patellar tendinopathy as well as identify improvements from therapeutic interventions among patients with patellar tendinopathy.38 The Oslo Sports Trauma Research Center–Patellar Tendinopathy (OSTRC-P) outcome measure was developed and studied among youth basketball players.39 The OSTRC-P is a 10-item questionnaire scored with a maximum of 100 points that is used to identify patellar tendinopathy and its severity. Higher values indicate increased severity.39 The OSTRC-P has demonstrated good sensitivity (79%) and excellent specificity (95%) compared with the clinical assessment of patellar tendinopathy.39 Visual analog scales are also used frequently and were reliable and sensitive tools in the evaluation of pain in patients with patellar tendinopathy.40 SOR: A
Table 1.
Core Domains for Tendinopathy Assessment (International Scientific Tendinopathy Symposium Consensus 2019)35 and Specific Examples Pertaining to Patellar Tendinopathy
| Core Domain for Tendinopathy |
Patellar Tendinopathy–Specific Example |
| Patient rating of condition | Global rating from 0% to 100% of the patient's feeling about patellar tendinopathy status |
| Activity participation | Tegner Activity Scale, Activities of Daily Living Scale |
| Pain during activity, loading, or both | 100-mm Visual analog scale immediately after single-legged squat on the affected limb(s) |
| Patient function | Lower Extremity Functional Scale, Lysholm Knee Scale |
| Psychological factors | Tampa Scale of Kinesiophobia, Pain Catastrophizing Scale |
| Physical function capacity | Quadriceps strength, quadriceps flexibility, single-limb hop for distance, 6-m hop test |
| Disability | Victorian Institute of Sport Assessment–Patella or Oslo Sports Trauma Research Center–Patellar Tendinopathy |
| Health-related quality of life | Short Form Survey-36 |
| Pain over a specific time | 100-mm Visual analog scale for pain |
CLINICAL MANAGEMENT
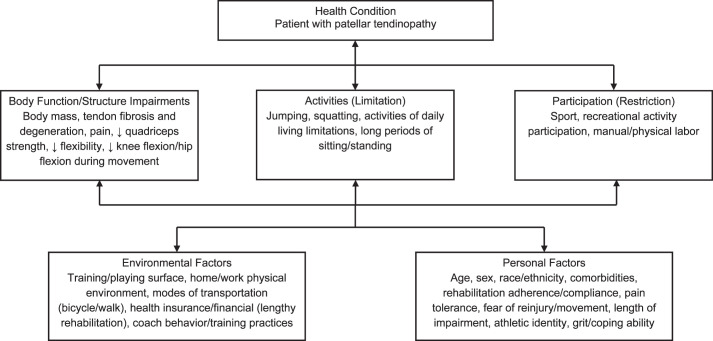
Patellar tendinopathy rehabilitation can be a lengthy, arduous process for patients and clinicians, as the condition often persists for months, if not years.12 Therefore, using the International Classification of Function model can provide an organized, patient-centered approach to caring for individuals with patellar tendinopathy (Figure 3).41 Conservative treatment is recommended. Surgical treatments should be considered only for those with advanced symptoms and reduced function and quality of life and after conservative treatment has failed.28 Consistent with treatment approaches to Achilles tendinopathy,42 rehabilitation for patellar tendinopathy can be segmented into 4 phases: symptom management and load reduction, recovery, rebuilding, and return to unrestricted sport participation (Table 2). Specific progressions depend on severity, compliance, pain, and duration of symptoms. Conservative management is multifaceted and can include activity modification, exercise rehabilitation, and therapeutic modalities.43
Figure 3.
An example using the International Classification of Function model for patients with patellar tendinopathy, which can also be individualized.
Table 2.
Patellar Tendinopathy Management Strategiesa
| Phase |
Symptom Management and Load Reduction |
Recovery |
Rebuilding |
Return to Unrestricted Sport Participation |
| Time | Wk 0–4 | Wk 2–6 | Wk 4–12 | Wk 12+ |
| Load management | ||||
| Visual analog scale score | <5 cm | <5 cm | <3 cm | <1 cm |
| Sport participation and volume | <25% | <50% | <75% | 100% |
| Goal | Understand condition, training loads, and pain tolerance to ↓ stress on patellar tendon | Gradually ↑ physical activity and introduce progressive loading programs | Continue to ↑ patient load capacity during physical activity and exercise program | Symptoms should be minimal to none during physical activity and progressive-loading phases |
| Activity modification | Replace jumping, squatting, etc, with cycling or aquatic therapy | Begin integrating submaximal jumping and squatting into exercise regimen | Begin introducing maximum jumping and moderate plyometric training | No restrictions |
| Exercise paradigm and progression | Complete exercises daily Isometric quadriceps activation (“quad sets”) sitting on table in full knee extension: 5 reps, ↑ time from 30 to 60 s each Isometric quadriceps contractions with leg-extension machine: 5 reps, ↑ time from 30 to 60 s each Spanish squat: 5 reps, ↑ time from 30 to 60 s each | Complete exercises daily Concentric double-legged knee extensions: 3 × 10 at tolerable weight, ↑ to 3 × 15, guided by pain-monitoring models as tolerated 25° Double-legged decline squats: approximately 30-s count; monitor tolerance and progress to single-limb loads guided by pain-monitoring models as tolerated | Exercises 3–5×/wk 25° Single-legged decline squats: approximately 30-s count with progressive load ↑ Squat: 4 sets × 15 RM Leg press: 4 sets × 15 RM Hack squat: 4 sets × 15 RM Progress patients to 6 RM using the pain-monitoring models as tolerated. | Exercises 2–3×/wk 25° Single-legged decline squats: approximately 30-s count with progressive load ↑ Squat: 4 sets × 6 RM Leg press: 4 sets × 6 RM Hack squat: 4 sets × 6 RM Progress to greater loads as strength capacity ↑ |
| Adjuvant therapy | Quadriceps-stretching exercises Noxious transcutaneous electrical nerve stimulation Low-powered laser therapy or iontophoresis | Quadriceps-stretching exercises Patellar tendon strapping during activity | Quadriceps-stretching exercises Patellar tendon strapping during activity | Quadriceps-stretching exercises |
Abbreviations: rep, repetition; RM, repetition maximum.
Exercises, timing, and load-management strategies are provided as an example and may require individualization based on the patient's symptoms, function, and goals.
Load-Management Strategies
For improving patellar tendinopathy–related symptoms and function, rest and passive modalities are inferior to exercise and progressive loading regiments.43 Thus, modifications and optimization of training loads throughout the recovery process are paramount to initially reduce patellar tendon stress, followed by progressive increases to improve tendon health.44 Load-management programs that involve reducing the volume and frequency of sporting or other exacerbating activities have been used successfully to manage initial symptoms and pain.45 Appropriate load management can be monitored and progressed using a pain-monitoring model. Pain-monitoring models most commonly rely on visual analog scales. The pain-monitoring model described by Silbernagel et al44 for patients with Achilles tendinopathy may be broadened for use with all tendinopathies: 5 points out of 10 on a numeric pain-rating scale is considered the threshold for allowable pain. Reaching a score of 5 during and after the exercise protocol is acceptable, but the tendon pain must be <5 the following day. If a patient reports an increased level of pain from week to week, the activity should be reduced.
A collaborative approach involving the sports medicine clinicians, strength and conditioning staff, and coaching staff is necessary to achieve appropriate load management. This also requires patient education and involvement in the decision-making processes (“buy in”) to ensure the greatest opportunity for success using conservative management techniques. Incorporating these professionals and the patient into the discussion of activity modification allows the athlete to continue to train or practice with limitations while minimizing the loss of skill development. For example, blocking drills in volleyball often use shuffle steps with maximum vertical jump blocking and a coordination of front-row players to “double block.” In the symptom-management and load-reduction phase, this drill could be modified by eliminating the vertical jump, which allows the athlete and his or her teammates to continue participating and maintaining their court awareness while reducing the load on the athlete's patellar tendon. In the recovery phase, this activity can be progressed by allowing submaximal jumping and touching only the top of the net. Later in the rebuilding phase, the vertical jumping component can be progressively increased to reintegrate the athlete into unrestricted sport participation.
Exercise Protocols
Exercise regimens consisting of progressive tendon loading have demonstrated the most consistent evidence for treating and providing long-term improvements in individuals with patellar tendinopathy.43 Tensile stresses are created within the patellar tendon during quadriceps-muscle contraction. Therefore, patellar tendon–loading exercise programs should be centered on quadriceps-strengthening exercises. Quadriceps-strengthening exercises can be effectively progressed using various methods that include increases in velocity, load, or volume.46 This allows the clinician to customize eccentric programs for specific athletes or sport positions. For example, an endurance athlete may benefit from progressions with increases in exercise volume, whereas an athlete who relies more on power may benefit from increases in velocity or load.
Eccentric quadriceps-strengthening programs have been the most studied and were shown to be effective in improving long-term pain and patient-reported outcomes. For any quadriceps-strengthening program, the pain-monitoring model can again be used to progress training loads adequately and appropriately. For eccentric protocols, the most common and effective programs include decline squats completed at a slow speed on a 25° slant board (Figure 4).47 Static stretching of the quadriceps combined with eccentric quadriceps strengthening may provide greater benefits than strengthening alone.48 Dimitrios et al48 had participants perform static stretching of the quadriceps and hamstrings muscles before and after strengthening exercises. The group that performed stretching combined with eccentric training demonstrated better outcomes at the end of treatment and at the 6-month follow-up than the eccentric-only group.48 SOR: A
Figure 4.

The 25° decline squat.
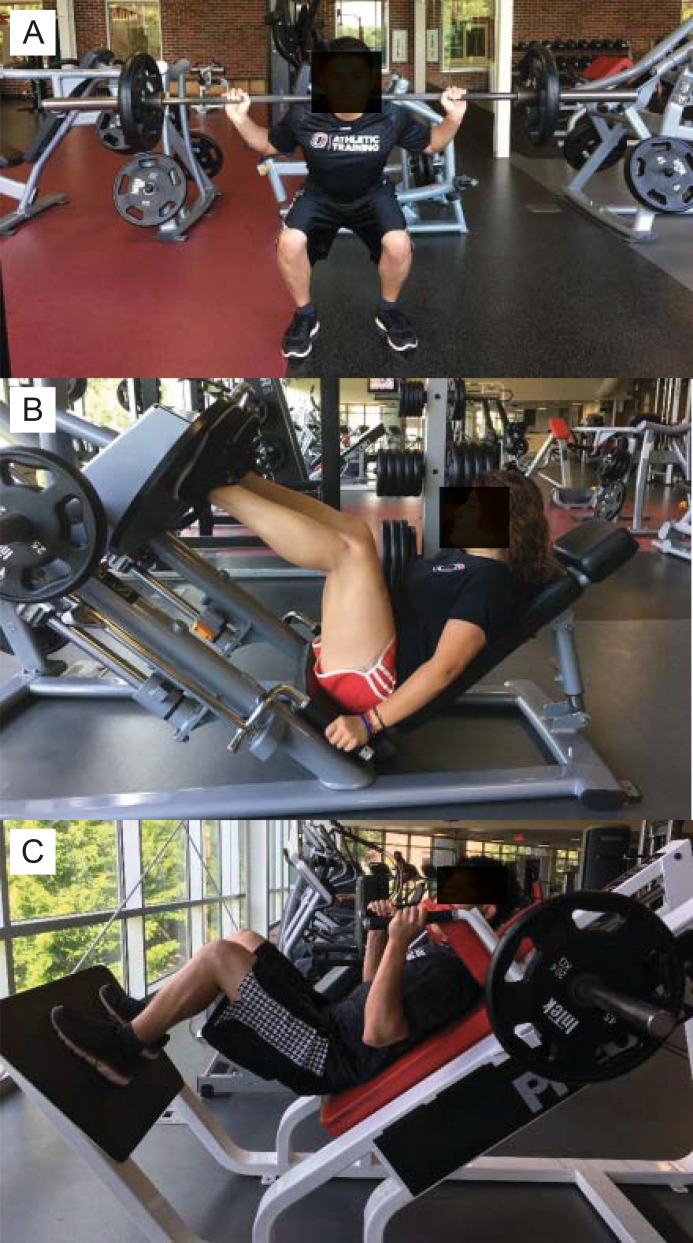
Protocols that progressively load the tendon through other methods of slow, heavy resistance exercises, such as concentric and isometric quadriceps-muscle contractions, may be less painful than eccentric quadriceps strengthening and can also result in long-term pain reduction and tendon healing. Recently, Breda et al49 reported that a progressive technique using a 3-stage approach of isometric, isotonic, and sport-specific loading in patients with patellar tendinopathy led to better subjective functional outcomes compared with eccentric loading alone. However, ultrasound imaging revealed no differences in markers of tendon healing. Kongsgaard et al38 observed that a heavy, slow, concentric and eccentric resistive-exercise protocol demonstrated better tendon morphologic changes and subjective function than eccentric exercises alone. The slow, heavy, concentric and eccentric resistive-exercise protocol38 used a progressive increase in load during the squat, leg press, and hack squat (Figure 5), each completed with 4 sets of 6-second repetitions (3 seconds concentric, 3 seconds eccentric). Their weekly progression began with a 15-repetition maximum (RM) during the first week, followed by a 12-RM during the second and third weeks, a 10-RM in weeks 4 and 5, an 8-RM in weeks 6 through 8, and finally a 6-RM in weeks 9 to 12.38 SOR: A
Figure 5.
A, Squat, B, leg press, and, C, hack squat.
Although progressive loading through slow, heavy quadriceps-resistance exercises has produced long-term effectiveness, in-season sport quadriceps isometric protocols may provide short-term pain relief to limit time loss during the season. Isometric exercises may improve adherence during the season, offering an alternative to more painful treatments such as eccentric or heavy, slow resistance exercises.50 In 1 study,51 a technique known as the Spanish or Catalan squat was used with a rigid belt or exercise band, and patients completed 5 repetitions of 30 seconds each (Figure 6). An alternate isometric exercise protocol used a leg-extension machine with the knee at 60° of flexion and 5 repetitions of 45 seconds each.52 These isometric protocols resulted in significant short-term pain relief for patients with patellar tendinopathy. SOR: B
Figure 6.

Spanish or Catalan squat using an exercise band.
Supportive Treatments
Therapeutic interventions and injection therapies beyond exercise regimens may offer symptomatic relief but typically only short-term benefits for tendon health. Several modalities that are standard in sports medicine clinics and are often used to treat tendinopathy have little evidence to support their use clinically. Contributing to the lack of clarity, research studies have often lacked a control or placebo group or frequently combined these adjuvant therapies with exercise regimens, muddling their efficacy as separate entities, or both.38,43,45,47,53,54 Therefore, we suggest supportive treatments be used only in combination with progressive quadriceps-strengthening and patellar tendon–loading programs.38,43,45,47,53,54 The 1 group55 that assessed low-powered laser therapy plus eccentric training for treating patellar tendinopathy found improvements in the VISA-P and pain, but multiple randomized controlled trials43 have demonstrated moderate effectiveness in reducing lateral elbow tendinopathy pain (SOR: A). Only single studies have been completed on iontophoresis and dry needling, and both produced short-term pain relief in patients with patellar tendinopathy (SOR: C).54 Neuromuscular stimulation in combination with quadriceps-muscle strengthening was assessed in 1 case series53 of 6 patients with patellar tendinopathy and resulted in decreased pain (SOR: C). In addition, some evidence56 suggests that localized noxious pain protocols as well as low- and high-frequency transcutaneous electrical nerve stimulation may relieve short-term pain in patients with lateral elbow tendinopathy, but again, this has not been studied in populations with patellar tendinopathy. Compared with placebo treatments, nonthermal ultrasound showed no differences and offered no therapeutic benefits to patients.47 SOR: A
Taping and strapping have been used to provide relief during sport activities. Patellar tendon strapping provided an approximately 25% reduction in pain with immediate application.57 Only 1 set of authors58 has evaluated Kinesio Taping as a potential therapy for patellar tendinopathy: they noted a small to moderate pain decrease versus sham taping. Neither of these techniques has demonstrated long-term benefits or an effect on tendon properties. SOR: B
Another treatment often used to manage patellar tendinopathy is injection-based treatments such as corticosteroids and platelet-rich plasma (PRP) therapy. Although corticosteroid injections displayed good short-term (approximately 1 week) pain relief, they provided little long-term benefit and are potentially harmful via joint, cartilage, and tendon degeneration and, thus, should be avoided (SOR: A).38,59 Platelet-rich plasma has been suggested as a viable treatment to assist in patellar tendinopathy recovery; however, the quality of research on its use is lacking (SOR: B).43 Leukocyte-rich PRP shows more promise than its leukocyte-poor counterpart.60 Furthermore, investigators61 in 1 study found that approximately 80% of participants returned to their previous sporting activities after PRP treatments; results were poorer in patients who had a longer history of symptoms. As such, leukocyte-rich PRP may be a viable option in patients who have failed to improve on other forms of conservative therapy. If PRP is determined to be appropriate, the injections should be performed under ultrasound guidance to identify the exact location of the tendinopathy.59
Surgical Interventions
In the most severe and chronic cases of advanced patellar tendinopathy, surgical intervention may be warranted. Surgery is typically not considered unless extensive conservative management for >6 months has failed to relieve symptoms.4 Although arthroscopic procedures have been described, open debridement with or without repair remains a reliable procedure.4 Surgical techniques involve identification of the macroscopically abnormal tissue (see Supplemental Figure, available online at https://doi.org/10.4085/1062-6050-0049.21.S1) with excision back to normal-appearing tissue borders.4 Depending on the volume of tissue involved and surgeon preference, subsequent repair of the tendon back to the patella can be undertaken. In 1 study4 of open procedures, patients had symptoms for an average of 3.8 years, had ceased sporting activities for approximately 7 months, and returned to participation between 7 and 12 months postoperatively. However, the outcomes of surgical interventions have been mixed. The authors62 of a recent systematic review concluded that surgery was no better than sham surgery in improving pain, function, or range of motion among patients with patellar tendinopathy. SOR: A
SUMMARY
Patellar tendinopathy is a complex condition that requires a multidisciplinary and multifaceted approach to ensure patient recovery. Understanding its pathophysiology and performing a comprehensive assessment will guide the clinician through treatment. Load-management strategies combined with tendon-loading exercise protocols are the most consistent and effective treatments for improving long-term outcomes in patients with patellar tendinopathy. Traditional modalities are supportive and may assist in pain relief, whereas more complex, persistent cases may require surgical intervention. Regardless of the treatment, patellar tendinopathy requires a lengthy course of appropriate rehabilitation and vigilance by both the patient and clinician.
Supplementary Material
SUPPLEMENTAL MATERIAL
Found at DOI: https://doi.org/10.4085/1062-6050-0049.21.S1
REFERENCES
- 1.Barber Foss KD, Myer GD, Chen SS, Hewett TE. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train . 2012;47(5):519–524. doi: 10.4085/1062-6050-47.5.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med . 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan KM, Maffulli N, Coleman BD, Cook JL, Taunton JE. Patellar tendinopathy: some aspects of basic science and clinical management. Br J Sports Med . 1998;32(4):346–355. doi: 10.1136/bjsm.32.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook JL, Khan KM, Harcourt PR, Grant M, Young DA, Bonar SF. A cross sectional study of 100 athletes with jumper's knee managed conservatively and surgically: the Victorian Institute of Sport Tendon Study Group. Br J Sports Med . 1997;31(4):332–336. doi: 10.1136/bjsm.31.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ . 2002;324(7338):626–627. doi: 10.1136/bmj.324.7338.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dakin SG, Martinez FO, Yapp C, et al. Inflammation activation and resolution in human tendon disease. Sci Transl Med . 2015. 7(311):311ra173. [DOI] [PMC free article] [PubMed]
- 7.Millar NL, Silbernagel KG, Thorborg K, et al. Tendinopathy. Nat Rev Dis Primers . 2021;7(1):1. doi: 10.1038/s41572-020-00234-1. [DOI] [PubMed] [Google Scholar]
- 8.Cannell LJ, Taunton JE, Clement DB, Smith C, Khan KM. A randomised clinical trial of the efficacy of drop squats or leg extension/leg curl exercises to treat clinically diagnosed jumper's knee in athletes: pilot study. Br J Sports Med . 2001;35(1):60–64. doi: 10.1136/bjsm.35.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebell MH, Siwek J, Weiss BD, et al. Strength of Recommendation Taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract . 2004;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 10.Albers IS, Zwerver J, Diercks RL, Dekker JH, Van den Akker-Scheek I. Incidence and prevalence of lower extremity tendinopathy in a Dutch general practice population: a cross sectional study. BMC Musculoskelet Disord . 2016;17:16. doi: 10.1186/s12891-016-0885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sport Exerc . 2013;45(3):462–469. doi: 10.1249/MSS.0b013e318277acca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lian OB, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross-sectional study. Am J Sport Med . 2005;33(4):561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 13.Benca E, Listabarth S, Flock FKJ, et al. Analysis of running-related injuries: the Vienna study. J Clin Med . 2020;9(2):428. doi: 10.3390/jcm9020438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fenwick SA, Hazleman BL, Riley GP. The vasculature and its role in the damaged and healing tendon. Arthritis Res . 2002;4(4):252–260. doi: 10.1186/ar416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peace KA, Lee JC, Healy J. Imaging the infrapatellar tendon in the elite athlete. Clin Radiol . 2006;61(7):570–578. doi: 10.1016/j.crad.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Almekinders LC, Vellema JH, Weinhold PS. Strain patterns in the patellar tendon and the implications for patellar tendinopathy. Knee Surg Sports Traumatol Arthrosc . 2002;10(1):2–5. doi: 10.1007/s001670100224. [DOI] [PubMed] [Google Scholar]
- 17.Moore JS. Function, structure, and responses of components of the muscle-tendon unit. Occup Med . 1992;7(4):713–740. [PubMed] [Google Scholar]
- 18.Sprague AL, Smith AH, Knox P, Pohlig RT. Grävare Silbernagel K. Modifiable risk factors for patellar tendinopathy in athletes: a systematic review and meta-analysis. Br J Sports Med . 2018;52(24):1575–1585. doi: 10.1136/bjsports-2017-099000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil . 2004;85(5):815–822. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 20.Jeon H, McGrath ML, Grandgenett N, Rosen AB. Clinical measures and their contribution to dysfunction in individuals with patellar tendinopathy. J Sport Rehabil . 2019;28(2):165–170. doi: 10.1123/jsr.2017-0196. [DOI] [PubMed] [Google Scholar]
- 21.Rosen AB, Ko J, Simpson KJ, Kim SH, Brown CN. Lower extremity kinematics during a drop jump in individuals with patellar tendinopathy. Orthop J Sports Med . 2015;3(3):2325967115576100. doi: 10.1177/2325967115576100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bisseling RW, Hof AL, Bredeweg SW, Zwerver J, Mulder T. Relationship between landing strategy and patellar tendinopathy in volleyball. Br J Sports Med . 2007;41(7):e8. doi: 10.1136/bjsm.2006.032565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Reproducibility and clinical utility of tendon palpation to detect patellar tendinopathy in young basketball players. Victorian Institute of Sport Tendon Study Group. Br J Sports Med . 2001;35(1):65–69. doi: 10.1136/bjsm.35.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coombes BK, Mendis MD, Hides JA. Evaluation of patellar tendinopathy using the single leg decline squat test: is pain location important? Phys Ther Sport . 2020;46:254–259. doi: 10.1016/j.ptsp.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 25.McAuliffe S, McCreesh K, Culloty F, Purtill H, O'Sullivan K. Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis. Br J Sports Med . 2016;50(24):1516–1523. doi: 10.1136/bjsports-2016-096288. [DOI] [PubMed] [Google Scholar]
- 26.Crossley KM, Thancanamootoo K, Metcalf BR, Cook JL, Purdam CR, Warden SJ. Clinical features of patellar tendinopathy and their implications for rehabilitation. J Orthop Res . 2007;25(9):1164–1175. doi: 10.1002/jor.20415. [DOI] [PubMed] [Google Scholar]
- 27.Rosen AB, Ko J, Brown CN. The relationship between acute pain and dynamic postural stability indices in individuals with patellar tendinopathy. Gait Posture . 2018;65:117–120. doi: 10.1016/j.gaitpost.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 28.Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper's knee in male athletes: a prospective follow-up study. Am J Sports Med . 2002;30(5):689–692. doi: 10.1177/03635465020300051001. [DOI] [PubMed] [Google Scholar]
- 29.Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, part I: terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med . 2016;50(14):839–843. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warden SJ, Kiss ZS, Malara FA, Ooi ABT, Cook JL, Crossley KM. Comparative accuracy of magnetic resonance imaging and ultrasonography in confirming clinically diagnosed patellar tendinopathy. Am J Sport Med . 2007;35(3):427–436. doi: 10.1177/0363546506294858. [DOI] [PubMed] [Google Scholar]
- 31.Helland C, Bojsen-Moller J, Raastad T, et al. Mechanical properties of the patellar tendon in elite volleyball players with and without patellar tendinopathy. Br J Sports Med . 2013;47(13):862–868. doi: 10.1136/bjsports-2013-092275. [DOI] [PubMed] [Google Scholar]
- 32.Pfirrmann CW, Jost B, Pirkl C, Aitzetmuller G, Lajtai G. Quadriceps tendinosis and patellar tendinosis in professional beach volleyball players: sonographic findings in correlation with clinical symptoms. Eur Radiol . 2008;18(8):1703–1709. doi: 10.1007/s00330-008-0926-9. [DOI] [PubMed] [Google Scholar]
- 33.Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Prospective imaging study of asymptomatic patellar tendinopathy in elite junior basketball players. J Ultrasound Med . 2000;19(7):473–479. doi: 10.7863/jum.2000.19.7.473. [DOI] [PubMed] [Google Scholar]
- 34.Yu JS, Popp JE, Kaeding CC, Lucas J. Correlation of MR imaging and pathologic findings in athletes undergoing surgery for chronic patellar tendinitis. AJR Am J Roentgenol . 1995;165(1):115–118. doi: 10.2214/ajr.165.1.7785569. [DOI] [PubMed] [Google Scholar]
- 35.Vicenzino B, de Vos RJ, Alfredson H, et al. ICON 2019—International Scientific Tendinopathy Symposium Consensus: there are nine core health-related domains for tendinopathy (CORE DOMAINS): Delphi study of healthcare professionals and patients. Br J Sports Med . 2020;54(8):444–451. doi: 10.1136/bjsports-2019-100894. [DOI] [PubMed] [Google Scholar]
- 36.Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis): Victorian Institute of Sport Tendon Study Group. J Sci Med Sport . 1998;1(1):22–28. doi: 10.1016/s1440-2440(98)80005-4. [DOI] [PubMed] [Google Scholar]
- 37.Hernandez-Sanchez S, Hidalgo MD, Gomez A. Responsiveness of the VISA-P scale for patellar tendinopathy in athletes. Br J Sports Med . 2014;48(6):453–457. doi: 10.1136/bjsports-2012-091163. [DOI] [PubMed] [Google Scholar]
- 38.Kongsgaard M, Kovanen V, Aagaard P, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports . 2009;19(6):790–802. doi: 10.1111/j.1600-0838.2009.00949.x. [DOI] [PubMed] [Google Scholar]
- 39.Owoeye OBA, Wiley JP, Walker REA, Palacios-Derflingher L, Emery CA. Diagnostic accuracy of a self-report measure of patellar tendinopathy in youth basketball. J Orthop Sport Phys Ther . 2018;48(10):758–766. doi: 10.2519/jospt.2018.8088. [DOI] [PubMed] [Google Scholar]
- 40.Huskisson EC. Measurement of pain. Lancet . 1974;2(7889):1127–1131. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 41.Snyder AR, Parsons JT, Valovich McLeod TC, Curtis Bay R, Michener LA, Sauers EL. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part I: disablement models. J Athl Train . 2008;43(4):428–436. doi: 10.4085/1062-6050-43.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Silbernagel KG, Hanlon S, Sprague A. Current clinical concepts: conservative management of Achilles tendinopathy. J Athl Train . 2020;55(5):438–447. doi: 10.4085/1062-6050-356-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Irby A, Gutierrez J, Chamberlin C, Thomas SJ, Rosen AB. Clinical management of tendinopathy: a systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scand J Med Sci Sports . 2020;30(10):1810–1826. doi: 10.1111/sms.13734. [DOI] [PubMed] [Google Scholar]
- 44.Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sport Med . 2007;35(6):897–906. doi: 10.1177/0363546506298279. [DOI] [PubMed] [Google Scholar]
- 45.Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med . 2013;43(4):267–286. doi: 10.1007/s40279-013-0019-z. [DOI] [PubMed] [Google Scholar]
- 46.Couppé C, Svensson RB, Silbernagel KG, Langberg H, Magnusson SP. Eccentric or concentric exercises for the treatment of tendinopathies? J Orthop Sports Phys Ther . 2015;45(11):853–863. doi: 10.2519/jospt.2015.5910. [DOI] [PubMed] [Google Scholar]
- 47.Larsson ME, Käll I, Nilsson-Helander K. Treatment of patellar tendinopathy—a systematic review of randomized controlled trials. Knee Surg Sports Traumatol Arthosc . 2012;20(8):1632–1646. doi: 10.1007/s00167-011-1825-1. [DOI] [PubMed] [Google Scholar]
- 48.Dimitrios S, Pantelis M, Kalliopi S. Comparing the effects of eccentric training with eccentric training and static stretching exercises in the treatment of patellar tendinopathy: a controlled clinical trial. Clin Rehabil . 2012;26(5):423–430. doi: 10.1177/0269215511411114. [DOI] [PubMed] [Google Scholar]
- 49.Breda SJ, Oei EHG, Zwerver J, et al. Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial. Br J Sports Med . 2021;55(9):501–509. doi: 10.1136/bjsports-2020-103403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vang C, Niznik A. The effectiveness of isometric contractions compared with isotonic contractions in reducing pain for in-season athletes with patellar tendinopathy. J Sport Rehabil . 2020;30(3):512–515. doi: 10.1123/jsr.2019-0376. [DOI] [PubMed] [Google Scholar]
- 51.Rio E, Purdam C, Girdwood M, Cook J. Isometric exercise to reduce pain in patellar tendinopathy in-season: is it effective “on the road”? Clin J Sport Med . 2019;29(3):188–192. doi: 10.1097/JSM.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 52.van Ark M, Cook JL, Docking SI, et al. Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. J Sci Med Sport . 2016;19(9):702–706. doi: 10.1016/j.jsams.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 53.Basas Á, Cook J, Gómez MA, et al. Effects of a strength protocol combined with electrical stimulation on patellar tendinopathy: 42 months retrospective follow-up on 6 high-level jumping athletes. Phys Ther Sport . 2018;34:105–112. doi: 10.1016/j.ptsp.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 54.Mendonça LM, Leite HR, Zwerver J, Henschke N, Branco G, Oliveira VC. How strong is the evidence that conservative treatment reduces pain and improves function in individuals with patellar tendinopathy? A systematic review of randomised controlled trials including GRADE recommendations. Br J Sports Med . 2020;54(2):87–93. doi: 10.1136/bjsports-2018-099747. [DOI] [PubMed] [Google Scholar]
- 55.Evangelos N, Anorthosis P, Dimitrios S, Lamnisos D. Treatment of chronic patellar tendinopathy using an exercise program consisting of eccentric training and static stretching exercises combined with high intensity light therapy: a pilot study. MOJ Orthop Rheumatol . 2018;10(2):157–161. doi: 10.15406/mojor.2018.10.00405. [DOI] [Google Scholar]
- 56.Dingemanse R, Randsdorp M, Koes BW, Huisstede BM. Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review. Br J Sports Med . 2014;48(12):957–965. doi: 10.1136/bjsports-2012-091513. [DOI] [PubMed] [Google Scholar]
- 57.Rosen AB, Ko J, Brown CN. Single-limb landing biomechanics are altered and patellar tendinopathy related pain is reduced with acute infrapatellar strap application. Knee . 2017;24(4):761–767. doi: 10.1016/j.knee.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 58.Freedman SR, Brody LT, Rosenthal M, Wise JC. Short-term effects of patellar kinesio taping on pain and hop function in patients with patellofemoral pain syndrome. Sports Health . 2014;6(4):294–300. doi: 10.1177/1941738114537793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fredberg U, Bolvig L, Pfeiffer-Jensen M, Clemmensen D, Jakobsen BW, Stengaard-Pedersen K. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper's knee and Achilles tendinitis: a randomized, double-blind, placebo-controlled study. Scand J Rheumatol . 2004;33(2):94–101. doi: 10.1080/03009740310004126. [DOI] [PubMed] [Google Scholar]
- 60.Fitzpatrick J, Bulsara M, Zheng MH. The effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials. Am J Sports Med . 2017;45(1):226–233. doi: 10.1177/0363546516643716. [DOI] [PubMed] [Google Scholar]
- 61.Filardo G, Kon E, Di Matteo B, Pelotti P, Di Martino A, Marcacci M. Platelet-rich plasma for the treatment of patellar tendinopathy: clinical and imaging findings at medium-term follow-up. Int Orthop . 2013;37(8):1583–1589. doi: 10.1007/s00264-013-1972-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Challoumas D, Clifford C, Kirwan P, Millar NL. How does surgery compare to sham surgery or physiotherapy as a treatment for tendinopathy? A systematic review of randomised trials. BMJ Open Sport Exerc Med . 2019;5(1):e000528. doi: 10.1136/bmjsem-2019-000528. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.