Abstract
Background
Treatment of acetabular dysplasia with a periacetabular osteotomy (PAO) has been shown to improve long term outcomes and is considered the gold standard in the setting of symptomatic hip dysplasia in patients younger than 35 years of age. Post-operative rehabilitation following a PAO plays an important role in helping patients return to their prior level of function and reduce the impact of strength deficits that may persist. Currently, there is a paucity of research supporting post-operative rehabilitation guidelines. The purpose of this study is to present expert-driven rehabilitation guidelines to reduce practice variation following a PAO.
Methods
A panel of 16 physiotherapists from across the United States and Canada who were identified as experts in PAO rehabilitation by high-volume hip preservation surgeons participated in this Delphi study. Panelists were presented with 11 questions pertaining to rehabilitation guidelines following a PAO. Three iterative survey rounds were presented to the panelists based on responses to these questions. This three-step Delphi method was utilized to establish consensus on post-operative rehabilitation guidelines following a PAO.
Results
Total (100%) participation was achieved for all three survey rounds. Consensus (>75%) was reached for 11/11 questions pertaining to the following areas: 1) weight-bearing and range of motion (ROM) precautions, 2) therapeutic exercise prescription including neuromuscular control, cardiovascular exercise, and flexibility, and 3) objective measures for return to straight line running and return to full participation in sports.
Conclusion
This Delphi study established expert-driven rehabilitation guidelines for use following a PAO. The standardization of rehabilitative care following PAO is essential for achieving optimal outcomes despite other factors such as geographical location and socioeconomic status. Further research on patient-reported outcomes is necessary to confirm successful rehabilitation following the guidelines outlined in this study.
Keywords: periacetabular osteotomy, rehabilitaiton, consensus statement, return to sport
BACKGROUND
Acetabular dysplasia, defined as a bony abnormality of the acetabulum with abnormal coverage of the femoral head, is a well-recognized cause of hip pain in young adults.1,2 This structural abnormality leads to a decrease in contact area of the hip, excessive wear on the articular cartilage, and degenerative changes of the acetabular labrum.3–5 Acetabular dysplasia can lead to severe pain, disability, and early onset arthritis without appropriate management.6,7 Treatment of acetabular dysplasia with a periacetabular osteotomy (PAO) has been shown to improve long-term outcomes and is considered the gold standard for symptomatic hip dysplasia.8–11 Although post-operative rehabilitation is important to help patients return to prior level of function, there a paucity of research supporting post-operative rehabilitation guidelines following a PAO.
Inadequate rehabilitation after PAO may lead to poor outcomes, which may include prolonged impairments in hip strength. It is well accepted that adequate strength of the lumbopelvic stabilizers is necessary to provide stability to the hip joint and maintain appropriate pelvic positioning during weight-bearing tasks.12,13 While improvements in isometric hip flexion and abduction are observed at one year following a PAO, strength values were shown to remain 13-34% lower than that of healthy controls.14 Other studies have reported similar improvements in hip abductor, hip flexor, and hip extensor strength values one year following a PAO when compared to pre-operative values, but no comparison was done to healthy controls.15,16 Prolonged impairments in hip strength may lead to decreased performance on functional tasks as hip abductor weakness is associated with impaired hip kinematics during a single-leg squat task when compared to healthy controls.17
Understanding important rehabilitation parameters, including early weight-bearing and range of motion (ROM) precautions, exercise progression throughout recovery, and metrics for clearance to return-to-run and return-to-sport, is crucial to maximize patient recovery following a PAO. The purpose of this study is to present expert-driven rehabilitation guidelines to reduce practice variation following a PAO.
METHODS
Delphi Panel
The expert panel in PAO rehabilitation consisted of sixteen physiotherapists who were purposefully sampled from geographically different institutions spread throughout the United States and Canada. Participants were selected based on multiple criteria, including (1) treating at least 10 patients following PAO per year, (2) identified by high-volume hip preservation surgeons as an expert in the rehabilitation of PAO patients, and/or (3) experts in rehabilitation of non-arthritic hip disorders. All members consented to participate in this IRB exempted study, and participants were blinded to each other for the entire duration of the study.
Delphi Structure and Data Collection
A three-step classic Delphi method was used to establish consensus techniques in the diagnostic evaluation of pediatric ACL injuries.18 Consensus was defined a priori as ≥75%, which is moderate per standard Delphi methods to account for expected variation in a content area with little available evidence.19 Definitions of consensus level are commonly based on accepted standards such as voting percentages (simple majority, two-thirds majority, absolute majority) and a supermajority was deteremine most appropriate for this study.19 This study had the dual objective of achieving consensus and, equally importantly, understanding areas where consensus could not be reached and reasons for disagreement.
Panelists were presented with three iterative rounds of surveys. Questionnaires for rounds one through three were distributed online via an emailed link with responses de-identified for analysis. For each survey round, analysis of the participants’ responses was completed by two study members (AD and KE). Any disagreements were resolved by a third team member (MM).
In the first survey round, panelists were presented with eleven free-response questions regarding their physical rehabilitation practice:
What weight-bearing precautions do you use? What objective measures do you use to discharge crutches?
What range of motion precautions do you utilize postoperatively? How long do you follow these precautions? When do you expect the patient to achieve full range of motion?
How do you begin to rehabilitate the hip flexor complex? When do you begin to rehabilitate the hip flexor complex?
Do you limit active long lever hip flexion? If so, how long?
What exercises do you utilize to improve lower extremity lumbopelvic control?
What exercises do you utilize to strengthen the gluteus medius? What exercises do you avoid when strengthening the gluteus medius?
What exercises do you utilize to facilitate lumbopelvic neuromuscular control? When do you begin these exercises?
When do you initiate end range stretching?
When do you begin low level cardiovascular exercise? (ie. upright stationary biking and elliptical)
What objective measures do you utilize to determine if a patient is ready to begin running?
What criteria do you utilize to determine if a patient is ready to return to full participation in sports?
Panelists provided detailed descriptions of treatment parameters for each question. Responses were collected and coded for common thematic content. Responses reported by ≥50% of panelists were considered modal, while responses reported by ≥25% of panelists formed a second tier of responses.
In round two, panelists were presented the original questions along with the modal response derived from the first round of responses. Panelists were asked to agree or disagree with the modal response, and those who disagreed were allowed to add or subtract items. The second-tier responses were included as potential additions, but free text addition was also permitted. Resulting responses were again coded for thematic content and modal responses were adjusted as appropriate.
In round three, panelists again received ten of the eleven questions with revised modal and second-tier responses. Similar to round two, panelists were asked to agree or disagree with the modal response, and those who disagreed were allowed to add or detract items. Disagreement prompted a free-response box for the panelist to explicitly detail their disagreement. Analysis of the third-round data provided concepts for which consensus had been gained as well as rationale for disagreement.
RESULTS
The expert panel in this study consisted of sixteen physiotherapists who were identified as an expert in PAO rehabilitation. Overall, 100% participation was achieved with all sixteen therapists completing all three Delphi rounds. The expert panel received eleven questions covering a variety of topics related to rehabilitation following a PAO, and 100% consensus was achieved for all topics of interest by the third Delphi round.
Weight-Bearing Precautions
For weight-bearing precautions that should be utilized immediately following a PAO, 15/16 (94%) panelists agreed that weight-bearing should be limited to 25%, foot-flat weight-bearing for 6-8 weeks. It was noted that concomitant procedures, such as hip arthroscopy or microfracture, may prolong these recommendations.
Discharging Crutches
For objective measures to discharge crutches after 6-8 weeks of protected weight-bearing, 16/16 (100%) panelists agreed that observed gait deviations and surgeon clearance should be utilized. Examples of gait deviations listed in the question included Trendelenburg gait, abductor lurch, and antalgic gait.
ROM Precautions
For ROM precautions immediately following a PAO, 13/16 (81%) panelists agreed that flexion should be limited to 90 degrees and external rotation limited to 20 degrees in 90 degrees of flexion. The 13 panelists agreed that these precautions should be maintained for 4-6 weeks. It was noted that concomitant procedures, such as hip arthroscopy or microfracture, may prolong or alter these recommendations to include limitations in hip extension and hip internal rotation.
Two dissenting panelists had different points of contention. One panelist felt that flexion should be limited to 70 degrees for three weeks, and then limited to 90 degrees for the following week along with avoidance of rotation of the femur in flexion and avoidance of hip extension until the fourth week. The second panelist stated that there should be no flexion past 90 degrees and no external rotation in any range. For achieving full ROM following an isolated PAO, 16/16 (100%) panelists agreed that the patient should achieve full hip ROM by 12-16 weeks (3-4 months).
For the initiation of end range stretching, 15/16 (94%) panelists agreed that it can begin somewhere between 8-12 weeks post-operatively as tolerated. The one dissenting panelist stated that it should only occur as needed after 16 weeks post-operatively.
Protection of the Hip Flexor Complex
For rehabilitation of the hip flexor complex following a PAO, 16/16 (100%) panelists agreed to the general protocol:
Long lever active hip flexion in supine should be limited for 8-12 weeks following an isolated PAO.
Initiation of therapeutic exercise targeting the hip flexor complex should begin between 4-8 weeks as tolerated by pain.
Active assistive ROM (AAROM), heel slides, and/or isometrics should be utilized to initiate rehabilitation of hip flexor complex, progressing as tolerated
Lumbopelvic and Posterior-Lateral Hip Strengthening
For the initiation of lumbopelvic control following a PAO, 16/16 (100%) panelists agreed that a core progression should include supine and quadruped activities.
For strengthening of the gluteus medius following a PAO, 15/16 (94%) panelists agreed to the general guidelines:
In general, gluteus medius strengthening should begin with isometrics progressing to non-weight bearing (NWB) progressive resistance exercises followed by double and single leg weight bearing exercises. Other positions and different lever arms can be utilized to progress strengthening exercises.
Exercises that increase anterior hip activation/pain (ie. hip flexor and tensor fascia lata compensation) should be avoided when beginning gluteus med strengthening.
The dissenting panelist stated that strengthening of the gluteus medius should begin with isometric strength exercises, followed by functional movements, then progress to weight-bearing exercises.
Lumbopelvic and Lower Extremity Neuromuscular Control
For improving lower extremity neuromuscular control following a PAO, 14/16 (88%) panelists agreed to the general guidelines:
Double and single leg exercises in the closed chain challenging frontal plane control and femoral IR control (valgus).
These exercises can begin in NWB as the patient tolerates and should progress to WB at six weeks or immediately after the patient is cleared for WB.
Only one of the dissenting panelists provided a retort, stating initiation of lower extremity neuromuscular control should begin in passive weight-bearing positions, such as quadruped or tall kneeling prior to double or single leg.
Return to Sport Criteria
For beginning low level cardiovascular exercise following a PAO, 13/16 (81%) panelists agreed to the general guidelines that patients may begin upright stationary biking 6-8 weeks post-operatively and begin using an elliptical by 10-12 weeks. Only two of the three dissenting panelists elaborated on their disagreement. One of the panelists stated that stationary biking may begin at two weeks with no resistance, followed by walking in the pool at four weeks. The other panelist stated that stationary biking may begin at two weeks maintaining 90-degree flexion precautions, and the elliptical may begin when the patient is walking normally, progressing through strength exercises, and can bike for 30 minutes.
For objective measures to begin a running progression, 14/16 (88%) panelists agreed to the general guidelines:
Normalized hip strength (with a focus on glute med and ER strength)
Performance on functional tasks (SL squat, Y-Balance, etc)
The two dissenting panelists agreed to the above guidelines but thought that quad/hamstring strength and surgeon clearance with radiographic support were needed to progress to running as well.
For objective criteria required to return to sport, 16/16 (100%) panelists agreed to the guidelines:
Involved: uninvolved hip abductor strength ratio of >80%.
Performance on functional tasks (single leg squat, Y-balance).
Performance on sport specific drills chosen based on patient specific demands
DISCUSSION
This Delphi study was performed to establish consensus among physiotherapy experts for post-operative rehabilitation guidelines following a PAO. No studies currently exist supporting specific weight-bearing and ROM precautions, therapeutic exercise prescription, or metrics for clearance to return-run and return-to-sport. Therefore, the Delphi method was utilized to generate expert opinion in a content area where evidence is lacking. Across all three rounds of this study, 100% participation was achieved from the 16 physiotherapists and consensus was achieved across all domains. These post-operative guidelines may reduce unwanted practice variation and help patients achieve more normal hip strength values to maximize functional potential and minimize reinjury risk. A summary of recommendations can be found in Table 1.
Table 1. Summary of rehabilitation guidelines for use following a periacetabular osteotomy (PAO).
| PAO Rehabilitation Guidelines | ||
|---|---|---|
|
Phase I: Immediate Post-Operative Phase
Weeks 1-4 | ||
|
Goals: Protect healing tissues and osteotomy sites Reduce post-operative pain and inflammation Normalize gait pattern with appropriate assistive device |
Precautions: Weightbearing: Foot flat weight bearing 25% body weight Range of Motion: Hip flexion limited to 90° Hip external rotation limited to 20° Active long lever hip flexion contraindicated until 8-12 |
|
|
Therapeutic Interventions: Ankle pumps and submaximal hip isometric exercises Cryotherapy and compression for inflammation and edema control | ||
|
Phase II: Early Post-Operative Phase
Weeks 4-6 | ||
|
Goals: Gentle progression of ROM Continue protecting healing osteotomy sites Limit irritation of surrounding soft tissues with increasing activity |
Precautions: Weightbearing: Foot flat weight bearing 25% body weight Range of Motion: Hip flexion limited to 90° Hip external rotation limited to 20° Active long lever hip flexion contraindicated until week 8-12 |
|
|
Physical Therapy: Submaximal isometrics in all directions Gradual loading of iliopsoas tendon is critical to avoid tendonitis Short lever A/AAROM Lumbopelvic neuromuscular control exercises in supine | ||
|
Phase III: Initial Strengthening Phase
Weeks 6-12 | ||
|
Goals: Near full, symmetrical ROM Improve hip and core strength and neuromuscular control Gradual WB progression (normalized gait pattern and physician clearance required for discharging assistive device) |
Precautions: Monitor for symptoms of intra- and extra-articular irritation with exercise and WB progression Avoid premature weaning from assistive device Active long lever hip flexion contraindicated until week 8-12 |
|
|
Physical Therapy: Gradual progression of functional ROM Introduce upright stationary bike between 6-8 weeks Introduce elliptical between 10-12 weeks as tolerated Introduce stretching progression between 8-12 weeks Initiate closed chain strengthening progression Progress lumbopelvic stabilization and postural control exercises | ||
|
Phase IV: Advanced Strengthening Phase
Weeks 12-20 | ||
|
Goals: Increase muscular and cardiovascular endurance Begin to re-establish neuromuscular control for sport-specific activity |
Precautions: Avoid provocation of symptoms with progression of exercise No running, jumping, hopping, or cutting/pivoting |
|
|
Physical Therapy: Progress multi-directional hip and LE strengthening Progress to end range strengthening with emphasis on dynamic control of lower extremity and pelvis Core stability progression to meet demands of sport | ||
|
Phase V: Return to Low Level Impact
(Weeks 20-26) | ||
|
Goals: Tolerance of running and straight plane agility drills with appropriate lumbopelvic and lower extremity control |
Precautions: Avoid provocation of symptoms with progression of exercise No jumping, hopping, cutting/pivoting |
|
|
Physical Therapy: Initiate running and agility progressions with emphasis on dynamic control of pelvis and lower extremity Continue high level strength and control exercises with emphasis on pelvis and lower extremity musculature | ||
|
Phase V: Return to Full Participation in Sports
(Weeks 26+) | ||
|
Goals: Tolerance of jumping, hopping, cutting/pivoting drills with appropriate lumbopelvic and lower extremity control Return to full participation in sports |
Precautions: Avoid provocation of symptoms with progression of exercise |
|
|
Physical Therapy: Initiate jumping and hopping progression with emphasis on dynamic control of lower extremity and pelvis Sport specific cutting and pivoting drills with emphasis on dynamic control of lower extremity and pelvis | ||
Weight-Bearing Precautions
Consensus Point : Patients should ambulate with 25% foot-flat weight-bearing through the affected lower extremity for 6-8 weeks following a PAO. Crutches can be discharged after radiographic evidence of bony healing and a normalized gait pattern.
In the immediate post-operative phase, modified weight-bearing is utilized to allow for bony healing. Post-operative stress fractures have been reported as a complication in the literature with an incidence between 2-18.4%.20–22 Early weight-bearing, pubic non-union, a larger preoperative deformity, advanced age, and a higher post-operative center-edge angle have been identified as possible factors for developing a stress fracture following a PAO. Ito et al.23 reported a higher incidence of postoperative fractures of the ischial ramus and posterior column with full weight-bearing immediately following surgery compared to two months of modified weight-bearing. In a normal pelvis, load transfer is higher through the superior pubic ramus as compared to the inferior pubic ramus. However, following a PAO, increased load transfer occurs through the inferior pubic ramus, ischium, and posterior column.24 These changes in load transmission patterns increase stress and strain through these bony structures and potentially result in a post-operative stress fracture. Therefore, modified weight-bearing in the early post-operative phase is indicated. The current results are consistent with these recommendations as 15/16 participants recommend 25% foot-flat weight-bearing until 6-8 weeks at which point weight-bearing can be progressed only if the patient demonstrates radiographic evidence of bony healing and a normalized gait pattern. It was noted that concomitant procedures, such as hip arthroscopy or microfracture, may prolong these recommendations to protect the healing capsuloligamentous structures and joint cartilage.
Range of Motion Precautions
Consensus Point: Hip flexion and external rotation ROM should be protected for 4-6 weeks followed by progressive, pain-free restoration of ROM. End range stretching can be initiated between 8-12 weeks as tolerated with full ROM achieved by 12-16 weeks post-operatively.
Restoration of hip range of motion is essential to allow for participation in both daily and recreational activities. Similar to a hip arthroscopy, end ranges of motion should be protected in the early post-operative period. This includes end range flexion, which approximates the femur and the acetabulum, and hip external rotation, which stresses the anterior hip capsule. After a period of protected motion allowing for a reduction in inflammation and bony healing, a gradual approach to improving range of motion is essential to limit joint irritation. Consensus regarding all passive and active ROM precautions was achieved as panelists agreed that hip flexion and external rotation ROM should be limited for 4-6 weeks, with normal passive hip motion being achieved by 12-16 weeks. Panelists agreed the upright stationary bike can be initiated between 6-8 weeks and the elliptical trainer between 10-12 weeks to facilitate early-stage passive range of motion as well as cardiovascular endurance. In the setting of concomitant procedures, such as a hip arthroscopy, panelists indicated that ROM precautions may be altered to include extension or internal rotation to further protect healing soft tissue structures.
Protection of the Hip Flexor Complex
Consensus Point: Progressive loading of the hip flexor complex should be done cautiously, with isometrics and short-lever active assistive hip flexion exercises beginning between 4-8 weeks as indicated by pain. Long-lever active hip flexion should be avoided for 8-12 weeks following a PAO.
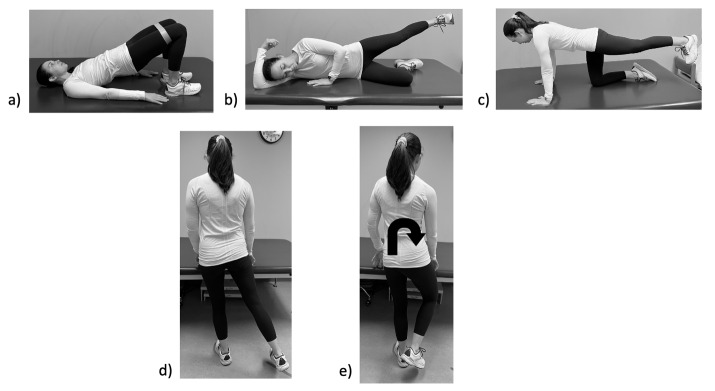
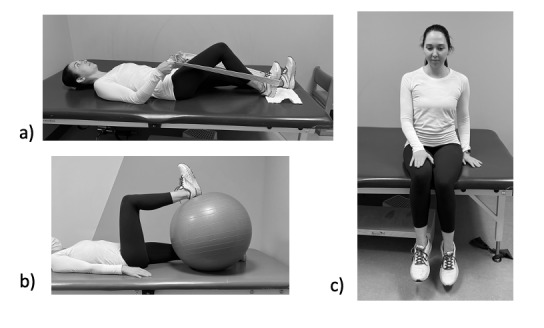
The iliopsoas courses directly anterior to the femoral head and acts as a secondary stabilizer to the hip joint.25 In the setting of hip dysplasia, the iliopsoas may overcompensate for the lack of bony stability and result in tendinous overload, inflammation, and pain.26,27 Furthermore, anecdotal evidence has linked weakness of the gluteus medius, which is a common finding in patients with dysplasia and a consequence of a PAO, to iliopsoas tendinitis.28 Following a PAO, the iliopsoas can impinge on the pubic osteotomy further predisposing these patients to hip flexor irritation.29 Extreme care should be taken to avoid additional hip flexor irritation in the early post-operative phase and therefore toe touch weight-bearing or non-weight-bearing during gait should be avoided. Instead, patients should ambulate with a foot-flat gait pattern to reduce activity of the iliopsoas. Progressive isometrics and short lever active assistive hip flexion exercises are recommended at 4-8 weeks to progressively load the iliopsoas tendon while all long lever hip flexion activities should be avoided for 8-12 weeks post-operatively. Recommended exercises to progressively load the hip flexor can be found in Figure 1. Additionally, strengthening exercises for the gluteus medius that also activate the anterior hip should be avoided, especially in the setting of iliopsoas pain. Philippon et al.28 reported sidelying hip abduction in external rotation and the clamshell exercises demonstrated considerable EMG activation of hip flexor. These findings support a recommendation that these exercises should be avoided or prescribed with caution in the presence of anterior hip pain.
Figure 1. Progressive loading of the iliopsoas including a) heel slides, b) physioball hip flexion, and c) isometric hip flexion in sitting.
Lumbopelvic and Posterior-Lateral Hip Strengthening
Consensus Statement: Lumbopelvic strengthening should begin in the early post-operative phase in non-weight-bearing and progress to double and single leg weightbearing exercises as tolerated.
The relationship with lumbopelvic and posterior-lateral hip muscle function to lower extremity injury has been demonstrated in the literature.30–35 One-year following PAO, patients demonstrate improvements in isometric hip flexion and abduction strength, however, these values were shown to remain 13-34% lower than that of healthy controls.14 Other studies have reported similar improvements hip abductor, hip flexor, and hip extensor strength values one year following a PAO when compared to pre-operative values, but no comparison was done to healthy controls.15,16 Additionally, it has been well established that females exhibit less hip strength, particularly in their hip abductors and external rotators, compared to males.33,36 Given that hip dysplasia is more prevalent in females and lumbopelvic strength lags post-operatively, extensive lumbopelvic strengthening is crucial for improving hip joint mechanics and maximizing outcome. Snyder et al.37 reported a strengthening program targeted at the hip abductors and external rotators altered lower extremity joint loading. In patients with hip dysplasia, strengthening of the hip abductors was shown to reduce dynamic instability during ambulation.38 Without normalization of strength, muscle imbalances in the hip and core can lead to altered force couple relationships and faulty joint arthrokinematics.39,40
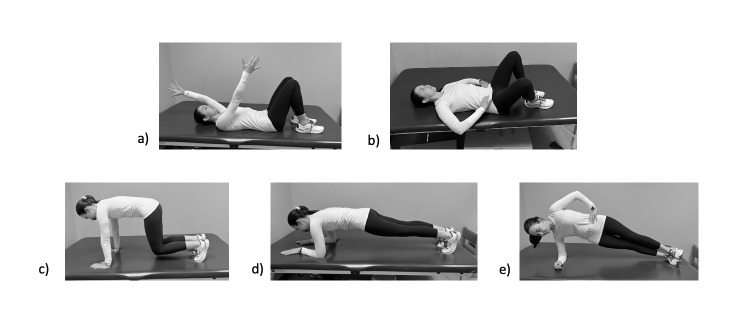
A graded approach to therapeutic exercise allows for improvements in strength while minimizing musculotendinous overload and joint irritation. This is an important concept following a PAO as the reorientation of the acetabulum affects the torque-generating capacities of the surrounding musculature which could may affect muscle strength and activation.41,42 Panelist consensus indicated that strengthening of the core muscles and gluteus medius should begin with non-weight-bearing isometrics and progress to single leg weight-bearing exercise as tolerated. The gluteus medius has been shown to demonstrate high EMG values in a single leg stance position.43,44 Therefore, when appropriate, exercises performed in a single-leg stance position should be a focus of post-operative rehabilitation to increase hip abductor strength. Recommended lumbopelvic strengthening exercises can be found in Figures 2 and 3.
Figure 2. Recommended exercises for posterior-lateral hip strengthening including a) double leg bridges with isometric hip abduction, b) sidelying hip abduction isometrics in neutral hip rotation, c) hip extension isometrics in quadruped, d) standing hip abduction, and e) weight-bearing hip external rotation.
Figure 3. Recommended exercises for lumbopelvic strengthening including a) hooklying transversus abdominis contraction with upper extremity flexion, b) hooklying transversus abdominis contraction with bent knee fall out, c) primal push up, d) forward plank, and e) side plank.
Lumbopelvic and Lower Extremity Neuromuscular Control
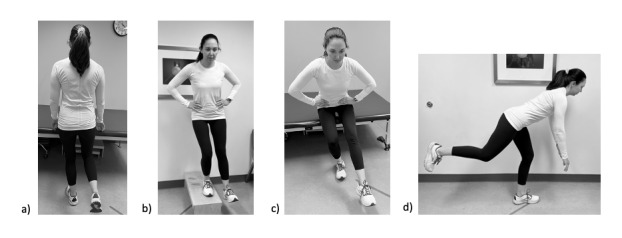
Consensus Statement: Lumbopelvic neuromuscular control exercises should begin in non-weight-bearing in the early post-operative phase with progression to weight-bearing exercises at 6-8 weeks or immediately after the patient is cleared for weight-bearing. In weight-bearing, exercises should consist of double and single leg exercises challenging frontal plane and femoral internal rotation control.
Neuromusuclar control training is utilized to improve functional performance, lower extremity biomechanics, and muscle activation patterns. Decreased neuromuscular control of the lumbopelvic region leads to uncontrolled trunk movement and lower extremity valgus, increasing the risk of lower extremity injury.45,46 During landing and pivoting movements, females demonstrate increased lower extremity valgus resulting in increased load through the lower extremity.47–51 The gluteus medius, gluteus maximus, and deep external rotators are responsible for maintaining stability of the pelvis in the closed chain while the core is responsible for providing a stable base for force transfer between the trunk and the lower extremity.39,52–56 The goal of rehabilitation is to improve dynamic stabilization of the hip, especially during single-leg weight-bearing tasks when loads within the hip are the highest.12,13,57 Myer et al.58 reported a 15% increase in hip abduction strength in healthy individuals with a 10-week targeted neuromuscular control training compared to no increase in strength in the control group. Similarly, Hewett et al.59 reported a significant improvement in hip external rotation moments and moment impulses, increased peak trunk flexion, and decreased peak trunk extension following a 10-week targeted neuromuscular control training program.
Panelists agreed that an emphasis should be placed on lumbopelvic and lower extremity neuromuscular control beginning in the immediate post-operative phase. Early education on the importance of the transversus abdomonis, which contributes to spinal stability during weight-bearing tasks, will set the foundation for appropriate lumbopelvic control for the later stages of recovery.60,61 These exercises should begin in supine during the immediate post-operative phase progressing to quadruped, tall-kneeling, and double and single leg stance as indicated. Recommended lumbopelvic and lower extremity neuromuscular control exercises can be found in Figure 4.
Figure 4. Recommended lumbopelvic and lower extremity neuromuscular control exercises including a) single leg stance, b) lateral step down, c) single leg squat, and d) single leg Romanian dead lift.
Return to Sport Criteria
Consensus Statement: The upright stationary bike can be initiated between 6-8 weeks and the elliptical trainer between 10-12 weeks to facilitate early-stage cardiovascular endurance, as well as passive range of motion of the hip. Panelists recommend utilizing a combination of strength, endurance, and functional performance measures during return to play testing, including but not limited to hip abductor to adductor strength ratios, the Y-Balance test, and various hop tests.
Return to sport is a goal of many patients undergoing a PAO, as these patients tend to be young, active individuals. Heyworth et al.62 found 80% of patients undergoing PAO procedures returned to play at a median of nine months post operatively with increased pain being the only independent predictor of delayed return. Of these patients, 73% returned to their previous level of sport. Takahashi et al.63 reported similar findings, with 72.2% of patients able to participate in both low and high impact sports following a PAO. It should be noted that no details were provided regarding rehabilitation protocols utilized in these studies. The importance of return to sport metrics to reduce reinjury rates has been well documented in the ACL literature, however, specific guidelines continue to remain elusive.64–69 Following hip arthroscopy, these guidelines are less defined with recommendations including the absence of pain and appropriate control during sport specific activities such as running, lateral agility, and single leg squats.70 These recommendations can serve as a guide when discussing return to sport following a PAO as none currently exist in the literature. Psychological readiness should also be considered during the return to sport phase as this may affect their ability to return to previous level of play and increase the risk of reinjury.71–74 A recent systematic review found positive psychological responses pertaining to motivation, confidence, and fear were associated with greater likelihood of returning to previous level of participation.73 It can be assumed that patients following a PAO will exhibit signs consistent with low confidence and fear given the longstanding nature of dysplasia symptoms and the extensive surgical procedure. These factors should be considered along with functional performance and strength measures when determining readiness to return to sport.
Panelists recommend utilizing a combination of strength, endurance, and functional performance measures during return to play testing, including but not limited to hip abductor/adductor strength ratios, single leg squats, and the star excursion balance test . Recommendations for objective measures for return to straight line running and return to full participation in sports can be found in Table 2.
Table 2. Author recommendations for objective criteria for utilization during return to straight line running and return to full participation in sport testing.
| Return to Straight Line Running | Return to Full Participation in Sports |
|---|---|
|
Range of Motion
Strength Testing
Endurance Testing†
Functional Testing†
|
Self-Reported Function
Strength and Range of Motion
Functional Testing†
Joint Loading Tasks†
Sport Specific Tasks†
|
†No reports of pain and appropriate lower extremity and pelvic control required during all tasks
Limitations
There are several limitations to our current study. There is a paucity of research supporting post-operative PAO rehabilitation guidelines. Ellis et al.75 published a rehabilitation protocol for use after concomitant PAO and hip arthroscopy, however, this Delphi study was focused on an isolated PAO. Therefore, initial study questions were generated by expert opinion which could result in bias. To minimize resultant bias in the modal responses, the authors recruited a diverse expert panel. It should be noted, however, that all panelists were from North America which may limit the international generalizability of our findings. Additionally, panelists completed all survey rounds on-line which does not allow for clarification or open discussion regarding survey items. Lastly, this Delphi study included recommendations pertaining to an isolated PAO, which does not cover the spectrum of possible concomitant procedures performed to address soft tissue injuries or revision procedures.
CONCLUSION
Although post-operative rehabilitation is important to help patients return to prior level of function, there a paucity of research supporting post-operative rehabilitation guidelines following a PAO. Inadequate rehabilitation after PAO may lead to poor outcomes, which may include prolonged impairments in hip strength. This Delphi study established expert-driven rehabilitation guidelines for use following a PAO. The standardization of rehabilitative care following PAO is essential for achieving optimal outcomes despite other factors such as geographical location and socioeconomic status. Further research on patient-reported outcomes is necessary to confirm successful rehabilitation following the guidelines outlined in this study.
Conflict of Interest Statement
The authors have no conflicts of interest.
Acknowledgments
Acknowledgements
We want to acknowledge all physiotherapists who put time and effort into answering all survey questions and provided feedback during this Delphi study. Their work was essential to creating this consensus statement.
References
- The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. Klaue K, Durnin C W, Ganz R. May;1991 The Journal of Bone and Joint Surgery. British volume. 73(3):423–429. doi: 10.1302/0301-620x.73b3.1670443. doi: 10.1302/0301-620x.73b3.1670443. [DOI] [PubMed] [Google Scholar]
- Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Henak C.R., Abraham C.L., Anderson A.E., Maas S.A., Ellis B.J., Peters C.L., Weiss J.A. Feb;2014 Osteoarthritis and Cartilage. 22(2):210–217. doi: 10.1016/j.joca.2013.11.003. doi: 10.1016/j.joca.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Nishii Takashi, Sugano Nobuhiko, Tanaka Hisashi, Nakanishi Katsuyuki, Ohzono Kenji, Yoshikawa Hideki. Feb;2001 Clinical Orthopaedics and Related Research. 383:183–190. doi: 10.1097/00003086-200102000-00020. doi: 10.1097/00003086-200102000-00020. [DOI] [PubMed] [Google Scholar]
- The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Crawford Matthew J, Dy Christopher J, Alexander Jerry W, Thompson Matthew, Schroder Steven J, Vega Charles E, Patel Rikin V, Miller Andrew R, McCarthy Joseph C, Lowe Walter R, Noble Philip C. Dec;2007 Clinical Orthopaedics & Related Research. 465:16–22. doi: 10.1097/blo.0b013e31815b181f. doi: 10.1097/blo.0b013e31815b181f. [DOI] [PubMed] [Google Scholar]
- Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Domb Benjamin G., Stake Christine E., Lindner Dror, El-Bitar Youssef, Jackson Timothy J. Aug 16;2013 The American Journal of Sports Medicine. 41(11):2591–2598. doi: 10.1177/0363546513499154. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. Murphy S B, Ganz R, Müller M E. Jul;1995 The Journal of Bone & Joint Surgery. 77(7):985–989. doi: 10.2106/00004623-199507000-00002. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- The John Charnley Award: Redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Wyles Cody C., Heidenreich Mark J., Jeng Jack, Larson Dirk R., Trousdale Robert T., Sierra Rafael J. Feb;2017 Clinical Orthopaedics & Related Research. 475(2):336–350. doi: 10.1007/s11999-016-4815-2. doi: 10.1007/s11999-016-4815-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14-year hip survivorship after periacetabular osteotomy: a follow-up study on 1,385 hips. Larsen Josefine Beck, Mechlenburg Inger, Jakobsen Stig Storgaard, Thilleman Theis Munchholm, Søballe Kjeld. Feb 28;2020 Acta Orthopaedica. 91(3):299–305. doi: 10.1080/17453674.2020.1731159. doi: 10.1080/17453674.2020.1731159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natural history of the dysplastic hip following modern periacetabular osteotomy. Wyles Cody C., Vargas Juan S., Heidenreich Mark J., Mara Kristin C., Peters Christopher L., Clohisy John C., Trousdale Robert T., Sierra Rafael J. May 15;2019 Journal of Bone and Joint Surgery. 101(10):932–938. doi: 10.2106/jbjs.18.00983. doi: 10.2106/jbjs.18.00983. [DOI] [PubMed] [Google Scholar]
- Periacetabular osteotomy: a systematic literature review. Clohisy John C., Schutz Amanda L., St. John Lauren, Schoenecker Perry L., Wright Rick W. Aug;2009 Clinical Orthopaedics & Related Research. 467(8):2041–2052. doi: 10.1007/s11999-009-0842-6. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Periacetabular osteotomy to treat residual dysplasia in adolescents and young adults: indications, complications, results. Millis M. B., McClincy M. Aug;2018 Journal of Children's Orthopaedics. 12(4):349–357. doi: 10.1302/1863-2548.12.180068. doi: 10.1302/1863-2548.12.180068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinesiology of the hip: a focus on muscular actions. Neumann Donald A. Feb;2010 Journal of Orthopaedic & Sports Physical Therapy. 40(2):82–94. doi: 10.2519/jospt.2010.3025. doi: 10.2519/jospt.2010.3025. [DOI] [PubMed] [Google Scholar]
- The architectural design of the gluteal muscle group: implications for movement and rehabilitation. Ward Samuel R., Winters Taylor M., Blemker Silvia S. Feb;2010 Journal of Orthopaedic & Sports Physical Therapy. 40(2):95–102. doi: 10.2519/jospt.2010.3302. doi: 10.2519/jospt.2010.3302. [DOI] [PubMed] [Google Scholar]
- Isometric hip strength impairments in patients with hip dysplasia are improved but not normalized 1 year after periacetabular osteotomy: a cohort study of 82 patients. Jacobsen Julie Sandell, Jakobsen Stig Storgaard, Søballe Kjeld, Hölmich Per, Thorborg Kristian. Oct 11;2021 Acta Orthopaedica. 92(6):765–765. doi: 10.1080/17453674.2021.1986292. doi: 10.1080/17453674.2021.1986292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscle strength improves after abductor-sparing periacetabular osteotomy. Ezoe Masamitsu, Naito Masatoshi, Asayama Isao. Mar;2006 Clinical Orthopaedics & Related Research. 444:161–168. doi: 10.1097/01.blo.0000196475.40151.8b. doi: 10.1097/01.blo.0000196475.40151.8b. [DOI] [PubMed] [Google Scholar]
- Gait, hip strength and functional outcomes after a Ganz periacetabular osteotomy for adolescent hip dysplasia. Sucato Daniel J., Tulchin Kirsten, Shrader Michael Wade, DeLaRocha Adriana, Gist Taylor, Sheu Geraldine. Jun;2010 Journal of Pediatric Orthopaedics. 30(4):344–350. doi: 10.1097/bpo.0b013e3181d9bfa2. doi: 10.1097/bpo.0b013e3181d9bfa2. [DOI] [PubMed] [Google Scholar]
- Hip kinematics during single-leg tasks in people with and without hip-related groin pain and the association among kinematics, hip muscle strength, and bony morphology. Harris-Hayes Marcie, Hillen Travis J., Commean Paul K., Harris Michael D., Mueller Michael J., Clohisy John C., Salsich Gretchen B. May;2020 Journal of Orthopaedic & Sports Physical Therapy. 50(5):243–251. doi: 10.2519/jospt.2020.9150. doi: 10.2519/jospt.2020.9150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delphi: a versatile methodology for conducting qualitative research. Murry John W., Hammons James O. 1995The Review of Higher Education. 18(4):423–436. doi: 10.1353/rhe.1995.0008. doi: 10.1353/rhe.1995.0008. [DOI] [Google Scholar]
- Consensus measurement in Delphi studies: review and implications for future quality assurance. von der Gracht Heiko A. Oct;2012 Technological Forecasting and Social Change. 79(8):1525–1536. doi: 10.1016/j.techfore.2012.04.013. doi: 10.1016/j.techfore.2012.04.013. [DOI] [Google Scholar]
- Extraarticular fractures after periacetabular osteotomy. Espinosa Norman, Strassberg Joshua, Belzile Etienne L., Millis Michael B., Kim Young-Jo. Jul;2008 Clinical Orthopaedics & Related Research. 466(7):1645–1651. doi: 10.1007/s11999-008-0280-x. doi: 10.1007/s11999-008-0280-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pubic/ischial stress fractures after eccentric rotational acetabular osteotomy. Tsuboi Masaki, Fujita Kanji, Kawabe Kiyoharu, Hasegawa Yukiharu. Jan;2011 Journal of Orthopaedic Science. 16(1):38–43. doi: 10.1007/s00776-010-0010-6. doi: 10.1007/s00776-010-0010-6. [DOI] [PubMed] [Google Scholar]
- The incidence of stress fracture following peri-acetabular osteotomy: an under-reported complication. Malviya A., Dandachli W., Beech Z., Bankes M. J., Witt J. D. Jan;2015 The Bone & Joint Journal. 97-B(1):24–28. doi: 10.1302/0301-620x.97b1.34525. doi: 10.1302/0301-620x.97b1.34525. [DOI] [PubMed] [Google Scholar]
- Early weight-bearing after periacetabular osteotomy leads to a high incidence of postoperative pelvic fractures. Ito Hiroshi, Tanino Hiromasa, Sato Tatsuya, Nishida Yasuhiro, Matsuno Takeo. Jul 11;2014 BMC Musculoskeletal Disorders. 15(1):234. doi: 10.1186/1471-2474-15-234. doi: 10.1186/1471-2474-15-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biomechanical study of load transfer of the pubic ramus due to pelvic inclination after hip joint surgery using a three-dimensional finite element model. Kaku Nobuhiro, Tsumura Hiroshi, Taira Hirofumi, Sawatari Tomoyuki, Torisu Takehiko. May;2004 Journal of Orthopaedic Science. 9(3):264–269. doi: 10.1007/s00776-004-0772-9. doi: 10.1007/s00776-004-0772-9. [DOI] [PubMed] [Google Scholar]
- Hip instability: a review of hip dysplasia and other contributing factors. Kraeutler M.J., Garabekyan T., Pascual-Garrido C., Mei-Dan O. 2016Muscle Ligaments and Tendons Journal. 6(3):343–353. doi: 10.32098/mltj.03.2016.10. doi: 10.32098/mltj.03.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walking patterns and hip contact forces in patients with hip dysplasia. Skalshøi Ole, Iversen Christian Hauskov, Nielsen Dennis Brandborg, Jacobsen Julie, Mechlenburg Inger, Søballe Kjeld, Sørensen Henrik. Oct;2015 Gait & Posture. 42(4):529–533. doi: 10.1016/j.gaitpost.2015.08.008. doi: 10.1016/j.gaitpost.2015.08.008. [DOI] [PubMed] [Google Scholar]
- Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Fabricant Peter D., Bedi Asheesh, De La Torre Katrina, Kelly Bryan T. Jul;2012 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 28(7):965–971. doi: 10.1016/j.arthro.2011.11.028. doi: 10.1016/j.arthro.2011.11.028. [DOI] [PubMed] [Google Scholar]
- Rehabilitation exercise progression for the gluteus medius muscle with consideration for iliopsoas tendinitis: an in vivo electromyography study. Philippon Marc J., Decker Michael J., Giphart J. Erik, Torry Michael R., Wahoff Michael S., LaPrade Robert F. May 12;2011 The American Journal of Sports Medicine. 39(8):1777–1786. doi: 10.1177/0363546511406848. doi: 10.1177/0363546511406848. [DOI] [PubMed] [Google Scholar]
- Iliopsoas tendon related pain following minimally invasive periacetabular osteotomy. Thiagarajah S, Verhaegen J, Balijepalli P, Bingham J, Grammatopoulos G, Witt J. 2019Orthopaedic Proceedings. 101-B(6) [Google Scholar]
- Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Beckman Scott M., Buchanan Thomas S. Dec;1995 Archives of Physical Medicine and Rehabilitation. 76(12):1138–1143. doi: 10.1016/s0003-9993(95)80123-5. doi: 10.1016/s0003-9993(95)80123-5. [DOI] [PubMed] [Google Scholar]
- Hip abductor weakness in distance runners with iliotibial band syndrome. Fredericson Michael, Cookingham Curtis L., Chaudhari Ajit M., Dowdell Brian C., Oestreicher Nina, Sahrmann Shirley A. Jul;2000 Clinical Journal of Sport Medicine. 10(3):169–175. doi: 10.1097/00042752-200007000-00004. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- Hip muscle weakness and overuse injuries in recreational runners. Niemuth Paul E., Johnson Robert J., Myers Marcella J., Thieman Thomas J. Jan;2005 Clinical Journal of Sport Medicine. 15(1):14–21. doi: 10.1097/00042752-200501000-00004. doi: 10.1097/00042752-200501000-00004. [DOI] [PubMed] [Google Scholar]
- Core stability measures as risk factors for lower extremity injury in athletes. Leetun DARIN T., Ireland MARY LLOYD, Willson JOHN D., Ballantyne BRYON T., Davis IRENE MCCLAY. Jun;2004 Medicine & Science in Sports & Exercise. 36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- Hip strength in females with and without patellofemoral pain. Ireland Mary Lloyd, Willson John D., Ballantyne Bryon T., Davis Irene McClay. Nov;2003 Journal of Orthopaedic & Sports Physical Therapy. 33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- Core strength and lower extremity alignment during single leg squats. Willson JOHN D., Ireland MARY LLOYD, Davis IRENE. May;2006 Medicine & Science in Sports & Exercise. 38(5):945–952. doi: 10.1249/01.mss.0000218140.05074.fa. doi: 10.1249/01.mss.0000218140.05074.fa. [DOI] [PubMed] [Google Scholar]
- The effect of sex and age on isokinetic hip-abduction torques. Brent Jensen L., Myer Gregory D., Ford Kevin R., Paterno Mark V., Hewett Timothy E. Feb;2013 Journal of Sport Rehabilitation. 22(1):41–46. doi: 10.1123/jsr.22.1.41. doi: 10.1123/jsr.22.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running. Snyder Kelli R., Earl Jennifer E., O’Connor Kristian M., Ebersole Kyle T. Jan;2009 Clinical Biomechanics. 24(1):26–34. doi: 10.1016/j.clinbiomech.2008.09.009. doi: 10.1016/j.clinbiomech.2008.09.009. [DOI] [PubMed] [Google Scholar]
- Dynamic hip stability, strength and pain before and after hip abductor strengthening exercises for patients with dysplastic hips. Kuroda Daisuke, Maeyama Akira, Naito Masatoshi, Moriyama Shigeki, Yoshimura Ichiro, Nakamura Yoshinari, Kiyama Takahiko. May 20;2013 Isokinetics and Exercise Science. 21(2):95–100. doi: 10.3233/ies-130480. doi: 10.3233/ies-130480. [DOI] [Google Scholar]
- Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Zazulak Bohdanna T., Hewett Timothy E., Reeves N. Peter, Goldberg Barry, Cholewicki Jacek. Jul;2007 The American Journal of Sports Medicine. 35(7):1123–1130. doi: 10.1177/0363546507301585. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Paterno Mark V., Schmitt Laura C., Ford Kevin R., Rauh Mitchell J., Myer Gregory D., Huang Bin, Hewett Timothy E. Aug 11;2010 The American Journal of Sports Medicine. 38(10):1968–1978. doi: 10.1177/0363546510376053. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Novais Eduardo N., Kim Young-Jo, Carry Patrick M., Millis Michael B. Oct;2014 Clinical Orthopaedics & Related Research. 472(10):3142–3149. doi: 10.1007/s11999-014-3720-9. doi: 10.1007/s11999-014-3720-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preservation of the rectus femoris origin during periacetabular osteotomy does not compromise acetabular reorientation. Peters Christopher L., Erickson Jill A., Anderson Mike B., Anderson Lucas A. Feb;2015 Clinical Orthopaedics & Related Research. 473(2):608–614. doi: 10.1007/s11999-014-3837-x. doi: 10.1007/s11999-014-3837-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A systematic review of rehabilitation cxercises to progressively load the gluteus medius. Ebert Jay R., Edwards Peter K., Fick Daniel P., Janes Gregory C. Sep;2017 Journal of Sport Rehabilitation. 26(5):418–436. doi: 10.1123/jsr.2016-0088. doi: 10.1123/jsr.2016-0088. [DOI] [PubMed] [Google Scholar]
- Rehabilitation exercises for the gluteus medius muscle segments: an electromyography study. Moore Damien, Pizzari Tania, McClelland Jodie, Semciw Adam I. Nov 1;2019 Journal of Sport Rehabilitation. 28(8) doi: 10.1123/jsr.2018-0340. doi: 10.1123/jsr.2018-0340. [DOI] [PubMed] [Google Scholar]
- Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Hewett Timothy E., Myer Gregory D., Ford Kevin R., Heidt Robert S. Jr., Colosimo Angelo J., McLean Scott G., van den Bogert Antonie J., Paterno Mark V., Succop Paul. Apr;2005 The American Journal of Sports Medicine. 33(4):492–501. doi: 10.1177/0363546504269591. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Hewett T E, Zazulak B T, Myer G D, Ford K R. Jun 1;2005 British Journal of Sports Medicine. 39(6):347–350. doi: 10.1136/bjsm.2005.018572. doi: 10.1136/bjsm.2005.018572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valgus knee motion during landing in high school female and male basketball players. Ford KEVIN R., Myer GREGORY D., Hewett TIMOTHY E. Oct;2003 Medicine & Science in Sports & Exercise. 35(10):1745–1750. doi: 10.1249/01.mss.0000089346.85744.d9. doi: 10.1249/01.mss.0000089346.85744.d9. [DOI] [PubMed] [Google Scholar]
- A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Chappell Jonathan D., Yu Bing, Kirkendall Donald T., Garrett William E. Mar;2002 The American Journal of Sports Medicine. 30(2):261–267. doi: 10.1177/03635465020300021901. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Ford Kevin R., Myer Gregory D., Smith Rose L., Vianello Rebecca M., Seiwert Shelly L., Hewett Timothy E. Jan;2006 Clinical Biomechanics. 21(1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- A comparison of knee joint motion patterns between men and women in selected athletic tasks. Malinzak Robert A., Colby Scott M., Kirkendall Donald T., Yu Bing, Garrett William E. Jun;2001 Clinical Biomechanics. 16(5):438–445. doi: 10.1016/s0268-0033(01)00019-5. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- Decrease in neuromuscular control about the knee with maturation in female athletes. Hewett Timothy E., Myer Gregory D., Ford Kevin R. Aug;2004 The Journal of Bone and Joint Surgery-American Volume. 86(8):1601–1608. doi: 10.2106/00004623-200408000-00001. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- Gluteus medius muscle activation patterns as a predictor of low back pain during standing. Nelson-Wong Erika, Gregory Diane E., Winter David A., Callaghan Jack P. Jun;2008 Clinical Biomechanics. 23(5):545–553. doi: 10.1016/j.clinbiomech.2008.01.002. doi: 10.1016/j.clinbiomech.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. An EMG study. Lyons Kathryn, Perry Jacquelin, Gronley Joanne K., Barnes Lee, Antonelli Dan. Oct 1;1983 Physical Therapy. 63(10):1597–1605. doi: 10.1093/ptj/63.10.1597. doi: 10.1093/ptj/63.10.1597. [DOI] [PubMed] [Google Scholar]
- The role of core stability in athletic function. Kibler W Ben, Press Joel, Sciascia Aaron. 2006Sports Medicine. 36(3):189–198. doi: 10.2165/00007256-200636030-00001. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- Assessing lateral stability of the hip and pelvis. Grimaldi Alison. Feb;2011 Manual Therapy. 16(1):26–32. doi: 10.1016/j.math.2010.08.005. doi: 10.1016/j.math.2010.08.005. [DOI] [PubMed] [Google Scholar]
- An appraisal of the short lateral rotators of the hip joint. Yoo Sarang, Dedova Irina, Pather Nalini. May 30;2015 Clinical Anatomy. 28(6):800–812. doi: 10.1002/ca.22568. doi: 10.1002/ca.22568. [DOI] [PubMed] [Google Scholar]
- Individual muscle contributions to support in normal walking. Anderson Frank C., Pandy Marcus G. Apr;2003 Gait & Posture. 17(2):159–169. doi: 10.1016/s0966-6362(02)00073-5. doi: 10.1016/s0966-6362(02)00073-5. [DOI] [PubMed] [Google Scholar]
- Differential neuromuscular training effects onACL injury risk factors in"high-risk" versus "low-risk" athletes. Myer Gregory D, Ford Kevin R, Brent Jensen L, Hewett Timothy E. May 8;2007 BMC Musculoskeletal Disorders. 8(1):39. doi: 10.1186/1471-2474-8-39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effectiveness of neuromuscular training based on the neuromuscular risk profile. Hewett Timothy E., Ford Kevin R., Xu Yingying Y., Khoury Jane, Myer Gregory D. Apr 25;2017 The American Journal of Sports Medicine. 45(9):2142–2147. doi: 10.1177/0363546517700128. doi: 10.1177/0363546517700128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postural and respiratory activation of the trunk muscles changes with mode and speed of locomotion. Saunders Steven W., Rath David, Hodges Paul W. Dec;2004 Gait & Posture. 20(3):280–290. doi: 10.1016/j.gaitpost.2003.10.003. doi: 10.1016/j.gaitpost.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Changes in three dimensional lumbo-pelvic kinematics and trunk muscle activity with speed and mode of locomotion. Saunders Steven W., Schache Anthony, Rath David, Hodges Paul W. Oct;2005 Clinical Biomechanics. 20(8):784–793. doi: 10.1016/j.clinbiomech.2005.04.004. doi: 10.1016/j.clinbiomech.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Return to Play After Periacetabular Osteotomy for Treatment of Acetabular Dysplasia in Adolescent and Young Adult Athletes. Heyworth Benton E., Novais Eduardo N., Murray Kerri, Cvetanovich Gregory, Zurakowski David, Millis Michael B., Kim Young-jo. Mar 11;2016 The American Journal of Sports Medicine. 44(6):1573–1581. doi: 10.1177/0363546516632743. doi: 10.1177/0363546516632743. [DOI] [PubMed] [Google Scholar]
- Sports activity participation after curved periacetabular osteotomy for acetabular dysplasia. Takahashi Yoshiki, Takahira Naonobu, Uchiyama Katsufumi, Fukushima Kensuke, Moriya Mitsutoshi, Shibuya Manaka, Tsuda Kouji, Tozaki Kiyoshi, Kudo Sho, Kaneda Hiroaki, Sekita Junya, Takaso Masashi. Sep 28;2020 BMC Musculoskeletal Disorders. 21(1):637. doi: 10.1186/s12891-020-03625-3. doi: 10.1186/s12891-020-03625-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. Di Stasi Stephanie, Myer Gregory D., Hewett Timothy E. Nov;2013 Journal of Orthopaedic & Sports Physical Therapy. 43(11):777–792,A1. doi: 10.2519/jospt.2013.4693. doi: 10.2519/jospt.2013.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Hewett Timothy E., Di Stasi Stephanie L., Myer Gregory D. 2013The American Journal of Sports Medicine. 41(1):216–224. doi: 10.1177/0363546512459638. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Barber-Westin Sue D., Noyes Frank R. Sep;2011 The Physician and Sportsmedicine. 39(3):100–110. doi: 10.3810/psm.2011.09.1926. doi: 10.3810/psm.2011.09.1926. [DOI] [PubMed] [Google Scholar]
- Criterion-based rehabilitation program with return to sport testing following ACL reconstruction: a case series. Joreitz Rick, Lynch Andrew, Popchak Adam, Irrgang Jay. Dec;2020 International Journal of Sports Physical Therapy. 15(6):1151–1173. doi: 10.26603/ijspt20201151. doi: 10.26603/ijspt20201151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Mandelbaum Bert R., Silvers Holly J., Watanabe Diane S., Knarr John F., Thomas Stephen D., Griffin Letha Y., Kirkendall Donald T., Garrett William Jr. Jul;2005 The American Journal of Sports Medicine. 33(7):1003–1010. doi: 10.1177/0363546504272261. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- The 2012 ABJS Nicolas Andry Award: The sequence of prevention: a systematic approach to prevent anterior cruciate ligament injury. Hewett Timothy E., Myer Gregory D., Ford Kevin R., Paterno Mark V., Quatman Carmen E. Oct;2012 Clinical Orthopaedics & Related Research. 470(10):2930–2940. doi: 10.1007/s11999-012-2440-2. doi: 10.1007/s11999-012-2440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to sport after hip arthroscopy: aggregate recommendations from high-volume hip arthroscopy centers. Domb Benjamin G., Stake Christine E., Finch Nathan A., Cramer T. Luke. Oct;2014 Orthopedics. 37(10):e902–5. doi: 10.3928/01477447-20140924-57. doi: 10.3928/01477447-20140924-57. [DOI] [PubMed] [Google Scholar]
- The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Ardern Clare L, Österberg Annika, Tagesson Sofi, Gauffin Håkan, Webster Kate E, Kvist Joanna. Oct 7;2014 British Journal of Sports Medicine. 48(22):1613–1619. doi: 10.1136/bjsports-2014-093842. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Ardern Clare L., Taylor Nicholas F., Feller Julian A., Whitehead Timothy S., Webster Kate E. Jun 3;2013 The American Journal of Sports Medicine. 41(7):1549–1558. doi: 10.1177/0363546513489284. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- A systematic review of the psychological factors associated with returning to sport following injury. Ardern Clare L, Taylor Nicholas F, Feller Julian A, Webster Kate E. 2013British Journal of Sports Medicine. 47(17):1120–1126. doi: 10.1136/bjsports-2012-091203. doi: 10.1136/bjsports-2012-091203. [DOI] [PubMed] [Google Scholar]
- Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Baez Shelby E., Hoch Matthew C., Hoch Johanna M. 2020Knee Surgery, Sports Traumatology, Arthroscopy. 28(2):495–501. doi: 10.1007/s00167-019-05696-9. doi: 10.1007/s00167-019-05696-9. [DOI] [PubMed] [Google Scholar]
- A comparison of 6-month outcomes between periacetabular osteotomy with concomitant hip arthroscopy to isolated hip arthroscopy for femoroacetabular impingement. Ellis Thomas, Kohlrieser Dave, Rao Brian, Enseki Keelan, Popchak Adam, Martin RobRoy L. 2022Archives of Orthopaedic and Trauma Surgery. 142(3):471–480. doi: 10.1007/s00402-021-03886-0. doi: 10.1007/s00402-021-03886-0. [DOI] [PubMed] [Google Scholar]