Context:
The COVID-19 pandemic has impacted health systems worldwide. Studies to date have largely focused on the health care system with less attention to the impact on public health systems and practice.
Objective:
To describe the early impacts of COVID-19 on public health systems and practice in 3 Canadian provinces from the perspective of public health system leaders and synthesize lessons learned.
Design:
A qualitative study using semistructured virtual interviews with public health leaders between October 2020 and April 2021. The World Health Organization's essential public health operations framework guided data collection and analysis.
Setting:
This study involved the Canadian provinces of Alberta, Ontario, and Québec. These provinces were chosen for their large populations, relatively high COVID-19 burden, and variation in public health systems.
Participants:
Public health leaders from Alberta (n = 21), Ontario (n = 18), and Québec (n = 19) in organizations with a primary mandate of stewardship and/or administration of essential public health operations (total n = 58).
Results:
We found that the COVID-19 pandemic led to intensified collaboration in public health systems and a change in workforce capacity to respond to the pandemic. This came with opportunities but also challenges of burnout and disruption of non-COVID-19 services. Information systems and digital technologies were increasingly used and there was greater proximity between public health leaders and other health system leaders. A renewed recognition for public health work was also highlighted.
Conclusions:
The COVID-19 pandemic impacted several aspects of public health systems in the provinces studied. Our findings can help public health leaders and policy makers identify areas for further investment (eg, intersectoral collaboration, information systems) and develop plans to address challenges (eg, disrupted services, workforce burnout) that have surfaced.
Keywords: COVID-19, intersectoral collaboration, public health practice, public health systems research, workforce
The 2021 report from Canada's Chief Public Health Officer (CPHO), the federal government's lead public health (PH) professional, acknowledges the COVID-19 pandemic as the most significant PH crisis that the country has faced in a century.1 The pandemic has had major impacts on health systems worldwide2,3 revealing challenges with structure and service delivery. Much research has focused on the impacts of COVID-19 on health care systems (ie, care for individuals and patients)4–6 while less attention has been paid specifically to the impact of the pandemic on PH systems.
Public health systems, embedded within health systems,1,7 focus on protecting and improving population health through surveillance and the delivery of population-level programs and services.8 The World Health Organization's “essential PH operations” (EPHOs) framework conceptualizes how structural factors such as governance, workforce, and organization enable key PH functions of health surveillance, protection, and promotion.9 The impacts of the COVID-19 pandemic on PH systems are still emerging in the literature. Preliminary findings from the United States10 and United Kingdom11 point to challenges of PH workforce shortages and historical underinvestment, as well as the need to focus on intersectoral collaboration. The pandemic has also increased the public profile of PH systems and created the potential for system improvement.10,11
Empirical findings on the impact of COVID-19 on PH systems and practice in Canada were missing during the earlier phases of the pandemic. Our objective was to examine the early impacts of the COVID-19 pandemic on PH systems and practice in 3 Canadian provinces (Alberta, Ontario, and Québec) from the perspective of PH system leaders. Our study builds on earlier discussions in the literature12,13 and complements the 2021 CPHO report, which presented strategic opportunities for the transformation of PH systems in response to current challenges.1 Our findings, ongoing research,14 the CPHO report,1 and other public inquiries15,16 come during a window of opportunity17 where we can synthesize lessons learned and inform future PH policy and practice.
Methods
Study design
We conducted a descriptive multiple case study of the COVID-19 response in 3 Canadian provinces (Alberta, Ontario, and Québec). We analyzed descriptive reports of provincial PH systems (forthcoming)18,19 to design a qualitative study to better understand the impacts of recent PH reforms, capacity to respond to COVID-19, and impacts of COVID-19 on PH systems. Because of the richness and breadth of the data collected, this article focuses on a subset of the study while findings related to PH system reforms20 and COVID-19 response21 are forthcoming elsewhere.
Conceptual framework
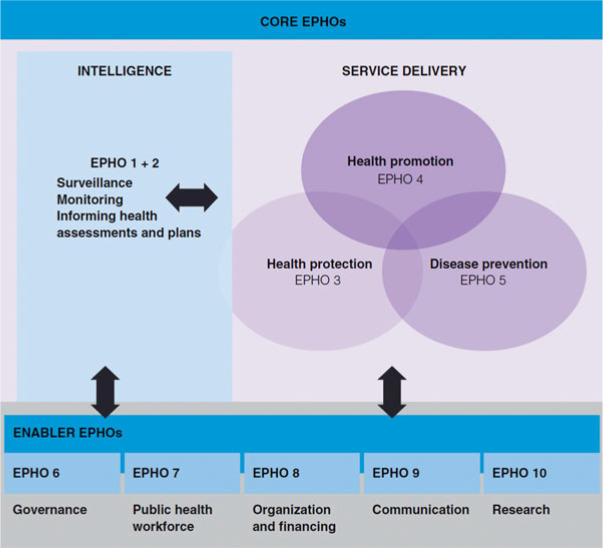
We used the EPHOs framework to narrow our focus and promote the international comparability of our findings (Figure 1).9,22–24 A PH system was defined as the collection of entities that utilize PH structures (enabler EPHOs) to deliver services (core EPHOs). We refer readers to Rechel et al9 for a further discussion of this conceptualization.
FIGURE 1.
A Conceptual Framework for the 10 EPHOsa
Abbreviation: EPHO, Essential Public Health Operations.
aReprinted with permission from the WHO Regional Office for Europe, Bernd Rechel, Elke Jakubowksi, Martin McKee, Ellen Nolte, Organization and financing of public health services in Europe, Page No. 11, Copyright (2018).9 This figure is available in color online (www.JPHMP.com).
Positionality and reflexivity
Constructivist and pragmatic worldviews guided our study design and conduct. The perspectives sought from the key informants (KIs) were seen to reflect individual subjective meanings created through their experiences, actions, and interactions.25,26 The research team consisted of graduate students (H.S.S., T.J.), researchers (R.W.S., S.A., M.O., E.D.R., R.S., L.C.R., A.P.), and practitioners (A.P.) at different career stages. The team met periodically to have reflexive discussions to understand how positionalities may have impacted the study and identify shared goals of advancing knowledge and drawing attention to findings that have the potential to strengthen PH systems.
Setting
Canada's PH system is a “system of systems”1(p46) in that PH mandates are spread across jurisdictional levels and are embedded in the country's federated health system. Provincial governments play a key role in coordinating regional/local PH units and supporting overall planning and administration.1 Each province has a PH lead who holds an advisory and public communications role in government (eg, a “Chief Medical Officer of Health” or CMOH).27 Local and regional PH leaders (eg, “Medical Officers of Health” or MOHs) oversee the implementation of PH programs and services, and health surveillance for their jurisdictions. The provinces of Alberta, Ontario, and Québec were chosen as case studies due to their variation in PH systems, large populations, and high burden of COVID-19.28,29 In terms of PH organization, Alberta is relatively more centralized with 5 regional PH units operating within a hierarchical province-wide authority (Alberta Health Services), Québec's PH system is organized into 18 PH regions that are integrated with health care and social services, and finally, Ontario is relatively decentralized with 34 PH units with comparatively little integration with health care or social services.21
Key informants
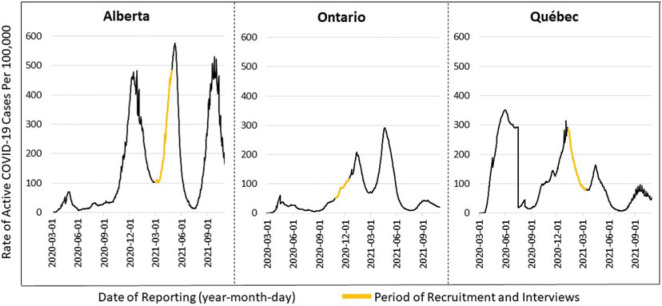
Interviews were conducted with KIs from Alberta, Ontario, and Québec from October 2020 to April 2021. Our recruitment involved a combination of purposive (maximum variation across jurisdictional levels within a province and across PH disciplines) and snowball sampling.30 Key informants held a variety of leadership positions in organizations with a mandate of stewardship and/or administration of the core EPHOs (Table 1). Key informants working within indigenous organizations (ie, First Nations or Inuit-led) that shared geographic boundaries with 1 of the 3 provinces were also included. Public health leaders with a national mandate and focus were not included. We invited 44 KIs from Alberta, 42 from Ontario, and 34 from Québec to participate. After accounting for nonresponse, declines, and scheduling conflicts, 21 interviews from Alberta (47.7% completion rate), 18 from Ontario (42.9%), and 19 from Québec (55.9%) were completed (total n = 58). The variation in completion rates may be explained by the burden of COVID-19 experienced by the provinces during recruitment and interviews (Figure 2).
TABLE 1. Key Informant Characteristics From 3 Canadian Provinces.
| Characteristic | Total n (%) |
|---|---|
| Role in the PH system | |
| Senior leadership (eg, deputy minister, chief medical officer of health, chief executive officer, senior provincial director) | 16 (28) |
| Medical officer of health (federal/provincial/regional/local) | 17 (29) |
| Other (eg, director, program manager/lead, medical specialist, consultant) | 25 (43) |
| Geography (catchment area) | |
| Urban | 40 (69) |
| Rural/northern | 18 (31) |
| Workplace | |
| PH department or authority (local/regional/provincial) | 39 (67) |
| Government (local/provincial) | 10 (17) |
| Other (eg, arms-length public health scientific institute, federal government agency, professional association, nongovernmental organization) | 9 (16) |
| Discipline (registered profession or area of work) | |
| Medical or nursing | 31 (53) |
| Other (eg, policy, management, dental, nutrition, health promotion, epidemiology, environmental and occupational health) | 27 (47) |
Abbreviation: PH, public health.
FIGURE 2.
Recruitment and Interview Time Frames and the Rate of Active COVID-19 Cases per 100 000 Population From March 2020 to October 202128 This figure is available in color online (www.JPHMP.com).
Data collection
Key informants were invited through email to participate in semistructured interviews conducted virtually by H.S.S., R.W.S., T.J., M.M.S., or M.S. An interview guide was developed on the basis of the EPHO framework and other literature9,22–24,31 before being internally pilot-tested. Key informants were prompted about the current state of PH systems, reforms, and COVID-19 response and impact. The interview questions relevant to this article are shown in Table 2 (the full interview guide is available upon request). The interviews lasted about 60 minutes and were audio-recorded and transcribed verbatim. Interviews conducted in French (for Québec) were translated to English by a professional transcriptionist and then reviewed for accuracy by M.M.S. or M.S. We estimated that conducting 15 to 20 interviews for each province would achieve data saturation.
TABLE 2. Interview Questions Used for This Study.
| No. | Question |
|---|---|
| 1 | How did the COVID-19 pandemic impact your organization and your role? |
| 2 | Can you provide any examples of how the COVID-19 pandemic caused changes to the function and structure of your organization and/or the public health system? |
| 3 | Were any of these changes invisible or only observable internally? |
| 4 | Do you think any of these changes should be preserved during and after the pandemic recovery phase? |
| 5 | Were any of these changes inspired or influenced by other jurisdictions and their pandemic responses? |
Data analysis
Directed content analysis32 was employed whereby a coding guide (available upon request) was developed before coding based on the conceptual framework and interview guide. Transcript coding was completed using NVivo (QSR International, Version 12). Three authors (H.S.S., R.W.S., and T.J.) with training in qualitative methods independently test-coded the same 2 transcripts for each province and met to discuss intercoder agreement and the appropriateness of the coding guide. Additional rounds of triple coding were completed until each coder felt that agreement was strong enough to proceed with independent coding of the remaining transcripts. One study team member (K.L.) also supported the coding of a few transcripts following the process described previously.
Thematic analysis was used to identify and characterize patterns of meaning in the codes.33 H.S.S. reviewed relevant codes and memos to develop preliminary themes reflecting salient perspectives for each province. The codes and preliminary themes were then independently assessed by M.O., R.W.S., and T.J., leading to revision, and then presented to S.A. and A.P. for review. This process ensured triangulation from multiple perspectives. Principles of credibility, dependability, confirmability, and transferability were also applied to improve the trustworthiness of our analysis.34 An audit trail was maintained via journaling to record observations, ideas, decisions, and reflexive notes. Finally, synthesized member checking35 was conducted to increase the accuracy of the themes and ensure that they resonated with KI experiences. Key informants from Alberta (n = 2), Ontario (n = 7), and Québec (n = 1) provided input at this stage to further inform our findings.
Research ethics considerations
This study was approved by the University of Toronto Research Ethics Board (REB-39438). Participation was confidential, voluntary, and informed written (or verbal) consent was obtained. We used the consolidated criteria for reporting qualitative research checklist and the Standards for Reporting Qualitative Research for the reporting of this study.36,37
Results
Our analysis yielded 5 crosscutting and salient themes that captured the main impacts of the pandemic on PH systems: (1) intensified collaborations; (2) changes in PH workforce capacity; (3) increased use of information and digital technologies; (4) greater proximity between PH leaders and health system decision makers; and (5) increased appreciation for PH work. We discuss each theme later with quotes that identify the province of the KI (ie, Alberta = AB, Ontario = ON, Québec = QC).
Intensified collaboration within and beyond the health system
The COVID-19 pandemic created a need for intensified collaborations and partnerships across all 3 provinces studied. Existing partnerships were strengthened, and new ones formed out of necessity. There was increased collaboration between health sector actors “such as primary care, acute care, [PH], all the players in the health system” (ON-08), and beyond. One KI noted how they now “had health promoters working with the long-term care sector, with shelters, and social services, congregate living groups, schools and daycares” (ON-17). Other sectors where there was an increase in collaboration included municipal governments, police services, hospitality, businesses, community-based organizations, indigenous governments, and federal-level health actors.
The mechanisms enabling collaborative partnerships varied. In some cases, multisectoral (or “liaison”) tables or working groups were set up to coordinate the COVID-19 response. In other cases, memoranda of understanding or other agreements between parties were established: “we've got CBOs [community-based organizations] who are immunizing their patient population or their client population under the delegation of a Medical Officer of Health and it's a formal arrangement” (AB-19).
Key informants reported being hopeful that these strengthened collaborations between health system and PH actors would continue even after the pandemic, as these new partnerships were seen to be vital for improving future PH work. Though, KIs also noted that expanded networks of actors involved in collaborative PH work also came with some instances of unclear roles and responsibilities (eg, between PH and health care actors in Ontario in terms of COVID-19 response and decision making), tensions around who is leading the pandemic response, and duplication of efforts.
Changes in PH workforce capacity
Significant redeployment and hiring of new staff took place to respond to COVID-19. Although redeployment was seen as necessary, there was concern about its impact on other EPHOs: “we have reallocated 80 percent of our team to work on COVID. And there are a lot of other important things we need to be doing” (ON-01). Key informants provided many examples of PH activities that had been disrupted because of redeployment (eg, routine immunizations, health promotion, oral health, community and stakeholder engagement, and long-term policy/planning). Some impacts were immediate: “You see a syphilis outbreak [...] because they're not able to do enough sexual health work” (ON-18). The long-term impacts of redeployment on other PH work were also a concern.
The provision of emergency funding into PH systems facilitated hiring to respond to the pandemic. For instance, “there has been hiring never before seen [...] If this hiring becomes permanent the potential for reinforcing [PH] action is real” (QC-05). Most KIs welcomed the new funding and opportunity to bolster the PH system, even if it came with challenges of hiring and training amidst an emergency. But there was no long-term guarantee of funding as one KI noted:
My concern is that, outside the pandemic period, [PH] will no longer be a priority, and that budgets will be given as a priority, to the hospitals [...] it is true when there is a national threat, [PH] will find the resources it requires, but when the pandemic ends, it is not certain that the current structure will serve [PH] appropriately (QC-03).
Finally, there were serious concerns related to workforce burnout: “our [redeployed] staff have had some really great meaningful work to support the pandemic. But they're tired and weary, and really looking forward to [coming] back to their regular jobs” (AB-11) and “we are burning out our workforce, really burning them out” (QC-10).
Increased use of information systems and digital technologies
Key informants from Alberta and Ontario discussed investments and changes in information systems and digital technologies. One KI noted how COVID-19 facilitated the adoption of new electronic systems:
The [...] resistance to that simple technological change that I faced pre-COVID was staggering compared to the fact that now we've been forced to do some of these things like online booking for testing and things like that, and people are seeing the value (ON-18).
For some services, the transition to online delivery helped improve accessibility for populations who otherwise may not have been able to attend in-person events. The use of text/phone-based services during the pandemic was also advanced (eg, for the notification of COVID-19 test results, prenatal health promotion). However, a switch to online delivery also came with a decrease in the quality of some services (eg, dental consultations). The transition to virtual service delivery was complemented by new flexibility in how and where PH professionals worked.
Information systems also received considerable investment and have the potential to improve surveillance and monitoring activities in the long-term:
there was money put forward for [...] Online booking systems, and dashboards that we didn't have access to the past [...] I think that that is a [...] good thing that this has brought forward, is the importance of surveillance and better access to detail [...] You know who's got vaccines, who doesn't, you know disparities, and who's getting the vaccine, or populations that aren't picking it up [...] it's all there at your fingertips (AB-16).
Greater proximity between PH leaders and health system leaders
The pandemic increased the proximity between MOHs to more senior health system leaders (eg, health agency chief executive officers or “CEOs”) leading to more opportunities for PH leaders to expand their authority and influence decision making across the health sector. In Québec, changes in working relationships and communication between MOHs and integrated health and social services centre executive leaders enabled them to work more closely. This led to expedited approvals for supporting COVID-19 activities and the potential to support future recovery work:
the proximity we have to power, that's clearly a transformative leverage that we didn't have before [...] If we were able to maintain that, at least for the first part of the recovery, that would be extraordinary [...] discussions are happening about what the involvement will be for me [as an MOH] with the [...] senior administration team, for the coming months. (QC-08)
This shift in linkages and communication between local and provincial PH leaders in Québec also facilitated COVID-19 vaccination strategies in one instance. A KI from Alberta noted a similar trend of greater proximity to health system decision making and the advancement of PH:
[O]ur senior MOH [...] has really now been better positioned through the pandemic with our executive leadership team and worked closely with the CEO. And so that's where we should have some continued, I think, development of our [PH] portfolios within AHS [Alberta Health Services], and more opportunity to work closely with our overall health system leadership to move forward (AB-14).
However, a closer proximity between PH leaders and provincial decision makers (eg, elected officials) also evoked concerns about the “scientific neutrality” (QC-10) of PH agencies (eg, Institut national de santé publique du Québec) as well as the overall autonomy of PH experts when considering decision makers' influence on PH decisions.
Increased appreciation for PH work
Key informants perceived that the COVID-19 pandemic may have increased an appreciation for PH work by the health system and the broader public:
[COVID-19 has] put an attention and an emphasis back on [PH] that we haven't seen here in a long time [...] people sort of like appreciated [PH] and like, ‘Oh, yeah, that's where I get my immunizations. They do the baby visits when people come home from the hospital.’ But I don't think [the public] truly understood the value of [PH] and the importance of [PH] until we're facing this huge challenge (AB-01).
Key informants thought that the pandemic had raised the profile of the health protection and emergency response while also creating possibilities to have discussions about other PH functions:
[PH] was really struggling in terms of public recognition and appreciation. And now [the public has] a better understanding of [...] what its mandates are in terms of health crisis and protection, and I hope that [...] this will contribute to opening more doors for us with new partners with whom we previously had little exchange to say [...] “we can also work in the scope of prevention, before crises occur,” and then introduce notions [...] such as chronic illness, climate change, so how to anticipate future problems (QC-16).
Discussion
The COVID-19 pandemic necessitated several changes to PH systems and created new challenges and opportunities for rebuilding and renewing PH systems post-COVID-19. From the perspective of PH leaders in 3 Canadian provinces, key adaptations included intensified collaboration between PH and other health sector actors, and non–health sector partners, workforce disruption and burnout, accelerated use of digital technologies, increased influence on (and by) health system leadership, and heightened appreciation for PH work.
Collaborative partnerships within and beyond the health sector are integral to PH work and improving and protecting the health of a community.38,39 The 2003 severe acute respiratory syndrome (SARS) outbreak led to discussions and an emphasis on the role of collaboration between various governments and sectors for PH work in Canada.40 During the 2009 H1N1 pandemic, collaboration between different levels of government and stakeholders was seen as a strength of the emergency response but areas for improvement included the clarification of roles, responsibilities, and collaborative mechanisms.41 These previous insights remain relevant during COVID-19. Public health actors are motivated to maintain newly formed and strengthened partnerships; however, more consideration needs to be given to clarifying roles and responsibilities, strengthening accountability to communities and the public, and supporting effective mechanisms enabling collaboration in nonemergency times as well as during crises such as COVID-19.
Redeployment and hiring of new PH human resources to respond to COVID-19 were expected. Although this shift facilitated response in the short term, other challenges emerged. Planning for surge capacity was lacking although this was highlighted after SARS and H1N1.40,41 The diversion of PH human resources toward COVID-19 and away from other functions came at a cost, which was also seen during SARS albeit at a smaller scale.40 An analysis in Ontario reported that in 2021, an average of 78% of PH unit resources were diverted to COVID-19.42 This adversely impacted a variety of services including chronic disease prevention and children's health programs.42 Disruptions to routine immunizations across Canada have been captured by Sell et al43 and a global World Health Organization assessment44 also showed a trend away from noncommunicable disease activities during the pandemic. Given these disruptions, long-term “shadow pandemics” of mental health45,46 and chronic disease47 have been hypothesized. The culmination of inadequate surge capacity, workforce burnout, and service disruption renders PH human resources and non–COVID-19 services precarious and must therefore be a focus of COVID-19 recovery and plans for PH system reforms.
According to Budd et al,48 EPHOs are likely to become increasingly digital due to advancements in information systems and technologies during COVID-19. Surveillance, data visualization, smartphone-based applications, and telehealth are some ways digital technologies were used during the COVID-19 response.48 Questions around the effectiveness and equitability of these technological changes remain. Public health systems in Canada will have to plan for how digital technologies will be utilized following the pandemic and applied to various EPHOs as part of a broader data system strategy.49 Building new technological infrastructure, integrating it with existing systems, and prioritizing data security are critical areas to ensuring the successful continuation of digital technologies for PH.48
The increase in PH leaders' proximity and interactions with health system leaders has placed MOHs in unique positions of power and influence in Québec and Alberta. Public health leaders could use this change to facilitate flow of information,50 help set agendas,50 and use softer power51 to influence health system leaders in the short term. At the same time, these newfound positions may bring tensions related to maintaining autonomy and having influence on decision makers while being constrained and influenced by decision makers.16,21 Maintaining PH leaders' access to decision makers, while preserving their independence and autonomy, is the balance that needs to be struck to improve future emergency preparedness, restore public trust in scientific institutions and PH expertise, and orient the health system toward enhancing wellness and reducing health inequities.1
Recognition of the role of PH by the public and health system actors may provide an opportunity for PH systems to advocate for further investments. Although the KIs perceived the potential benefits of a renewed appreciation in PH, other developments point to some hostility toward PH leaders and the COVID-19 response as captured in a US analysis.52 Ultimately, the COVID-19 pandemic has sparked much interest and debate about PH. The 2021 CPHO report capitalizes on this interest to analyze the ongoing response to COVID-19 in Canada and echoes many of our findings that emerged in various ways across Canada.1 As other inquiries into pandemic response and impact emerge, there remains a need to continue triangulating and critically reflecting before definitive lessons29 can be drawn for future policy and practice.
Limitations
Our flexible qualitative approach53 meant that we iteratively updated our data collection and analytical methods as the study progressed. Our findings are limited to the earlier period of the pandemic when provincial governments had relaxed and then reintroduced a wide range of PH measures and at a time when vaccines were not yet available (Ontario), were just beginning to roll out to priority groups (Québec), or were about to be rolled out to the broader public (Alberta). Our focus on this relatively early stage in the pandemic helps reduce recall bias and allows us to learn about the challenges and experiences at a time when the PH system was in an acute emergency response phase of the pandemic and adapting to a rapidly evolving evidence base. However, the emphasis many KIs placed on the positive potential opportunities may reflect an interest in advocating for changes they hope to preserve. In light of these limitations, generalizing beyond the study period, KI sample, and 3 provinces is cautioned and we recognize that our findings may not reflect changes seen in Indigenous-led PH organizations that may face mandate ambiguity with provincial and federal PH actors.21 Finally, we did not collect sociodemographic information. Diverse representation of identities and experiences was an implicit goal; however, a more systematic capturing of these data could have helped ensure this goal and deepen the relevance and trustworthiness of our findings.
Implications for Policy & Practice
COVID-19 has established a context in which PH is being given more attention, PH leaders are working more closely with health system leaders, and intersectoral partnerships have expanded. There is an opportunity for PH leaders and advocates to ensure that PH actors have continued access to health system leaders with a balance of independence and that increased investments in human resources and information systems are sustained for the betterment of future emergency preparedness and other EPHOs.
The redeployment of PH human resources to the COVID-19 response disrupted other PH services, and workforce burnout has emerged as a challenge. It may be time for PH systems to conduct a systematic assessment of services that have been disrupted, plan to “catch up” on any lost time, and invest in further supporting the workforce.
This study has captured some of the early impacts of COVID-19 on 3 PH systems in Canada from the perspectives of PH leaders; however, a more in-depth and critical cross-national assessment that incorporates broader perspectives is needed to fully understand the ongoing impacts of the pandemic, shortcomings in the response, and lessons for PH system renewal. National and subnational governments in Canada may be well placed to initiate these assessments.
Conclusion
The pandemic continues to impact Canadians and PH systems. Our study highlights some of the early impacts on PH systems in Alberta, Ontario, and Québec. Although many of these changes were seen as beneficial, such as increased collaborations across actors and sectors and investments in workforce and information technologies, challenges also emerged in workforce burnout and disruptions to non–COVID-19 PH programs and services. Uncertainty exists as to whether these changes will be maintained in the long term, and emerging literature may shed more light on how PH systems continue to evolve and adapt.
Footnotes
The authors acknowledge their advisory working group comprising Canadian health systems and public health researchers, physicians, and practitioners who provided feedback and guidance on their study design: Dr Mehdi Ammi, Dr Olivier Bellefleur, Dr Susan Chatwood, Dr Jasmine Pawa, and Dr Amélie Quesnel-Vallée. The authors also thank Muriel Mac-Seing (M.M.S.) and Melanie Seabrook (M.S.) for assistance with the French interviews and translation, and Kathy Luu (K.L.) for assistance with coding.
This research was supported by a Catalyst Grant from the Canadian Institutes of Health Research (grant no. 170320).
The authors declare no conflicts of interest.
Contributor Information
Harman S. Sandhu, Email: hsandhu.ph@gmail.com.
Robert W. Smith, Email: robw.smith@mail.utoronto.ca.
Tamika Jarvis, Email: jarvistl@mcmaster.ca.
Meghan O'Neill, Email: meghan.oneill@utoronto.ca.
Erica Di Ruggiero, Email: e.diruggiero@utoronto.ca.
Robert Schwartz, Email: robert.schwartz@utoronto.ca.
Laura C. Rosella, Email: laura.rosella@utoronto.ca.
Sara Allin, Email: sara.allin@utoronto.ca.
Andrew D. Pinto, Email: andrew.pinto@utoronto.ca.
References
- 1.Chief Public Health Officer of Canada. A vision to transform Canada's public health system: chief public health officer's report on the state of public health in Canada 2021. https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/state-public-health-canada-2021.html. Published 2021. Accessed August 17, 2022.
- 2.OECD. Strengthening the frontline: how primary health care helps health systems adapt during the COVID-19 pandemic. https://read.oecd-ilibrary.org/view/?ref=1060_1060243-snyxeld1ii&title=Strengthening-the-frontline-How-primary-health-care-helps-health-systems-adapt-during-the-COVID-19-pandemic. Published 2021. Accessed August 17, 2022.
- 3.OECD. Adaptive Health Financing: Budgetary and Health System Responses to Combat COVID-19. OECD J Budg. 2021;21(1). doi: 10.1787/69b897fb-en [Google Scholar]
- 4.Lurie N, Fremont A. Building bridges between medical care and public health. JAMA. 2009;302(1):84–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information. Overview: impacts of COVID-19 on health care workers. https://www.cihi.ca/en/health-workforce-in-canada-highlights-of-the-impact-of-covid-19/overview-impacts-of-covid-19-on. Published 2021. Accessed February 6, 2022.
- 6.Mihailescu M, Sim J, Bourgeault I. Afterword: COVID-19 and the Canadian Health Workforce. https://www.hhr-rhs.ca/en/text.html. Published 2021. Accessed August 17, 2022.
- 7.Jarvis T, Scott F, El-Jardali F, Alvarez E. Defining and classifying public health systems: a critical interpretive synthesis. Heal Res Policy Syst. 2020;18(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercer N. How public health differs from acute care. Wellington-Dufferin-Guelph Public Health. https://wdgpublichealth.ca/blog/how-public-health-differs-acute-care. Published 2017. Accessed August 17, 2022.
- 9.Rechel B, Jakubowski E, McKee M, Nolte E. Conceptual framework. In: Organization and Financing of Public Health Services in Europe. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2018. https://www.ncbi.nlm.nih.gov/books/NBK535721/. Accessed February 6, 2022. [PubMed] [Google Scholar]
- 10.DeSalvo K, Hughes B, Bassett M, et al. Public health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. 2021;2021:10.31478/202104c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross S, Fenney D, Thorstensen-Woll C, Buck D. Directors of public health and the Covid-19 pandemic: “a year like no other.” https://www.kingsfund.org.uk/publications/directors-public-health-covid-19-pandemic. Published 2021. Accessed August 17, 2022.
- 12.Boin A, Brock K, Craft J, et al. Beyond COVID-19: five commentaries on expert knowledge, executive action, and accountability in governance and public administration. Can Public Adm. 2020;63(3):339–368. [Google Scholar]
- 13.Béland F. Pandemics, inequities, public health, information, response: Canada's failure? Can J Public Heal. 2021;112(3):349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plante C, Bandara T, Baugh Littlejohns L, Sandhu N, Pham A, Neudorf C. Surveying the local public health response to COVID-19 in Canada: study protocol. PLoS One. 2021;16(11):e0259590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office of the Auditor General of Ontario. COVID-19 Preparedness and Management Chapter 2 Special Report on Outbreak Planning and Decision-Making. Toronto, ON; 2020. https://www.auditor.on.ca/en/content/specialreports/specialreports/COVID-19_ch2outbreakplanning_en20.pdf. Accessed August 17, 2022. [Google Scholar]
- 16.Champagne C, Denis J-L, Allin S, Smith R. The Organization of Public Health in Quebec, Nova Scotia, Ontario, Alberta and British Columbia. https://www.csbe.gouv.qc.ca/publications/publication.html?tx_csbepublication_liste%5Bpublication%5D=160&tx_csbepublication_liste%5Baction%5D=fiche&cHash=71a03565f932e53c55feccd0c091e27d. Published 2022. Accessed August 17, 2022.
- 17.Auener S, Kroon D, Wackers E, van Dulmen S, Jeurissen P. Covid-19: a window of opportunity for positive healthcare reforms. Int J Heal Policy Manag. 2020;9(10):419–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith RW, Allin S, Rosella L, et al. Profiles of public health systems in Canada: jurisdictional review methodology. https://ccnpps-ncchpp.ca/profiles-of-public-health-systems-in-canadian-provinces-and-territories/. Published 2021. Accessed August 17, 2022.
- 19.Smith RW, Allin S, Rosella L, et al. Profiles of public health systems in Canada: Ontario. https://ccnpps-ncchpp.ca/profiles-of-public-health-systems-in-canadian-provinces-and-territories/. Published 2021. Accessed August 17, 2022.
- 20.Jarvis T, Smith RW, Sandhu HS, Allin S, Pinto AD. Examining reforms that centralized public health practice: a qualitative multi-case study involving Alberta, Québec and Ontario. [submitted for publication]. 2022.
- 21.Smith RW, Jarvis T, Sandhu HS, et al. Centralization and integration of public health systems: Perspectives of public health leaders on factors facilitating and impeding COVID-19 responses in three Canadian provinces. [submitted for publication]. 2022. [DOI] [PMC free article] [PubMed]
- 22.World Health Organization. Self-Assessment Tool for the Evaluation of Essential Public Health Operations in the WHO European Region. Copenhagen, Denmark: World Health Organization; 2015. https://www.euro.who.int/__data/assets/pdf_file/0018/281700/Self-assessment-tool-evaluation-essential-public-health-operations.pdf?ua=1. Accessed August 17, 2022. [Google Scholar]
- 23.Rechel B, Maresso A, Sagan A, et al. Organization and Financing of Public Health Services in Europe: Country Reports. Copenhagen, Denmark: WHO Regional Office Europe on behalf of the European Observatory on Health Systems and Policies; 2018. https://www.ncbi.nlm.nih.gov/books/NBK507325/pdf/Bookshelf_NBK507325.pdf. Accessed August 17, 2022. [PubMed] [Google Scholar]
- 24.World Health Organization Regional Office For Europe. The 10 essential public health operations. https://www.euro.who.int/en/health-topics/Health-systems/public-health-services/policy/the-10-essential-public-health-operations. Accessed February 6, 2022.
- 25.Creswell JW. Qualitative Methods. In: Research Design: Qualitative, Quantitative and Mixed Methods Approaches. 4th ed. Thousand Oaks, CA: SAGE Publications Inc; 2014:183–213. [Google Scholar]
- 26.Kelly LM, Cordeiro M. Three principles of pragmatism for research on organizational processes. Methodol Innov. 2020;13(2):2059799120937242. [Google Scholar]
- 27.Fafard P, McNena B, Suszek A, Hoffman SJ. Contested roles of Canada's Chief Medical Officers of Health. Can J Public Heal. 2018;109(4):585–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Government of Canada. Interactive data visualizations of COVID-19. https://health-infobase.canada.ca/covid-19/?stat=rate&measure=active#a2. Published 2021. Accessed February 6, 2022.
- 29.Alami H, Lehoux P, Fleet R, et al. How can health systems better prepare for the next pandemic? Lessons learned from the management of COVID-19 in Quebec (Canada). Front public Heal. 2021;9:671833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Heal Ment Heal Serv Res. 2015;42(5):533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rechel B, Jakubowski E, McKee M, Nolte E. Organization and financing of public health services in Europe. European Observatory on Health Systems and Policies. https://www.ncbi.nlm.nih.gov/books/NBK535724/. Published 2018. Accessed February 6, 2022. [PubMed]
- 32.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 33.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 34.Houghton C, Casey D, Shaw D, Murphy K. Rigour in qualitative case-study research. Nurse Res. 2013;20(4):12–17. [DOI] [PubMed] [Google Scholar]
- 35.Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res. 2016;26(13):1802–1811. [DOI] [PubMed] [Google Scholar]
- 36.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 37.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. [DOI] [PubMed] [Google Scholar]
- 38.Hann NE. Transforming public health through community partnerships. Prev Chronic Dis. 2005;2(spec no):A03. [PMC free article] [PubMed] [Google Scholar]
- 39.Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health. 2000;21:369–402. [DOI] [PubMed] [Google Scholar]
- 40.National Advisory Committee on SARS and Public Health. Learning from SARS: renewal of public health in Canada. https://www.canada.ca/en/public-health/services/reports-publications/learning-sars-renewal-public-health-canada.html. Published 2004. Accessed February 6, 2022.
- 41.Public Health Agency of Canada, Health Canada. Lessons learned review: Public Health Agency of Canada and Health Canada response to the 2009 H1N1 pandemic. https://www.canada.ca/en/public-health/corporate/mandate/about-agency/office-evaluation/evaluation-reports/lessons-learned-review-public-health-agency-canada-health-canada-response-2009-h1n1-pandemic.html. Published 2010. Accessed August 17, 2022.
- 42.Association of Local Public Health Agencies. Public Health Resilience in Ontario. https://www.alphaweb.org/page/PH_Reports. Published 2022. Accessed August 17, 2022.
- 43.Sell H, Assi A, Driedger SM, et al. Continuity of routine immunization programs in Canada during the COVID-19 pandemic. Vaccine. 2021;39(39):5532–5537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization. The Impact of the COVID-19 Pandemic on Noncommunicable Disease Resources and Services: Results of a Rapid Assessment. Geneva, Switzerland; 2020. https://www.who.int/publications/i/item/9789240010291. Accessed August 17, 2022. [Google Scholar]
- 45.Nabavi N. Covid-19: pandemic will cast “a long shadow” on mental health, warns England's CMO. BMJ. 2021;373:n1655. [DOI] [PubMed] [Google Scholar]
- 46.The Lancet Public Health. COVID-19 pandemic: what's next for public health? Lancet Public Heal. 2022;7(5):e391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.HealthPartners. A silent wave: the shadow pandemic of chronic illness. https://healthpartners.ca/news/silent-wave-shadow-pandemic-chronic-illness. Published 2021. Accessed February 6, 2022.
- 48.Budd J, Miller BS, Manning EM, et al. Digital technologies in the public-health response to COVID-19. Nat Med. 2020;26(8):1183–1192. [DOI] [PubMed] [Google Scholar]
- 49.Buckeridge D. An evidence-informed vision for a public health data system in Canada. https://nccph.ca/projects/reports-to-accompany-the-chief-public-health-officer-of-canadas-report-2021. Published 2022. Accessed August 17, 2022.
- 50.Abimbola S, Baatiema L, Bigdeli M. The impacts of decentralization on health system equity, efficiency and resilience: a realist synthesis of the evidence. Health Policy Plan. 2019;34(8):605–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Galea S. Power and Public Health. Boston, MA: Boston University School of Public Health. https://www.bu.edu/sph/news/articles/2018/power-and-public-health/. Published 2018. Accessed February 6, 2022. [Google Scholar]
- 52.Baker M, Ivory D. Why public health faces a crisis across the U.S. The New York Times. https://www.nytimes.com/2021/10/18/us/coronavirus-public-health.html. Published 2021. Accessed February 6, 2022.
- 53.Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74(8):141. [DOI] [PMC free article] [PubMed] [Google Scholar]