Significance Statement
Hurricanes are disruptive weather events that can impede the provision of dialysis. The mortality risk for patients who are dialysis dependent and exposed to hurricanes is unknown. This study describes the association between hurricane exposure and 30-day mortality in the eastern United States from 1997 to 2017. Exposure to a hurricane with peak local wind speeds of hurricane force (≥64 knots) was associated with a higher mortality risk that peaked immediately after the hurricane and waned over time. This suggests that patients who are dialysis dependent are vulnerable during hurricanes, and highlights the need to safeguard this population, especially amidst the predicted increased hurricane intensity in the setting of anthropogenic climate change.
Keywords: mortality risk, extreme weather, tropical cyclones, hurricanes, climate change, dialysis, USRDS
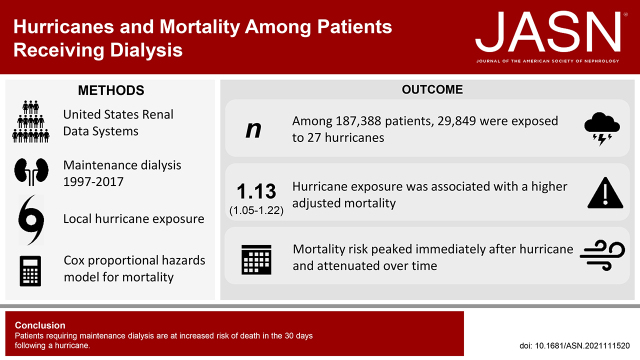
Visual Abstract
Abstract
Background
Hurricanes are severe weather events that can disrupt power, water, and transportation systems. These disruptions may be deadly for patients requiring maintenance dialysis. We hypothesized that the mortality risk among patients requiring maintenance dialysis would be increased in the 30 days after a hurricane.
Methods
Patients registered as requiring maintenance dialysis in the United States Renal Data System who initiated treatment between January 1, 1997 and December 31, 2017 in one of 108 hurricane-afflicted counties were followed from dialysis initiation until transplantation, dialysis discontinuation, a move to a nonafflicted county, or death. Hurricane exposure was determined as a tropical cyclone event with peak local wind speeds ≥64 knots in the county of a patient’s residence. The risk of death after the hurricane was estimated using time-varying Cox proportional hazards models.
Results
The median age of the 187,388 patients was 65 years (IQR, 53–75) and 43.7% were female. There were 27 hurricanes and 105,398 deaths in 529,339 person-years of follow-up on dialysis. In total, 29,849 patients were exposed to at least one hurricane. Hurricane exposure was associated with a significantly higher mortality after adjusting for demographic and socioeconomic covariates (hazard ratio, 1.13; 95% confidence interval, 1.05 to 1.22). The association persisted when adjusting for seasonality.
Conclusions
Patients requiring maintenance dialysis have a higher mortality risk in the 30 days after a hurricane.
Tropical cyclones are rotational storm systems that derive energy from tropical and subtropical ocean waters. In the Atlantic and Northeast Pacific Oceans, these storms include tropical depressions, tropical storms, and hurricanes,1 whereas in other regions they are referred to by other names, such as typhoons. On landfall, these storms bring high winds, storm surges, and heavy rain, which results in massive infrastructural and economic damage.2–4 With anthropogenic climate change, the average intensity of tropical cyclones may rise, thereby increasing the proportion of category 4 and 5 hurricanes, cyclone-associated precipitation, and coastal storm surge.5,6
Official storm-related death tolls may underestimate loss of life from indirect causes (e.g., disrupted access to medical care). For example, estimates of excess deaths in Puerto Rico after Hurricane Maria in 2017 ranged from 18- to 72-fold higher than the official death count of 64.7–10 Storms may fragment health care delivery, leading to poor outcomes in vulnerable populations, such as those with cancer.11
Patients who require maintenance dialysis are particularly vulnerable to extreme weather events. Studies have shown higher mortality among patients who are dialysis dependent when exposed to heat waves and wildfire smoke.12,13 Failed power, water, and transportation systems, patient displacement, and hospital surges can impede dialysis access.14,15 Hurricanes have been linked to higher rates of missed dialysis,16 emergency department visits,17–19 and hospitalizations.17,20 Studies examining mortality risk in patients receiving maintenance dialysis after individual hurricanes, however, have yielded mixed findings.17,18
To determine the potential effect of severe weather events on death in the dialysis population, we estimated the association between time-varying, county-level hurricane exposure and 30-day mortality among patients receiving in-center and home dialysis in the United States. Because hurricanes may interrupt dialysis delivery, we hypothesized that hurricane exposure would be associated with an increased risk of death among patients receiving dialysis.
Methods
Study Population
We performed a retrospective cohort analysis of patients in the United States Renal Data System (USRDS) database. This is a national registry of patients requiring maintenance dialysis using information collected through a collaboration with the Centers for Medicare & Medicaid Services, the United Network for Organ Sharing, and the ESRD Networks.
The cohort included patients who initiated dialysis for kidney failure from January 1, 1997 to December 31, 2017 in a county in the eastern half of the United States where at least one tropical cyclone occurred with local peak sustained wind speeds of ≥64 knots during this timeframe. Use of USRDS data was deemed exempt at the Johns Hopkins School of Medicine because patients cannot be identified directly or through linked identifiers.
Exposure
Hurricane data were derived from the hurricaneexposure21 and hurricaneexposuredata22 R packages, which contain continuous county-level spatiotemporal storm metrics tracking all tropical cyclones that came within 250 km of any county in the eastern half of the United States from 1988 to 2018. Details have been previously described.23–25 In brief, using storm-tracking observations recorded in the Atlantic hurricane database,26 1-minute surface wind speeds throughout each storm were estimated at each county mean population center through modeling each storm’s wind field. From these local wind measures, the peak sustained wind speed per county was determined for each storm.
In the primary analysis, we defined a hurricane exposure as the occurrence of tropical cyclone–associated local peak sustained winds of hurricane force on the Beaufort Wind Scale (≥64 knots) at the mean population center of a patient’s county of residence.24 Of note, this is distinct from the Saffir–Simpson Hurricane Wind Scale, which classifies hurricanes by their storm-wide maximum sustained wind speeds.27 Exposure was at the county level and thus shared among all patients residing in the same county at a given time. Time-updated county of residence was obtained from the USRDS database.
In secondary analyses, we evaluated exposure to a tropical storm or hurricane, defined as tropical cyclone–associated local sustained wind speeds of at least gale-force on the Beaufort Wind Scale (≥34 knots). In addition, we incorporated precipitation levels. Daily county-level precipitation totals from 5 days before, through 3 days after cyclone exposure were derived from the hurricaneexposure R package and summed over this 9-day span to calculate the cumulative precipitation for each county. We then evaluated exposures to hurricanes or tropical storm/hurricanes with heavy precipitation events, defined as either ≥150 mm or ≥200 mm. Precipitation levels were available through 2011.
Outcome
The primary outcome was all-cause mortality. Date of death was reported in the USRDS database. Patients were considered at risk from dialysis initiation until: (1) recovery of kidney function, (2) dialysis discontinuation, (3) loss to follow-up, (4) change of residence to a county unaffected by a hurricane during the study period, or (5) transplantation. Patients could re-enter the risk set if they returned to dialysis after dialysis discontinuation or if they moved to an at-risk county. Patients were followed through December 31, 2017.
Covariate Selection
We incorporated both individual-level and ZIP code–level covariates. Individual-level covariates were extracted from the USRDS database. Age was defined by years at the time of dialysis initiation. Sex was reported as male or female. Given previously reported differences in dialysis survival by race,28–30 we included race and ethnicity, which was categorized as non-Hispanic Black, non-Hispanic White, Hispanic, and other, which included missing race and ethnicity. Socioeconomic covariates were assessed at the ZIP-code level and abstracted from the US Census Bureau 2011 American Community Survey. These included percent having completed college or additional education, percent with household income below the federal poverty level, and the median monthly housing cost. Patient ZIP codes were time-updated whenever the county of residence changed. Additional variables of interest for subgroup and effect modification analyses included ESKD cause (diabetes mellitus, hypertension, glomerulonephritis, or other), which were retrieved from the USRDS Database Medical Evidence Form, and time-updated dialysis modality (in-center hemodialysis, home hemodialysis, peritoneal dialysis, or unknown).
Statistical Analyses
Baseline characteristics were reported for the population overall and stratified by whether a patient was ever exposed to a hurricane. The number of patient-hurricane exposures was mapped by county (QGIS, version 3.20.3). The following were reported for each individual storm: the number of exposed counties, the percent of exposed patients who died, and the mean and range of county level, sustained wind speeds and cumulative precipitation.
Cox proportional hazards regression models were fit to estimate the association between hurricane exposure and mortality. Patients entered the risk set on the date of first dialysis. Hurricane exposure was modeled as a time-varying covariate lasting 30 days or until a subsequent hurricane exposure, whichever came first (Supplemental Figure 1). We sequentially adjusted for age, sex, race and ethnicity, and year of dialysis initiation (modeled as a nominal categorical variable by year to account for long-term trends) in a demographic-adjusted model, and additionally adjusted for educational attainment, poverty level, and monthly housing cost in a demographic and socioeconomic status (SES)–adjusted model. Complete case analysis was used (Supplemental Table 1). All regressions were stratified by county (i.e., an adjusted baseline hazard was estimated for each county) to account for mortality variation by county. Variation in survival by county was shown by graphing the 25th to 75th percentile baseline survival adjusted for demographic and SES model covariates.
Subgroup analyses were performed by dialysis modality (in-center hemodialysis compared with combined home modalities), sex, race and ethnicity, cause of ESKD, year of dialysis initiation (categorized as 1997–2003, 2004–2010, 2011–2017), percent below federal poverty level (by quartile), and state of residence. Multiplicative effect modification was tested by including a product term of hurricane exposure and covariate of interest.
In the sensitivity analysis, we evaluated whether hurricane-associated mortality risk varied over time. To do this, we redefined the length of exposure time associated with a hurricane from 30 days to 1, 3, 7, 14, 60, and 90 days in the demographic/SES adjusted model.
We also tested for confounding by season in two ways: first, by further adjusting for month of cohort exit as a nominal categorical variable, and second, by assessing the unadjusted association between tropical cyclone exposure and death as a case-control study using each patient as their own control. This was achieved by limiting the study population to all patients with dialysis vintage of ≥13 months who died. We assessed cyclone exposure in the 30 days before death, compared with the 30 days before the same date 1 year earlier.
Primary analyses were repeated using tropical storm or hurricane as the exposure (increasing the sample size to include patients who lived in a county that had at least one tropical storm or hurricane between 1997 and 2017). We evaluated tropical storm– or hurricane-associated mortality over multiple exposure time periods as described above for hurricanes. We also repeated primary analyses using combined windspeed (hurricane or tropical storm/hurricane) and cumulative precipitation components (150 mm or 200 mm) as the exposure. For these analyses, patients were only considered exposed if their county of residence met both wind and precipitation thresholds. Because precipitation data were limited to storms before 2012, these analyses were censored on December 31, 2011. P values <0.05 were considered significant. Statistical analysis was performed using R version 4.0.2 (Vienna, Austria) and Stata SE version 17.0 (StataCorp LLC, College Station, TX).
Results
Study Population
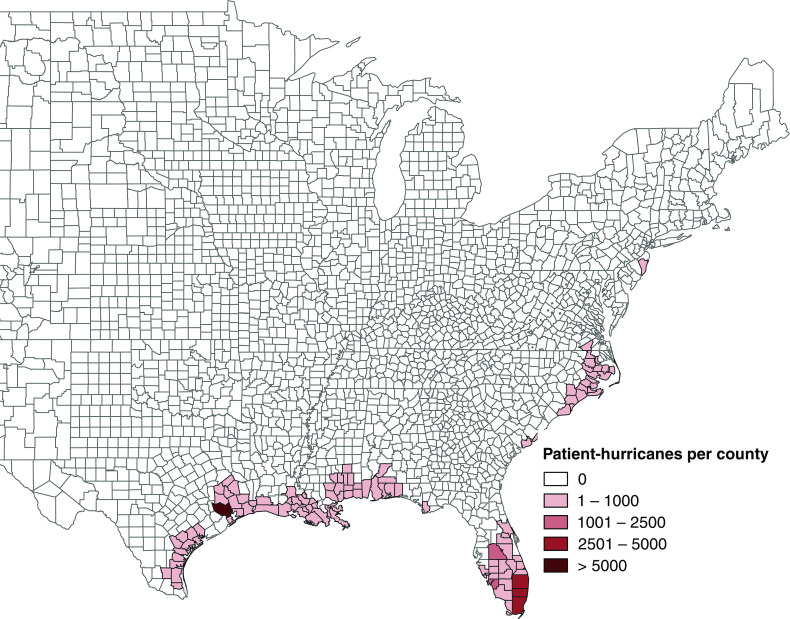
There were 27 hurricanes affecting 108 counties in total (Figure 1). A total of 187,388 patients were included in the analysis. The median age was 65 years (interquartile range, 53–75), 43.7% were female, and 92.5% of patients were receiving hemodialysis at baseline (Table 1). The 29,849 patients exposed to at least one hurricane had slightly lower socioeconomic indicators compared with those not exposed including lower educational attainment, larger proportion below the poverty level, and lower median monthly housing costs. Metrics for specific hurricanes are reported in Supplemental Table 2.
Figure 1.
Map of the number of hurricanes experienced by patients who are dialysis dependent in the United States by county from 1997 to 2017. Hurricane exposure is defined by exposure to a tropical cyclone with local peak wind speeds of ≥64 knots in the county of residence.
Table 1.
Characteristics at the time of dialysis initiation among patients who are dialysis dependent in the United States living in counties with at least one hurricane from 1997 to 2017, stratified by patient exposure status
| Characteristic | Overall | Never Exposed to Hurricanea | Exposed to at Least One Hurricane |
|---|---|---|---|
| Patients, n | 187,388 | 157,539 | 29,849 |
| Age, median (IQR) | 65 (53–75) | 65 (54–75) | 60 (49–71) |
| Female, n | 81,939 (43.7%) | 68,801 (43.7%) | 13,138 (44.0%) |
| Race and ethnicity, n | |||
| Hispanic | 34,204 (18.3%) | 28,510 (18.1%) | 5694 (19.1%) |
| Non-Hispanic Black | 65,226 (34.8%) | 52,931 (33.6%) | 12,295 (41.2%) |
| Non-Hispanic White | 84,206 (44.9%) | 72,948 (46.3%) | 11,258 (37.7%) |
| Other | 3752 (2.0%) | 3150 (2.0%) | 602 (2.0%) |
| Year of dialysis initiation, n | |||
| 1997–2003 | 52,646 (28.1%) | 39,591 (25.1%) | 13,055 (43.7%) |
| 2004–2010 | 63,443 (33.9%) | 50,930 (32.3%) | 12,513 (41.9%) |
| 2011–2017 | 71,299 (38.0%) | 67,018 (42.5%) | 4281 (14.3%) |
| Cause of ESKD, n | |||
| Diabetes mellitus | 82,942 (44.3%) | 69,438 (44.1%) | 13,504 (45.2%) |
| Hypertension | 61,171 (32.6%) | 51,405 (32.6%) | 9766 (32.7%) |
| Glomerulonephritis | 14,022 (7.5%) | 11,374 (7.2%) | 2648 (8.9%) |
| Other | 29,253 (15.6%) | 25,322 (16.1%) | 3931 (13.2%) |
| Initial dialysis modality, n | |||
| In-center hemodialysis | 173,334 (92.5%) | 145,557 (92.4%) | 27,777 (93.1%) |
| Home hemodialysis | 1635 (0.9%) | 1479 (0.9%) | 156 (0.5%) |
| Peritoneal dialysis | 12,165 (6.5%) | 10,306 (6.5%) | 1859 (6.2%) |
| Unknown modality | 254 (0.1%) | 197 (0.1%) | 57 (0.2%) |
| ZIP code-level characteristics, median (IQR) | |||
| Percent education college or above | 18.8 (12.5–28.2) | 19.1 (12.6–28.5) | 18.3 (11.9–27.4) |
| Percent below federal poverty level | 13.0 (8.1–20.1) | 12.9 (8.0–20.0) | 13.7 (8.3–20.6) |
| Monthly housing cost (USD) | 939 (751–1188) | 943 (753–1193) | 921 (728–1160) |
IQR, interquartile range; USD, US dollars.
Hurricane exposure is defined by exposure to a tropical cyclone with local peak wind speeds of ≥64 knots in the county of residence.
Association between Hurricane Exposure and Death
There were 105,398 deaths, over a mean time on dialysis of 2.82 years. Adjusted overall survival was fairly similar between counties (Supplemental Figure 2). Hurricane exposure was associated with higher mortality in the unadjusted model (hazard ratio [HR], 1.21; 95% confidence interval; [95% CI], 1.13 to 1.30), the demographic-adjusted model (HR, 1.13; 95% CI, 1.06 to 1.22), and the demographic and SES-adjusted model (HR, 1.13; 95% CI, 1.05 to 1.22; Table 2).
Table 2.
Associations of hurricane exposure and mortality among patients who are dialysis dependent in the United States from 1997 to 2017
| Adjustment Model | No. of Eligible Patients, n | Deaths, n | Deaths per 1000 Person-Years (95% Confidence Interval) | Hazard Ratio (95% Confidence Interval)a | P |
|---|---|---|---|---|---|
| Unadjusted | 187,388 | 105,398 | 199 (198 to 200) | 1.21 (1.13 to 1.30) | <0.001 |
| Demographic-adjusted modelb | 187,363 | 105,385 | 199 (198 to 206) | 1.13 (1.06 to 1.22) | <0.001 |
| Demographic and SES-adjusted modelc | 182,706 | 102,385 | 199 (198 to 200) | 1.13 (1.05 to 1.22) | <0.001 |
SES, socioeconomic status.
Death was attributed to a hurricane exposure if it occurred within 30 days of a qualifying weather event.
Adjusted for age, sex, race, and ethnicity, and year of dialysis initiation.
Additionally adjusted for educational attainment, poverty level, and monthly housing cost.
The risk of mortality after a hurricane was similar across subgroups (Figure 2). There was no significant difference in mortality risk by sex, race and ethnicity, year of dialysis initiation, cause of ESKD, time-updated dialysis modality, or percent below federal poverty level (Supplemental Table 3). The risk of death with hurricane exposure was also qualitatively similar across states (Supplemental Figure 3); in the full cohort, no effect modification by state was detected (Supplemental Table 4).
Figure 2.
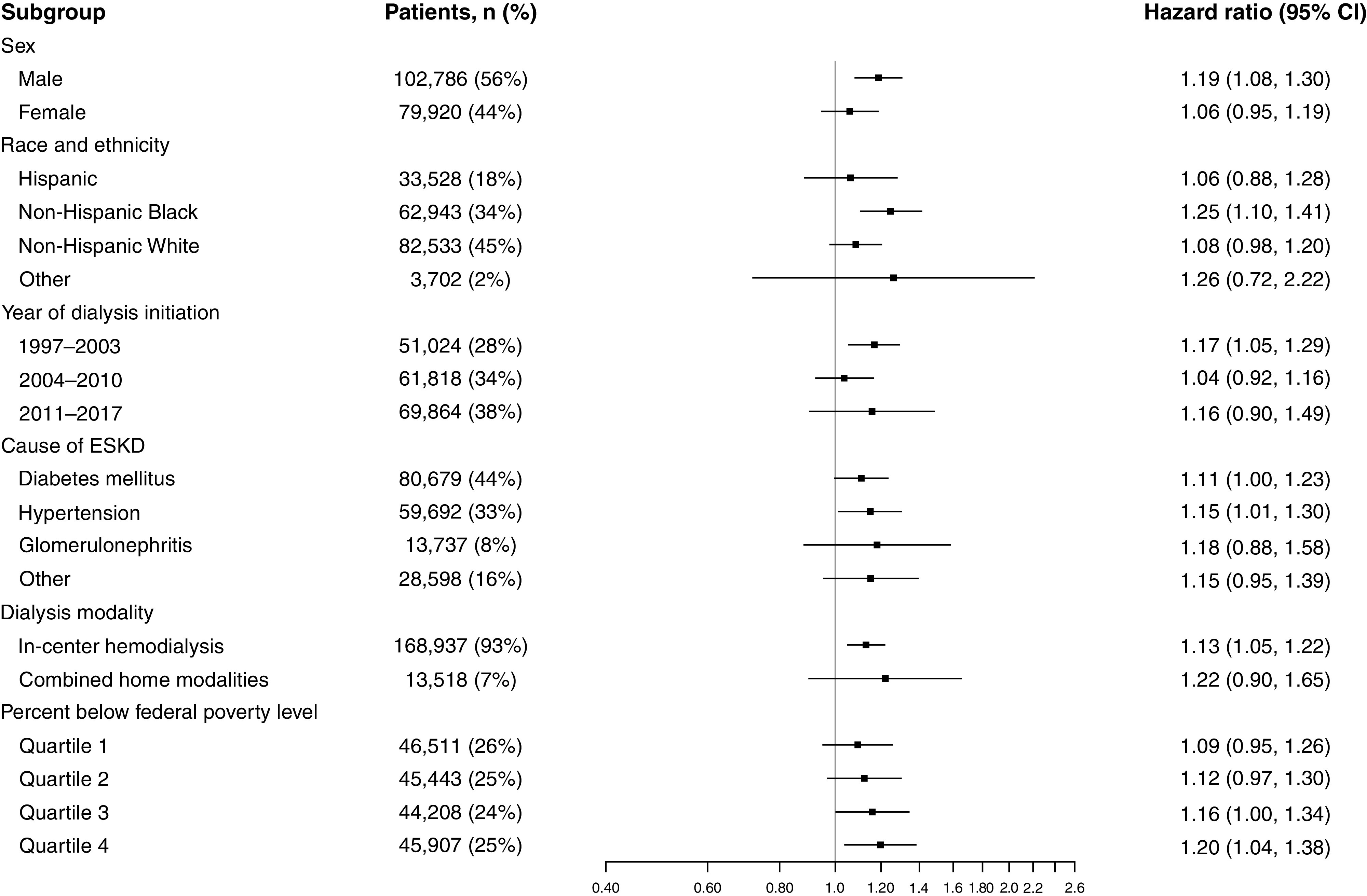
Forest plot demonstrating the associations of hurricane exposure and mortality in patients who are dialysis dependent in the United States from 1997 to 2017, stratified by subgroup. Patients with an unknown dialysis modality were excluded from this figure due to a lack of hurricane-related deaths.
Sensitivity Analyses
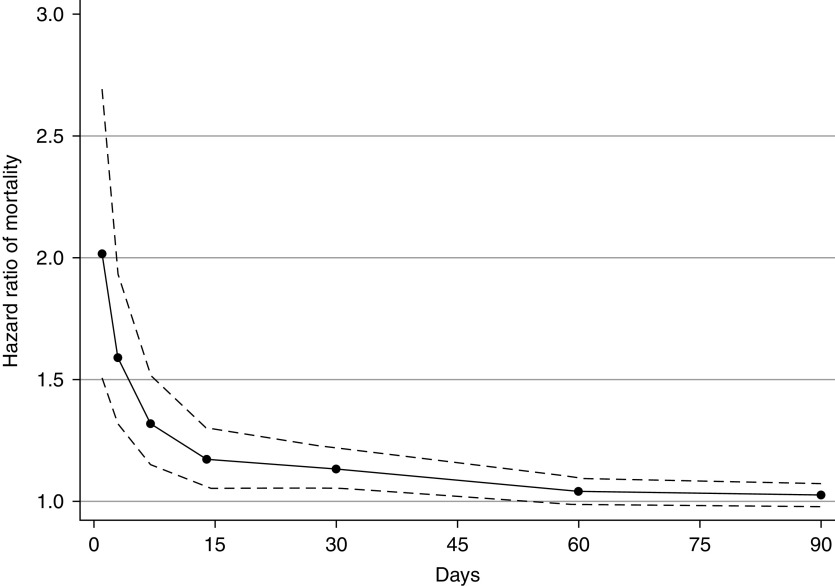
Hurricane-associated mortality risk was highest 1 day after the hurricane and then waned over time (Figure 3 and Supplemental Table 5).
Figure 3.
Hurricane-associated mortality HRs across varying poststorm mortality periods.
When additionally adjusting for the month of cohort exit, the hurricane-mortality association persisted (HR, 1.13; 95% CI, 1.05 to 1.21, Table 3). Similarly, patients receiving dialysis for ≥13 months had 20% higher odds (95% CI, 1.06 to 1.37) of exposure to a hurricane in the month before death compared with 1 year prior.
Table 3.
Sensitivity analyses for the association of hurricane exposure and mortality among patients who are dialysis dependent in the United States from 1997 to 2017
| Demographic and SES-Adjusted Modela | |||||
|---|---|---|---|---|---|
| Sensitivity Analysis | No. of Eligible Patients, nb | Events, nb | Events per 1000 Person-Years (95% Confidence Interval)b | Hazard Ratio (95% Confidence Interval)c | P |
| Accounting for seasonality | |||||
| Hurricane,d adjusted for month of cohort exit | 182,706 | 102,385 | 199 (198 to 200) | 1.13 (1.05 to 1.21) | 0.001 |
| Varying exposure definition | |||||
| Tropical storm or hurricanee | 975,261 | 564,644 | 197 (197 to 198) | 1.02 (1.00 to 1.05) | 0.02 |
| Including precipitationf | |||||
| Tropical storm or hurricanee and ≥150 mm precipitation | 666,461 | 370,721 | 217 (217 to 218) | 1.02 (0.98 to 1.06) | 0.44 |
| Tropical storm or hurricanee and ≥200 mm precipitation | 666,461 | 370,721 | 217 (217 to 218) | 1.05 (0.98 to 1.12) | 0.16 |
| Hurricaned and ≥150 mm precipitation | 122,100 | 66,083 | 220 (218 to 222) | 1.11 (0.98 to 1.27) | 0.11 |
| Hurricaned and ≥200 mm precipitation | 122,100 | 66,083 | 220 (218 to 222) | 1.27 (1.08 to 1.49) | 0.003 |
SES, socioeconomic status.
Adjusted for age, sex, race, and ethnicity, year of dialysis initiation, educational attainment, poverty level, and monthly housing cost.
Values are reported for demographic and SES-adjusted model. Complete case analysis was performed.
Death was attributed to a hurricane exposure if it occurred within 30 days of a qualifying weather event.
Hurricane exposure is defined by exposure to a tropical cyclone with local peak wind speeds of ≥64 knots in the county of residence.
Tropical storm or hurricane exposure is defined by exposure to a tropical cyclone with local peak wind speeds of ≥34 knots in the county of residence.
Analyses including precipitation were censored on December 31, 2011.
When lowering the local peak wind speed threshold to ≥34 knots, there were 76 tropical storms or hurricanes affecting 929 counties in total (Supplemental Figure 4, Supplemental Table 6). Of the 989,317 patients who are dialysis dependent living in these counties, 338,869 were exposed to at least one tropical storm or hurricane. Tropical storm or hurricane exposure was associated with increased mortality in the demographic and SES-adjusted model (HR, 1.02; 95% CI, 1.00 to 1.05). Mortality risk was highest 1 day after tropical storm or cyclone and declined rapidly (Supplemental Figure 5, Supplemental Table 7). When combining windspeed and cumulative precipitation thresholds, there was no increased risk of mortality for tropical storms or hurricanes with either ≥150 mm or ≥200 mm of precipitation. However, the hurricane-mortality association was qualitatively stronger after incorporating a cumulative precipitation threshold of ≥200 mm (HR, 1.27; 95% CI, 1.08 to 1.49), but not ≥150 mm (HR 1.11; 95% CI, 0.98 to 1.27).
Discussion
In a cohort of 187,388 patients receiving maintenance dialysis, mortality was significantly higher in the 30 days after a hurricane. Mortality risk peaked immediately after the hurricane, then attenuated over time. A slight but statistically significant mortality risk was observed when evaluating lower-severity storm exposures (local wind speeds ≥34 knots). Overall, this study suggests local exposure to tropical cyclones poses a risk for the survival of patients on dialysis.
Recent work has highlighted the range of disruption to dialysis services brought forth by natural disasters, including loss of power, water, transportation, and communication systems, along with evacuations and hospital surges.14 However, studies of dialysis-related outcomes have been limited to case studies of individual storms. After Hurricane Katrina in 2005, 94 Gulf Coast dialysis units were closed for ≥1 week,31 resulting in missed dialysis16 and excess hospitalizations,20 but no association between exposure to Hurricane Katrina and mortality among patients receiving dialysis was seen.32 In contrast, after Hurricane Sandy in 2012, patients receiving dialysis were found to have a higher 30-day mortality,17 along with increased dialysis-related emergency department visits17–19 and hospitalizations.17
The development of an open-access tropical cyclone database has facilitated the examination of multiple tropical cyclone events across time.23 Linking weather databases to national registries allows for a broader accounting of human health effects beyond direct fatalities and highlights storm and patient features associated with higher risk. In our study, we found evidence of a graded association with wind speed, in which hurricane-force winds had a mortality association of larger magnitude than gale-force winds. This is concerning in light of the projected increase in high-intensity hurricanes with climate change,5 potentially leading to a higher proportion of these deadlier storms. Although slower-moving storms may produce higher amounts of rainfall and resultant flooding, we did not observe increased mortality when coupling the slower wind threshold with high cumulative precipitation. This suggests high cyclone-related wind speeds may drive death more than cumulative precipitation.
The risk of mortality was greatest immediately after a hurricane and was detected through 30 days. The temporal pattern may reflect multiple processes including direct storm-related effects, exacerbation of underlying comorbid conditions, and missed dialysis. In the general US population, tropical cyclone exposure has been linked to higher death rates from infectious, respiratory, cardiovascular, neuropsychiatric, and injury-related causes.33 Furthermore, tropical cyclones often bring extreme heat, which has been linked to increased mortality among patients with ESKD.12 Dialysis sessions missed due to weather may contribute to early mortality after a hurricane event. Potassium, fluid, and uremic toxins accumulate with missed dialysis, leaving patients susceptible to cardiovascular events.34,35 Over longer poststorm durations, patients may face risks related to additional missed dialysis sessions, inadequate dialysis, complications from hospitalization, infectious risks, and lack of medication access. This is consistent with observations from Hurricane Katrina, in which 44% of patients in the affected area missed at least one dialysis session, 17% of patients missed at least three sessions, and 23% of patients were hospitalized within 1 month of the storm.16 Although patients receiving home dialysis modalities may be more resilient to natural disasters,36 we did not detect an effect modification by modality. This may be in part due to reduced statistical power among the lower number of patients receiving home modalities.
Coordinated efforts have supported patients who are dialysis dependent during natural disasters. The Renal Disaster Relief Task Force was established in 1989 after challenges providing dialytic care for crush victims of the 1988 Armenian earthquake.37,38 This organization provided first responders with logistical, personnel, and material support for kidney disease–related disasters around the world.37,38 After Hurricane Katrina, the Kidney Community Emergency Response Coalition was established in 2006.37,39 This multidisciplinary group disseminates preparatory guidance for dialysis care in the setting of a disaster. One recommendation is to administer early dialysis treatment before anticipated disruptions. When this was employed during Hurricane Sandy, 60% of patients in affected areas received early dialysis, and this was associated with lower odds of emergency department visit, hospitalization, and 30-day mortality compared with those who did not receive early dialysis.40 Given the possibility of increasing severity of tropical cyclone events, dialysis units and public health professionals should continue to enhance contingency plans to safeguard the welfare of patients who are dialysis dependent.
The strengths of this study include the large cohort size, the incorporation of numerous storms over time, and the assessment of two wind-speed thresholds. Although other studies have examined trends in community-level insurance claims, we were able to examine individual-level exposure and outcomes. Weaknesses include the lack of individual-level socioeconomic indicators and validated clinical comorbid conditions, because Centers for Medicare and Medicaid Services 2728–reported comorbidities have limited accuracy.41,42 We did not estimate the effect of other tropical cyclone features beyond high winds and precipitation such as flooding and storm surge, and precipitation totals were unavailable for storms since 2012. Consequently, our analysis may not include the mortality risk of storms that caused heavy flooding without hurricane-force winds. There may be exposure misclassification if a patient’s county of address does not match their location at the time of hurricane exposure, and residual confounding may be present. We were unable to compare the hurricane-related mortality among patients who are dialysis dependent with that of the general population. Future work should consider cause-specific mortality, additional storm features associated with higher mortality, and the comparative effectiveness of different storm response protocols. Efforts to model climate change-related health effects and mortality should consider the dialysis-dependent population.
In summary, we demonstrated that patients receiving maintenance dialysis are at increased risk of death after a tropical cyclone with hurricane-force winds. Future efforts should prioritize safeguarding this vulnerable population.
Disclosures
D. Segev reports having consultancy agreements with AstraZeneca, Bridge to Life, Caredx, CSL Behring, Jazz Pharmaceuticals, Kamada, Mallinckrodt, MediGO, Novartis, Regeneron, Sanofi, Takeda, Thermo Fisher Scientific, Transmedics, and Veloxis; reports receiving honoraria from AstraZeneca, Caredx, and Sanofi; and reports having an advisory or leadership role as Editor in Chief of Current Transplant Reports. G. Anderson reports employment with Arnold & Porter (spouse is a partner at this law firm) and Colorado State University; reports having a part-ownership in a family farm (privately held as LLC); and reports having patents or royalties through the university's technology transfer office for a role in codeveloping and coteaching several courses on Coursera, a platform for Massive Open Online Courses. M. Grams reports receiving honoraria from academic institutions for giving grand rounds and American Diabetes Assocation for reviewing abstracts; reports having an advisory or leadership role with the American Journal of Kidney Diseases, CJASN, JASN Editorial Board, Kidney Disease Improving Global Outcomes Executive Committee, NKF Scientific Advisory Board, and the USRDS Scientific Advisory Board; and reports having other interests or relationships with grant funding from the NKF, which receives funding from multiple pharmaceutical companies. M. McAdams-DeMarco reports receiving honoraria from UptoDate. All remaining authors have nothing to disclose.
Funding
This work was supported by National Institutes of Health, National Heart, Lung, and Blood Institute grants T32HL007024 (M. Blum) and K24HL155861 (M. Grams).
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Author Contributions
M. Blum, G. Brooke Anderson, M. Grams, and M. McAdams-DeMarco conceptualized the study; M. Blum, Y. Feng, and M. Grams were responsible for the formal analysis; G. Brooke Anderson, M. McAdams-DeMarco, and D. Segev were responsible for the data curation; M. Grams, M. McAdams-DeMarco, and D. Segev provided supervision; M. Blum and M. Grams wrote the original draft; and M. Blum, G. Brooke Anderson, Y. Feng, M. Grams, M. McAdams-DeMarco, and D. Segev reviewed and edited the manuscript.
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2021111520/-/DCSupplemental.
Supplemental Table 1. Number of patients with missing baseline covariates.
Supplemental Table 2. Characteristics of hurricanes that brought hurricane-force winds to one or more study counties.
Supplemental Table 3. Multiplicative effect modification terms for the association of hurricanes and mortality by subgroup.
Supplemental Table 4. Multiplicative effect modification terms for the association of hurricanes and mortality by state of residence.
Supplemental Table 5. Associations of hurricane exposure and mortality across varied poststorm mortality periods among patients who are dialysis dependent in the United States from 1997 to 2017.
Supplemental Table 6. Characteristics of tropical storms or hurricanes that brought gale-force or higher winds to one or more study counties.
Supplemental Table 7. Associations of tropical storm or hurricane exposure and mortality across varied postcyclone mortality periods among patients who are dialysis dependent in the USRDS population from 1997 to 2017.
Supplemental Figure 1. Schematic of time-varying hurricane exposure and 30-day mortality with examples to illustrate exposure and outcome.
Supplemental Figure 2. Adjusted survival of patients who are dialysis dependent in the United States living in a county with a hurricane exposure from 1997 to 2017, delineated by county, among counties with the 25th to 75th percentile adjusted survival.
Supplemental Figure 3. Forest plot demonstrating the associations of hurricane exposure and mortality in patients who are dialysis dependent in the United States from 1997 to 2017, stratified by state.
Supplemental Figure 4. Map of the number of patient-tropical storm or hurricanes experienced by patients who are dialysis dependent in the United States by county from 1997 to 2017. Tropical storm or hurricane exposure is defined by exposure to a tropical cyclone with local peak wind speeds of ≥34 knots in the county of residence.
Supplemental Figure 5. Tropical storm and hurricane-associated mortality HRs across varying poststorm mortality periods.
References
- 1.National Hurricane Center and Central Pacific Hurricane Center : National Oceanic and Atmospheric Administration: Glossary of NHC Terms. Available at: https://www.nhc.noaa.gov/aboutgloss.shtml. Accessed September 1, 2021
- 2.Alemazkoor N, Rachunok B, Chavas DR, Staid A, Louhghalam A, Nateghi R, et al. : Hurricane-Induced power outage risk under climate change is primarily driven by the uncertainty in projections of future hurricane frequency. Sci Rep 10: 15270, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lenzen M, Malik A, Kenway S, Daniels P, Leung Lam K, Geschke A: Economic damage and spillovers from a tropical cyclone. Nat Hazards Earth Syst Sci 19: 137–151, 2019 [Google Scholar]
- 4.Weinkle J, Landsea C, Collins D, Musulin R, Crompton RP, Klotzbach PJ, et al. : Normalized hurricane damage in the continental United States 1900–2017. Nat Sustain 1: 808–813, 2018 [Google Scholar]
- 5.Hoegh-Guldberg O, Jacob D, Taylor M, Bindi M, Brown S, Camilloni I, et al. : Impacts of 1.5°C Global Warming on Natural and Human Systems. In: Global Warming of 1.5°C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C Above Pre-industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, edited by Masson-Delmotte V, Zhai P, Pörtner H-O, Roberts D, Skea J, Shukla PR, et al., New York, Cambridge University Press, 2018, pp 1753–12 [Google Scholar]
- 6.Knutson T, Camargo SJ, Chan JCL, Emanuel K, Ho CH, Kossin J, et al. : Tropical cyclones and climate change assessment: Part II: Projected response to anthropogenic warming. Bull Am Meteorol Soc 101: E303–E322, 2020 [Google Scholar]
- 7.Kishore N, Marqués D, Mahmud A, Kiang MV, Rodriguez I, Fuller A, et al. : Mortality in Puerto Rico after Hurricane Maria. N Engl J Med 379: 162–170, 2018 [DOI] [PubMed] [Google Scholar]
- 8.Santos-Lozada AR, Howard JT: Use of death counts from vital statistics to calculate excess deaths in Puerto Rico following Hurricane Maria. JAMA 320: 1491–1493, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Santos-Burgoa C, Sandberg J, Suárez E, Goldman-Hawes A, Zeger S, Garcia-Meza A, et al. : Differential and persistent risk of excess mortality from Hurricane Maria in Puerto Rico: A time-series analysis. Lancet Planet Health 2: e478–e488, 2018 [DOI] [PubMed] [Google Scholar]
- 10.Cruz-Cano R, Mead EL: Causes of excess deaths in Puerto Rico after Hurricane Maria: A time-series estimation. Am J Public Health 109: 1050–1052, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nogueira LM, Sahar L, Efstathiou JA, Jemal A, Yabroff KR: Association between declared hurricane disasters and survival of patients with lung cancer undergoing radiation treatment. JAMA 322: 269–271, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Remigio RV, Jiang C, Raimann J, Kotanko P, Usvyat L, Maddux FW, et al. : Association of extreme heat events with hospital admission or mortality among patients with end-stage renal disease. JAMA Netw Open 2: e198904, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xi Y, Kshirsagar AV, Wade TJ, Richardson DB, Brookhart MA, Wyatt L, et al. : Mortality in US hemodialysis patients following exposure to wildfire smoke. J Am Soc Nephrol 31: 1824–1835, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith RS, Zucker RJ, Frasso R: Natural disasters in the Americas, dialysis patients, and implications for emergency planning: A systematic review. Prev Chronic Dis 17: E42, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abir M, Jan S, Jubelt L, Merchant RMLN, Lurie N: The impact of a large-scale power outage on hemodialysis center operations. Prehosp Disaster Med 28: 543–546, 2013 [DOI] [PubMed] [Google Scholar]
- 16.Anderson AH, Cohen AJ, Kutner NG, Kopp JB, Kimmel PL, Muntner P: Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int 75: 1202–1208, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Kelman J, Finne K, Bogdanov A, Worrall C, Margolis G, Rising K, et al. : Dialysis care and death following Hurricane Sandy. Am J Kidney Dis 65: 109–115, 2015 [DOI] [PubMed] [Google Scholar]
- 18.Gotanda H, Fogel J, Husk G, Levine JM, Peterson M, Baumlin K, et al. : Hurricane Sandy: Impact on emergency department and hospital utilization by older adults in lower Manhattan, New York (USA). Prehosp Disaster Med 30: 496–502, 2015 [DOI] [PubMed] [Google Scholar]
- 19.Lee DC, Smith SW, Carr BG, Doran KM, Portelli I, Grudzen CR, et al. : Geographic distribution of disaster-specific emergency department use after Hurricane Sandy in New York City. Disaster Med Public Health Prep 10: 351–361, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howard D, Zhang R, Huang Y, Kutner N: Hospitalization rates among dialysis patients during Hurricane Katrina. Prehosp Disaster Med 27: 325–329, 2012 [DOI] [PubMed] [Google Scholar]
- 21.Anderson B, Yan M, Ferreri J, Crosson W, Al-Hamdan M, Schumacher A, et al. : hurricaneexposure: Explore and map county-level hurricane exposure in the United States. R package version 0.1.1, 2020. Available at https://cran.r-project.org/package=hurricaneexposure. Accessed June 3, 2021
- 22.Anderson B, Schumacher A, Crosson W, Al-Hamdan M, Yan M, Ferreri J, et al. : hurricaneexposuredata: Data characterizing exposure to hurricanes in United States counties. R package version 0.1.0, 2020. Available at https://github.com/geanders/hurricaneexposuredata. Accessed June 3, 2021
- 23.Anderson GB, Ferreri J, Al-Hamdan M, Crosson W, Schumacher A, Guikema S, et al. : Assessing United States county-level exposure for research on tropical cyclones and human health. Environ Health Perspect 128: 107009, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parks RM, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, Kioumourtzoglou MA: Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat Commun 12: 1545, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yan M, Wilson A, Dominici F, Wang Y, Al-Hamdan M, Crosson W, et al. : Tropical cyclone exposures and risks of emergency Medicare hospital admission for cardiorespiratory diseases in 175 Urban United States counties, 1999-2010. Epidemiology 32: 315–326, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Landsea C, Franklin J, Beven J: The revised Atlantic hurricane database (HURDAT2). Available at: https://www.nhc.noaa.gov/data/hurdat/hurdat2-format-atlantic.pdf. Accessed July 26, 2021
- 27.National Hurricane Center and Central Pacific Hurricane Center : National Oceanic and Atmospheric Administration: Saffir-Simpson Hurricane Wind Scale. Available at: https://www.nhc.noaa.gov/aboutsshws.php. Accessed February 2, 2022
- 28.Crews DC, Sozio SM, Liu Y, Coresh J, Powe NR: Inflammation and the paradox of racial differences in dialysis survival. J Am Soc Nephrol 22: 2279–2286, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kucirka LM, Grams ME, Lessler J, Hall EC, James N, Massie AB, et al. : Association of race and age with survival among patients undergoing dialysis. JAMA 306: 620–626, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ku E, Yang W, McCulloch CE, Feldman HI, Go AS, Lash J, et al. ; CRIC Study Investigators : Race and mortality in CKD and dialysis: Findings From the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis 75: 394–403, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, et al. : Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol 2: 814–824, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Kutner NG, Muntner P, Huang Y, Zhang R, Cohen AJ, Anderson AH, et al. : Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int 76: 760–766, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Parks RM, Benavides J, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, et al. : Association of tropical cyclones with county-level mortality in the US. JAMA 327: 946–955, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Foley RN, Gilbertson DT, Murray T, Collins AJ: Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med 365: 1099–1107, 2011 [DOI] [PubMed] [Google Scholar]
- 35.Flythe JE, Lacson E Jr: Outcomes after the long interdialytic break: Implications for the dialytic prescription. Semin Dial 25: 1–8, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdel-Kader K, Unruh ML: Disaster and end-stage renal disease: Rargeting vulnerable patients for improved outcomes. Kidney Int 75: 1131–1133, 2009 [DOI] [PubMed] [Google Scholar]
- 37.Kenney RJ: Emergency preparedness concepts for dialysis facilities: Reawakened after Hurricane Katrina. Clin J Am Soc Nephrol 2: 809–813, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Vanholder R, van der Tol A, De Smet M, Hoste E, Koç M, Hussain A, et al. : Earthquakes and crush syndrome casualties: Lessons learned from the Kashmir disaster. Kidney Int 71: 17–23, 2007 [DOI] [PubMed] [Google Scholar]
- 39.Dent L, Finne K, Lurie N: Progress in emergency preparedness for dialysis care 10 years after Hurricane Katrina. Am J Kidney Dis 66: 742–744, 2015 [DOI] [PubMed] [Google Scholar]
- 40.Lurie N, Finne K, Worrall C, Jauregui M, Thaweethai T, Margolis G, et al. : Early dialysis and adverse outcomes after Hurricane Sandy. Am J Kidney Dis 66: 507–512, 2015 [DOI] [PubMed] [Google Scholar]
- 41.Longenecker JC, Coresh J, Klag MJ, Levey AS, Martin AA, Fink NE, et al. : Validation of comorbid conditions on the end-stage renal disease medical evidence report: The CHOICE study. Choices for healthy outcomes in caring for ESRD. J Am Soc Nephrol 11: 520–529, 2000 [DOI] [PubMed] [Google Scholar]
- 42.Krishnan M, Weinhandl ED, Jackson S, Gilbertson DT, Lacson E Jr: Comorbidity ascertainment from the ESRD Medical Evidence Report and Medicare claims around dialysis initiation: A comparison using US Renal Data System data. Am J Kidney Dis 66: 802–812, 2015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.