Abstract
Background
Owing to important differences in surgical technique, laparoscopic right colectomy with intracorporeal (ICA) compared to extracorporeal (ECA) anastomotic technique may result in improved patient outcomes. We aimed to compare both techniques according to incisional hernias and other pertinent perioperative characteristics, post-operative complications, and oncologic quality markers.
Methods
All adult patients undergoing laparoscopic right colectomies between 2015 and 2020 at a single institution were included. ICA and ECA techniques were compared based on selected outcomes using univariable and multivariable statistical analyses, as appropriate. Subgroup analyses were restricted to patients with neoplastic indications for surgery and non-urgent operations.
Results
A total of 517 patients met inclusion criteria, of which 139 (26.9%) underwent ICA and 378 (73.1%) underwent ECA. ICA and ECA patients had similar baseline characteristics. At two years of follow-up, a lower proportion of ICA patients developed a hernia at the extraction incision (1.5% vs. 7.1%, p = 0.02) and ICA was associated with an 80% reduction in extraction incision hernias (aHR 0.20, p = 0.03). These results were stable through subgroup and sensitivity analyses. Median operative time was longer in the ICA group (186 min vs. 135 min, p < 0.001), but the gap in operative time narrowed during the study period. Median length of stay was one calendar day shorter in the ICA group (3 days vs. 4 days, p = 0.007) and ICA was associated with a 13% decrease in the length of stay (aRR 0.87, p = 0.02). The incidence of superficial wound infections, anastomotic leaks and re-interventions was lower in ICA patients, but this difference was not statistically significant. 90-day unscheduled visits, readmissions, and mortalities were similar across both groups, as were oncologic outcomes.
Conclusion
Laparoscopic right colectomies with intracorporeal anastomoses are associated with a reduction in incisional hernias and shorter hospital lengths of stay without compromising on patient safety or oncologic principles.
Graphical abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s00464-022-09585-0.
Keywords: Intracorporeal anastomosis, Incisional hernia, Laparoscopic colectomy
The advent of a laparoscopic approach to patients with right-sided colonic pathologies transformed patient care [1, 2] and the progression from laparoscopic-assisted extracorporeal anastomosis (ECA) to totally laparoscopic intracorporeal ileocolic anastomosis (ICA) held similar promise to those championing this technique. ICA circumvents the morbid and painful midline extraction incisions which plague most patients undergoing ECA, and can mitigate the mesenteric traction on the terminal ileum and transverse colon necessary to exteriorize them for anastomosis. Therefore, ICA may be associated with reduced rates of extraction incision hernias and faster recovery [3].
Despite many publications on favorable outcomes over the past two decades, [4–7] ICA’s uptake has slowed, and its utilization has not surpassed ECA. A recent international survey found that most surgeons performing laparoscopic right colon resections employed ECA in the majority of their operations. Barriers to uptake of ICA are likely the result of increased operative time and the required proficiency in laparoscopic suturing and knot tying [8–10].
This study aims to provide a granular and pragmatic comparison of both techniques according to incisional hernias and other pertinent perioperative characteristics, post-operative complications, and oncologic quality markers.
Method
Study design and cohort
This is a single institution retrospective cohort study leveraging institutional chart review health data. This study was approved by the Health Sciences Research Ethics Board at the University of Western Ontario. Reporting is in accordance with the REporting of studies Conducted using Observational Routinely collected Data (RECORD) Statement (Appendix 1) [11]. The hospital’s administrative healthcare registry was interrogated and all adults who underwent a right-sided colon resection at London Health Sciences Centre’s University Hospital in London, Canada between 2015 and 2020 were identified. There was no exclusion based on indication or urgency of surgery. Patients’ operative reports were reviewed to assess for eligibility. Only patients who underwent their first ileocolic resections, right colectomies, or extended right colectomies were included. For simplicity, these are referred to as right colectomies in this study. Those who underwent segmental colon resections, subtotal colectomies, or total abdominal colectomies were not eligible for inclusion. If patients had undergone a previous eligible surgery, only the first surgery was included, provided it occurred during the eligible time-period. Patients were excluded if they underwent a planned laparotomy, conversion to a laparotomy for a purpose other than an extracorporeal anastomosis, or a stoma formation. Additionally, patients were excluded if they underwent any concomitant procedure apart from primary repairs of umbilical or ventral hernias without mesh. Patients with previous hernia repairs with or without mesh were not excluded.
Exposure
Patient groups were based on the ileocolic anastomotic technique. ECA was defined by exteriorization of the bowel through an extraction incision for anastomosis where at least the colonic mobilization and ileocolic pedicle ligation were performed laparoscopically; if either of these were performed after the extraction incision, then the patient was deemed to have undergone a conversion to laparotomy and was excluded from the study. ICA was defined as a totally laparoscopic resection and anastomosis, where non laparoscopic port incision was made only for extraction of the specimen.
Outcomes
This study provides a granular comparison of both anastomotic techniques according to incisional hernias and other meaningful clinical outcomes.
Incisional hernias were specified as those occurring at the extraction incision or elsewhere, and included if they were described in the patient’s chart within two years of the index surgery. These were further characterized according to whether they were surgically repaired, as these may represent more severe hernias. Hernias were also considered surgically repaired if an operative hernia repair was planned but not yet performed in order to account for COVID-19 pandemic delays.
Operative time was measured from first skin incision to skin closure and excluding anesthesia time. Length of stay was measured as the number of calendar days between date of surgery and date of discharge. Superficial wound infections were characterized according to the American College of Surgeons National Surgical Quality Improvement Project criteria. Anastomotic leak was assessed clinically on chart review according to previously published definitions for presence and grade [12, 13]. Re-interventions were subclassified as percutaneous, endoscopic, or operative procedures performed for complications relating to surgery. Patients’ charts were reviewed for emergency department visits, readmissions, and mortalities occurring within 90 days of their index surgery date. Nodal counts, adequate node sample (at least 12 nodes) [14], and receipt of chemotherapy were recorded and compared in patients with pathologically proven colonic or appendiceal malignancies which were of adenocarcinoma, neuroendocrine, or mixed histology.
Covariates
Clinically relevant patient characteristics were collected and included age, sex, smoking status, American Society of Anesthesiologists physical status classification (ASA), previous abdominal surgeries, previous abdominal wall hernia repairs, presence of intra-abdominal mesh for hernia repair, year of surgery, urgency category of surgery (scheduled or urgent), indication for surgery (malignancy, benign neoplasm, inflammatory bowel disease or other), location of pathology, surgery type (ileocolic, right hemicolectomy, and extended right hemicolectomy), and the presence of abdominal wall hernias at the index surgery.
Statistical analysis
Patient baseline characteristics were compared using appropriate statistical tests. Multivariable regression models were selected according to distribution and dispersion and were specified to characterize the association between ICA/ECA and the selected outcomes. Covariates were selected a priori as potential confounders based on clinical relevance. These covariates were assessed for statistical collinearity and covariates were limited to avoid overparameterization. Model adjustments and effect estimates are presented in Appendix 2.
The extraction incision hernia definition was expanded to include all incisional hernias in a sensitivity analysis to account for patients undergoing reoperation laparotomies, since these patients may develop a midline hernia which could not be differentiated from the original midline extraction incision predominantly performed in ECA patients. Additional sensitivity analyses were planned to examine only surgically repaired hernias. A secondary analysis was planned to assess the association between superficial wound infections at the extraction incision and the development of an extraction incision hernia.
Length of stay was modeled with inclusion and exclusion of patients with early mortalities or transfer to other hospitals. Loss of follow-up due to mortality or relocation was compared between both groups. It was accounted for as competing risks for anastomotic leaks and reinterventions by specifying a composite outcome of all three states in sensitivity analyses. In time-to-event analyses, when follow-up was no longer possible, patients were censored on their last day of contact.
Some of the surgeons in this study have exclusively colorectal practices and a preponderance of patients with Crohn’s Disease. Given the difference in case-mix, a subgroup analysis was performed excluding non-neoplastic indications for surgery and urgent (non-scheduled) surgeries.
Statistical analyses were performed using SAS 3.8 Enterprise Edition (SAS Institute Inc., Cary, NC, USA). All tests were two-sided with p-values of < 0.05.
Results
Study cohort
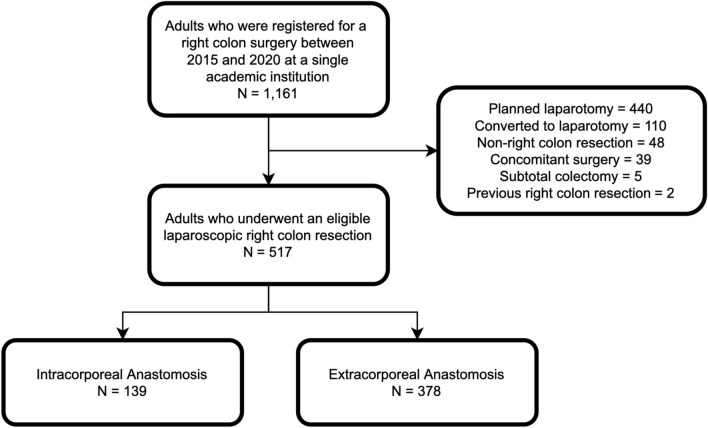
There were 1161 adults who underwent a right-sided colon resection between 2015 and 2020 at our institution (Fig. 1). Of these, 517 patients underwent an eligible laparoscopic right colectomy: 139 ICA (26.9%) and 378 ECA (73.1%). ICA and ECA patients had similar baseline characteristics (Table 1). There were five patients (3.6%) in the ICA group and ten patients (2.7%) in the ECA group who had undergone a prior ventral hernia repair. There was an increase uptake of ICA technique during the study period, consequently the median year of surgery was more recent in ICA patients (2019 vs. 2017, p < 0.001).
Fig. 1.
Patient Flow Diagram
Table 1.
Baseline Demographics and disease-related characteristics
| Characteristic | ICA (n = 139) | ECA (n = 378) | p-value |
|---|---|---|---|
| Age, median (IQR) | 71 (63–79) | 71 (58–78) | 0.28 |
| Female sex, n (%) | 71 (51.1%) | 215 (56.9%) | 0.24 |
| Active smoker, n (%) | 13 (9.4%) | 53 (14.0%) | 0.16 |
| ASA, n (%) | 0.15 | ||
| I | 2 (1.4%) | 4 (1.1%) | |
| II | 26 (18.7%) | 95 (25.1%) | |
| III | 94 (67.6%) | 215 (56.9%) | |
| IV | 17 (12.2%) | 64 (16.9%) | |
| Previous abdominal surgery, n (%) | 70 (50.4%) | 176 (46.6%) | 0.44 |
| Previous abdominal wall hernia repair, n (%) | 5 (3.6%) | 10 (2.7%) | 0.57 |
| Previous abdominal wall mesh, n (%) | 1 (0.7%) | 4 (1.1%) | 0.73 |
| Year of surgery, median (IQR) | 2019 (2017–2020) | 2017 (2016–2019) | < 0.001 |
Caption comparison of ICA and ECA patients
ICA intracorporeal anastomosis, ECA extracorporeal anastomosis, IQR interquartile range, ASA american society of anesthesiologists physical status classification
Operative characteristics
There were 19 surgeons included in this study, of which seven performed ICA. Four of these seven ICA surgeons performed nearly all included right colon resections with ICA (97%) and all are fellowship trained in minimally invasive surgery. Urgent surgeries (ICA 16.5% vs. ECA 29.1%, p = 0.004) and ileocolic resections (ICA 1.4% vs. ECA 8.5%, p = 0.01) were associated with lower rates of ICA. Specimen extraction incisions were predominantly Pfannestiel incisions in ICA patients (93.5%) and midline incisions in ECA patients (93.4%). Other operative characteristics were similar across both groups (Table 2).
Table 2.
Operative characteristics
| Characteristic | ICA (n = 139) | ECA (n = 378) | p-value |
|---|---|---|---|
| Urgent surgery, n (%) | 23 (16.5%) | 110 (29.1%) | 0.004 |
| Indication for surgery, n (%) | 0.17 | ||
| Malignancy | 98 (70.5%) | 244 (64.6%) | |
| Benign neoplasm | 32 (23.0%) | 83 (22.0%) | |
| IBD | 7 (5.0%) | 37 (9.8%) | |
| Other | 2 (1.4%) | 14 (3.7%) | |
| Location of pathology, n (%) | 0.09 | ||
| Cecum | 58 (41.7%) | 149 (39.4%) | |
| Ascending colon | 39 (28.1%) | 105 (27.8%) | |
| Hepatic flexure | 15 (10.8%) | 28 (7.4%) | |
| Transverse colon | 16 (11.5%) | 27 (7.1%) | |
| Appendix | 2 (1.4%) | 14 (3.7%) | |
| Terminal ileum | 1 (0.7%) | 6 (1.6%) | |
| Not reported | 8 (5.8%) | 49 (13.0%) | |
| Surgery type, n (%) | 0.01 | ||
| Ileocolic | 2 (1.4%) | 32 (8.5%) | |
| Right hemicolectomy | 129 (92.8%) | 320 (84.7%) | |
| Extended right hemicolectomy | 8 (5.8%) | 26 (6.9%) | |
| Extraction incision, n (%) | < 0.001 | ||
| Midline | 8 (5.8%) | 353 (93.4%) | |
| Transverse | 1 (0.7%) | 18 (4.8%) | |
| Paramedian | 0 (0.0%) | 1 (0.3%) | |
| Pfannestiel | 130 (93.5%) | 6 (1.6%) | |
| Hernia at index surgery, n (%) | 14 (10.1%) | 26 (6.9%) | 0.23 |
| Suture repair of hernia, n (%) | 14 (10.1%) | 26 (6.9%) | 0.23 |
Caption comparison of ICA and ECA operative characteristics
ICA intracorporeal anastomosis, ECA extracorporeal anastomosis
Incisional hernias
At two years of follow-up, a lower proportion of ICA patients developed a hernia at the extraction incision (1.5% vs. 7.1%, p = 0.02) or at any incision (3.0% vs. 7.1%, p = 0.09). All incisional hernias in the ECA group occurred at the extraction incision, compared to 50% in the ICA group. These are reported in Table 3. Four ICA patients developed incisional hernias: one at a midline extraction incision, one at a midline incision performed for anastomotic leak, one at a Pfannestiel extraction incision, and one at a laparoscopic port incision. 26 ECA patients developed incisional hernias: 23 at a midline extraction incision, and 3 at a transverse extraction incision.
Table 3.
Post-operative outcomes
| Outcome | ICA (n = 139) | ECA (n = 378) | p-value |
|---|---|---|---|
| Superficial wound infection, n (%) | 7 (5.0%) | 26 (6.9%) | 0.45 |
| Extraction incision wound infection | 3 (2.2%) | 24 (6.4%) | 0.06 |
| Anastomotic leak, n (%) | 6 (4.3%) | 18 (4.8%) | 0.83 |
| Grade of leak based on treatment, n (%) | 0.98 | ||
| Antibiotics only | 2 (1.4%) | 7 (1.9%) | |
| Drain | 3 (2.2%) | 8 (2.1%) | |
| Reoperation | 1 (0.7%) | 4 (1.1%) | |
| Reintervention, n (%) | 6 (4.3%) | 22 (5.8%) | 0.50 |
| Reintervention type (multiple per patient), n (%) | |||
| Percutaneous procedure | 4 (2.9%) | 10 (2.6%) | 0.86 |
| Endoscopic procedure | 2 (1.4%) | 4 (1.1%) | 0.72 |
| Operative procedure | 3 (2.2%) | 11 (2.9%) | 0.64 |
| 90-day emergency department visit, n (%) | 16 (11.5%) | 40 (10.6%) | 0.76 |
| 90-day readmission to hospital, n (%) | 18 (13.0%) | 44 (11.6%) | 0.68 |
| 90-day mortality, n (%) | 2 (1.4%) | 4 (1.1%) | 0.72 |
| Extraction incision hernia, n(%)a | 2 (1.5%) | 26 (7.1%) | 0.02 |
| Clinically significant extraction incision herniaa | 1 (0.8%) | 20 (5.3%) | 0.02 |
| Incisional hernia, n (%)a | 4 (3.0%) | 26 (7.1%) | 0.09 |
| Clinically significant incisional herniaa | 2 (1.5%) | 20 (5.3%) | 0.05 |
Caption Comparison of post-operative outcomes in ICA and ECA patients
ICA intracorporeal anastomosis, ECA extracorporeal anastomosis
aPatients were censored due to relocation or death leading to loss of follow-up in 7 (5.0%) ICA and 13 (3.4%) ECA patients
Only half of incisional hernias in the ICA group were surgically repaired, both by open herniorrhaphy with mesh. In the ECA group, 77% of incisional hernias were surgically repaired: 16 with mesh, two with sutures alone, and two are still awaiting surgery. Of the 18 repaired, only one underwent a laparoscopic repair. Importantly, the proportion of patients lost to follow-up due to death or relocation were similar between both groups (ICA 5.7% vs. ECA 3.9%, p = 0.07).
On adjusted time to event analysis, ICA was associated with an 80% reduction in extraction incision hernias [adjusted hazard ratio (aHR) 0.20 (95% CI 0.05–0.82), p = 0.03]. Several sensitivity analyses were performed. When restricting to surgically repaired extraction incision hernias, ICA was associated with an 86% reduction [aHR 0.14 (95% CI 0.02–0.98), p = 0.05]. When all incisional hernias were accounted for, ICA was associated with a 60% reduction in any incisional hernia [aHR 0.40 (0.14–1.17), p = 0.09] and a 73% reduction in any surgically repaired incisional hernia [aHR 0.27 (0.06–1.14), p = 0.08].
The incidence of extraction incision hernias in the 27 patients who developed an extraction incision wound infection was significantly higher than in those without a wound infection (33.3% vs. 3.9%, p < 0.001). On adjusted analysis, extraction incision wound infection was associated with a nearly tenfold increase in extraction incision hernias [aHR 9.75 (95% CI 3.86–24.63), p < 0.001].
Operative time
Median operative time was 51 min longer in the ICA group [186 min (Interquartile Range (IQR) 159–219) vs. 135 min (IQR 107–164), p < 0.001]. On adjusted analysis, ICA was associated with increased operative time [+ 51 min (Standard Error 4.3), p < 0.001]. This association was robust when restricting to scheduled surgeries (+ 55 min) and neoplastic indications (+ 53 min). Operative time decreased moderately by year in ICA patients (Pearson Correlation Coefficient − 0.42, p < 0.001) and less-so in ECA patients (Pearson Correlation Coefficient − 0.13, p = 0.01). The difference in operative time decreased throughout the study period and was 70 min in 2015 (218 vs. 148 min), and 35 min in 2020 (172 vs. 137 min).
Length of stay
Median length of stay was one calendar day shorter in the ICA group [3 days (IQR 3–4) vs. 4 days [3–5], p = 0.007]. On adjusted analysis, ICA was associated with a 13% decrease in the length of stay {Adjusted Risk Ratio (aRR) 0.87 [95% confidence interval (95% CI) 0.78–0.97], p = 0.02}. Results were consistent when excluding deaths and transfers to other hospitals [aRR 0.89 (95% CI 0.79–0.99), p = 0.03], and in subgroup analyses restricted to scheduled surgeries [aRR 0.87 (95% CI 0.78–0.99), p = 0.02] and neoplastic indications [aRR 0.86 (95% CI 0.77–0.97), p = 0.01].
Wound infections, anastomotic leaks, and reinterventions
The incidence of superficial wound infections, anastomotic leaks, and re-interventions are presented in Table 3. These events occurred in a lower proportion of ICA compared to ECA patients, but this difference was not statistically significant. Wound infections were identified in 33 patients (6.4%) and occurred predominantly at the extraction incision in ECA patients (92.3%) but more commonly affected non-extraction incisions in ICA patients (57.1%). There were 6 ICA patients (4.3%) and 18 ECA patients (4.8%) with anastomotic leaks, and the leak severity based on the treatment required was evenly distributed between groups. Percutaneous, endoscopic, and/or operative reinterventions for post-operative complications were required in 28 patients (5.4%); these were performed for abscesses or anastomotic leaks in 17 patients (3.3%), intraperitoneal or intraluminal hemorrhage in 13 patients (2.5%), bowel obstruction in 2 patients (0.4%), and dehiscence in 2 patients (0.4%).
On adjusted analyses, anastomotic technique was not associated with these outcomes even when restricting to scheduled surgeries and neoplastic indications. Anastomotic technique was similarly not associated with anastomotic leak or reinterventions when each were expanded to a composite outcome including mortality or lost to follow-up before 90 days.
90 day outcomes
The rates of emergency department visits, post-operative readmissions, and mortality 90 days following index surgery were similar between both groups, and are presented in Table 3. On adjusted analysis, anastomotic technique was not associated with these outcomes even when restricting to scheduled surgeries and neoplastic indications. The proportion of patients censored before 90 days for loss of follow-up were not different between ICA and ECA groups (0.7% vs. 0.5%, p = 0.80).
Cancer outcomes
There were 98 ICA (70.5%) and 238 ECA (63.0%) patients with a colonic or appendiceal malignancy. Stage and oncologic quality outcomes are presented in Table 4. Nearly all these malignancies were of adenocarcinoma histology. The median number of nodes sampled, the adequacy of nodal sample, and receipt of chemotherapy were similar across both groups.
Table 4.
Oncologic outcomes in patients with intestinal malignancies
| Outcome | ICA (n = 98) | ECA (n = 238) | p-value |
|---|---|---|---|
| Intestinal malignancy, n (%) | 98/139 (70.5%) | 238/378 (63.0%) | 0.11 |
| Histologic subtype, n (%) | 0.60 | ||
| Adenocarcinoma | 95 (96.9%) | 229 (96.2%) | |
| Mixed neuroendocrine neoplasm | 2 (2.0%) | 3 (1.3%) | |
| Neuroendocrine tumor | 1 (1.0%) | 6 (2.5%) | |
| Stage, n (%) | 0.35 | ||
| I | 29 (29.6%) | 60 (25.2%) | |
| II | 28 (28.6%) | 94 (39.5%) | |
| III | 33 (33.7%) | 66 (27.7%) | |
| IV | 8 (8.2%) | 18 (7.6%) | |
| Nodes sampled, median (IQR) | 22 (16–33) | 22 (17–30) | 0.47 |
| Adequate node sample, n (%) | 96 (98.0%) | 228 (95.8%) | 0.33 |
| Chemotherapy received, n (%) | 30 (30.6%) | 69 (29.0%) | 0.94 |
Caption comparison of oncologic outcomes in ICA and ECA patients with intestinal malignancies
ICA intracorporeal anastomosis, ECA extracorporeal anastomosis, IQR interquartile range
Discussion
The study conducted is an observational study of a contemporary cohort made up of all patients who have undergone a standard laparoscopic right colectomy at a single institution and aimed to compare important post-operative outcomes across ICA and ECA techniques. There are four major findings: ICA is associated with reduced incisional hernias and shortened length of stay, has a similar safety profile to ECA, and does not compromise the oncologic specimen.
Incisional hernias following Pfannenstiel incisions are considerably less common than with midline incisions [15, 16]. Yet the use of a midline incision for ECA persists secondary to improved exposure and decreased mesenteric traction necessary for fashioning an anastomosis. In this study, nearly all ECA patients had a midline extraction incision, and a similar proportion of ICA patients had a Pfannestiel extraction incision. This study focused on incisional hernias occurring at the extraction incision, and these occurred in significantly more ECA patients (7.1% vs. 1.5%). In fact, all incisional hernias occurred at the extraction incision in ECA patients. On adjusted analysis ICA was associated with an 80% reduction in extraction incision hernias. Findings were similar when considering only surgically repaired hernias. It is understood that this study does not infer that the association between ICA and hernias is causative, not only because of the observational nature of the data, but because of implausibility. It is not the anastomotic technique that prevents the hernia, but rather the ability to complete the operation while avoiding a midline incision. It is imperative that surgeons consider this when performing a laparoscopic right colectomy with intracorporeal anastomosis, especially if the intention of doing so is to mitigate the risk of an incisional hernia post-operatively.
Interestingly, extraction incision wound infections were associated with a nearly tenfold increase in incisional hernias and occurred approximately three times more frequently in ECA patients. Midline incisions for ECA may have a predilection for wound infection compared to Pfannenstiel incisions based on their length and their proximity to where the anastomosis is fashioned, which can lead to spillage and contamination of the subcutaneous space.
On average, ICA and ECA patients were discharged following a median of 3 and 4 days, respectively. These lengths of stay are shorter than those reported by nearly all studies included in a meta-analysis published in 2019 [17]. This is likely secondary to the expanding paradigm shift in colorectal surgery with enhanced recovery programs which have been shown to shorten hospital stays [18]. ICA was associated with decreased length of stay after adjusting for several clinically meaningful characteristics. These results were stable when accounting for early mortalities, loss to follow-up, and subgroup analyses excluding urgent operations and non-neoplastic indications such as Crohn’s disease. While shorter length of stay for ICA patients has not been consistently shown in the literature, it has been demonstrated in two separate meta-analyses [17, 19] and has several important patient satisfaction, healthcare delivery, and economic implications [20, 21].
Post-operative outcomes were statistically equivalent for all short-term outcomes including wound infections, anastomotic leaks, reinterventions, and 90-day emergency department visits, readmissions, and mortality. These results were stable through adjusted analyses, sensitivity analyses and subgroup analyses. Several studies have found reduced wound infection and morbidity rates for ICA [4–6, 22], but the majority of studies to date have failed to show a differences in post-operative complications [7, 19]. In this study, the trends of wound infections, anastomotic leaks, and reinterventions favored ICA, therefore ICA was deemed at least as safe as ECA.
Node sampling and receipt of chemotherapy have long been regarded as measurable and actionable oncologic quality metrics [23]. In this study, lymph node sampling was excellent in both groups and was quantified according to absolute value (median 22) and an adequacy cut-off value of 12 (> 95%). These results were superior to most published studies examining this outcome [17, 19]. Adjuvant chemotherapy rates was similar across ICA (30.6%) and ECA patients (28.9%). To our knowledge this outcome has only been reported previously in a randomized control trial comparing transverse and midline extraction incisions by Lee et al. [24].
The one drawback found in this study for ICA was the additional operative time. However, similar to the present study, operative time for ICA has been shown to decrease with increased experience [6, 25], and two meta-analyses have found similar times for ICA and ECA [19, 26]. This discrepancy may be secondary to the perpetual learning curve at our academic institution propagated by the constant influx of new trainees learning laparoscopic common enterotomy closure with free-needle laparoscopic suturing. Additionally, others have suggested that the time spent on the intracorporeal anastomosis is offset by the time saved with less extensive ileocolic mobilization due to reduced mesenteric traction for intracorporeal anastomosis [21] and as described below, the most technically challenging resections with ECA were excluded from this analysis. In fact, the average operative time for ECA cases in this study was shorter than in most published studies [17]. Nevertheless, we propose that the additional operative time in exchange for one day of post-operative hospital stay and trainees learning an important surgical technique is a worthwhile trade-off.
As with all non-randomized studies, confounding and inherent biases to observational studies must be considered. Determining whether a conversion to laparotomy occurred by reviewing the operative report was more straightforward in ICA patient than in ECA patients. Since most right colectomies with ECA required a midline incision, surgeons could make their standard midline incision prematurely or extend it in challenging cases and complete part of the procedure through it. Whereas, nearly all midline incision in an ICA would be regarded as a conversion to laparotomy and excluded. In order to avoid a selection bias unfairly effecting the ECA cohort, both the vascular ligation and a full colon mobilization had to be completed laparoscopically in order to be considered an ECA. We recognize that many surgeons would find these criteria too restrictive and that according to this definition more ECA operations would be excluded based on surgeon technique rather than an inability to progress safely. Therefore, the ECA cohort in this study is less technically challenging and estimates favoring ICA are conservative, such that ICA may provide even greater benefits than reported.
Radiographic studies were not probed for hernias since these were not equally distributed according to indication for surgery, with a preponderance occurring in cancer patients. Instead, we depended on physical examinations described in clinical notes, and these were further classified according to surgical management versus observation. It is likely that clinically occult hernias were missed which may explain the relatively low rate of hernias in this study [15, 16]. Furthermore, only hernias described in clinic notes within our institutions were available for review. Loss of follow-up due to relocation or death and the risk of informative censoring was accounted for in every relevant association using absorbing composite outcomes and time-to-event analyses. In our institution, most surgeons with inflammatory bowel disease practices perform exclusively ECA, and this difference in case-mix is clearly depicted in Table 1, whereby ileocolic and urgent resections were more likely to undergo an ECA. Subgroup analyses excluding urgent and non-neoplastic indications for surgery were planned a priori and were consistent with the primary analyses. Certainly, this study was limited by the unavailability of specific data such as body mass index, an important covariate potentially associated with both the decision to perform an ICA and the risk of an incisional hernia.
In conclusion, laparoscopic right colectomies with intracorporeal anastomoses are associated with a reduction in incisional hernias and shorter hospital lengths of stay without compromising on patient safety or oncologic principles.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This study is not supported by any funding sources.
Declarations
Disclosures
Sydney Selznick, Jordan Levy, Ruxandra-Maria Bogdan, Jeffrey Hawel, Ahmad Elnahas, Nawar A. Alkhamesi and Christopher M. Schlachta have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sydney Selznick and Jordan Levy are considered as joint first authors.
References
- 1.Clinical Outcomes of Surgical Therapy Study Group A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 2.Colon Cancer Laparoscopic or Open Resection Study Group Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 3.Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, et al. Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg. 2010;200(2):265–269. doi: 10.1016/j.amjsurg.2009.08.044. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D. Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc. 2016;30(9):3823–3829. doi: 10.1007/s00464-015-4684-x. [DOI] [PubMed] [Google Scholar]
- 5.Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP, et al. Intracorporeal versus extracorporeal anastomosis. results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg endosc. 2015;29(8):2314–2320. doi: 10.1007/s00464-014-3950-7. [DOI] [PubMed] [Google Scholar]
- 6.Fabozzi M, Allieta R, Contul RB, Grivon M, Millo P, Lale-Murix E, et al. Comparison of short-and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24(9):2085–2091. doi: 10.1007/s00464-010-0902-8. [DOI] [PubMed] [Google Scholar]
- 7.van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc. 2017;31(1):64–77. doi: 10.1007/s00464-016-4982-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Taher M, Okamoto N, Mutter D, Stassen LPS, Marescaux J, Diana M, et al. International survey among surgeons on laparoscopic right hemicolectomy: the gap between guidelines and reality. Surg Endosc. 2022 doi: 10.1007/s00464-022-09044-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grams J, Tong W, Greenstein AJ, Salky B. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc. 2010;24(8):1886–1891. doi: 10.1007/s00464-009-0865-9. [DOI] [PubMed] [Google Scholar]
- 10.Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008;143(8):762–767. doi: 10.1001/archsurg.143.8.762. [DOI] [PubMed] [Google Scholar]
- 11.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010;147(3):339–351. doi: 10.1016/j.surg.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Reinke CE, Showalter S, Mahmoud NN, Kelz RR. Comparison of anastomotic leak rate after colorectal surgery using different databases. Dis Colon Rectum. 2013;56(5):638–644. doi: 10.1097/DCR.0b013e31827886db. [DOI] [PubMed] [Google Scholar]
- 14.McDonald JR, Renehan AG, T O’ Dwyer S, Haboubi NY. Lymph node harvest in colon and rectal cancer: current considerations. World J gastrointest surg. 2012;4(1):9. doi: 10.4240/wjgs.v4.i1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, et al. High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc. 2012;26(11):3180–3185. doi: 10.1007/s00464-012-2311-7. [DOI] [PubMed] [Google Scholar]
- 16.DeSouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H. Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc. 2011;25(4):1031–1036. doi: 10.1007/s00464-010-1309-2. [DOI] [PubMed] [Google Scholar]
- 17.Emile SH, Elfeki H, Shalaby M, Sakr A, Bassuni M, Christensen P, et al. Intracorporeal versus extracorporeal anastomosis in minimally invasive right colectomy: an updated systematic review and meta-analysis. Tech Coloproctol. 2019;23(11):1023–1035. doi: 10.1007/s10151-019-02079-7. [DOI] [PubMed] [Google Scholar]
- 18.Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study) Ann Surg. 2011;254(6):868–875. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 19.Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, et al. A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg. 2017;402(3):417–427. doi: 10.1007/s00423-016-1509-x. [DOI] [PubMed] [Google Scholar]
- 20.Thiele RH, Rea KM, Turrentine FE, Friel CM, Hassinger TE, Goudreau BJ, et al. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220(4):430–443. doi: 10.1016/j.jamcollsurg.2014.12.042. [DOI] [PubMed] [Google Scholar]
- 21.Cohen ME, Bilimoria KY, Ko CY, Richards K, Hall BL. Variability in length of stay after colorectal surgery: assessment of 182 hospitals in the national surgical quality improvement program. Ann Surg. 2009;250(6):901–907. doi: 10.1097/SLA.0b013e3181b2a948. [DOI] [PubMed] [Google Scholar]
- 22.Erguner I, Aytac E, Baca B, Hamzaoglu I, Karahasanoglu T. Total laparoscopic approach for the treatment of right colon cancer: a technical critique. Asian J Surg. 2013;36(2):58–63. doi: 10.1016/j.asjsur.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 23.West NP, Sutton KM, Ingeholm P, Hagemann-Madsen RH, Hohenberger W, Quirke P. Improving the quality of colon cancer surgery through a surgical education program. Dis Colon Rectum. 2010;53(12):1594–1603. doi: 10.1007/DCR.0b013e3181f433e3. [DOI] [PubMed] [Google Scholar]
- 24.Lee L, Mata J, Droeser RA, Kaneva P, Liberman S, Charlebois P, et al. Incisional hernia after midline versus transverse specimen extraction incision: a randomized trial in patients undergoing laparoscopic colectomy. Ann Surg. 2018;268(1):41–47. doi: 10.1097/SLA.0000000000002615. [DOI] [PubMed] [Google Scholar]
- 25.Hanna MH, Hwang GS, Phelan MJ, Bui T-L, Carmichael JC, Mills SD, et al. Laparoscopic right hemicolectomy: short- and long-term outcomes of intracorporeal versus extracorporeal anastomosis. Surg Endosc. 2016;30(9):3933–3942. doi: 10.1007/s00464-015-4704-x. [DOI] [PubMed] [Google Scholar]
- 26.Wu Q, Jin C, Hu T, Wei M, Wang Z. Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech. 2017;27(4):348–357. doi: 10.1089/lap.2016.0485. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.