Abstract
Purpose
Global studies show an increase in hospitalizations for pediatric eating disorders (EDs). No published Canadian studies have confirmed these findings in pediatric ED programs for one-year post onset of the COVID-19 pandemic. The primary objective was to examine health administrative data from two pediatric tertiary care ED programs: Alberta Children's Hospital (ACH) and Hospital for Sick Children (SickKids) to determine the number of pediatric hospitalizations with the most responsible discharge diagnosis of anorexia nervosa (AN).
Methods
This hospital-based design explored monthly pediatric hospitalizations in seven-year-olds to 18-year-olds between March 11, 2014 and March 11, 2021 using the Discharge Abstract databases. The analysis used negative binomial regression with robust standard errors to compare hospitalization counts in the months preceding and following the World Health Organization pandemic declaration (March 11, 2020).
Results
Hospitalizations due to pediatric AN increased by 63% and 132% at SickKids (p < .001) and ACH (p < .001), respectively, in the first year of the pandemic compared to the previous six years. The total number of non-ED hospitalizations decreased by 29.3% and 2.4% at SickKids and ACH, respectively.
Discussion
This is the first Canadian study to show a rise in pediatric hospitalizations over one year due to AN in two tertiary care hospitals following the onset of the pandemic, confirming the impact that the pandemic has had on children and adolescents with AN in Canada.
Keywords: Feeding and eating disorders, Anorexia nervosa, COVID-19, SARS-CoV-2, Pandemics
Implications and Contribution.
This Canadian study uses health administrative data to demonstrate an increase in pediatric hospitalizations due to AN one year from the onset of the COVID-19 pandemic compared with the previous six years. These data will inform preparedness for pediatric ED services now and for future pandemics.
See Related Editorial on p.321
Since the onset of the COVID-19 pandemic in Canada, pediatric healthcare providers have reported an increase in the number and severity of children and adolescents with eating disorders (EDs) requiring medical admissions to hospitals compared to prior years [[1], [2], [3], [4], [5], [6], [7]]. This is concerning as EDs are life-threatening mental illnesses with the highest mortality rate of any psychiatric disorder and are associated with significant physical and mental health morbidity [8].
Several pandemic-related factors may have contributed to the increase in the number of children and adolescents with EDs [9]. These factors include heightened feelings of anxiety, depression, post-traumatic symptoms, and lack of control [1,6,10,11]; disruption and restrictions to daily routines; closures of schools and recreational facilities; loss of regular connections with peers; and loss of extracurricular and social activities [4,12,13]. Furthermore, worsening EDs have been linked to social media use, exposing young people to harmful ED messages, preoccupation around body image, and heightened focus on appearance [[14], [15], [16]]. Public health measures including an increased focus on hand hygiene, social distancing, and mask wearing may have adversely impacted the psychological wellbeing of adolescents with comorbid mental illnesses such as depression, anxiety, and obsessive-compulsive disorder and common comorbidities among children and adolescents with EDs [6,9,17,18]. In addition, shifting to virtual care for a disorder that requires in-person medical evaluations, closure of outpatient healthcare facilities and ED day hospitals, long waitlists, pandemic-related screening and isolation protocols, and concern of exposure to SARS-CoV-2 may have hindered patients and families from receiving timely assessments and interventions, resulting in progression of the ED, increased emergency visits, and hospitalizations [[2], [3], [4], [5], [6], [7],11,15,[18], [19], [20], [21], [22], [23], [24]]. Finally, access to healthcare has been impacted by the economic changes and resultant financial stress for many families [1,6,25]. Together, these biopsychosocial determinants of health potentially created the perfect storm for the development or worsening of EDs in young people during the pandemic.
Global data have shown an increase in acute care visits to emergency departments and increased hospitalizations of children and adolescents with EDs compared to the years prior to the pandemic [[1], [2], [3], [4], [5], [6], [7],16,26,27]. Others speculate that the pandemic impacted the rate of relapse and severity of presentation in patients with EDs [11,16,26]. It is important to expand on findings from earlier studies during the pandemic to determine whether outcomes were sustained or whether the phenomenon was limited to the initial waves of the pandemic. To date, there have been no Canadian studies examining hospitalization rates and severity of clinical presentation in children and adolescents with AN in two geographically distinct pediatric tertiary care ED programs for one year from the onset of the COVID-19 pandemic. The primary objective of this study was to examine hospital health administrative data from two Canadian pediatric tertiary care ED programs (Alberta Children's Hospital [ACH], Calgary, Alberta and the Hospital for Sick Children [SickKids], Toronto, Ontario) to determine the number of pediatric hospitalizations, with AN as the most responsible discharge diagnosis (the diagnosis that can be described as being the most responsible for the patient's hospitalization) during the first year of the COVID-19 pandemic, compared to the number of hospitalizations in the same time period six years prior. Second, we assessed indicators of severity of illness prepandemic and postpandemic onset by looking at length of stay (LOS), complications secondary to AN and complexity of illness based on medical and/or psychiatric comorbidity.
Methods
We conducted a hospital-based study of monthly hospital discharges of children and adolescents aged 7 years to 18 years with a primary diagnosis of AN as defined by the International Classification of Disease, 10th Revision, Canada (ICD-10-CA) [28] F50 codes based on Discharge Abstract Database obtained from SickKids and ACH between March 11, 2014 and March 11, 2021. The analysis used negative binomial regression with robust standard errors to compare hospitalization counts in the months preceding and following the World Health Organization pandemic declaration (March 11, 2020).
The initial data request included all discharges with a primary diagnosis of an ED including F50.0 (anorexia nervosa [AN]), F50.1 (atypical AN), F50.2 (bulimia nervosa), F50.8 (other EDs), and F50.9 (ED, unspecified). The analysis was repeated with and without inclusion of the remaining codes (F50.1, F50.2, F50.8, and F50.9) for purposes of comparison. The final analysis was restricted to the most responsible diagnosis of AN (F50.0) since it is the most frequent code at both ACH and SickKids and we were able to reliably capture a clearly identifiable diagnosis associated with hospitalization. Furthermore, the results were unchanged with or without inclusion of the other codes as an aggregate group. Based on this, the primary outcome was a discharge diagnosis of AN.
The primary outcome was children and adolescents with a discharge diagnosis of AN. The analysis focused on monthly counts of AN hospitalizations. Both Calgary and Toronto have experienced small changes in population size but neither hospital has a fully defined catchment area. The ACH program has a more regional focus as it is the only specialized pediatric ED program in Southern Alberta. Conversely, SickKids is the only tertiary care pediatric ED program in the greater Toronto area but one of several hospitals that admit children and adolescents with EDs. An analysis of monthly hospitalization rates was conducted, using Statistics Canada population estimates for the Calgary and Toronto economic regions as denominators. The results of the two analyses were unchanged, suggesting that changes in the size of the local populations had a little impact on hospitalization trends. Therefore, the estimates presented below are those based on counts rather than rates.
The analysis initially examined the mean monthly counts of discharges, using a linear spline, with a knot placed at March 11, 2020, the date the pandemic was declared by the World Health Organization. This analysis used the “mkspline” command in Stata v16 (College Station, Texas). This analysis identified a nonsignificant slope prior to onset of the pandemic at both centers. However, the monthly slope before the pandemic onset was not significantly different from zero at each site. An examination of residuals in the period after the pandemic onset suggested nonlinearity, such that negative binomial regression models including a binary prepandemic and postpandemic indicator were fit as a means of comparing prepandemic and postpandemic hospitalization counts. A negative binomial model was selected due to evidence of overdispersion when Poisson models were fit. Fisher's exact test and t-tests were used to compare the characteristics of prepandemic and postpandemic hospitalizations and to compare characteristics of the sample at each site.
In addition to diagnostic codes, the Discharge Abstract Database provides demographic (age and gender), administrative, and clinical data. For analysis, LOS was log transformed in the analysis due to non-normality. As many ICD-10-CA codes for conditions other than EDs were present, three members of the research team (A.H., D.K., and E.V.) characterized each of the listed ICD-10-CA codes into the following categories based on clinical judgment: medical comorbidity, psychiatric comorbidity, ED complications, medically nonspecific (unclear whether medical comorbidity or medical complication), irrelevant, or psychosocial issues. Divergent opinions were discussed and reconciled. If they could not reach full consensus, one of the senior investigators (D.K.) made the final decision. All analyses were conducted using Stata 16 (College Station, Texas). Two-sided tests were used in all these comparisons. Due to differences in the two institutions studied (see above), an a priori decision was made to analyze the datasets separately, except for descriptive comparisons of the two samples.
The Research Ethics Boards at the University of Calgary and at SickKids approved this study.
Results
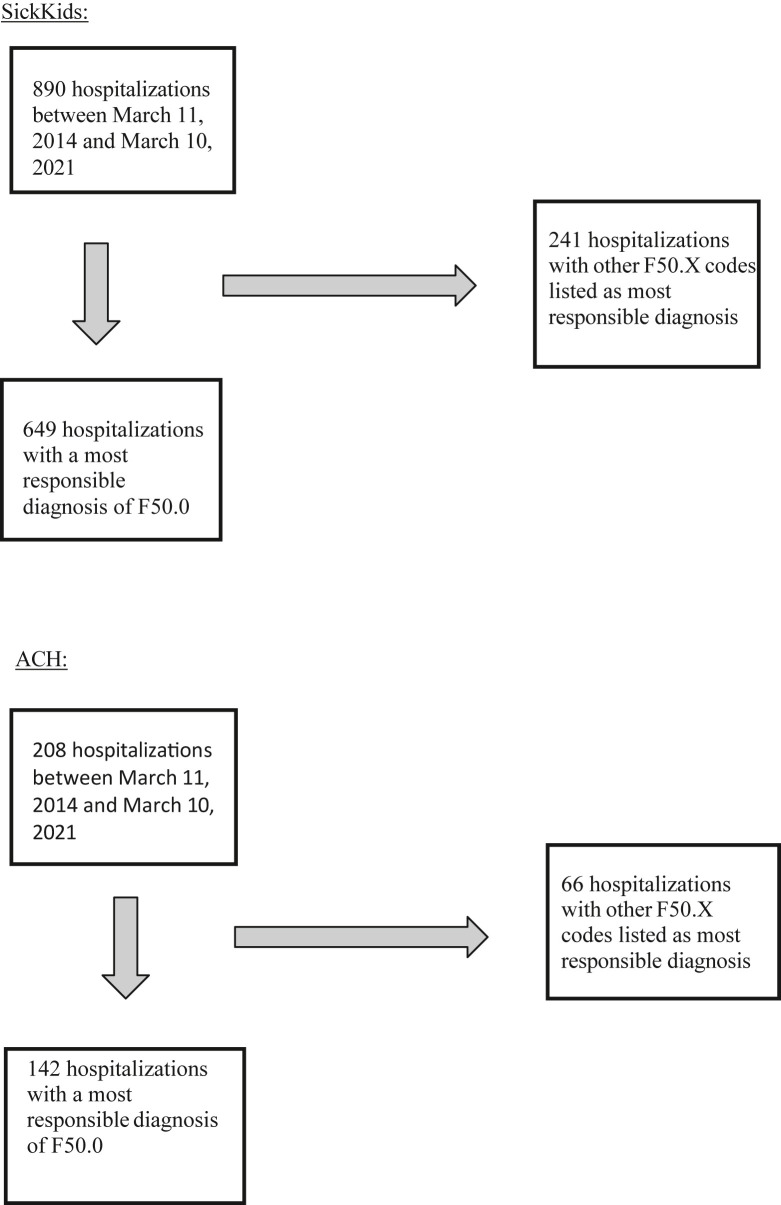
The SickKids and ACH data included 890 and 208 children and adolescents hospitalized with an F50 code from March 11, 2014 to March 11, 2021 as the most responsible diagnosis, respectively; 649 (72.9%) children and adolescents from SickKids and 142 (68.3%) from ACH had the most responsible diagnosis of AN (F50.0) (Figure 1 ).
Figure 1.
Origins of the samples at SickKids and Alberta Children's Hospital.
Table 1 presents the demographic and clinical characteristics of each sample over the seven-year study period. There were no differences in the gender, age, mean LOS, and rehospitalization rates at day 30 between the two sites. There were no deaths at either site. Both sites had notable psychiatric comorbidity and medical complications with higher rates of psychiatric comorbidity and medically nonspecific diagnoses at the ACH site.
Table 1.
Demographic and clinical characteristics of total number of children and adolescents with discharge diagnosis of anorexia nervosa at SickKids and Alberta Children's Hospital between March 11, 2014 and March 11, 2021
| SickKids (n = 649) | ACH (n = 142) | p value | |
|---|---|---|---|
| Female, n (%) | 580 (89.4) | 136 (94.4) | .08 |
| Mean age in years (SD) | 14.2 (1.78) | 14.0 (1.96) | .30∗∗ |
| Mean length of stay in days (range) | 19.6 (1–88) | 20.5 (1–139) | .77∗∗∗ |
| Readmission within 30 days, n (%) | 42 (6.5) | 13 (9.2) | .27 |
| Readmission within 6 months, n (%) | ∗ | 34 (23.9) | N.A. |
| Number of deaths, n (%) | 0 (0) | 0 (0) | N.A. |
| DAD abstracts with codes for ICD-10-CA categories | |||
| Medical Comorbidity, n (%) | 84 (12.9) | 18 (12.7) | 1.0 |
| Psychiatric Comorbidity, n (%) | 249 (38.4) | 72 (50.7) | .008 |
| Medical Complications, n (%) | 482 (74.3) | 102 (71.8) | .60 |
| Medically unspecified, n (%) | 84 (12.9) | 37 (26.1) | < .001 |
| Irrelevant, n (%) | 119 (18.3) | 27 (19.0) | .90 |
| Psychosocial, n (%) | 52 (8.0) | 19 (13.4) | .05 |
| Mean number of diagnoses per hospitalization (SD) | 4.45 (3.08) | 3.58 (2.93) | .002∗∗ |
| Mood disorders, n (%) | 63 (9.71) | 30 (21.3) | < .001 |
| Anxiety disorders, n (%) | 174 (26.8) | 48 (33.8) | .01 |
DAD = Discharge Abstract Database.
Medically unspecified = unclear whether medical comorbidity or medical complication.
Irrelevant = neither a comorbidity nor medical complication.
Psychosocial = problems related to family, interpersonal relationships, education, and social environment as per the International Statistical Classification of Diseases, 10th Revision, Canada (ICD-10-CA).
∗Not available in the SickKids data, ∗∗ two-sided t-test, ∗∗∗ two-sided t-test on log length of stay. Remainder of p values is from Fisher's exact test.
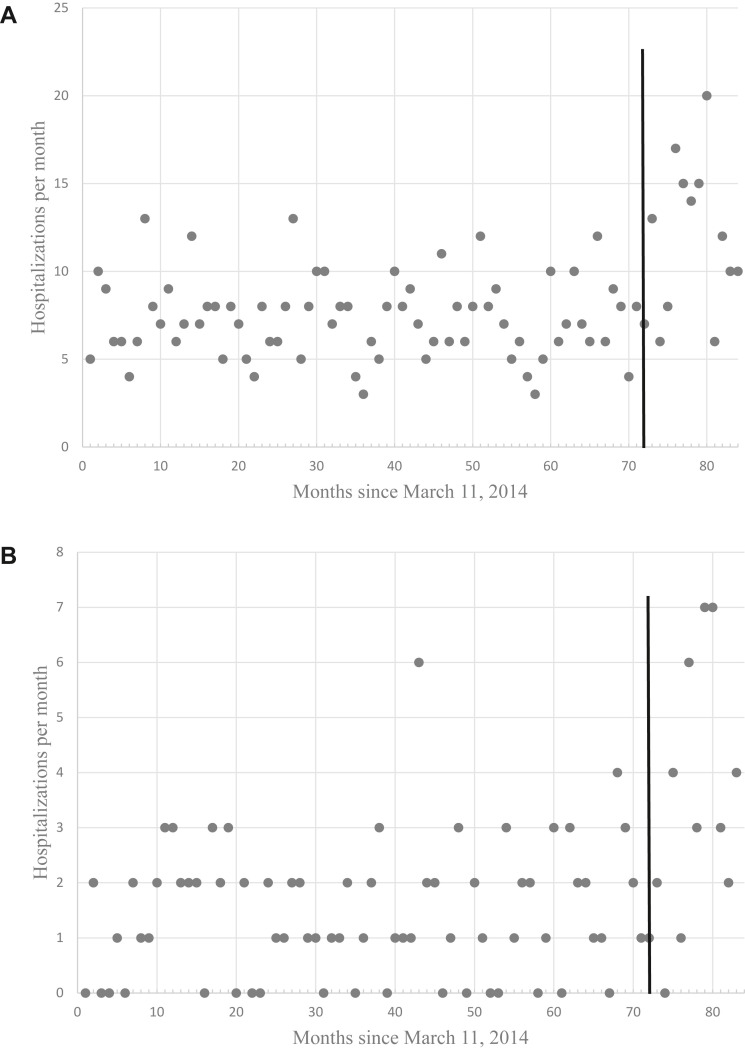
Figure 2A (SickKids) and 2B (ACH) present scatter plots of hospitalization counts per month over time. The patterns are similar, suggesting an increase in hospitalizations after the pandemic onset. However, at each site, the final three months (December 11, 2020 to March 11, 2021) had lower counts, suggesting a nonlinear pattern.
Figure 2.
(A) Hospitalization counts of patients with anorexia nervosa by month at SickKids. ∗Vertical line denotes the start of COVID-19 pandemic date of March 11, 2020. (B) Hospitalization counts of patients with anorexia nervosa by month at Alberta Children's Hospital. ∗Vertical line denotes the start of COVID-19 pandemic date of March 11, 2020.
Negative binomial regression models confirmed that the rate of hospitalization postpandemic was significantly greater than prepandemic at both sites. At SickKids, the rate ratio was 1.63 (95% confidence interval [CI] 1.31–2.03, p < .001), whereas at ACH the rate ratio was 2.32 (95% CI 1.51–3.57, p < .001), indicating a 63% and 132% increase in AN hospitalizations, respectively. However, the overlapping CIs suggest that both estimates are consistent with the same underlying population rate ratio at the 95% level of confidence.
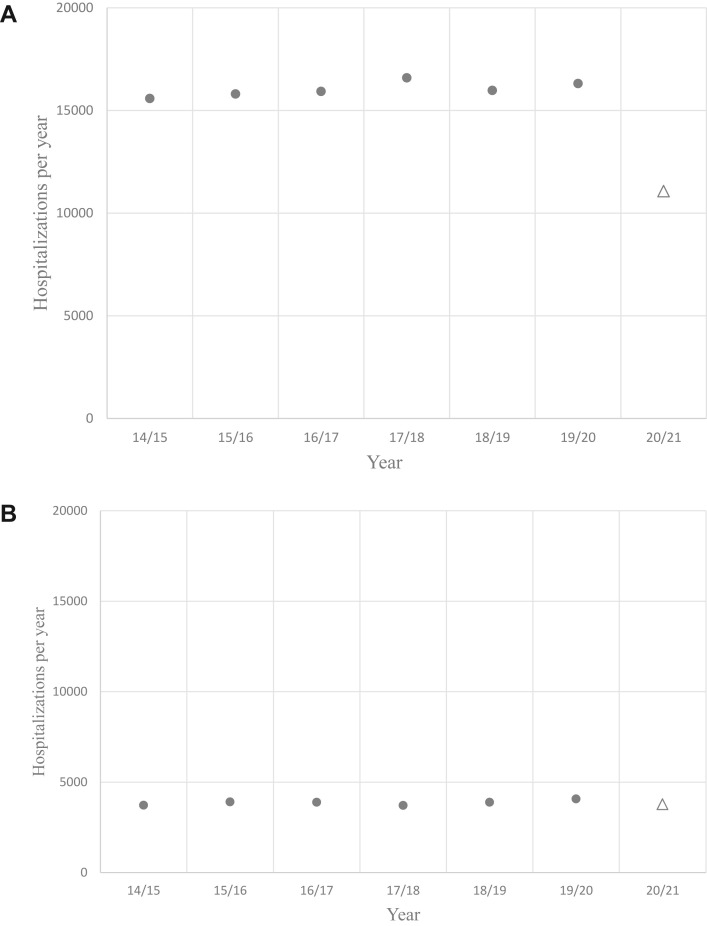
The trends in discharge counts for non-ED patients at SickKids and ACH over the same time interval are presented in Figures 3A and 3B, respectively. The total number of non-EDs hospitalizations at SickKids decreased by 29.3% in the first year of the pandemic, whereas ACH showed a similar rate (decrease of 2.4%) in the first year of the pandemic compared to the years prior.
Figure 3.
(A) Hospitalization counts of patients without an eating disorder diagnosis by year at SickKids. • Prepandemic years March 11, 2014 to March 10, 2020 Δ March 11, 2020 to March 10, 2021. (B) Hospitalization counts of patients without an eating disorder diagnosis by year at Alberta Children'’s Hospital. • Prepandemic years March 11, 2014 to March 10, 2020 Δ March 11, 2020 to March 10, 2021.
Few differences in clinical characteristics of hospitalizations before or after the pandemic declaration at either hospital emerged (Table 2 ). There was no evidence of a difference in gender at either site (SickKids: Fisher's exact test, p = 1.0; ACH: Fisher's exact test, p = .45). The mean age of hospitalization was slightly higher during the pandemic at ACH (14.5 vs. 13.8, t = −2.05, degrees of freedom (d.f.) = 140, p = .042) but not at SickKids (14.1 vs. 14.2, t = 0.5383, d.f. = 647, p = .59). The log LOS was slightly lower after the pandemic's onset at SickKids: 2.81 prepandemic and 2.54 postpandemic onset, t = 3.84, d.f. 647, p < .001 but not at ACH: 2.74 prepandemic and 2.70 postpandemic onset, t = 0.25, d.f. 140, p = .78. There were no significant differences in the count of diagnoses nor specific categories of diagnoses (i.e., medical and psychiatric comorbidity and complications) before and after the pandemic onset at ACH, whereas at SickKids the mean number of diagnoses was lower for admissions occurring after the onset of the pandemic compared to before (3.39 vs. 4.75, t = 4.75, d.f. = 647, p < .001). Due to lower frequencies of psychiatric comorbidities, medically nonspecific or psychosocial and mood disorder diagnostic codes. The proportion of 30-day rehospitalizations was higher after pandemic onset (17.9%) versus before (5.8%) at the ACH (Fisher's exact test, p = .045) but not at SickKids (6.3% before, 7.0% after; Fisher's exact test, p = .70).
Table 2.
Demographic and clinical characteristics of total number of children and adolescents with discharge diagnosis of anorexia nervosa at SickKids and Alberta Children's Hospital between March 11, 2014 and March 11, 2021, before versus after the pandemic declaration (March 11, 2020)
| SickKids (n = 649) |
p value | ACH (n = 142) |
p value | |||
|---|---|---|---|---|---|---|
| Before | After | Before | After | |||
| Female, n (%) | 453/507 (89.4) | 127/142 (89.4) | 1.0 | 96/103 (93.2) | 38/39 (97.4) | .45 |
| Mean age in years (SD) | 14.2 (1.79) | 14.1 (1.76) | .59∗∗ | 13.8 (1.92) | 14.5 (1.97) | .042∗∗ |
| Mean length of stay in days (range) | 20.4 (1–88) | 16.6 (1–69) | < .001∗∗∗ | 20.2 (1–139) | 21.4 (1–102) | .78∗∗∗ |
| Readmission within 30 days, n (%) | 32/507 (6.3) | 10/142 (7.0) | .70 | 6/103 (5.8) | 7/32 (17.9) | .045 |
| Readmission within 6 months, n (%) | ∗ | ∗ | ∗ | 22/103 (21.4) | 12/39 (30.8) | .27 |
| Number of deaths, n (%) | 0 | 0 | 0 | 0 | ||
| DAD abstracts with codes for ICD-10-CA categories | ||||||
| Medical Comorbidity, n (%) | 72/507 (14.2) | 12/142 (8.5) | .089 | 15/103 (14.6) | 3/39 (7.7) | .40 |
| Psychiatric Comorbidity, n (%) | 207/507 (40.8) | 42/142 (29.6) | .015 | 47/103 (45.6) | 25/39 (64.1) | .06 |
| Medical Complications, n (%) | 381/507 (75.1) | 101/142 (71.1) | .33 | 75/103 (72.8) | 27/39 (69.2) | .68 |
| Medically unspecified, n (%) | 69/507 (13.6) | 15/142 (10.6) | .40 | 26/103 (25.2) | 11/39 (28.2) | .83 |
| Irrelevant, n (%) | 111/507 (21.9) | 8/142 (5.6) | < .001 | 21/103 (20.4) | 6/39 (15.4) | .63 |
| Psychosocial, n (%) | 51/507 (10.1) | 1/142 (0.7) | < .001 | 13/103 (12.6) | 6/33 (15.4) | .78 |
| Mean number of diagnoses per hospitalization (SD) | 4.75 (3.2) | 3.39 (2.2) | < .001∗∗ | 3.6 (2.8) | 3.5 (3.2) | .91∗∗ |
| Mood disorders | 61/507 (12.0) | 2/142 (1.4%) | < .001 | 19/103 (18.4) | 11/39 (28.2) | .25 |
| Anxiety disorders | 140/507 (27.6) | 34/142 (23.9) | .45 | 32/103 (31.1) | 16/39 (41.0) | .32 |
DAD = Discharge Abstract Database.
Medically unspecified = unclear whether medical comorbidity or medical complication.
Irrelevant = neither a comorbidity nor medical complication.
Psychosocial = problems related to family, interpersonal relationships, education, and social environment as per the International Statistical Classification of Diseases, 10th Revision, Canada (ICD-10-CA).
∗Not available in the SickKids data, ∗∗ two-sided t-test, ∗∗∗ two-sided t-test on log length of stay. Remainder of p values is from Fisher's exact tests.
Discussion
Using administrative health data, this is the first Canadian study to examine the number of hospitalizations for children and adolescents with AN at two geographically distinct pediatric tertiary care hospitals for one year from the onset of the COVID-19 pandemic (March 11, 2020), compared with the previous six years. Although these centers did not differ with respect to gender, age, mean LOS, and rehospitalization rates at day 30 between the two sites over the seven-year study period, ACH had higher rates of psychiatric comorbidity and medically nonspecific diagnoses. This may in part be explained by the fact that ACH serves numerous rural communities where specialized pediatric ED services are not available and accessing tertiary care services may be challenging. These differences could also be related to coding variances at the two sites. Despite this, the study showed an increase in hospitalizations (63% increase at SickKids and 132% increase at ACH) for children and adolescents with AN during the first year of the COVID-19 pandemic in comparison to the previous six years. These results are consistent with reports from other pediatric centers globally. Jones et al. [26] at the Gold Coast University Hospital reported a two-fold increase in the number of adolescents requiring acute inpatient care for their ED, a near three-fold increase in symptom and illness acuity, and a 42% increase in average LOS compared to a similar period in 2019. An Australian study reported a 104% increase in the number of hospitalizations for AN during COVID-19 in comparison to the previous three years [2]. Similarly, in New Zealand, Hansen et al. [27] reported an overall increase in ED monthly hospitalizations during the initial lockdown period (March and April 2020) compared to the corresponding time in 2019. In the United States, rates of ED-related hospitalizations, LOS, number of referrals, and rehospitalizations to hospital increased significantly over the course of the pandemic [3,6]. Matthews et al. [16] reported a nine-times greater likelihood of rehospitalizations within 30 days of discharge for adolescents hospitalized for AN or atypical AN during or after the lockdown period, compared to those admitted pre-COVID. Furthermore, patients with rehospitalizations or multiple hospitalizations were 19 times more likely to have had their first hospitalization during the COVID-19 pandemic compared to patients admitted pre-COVID [16]. Likewise, Otto et al. [6] reported a 123% increase in total number of hospitalizations in the first 12 months of the pandemic in comparison to the corresponding period for the previous three years.
In Canada, a population-based study of children and adolescents with EDs in Ontario reported a 66% increase in risk for pediatric ED emergency department visits and a 37% increase in risk for subsequent hospitalizations [5]. In addition, upwards of 46% of all ED hospitalizations came from the emergency department, suggesting possible barriers in accessing outpatient care during the early stages of COVID-19 [5]. Another Canadian cross-sectional study examined the incidence of adolescents with newly diagnosed AN and atypical AN during the first wave of the COVID-19 pandemic across six pediatric hospitals in Canada between January 2015 and November 2020 [7]. The rates of newly diagnosed patients with AN or atypical AN increased from March to November 2020 by more than 60% with a corresponding three-fold increase in hospitalizations compared to prepandemic rates [7]. This study adds to the existing evidence by demonstrating a persistent increase in hospitalizations of children and adolescents with AN one year after the start of the pandemic. As such, future research is needed to document the long-term hospital trends and impact of the pandemic.
Researchers and clinicians suggest several precipitating and perpetuating factors for the rise in hospitalization in patients with AN including isolation from peers and social circles; disruptions to regular routines; online schooling and closures of recreational activities; increase in social media messages that convey strong fears of gaining weight; increased attention to food and exercise; and increased contact with family members leading to greater detection of ED symptoms and weight changes [5,7,13,16,27].
Shifts and disruptions in ED treatment during COVID-19 may further explain the rise in hospitalizations. In the United Kingdom, Ayton et al. [24] noted a significant increase in ED referrals during COVID-19 resulting in long wait times for hospitalization and decreasing ED recovery rates. In the process of waiting for care, referrals and hospitalizations may have risen as patients deteriorated to the point of needing hospitalization for medical stabilization [3]. Shifts to virtual care/telehealth and reduced in-person medical care may have impeded early detection of signs of illness and access to care to prevent the progression of weight loss and disease [7].
Similar to pediatric hospitals nationally and internationally [2,5], the non-ED hospitalizations at SickKids fell significantly during the first-year postpandemic by almost 30%. This was not the case at ACH, the sole tertiary pediatric hospital in southern Alberta, suggesting geographic variations may have impacted observed differences. During the pandemic, community hospitals redeployed staff to other overburdened hospitals or converted pediatric beds to adult care, which resulted in pediatric hospitalizations being directed to ACH; ability to transfer patients to community hospitals was not available to ACH. Simultaneously, SickKids set up processes with regional and community pediatric teams for young people with EDs to be transferred from SickKids at assessment or during hospitalization to one of these Ontario hospitals. This may partially explain the difference in non-ED hospitalizations at the two institutions and the decrease in LOS at SickKids.
Differences were found in the two centers before and after the onset of the pandemic (Table 2). The significantly shorter mean LOS at SickKids after the onset of the pandemic may in part explain the significantly decreased psychiatric comorbidity, psychosocial diagnoses, and mean number of diagnoses. It is postulated that the primary focus during this shorter LOS was on medical stabilization with less emphasis on assessment of psychiatric comorbidity and other complexity. Finally, the mean readmission rate within 30 days significantly increased at ACH after the onset of the pandemic. Administrative health data did not allow for exploration of specific clinical information limiting our ability to further explore and address this finding.
The consistent rise in hospitalizations for children and adolescents with AN observed in this study has several salient clinical implications. This study highlights the importance of adapting service delivery for children and adolescents with AN including immediate access to outpatient interdisciplinary assessments and interventions. There is an urgent need to develop public health prevention strategies for children and adolescents with EDs and targeted interventions to reduce ED acuity, decrease LOS, and improve treatment outcomes. For example, parents/caregivers play a critical role in early detection and intervention for this population and will be useful targets to intervene swiftly and effectively to support their child with emerging ED symptoms [19,29]. Thus, public health responses and clinical interventions should integrate family-based approaches to prevent hospitalizations for patients with EDs during COVID-19. The Canadian pediatric ED health system requires increased training for healthcare professionals to allow for prompt identification and treatment and improvements in the design and delivery of the current health system to meet the increased demands of the clinical burden and preparedness for future outbreaks.
This study has several important strengths. The study includes a large sample of children and adolescents with AN and a systematic collection and monitoring of two tertiary-center hospitalization trends over a large geographic area (Western and Central Canada) using comprehensive administrative data. To our knowledge, this is the first study to include collection of data for a full one-year postpandemic onset. It also included a prolonged period preceding the onset of the COVID-19 pandemic to establish a year-on-year change.
Our study has several limitations. The main limitation includes the possible lack of similar coding criteria across individuals and institutions. This limitation, although relevant, may be less important as this study has a clearly identified event (e.g., AN) associated with hospitalization. Other limitations may include data quality, coding accuracy, and methods for classifying and coding comorbidities and complications. We attempted to ascertain severity of illness using LOS, medical and psychiatric comorbidity, associated medical complications, and death. However, administrative health data did not allow for exploration of clinical variables (e.g., body weight, weight loss, heart rate); such information would have helped characterize this population further.
Finally, findings from SickKids are likely an underestimation of hospitalizations; in January 2021, patients with EDs requiring hospitalization were transferred to community or regional hospitals in Ontario if SickKids ED beds were at capacity. Conversely, non-ED hospitalizations at ACH may be an overestimation since many community pediatric beds throughout southern Alberta were converted to adult beds, resulting in a surplus of pediatric hospitalizations being directed to ACH. Nevertheless, the study adds to the robustness of the existing literature by showing a consistent pattern of increased hospitalizations over a year postpandemic in both geographical settings.
Conclusion
This study provides a detailed two-center Canadian perspective on pediatric tertiary care hospitalizations for young people with AN one year postpandemic and six years prior to the COVID-19 pandemic. While we did not explore specific drivers for increased hospitalizations, our findings are consistent with global reports indicating that the incidence of pediatric ED hospitalizations increased during the pandemic. Future research is needed to better understand the contributing factors leading to the surge in hospitalizations. Multimethod studies are necessary to capture future patterns and rates, longstanding trends in ED hospitalizations, and multiple stakeholder perspectives on the biopsychosocial factors contributing to the rapid rise in ED hospitalizations. Preparation and capacity building for pediatric ED services should be regarded as a component of pandemic preparedness for all health systems.
Disclosure
Drs. Katzman and Vyver are currently co-principal investigators and Drs. Devoe, Dimitropoulos, and Patten are co-investigators on a study of first-time hospitalizations for Anorexia Nervosa during the COVID-19 pandemic and are receiving funding from the Canadian Paediatric Surveillance Program. Dr. Katzman is an associate editor of the Journal of Adolescent Health and Editor-in-Chief of the Neinstein's Adolescent and Young Adult Healthcare, Wolters Kluwer.
Acknowledgments
We wish to acknowledge Tara A. Whitten, Ph.D., Data & Analytics, Alberta Health Services, Alberta, Canada and Ethel Lagman, Manager, Decision Support, Hospital for Sick Children, Toronto, Canada for their assistance with the Discharge Abstract Database.
Author Contributions: All authors conceptualized and designed the study; participated in the interpretation of the data; drafted the initial manuscript, reviewed, and revised the manuscript; and approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Drs. Han, Katzman, Patten, and Vyver and Ms. Marcoux-Louie participated in the acquisition of data and carried out the initial analyses.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
References
- 1.Touyz S., Lacey H., Hay P. Eating disorders in the time of COVID-19. J Eat Disord. 2020;8:19. doi: 10.1186/s40337-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haripersad Y.V., Kannegiesser-Bailey M., Morton K., et al. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child. 2021;106:e15. doi: 10.1136/archdischild-2020-319868. [DOI] [PubMed] [Google Scholar]
- 3.Lin J.A., Hartman-Munick S.M., Kells M.R., et al. The impact of the covid-19 pandemic on the number of adolescents/young adults seeking eating disorder-related care. J Adolesc Health. 2021;69:660–663. doi: 10.1016/j.jadohealth.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spettigue W., Obeid N., Erbach M., et al. The impact of COVID-19 on adolescents with eating disorders: A cohort study. J Eat Disord. 2021;9:1–8. doi: 10.1186/s40337-021-00419-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toulany A., Kurdyak P., Guttmann A., et al. Acute care visits for eating disorders among children and adolescents after the onset of the COVID-19 pandemic. J Adolesc Health. 2022;70:42–47. doi: 10.1016/j.jadohealth.2021.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otto A.K., Jary J.M., Sturza J., et al. Medical admissions among adolescents with eating disorders during the COVID-19 pandemic. Pediatrics. 2021;148 doi: 10.1542/peds.2021-052201. [DOI] [PubMed] [Google Scholar]
- 7.Agostino H., Burstein B., Moubayed D., et al. Trends in the incidence of New-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Netw Open. 2021;4:e2137395. doi: 10.1001/jamanetworkopen.2021.37395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arcelus J., Mitchell A.J., Wales J., Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 9.Rodgers R.F., Lombardo C., Cerolini S., et al. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogers A.A., Ha T., Ockey S. Adolescents' Perceived Socio-Emotional impact of COVID-19 and implications for mental health: Results from a U.S.-Based Mixed-methods study. J Adolesc Health. 2021;68:43–52. doi: 10.1016/j.jadohealth.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castellini G., Cassioli E., Rossi E., et al. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int J Eat Disord. 2020;53:1855–1862. doi: 10.1002/eat.23368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cost K.T., Crosbie J., Anagnostou E., et al. Mostly worse, occasionally better: Impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. 2022;31:671–684. doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Springall G., Cheung M., Sawyer S.M., Yeo M. Impact of the coronavirus pandemic on anorexia nervosa and atypical anorexia nervosa presentations to an Australian tertiary paediatric hospital. J Paediatr Child Health. 2022;58:491–496. doi: 10.1111/jpc.15755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodgers R.F., Slater A., Gordon C.S., et al. A biopsychosocial model of social media use and body image concerns, disordered eating, and muscle-building behaviors among adolescent girls and boys. J Youth Adolesc. 2020;49:399–409. doi: 10.1007/s10964-019-01190-0. [DOI] [PubMed] [Google Scholar]
- 15.Fernández-Aranda F., Casas M., Claes L., et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28:239–245. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthews A., Kramer R.A., Peterson C.M., Mitan L. Higher admission and rapid readmission rates among medically hospitalized youth with anorexia nervosa/atypical anorexia nervosa during COVID-19. Eat Behav. 2021;43:101573. doi: 10.1016/j.eatbeh.2021.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walsh O., McNicholas F. Assessment and management of anorexia nervosa during COVID-19. Ir J Psychol Med. 2020;37:187–191. doi: 10.1017/ipm.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis C., Ng K.C., Oh J.Y., et al. Caring for children and adolescents with eating disorders in the current COVID-19 outbreak: A Singapore perspective. J Adolesc Health. 2020;67:131–134. doi: 10.1016/j.jadohealth.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Couturier J., Pellegrini D., Miller C., et al. The COVID-19 pandemic and eating disorders in children, adolescents, and emerging adults: Virtual care recommendations from the Canadian consensus panel during COVID-19 and beyond. J Eat Disord. 2021;9:46. doi: 10.1186/s40337-021-00394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khosravi M. The challenges ahead for patients with feeding and eating disorders during the COVID-19 pandemic. J Eat Disord. 2020;8:1–43. doi: 10.1186/s40337-020-00322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gordon C.M., Katzman D.K. Lessons learned in caring for adolescents with eating disorders: A Singapore experience. J Adolesc Health. 2020;67:5–6. doi: 10.1016/j.jadohealth.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Todisco P., Donini L.M. Eating disorders and obesity (ED&O) in the COVID-19 storm. Eat Weight Disord. 2021;26:747–750. doi: 10.1007/s40519-020-00938-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weissman R.S., Bauer S., Thomas J.J. Access to evidence-based care for eating disorders during the COVID-19 crisis. It J Eat Disord. 2020;53:369–376. doi: 10.1002/eat.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayton A., Viljoen D., Ryan S., et al. Risk, demand, capacity and outcomes in adult specialist eating disorder services in South-East of England before and since COVID-19. BJPsych Bull. 2022;46:89–95. doi: 10.1192/bjb.2021.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID-19 in Canada: A one-year Update on social and economic impacts. https://www150.statcan.gc.ca/n1/pub/11-631-x/11-631-x2021001-eng.htm Available at:
- 26.Jones P.D., Gentin A., Clarke J., Arakkakunnel J. Fewer respiratory admissions in the COVID-19 era. J Paediatr Child Health. 2020;56:1997–1999. doi: 10.1111/jpc.15248. [DOI] [PubMed] [Google Scholar]
- 27.Hansen S.J., Stephan A., Menkes D.B. The impact of COVID-19 on eating disorder referrals and admissions in Waikato, New Zealand. J Eat Disord. 2021;9:105. doi: 10.1186/s40337-021-00462-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Canadian Institute for Health Information . Canadian Institute for Health Information; Ottawa, Ontario: 2018. International statistical classification of diseases and related health problems, 10th revision, Canada (ICD-10-CA) [Google Scholar]
- 29.Solmi F., Downs J.L., Nicholls D.E. COVID-19 and eating disorders in young people. Lancet Child Adolesc Health. 2021;5:316–318. doi: 10.1016/S2352-4642(21)00094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]