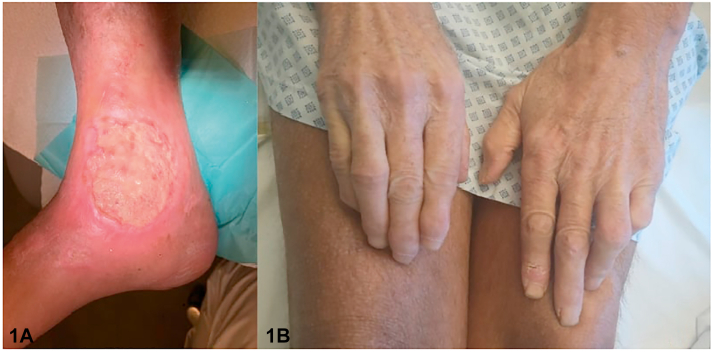
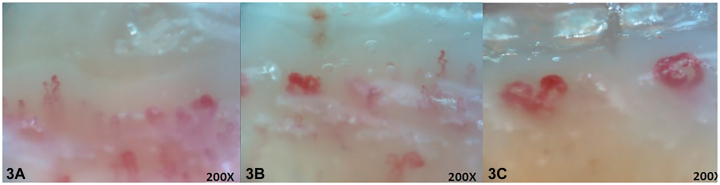
A 64-year -old patient sought medical advice for an ulcer of the lower extremities (Fig 1). He also presented with claudication, chronic dyspnea, skin thickening, and late-onset Raynaud's phenomenon (RP). There were no palpable dorsalis pedis or posterior tibial pulses. Skin examination showed reduction of forehead folds, facial and tongue telangiectasias, xerosis cutis, salt-and-pepper hyperpigmentation, sclerodactyly, digital ulcerations, and pitting scars (Fig 2). Chest auscultation revealed crackles on the lower lobes. Nailfold videocapillaroscopy showed decreased capillary density with several abnormally shaped capillaries, giant capillaries, and hemorrhages (Fig 3). Laboratory tests revealed elevated C-reactive protein levels, leukocytosis, and the presence of antinuclear antibodies (1/1280 titer). A diagnosis of systemic sclerosis (SSc) was suspected.
Fig 1.
Fig 2.
Fig 3.
Question 1: Which of the following statements is false about lower limb ulcers (LLUs) in SSc (one correct answer)?
-
A.
Complications are more likely described for LLUs in comparison with upper limb ulcers in patients with SSc
-
B.
Venous insufficiency may be part of the pathogenesis of LLU in patients with SSc
-
C.
Calcinosis can be a cause of LLU
-
D.
Necrotic angiodermatitis (NA) is a frequent cause of LLU in patients with SSc
-
E.
The prevalence of antiphospholipid antibodies is higher in patients with SSc with LLU
Answers:
-
A.
Complications are more likely described for LLUs in comparison with upper limb ulcers in patients with SSc – Incorrect. Longer wound healing time and high rate of infections and amputations are described in patients with SSc with LLU.1 Overlap of lymphatic, venous, and arterial angiopathy could be an explanation for this phenomenon.
-
B.
Venous insufficiency may be part of the pathogenesis of LLU in patients with SSc – Incorrect. Venous insufficiency may overlap with SSc-related microangiopathy and macroangiopathy. It has been reported in half of patients with SSc with LLU.1
-
C.
Calcinosis can be a cause of LLU – Incorrect. Hydroxyapatite crystals deposits in cutaneous and subcutaneous tissue can cause skin ulceration in patients with SSc. It has been observed in 10% to 25% of patients, with a similar prevalence in limited or diffuse cutaneous SSc.1
-
D.
NA is a frequent cause of LLU in patients with SSc– Correct. NA (or Martorell ulcer) is a painful ischemic ulcer of leg affecting small vessels associated with arteriolosclerosis and vasospams. It is defined by a livedoid and purpuric patch followed by a necrotic ulcer that generally affects the supramalleolar region of anterolateral aspect of the leg (our patient presented a right medial malleolus ulcer). NA is a noninflammatory condition typically associated with arterial hypertension or diabetes.2
-
E.
The prevalence of antiphospholipid antibodies is higher in patients with SSc with LLU – Correct. It is recommended to perform a prothrombotic workup, including search of antiphospholipid antibodies and mutation of methyltetrahydrofolate reductase C677 T in case of LLU in patients with SSc.3 Evaluation of antiphospholipid antibodies were negative but mutation of methyltetrahydrofolate reductase C677 T was not determined in our patient.
Question 2: Which of the following arguments are in favor of secondary RP?
-
A.
Trophic disorders
-
B.
Sparing of the thumb
-
C.
Female patient
-
D.
Normal nailfold videocapillaroscopy
-
E.
Early onset
Answers:
-
A.
Trophic disorders – Correct. Trophic disorders of the digital skin are not seen in primary RP.4
-
B.
Sparing of the thumb – Incorrect. Relative sparing of the thumb is more pronounced in primary RP.4
-
C.
Female patient – Incorrect. Primary RP is more common in female patients.4
-
D.
Normal nailfold videocapillaroscopy – Incorrect. Normal nailfold videocapillaroscopy argues for primary RP.4
-
E.
Early onset – Incorrect. Primary RP usually affects patients in their young age.4
Question 3: Regarding RP treatment, which of the following statements are true?
-
A.
Beta blockers may be used in the treatment of RP
-
B.
Calcium channel blockers constitute the first-line drug treatment of RP
-
C.
Fluoxetine could be an alternative to calcium channel blockers in cases of intolerance
-
D.
Botulinum toxin A could be used in the management of RP
-
E.
Ilopros t could be proposed as a second-line treatment after failure of calcium channel blockers
Answers:
-
A.
Beta blockers may be used in the treatment of RP – Incorrect. Beta block ers (especially nonselective beta blockers) should be avoided, as they may promote RP attacks.4
-
B.
Calcium channel blockers constitute the first-line drug treatment of RP – Correct. Calcium channel blockers are recommended if lifestyle modification alone is insufficient. These drugs influence the number and severity of RP attacks. Long-acting calcium channel blockers may be preferred in order to reduce vasodilatory adverse effects.4
-
C.
Fluoxetine could be an alternative to calcium channel blockers in cases of intolerance – Correct. Fluoxetine is a selective serotonin reuptake inhibitor commonly used in the treatment of depression. Furthermore, it also showed benefit on frequency and severity of RP attacks in comparison to nifedipine in an open-label cross-over study.4
-
D.
Botulinum toxin A could be used in the management of RP – Correct. Botulinum toxin A is a protein produced by Clostridium botulinum that inhibits acetylcholine release in the motor plate and parasympathetic system. Locally injected into the digit or the palmar skin, it may reduce severity of RP attacks.5
-
E.
Iloprost could be proposed as a second-line treatment after failure of calcium channel blockers – Correct. Iloprost is an analog of prostacyclin and may be used as a second-line treatment of RP, as it reduces the frequency and severity of the RP attacks. Iloprost is originally used in the treatment of digital ulcers in SSc.4
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Blagojevic J., Piemonte G., Benelli L., et al. Assessment, definition, and classification of lower limb ulcers in systemic sclerosis: a challenge for the rheumatologist. J Rheumatol. 2016;43(3):592–598. doi: 10.3899/jrheum.150035. [DOI] [PubMed] [Google Scholar]
- 2.Hafner J., Nobbe S., Partsch H., et al. Martorell hypertensive ischemic leg ulcer: a model of ischemic subcutaneous arteriolosclerosis. Arch Dermatol. 2010;146(9):961–968. doi: 10.1001/archdermatol.2010.224. [DOI] [PubMed] [Google Scholar]
- 3.Shanmugam V.K., Price P., Attinger C.E., Steen V.D. Lower extremity ulcers in systemic sclerosis: features and response to therapy. Int J Rheumatol. 2010;2010 doi: 10.1155/2010/747946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belch J., Carlizza A., Carpentier P.H., et al. ESVM guidelines - the diagnosis and management of Raynaud's phenomenon. Vasa. 2017;46(6):413–423. doi: 10.1024/0301-1526/a000661. [DOI] [PubMed] [Google Scholar]
- 5.Jerjen R., Nikpour M., Krieg T., Denton C.P., Saracino A.M. Systemic sclerosis in adults. Part II: Management and therapeutics. J Am Acad Dermatol. 2022 doi: 10.1016/j.jaad.2021.10.066. S0190-9622(22)00191-8. [DOI] [PubMed] [Google Scholar]