Abstract
The availability of voluntary nonremunerated blood donors is a major concern in low- and middle-income countries because there is a substantial scarcity of safe blood supply against the expected demand. This study explores the status of knowledge, attitude, and practice regarding blood donation among students and teachers of residential religious academic institutions in Jamalpur district in Bangladesh. Religious institutions were selected through simple random sampling, and the cross-sectional survey included 512 participants. Descriptive and inferential statistics were performed with statistical significance defined as p < 0.05. Over 90% of the participants were students, non-smokers, and aged 18–30 years. The majority (92%) did not ever donate blood to anyone, yet over 42% wanted to be regular donors. More than 80% considered blood donation a moral responsibility and an Islamic act. The common reasons for not donating blood were lack of knowledge (40%), lack of opportunity (20%), thinking it was harmful to health (21%), fearing needles (16%), and no financial benefit (6%). Interestingly, more than 67% did not know their blood group, and about 61% of the respondents said they did not hear of or could not remember any blood donation program. The participants had poor knowledge of general eligibility criteria but an overall positive attitude towards blood donation. There was a weak positive correlation between knowledge, attitude, and practice scores. Participants willing to donate blood to strangers were four times more likely to do so regularly. Those who considered blood donation a religious act and a moral responsibility were twice as likely to become regular blood donors. This study reveals that many potential donors are being neglected, although they may be a valuable resource in addressing the ongoing blood donation issue.
Keywords: Voluntary nonremunerated blood donors, Blood donation, Blood, Bangladesh, Religious motivation, Religious institute, Transfusion, Community
Voluntary nonremunerated blood donors; Blood donation; Blood; Bangladesh; Religious motivation; Religious institute; Transfusion; Community.
1. Introduction
Blood is a crucial healthcare resource linked to saving patients' lives with accidents, surgeries, bleeding disorders, pregnancy-related complications, inherited/acquired hematological diseases, and malignancies. Globally, about 118.5 million blood units are collected annually, yet the demand exceeds the existing capacity [1]. Since blood cannot be stored for an indefinite amount of time, a constant source of blood donation is required. According to the WHO, the sustainable approach toward ensuring prompt and effective access to the sources of safe blood and blood products is to develop a nationwide organized blood transfusion program focused on voluntary nonremunerated blood donors (VNRBD) [2]. Recruiting voluntary blood donors remains one of the significant challenges for any blood transfusion service. Out of 193 WHO Member States, only 62 countries (32%) reported receiving more than 99% of their blood supply through VNRBD [1].
In general, blood banks face multifaceted challenges in resource-limited conditions like rural areas of Bangladesh. Blood storage is a big concern due to the unavailability of continuous electricity supply in many parts of Bangladesh and other parts of the world. Improper storage can deteriorate the quality of stored blood, leading to wastage. Besides, blood from voluntary donors is challenging to obtain on short notice because of poor networking, the absence of databases of potential donors, and transportation. Professional donors often take this opportunity to sell blood to earn money. These blood sources can be of poor quality due to blood being frequently sold (often having less than four months intervals) or posing a risk of transmissible infections such as HIV, hepatitis, syphilis, and malaria [3]. The blood screening program in Bangladesh showed that as high as 47% of the blood collected in 2000 was from professional blood donors. They were found to contain transfusion-transmitted infections (TTI). The paid donors had a high prevalence of infectious markers such as HBsAg, VDRL, Anti-HCV, and Anti-HIV [4]. Our previous study found that over 28% of transfusion-dependent thalassemia patients had been infected with the hepatitis C (HCV) virus [5].
In Bangladesh, a major crisis exists regarding safe blood sources for transfusion because it is one of the most vulnerable countries in the world in terms of beta-thalassemia patients. The prevalence of beta-thalassemia carriers could be about 10% of the total population, corresponding to 16 million carriers in Bangladesh. One study estimated that 60,000–70,000 patients suffer from thalassemia; about 67% are dependent on blood, and 41% require blood transfusion every 2–4 weeks for survival [5]. However, against an expected demand of 800,000 blood units in 2016, about 600,000 were collected, of which only 31% came from voluntary donors [6]. This figure is abysmal compared to other countries in South-East Asia, such as Thailand, India, and Sri Lanka [6]. In addition, only half of the district health facilities in Bangladesh keep a stock of blood for later use; almost 41% of them are facing a supply shortage [6]. This suggests a general gap between demand for blood and supply.
It is noteworthy that the supply of blood has been hampered due to the COVID-19 crisis [7]. With prolonged lockdown and burdened healthcare, Bangladesh faced an insurmountable challenge to ensure a safe blood supply to critical patients within its existing framework. Moreover, research surrounding the motivational factors and barriers affecting blood donations in developing countries is scarce. In Bangladesh, most existing blood donation drives heavily rely on various occasions to collect blood from donors. A significant portion of this blood becomes unusable due to inadequate networking to reach the appropriate recipients. A recent review of what motivates people to donate showed that the convenience of a collection site was the key factor among first-time and repeat donors [8]. Studies show that college-level students, if encouraged and recruited, can be a valuable source of voluntary blood donation with timely access [9, 10, 11].
Due to the convenience and availability of a pool of students and teachers eligible for blood donation, religious residential academic (RRA) institutions or Madrasahs could be a potential source of blood donors. In Bangladesh, blood donation campaigns are usually held at conventional educational institutions. In contrast, a large body of religious institutions outside of these campaign targets. The role of religious motivation could become a key determinant in Bangladeshi communities since religion presumably plays an extensive influence in people's lives [12, 13]. Religious motivation as a charity was found to be effective in Iran, Brazil, and other western countries for donating blood [14, 15, 16]. Therefore, in this study, we aimed to fill the colossal gap in the literature by investigating the knowledge, attitude, and practice (KAP) of residential students and teachers of RRA institutions regarding blood donation. This may lead to safe, quick, and voluntary blood donation across the country.
2. Materials and methods
2.1. Study setting and participants
A cross-sectional study was conducted from June 2018 to December 2018 using a structured questionnaire on the students and teachers in two upazillas (Jamalpur Sadar and Melandha) of Jamalpur district in the Mymensingh division. Jamalpur is located 140 km northwest of Dhaka and has a population of 2.3 million, according to the 2011 census. Regarding demographic and socio-economic factors, our study setting (Jamalpur district) is representative of 33 other districts in Bangladesh [17]. The survey was conducted among conservative religious students and teachers in Madrasahs (known as Qawmi Madrasah in the Indian subcontinent). These institutions are not state-funded but are primarily supported by private donations. In contrast to mainstream education, Qawmi Madrasah education in Bangladesh includes a specialized curriculum that is highly focused on theology and rigorous religious studies centered on the Arabic language.
2.2. Sampling
A random sampling method was used to select institutions from two sub-districts (upazilla) of Jamalpur, followed by convenience sampling to enroll the interested participants. The inclusion criteria for participants were males aged 16–65 years living at religious academic residential campuses. There are 47 private residential religious institutions available in the Jamalpur Sadar and 46 such institutions in Melandha. A total of 10 religious institutes from Jamalpur Sadar and Melandha were selected using a simple random sampling method. A team of trained data enumerators administered the questionnaire after obtaining written approval from the respective college authority. On the day of the survey, an announcement was made on the campus about the study. Those interested in the survey gathered in a hall room to fill out the study questionnaire. A total of 659 respondents were surveyed in the study, of which 147 samples were carefully discarded due to incompleteness and inconsistent response, leaving 512 responses for the final analysis.
2.3. Study instrument
The study questionnaire was developed after reviewing published studies and consultation with experts, including physicians, public health researchers, and a statistician [18, 19, 20]. The questionnaire was written in the Bengali language. The 22-questions printed version of the questionnaire contained two pages. Page one consisted of demographic questions and blood donation practices. Page two assessed the participants' general knowledge about eligibility criteria and attitudes, including views on moral responsibility, religious viewpoints, and blood donation as a charity. The correct answers to general knowledge questions regarding eligibility criteria for blood donation were determined based on the World Health Organization (WHO) guidelines and the standard practice in Bangladesh [21]. However, participants' attitudes towards blood donation were assessed using a 5-points Likert scale (strongly agreed, agreed, don't know, disagreed, and strongly disagreed).
2.4. Statistical analysis
Data were entered manually and managed using REDCap electronic data capture tool hosted at BRF. Data were analyzed using SPSS Software Version 25 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to measure central tendency and dispersion (mean, median, and range) and to obtain frequencies and percentages for categorical variables. The correct answers to knowledge-based questions, positive answers to attitude-based questions, and responses in favour of good practice were converted into binary scores. The missing values were excluded listwise. Spearman's rank-order correlation analysis was performed among knowledge, attitude, and practice scores. The multiple logistic regression analysis identified factors influencing the positive outcome for the participants becoming regular blood donors. There were six variables in the model consisting of two knowledge-based factors: aware of the blood donation program, knowledge of blood donation interval; four attitude-based factors: interest in donating blood, willingness to donate to an unknown person, considering blood donation as a religious act, and considering blood donation as a moral responsibility. A P-value of <0.05 was considered statistically significant.
2.5. Ethical consideration
The study protocol was reviewed and approved by the institutional review board of the Biomedical Research Foundation, Bangladesh (Ref. no: BRF/ERB/2018/004). Trained enumerators first approached and explained the study purpose and nature to the prospective participants, and the study questionnaire was shared or discussed with them. Informed written consent was obtained from all the participants, and confidentiality was maintained during and after the data collection.
3. Results
Most respondents (91%) were students, while roughly 9% were teachers. More than 90% of those who participated in the study were between 18 and 30, with just a tiny number over 30. Smoking was not common among the participants since more than 97% identified themselves as non-smokers. The self-reported mean duration of formal education was 11.3 years (SD of 3.7). Despite the educational exposure, about 76% of the respondents did not know the names of common blood groups, and 67% did not know their blood group (Table 1).
Table 1.
Demographic characteristics of the participants.
| Variables | n (%) |
|---|---|
| Type of respondent | |
| Students | 467 (91.2%) |
| Teachers | 45 (8.8%) |
| Age | |
| <18 | 27 (5.3%) |
| 18–30 | 473 (92.4%) |
| 31–40 | 10 (2.0%) |
| >40 | 2 (0.4%) |
| Education Level (Academic years) | |
| Primary (<5) | 26 (5.1%) |
| Metric (6–10) | 184 (35.9%) |
| Intermediate (11–12) | 126 (24.6%) |
| Undergraduate (13–16) | 137 (26.8%) |
| Graduate >16 | 39 (7.6%) |
| Mean (SD) | 11.34 (3.66) |
| Median (IQR) | 12 (4) |
| Smoker | |
| Yes | 12 (2.3%) |
| No | 500 (97.7%) |
| Knowledge about common blood groups | |
| Yes | 125 (24.4%) |
| No | 387 (75.6%) |
| Knowledge of own blood group | |
| Yes | 169 (33%) |
| No | 343 (67%) |
About 92% of the respondents said they never donated blood to anyone. Of the 8% of participants who donated blood, everyone was above 18 years of age. While 27% of the respondents reported that their relatives took blood from someone else, the rest said that either the relatives did not need a blood transfusion (33.5%) or were unaware of it (39.6%). This is consistent with 61.1% who said they did not hear about any blood donation program. Furthermore, only 11% responded that they were encouraged by organizations working on blood donation programs. Only 22% of respondents reported that individuals approached them to donate blood (Table 2).
Table 2.
Distribution of responses of participants regarding blood donation practice.
| Variables | n (%) |
|---|---|
| Have you ever donated blood? | |
| Yes | 41 (8.0%) |
| No | 471 (92.0%) |
| Have you heard of blood donation program? | |
| Yes | 199 (38.9%) |
| No | 313 (61.1%) |
| Did any organization encourage you to donate blood? | |
| Yes | 61 (11.9%) |
| No/Don't remember | 451 (88.1%) |
| Did anybody other than an organization encourage you to donate blood? | |
| Yes | 112 (21.9%) |
| No/Don't remember | 400 (78.1%) |
| Did any of your relatives ever receive blood from others? | |
| Yes | 176 (26.8%) |
| No | 220 (33.5%) |
| Don't know | 260 (39.6%) |
Those who did not donate blood reported diverse types of reasons. About 42% of the respondents said they did not know much about blood donation, and 20% claimed they wanted to donate but did not have the chance. Moreover, 42% of the respondents said they had not considered donating blood. As many as 21.3% refrained from donating, assuming it might harm health. More than 16% were scared of needles, with about 12% mentioning health reasons, 5.5% citing no financial benefit, and 5.5% mentioning other reasons (Figure 1).
Figure 1.
Common reasons for not donating blood among the participants. The total adds up to over 100% since multiple answers were possible, and many participants chose multiple reasons for not donating blood.
Despite some fears, overall, the study participants reported a positive attitude. The participants' responses are as follows: blood donation can save a life (89%), blood donation is a charitable act (57%; 34% remained neutral), blood donation was moral responsibility (83%; 12% stayed neutral), and blood donation was an Islamic act (82%; 15% remained neutral) (Table 3).
Table 3.
Distribution of responses of participants regarding attitude towards blood donation.
| Variables | Strongly Agree n (%) | Agree n (%) | Combined Agree n (%) |
Neutral n (%) | Disagree n (%) | Strongly disagree n (%) | Combined disagree n (%) |
|---|---|---|---|---|---|---|---|
| Opinion | |||||||
| Blood donation can save a life | 294 (57.4) | 165 (32.2) | 459 (89.6) | 32 (6.3) | 8 (1.6) | 13 (2.5) | 21 (4.1) |
| Donating blood is bad for the health | 44 (8.6) | 45 (8.8) | 89 (17.4) | 152 (29.7) | 136 (26.6) | 135 (26.4) | 271 (53.0) |
| Intention towards donation | |||||||
| Want to donate to the unknown person | 217 (42.4) | 196 (38.3) | 413 (80.7) | 40 (7.8) | 31 (6.1) | 28 (5.5) | 59 (11.6) |
| Want to be a regular donor | 109 (21.3) | 106 (20.7) | 215 (42.0) | 110 (21.5) | 111 (21.7) | 76 (14.8) | 187 (36.5) |
| Moral and religious motivation | |||||||
| Donating blood is a moral responsibility | 238 (46.5) | 191 (37.3) | 429 (83.8) | 63 (12.3) | 11 (2.1) | 9 (1.8) | 20 (3.9) |
| Blood donation is an Islamic act | 247 (48.2) | 175 (34.2) | 422 (82.4) | 79 (15.4) | 9 (1.8) | 2 (0.4) | 11 (2.2) |
| Blood donation is charitable or sadaka | 189 (36.9) | 104 (20.3) | 293 (57.2) | 177 (34.6) | 33 (6.4) | 9 (1.8) | 42 (8.2) |
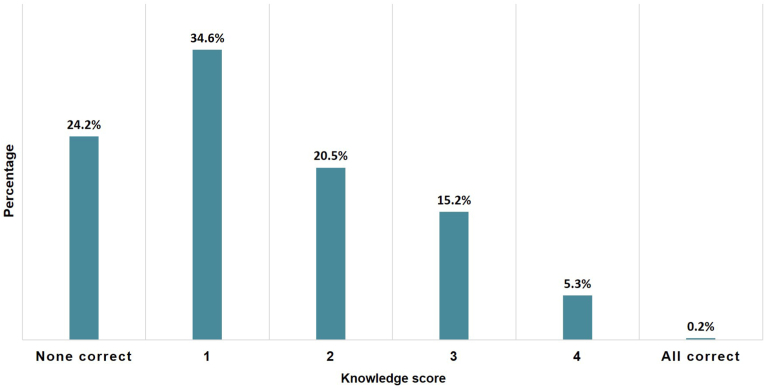
Despite the widespread positive attitude about blood donation, 17% believed blood donation could be harmful (29% remained neutral to this question). Although there was some hesitation regarding blood donation, 80% would be happy to donate blood to unknown persons. The most important highlight of the study was that 42% of respondents wanted to be regular blood donors. Only 0.2% of participants correctly answered the five-item general knowledge questions. More than 25% could not provide any correct response, and 34.6% provided only one right answer (Figure 2). Overall, the knowledge regarding blood donation was poor; only 8%, 11%, 16%, and 39% correctly identified the minimum interval required between subsequent donations (4 months), amount of blood to be taken each time (450mL), minimum weight (to be 50 kg), and minimum age (18 years), respectively. Interestingly, 66% correctly identified that blood transfusion could be a means for spreading germs from person to person (Table 4).
Figure 2.
Frequency distribution of the respondents based on the knowledge scores regarding five-item general knowledge questions.
Table 4.
Participants’ general knowledge of eligibility criteria for blood donation.
| Variables | Correct n (%) | Incorrect n (%) | Don't know n (%) |
|---|---|---|---|
| Duration of blood donation (Correct: 4 months) | 45 (8.8) | 192 (37.5) | 275 (53.7) |
| Minimum age for blood donation (Correct: 18 years) | 204 (39.8) | 33 (6.5) | 275 (53.7) |
| Minimum weight for blood donation (Correct: 50 kg) | 85 (16.6) | 79 (15.4) | 348 (68.0) |
| Every time how much blood taken (Correct: 450 ml) | 60 (11.7) | 69 (13.5) | 383 (74.8) |
| Germs can be spread through infected blood (Correct: yes) | 340 (66.4) | 26 (5.1) | 146 (28.5) |
The relationship among knowledge, attitude, and practice scores was determined using Spearman rank correlation, as shown in Table 5. Knowledge was related to attitude (rs = 0.186, P < 0.01) and practice (rs = 0.317, P < 0.01). Attitude was weakly positively related to practice (rs = 0.150, P < 0.01).
Table 5.
Correlation between knowledge, attitude, and practice scores.
| Variable | Spearman's ρ | P-value |
|---|---|---|
| Knowledge-Attitude | 0.18 | <0.01 |
| Knowledge-Practice | 0.31 | <0.01 |
| Attitude-Practice | 0.15 | <0.01 |
Logistic regression analysis found six significant factors likely influencing the participants to become regular blood donors. The model was overall statistically significant with P-value<0.01. Participants who were aware (AOR: 1.68; CI:1.13–2.48) and interested (AOR: 1.99; CI:1.27–3.12) about blood donation and those who knew blood donation interval (AOR: 2.75; CI: 1.37–5.52) were more likely to become regular blood donors. The participants willing to donate to unknown persons were four times more likely to donate blood regularly. The odds of becoming a regular blood donor were twice as higher for those who considered blood donation a religious act and a moral responsibility. The results of the regression analysis are shown in Table 6.
Table 6.
Significant factors associated with becoming a regular blood donor.
| Variables | P-value | AOR | AOR 95% CI |
|
|---|---|---|---|---|
| Lower | Upper | |||
| Aware of blood donation | 0.009 | 1.68 | 1.13 | 2.48 |
| Interested in blood donation | 0.001 | 1.99 | 1.27 | 3.12 |
| Knowledge of blood donation interval | 0.004 | 2.75 | 1.37 | 5.52 |
| Willingness to donate to an unknown person | 0.001 | 4.26 | 2.26 | 8.02 |
| Considering blood donation as a religious act | 0.001 | 2.78 | 1.48 | 5.23 |
| Considering blood donation as a moral responsibility | 0.002 | 2.85 | 1.45 | 5.59 |
4. Discussion
This study explores the status of knowledge, attitude, and practice of students and teachers of residential religious academic (RRA) institutions in Bangladesh towards blood donation. To the best of our knowledge, this study is the first of its kind in Bangladesh that involves RRA institutions to address the currently underutilized resources to mitigate the blood donation crisis.
In our study, an overwhelming majority (∼92%) of the participants did not ever donate blood, yet 42% expressed intentions to become regular blood donors. This number is less than what was observed in another survey conducted among university students in Bangladesh, which found about 74% of students showed a positive attitude toward blood donation [22]. Similarly, a high level of positive attitude toward blood donations was reported from other countries, including Tanzania (93%) and Ethiopia (∼95%) [9, 23]. This poor intention among religious students in Bangladesh indicates that blood donation drives targeting students at religious residential academic institutions were insufficient. Our study revealed that the students and the teachers of the RRA institution were hardly approached (12%) for blood donation by any organization. This demonstrates a systematic failure of blood donation campaigns that left out a large segment of the population who could donate blood. These religious academic institutions in upazillas, villages and local communities could offer a viable alternative source of voluntary blood donors.
In Bangladesh, nearly 18% of male adolescents and adults (over 15 years of age) smoke [24]. Since the study participants were males, mostly young and non-smokers, they provided an extra advantage in terms of safety in blood donation. In contrast, women are at higher risk of developing post-blood-donation adversities, and smokers risk heavy metal concentration (e.g., nickel, lead) in their blood [25, 26]. One study found that concentrations of cadmium, lead, and nickel in the blood of smokers and non-smokers were significantly correlated [26]. Another research observed a high concentration of carbon monoxide (CO) in donated blood from smokers [27].
The prime reason for students of RRA institutions in our study not donating blood was the lack of knowledge about and opportunity for blood donation. This finding is in line with another study conducted among university students in Tanzania, where 36% of the participants did not donate blood due to poor knowledge [9]. Conversely, studies conducted in India and Nigeria showed the primary reason for the hesitation in blood donation was the fear of pain [18, 28]. Interestingly, the Nigerian study also reported that many donated with the hope of obtaining future hospital benefits such as antenatal registration and saving relatives' lives [28]. An assessment of knowledge regarding blood donation among university students in the USA found a strong association between knowledge and intention of blood donation [29]. It also demonstrated that with the increase in knowledge, the blood donation intention also increases for current blood donors [29]. However, the absence of basic knowledge regarding blood donation was apparent among Bangladeshi Madrasah students. The mean number of years of education was 11.4 years, close to the national standard of 12 years of combined primary and secondary education [30]. Notably, the absence of knowledge about the common blood types implies that the Qawmi Madrasah education syllabus lacks the necessary information. In our study, a lack of awareness led a sizable proportion of participants (21%) to conclude that blood donation was potentially harmful. This suggests that Madrasah students were not exposed to proper knowledge about blood donation. However, the correlation analysis showed a weakly positive relationship between knowledge and practice. It is, therefore, essential to use this study as a reference and conduct more comprehensive research regarding the association of knowledge with blood donation practice. This study also highlighted that nearly twice the number of students (22%) were approached by individuals other than organizations (12%) for blood donation. This finding might indicate a local demand; however, a lack of information regarding blood groups, the blood donation process, safety, and health benefits had likely prevented the young students from donating blood. Introduction to the blood donation process and its benefits both for personal health and social welfare can thus remove the common knowledge gap and increase the number of potential donors in a community.
The association between religious motivation and blood donation has been documented by various studies around the world [16, 31, 32]. One study in Brazil found that religiosity was more common among regular donors than those who donated only once [14]. Religious motivation toward blood donation among Madrasah students was also evident in our study. Participants who considered blood donation a form of religious act or moral responsibility were more likely to become regular blood donors. This is unsurprising given that RRA institutions are mainly run by private donations and have been involved in providing charitable and social works for centuries [12].
Furthermore, as a country with high religiosity, the everyday life of many Bangladeshis and the cultural and social dynamics are directly impacted by religious norms [12]. Since charity remains at the heart of Muslim tradition, it is critical to highlight other forms of charitable and humanitarian works, such as blood donation, to the concern of religious leaders [13]. Teachers of RRA institutions are highly respected in the community. They are also often Imams who lead the prayers. They could be a great resource to motivate and mobilize students to donate blood.
Our study has a few limitations and strengths. First, due to the cross-sectional nature of the work, attitudes and practices could not be determined over a long period. Second, each question was given the same weight while generating a knowledge score. Third, we invited all eligible students and teachers to gather in a hall during the survey. Because only interested students appeared to participate in the poll, we could not ascertain the percentage of students who were not interested.
Furthermore, response rates among participants from different study institutes were not the same. All of these factors can introduce bias. Fourth, our study findings are not generalizable to the entire country since respondents were only from two sub-districts. Given the lack of literature, we believe that our study would contribute to defining health policies and assisting future studies with more rigorous approaches.
5. Conclusion
This study highlights an overlooked segment of the community that would otherwise be an excellent resource for voluntary blood donors. We found that the blood group was unknown to most of the students and teachers of religious institutions at the community level. Still, we found them highly motivated to donate blood as charity. Building community-based models considering the young students from religious residential academic institutions would be instrumental in taking advantage of this underutilized resource and ensuring a regular supply of voluntary donors. Blood donation practice within a local community is also expected to bring meaningful societal cohesion and strengthen communal bonding.
Declarations
Author contribution statement
Mohammad Sorowar Hossain: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Md. Hasanul Banna Siam, Mohammad Nayeem Hasan, Rifat Jahan: Analyzed and interpreted the data; Wrote the paper.
Mahbubul H Siddiqee: Conceived and designed the experiments; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to convey their immense gratitude to Dr. Enayetur Raheem for his technical suggestions for data validation and cleaning. We also would like to thank all participating religious schools, participants, and data collectors.
References
- 1.WHO Blood safety and availability, (n.d) https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability (accessed April 16, 2021)
- 2.Global Status Report on Blood Safety and Availability. 2016. https://apps.who.int/iris/bitstream/handle/10665/254987/9789241565431-eng.pdf;jsessionid=141CF566791CA5DA25317FC1083C9F98?sequence=1 (accessed April 16, 2021) [Google Scholar]
- 3.WHO Voluntary Non-remunerated Blood Donation. 2011. https://www.who.int/bloodsafety/voluntary_donation/en/ (accessed April 17, 2021) [Google Scholar]
- 4.Islam M.B. Blood transfusion services in Bangladesh. Asian J. Transfus. Sci. 2009;3:108–110. doi: 10.4103/0973-6247.53880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hossain M.S., Raheem E., Sultana T.A., Ferdous S., Nahar N., Islam S., Arifuzzaman M., Razzaque M.A., Alam R., Aziz S., Khatun H., Rahim A., Morshed M. Thalassemias in South Asia: clinical lessons learnt from Bangladesh. Orphanet J. Rare Dis. 2017;12:93. doi: 10.1186/s13023-017-0643-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO Bangladesh Is Still to Meet the Demand of Safe Blood Supply. 2017. https://www.who.int/bangladesh/news/detail/14-06-2017-bangladesh-is-still-to-meet-the-demand-of-safe-blood-supply (accessed April 16, 2021) [Google Scholar]
- 7.Hossain M.S., Raheem E., Siddiqee M.H. The forgotten people with thalassemia in the time of COVID-19: South Asian perspective. Orphanet J. Rare Dis. 2020;15:265. doi: 10.1186/s13023-020-01543-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bednall T.C., Bove L.L. Donating blood: a meta-analytic review of self-reported motivators and deterrents. Transfus. Med. Rev. 2011;25:317–334. doi: 10.1016/j.tmrv.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Elias E., Mauka W., Philemon R.N., Damian D.J., Mahande M.J., Msuya S.E. Knowledge, attitudes, practices, and factors associated with voluntary blood donation among university students in Kilimanjaro, Tanzania. J. Blood Transfus. 2016;2016:1–8. doi: 10.1155/2016/8546803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salaudeen A.G., Odeh E. Knowledge and behavior towards voluntary blood donation among students of a tertiary institution in Nigeria, Niger. J. Clin. Pract. 2011;14:303–307. doi: 10.4103/1119-3077.86773. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed Z., Zafar M., Khan A., Anjum M., Siddique M. Knowledge, attitude and practices about blood donation among undergraduate medical students in Karachi. J. Infect. Dis. Ther. 2014;2:1–5. [Google Scholar]
- 12.Adam N. 2015. Faith and Development in Focus: Bangladesh.https://berkleycenter.georgetown.edu/publications/faith-and-development-in-focus-bangladesh (accessed April 16, 2021) [Google Scholar]
- 13.Nathaniel A. 2016. Islam and Development in Bangladesh: A Grassroots Perspective.http://hdl.handle.net/10822/1052055 (accessed April 17, 2021) [Google Scholar]
- 14.Zangiacomi Martinez E., Dos Santos Almeida R.G., Garcia Braz A.C., Duarte De Carvalho A.C. Association between religiousness and blood donation among Brazilian postgraduate students from health-related areas. Rev. Bras. Hematol. Hemoter. 2014;36:184–190. doi: 10.1016/j.bjhh.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toni-Uebari T.K., Inusa B.P.D. The role of religious leaders and faith organisations in haemoglobinopathies: a review. BMC Blood Disord. 2009;9:6. doi: 10.1186/1471-2326-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charseatd P. Role of religious beliefs in blood donation behavior among the youngster in Iran: a theory of planned behavior perspective. J. Islam. Mark. 2016;7:250–263. [Google Scholar]
- 17.Hossain M.S., Hasan M.M., Raheem E., Islam M.S., Al Mosabbir A., Petrou M., Telfer P., Siddiqee M.H. Lack of knowledge and misperceptions about thalassaemia among college students in Bangladesh: a cross-sectional baseline study. Orphanet J. Rare Dis. 2020;15:54. doi: 10.1186/s13023-020-1323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uma S., Arun R., Arumugam P. The knowledge, attitude and practice towards blood donation among voluntary blood donors in Chennai, India. J. Clin. Diagn. Res. 2013;7:1043–1046. doi: 10.7860/JCDR/2013/4851.3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucindo Zucoloto M., Zangiacomi Martinez E. Development of a questionnaire to assess knowledge regarding blood donation in a Brazilian population. Rev. Bras. Hematol. Hemoter. 2016;38:175–177. doi: 10.1016/j.bjhh.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Urgesa K., Hassen N., Seyoum A.S. Knowledge, attitude, and practice regarding voluntary blood donation among adult residents of Harar town, Eastern Ethiopia: a community-based study. Hematol. Res. Rev. 2017;8:13–20. doi: 10.2147/JBM.S121460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO Who can give blood. https://www.who.int/campaigns/world-blood-donor-day/2018/who-can-give-blood (accessed January 16, 2022)
- 22.Karim M., Alam M., Farazi M., Labone R. Factors influencing blood donation behavior of university level students in Bangladesh. J. Inf. Technol. 2012;1:35–40. [Google Scholar]
- 23.Enawgaw B., Yalew A., Shiferaw E. Blood donors’ knowledge and attitude towards blood donation at North Gondar district blood bank, Northwest Ethiopia: a cross-sectional study. BMC Res. Notes. 2019;12:1–6. doi: 10.1186/s13104-019-4776-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Global Adult Tobacco Survey Bangladesh Report 2017. 2017. https://ntcc.gov.bd/ntcc/uploads/editor/files/GATS Report Final-2017_20 MB.PDF [Google Scholar]
- 25.Bani M., Giussani B. Gender differences in giving blood: a review of the literature. Blood Transfus. 2010;8:278–287. doi: 10.2450/2010.0156-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hashim A., Haneena F., Muhammed Rashid C.S., Dsouza N.D.R. Analysis of lead, cadmium, and nickel in blood donors in relation to smoking—a comparative study. J. Environ. Pathol. Toxicol. Oncol. 2019;38:165–172. doi: 10.1615/JEnvironPatholToxicolOncol.2019028792. [DOI] [PubMed] [Google Scholar]
- 27.Åberg A.-M., Sojka B.N., Winsö O., Abrahamsson P., Johansson G., Larsson J.E. Carbon monoxide concentration in donated blood: relation to cigarette smoking and other sources. Transfusion. 2009;49:347–353. doi: 10.1111/j.1537-2995.2008.01951.x. [DOI] [PubMed] [Google Scholar]
- 28.Olaiya M.A., Alakija W., Ajala A., Olatunji R.O. Knowledge, attitudes, beliefs and motivations towards blood donations among blood donors in Lagos, Nigeria. Transfus. Med. 2004;14:13–17. doi: 10.1111/j.0958-7578.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- 29.Allerson J. Minnesota State University; Mankato: 2012. Assessment of Selected University Students’ Knowledge of Blood Donation and the Relationship with Intent to Donate Blood.https://cornerstone.lib.mnsu.edu/cgi/viewcontent.cgi?article=1053&context=etds [Google Scholar]
- 30.Education in Bangladesh Bangladesh.com. https://www.bangladesh.com/culture/education/ (accessed July 1, 2022)
- 31.Beyerlein K. The effect of religion on blood donation in the United States. Sociol. Relig. 2016;77:408–435. [Google Scholar]
- 32.Zucoloto M.L., Bueno-Silva C.C., Ribeiro-Pizzo L.B., Martinez E.Z. Knowledge, attitude and practice of blood donation and the role of religious beliefs among health sciences undergraduate students. Transfus. Apher. Sci. 2020;59 doi: 10.1016/j.transci.2020.102822. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.