Abstract
Point of care ultrasound (POCUS) is an essential component of emergency medicine training that has not taken hold in internal medicine training programs. Internal medicine residents can use POCUS to perform focused examinations and aid complicated procedures. However, while there is widespread interest in learning POCUS, training is not standardized amongst residency curriculums. Therefore, more strides are necessary to correctly implement POCUS training during residency training.
Keywords: POCUS, Internal medicine, Ultrasound training, Residency, Hospitalist
1. Introduction & background
Point of care ultrasound (POCUS) is defined as the ultrasound performed by the physician at bedside for evaluating and managing the patient.1 Due to its point of care or bedside use, it is increasingly used in many specialties and helps answer brief but essential questions regarding a patient’s symptoms. Using POCUS can narrow down the differential diagnosis by adding more information to the findings revealed by a physical examination done by the physician. It also reduces the cost and length of hospital stays by decreasing procedure-related complications.2 Ultrasound to detect varying pathologies in an undifferentiated patient may be a game-changer in medicine. POCUS enables the provider to a rapid evaluation of the patient. Given its portability and guidance in decision-making, the use of POCUS has expanded across various hospital settings like the emergency department and acute care units. It assists the physician with immediate decision-making, hence saving the need for more complex imaging and thus saving time.3
POCUS is resourceful in health care facilities in rural areas where providers don’t have access to any diagnostic laboratory and imaging equipment. POCUS serves many purposes in these settings. Besides saving space, it also prevents lengthy transports and delays in treatment and decreases the overall cost for both the patient and the hospital.4 POCUS is also particularly useful in a community hospital setting where urgent or emergency standard of care imaging is not readily available. Usage of POCUS by internist or internal medicine residents in a community hospital ensures timely transfer of patients to a higher center when more expert care is available.5
POCUS has some undisputed applications across the spectrum of various pathologies. It can serve as a tool for diagnosis and performing specific procedures. POCUS is utilized to guide therapeutic procedures like central and peripheral venous catheter insertions, thoracentesis, and paracentesis.6 Various applications of POCUS were also reported by Watson K et al. through an online survey of 238 internal medicine residents, which showed that participants found POCUS helpful in diagnosing ascites, analyzing left ventricular function, and pericardial effusion. The residents also felt that POCUS was highly applicable in therapeutic procedures like thoracocentesis, paracentesis, and central line insertion.7
G Bedetti et al. found that handheld ultrasound to evaluate lung ultrasound comets, a sign of pulmonary edema, could be seen by novice users of POCUS and was as reliable as a complex and expansive echocardiography technology used by a trained physician. It also prevented exposure to harmful X-rays, was low cost, and could be performed at the bedside.8 A prospective study involving 104 patients concluded that POCUS was effective and accurate in abdominal aortic aneurysm screening, and the results obtained were comparable to traditional duplex ultrasound. It could be an added asset in the physical examination of such patients.9 It is a valuable tool in the Covid-19 outbreak as a study showed lung ultrasound had a sensitivity of 97% and a negative predictive value of 98% in diagnosing Covid-19 infection. Therefore it helped the physicians in properly identifying patients who tested negative for the virus (RT-PCR).10
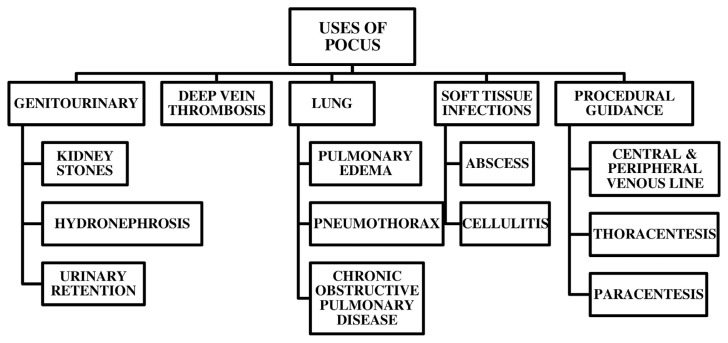
In the emergency department, various protocols employ POCUS, like the BLUE (bedside lung ultrasound in an emergency) protocol, to diagnose patients presenting with acute respiratory distress. A study showed that POCUS was equally efficient as a CT scan in diagnosing the cause of respiratory failure.11 The Rapid Ultrasound for Shock and Hypotension (RUSH) is also used in the emergency department to evaluate patients presenting with hypotension to assist the provider in finding the origin of the shock.12 POCUS is also being increasingly used to diagnose Skin and Soft Tissue Infections in the urgent care setting. It improves the diagnostic abilities of the physician for ruling in abscesses and preventing unnecessary procedures.13 Fig. 1 below summarizes various easy-to-learn uses of POCUS and its applications in the internal medicine residency program.14
Fig. 1.
Uses of POCUS.14
Hence, there are numerous applications of POCUS, and its implementation will empower physicians in providing better care to their patients.2 Implementation of POCUS will not come easily as it faces many challenges like being operator dependent[1], a small number of trainers and supervisors, and no well-structured learning and training programs.15 Ultrasound is an essential component of fields such as emergency medicine (EM) that has yet to take hold in internal medicine (IM) programs. However, The American College of Physicians recognized the significance of ultrasound in the practice of internal medicine in 2018.6 An anonymous survey to assess 52 internal medicine residents’ attitudes toward POCUS found that 90% of residents were interested in POCUS, and 83% found it helpful in the inpatient setting.16 Similarly, a needs assessment distributed to internal medicine residents at a small community-based teaching hospital found that 94% of 17 respondents had an interest in POCUS training and found it to be necessary.17 According to the American Medical Association, the use of ultrasound does not belong to anyone’s specialty. Therefore internal medicine residencies should define their own goals regarding the implementation of POCUS and regular competency assessments of the residents.18
Below we will discuss various challenges of implementing POCUS and how to overcome those obstacles.
2. Review
This manuscript is a narrative review of the current state of POCUS in internal medicine residency program. A thorough review of literature was performed by Devyani Ramgobin, Vasu Gupta, Rea Mittal and Lilly Su using PubMed. Various keywords like POCUS, internal medicine curriculum, emergency medicine, challenges of POCUS, applications of POCUS, certification, hospitalists and POCUS, etc were used to write this review. No specific inclusion or exclusion criteria was used by the authors.
2.1. Challenges to implementation of POCUS
Despite having many undisputed applications, well-structured POCUS training has only recently been integrated as a part of the internal medicine residency program. Many program directors believe formal training should be a part of the curriculum.18 Before POCUS can be universally implemented in internal medicine training, it faces many challenges and barriers.
Firstly, there are issues related to technology. Using small handheld devices for ultrasonography should not be expected to replicate the image quality produced by a machine costing almost ten times more.19
Secondly, there is the big question of operator competency. The utility of POCUS highly depends on the training and skill level of the examiner. RA Filly 1988 described ultrasound as the stethoscope of the future, but several general obstacles should be considered.20 It is one thing to teach medical students about ultrasound on cadavers or healthy volunteers where no clinical decisions are being made, but in a clinical setting, the providers need to have good knowledge about the physics of ultrasound, interpretation of images in a way that is correct and adds on to the physical examination and documenting these findings for future reference as well as for billing purposes.21
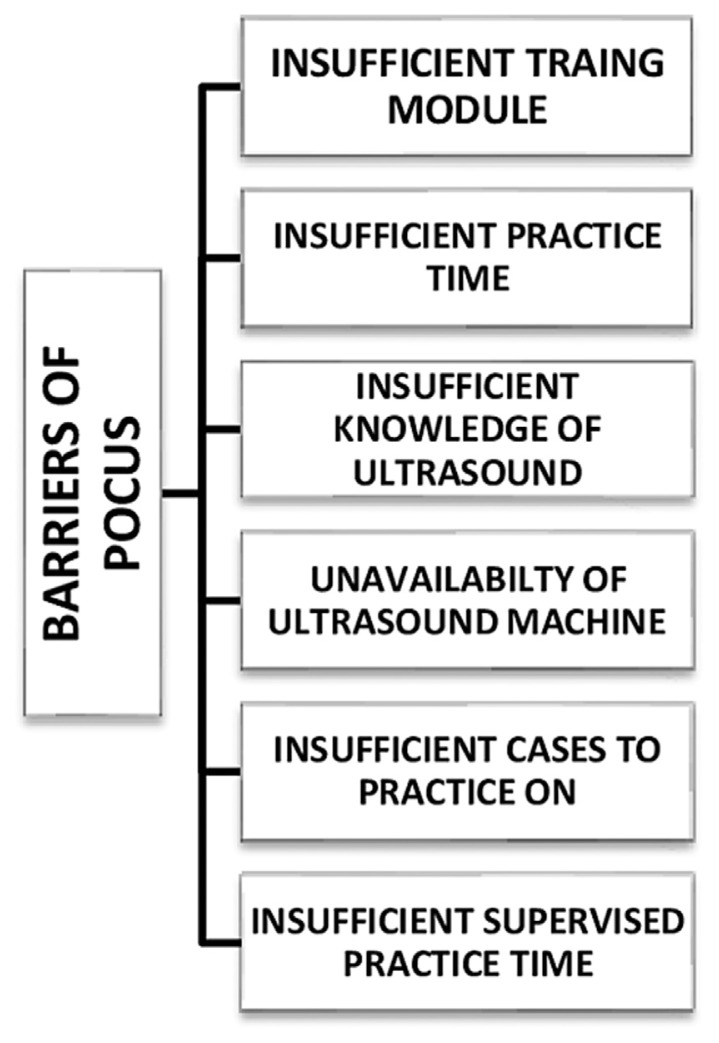
The report’s authenticity and quality assurance will depend upon how well the physician is trained to use ultrasound during their residency. A cross-sectional study done at an internal medicine program in Indonesia noted that almost all respondents (99.4%) felt that POCUS is a valuable tool in internal medicine residency. Still, only 40% reported competency in POCUS, with 62% of the residents feeling that the POCUS training they received during their residency was not satisfactory.22 Some barriers highlighted in this study by Martha et al. are summarized below in Fig. 2 22
Fig. 2.
Barriers to the use of POCUS.22
Similar findings were reported in a national-level survey in the Netherlands involving all internal medicine residents. According to the survey, 92% of residents felt POCUS is a valuable skill for an internist, but 78.6% received less than 10 h of training, with 40% never making it to an ultrasound room.23 In another multicentre, cross-sectional survey of internal medicine residents conducted in 2008 with 367 respondents, 64% reported procedural complications, and 88% felt that complications could have been avoided. Some of the reported factors that could have helped avoid complications included the use of ultrasound (11%) and better training in proper procedure techniques (10%).24 Hence, internal medicine residents receiving ultrasound training would improve their confidence and comfort when performing an invasive bedside procedure. To emphasize the importance of training, a study was done at a teaching hospital in Wisconsin where novice operators (medical students) were given a 3-h training session on using a pocket-sized ultrasound device. They also completed two handson sessions to learn the device’s settings and identify gross anatomical structures. When asked to measure the aortic diameter of 56 patients and then compare it to experts, it was found that novice operators could obtain the measurements reliably. It also demonstrates that novice operators can identify and perform ultrasounds with confidence and reliability with proper training.25 Schnitkke and Danewood’s article on overcoming barriers to POCUS use highlighted unfamiliarity with documentation as the key deterrent to resident use of POCUS. However, when provided with a streamlined in-person education on POCUS documentation protocol, POCUS use by residents increased significantly.26
Integrating POCUS into the internal medicine curriculum still does not solve the problem for hospitalists already in practice. However, hands-on local or national training programs and continued longitudinal training once the hands-on training is started can help the hospitalists get comfortable with POCUS.27
Lastly, the use of POCUS is the complications that may present with billing. POCUS can affect the evaluation of management code by affecting the complexity of medical decision-making. Some see reimbursement as essential to cover the cost of POCUS education and equipment. To effectively bill for POCUS, mainstream guidelines must be set in place and education on proper billing.2
2.2. Overcoming the barrier
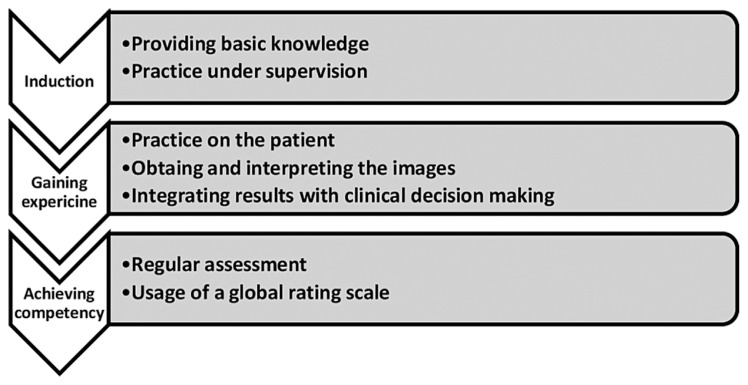
The International Federation of Emergency Medicine (IFEM) mentions three basic steps regarding POCUS training that may also be helpful for internal medicine residents as well. Fig. 3 below summarizes the same.28
Fig. 3.
Steps for POCUS training.28
The goals and aim of training can be educational, like augmenting the anatomical and pathophysiological knowledge, or clinical, like using POCUS for diagnostic and procedural purposes.29
Many education models can train internal medicine residents and increase their efficiency in performing the ultrasound, like didactic lectures, live models, simulation, dedicated ultrasound trainers providing one-on-one training, and direct patient scanning.18 A study that used simulation-based training and didactic lectures on POCUS during the PGY-1 orientation reported increased confidence in using ultrasound and correctly identifying common anatomical structures.30 Simulation-based learning has shown an improved competency in performing ultrasound. However, further research is needed in this field as there is more room for developing more advanced POCUS simulations and incorporating them into undergraduate and graduate medical curricula.31 In another study involving internal medicine residents in their PGY-1 years, after 30-h POCUS training, there was a statistical increase in knowledge regarding image acquisition and interpretation and using the results for clinical decision making.32
The POCUS education may be integrated as a part of internal medicine residency program or as a post-residency fellowship. For instance, at the Scripps Mercy Hospital in San Diego, the Cardiovascular Limited Ultrasound Exam (CLUE) is part of the internal medicine residency curriculum with online modules, monthly lectures along with bedside rounds.33 Another successful POCUS program is at the Oregon Health and Science University. The Internal Medicine Division and POCUS group of the university together created a one-year fellowship program. The curriculum includes weekly conferences focusing on image and literature review along with being mentored by the POCUS faculty.34
Therefore, with proper integration into the curriculum, internal medicine residents’ confidence and competency in performing the ultrasound can be increased.35
2.3. Assessment and supervision
The teaching program’s responsibility is to supervise and provide regular resident assessments. This might be challenging as the majority of the internal medicine program faculty aren’t proficient in performing and thus teaching POCUS.18 Kumar et al. provide a framework for evaluating the POCUS competency of the trainees by standardizing assessments to assess skill. Recommendations include assessing knowledge acquisition, applying knowledge, and technical skill demonstration.36 Maw et al. demonstrated that a short training course consisting of didactics and hands-on training resulted in significant improvements in the ability of internal medicine faculty to acquire and interpret ultrasound data. The intervention also changed faculty attitudes regarding the use of ultrasound, demonstrating that faculty exposure and understanding of POCUS may lead to the incorporation of POCUS in the resident curriculum.37 Hence, it must be noted that to train residents properly, faculty must first be trained and motivated to integrate POCUS into clinical practice. Therefore, internal medicine departments will need to develop a strategy to train faculty and assess their competency to provide proper POCUS training to residents. Charles M. LoPresti emphasizes that it is essential for legal support and oversight from major medical societies to develop standardized POCUS training. They also highlight that medical schools train students on ultrasound, who may then enter a residency program unequipped to continue training on POCUS.18
However, it is difficult to ensure that all POCUS providers have the same training. For example, a cross-sectional survey of 14 family medicine (FM) program directors in Canada revealed inconsistent POCUS training.38
2.4. Certification
Certificate of completion and the certificate of competency are two different things and at times may be interpreted as the same. Although, at present, these is no formal certificate of competency available,27 but many online sources like the Society of Hospital Medicine (SHM), American College of Physicians (ACP), and other agencies like the Alliance for Physician Certification & Advancement (APCA) provide courses on POCUS like continued medical education (CME) or dedicated online modules.39–41 Another organisation that provides certification for critical echocardiography is the National Board of Echocardiography (NBE). The certification requires a physician to perform at least 150 ultrasound examinations which are medically necessary along with 20 h of AMA continued medical education.42
The POCUS curriculum must be highly structured to be successfully implemented in internal medicine residency programs. If incorporated into residency training, will POCUS be taught the same across the board effectively and efficiently to future clinicians? There are several challenges to consider when using POCUS, including ACGME guidelines regarding resident training.
In the past, the American Board of Internal Medicine (ABIM) stipulated that internal medicine residents should document performing a minimum of 5 procedures-ACLS, abdominal paracentesis, arthrocentesis, drawing arterial blood gas (ABG), central venous line placement, nasogastric tube placement (NG), lumbar puncture, pap smear, and thoracocentesis-to graduate from residency. Ultrasound use is indicated in procedures such as thoracocentesis, paracentesis, and central venous line placements. However, in 2007, the requirements were changed and reduced to ACLS, drawing ABG, drawing venous blood, pap smears, and placing a peripheral IV. This change of conditions effectively eliminated any indication and motivation for residents to perform more complex procedures such as paracentesis or inserting central venous catheters. Therefore, this has eliminated the use of ultrasound guidance. Hence, ABIM has none official guidelines for the use, training, assessment and certification of POCUS.27 Currently, there are no requirements by the Accreditation Council for Graduate Medical Education (ACGME) for the use and training of POCUS during internal medicine residency. Although fellowship programs are available for training in POCUS, they are not ACGME accredited. This is in stark contrast to their requirement of achieving POCUS competency in graduating emergency medicine residents. Every emergency medicine residency program accredited by ACGME provides POCUS training guided by consensus recommendations published by the ACEP in 2009.6
In an article by The Canadian Internal Medicine Ultrasound group, they reached a consensus on POCUS applications across internal medicine residency programs. The group recommended specific POCUS applications in the PGY 1–3 and 4–5 curriculum. The article highlighted the next steps after establishing curricula, which included designing educational strategies and developing competency-based assessment procedures to assess trainee skills. Following in these footsteps, programs in the United States should also agree on POCUS applications and then seek to implement the training into the residency curriculum.43
3. Conclusions
There is strong evidence that internal medicine residents across the country are interested in the use of POCUS. A standardized curriculum must be developed and established to ensure that residents are provided with similar exposure to POCUS. Evaluations to assess resident competency must also be found to ascertain that adequate training is provided adequately. While there is much resident interest in POCUS, faculty interest must also be equally on par for POCUS to be adopted into the training curriculum. With proper exposure and training, more faculties will likely become interested in POCUS and recognize the benefits. In addition, with the implementation of ultrasound training in undergraduate medical education, the succeeding graduates have more prior experience and interest in ultrasound use. Thus, internal medicine programs must push to develop a standardized POCUS curriculum with proper forms of evaluation and assessment of trainees.
Footnotes
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Statement of disclosure
The authors have no relevant financial or nonfinancial interests to disclose.
Author contribution
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Devyani Ramgobin, Vasu Gupta, Rea Mittal and Lilly Su. Meet A. Patel and Kinna Parikh assisted in editing the first draft. Nour Shaheen perfomed proof reading. Rohit Jain approved the final draft. All authors read and approved the final manuscript.
Conflict of interest
Authors have no interests to disclose.
References
- 1. Olgers TJ, Azizi N, Blans MJ, Bosch FH, Gans ROB, Ter Maaten JC. Point-of-care ultrasound (PoCUS) for the internist in acute medicine: a uniform curriculum. Neth J Med. 2019;77:168–176. [PubMed] [Google Scholar]
- 2. Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-Care ultrasonography for primary care physicians and general internists. Mayo Clin Proc. 2016;91:18111827. doi: 10.1016/j.mayocp.2016.08.023. [DOI] [PubMed] [Google Scholar]
- 3. Rice JA, Brewer J, Speaks T, Choi C, Lahsaei P, Romito BT. The POCUS consult: how point of care ultrasound helps guide medical decision making. Int J Gen Med. 2021;202114:9789–9806. doi: 10.2147/IJGM.S339476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rominger AH, Gomez GAA, Elliott P. The implementation of a longitudinal POCUS curriculum for physicians working at rural outpatient clinics in Chiapas, Mexico. Crit Ultrasound J. 2020;2018101:19–2018. doi: 10.1186/s13089-018-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sabath BF, Singh G. Point-of-care ultrasonography as a training milestone for internal medicine residents: the time is now. J Community Hosp Intern Med Perspect. 2016;6(5) doi: 10.3402/jchimp.v6.33094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care. 2016:227–2016. doi: 10.1186/s13054-016-1399-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Watson K, Lam A, Arishenkoff S, et al. Point of care ultrasound training for internal medicine: a Canadian multi-centre learner needs assessment study. BMC Med Educ. 2018;2018181:217–2018. doi: 10.1186/s12909-018-1326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bedetti G, Gargani L, Corbisiero A, Frassi F, Poggianti E, Mottola G. Evaluation of ultrasound lung comets by handheld echocardiography. Cardiovasc Ultrasound. 2006;34:20064. doi: 10.1186/1476-7120-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin PH, Bush RL, McCoy SA, et al. A prospective study of a hand-held ultrasound device in abdominal aortic aneurysm evaluation. Am J Surg. 2003;186:455–459. doi: 10.1016/j.amjsurg.2003.07.018. [DOI] [PubMed] [Google Scholar]
- 10. Bianchi S, Savinelli C, Paolucci E, et al. Point-of-care ultrasound (PoCUS) in the early diagnosis of novel coronavirus 2019 disease (COVID-19) in a first-level emergency department during a SARS-CoV-2 outbreak in Italy: a real-life analysis. Intern Emerg Med. 2022;17:193–204. doi: 10.1007/s11739-021-02643-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel CJ, Bhatt HB, Parikh SN, Jhaveri BN, Puranik JH. Bedside lung ultrasound in emergency protocol as a diagnostic tool in patients of acute respiratory distress presenting to emergency department. J Emergencies, Trauma, Shock. 2018;11:125–129. doi: 10.4103/JETS.JETS_21_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gonzalez JM, Ortega J, Crenshaw N, de Tantillo L. Rapid ultrasound for shock and hypotension: a clinical update for the advanced practice provider: Part 2. Adv Emerg Nurs J. 2020;42:284–292. doi: 10.1097/TME.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 13.Burgin CM, Morrow DS.Utility of POCUS in the skin and soft tissue infection. J Urgent Care Med. 2020. Available at: https://www.jucm.com/utility-of-pocus-in-skin-and-soft-tissue-infection/
- 14. Fuller F, Norman F. Five easy-to-master uses for point-of-care ultrasound. JAAPA. 2017;30:48–51. doi: 10.1097/01.JAA.0000526786.04153.5c. [DOI] [PubMed] [Google Scholar]
- 15. Moulin V, Monti M. Roles and challenges of Point-of-Care Ultrasonography in internal medicine. 2021;17:1819–1823. [PubMed] [Google Scholar]
- 16. Elhassan M, Gandhi KD, Sandhu C, Hashmi M, Bahl S. Internal medicine residents’ point-of-care ultrasound skills and need assessment and the role of medical school training. Adv Med Educ Pract. 2019:379–386. doi: 10.2147/AMEP.S198536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dhanani M, Hou A, Moll M, Schembri F. Introduction of an academic medical center’s point-of-care ultrasound curriculum to internal medicine residents at a community-based teaching hospital. J Community Hosp Intern Med Perspect. 2020:93–98. doi: 10.1080/20009666.2020.1742483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. LoPresti CM, Schnobrich DJ, Dversdal RK, Schembri F. A road map for point-of-care ultrasound training in internal medicine residency. Ultrasound J. 2019;11 doi: 10.1186/s13089-019-0124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26:567–581. doi: 10.1016/j.echo.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 20. Filly RA. Ultrasound: the stethoscope of the future, alas. Radiology. 1988;167:400. doi: 10.1148/radiology.167.2.3282260. [DOI] [PubMed] [Google Scholar]
- 21. Geria RN, Raio CC, Tayal V. Point-of-care ultrasound: not a stethoscope-a separate clinical entity. J Ultrasound Med. 2015;34:172–173. doi: 10.7863/ultra.34.1.172. [DOI] [PubMed] [Google Scholar]
- 22. Rosana M, Asmara OD, Pribadi RR, Kalista KF, Harimurti K. Internal medicine residents’ perceptions of point-of-care ultrasound in residency program: highlighting the unmet needs. Acta Med Indones. 2021;53:299–307. [PubMed] [Google Scholar]
- 23. Olgers T, ter Maaten J. Point-of-care ultrasound curriculum for internal medicine residents: what do you desire? A national survey. BMC Med Educ. 20:30. doi: 10.1186/s12909-020-1949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mourad M, Kohlwes J, Maselli J, Auerbach AD. MERN Group. Supervising the supervisors–procedural training and supervision in internal medicine residency. J Gen Intern Med. 2010;25:351–356. doi: 10.1007/s11606-009-1226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bonnafy T, Lacroix P, Desormais I, et al. Reliability of the measurement of the abdominal aortic diameter by novice operators using a pocket-sized ultrasound system. Arch Cardiovasc Dis. 2013;106:644–650. doi: 10.1016/j.acvd.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 26. Schnittke N, Damewood S. Identifying and overcoming barriers to resident use of point-of-care ultrasound. West J Emerg Med. 2019:918–925. doi: 10.5811/westjem.2019.8.43967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Soni NJ, Schnobrich D, Mathews BK, et al. Point-of-Care ultrasound for hospitalists: a position statement of the society of hospital medicine. J Hosp Med. 2019;14:E1–E6. doi: 10.12788/jhm.3079. . Published 2019 Jan 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Point-of-Care ultrasound curriculum guidelines. [2014 Accessed]. https://www.ifem.cc/wp-content/uploads/2016/03/IFEM-Point-of-Care-Ultrasound-Curriculum-Guidelines-2014-2.pdf .
- 29. LoPresti CM, Jensen TP, Dversdal RK, Astiz DJ. Point-of-Care ultrasound for internal medicine residency training: a position statement from the alliance of academic internal medicine. Am J Med. 2019;132:1356–1360. doi: 10.1016/j.amjmed.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 30. Keddis MT, Cullen MW, Reed DA, et al. Effectiveness of an ultrasound training module for internal medicine residents. BMC Med Educ. 2011;75:201111. doi: 10.1186/1472-6920-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Singh J, Matern LH, Bittner EA, Chang MG. Characteristics of simulation-based point-of-care ultrasound education: a systematic review of MedEdPORTAL curricula. Cureus. 2022142:22249–32022. doi: 10.7759/cureus.22249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schnobrich DJ, Olson AP, Broccard A, Duran-Nelson A. Feasibility and acceptability of a structured curriculum in teaching procedural and basic diagnostic ultrasound skills to internal medicine residents. J Grad Med Educ. 2013;5:493–497. doi: 10.4300/JGME-D-12-00214.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Residency program - scripps mercy internal medicine. Scripps Health. https://www.scripps.org/for-health-care-professionals/graduate-medical-education-gme/residencyprograms/scripps-mercy-internal-medicine-residency . [Google Scholar]
- 34. School of medicine general internal medicine. [Accessed June 18, 2022]; OHSU. https://www.ohsu.edu/school-of-medicine/general-internal-medicine/ultrasound-fellowship . Accessed. [Google Scholar]
- 35. Kessler C, Bhandarkar S. Ultrasound training for medical students and internal medicine residents–a needs assessment. J Clin Ultrasound. 2010;38:401–408. doi: 10.1002/jcu.20719. [DOI] [PubMed] [Google Scholar]
- 36. Kumar A, Kugler J, Jensen T. Evaluation of trainee competency with point-of-care ultrasonography (POCUS): a conceptual framework and review of existing assessments. J Gen Intern Med. 2019;34:1025–1031. doi: 10.1007/s11606-01904945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Maw A, Jalali C, Jannat-Khah D, et al. Faculty development in point of care ultrasound for internists. Med Educ Online. 2016;201621:33287–42016. doi: 10.3402/meo.v21.33287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Micks T, Braganza D, Peng S, et al. Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician. 2018;64:462–467. [PMC free article] [PubMed] [Google Scholar]
- 39.Pocus certificate of completion. Society of hospital medicine; [Accessed June 19, 2022]. https://www.hospitalmedicine.org/clinical-topics/ultrasound/pocus-certificate-of-completion/ Accessed. [Google Scholar]
- 40.Search: “pocus”. Search: “pocus”. ACP online; [Accessed June 19, 2022]. https://www.acponline.org/facet/search?collection=acp-online-learning-center-web&query=pocus . Accessed. [Google Scholar]
- 41.Point-of-care ultrasound certification academy. APCA.org. [Accessed June 19, 2022]. Published April 2, 2020. https://www.apca.org/point-of-care-ultrasound-pocus/
- 42.Application for certification in critical care echocardiography (CCEeXAM) [Accessed June 19, 2022]. https://echoboards.org/docs/CCEeXAM-Cert_App-2020.pdf . Accessed.
- 43. Ma IWY, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian internal medicine ultrasound (CIMUS) group. J Gen Intern Med. 2017;32:1052–1057. doi: 10.1007/s11606-017-4071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]