Abstract
Objective:
Poverty, racial bias, and disparities are linked to adverse health outcomes for children in the United States. The social vulnerability and child opportunity indices are composite measures of the social, economic, education, health, and environmental qualities that impact human health for every U.S. census tract. Composite measures of social vulnerability and child opportunity were compared for neighborhood hot spots, where pediatric intensive care unit admissions for acute respiratory failure requiring invasive mechanical ventilation were at the 90th percentile or greater per 1,000 children, versus non-hot spots.
Design:
Population-based ecological study.
Setting:
Two urban free-standing children’s hospital pediatric intensive care units consisting of a 36-bed quaternary academic and a 56-bed tertiary community center, in Atlanta, Georgia.
Interventions:
None.
Measurements and Main Results:
Residential addresses were geocoded and spatially joined to census tracts. Composite measures of social vulnerability and childhood opportunity, PICU readmission rates, and hospital length of stay were compared between neighborhood hot spots versus non-hot spots. There were 340/3,514 (9.7%) children who lived within a hot spot. Hot spots were associated with a higher (worse) composite social vulnerability index ranking, reflecting differences in socioeconomic status, household composition and disability, and housing type and transportation. Hot spots also had a lower (worse) composite childhood opportunity index percentile ranking, reflecting differences in the education, health and environment, and social and economic domains. Higher social vulnerability and lower childhood opportunity were not associated with readmission rates, but were associated with longer total median duration of hospital days per 1000 children in a census tract.
Conclusions:
Social determinants of health identified by geospatial analyses are associated with acute respiratory failure requiring invasive mechanical ventilation in critically ill children. Interventions addressing the neighborhood social vulnerability and child opportunity are needed to decrease disparities in intensive care admissions for acute respiratory failure requiring mechanical ventilation.
Tweet:
Intubated children living in Georgia neighborhoods with higher social vulnerability and lower child opportunity are associated with longer per capita hospital stays.
Keywords: social determinants of health, disparities, acute respiratory failure, social vulnerability index, child opportunity index, pediatric intensive care unit, census tract, neighborhood, geocoding
INTRODUCTION
Acute respiratory failure is a leading cause of admission to a pediatric intensive care unit (1, 2). The aggregate cost in children hospitalized for a respiratory system diagnosis with a ventilator greater than 96 hours, excluding neonatal admissions, was $580 million in 2016 (3). We and others have described the social determinants of health and outcome disparities in critically ill children (4–8). For example, children living in impoverished neighborhoods are more likely to be admitted to a PICU and are hospitalized for a longer duration (4, 8).
Composite indices, such as the Social Vulnerability Index (SVI) and the Child Opportunity Index 2.0 (COI) are multi-dimensional measures of neighborhood (census tract) factors that contribute to a community’s health (9, 10). The SVI and COI have been used to determine the association of social determinants of health with the use of heath care services and outcomes (6, 11–15). The objective of this study was to identify neighborhoods where PICU admission rates for invasively mechanically ventilated children per 1,000 children were greater than or equal to the 90th percentile using geospatial analysis. We hypothesized that hot spot neighborhoods with the highest admissions (per 1,000 children) would have higher neighborhood SVI and lower neighborhood COI. Furthermore, we hypothesized that hot spot neighborhoods would also have a longer population-based total inpatient bed day rate per 1,000 children residing in the census tract, and that neighborhoods with greater total inpatient bed days per 1,000 children would be associated with higher SVI and lower COI.
METHODS
Study Setting and Design
We identified children under 18 years of age with acute respiratory failure listed as a problem in their electronic health record (EHR) who were admitted to the PICU at Children’s Healthcare of Atlanta’s Egleston campus (a 36-bed academic quaternary care hospital) and Scottish Rite campus (a 56-bed tertiary care community hospital) between January 1, 2015 and May 31, 2020. We selected only intubated and mechanically ventilated children with a Georgia residential address who were admitted to a PICU for at least one day. Children with multiple admissions were included in the analysis only once during their first PICU encounter.
Ethics Statement
This study was approved by the Children’s Healthcare of Atlanta Institutional Review Board (IRB0483) with a waiver of informed consent due to the retrospective observational study design prior to the request and retrieval of any EHR data.
Geocoding, Mapping, and Census Tract Data
We mapped patient residential addresses by geocoding to census tracts using the R package tidygeocoder (16). The U.S. Census 2018 GEOIDs for each census tract in Georgia were retrieved using the R package tigris (17). Socioeconomic data for each census tract was obtained using the R package tidycensus using the census tract GEOID (18). The Social Vulnerability Index (SVI) data for 2018 were downloaded from the Centers for Disease Control and Prevention (CDC) website and joined to the patient data using the census tract GEOID (9). The Child Opportunity Index 2.0 (COI 2.0) for 2015 was downloaded from the diversitydatakids.org website and joined to the patient data using the census tract GEOID (10). The state-based COI 2.0 rankings for Georgia were used in the analysis. The R package mapview was used to create choropleth maps (19).
Hot spot Identification
The PICU acute respiratory failure admission rate (per 1000 children in the census tract) was calculated by summing the number of first-encounter (index PICU admission) patients within a specified census tract and dividing by the number of children residing within that census tract as estimated by the 2015 – 2019 5-year American Community Survey (2019 ACS-5). Neighborhood hot spots were defined as census tracts with PICU admission rates in the 90th percentile or greater.
Outcome Measures
The primary outcome measure was the population-level inpatient bed days rate for acute respiratory failure with mechanical ventilation admissions. The inpatient bed days rate is the median aggregate inpatient bed days for children residing within a census tract divided by the number of children residing within that census tract estimated from the 2019 ACS-5 and normalized per 1000 children. Individual patient-level outcomes included the number of deaths, duration of hospitalization in days, the number of patients with multiple admissions, the median number of subsequent (multiple) admissions, and the median time to readmission in days.
Statistical analyses
Data were analyzed using R version 4.0.2 (20). The Wilcoxon rank sum and chi-square tests were used for group differences. A subgroup analysis excluding post-operative patients was performed by hot spot status for SVI themes, COI domains, and outcomes. A p-value less than 0.05 was considered significant.
RESULTS
Study population
During the study period, there were 3,514 children admitted to the PICU for at least one day who were intubated for acute respiratory failure between January 1, 2015 and May 31, 2020 with matching SVI and COI census tract level data (eFigure 1). 9.7% lived within a neighborhood hot spot. The admission rate per 1000 children living in a hot spot neighborhood was 6.3 (Q1, Q3: 5.2, 6.9 days per 1000 children) compared to a non-hot spot neighborhood at 2.2 (Q1, Q3: 1.6, 3.2 days per 1000 children; p < 0.0001). The patient-level demographic and clinical characteristics of the children, stratified by hot spot residence, are shown in Table 1. There was no difference in median age or proportion of female/male children, ethnicity, primary spoken language, or hospital discharge disposition between children who lived within a hot spot compared to children who lived outside a hot spot. Children living in hot spot neighborhoods were more likely to self-identify as being Black and have public/government-sponsored health insurance (Table 1). There was no difference in common diagnoses, including pneumonia, bronchiolitis, status asthmaticus, trauma, sepsis, cardiac arrest, child abuse, status epilepticus or post-operative status, for children living in a hot spot compared to a non-hot spot neighborhood (Table E1). The mapped intensive care admissions were distributed throughout Georgia; however, the majority of children admitted to an intensive care unit resided in the 29 county Atlanta-Sandy Springs-Roswell metropolitan statistical area (ATL MSA) (Figure 1A).
Table 1.
Patient-Level Characteristics of Children with Acute Respiratory Failure Requiring Invasive Mechanical Ventilation by Residence within a Hot Spot Neighborhood
| Patients Residing in a Hot Spota | ||
|---|---|---|
| Characteristic | No n = 3174 (90.3%) |
Yes n = 340 (9.7%) |
| Age (years), median (Q1, Q3)) | 3.39 (0.75, 9.98) | 2.17 (0.46, 9.12) |
| Sex, n (%) | ||
| Female | 1414 (44.5) | 141 (41.5) |
| Male | 1759 (55.4)b | 199 (58.5) |
| Race, n (%) | ||
| Black | 1376 (43.4) | 230 (67.6)** |
| White | 79 (23.2) | 79 (23.2) |
| Multiple | 100 (3.2) | 5 (1.5) |
| Asian | 124 (3.9) | 9 (2.7) |
| Other | 13 (0.4) | 2 (0.6) |
| Unknown | 212 (6.7) | 15 (4.4) |
| Ethnicity, n (%) | ||
| Non-Hispanic / Latino | 2647 (83.4) | 302 (88.8) |
| Hispanic / Latino | 510 (16.1) | 38 (11.2) |
| Declined / Unknown | 17 (0.5) | 0 (0.0) |
| Primary Language, n (%) | ||
| English | 2847 (89.7) | 306 (90) |
| Spanish | 271 (8.5) | 28 (8.2) |
| Other | 56 (1.8) | 6 (1.8) |
| Insuranced, n (%) | ||
| Public | 2195 (69.2) | 281 (82.6)** |
| Private | 861 (27.1) | 48 (14.1) |
| Military | 54 (1.7) | 5 (1.5) |
| None / Self-pay | 64 (2.0) | 6 (1.8) |
| Hospital Location, n (%) | ||
| Egleston Campus | 1677 (52.8) | 221 (65)** |
| Scottish Rite Campus | 1497 (47.2) | 119 (35) |
| Hospital Discharge Disposition, n (%) | ||
| Home | 2379 (74.9) | 251 (73.8) |
| Expired | 328 (10.3) | 36 (10.6) |
| Home Health | 118 (3.7) | 13 (3.8) |
| Other Hospital | 233 (7.3) | 27 (7.9) |
| Psychiatric Hospital | 73 (2.3) | 6 (1.8) |
| Inpatient Rehabilitation | 10 (0.3) | 2 (0.6) |
| Hospice | 9 (0.3) | 0 (0) |
| Missing/Other | 24 (0.8) | 5 (1.5) |
Hotspot is a census tract ranked at or above the 90th percentile for the highest number of children admitted to intensive care with acute respiratory failure per 1000 children living in the census tract
Missing n = 1 sex for the Patients Residing in a Hot Spot: No
Hospital Admission Rate is the number of children admitted to intensive care for acute respiratory failure living in a census tract per 1000 children living in the census tract; this is how hotspots were defined
p < 0.05,
p < 0.0001 Chi-squared test
Figure 1. Distribution of children admitted to two Atlanta, Georgia pediatric intensive care units for acute respiratory failure requiring mechanical ventilation during the 2015 – 2020 study period.
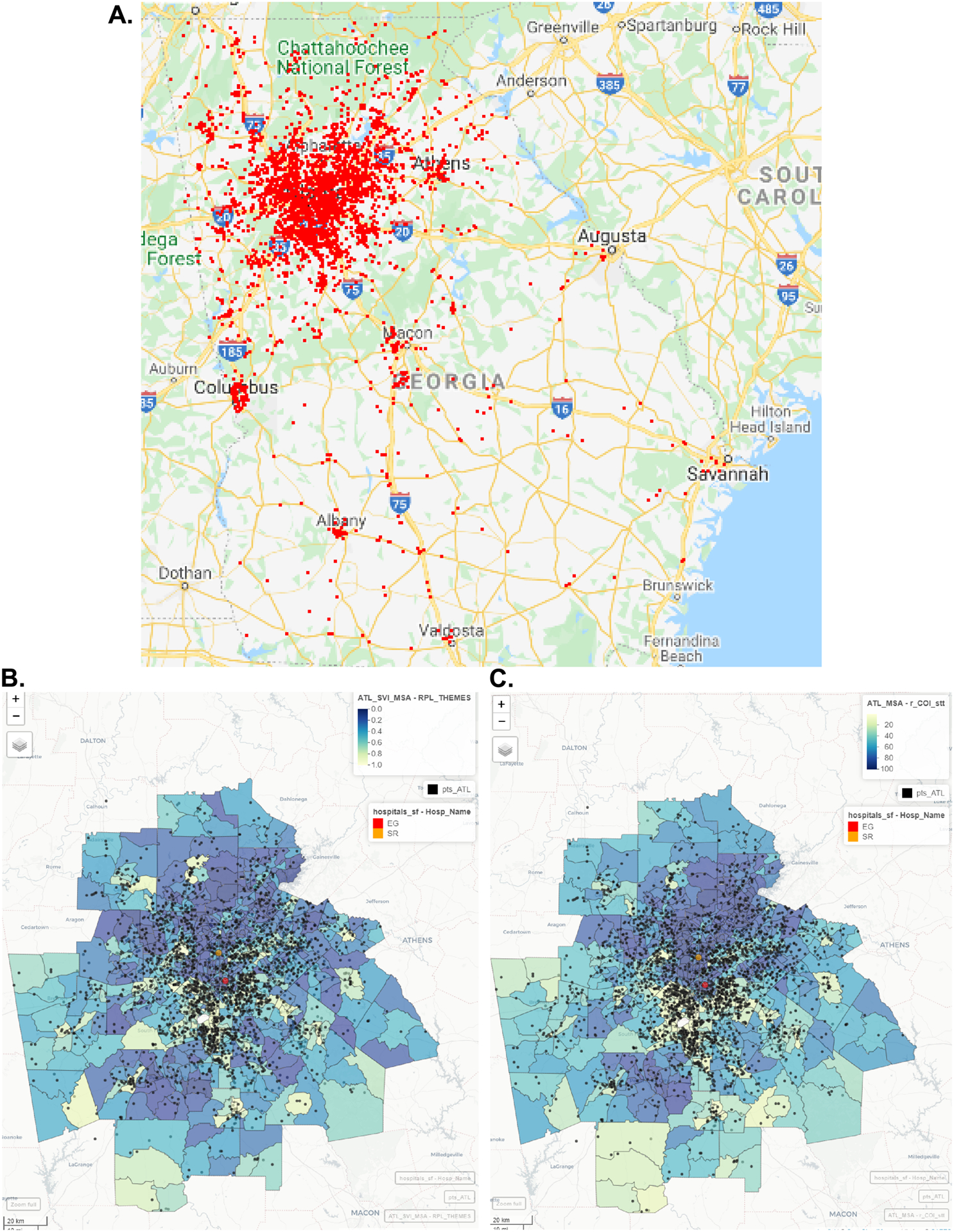
A) Roadmap of Georgia with residences indicated by red dots. Choropleth maps of the Atlanta-Sandy Springs-Roswell metropolitan statistical area showing B) the Overall Social Vulnerability Index state-based rankings from 0 to 1, and C) the Overall Child Opportunity Index (COI) 2.0 state-based rankings from 1 – 100. Yellow indicates a census tract with a high (worse) SVI and low (worse) COI 2.0. Purple indicates a census tract with a low (better) SVI and high (better) COI 2.0. Black dots indicate individual residences. The Children’s Healthcare of Atlanta hospital with pediatric intensive care units are indicated by a red circle (Egleston campus) and an orange circle (Scottish Rite campus). The gray census tract south of Atlanta contains Hartsfield-Jackson International airport. It is colored gray because there is no SVI or COI index data for this tract.
Social Vulnerability Index is higher in children residing in neighborhood hot spots
The social vulnerability indicators for children stratified by neighborhood hot spot residential status are summarized in Table 2 by thematic domain and overall percentile summary ranking. The composite individual domains and the overall SVI scores are ranked by percentile from 0 to 1, with higher values indicating greater vulnerability. All individual indicators were significantly different by neighborhood hot spot status along with the composite percentile ranking of all four themes including socioeconomic status, household composition and disability, minority status and language, and housing type and transportation. Within the socioeconomic theme, the percentage of households below poverty, with high unemployment, and low high school graduation, contributed the most to the disparity between hot spot and non-hot spot neighborhoods (Table 2). Within the household composition and disability theme, a higher proportion of disabled individuals and single-parent households contributed to the difference between groups (Table 2). Within the housing and transportation theme, high-density housing, crowding (housing units with more people than rooms), and lack of access to a household vehicle contributed the most to disparity between groups (Table 2). Within the minority status and language theme, there was a 30% difference in English-speaking minorities living inside versus outside of a hot spot neighborhood (Table 2). The percentile difference for the three SVI themes including socioeconomic status, household composition and disability, and housing type and transportation contributed the most to the differences in percentile ranking for hot spot versus non-hot spot neighborhoods (Table 2); however, the social vulnerability percentile ranking for all four composite themes and the overall SVI measure were higher for children living within a hot spot versus non-hot spot neighborhood. A map of the ATL MSA shows that intensive care admissions are clustered in tracts with higher SVI (Figure 1B).
Table 2.
Social Vulnerability Index for Children with Acute Respiratory Failure Requiring Invasive Mechanical Ventilation by Hot Spot Residence
| Patients Residing in a Hot Spota | ||||
|---|---|---|---|---|
| No n = 3174 |
Yes n = 340 |
|||
| Characteristic | Median | Q1, Q3 | Median | Q1, Q3 |
| Socioeconomic Status, % | ||||
| Below Poverty | 14.5 | 8.2, 22.2 | 22.4**** | 14.8, 31.3 |
| Unemployment | 5.6 | 4.0, 8.5 | 10.6**** | 6.1, 14.7 |
| Per Capita Income, $ | 25,488 | 20,514; 31930 | 19,946**** | 16,336; 24289 |
| No High School Diploma (≥ 25 years) | 12.0 | 7.4, 19.0 | 17.0**** | 10.5, 23.7 |
| Household Composition & Disability, % | ||||
| Age ≥ 65 years | 11.4 | 8.5, 15.0 | 11.6* | 9.4, 16.4 |
| Age ≤ 17 years | 26.0 | 23.2, 28.8 | 24.0**** | 19.0, 27.7 |
| Disability | 11.3 | 8.0, 14.6 | 13.6**** | 11.2, 17.8 |
| Single Parent Households | 10.6 | 7.1, 15.9 | 11.9** | 7.5, 16.9 |
| Minority Status & Language, % | ||||
| Minority, % | 52.7 | 28.8, 81.7 | 83.7**** | 52.6, 97.9 |
| Limited English, % | 1.5 | 0.4, 4.4 | 1.2**** | 0.0, 3.1 |
| Housing Type & Transportation, % | ||||
| Housing with ≥ 10 units | 3.3 | 0.0, 16.9 | 7.2**** | 2.5, 19.6 |
| Mobile Homes | 1.5 | 0.0, 7.4 | 0.6**** | 0.0, 2.6 |
| Housing units with more people than rooms | 1.9 | 0.7, 3.7 | 2.8*** | 1.2, 4.0 |
| Households with no vehicle | 4.4 | 1.9, 8.9 | 12.1**** | 5.2, 21.9 |
| Persons living in group quarters | 0.1 | 0.0, 0.6 | 0.1 | 0.0, 0.9 |
| Overall Percentile Ranking Summary by Theme, Rank (scale: 0 – 1) | ||||
| Theme 1: Socioeconomic Status | 0.45 | 0.26, 0.71 | 0.70**** | 0.57, 0.93 |
| Theme 2: Household Composition & Disability | 0.47 | 0.27, 0.70 | 0.60**** | 0.32, 0.81 |
| Theme 3: Minority Status & Language | 0.65 | 0.35, 0.86 | 0.67** | 0.47, 0.89 |
| Theme 4: Housing Type & Transportation | 0.48 | 0.23, 0.72 | 0.63**** | 0.37, 0.75 |
| Overall Percentile Ranking | 0.49 | 0.26, 0.75 | 0.73**** | 0.49, 0.88 |
Hot spot = census tracts ranked at or above the 90th percentile for the highest number of children admitted to intensive care with acute respiratory failure per 1000 children living in the census tract
Wilcoxon Rank sum test with continuity correction,
p < 0.05,
p < 0.01,
p < 0.001,
p < 0.0001
Child Opportunity Index is lower in children residing in neighborhood hot spots
The raw child opportunity indicators for children stratified by neighborhood hot spot residential status are summarized in Table 3 by thematic domain and overall percentile summary ranking. The standardized and scaled z-scores for the census tracts in Georgia are reported in Table E2. Some indicators are reversed such that a higher z-score always indicates more child opportunity. The composite individual domains and the overall COI 2.0 scores are ranked by percentile from 1 to 100. All but one of the individual indicators were significantly different by neighborhood hot spot status. The composite percentile ranking of all three domains including education, health and environment, and social and economic along with the overall percentile summary ranking showed lower child opportunity (Table 3). Within the education domain, lower enrollment in early childhood education, worse third grade reading and math proficiency, lower high school graduation, higher school poverty, fewer experienced teachers, and lower adult educational attainment contributed to the most to the difference between the groups (Table 3 and Table E2). Within the health and environment domain, lower access to healthy food, higher housing vacancy rates, greater levels of industrial pollutants and airborne microparticles, and lower health insurance coverage contributed to the disparity between groups (Table 3 and Table E2). Within the social and economic domain, lower employment rate, having a longer commute, a higher poverty and public assistance rate, and a greater proportion of single-headed households contributed to the differences between neighborhoods (Table 3 and Table E2). The domain summary percentile rankings and the overall percentile ranking summary were markedly different between hot spot versus non-hot spot neighborhoods (Table 3). A map of the ATL MSA shows that intensive care admissions are clustered in tracts with lower COI 2.0 (Figure 1C).
Table 3.
Child Opportunity Index Raw Score Indicators by Domains for Children with Acute Respiratory Failure Requiring Invasive Mechanical Ventilation by Hot Spot Residence
| Patients Residing in a Hot Spota | ||||
|---|---|---|---|---|
| No n = 3174 |
Yes n = 340 |
|||
| Characteristic | Median | Q1, Q3 | Median | Q1, Q3 |
| Education | ||||
| Early Childhood Education Centersb | 3.66 | 2.79, 4.41 | 4.56**** | 3.76, 4.95 |
| High Quality Early Childhood Education Centersb | 0.16 | −2.51, 1.38 | 1.56**** | 0.00, 2.30 |
| Early Childhood Education Enrollmentc | 49.90 | 33.90, 67.10 | 44.30**** | 24.40, 61.40 |
| Third Grade Reading Proficiencyd | 195.25 | 137.45, 246.67 | 114.59**** | 82.70, 166.10 |
| Third Grade Math Proficiencyd | 211.98 | 148.72, 267.07 | 121.83**** | 97.71, 201.15 |
| High School Graduation Rate | 78.65 | 68.98, 85.36 | 73.87**** | 67.02, 81.24 |
| Advanced Placement Course Enrollmentd | 0.50 | 0.37, 0.65 | 0.39**** | 0.31, 0.51 |
| College Enrollment in Nearby Institutions | 39.16 | 36.12, 41.62 | 40.23**** | 36.93, 42.98 |
| School Povertyd | 70.91 | 51.88, 89.42 | 94.19**** | 77.20, 99.22 |
| Teacher Experienced | 9.38 | 5.31, 16.06 | 15.22**** | 8.05, 20.97 |
| Adult Educational Attainment | 24.73 | 16.29, 35.65 | 19.80**** | 12.83, 25.60 |
| Health and Environment | ||||
| Access to healthy food | 3.44 | 1.44, 6.05 | 7.37**** | 3.38, 15.76 |
| Access to green space | 14.60 | 5.20, 23.20 | 19.70**** | 14.10, 28.30 |
| Walkability | 7.04 | 5.62, 8.59 | 9.31**** | 6.24, 11.73 |
| Housing vacancy rate | 8.33 | 5.43, 12.28 | 14.00**** | 8.54, 19.05 |
| Hazardous waste dump sites | −13.82 | −13.82, −13.82 | −13.82 | −13.82, −13.82 |
| Industrial pollutants in air, water, or soil | 8.88 | 7.48, 9.55 | 9.56**** | 9.22, 9.97 |
| Airborne microparticles, PM2.5 | 11.10 | 10.79, 11.33 | 11.45**** | 11.22, 11.54 |
| Ozone Concentrations | 38.41 | 38.18, 38.71 | 38.11**** | 37.93, 38.36 |
| Extreme Heat Exposure, summer days | 59.00 | 53.00, 63.67 | 59.67**** | 58.00, 61.33 |
| Health Insurance Coverage | 83.49 | 77.66, 88.50 | 78.84**** | 74.40, 85.18 |
| Social and Economic | ||||
| Employment rate | 77.00 | 71.64, 81.06 | 72.50**** | 64.85, 76.77 |
| Commute duration > 1h one-way | 32.54 | 24.00, 40.65 | 23.59**** | 17.46, 31.02 |
| Poverty rate | 15.47 | 9.12, 23.66 | 22.67**** | 14.20, 34.15 |
| Public assistance rate | 14.68 | 7.73, 22.84 | 22.23**** | 12.96, 34.91 |
| Homeownership rate | 66.51 | 45.70, 80.27 | 47.47**** | 34.67, 66.55 |
| High-skill employment | 11.96 | 7.27, 16.36 | 13.49** | 9.08, 16.95 |
| Median household income | 52,705 | 40,685; 69,737 | 37,311**** | 30,497; 50,142 |
| Single-headed households | 36.89 | 24.24, 52.95 | 58.67**** | 37.43, 76.34 |
| Overall Percentile Ranking Summary by Domain e | ||||
| Domain 1: Education | 49 | 23, 72 | 16**** | 6, 31 |
| Domain 2: Health and Environment | 49 | 24, 72 | 16**** | 4.75, 41.25 |
| Domain 3: Social and Economic | 49 | 24, 71 | 16**** | 6, 43 |
| Overall Percentile Ranking (scale: 1 – 100) | 48 | 24, 72 | 14**** | 4, 42 |
Hotspot is a census tract ranked at or above the 90th percentile for the highest number of children admitted to intensive care with acute respiratory failure per 1000 children living in the census tract
Missing n = 1 sex for the Patients Residing in a Hot Spot: No
Hospital Admission Rate is the number of children admitted to intensive care for acute respiratory failure living in a census tract per 1000 children living in the census tract; this is how hotspots were defined.
p < 0.05,
p < 0.0001 Chi-squared test
Outcomes
Children living in a neighborhood hot spot had a greater number of inpatient bed days and a higher inpatient bed day rate (Table 4). Inpatient bed day rate (per 1000 children) was further dichotomized into a high and low group, with a high rate defined as greater than or equal to the 90th percentile by census tract corresponding to 94.375 or more inpatient bed days (per 1000 children). There were 353 (10%) children living in census tracts with a high inpatient bed day rate. Children living in a high inpatient bed day rate neighborhood had greater social vulnerability, evidenced by all four themes and the overall composite index (Figure E2). Additionally, children with the high inpatient bed day rate had less child opportunity in all three domains and the overall composite index (Figure E3). There were 162 children living in both a neighborhood hot spot and in a census tract with an inpatient bed day rate at the ninetieth percentile or greater.
Table 4.
Outcomes by Hot Spot Status
| Patients Residing in a Hot Spota | ||
|---|---|---|
| Died, n (%) | 328 (10.3) | 36 (10.6) |
| Hospital Length of Stay (days), median (Q1, Q3) | 9.3 (4.0, 19.5) | 9.4 (4.2, 18.8) |
| Inpatient Bed Day | 51.3 (25.4, 95.7) | 81.1 (49.2, 150.6)**** |
| Inpatient Bed Day Rateb | 29.9 (17.3, 50.4) | 85.57 (64.2, 119.9)**** |
| Multiple Admissions, n (%) | 277 (8.7) | 26 (7.6) |
| Number of Admissions, median (Q1, Q3) | 1 (1, 1) | 1 (1, 1) |
| Time to readmission (days), median (Q1, Q3) | 219 (62.4, 451) | 170 (106, 392) |
Hotspot is a census tract ranked at or above the 90th percentile for the highest number of children admitted to intensive care with acute respiratory failure per 1000 children living in the census tract.
Inpatient Bed Day Rate is the sum of total days in the hospital for children living in a census tract per 1000 children living in the census tract.
p < 0.05,
p < 0.0001 Wilcoxon Rank sum test or Chi-squared test
Other outcomes, stratified by neighborhood hot spot residence, are shown in Table 4. Death occurred in 10% of the cohort and did not differ by residence in versus out of a neighborhood hot spot. Neither the duration of a hospitalization, nor the time to readmission for individual patients, was higher in neighborhood hot spots compared to non-hot spots (Table 4). PICU readmission rates did not differ by hot spot status (Table 4). Excluding post-operative patients from the cohort did not change the outcome results (data not shown).
DISCUSSION
In this study, we used geospatial analysis to show that greater social vulnerability and lower child opportunity are associated with PICU admission of children requiring intubation and mechanical ventilation for acute respiratory failure in metropolitan Atlanta, Georgia. Children residing within neighborhood hot spots had greater aggregate inpatient lengths of stay when normalized to the number of children residing within a census tract. The disparities between hot spot (median SVI 0.73) and non-hot spot (median SVI 0.49) neighborhoods were large. A typical child living within the metropolitan Atlanta region with a median COI 2.0 score of 48 is considered to live within a moderate-opportunity area by national rankings (21); however, the median COI 2.0 score for a child residing in a neighborhood hot spot in the present study was in the lowest quintile, with a score of 14. These findings add to the literature on social determinants of health and pediatric hospital admissions for acute respiratory failure requiring mechanical ventilation – one of the most common reasons for PICU admission. By using complimentary and multi-dimensional composite measures of social vulnerability and child opportunity we build upon prior work that has focused exclusively on poverty as a driver of health outcome disparities in critically ill children.
Poverty is a factor associated with adverse health outcomes in critically ill children (4, 8). Andrist and colleagues performed a population-level, retrospective analysis of children residing in Hamilton County in Cincinnati, Ohio and showed that PICU admissions and inpatient bed day rates were higher for children in the most impoverished neighborhoods (4). Children with critical bronchiolitis living in low-income neighborhoods had longer PICU and hospital lengths of stay (8). Children living in impoverished neighborhoods, defined by the Area Deprivation Index of a ranked state Census Block Group, were nearly three times further distance from a hospital with a pediatric intensive care unit compared with children living in wealthier neighborhoods regardless of urban/suburban and rural area (22).
Poverty is one measure of risk associated with health disparities; however, health inequality is comprised of more complex and interrelated factors than measures of socioeconomics alone. For example, adverse childhood experiences, lack of access to education, provider bias, lack of access to healthcare and transportation, household crowding, structural racism, lack of access to healthy food and safe recreational spaces, and high levels of air and water pollution, also contribute to health disparities. The SVI and COI 2.0 are powerful tools because both indices encompass a more comprehensive measure of neighborhood vulnerability and opportunity by incorporating educational, environmental, household and transportation, and racial/ethnic minority and language metrics to hone in on broader aspects of the social determinants of health (6, 11, 13, 15, 23).
Protective factors, such as access to Early Childhood Education Centers, were higher in hot spot compared to non-hot spot neighborhoods. Despite having more Early Childhood Education Centers, including those rated as high-quality in hot spot neighborhoods, fewer children were enrolled compared to non-hot spot neighborhoods. Every other marker of opportunity was worse in a hot spot neighborhood compared with a non-hot spot neighborhood. Identifying modifiable causal neighborhood and environmental factors is critical to narrowing the gap in health disparities.
Much of the work identifying health disparities in pediatric critical illness is performed using large, administrative claims databases with information on geographical location limited to region in the United States. For example, Mitchell and colleagues used the 2016 Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID) to show that Black children with severe sepsis had an odds of death that was 1.19 (95% confidence interval: 1.02 – 1.38) times that of White children; this mortality difference was driven by Black neonates in the South (7). Furthermore, Hispanic and Black children had longer duration of hospitalization compared to White children (7). Causal reasons for health outcome disparities in children with severe sepsis include differential recognition of sepsis, bias in treatment approaches, and differential access to timely healthcare services for children of racial and ethnic minorities and those living in poverty (7). Race is a social construct, and race as a social variable by itself ignores the socioeconomic disparities and access to healthcare resources that exist secondary to systemic, structural racism (24). While many individual characteristics affecting health outcomes are not modifiable, community and policy changes can improve neighborhood conditions that contribute to disparate health outcomes. Incorporating neighborhood level metrics into pediatric intensive care and screening for individual level adverse childhood experiences may lead to novel causal mechanisms of increased disease severity and worse health outcomes for critically ill children (24).
How does a pediatric intensivist address larger issues of affordable housing, public transportation, employment training, access to quality education, and access to healthy food and recreational facilities within the confines of the intensive care unit? First, screening and incorporating social determinants of health should be universally incorporated into discharge planning to avoid stigmatization and stereotyping of individuals from racial and ethnic minority backgrounds. Second, families should be asked about their desire for help. Third, providers should refer families to community-based nonmedical services. Following the critical illness of a child, families need access to quality medical, psychological, and rehabilitation services. Pediatric intensivists must become advocates for their patients and families, and they must work collaboratively with community partners to mitigate the effects of critical illness. Without consideration of the social determinants of health, disparity in health outcomes following critical illness will widen (24).
Our study is limited by the retrospective review of EHR data for children admitted to two large Atlanta, Georgia PICUs for at least one day who were mechanically ventilated. The majority of children in the study live within the 29-county Atlanta metropolitan statistical area; however, the widest variation in child opportunity occurs within metropolitan regions (25). Residential address stability was not available for children admitted only once during the study period. We cannot account for children who may split time living at multiple addresses. We used neighborhood-level socioeconomic factors defined in the COI 2.0 rather than using individual level measures, which are unavailable in the EHR. We cannot verify the accuracy of a participants’ demographic data (24). An exploration of protective factors may inspire intervention efforts to lessen disparities in PICU admissions for acute respiratory failure requiring mechanical ventilation. Future prospective work should develop causal models to determine whether child neighborhood opportunity predicts better quality of life and functional status outcomes in survivors of pediatric critical illness.
In summary, children who live in hot spot neighborhoods who are admitted to a PICU for acute respiratory failure requiring mechanical ventilation, on average, live in areas with a high SVI and low COI. Attention to geospatial social determinants of health may provide further understanding of how physical and social environments contribute to critical illness in children. Ultimately, comprehensive assessment and mitigation of these social determinants in outpatient settings may help improve health equity and the need for PICU admission in children with acute respiratory failure requiring mechanical ventilation.
Supplementary Material
Research in Context:
Race and ethnicity are social constructs that are often used as surrogates for the social determinants of health. This practice lacks rigor, ignores the complexity of race and ethnicity, and exacerbates systemic racism in healthcare and research.
Social vulnerability and childhood opportunity indices are composite population variables at the census tract level that capture important aspects of the social determinants of health. These indices can help answer why racial/ethnic differences exist in pediatric critical care.
This retrospective, population-based ecological study links high social vulnerability and low childhood opportunity neighborhoods with higher frequency of admissions for acute respiratory failure with mechanical ventilation and with longer per capita hospital stays.
At the Bedside:
Neighborhood level geography, access to care, poverty, education opportunities and quality, food insecurity, access to green recreational spaces, and environmental pollution are associated with admissions for acute respiratory failure with mechanical ventilation.
Rather than using race/ethnicity as a proxy for social experiences, consideration of complex, multi-dimensional indices of social vulnerability and childhood opportunity get at the “why” behind healthcare disparities that race/ethnicity.
To lessen systemic structural racism in research and healthcare, sociologic factors – such as those in the social vulnerability and childhood opportunity indices – should be used when describing health disparities and considered when caring for a critically ill child.
This study was supported in part by:
K24 NR018866 awarded to AF; K23HL151897 awarded to JG; Buchter Resident Research Award awarded to NN
Copyright Form Disclosure:
Dr. Najjar disclosed that she received the Buchter Resident Research Award; she received support for article research from the Emory Department of Pediatrics and Children’s Healthcare of Atlanta. Dr. Fitzpatrick’s institution received funding from the National Institutes of Health (NIH) (K24 NR018866); she received support for article research from the NIH (K24 NR018866). Dr. Grunwell’s institution received funding from the NIH (K23HL151897-01); she received support for article research from the NIH. Dr. Opolka has disclosed that she does not have any potential conflicts of interest.
ABBREVIATIONS
- COI
Childhood Opportunity Index
- EHR
Electronic health record
- PICU
Pediatric intensive care unit
- SVI
Social Vulnerability Index
- TIGER
Topologically Integrated Geographic Encoding and Referencing
Footnotes
Author Disclosures: The authors have nothing to disclose.
REFERENCES
- 1.Ibiebele I, Algert CS, Bowen JR, et al. : Pediatric admissions that include intensive care: a population-based study. BMC Health Serv Res 2018; 18(1):264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khemani RG, Smith L, Lopez-Fernandez YM, et al. : Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med 2019; 7(2):115–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health) MBIW, (AHRQ) FW, (AHRQ) JH: Costs of Pediatric Hospital Stays, 2016. In: Quality AfHRa (Ed). Rockville, MD, Agency for Healthcare Research and Quality, 2019, p^pp [PubMed] [Google Scholar]
- 4.Andrist E, Riley CL, Brokamp C, et al. : Neighborhood Poverty and Pediatric Intensive Care Use. Pediatrics 2019; 144(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein D, Reibel M, Unger JB, et al. : The effect of neighborhood and individual characteristics on pediatric critical illness. J Community Health 2014; 39(4):753–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grunwell JR, Opolka C, Mason C, et al. : Geospatial Analysis of Social Determinants of Health Identifies Neighborhood Hot Spots Associated with Pediatric Intensive Care Use for Life-threatening Asthma. J Allergy Clin Immunol Pract 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell HK, Reddy A, Montoya-Williams D, et al. : Hospital outcomes for children with severe sepsis in the USA by race or ethnicity and insurance status: a population-based, retrospective cohort study. Lancet Child Adolesc Health 2021; 5(2):103–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slain KN, Shein SL, Stormorken AG, et al. : Outcomes of Children With Critical Bronchiolitis Living in Poor Communities. Clin Pediatr (Phila) 2018; 57(9):1027–1032 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention/ Agency for Toxic Substances and Disease Registry/ Geospatial Research A, and Services Program.: Social Vulnerability Index Data Documentation. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html. Accessed August 25, 2021 [Google Scholar]
- 10.Kids DD: Childhood Opportunity Index 2.0 Database. Available at: https://data.diversitydatakids.org/dataset/coi20-child-opportunity-index-2-0-database. Accessed August 25, 2021
- 11.Beck AF, Huang B, Wheeler K, et al. : The Child Opportunity Index and Disparities in Pediatric Asthma Hospitalizations Across One Ohio Metropolitan Area, 2011–2013. J Pediatr 2017; 190:200–206 e201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Givens M, Teal EN, Patel V, et al. : Preterm birth among pregnant women living in areas with high social vulnerability. Am J Obstet Gynecol MFM 2021; 3(5):100414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Javalkar K, Robson VK, Gaffney L, et al. : Socioeconomic and Racial and/or Ethnic Disparities in Multisystem Inflammatory Syndrome. Pediatrics 2021; 147(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paro A, Hyer JM, Diaz A, et al. : Profiles in social vulnerability: The association of social determinants of health with postoperative surgical outcomes. Surgery 2021 [DOI] [PubMed] [Google Scholar]
- 15.Krager MK, Puls HT, Bettenhausen JL, et al. : The Child Opportunity Index 2.0 and Hospitalizations for Ambulatory Care Sensitive Conditions. Pediatrics 2021; 148(2) [DOI] [PubMed] [Google Scholar]
- 16.Cambon J: tidygeocoder: Geocoding Made Easy. R package version 1.0.1 ed. 2020 [Google Scholar]
- 17.Walker K: tigris: Load Census TIGER/Line Shapefiles. R package version 1.0 ed. 2020 [Google Scholar]
- 18.Walker K, Herman M: tidycensus: Load US Census Boundary and Attribute Data as ‘tidyverse’ and ‘sf’-Ready Data Frames. R package version 0.10.2 ed. 2020 [Google Scholar]
- 19.Applehans T, Detsch F, Reudenbach C, et al. : mapview: Interactive Viewing of Spatial Data in R. R package version 2.9.0 ed. 2020 [Google Scholar]
- 20.Team RC: R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2013 [Google Scholar]
- 21.Kids DD: Data Visualization Childhood Opportunity Index by Metropolitan Statistical Area. Available at: https://www.diversitydatakids.org/research-library/data-visualization/snapshot-child-opportunity-across-us. Accessed August 25, 2021
- 22.Brown LE, Franca UL, McManus ML: Socioeconomic Disadvantage and Distance to Pediatric Critical Care. Pediatr Crit Care Med 2021; 22(12):1033–1041 [DOI] [PubMed] [Google Scholar]
- 23.Kersten EE, Adler NE, Gottlieb L, et al. : Neighborhood Child Opportunity and Individual-Level Pediatric Acute Care Use and Diagnoses. Pediatrics 2018; 141(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zurca AD, Suttle ML, October TW: An Antiracism Approach to Conducting, Reporting, and Evaluating Pediatric Critical Care Research. Pediatr Crit Care Med 2022; 23(2):129–132 [DOI] [PubMed] [Google Scholar]
- 25.Acevedo-Garcia D, Noelke C, McArdle N: The Geography of Child Opportunity: Why Neighborhoods Matter for Equity. Brandeis: The Heller School for Social Policy and Management, 2020, 1–53 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


