Abstract
Background
Recent studies with functional endoluminal imaging probe (EndoFLIP®) measure physiologic characteristics of the pylorus. EndoFLIP® has the potential to select optimal candidates for gastric peroral endoscopic myotomy (G-POEM). Normative values of the pylorus using EndoFLIP® have not been established.
Methods:
24 healthy volunteers (20–56 years old; 15 females) underwent unsedated, transoral EndoFLIP® measurements of the pylorus after 8 hours of fasting. Measurements of diameter (DM), balloon pressure, and distensibility index (DI) of the pylorus were obtained twice over 5 minutes at 40, 50, and 60mL balloon distensions.
Key Results:
Pyloric DM at 40, 50, and 60mL balloon distensions were 13.0±2.5, 14.3±1.8, and 17.2±2.0 mm, respectively. DM with 60mL distension was notably higher than with 40 and 50mL distensions. Pyloric DI at 40, 50, and 60mL distensions were 10.9±4.8, 11.3±5.8, and 11.1±4.3 mm2/mm Hg, respectively (P=0.86). Linear regression and Bland-Altman plots showed similar distribution of the DM and DI during the second minute compared to the full 5-minute measurements at 50mL distension, as well as between two sequential measurements using 50mL distension. With 50mL balloon distension, intraindividual coefficients of variation (COVintra) for DM and DI were 13.8% and 29.6%, respectively and interindividual COV (COVinter) were 12.6% and 51.3%, respectively. Similar reproducibility was obtained with 40mL balloon distension.
Conclusions & Inferences:
Unsedated EndoFLIP® can be used to characterize human fasting pyloric diameter and distensibility, with best performance observed with 40mL and 50mL distensions and data collection during the second minute. Normative values reported serve as reference values for future studies.
Keywords: area, tone, compliance, gastroparesis, G-POEM
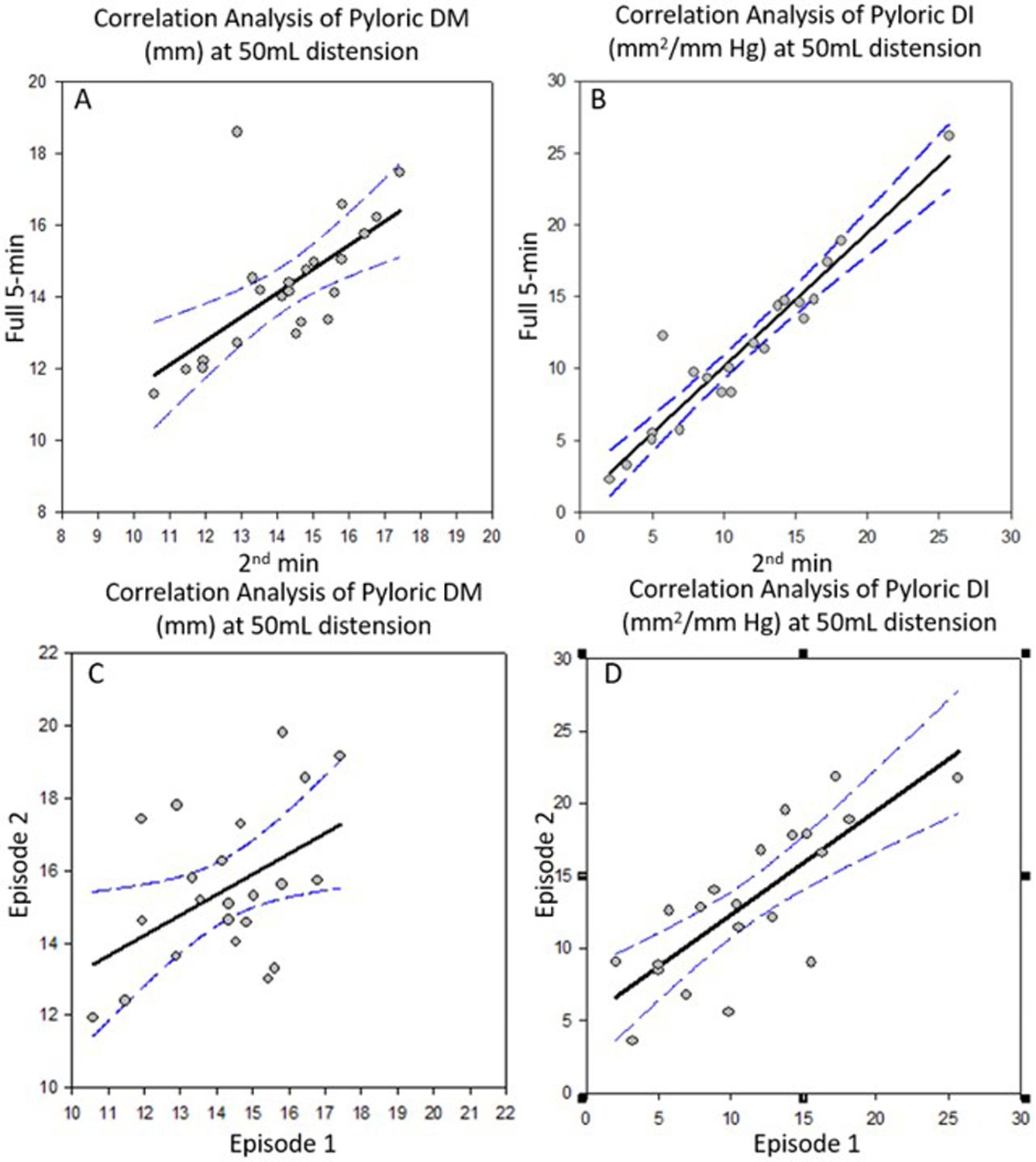
Graphcial Abstract
EndoFLIP® was used to characterize fasting pyloric diameter and distensibility in unsedated healthy volunteers. Stable measurements were observed at 2 minutes after balloon distension with optimal volume of 40–50mL.
INTRODUCTION
Pyloric dysfunction is associated with gastroparesis.1 In recent years, several open-label studies have suggested that gastric peroral endoscopic myotomy (G-POEM) could be a promising therapy for patients with refractory gastroparesis.2 Vosoughi et al. reported 12-month clinical efficacy of 56% for 75 patients with refractory gastroparesis who received G-POEM.3 A preliminary report documents benefit of G-POEM in a sham-controlled trial.4 However, predictors for the success of G-POEM remain unclear.5 This knowledge is critical considering the procedural risks, irreversible change in anatomy, and theoretical adverse events such as dumping syndrome.
Just as the endoscopic functional luminal imaging probe (EndoFLIP®) device is used to appraise the lower esophageal sphincter, transpylorically placed EndoFLIP® can measure physiologic characteristics of the pylorus, including diameter (DM) and distensibility index (DI), and thus has the potential to assist in selecting the optimal candidate for botulinum toxin injection6 or G-POEM. Pre-procedure pyloric distensibility less than 9.2 mm2/mmHg was predictive of clinical success of G-POEM with 72% sensitivity and 100% specificity.7 However, there is a dearth of data on normal pyloric function to guide clinical decision making. Furthermore, pyloric measurements are typically obtained during the G-POEM procedure under propofol anesthesia and opioid analgesia.7–12 Opioids increase pyloric tone and cause antral hypomotility,13,14 and propofol affects lower esophageal sphincter pressure,15 duodenal contractility,16 gastric emptying,17 and colonic motility.18 Only two prior studies have reported pyloric diameter and DI in healthy volunteers, one at 40mL balloon distension under propofol19, and the other at 10, 20, 30, and 40mL balloon distensions without sedation.20 Our aim was to optimize measurement and establish normative diameter and DI data for the fasting pylorus in unsedated, healthy adults using the EndoFLIP®.
METHODS
Data Source and Participants
Twenty-four healthy volunteers (15 females) between the ages of 18 and 65 years and body mass index between 18 and 35kg/m2 were screened with the validated Talley Bowel Disease Questionnaire for gastroesophageal reflux disease and gastrointestinal symptoms21,22 and were selected based on the absence of heartburn, regurgitation, dysphagia, or symptoms suggestive of gastroparesis.
All participants underwent clinical evaluations including physical examination and review of their medical records to exclude confounders such as use of opioids or treatments that could alter gastric motility.
Written informed consent was obtained from all participants. The study was approved by Mayo Clinic Institutional Review Board (IRB #20–012285).
Impedance Planimetry
Device:
Intraluminal measurements of the physiologic characteristics of the pylorus were obtained using a commercially available FLIP technology (EndoFLIP® EF-322, Medtronic Inc., Shoreview, MN). The assembly consists of a 240cm-long, 3mm outer diameter catheter with an infinitely compliant balloon mounted near the distal end of the catheter. The balloon assumes a 16cm-long cylindrical shape in the center, and it houses 16 impedance planimetry ring electrodes spaced at 1cm intervals and a solid-state pressure transducer. When positioned across the antropyloroduodenal junction, the electrodes simultaneously measure diameter corresponding to 16 channels, and intraballoon pressure (mmHg) is recorded by the pressure transducer.
Procedure:
Participants attended the Clinical Research Trials Unit at Mayo Clinic after an overnight fast lasting at least 8 hours. Under local anesthesia of the throat using 20% benzocaine spray, the EndoFLIP® catheter was inserted transorally, advanced and positioned across the antropyloroduodenal junction, with the distal 2–3 impedance sensors beyond the pylorus, as confirmed on fluoroscopy and by demonstration of a topographic waist (identifying the pylorus) in the impedance planimetry segment at a balloon distension volume of 20–30ml. After a 5-minute rest, the balloon was sequentially inflated to 40, 50, and 60mL, with continuous measurements of diameter, distensibility index, and intraballoon pressure for at least 5 minutes with each distension. This sequence was repeated once, providing two replicate measurements at each distension approximately 15 minutes apart. Throughout the measurement period, the transpyloric placement of the EndoFLIP® was continuously monitored by the study physician (TZ) and confirmed by the presence of distinct antral contractions (lasting >5 seconds and frequency up to 3 per minute) proximally and duodenal contractions (lasting <5 seconds and frequency up to 11 per minute) distal to the topographic waist. When catheter displacement was suspected, repositioning was performed under fluoroscopic guidance.
Data Analysis
EndoFLIP® data, including distension volume, intraballoon pressure, and 16 channels of luminal DM and DI for each subject, were exported to Microsoft Excel. Median DM and DI values of each channel, and intraballoon pressure during each minute of the distension at each volume and over the full 5-minute measurement period were calculated. The channel corresponding to the pylorus was identified as the one with the narrowest DM. This was visually cross-checked with the recorded EndoFLIP® topography by a study physician (TZ). The cross-sectional area (CSA) was calculated based on the assumption of circular geometry [area = (π*DM2/4)]. Analysis of the results for each minute during the different distensions showed that there was greater variation during the first minute and stable and consistent recordings during the second to fifth minutes. Therefore, all primary analyses were based on the second minute for each distension volume.
Statistical analysis consisted of descriptive analysis of mean and range for diameter, intraballoon pressure, CSA, and DI. Data show mean (SD) and median [10th, 90th percentiles]. Comparisons among all 3 balloon distension volumes were assessed by Repeated Measures Analysis of Variance. Intrasubject reproducibility between two replicate measurements of the same balloon distension for the second minute, and between the second minute and average over 5 minutes were assessed using correlation analysis and Bland-Altman plots (SigmaPlot®12 Systat Software Inc., Palo Alto, California). The correlation between intraballoon pressure and BMI was assessed using Spearman Rank Order Test. These data were presented for the 50mL balloon distension studies.
RESULTS
Demographics
Twenty-four healthy volunteers were evaluated. The mean age was 34.9 (range, 20–56) years and 16 (67%) were females. The mean (SD) body mass index (BMI) was 26.6 (3.6) kg/m2.
Fasting Pyloric Diameter, Pressure, and Compliance
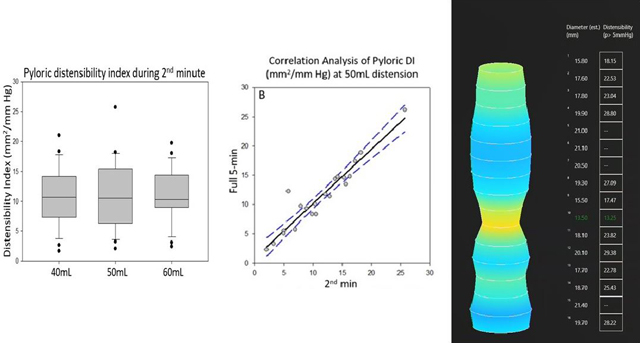
Pyloric DM and DI at 40, 50, and 60mL balloon distensions are shown in Figure 1. Supplemental Table 1 shows the measurements at all balloon distension volumes. Pair-wise comparisons showed statistical differences for pyloric DM (and correspondingly, CSA) across the 3 distension levels; however, only the 60mL distension resulted in notably higher DM, compared with 40 and 50mL distensions (Figure 1). Pyloric DI at 40, 50, and 60mL distensions were not different (P=0.86) (Figure 1 and Supplemental Table 1). There was no association between fasting pyloric intraballoon pressure and BMI (Supplemental Figure 1).
Figure 1.
Box plot of fasting pyloric diameter (left) and distensibility index (right) for unsedated healthy volunteers measured by EndoFLIP® during the second minute
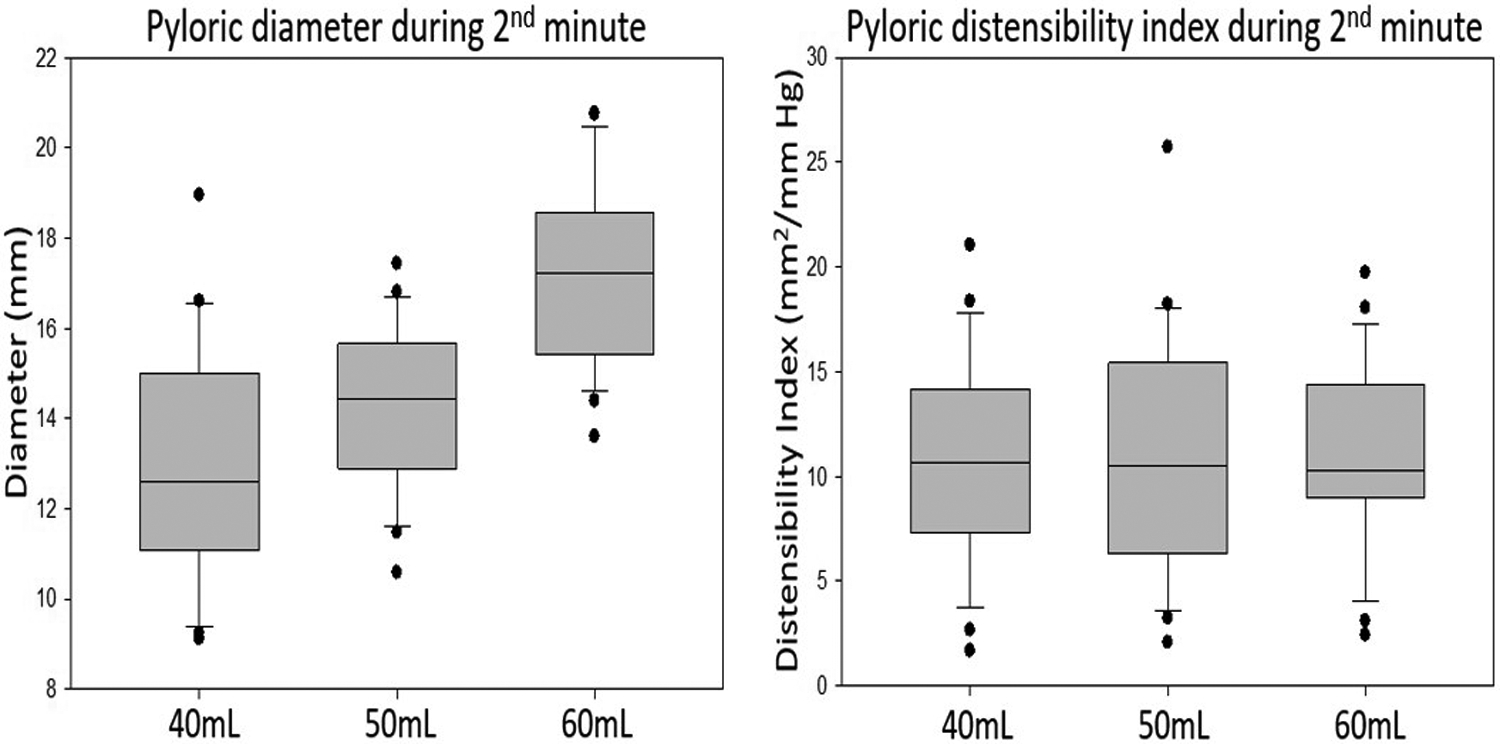
Correlation and Bland-Altman plots (Figure 2) showed similar distributions of DM and DI during the second minute compared to the full 5-minute measurements at 50mL distension. The lower panel of Figure 2 shows the reproducibility between the replicate measurements during two sequential measurements (termed “episodes”) using 50mL distension. The intraindividual coefficients of variation (COVintra) between episode 1 and episode 2 for DM and DI at 50mL distension were 13.8% and 29.6%, respectively. The interindividual coefficients of variation (COVinter) for DM and DI at 50mL distension were 12.6% and 51.3%, respectively (Supplemental Table 1). Similar reproducibility was obtained with 40mL and 60mL balloon distensions.
Figure 2.
Correlation analysis of pyloric diameter (DM) (A) and distensibility index (DI) (B) at 50mL distension for 2nd minute versus full 5-minute measurements, as well as for episode 1 (C) versus episode 2 (D)
DISCUSSION
In this study, fasting pyloric diameter of 24 unsedated, healthy volunteers measured with 40 and 50mL balloon distensions were similar and significantly smaller than with 60mL balloon distension. Given that DI were not significantly different for 40, 50, and 60mL balloon distensions, our study suggests that pyloric diameter, pressure, and distensibility can be most accurately measured by EndoFLIP® with balloon distension volume of 40–50mL. This range of balloon distension volumes was the most widely used in prior studies.6–12,19,20,23,24 Prior studies which used the EndoFLIP® for the assessment of the esophagogastric junction (EGJ) showed increasing CSA with increasing volumes of balloon distention from 20–50mL.25 At the pylorus, there was less prominent increase in CSA with increasing balloon distention, compared to the EGJ. This discrepancy may reflect the larger luminal size of the EGJ, compared to the pylorus. Therefore, it is conceivable that reported CSA of the EGJ at lower balloon volumes were confounded by under-distention. In a prior study, Gourcerol et al. reported increased pyloric pressure with balloon inflation from 10 to 40mL, yet this increase was numerically small. Similar to our study, there were no differences in fasting pyloric compliance (DI) across 10–40mL balloon distensions.20 Our findings of normative values of the pylorus are partially consistent with prior studies. For example, at 40mL balloon distension, Jagtap et al. reported similar values of pyloric DM, higher values of intraballoon pressure, and lower values of DI.19 On the other hand, Gourcerol et al. reported higher pyloric compliance (DI) and similar pyloric pressure.20 These reported differences highlight the need for standardization in pyloric assessment with EndoFLIP® and additional future studies.
Our study demonstrated excellent correlation of measurements between the second minute and the full 5-minute period for both pyloric diameter and distensibility. The distribution of measurements between two sequential periods under the same volume distensions showed good correlation, as reflected in the COVintra. Moreover, the COVinter are similar for the 40mL and 50mL balloon distensions. These results suggest that, despite differences in anatomy and physiology, the EndoFLIP® device initially designed to evaluate the esophageal sphincters can be used to study the gastric pylorus. While the COVintra and COVinter are similar for pyloric DM, the COVinter for DI is higher than COVintra, suggesting that EndoFLIP® measurements in assessing treatments might be best appraised in crossover studies.
As in prior studies, we noted phasic changes in pressure, DM, and DI due to the concomitant antral and duodenal contractions. Prior studies have attempted to mitigate this variability by taking measurements over a period of seconds where the readings are steady.6,19,20 Others measured over a longer period of time to improve stability.8,9,11 We took the precaution to take 5-minute continuous measurements, and analyzed the data stability for the first, second, and across the full 5 minute of measurements to appraise potential effect of the phasic changes. Since recordings became more stable after the first minute of balloon inflation and there was no difference between the second minute and across the full 5-minute intervals as shown in the correlation analyses, these validation studies favor waiting for the second minute after distension, and this recommendation differs from most studies which report readings within 1 minute of balloon inflation.6,8,9,19,20,23,24
One of the strengths of our study is that pyloric measurements were conducted in the absence of confounding agents such as propofol and opioid analgesia. A limitation of this study was the measurement of the pylorus in a fasting state, while postprandial assessment may be more relevant in the clinical setting. Although the sample size is relatively small, with uneven number of male and female volunteers, this study provides guidance on the standardization of transpyloric measurement with optimal performance observed during the second minute with 40mL and 50mL distensions as well as normative data which are useful for future studies in disease states such as gastroparesis.
Supplementary Material
Acknowledgements:
The authors thank the nursing staff in the Mayo Clinic Clinical Research Trials Unit for assistance with performance of motility measurements, and Mrs. Cindy Stanislav for excellent secretarial support.
Funding:
Dr. Michael Camilleri’s research on gastroparesis is funded by grant R01-DK122280 and DK125680 from National Institutes of Health. The study was conducted in the Clinical Trials Research Unit (supported by Mayo Clinic Center for Clinical and Translational Science (CCaTS) grant UL1-TR000135).
Footnotes
Conflicts of interest: The authors have no conflicts of interest.
References
- 1.Mearin F, Camilleri M, Malagelada JR. Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology. 1986;90(6):1919–1925. [DOI] [PubMed] [Google Scholar]
- 2.Aghaie Meybodi M, Qumseya BJ, Shakoor D, et al. Efficacy and feasibility of G-POEM in management of patients with refractory gastroparesis: a systematic review and meta-analysis. Endosc Int Open. 2019;7(3):E322–E329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vosoughi K, Ichkhanian Y, Benias P, et al. Gastric per-oral endoscopic myotomy (G-POEM) for refractory gastroparesis: results from an international prospective trial. Gut. 2021. [DOI] [PubMed] [Google Scholar]
- 4.Hustak RMJ, Vackova1 Z, et al. Endoscopic pyloromyotomy (G-POEM) improves symptoms in patients with refractory gastroparesis – a randomized sham controlled trial. United European Gastroenterol J. 2021;9:10–11. [Google Scholar]
- 5.Zheng T, Camilleri M. Selecting optimal patients with gastroparesis for G-POEM procedure. Gut. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desprez C, Melchior C, Wuestenberghs F, et al. Pyloric distensibility measurement predicts symptomatic response to intrapyloric botulinum toxin injection. Gastrointest Endosc. 2019;90(5):754–760 e751. [DOI] [PubMed] [Google Scholar]
- 7.Jacques J, Pagnon L, Hure F, et al. Peroral endoscopic pyloromyotomy is efficacious and safe for refractory gastroparesis: prospective trial with assessment of pyloric function. Endoscopy. 2019;51(1):40–49. [DOI] [PubMed] [Google Scholar]
- 8.Gregor L, Wo J, DeWitt J, et al. Gastric peroral endoscopic myotomy for the treatment of refractory gastroparesis: a prospective single-center experience with mid-term follow-up (with video). Gastrointest Endosc. 2021;94(1):35–44. [DOI] [PubMed] [Google Scholar]
- 9.Conchillo JM, Straathof JWA, Mujagic Z, et al. Gastric peroral endoscopic pyloromyotomy for decompensated gastroparesis: comprehensive motility analysis in relation to treatment outcomes. Endosc Int Open. 2021;9(2):E137–E144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Attaar M, Su B, Wong HJ, et al. Significant changes in impedance planimetry (EndoFLIP) measurements after peroral pyloromyotomy for delayed gastric emptying. Surg Endosc. 2021. [DOI] [PubMed] [Google Scholar]
- 11.Watts LS, Baker JR, Lee ALA, et al. Impact of gastric per-oral endoscopic myotomy on static and dynamic pyloric function in gastroparesis patients. Neurogastroent Motil. 2020;32(11). [DOI] [PubMed] [Google Scholar]
- 12.Vosoughi K, Ichkhanian Y, Jacques J, et al. Role of endoscopic functional luminal imaging probe in predicting the outcome of gastric peroral endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2020;91(6):1289–1299. [DOI] [PubMed] [Google Scholar]
- 13.Camilleri M, Lembo A, Katzka DA. Opioids in Gastroenterology: Treating Adverse Effects and Creating Therapeutic Benefits. Clin Gastroenterol Hepatol. 2017;15(9):1338–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camilleri M, Sanders KM. Opiates, the Pylorus, and Gastroparesis. Gastroenterology. 2020;159(2):414–421. [DOI] [PubMed] [Google Scholar]
- 15.de Leon A, Ahlstrand R, Thorn SE, Wattwil M. Effects of propofol on oesophageal sphincters: a study on young and elderly volunteers using high-resolution solid-state manometry. Eur J Anaesthesiol. 2011;28(4):273–278. [DOI] [PubMed] [Google Scholar]
- 16.Schnoor J, Unger JK, Kuepper T, et al. Effects of propofol and fentanyl on duodenal motility activity in pigs. Can Vet J. 2005;46(11):995–1001. [PMC free article] [PubMed] [Google Scholar]
- 17.Inada T, Asai T, Yamada M, Shingu K. Propofol and midazolam inhibit gastric emptying and gastrointestinal transit in mice. Anesth Analg. 2004;99(4):1102–1106. [DOI] [PubMed] [Google Scholar]
- 18.Diss LB, Villeneuve S, Pearce KR, Yeoman MS, Patel BA. Region specific differences in the effect of propofol on the murine colon result in dysmotility. Auton Neurosci. 2019;219:19–24. [DOI] [PubMed] [Google Scholar]
- 19.Jagtap N, Kalapala R, Reddy DN. Assessment of Pyloric Sphincter Physiology Using Functional Luminal Imaging Probe in Healthy Volunteers. J Neurogastroenterol Motil. 2020;26(3):391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gourcerol G, Tissier F, Melchior C, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41(4):360–367. [DOI] [PubMed] [Google Scholar]
- 21.Talley NJ, Phillips SF, Wiltgen CM, Zinsmeister AR, Melton LJ 3rd. Assessment of functional gastrointestinal disease: the bowel disease questionnaire. Mayo Clin Proc. 1990;65(11):1456–1479. [DOI] [PubMed] [Google Scholar]
- 22.Locke GR, Talley NJ, Weaver AL, Zinsmeister AR. A new questionnaire for gastroesophageal reflux disease. Mayo Clin Proc. 1994;69(6):539–547. [DOI] [PubMed] [Google Scholar]
- 23.Jehangir A, Malik Z, Petrov RV, Parkman HP. EndoFLIP and Pyloric Dilation for Gastroparesis Symptoms Refractory to Pyloromyotomy/Pyloroplasty. Dig Dis Sci. 2021;66(8):2682–2690. [DOI] [PubMed] [Google Scholar]
- 24.Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27(4):524–531. [DOI] [PubMed] [Google Scholar]
- 25.Desprez C, Roman S, Leroi AM, Gourcerol G. The use of impedance planimetry (Endoscopic Functional Lumen Imaging Probe, EndoFLIP(R)) in the gastrointestinal tract: A systematic review. Neurogastroent Motil. 2020;32(9). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


