Abstract
Background.
The optimal methods for measuring and analyzing anal resting and squeeze pressure with high-resolution manometry (HRM) are unclear.
Methods.
Anal resting and squeeze pressures were measured with HRM in 90 healthy women, 35 women with defecatory disorders (DD), and 85 with fecal incontinence (FI). Pressures were analyzed with Manoview™ software and a customized approach. Resting pressures measured for 20s, 60s, and 300s were compared. During the squeeze period, (3 maneuvers, 20s each), the squeeze increment, which was averaged over 5s, 10s, 15s, and 20s, and squeeze duration were evaluated.
Results.
Compared to healthy women, the anal resting pressure, squeeze pressure increment, and squeeze duration were lower in FI (P≤.04) but not in DD. The 20s, 60s, and 300s resting pressures were strongly correlated (concordance correlation coefficients=0.96–0.99) in healthy and DD women. The 5s squeeze increment was the greatest; 10s, 15s, and 20s values were progressively lower (P<.001). The squeeze pressure increment and duration differed (P<.01) among the three maneuvers in healthy and DD women but not in FI women. The upper 95th percentile limit for squeeze duration was 19.5s in controls, 19.9s in DD, and 19.3s in FI. Adjusted for age, resting pressure and squeeze duration, a greater squeeze increment was associated with a lower risk of FI vs health (OR,0.96; 95% CI, 0.94–0.97).
Conclusions.
These findings suggest that anal resting and squeeze pressures can be accurately measured over 20 seconds. In most patients, one squeeze maneuver is probably sufficient.
Keywords: Pelvic floor dysfunction, dyssynergic defecation, anal hypotonia
BACKGROUND
Anorectal manometry is widely used to assess diagnose defecatory disorders (DD) and evaluate anorectal functions in patients with fecal incontinence (FI) 1–5. There is consensus that anorectal pressures should be measured at rest, during squeeze, simulated evacuation, and a Valsalva maneuver 3,6,7. The rectoanal inhibitory reflex and rectal sensation are also evaluated during this test. Some centers also evaluate rectoanal pressures during a cough maneuver 8. The equipment, methods used to conduct anorectal manometry, and analyze studies are not standardized 9. The procedure can be performed with water-perfused, solid state, air-charged, or high-resolution catheters 2. High resolution manometry (HRM) catheters provide better spatial resolution than non-HRM catheters. However, HRM catheters made by different manufacturers are not identical. The methods, for HRM (e.g., the number and duration of squeeze maneuvers) are not standardized 9. Hence, the findings in patients need to be compared against normal values acquired with the same equipment and techniques. Towards the objective of standardizing anorectal manometry, a multi-center International Anorectal Physiology Working Group (IAPWG) suggested an anorectal manometry protocol 8. This protocol recommends that anal resting pressure should be measured once for 60s while anal squeeze pressure should be measured 4 times (i.e., 3 short (5s) and 1 long (30s) maneuvers). These recommendations are reasonable but are not evidence-based and differ from the protocol used at other centers and other guidelines 6. Other studies have explored approaches to improve the assessment and analysis of rectoanal pressures during evacuation 10,11. By comparing anal resting and squeeze pressures measured and analyzed with different methods, this study aimed to identify the optimal methods for measuring these pressures.
MATERIALS AND METHODS
Study Design
This report is compiled from four research studies in which rectoanal pressures were measured with anorectal HRM in healthy women, women with DD, and women with FI Mayo Clinic, Rochester, MN between 2008 and 2020. All participants consented to participate in these studies that were approved by the Institutional Review Board at Mayo Clinic.
Participants
This report comprises 90 healthy volunteers, 35 patients with DD, and 85 patients with FI, all women aged 18 years and older. The findings from all healthy volunteers and patients with DD, and 30 of 85 patients with FI have been published 12–15. The healthy volunteers were recruited by public advertisement and the patients were enrolled from the clinical practice. The healthy volunteers did not have symptom criteria for a functional bowel disorder as assessed with an interview and a validated questionnaire 16, and had no documented anorectal trauma during delivery (i.e., grade 3 or 4 laceration, forceps- assisted delivery) or any previous anorectal operations, including hemorrhoid procedures. Patients had symptom criteria for constipation-predominant IBS or urge-predominant fecal incontinence for 1 year or longer 16,17. Among FI patients, the severity of FI was computed with the Fecal Incontinence Severity Score (FISS) 17. Neither patients nor controls had clinically significant systemic (eg, cardiovascular, respiratory, neurologic) disease. Table 1 summarizes these studies and the participants.
Table 1.
Studies Included in this Report
| Feature | Study 1 13,14 | Study 2 34 | Study 1 13,14 | Study 3 12 | Study 4 | P value vs status (ANOVA) |
|---|---|---|---|---|---|---|
| N | 36 | 54 | 35 | 30 | 55 | NA |
| Disease | Asymptomatic healthy women | Asymptomatic healthy women | Defecatory disorders | Fecal incontinence | Fecal incontinence | |
| Duration for measuring anal resting pressure | 5 minutes | 20 seconds | 5 minutes | 20 seconds | 20 seconds | NA |
| Duration for measuring anal squeeze pressure | 20 seconds; 3 epochs | 20 seconds; 3 epochs | 20 seconds; 3 epochs | 20 seconds; 3 epochs | 20 seconds; 3 epochs | NA |
| Study status | Completed | Completed | Completed | Completed | Ongoing | NA |
| Demographic features | ||||||
| Age, years | 41 (16) | 45 (16) | 40 (12) | 55 (12) | 61 (10) | < .001 |
| BMI, kg/m2 | 26 (4) | 27 (5) | 26 (6) | 30 (5) | 29 (8) | < .001 |
| Clinical Features | ||||||
| Chronic constipation, n (%) | NA | NA | 34 (97%) | 10 (33%) | 11 (20%) | < .001 |
| Constipation-predominant IBS, n (%) |
NA | NA | 15 (43%) | 1 (3%) | 0 (0%) | < .001 |
| Functional diarrhea, n (%) | NA | NA | 0 (0%) | 3 (10%) | 4 (7%) | .005 |
| Diarrhea-predominant IBS, n (%) | NA | NA | 0 (0%) | 12 (40%) | 27 (49%) | < .001 |
|
Severity of FI (Fecal incontinence symptom severity score)
| ||||||
| Mild, n | NA | NA | NA | 0 | 1 (2%) | N/A |
| Moderate, n | NA | NA | NA | 17 (57%) | 42 (76%) | N/A |
| Severe, n | NA | NA | NA | 13 (43%) | 12 (22%) | N/A |
| Anorectal parameters | ||||||
| Mean anal resting pressure, mmHg 1 | 86 (20) | 76 (25) | 83 (26) | 60 (18) | 69 (28) | < .001 |
| Anal squeeze pressure, mmHg 1, 2 | 222 (62) | 198 (60) | 197 (50) | 132 (60) | 133 (61) | < .001 |
| Rectal balloon expulsion time (s) | 27 (53) | 11 (10) | 85 (84) | NA | 24 (47) | < .001 |
| Rectal balloon expulsion time >60s, n | 4 | 0 | 15 | NA | 6 | < .001 |
All values are mean (SD) unless specified otherwise
Analyzed with Manoview software.
This the highest of three values.
NA – not available
High Resolution Manometry
After 1–2 sodium phosphate enemas (Fleets, C.B. Fleet; Lynchburg,VA), HRM was performed with participants in the left lateral position with their hips and knees flexed. After the catheter was introduced per anus, pressures were allowed to stabilize and return to baseline for 2 minutes. Rectoanal pressures at rest and during squeeze were measured with Manoscan™ high resolution manometry catheters (currently Medtronic Inc, Minneapolis, MN, USA). These catheters (4.2 mm diameter) have 2 sensors within a rectal balloon and 10 equidistant sensors that are located at 6mm intervals along the anal canal. At each level, the values from 36 circumferential pressure sensors that measure pressures at 35Hz over a length of 2.5mm are averaged to obtain a single value. Pressures were measured at 10Hz at rest and during squeeze. The data were analyzed with the commercial software (Manoview AR v3.0, Medtronic Inc) and separately with a customized approach (Microsoft Excel, Microsoft Corporation).
Resting Pressure
Methods.
Anal resting pressure was measured for 20s in all participants. Among 35 healthy women and 35 patients with DD (Study 1, Table 1) 13,14, anal resting pressure was measured three times in the same study for 5 minutes on each occasion.
Data Analysis.
In all 210 participants, the 20s average values were computed with the Manoview program. Among study participants (i.e., in 35 healthy and 35 DD patients) in whom the resting pressure was measured for a longer duration, the resting pressure was only analyzed with the customized approach. The Manoview software analyzes pressures as follows. First, at each point in time, the eSleeve™ selects the highest single pressure recorded by any of the ten anal sensors. Then, the program averages these 200 eSleeve™ values (ie, over 20s) to obtain the mean resting pressure. By contrast to this method, which only uses the highest pressure at every instant, the customized analysis averages the values from 5 adjacent anal sensors to calculate the resting pressure. The location of these 5 sensors was individualized per participant. These 5 sensors span 2.4 cm, which is the 10th percentile value for the length of the anal high-pressure zone in asymptomatic women 15. These average values were averaged over 20s in all participants and over the first 20s, first 60s, and the entire 300s in the 35 healthy and 35 DD women.
Anal Squeeze Pressure Increment and Duration
Methods.
Participants were asked to contract or squeeze the anal sphincter three times (20s each), separated by 2 rest periods, each lasting 30s. They were encouraged to squeeze for as long as possible before they began the maneuver and through verbal feedback during the 20s maneuver.
Data Analysis.
The anal squeeze pressure was obtained from the Manoview™ program. Since the squeeze duration calculated by the Manoview™ software is erroneous (Supplementary Figure 1), the anal squeeze increment and duration were calculated with the customized program as follows. First, similar to the Manoview™ analysis, the highest pressure across all sensors was identified at every instant during the 20s squeeze maneuver. The anal squeeze pressure was the greatest 1s average value of these pressures. The squeeze increment was the difference (i.e., anal squeeze – resting pressure), where the anal resting pressure was measured over 1.5s immediately before the squeeze maneuver. The squeeze duration was the duration for which the anal pressure exceeded a threshold value, which was defined as follows:
where Prest is the resting pressure measured over 1.5s before to the squeeze maneuver and Pmax is the maximum pressure measured over 1s during the squeeze maneuver. In essence, this threshold is 50% of the squeeze pressure increment. The squeeze duration was computed by 2 approaches that considered all values and the longest consecutive series of values that exceeded this threshold during the 20s squeeze period.
Rectal balloon expulsion time
Participants were asked to expel a 4-cm-long balloon filled with 50 ml water from the rectum in privacy while seated on a commode 18,19. A balloon expulsion time greater than 60 seconds was considered to be prolonged 18,20.
Statistical Analysis
Lin’s concordance correlation coefficients (CCC) 21, Bland-Altman plots, and paired t-tests were used to compare the rest pressure measured over the first 20 s, first 60 s, and entire 5 minute epoch.
Wilcoxon’s rank sum test was used to compare the squeeze pressure increment computed over 5, 10, 15, and 20s durations, the squeeze pressure increment and duration for the first, second, and third maneuvers, and the squeeze pressure increment measured with all values and only consecutive values. Univariate and multiple predictor variable logistic regression models were used to identify anorectal dysfunctions associated with FI. Odds ratios are reported relative to healthy women. All analyses were performed with JMP 16 (SAS Institute, Cary, NC).
RESULTS
Clinical Features and Anal Pressures Measured with Manoview™ Analysis
The mean (SD) age was 43.3 (16.4) years in healthy women, 59.6 (11.0) years in women with FI, and 39.8 (11.7) years in women with DD (P<.001). The BMI was 26.2 (4.5) in healthy women, 29.6 (7.0) in FI, and 25.6 (5.9) in DD (P<.001).
Among patients, symptoms of chronic constipation (34 DD patients [97%] vs 21 FI patients [20%]) and constipation-predominant irritable bowel syndrome (15 DD patients [43%] vs 2 FI patients [.02%]) were more common in DD than in FI (P < 0.001). Conversely, functional diarrhea (7 FI patients [8%] vs 0 DD patients, P=.007) and diarrhea-predominant IBS (39 FI patients [46%] vs 0 DD patients, P<.001) were more prevalent in FI than in DD. Among FI patients, the mean (SD) fecal incontinence severity scale (FISS) score was 9.7 (1.4); scores between 7–10 reflect moderately severe FI.
Compared to healthy (80 [24] mmHg) and DD women (83 [26] mmHg), the 20s Manoview anal resting pressure was lower (P<.0001) in FI women (66 [25] mmHg). Table 1 provides the distribution of pressures in individual studies. Compared to healthy women, the 20s squeeze increment was not significantly different in DD (76 [41] vs 82 [42] mmHg, P=.46) but was lower (76 [41] vs. 33[23] mmHg) in FI (P<.001).
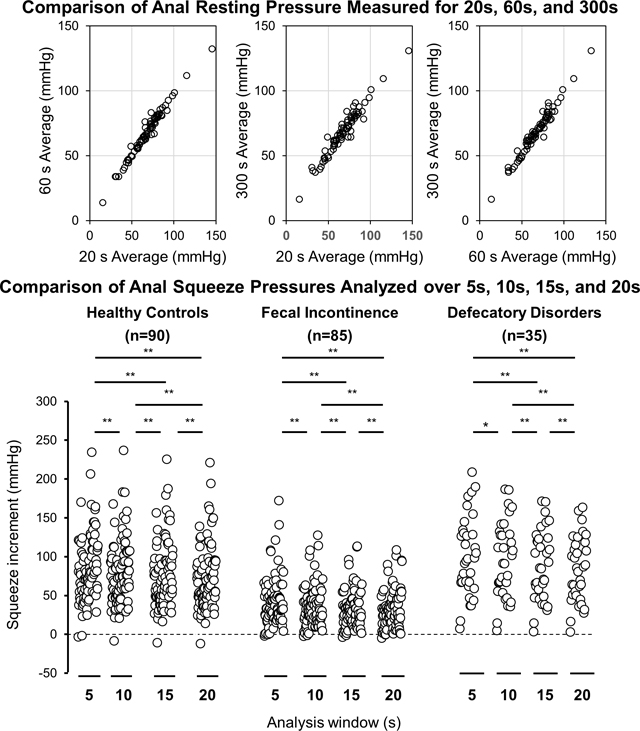
Anal resting pressure
The resting pressure analyzed with the Manoview method was correlated with (rho = .93, P<.0001) but lower (i.e., 57 (22) vs 75 (26) mmHg, P<.0001) than the corresponding pressure analyzed by the customized approach, which was averaged across 5-sensors.
During the first rest maneuver, the anal resting pressures averaged over the first 20s, first 60s, and the entire 300s were respectively 69 (17) in HV vs 67 (23) mmHg in DD, 68 (17) in HV vs 67 (21) mmHg in DD, and 69 (16) in HV vs 68 (20) mmHg in DD. The differences between healthy and DD women were not significant.
The resting pressures averaged over 20s, 60s, and 300s were significantly correlated with each other, i.e., the CCCs for 20s vs 60s, 60s vs 300s and 20s vs 300s measurements were respectively 0.98, 0.98, and 0.96. (Supplementary Figure 2, Table 2). Of these comparisons, only differences between 60s and 300s pressures were significant (P=.02), but the difference was only −1.1 (95% CI, −0.2 −-1.9) mmHg. The Bland Altman test indicates that the differences between these variables were not significantly related to the average value of both measurements (Supplementary Figure 2).
Table 2.
Comparison of Anal Resting Pressure Measured over 20s, 60s, and 300s in Healthy Women and Defecatory Disorders 1
| Rest Period | Comparisons | Concordance correlation coefficient [95% CI] | P value (paired t-test) | Bland-Altman plot mean difference [95% CI] |
|---|---|---|---|---|
| Rest 1 | 20s vs. 60s | 0.98 [0.97, 0.99] | P = .47 | 0.30 [−6.62, 7.23] |
| 20s vs. 300s | 0.96 [0.94, 0.98] | P = .22 | −0.76 [−10.93, 9.41] | |
| 60s vs. 300s | 0.98 [0.97, 0.99] | P= .02 | −1.06 [−8.11, 5.98] | |
| Rest 2 | 20s vs. 60s | 0.98 [0.96, 0.99] | P = .09 | −0.73 [−7.77, 6.30] |
| 20s vs. 300s | 0.97 [0.95, 0.98] | P = .20 | −0.65 [−9.06, 7.75] | |
| 60s vs. 300s | 0.99 [0.98, 0.99] | P = .79 | 0.08 [−4.65, 4.81] | |
| Rest 3 | 20s vs. 60s | 0.99 [0.98, 0.99] | P = .97 | 0.01 [−4.70, 4.72] |
| 20s vs. 300s | 0.97 [0.95, 0.98] | P = .29 | 0.53 [−7.78, 8.85] | |
| 60s vs. 300s | 0.98 [0.97, 0.99] | P = .19 | 0.52 [−6.05, 7.10] |
Resting pressure was measured three times for 300s each. The values are measurements averaged for the first 20s, first 60s, and the entire 300s period.
Comparison of anal squeeze pressure increment measured over different analysis windows
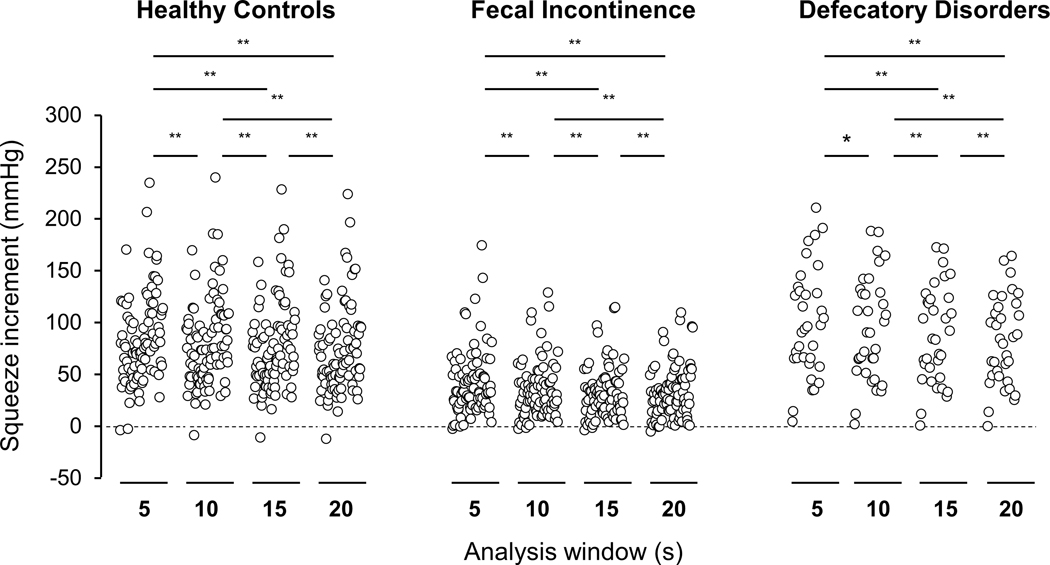
During the first squeeze maneuver, the anal squeeze increments measured for the first 5s, first 10s, first 15s, and the entire 20s period were respectively 87 (41), 82 (41), 79 (42), and 76 (41) mmHg in healthy women, 99 (51), 94 (49), 87 (46), and 82 (42) mmHg in women with DD, and 46 (31), 39 (27), 36 (25), and 34 (24) mmHg in women with FI (Figure 1). In all 3 groups, the differences between 5s vs 10s values, 5s vs 15s, 5s vs 20s, 10s vs 15s, 10s vs. 20s, and 15s vs. 20s were significant (P<.001).
Figure 1.
Comparison of anal squeeze increment computed for the first 5 s, 10s, and 15s, and the entire maneuver (20s) during the first squeeze maneuver. * P < .05; ** P < .01.
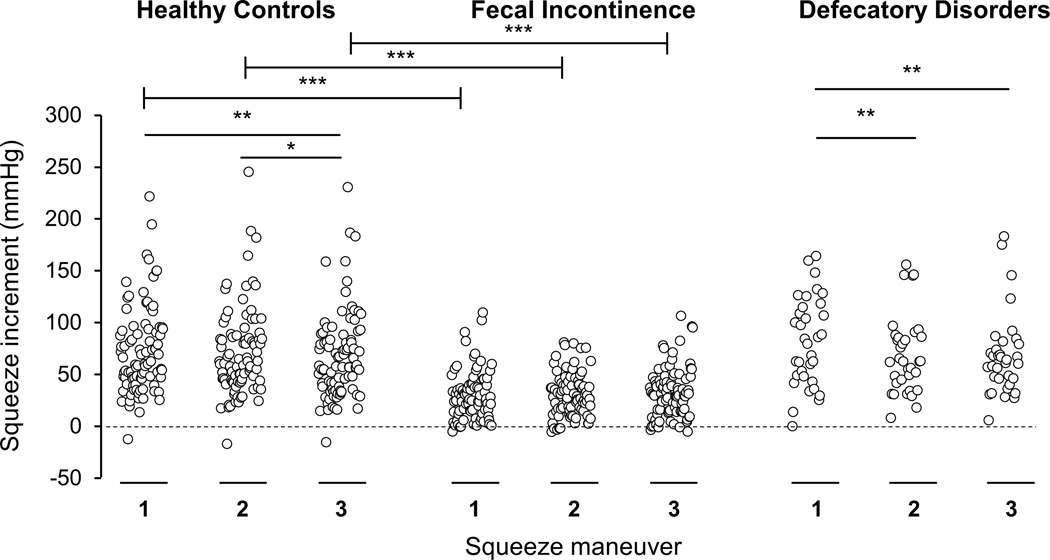
Comparison of anal squeeze pressure increment among maneuvers
In healthy women, the 20s squeeze pressure increment was not different between the first and second maneuvers (P=.06) (Table 3, Figure 2). Compared to the third maneuver, this increment was greater during the first (P=.003) and second (P=.02) maneuvers. By contrast, in women with FI, the squeeze pressure increment was not significantly different among the three maneuvers. In DD women, the squeeze increment was greater during the first than the second (P=.003) and the third maneuvers (P=.006).
Table 3.
Comparison of Anal Squeeze Pressure Increment and Duration in Healthy Women, Fecal Incontinence, and Defecatory Disorders
| Variable 1 | Healthy women | Fecal incontinence | Defecatory disorders | Healthy women vs FI | Healthy women vs DD |
|---|---|---|---|---|---|
| Increment (20s) | |||||
| Squeeze 1, mmHg | 76 (41) | 33 (23) | 82 (42) | P < .001 | ns |
| Squeeze 2, mmHg | 73 (41) | 33 (20) | 70 (37) | P < .001 | ns |
| Squeeze 3, mmHg | 69 (41) | 33 (21) | 69 (38) | P < .001 | ns |
| Squeeze 1 vs 2 | ns | Ns | P = .003 | - | - |
| Squeeze 1 vs 3 | P = .003 | Ns | P = .006 | - | - |
| Squeeze 2 vs 3 | P = .02 | Ns | ns | - | - |
| Longest consecutive method | |||||
| Squeeze 1, s | 8.1 (6.6)* | 5.8 (4.9)* | 10.0 (6.1)* | P = .04 | ns |
| Squeeze 2, s | 7.0 (5.9)* | 6.5 (5.9)* | 7.7 (5.7)* | ns | ns |
| Squeeze 3, s | 6.6 (5.4)* | 6.4 (5.2)* | 8.2 (6.1)* | ns | ns |
| Squeeze 1 vs 2 | ns | Ns | P = .008 | - | - |
| Squeeze 1 vs 3 | P = .003 | Ns | ns | - | - |
| Squeeze 2 vs 3 | ns | Ns | ns | - | - |
| All values | |||||
| Squeeze 1, s | 9.7 (6.6) | 8.2 (6.0) | 12.1 (5.8) | ns | ns |
| Squeeze 2, s | 9.8 (6.5) | 8.7 (6.4) | 10.8 (6.4) | ns | ns |
| Squeeze 3, s | 8.9 (6.3) | 9.5 (6.3) | 10.4 (6.2) | ns | ns |
| Squeeze 1 vs 2 | ns | ns | ns | - | - |
| Squeeze 1 vs 3 | ns | P = .02 | ns | - | - |
| Squeeze 2 vs 3 | P = .048 | ns | ns | - | - |
Values are Mean (SD) unless specified otherwise
Squeeze 1, 2, and 3 represent the three squeeze maneuvers.
ns = not significant; P value < .05
P < .001 for squeeze duration computed with all values versus longest consecutive sequence of values
Figure 2.
Comparison of anal squeeze increment (20s) during the three maneuvers. In healthy controls and DD but not FI patients, differences among maneuvers were significant. The increment was lower in FI than in healthy women. * P < .05 and ** P < .01 for within group comparisons; *** P < .001 for healthy controls vs FI.
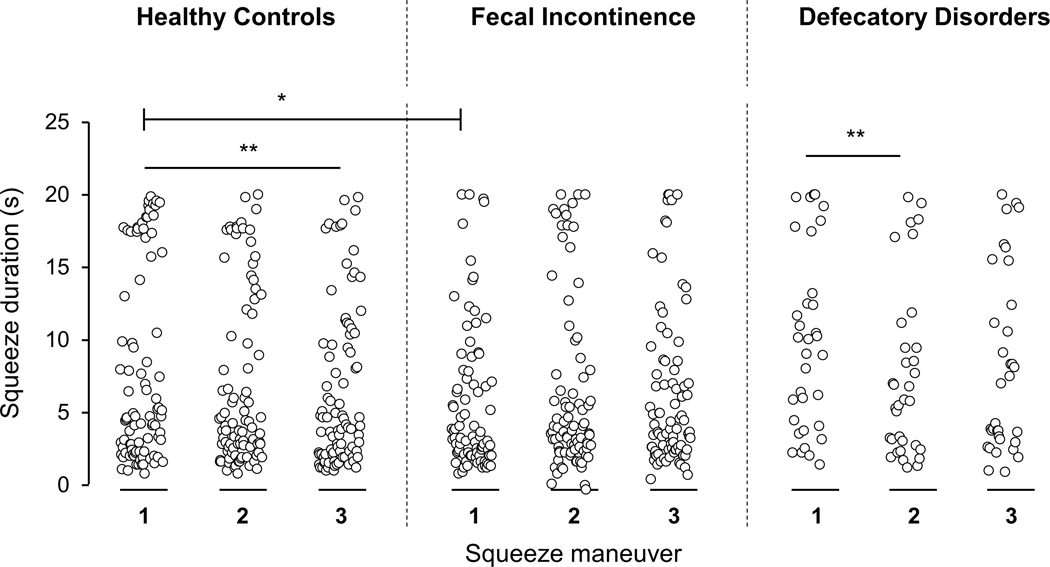
Assessment of anal squeeze duration
Of the 2 methods used to calculate this variable, the squeeze duration was longer when measured with all values rather than the longest consecutive sequence of values (P<.001) (Table 3). Compared to controls, the squeeze duration was shorter in FI and separately in DD women only when the duration was estimated with consecutive values in the first maneuver (Table 3, Figure 3). Hence, the squeeze duration calculated with consecutive values was used for subsequent analyses.
Figure 3.
Comparison of squeeze duration between controls and patients. Compared to the first squeeze maneuver, the third and second maneuvers were respectively shorter in controls and DD patients (** P < .01). During the first maneuver, the squeeze duration was also shorter in FI women than in healthy controls (*P < .05).
The upper 95th percentile value for squeeze duration (first maneuver) was 19.5s in healthy controls, 19.3s in FI, and 19.9s in DD. During the first maneuver, the squeeze duration computed with consecutive values was less useful (AUROC = 0.59) than the squeeze increment (AUROC = 0.85) for discriminating between healthy and FI women (Table 4).
Table 4.
Comparison of Squeeze Increment and Duration in Healthy Women and Fecal Incontinence1
| Variable | Area under ROC (5s window) | Area under ROC (10s window) | Area under ROC (15s window) | Area under ROC (20s window) |
|---|---|---|---|---|
| Squeeze increment | ||||
| Squeeze 1 | 0.83 | 0.85 | 0.85 | 0.85 |
| Squeeze 2 | 0.80 | 0.83 | 0.83 | 0.83 |
| Squeeze 3 | 0.80 | 0.81 | 0.81 | 0.80 |
| Squeeze duration (Consecutive values) | ||||
| Squeeze 1 | 0.51 | 0.60 | 0.59 | 0.59 |
| Squeeze 2 | 0.56 | 0.55 | 0.53 | 0.51 |
| Squeeze 3 | 0.60 | 0.50 | 0.49 | 0.49 |
Values represent the area under the receiving operator characteristic (ROC) curve for discriminating between healthy women and women with FI.
The squeeze duration was longer during the first than the third maneuver in healthy controls (P=.003, Table 3, Figure 3) and during the first than the second maneuver in DD patients (P=.008, Table 3, Figure 3). In FI women, neither the squeeze increment nor duration differed among the three maneuvers.
Comparison of anal squeeze pressures in healthy and FI women
In the univariate model, age was associated with an increased risk of FI (OR, 1.08; 95% CI, 1.05–1.11) (Table 5). After adjusting for age, the anal squeeze increment (OR, 0.96; 95% CI, 0.94 – 0.97) but not duration were associated with a lower risk of FI (Models 2 and 3). The anal squeeze increment remained significant after adjusting for age and anal squeeze duration (Model 5) and also for resting anal pressure (Model 6).
Table 5:
Utility of Anorectal Variables for Discriminating between Healthy Women and Fecal Incontinence
| Variables | Model 1 Odds Ratios (95% CI) | Model 2 Odds Ratios (95% CI) | Model 3 Odds Ratios (95% CI) | Model 4 Odds Ratios (95% CI) | Model 5 Odds Ratios (95% CI) | Model 6 Odds Ratios (95% CI) |
|---|---|---|---|---|---|---|
| Age, y | 1.08 (1.05,1.11) |
1.07 (1.05, 1.11) |
1.06 (1.03, 1.09) |
1.08 (1.05, 1.11) |
1.06 (1.03,1.10) |
1.06 (1.03, 1.10) |
| Anal resting pressure, mmHg | 0.99 (0.97, 1.002) |
1.00 (0.98, 1.02) |
||||
| Anal squeeze increment, mmHg | - | 0.96 (0.94, 0.97) |
- | 0.96 (0.94,0.97) |
0.96 (0.94, 0.97) |
|
| Anal squeeze duration, s | - | - | 0.98 (0.92, 1.04) |
1.04 (0.97,1.13) |
1.04 (0.97, 1.13) |
|
| Area under receiver operating characteristic curve | 0.78 | 0.79 | 0.87 | 0.78 | 0.87 | 0.87 |
DISCUSSION
We compared several approaches for computing anal resting and squeeze pressures with the Manoscan HRM system in healthy women, women with FI, and DD. In healthy women and DD patients, anal resting pressures measured for 20s, 60s, and 300s were significantly correlated. Except for a numerically small but statistically significant difference between 60s and 300s pressures, these values were not significantly different vs each other. In a paper that was published after we completed our study, the 60s resting pressure was perfectly correlated with the 30s pressure and strongly correlated with 10s pressure in FI women 22. Taken together, these observations suggest that anal resting pressure can be accurately measured for 30s rather than 60s as recommended in the IAPWG protocol 1. Neither 20s nor 60s measurements are sufficient to detect ultraslow waves, which have a frequency of 1–1.5 cycles/minute and an amplitude of 40mmHg or greater; however, the clinical significance of ultraslow waves is uncertain 6.
The 5s anal squeeze pressure increment was greater than the increment measured over the first 10s, first 15s and the entire 20s squeeze maneuver. The squeeze increment was not significantly different among the 3 squeeze maneuvers in FI. The squeeze duration was shorter in FI than in healthy women only during the first maneuver. Since the squeeze maneuver is primarily used to identify anal hypocontractility 8, which predisposes to FI, one squeeze maneuver is probably sufficient unless there is a concern that patients did not understand instructions during the first maneuver. Other authors too observed a significant correlation between the first and subsequent squeeze maneuvers in DD and FI patients and concluded that little is gained by performing more than one squeeze maneuver in FI 23.
The squeeze duration calculated with consecutive values was shorter than the duration calculated with all values. Intuitively, the squeeze pressure calculated from consecutive values is probably more representative of sphincter endurance than the calculation based on all values. Only the duration calculated with consecutive values discriminated between healthy women and patients with FI. Hence, this approach should be used to calculate the squeeze duration.
The squeeze duration provided by the Manoview™ program is erroneous. Prior studies that compared anal pressures measured with HRM in healthy people and FI patients did not report the anal squeeze duration 24–26. One study calculated the contractile integral 26, which is a product of the squeeze increment and duration. The anal squeeze duration is a physiologically relevant measure of sphincter endurance that improves with pelvic floor biofeedback therapy in men and women with FI 27. Since the 95th percentile value for squeeze duration is 19.5 s in healthy women, we recommend that patients should be asked to contract the anal sphincter for 20 seconds. After adjusting for other variables, age and the squeeze increment but not duration independently discriminated between healthy women and women with FI, which suggests that the squeeze duration is not independently useful for discriminating between healthy and FI women.
Perhaps the anal squeeze increment and duration predominantly represent the function of fast-twitch (type 2) and slow-twitch (type 1) fibers respectively 28. Compared to other striated muscles, the external anal sphincter has a higher percentage of slow-twitch fibers and is therefore relatively fatigue resistant. In studies that were performed with non–high-resolution manometry, the external anal sphincter was more fatigable after childbirth 29 and in women with FI 30,31. However, differences between men and women with FI were not significant 27.
Similar studies are necessary to determine if these findings apply to other catheters, and to men, because the anal squeeze pressure is higher than in men than women 15. The upper 95th percentile value for squeeze duration (first maneuver) was between 19.3 – 19.9s in all 3 cohorts. Consistent with the standard, automated recording time for the squeeze maneuver in the Manoscan HRM program, participants were asked to squeeze for 20s. It is conceivable that a longer assessment may uncover more pronounced differences in the squeeze duration between healthy and FI women.
Taken together with other recent studies, these findings provide the basis for streamlining the anorectal HRM procedure. Because anal pressures stabilized within 150s, typically in 90s, after the catheter was inserted 32, the equilibration period before pressure measurements commence can perhaps be shortened to less than the 3 minutes recommended by the IAPWG 8. Among FI patients, the London group observed that resting pressures can be evaluated over 30 instead of 60 seconds recommended by the IAPWG protocol 33 and that 2 rather than 3 squeeze maneuvers are sufficient 22. Our findings suggest that anal resting and squeeze pressures should each be measured for 20s. As suggested above, arguably, a longer squeeze maneuver may be more useful for distinguishing between healthy and FI women. While one squeeze maneuver is probably sufficient 23, an additional maneuver may be reasonable if there is concern that patients did not understand the instructions during the first squeeze maneuver. So implemented, these changes will take less time than the IAPWG guidelines that recommend one resting maneuver lasting 60s followed by 3 squeeze maneuvers of 5s and 1 squeeze maneuver lasting 20s each.
Supplementary Material
ACKNOWLEDGEMENTS
• NO analyzed and reviewed the data and authored the manuscript
• BD, SR, and ZC analyzed and reviewed the data
• KF collected the data
• AEB designed the study, analyzed the data and authored the manuscript
• All authors reviewed and approved the final submitted version.
FUNDING
This work was supported in part by USPHS NIH Grant R01 DK78924 to Dr. Bharucha.
Footnotes
DISCLOSURES
Dr. Bharucha jointly holds a patent for an anorectal catheter fixation clip with Medtronic, Inc and a patent for a portable anorectal manometry device made by Medspira, Inc.
REFERENCES
- 1.Lee TH, Bharucha AE. How to Perform and Interpret a High-resolution Anorectal Manometry Test. Journal of neurogastroenterology and motility. 2016;22(1):46–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basilisco G, Bharucha AE. High-resolution anorectal manometry: An expensive hobby or worth every penny? Neurogastroenterology & Motility. 2017;29(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carrington EV, Scott SM, Bharucha A, et al. Expert consensus document: Advances in the evaluation of anorectal function. Nature Reviews Gastroenterology & Hepatology. 2018;15(5):309–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bharucha AE, Wald A. Chronic Constipation. Mayo Clinic Proceedings. 2019;94(11):2340–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bharucha AE, Lacy BE. Mechanisms, Evaluation, and Management of Chronic Constipation. Gastroenterology. 2020;158(5):1232–1249.e1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao SS, Azpiroz F, Diamant N, Enck P, Tougas G, Wald A. Minimum standards of anorectal manometry. Neurogastroenterology & Motility. 2002;14(5):553–559. [DOI] [PubMed] [Google Scholar]
- 7.Srinivasan SG, Sharma M, Feuerhak K, Bailey KR, Bharucha AE. A comparison of rectoanal pressures during Valsalva maneuver and evacuation uncovers rectoanal discoordination in defecatory disorders. Neurogastroenterology & Motility. 2021:e14126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil. 2020;32(1):e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrington EV, Heinrich H, Knowles CH, et al. Methods of anorectal manometry vary widely in clinical practice: Results from an international survey. Neurogastroenterology & Motility. 2017;29(8):e13016. [DOI] [PubMed] [Google Scholar]
- 10.Heinrich H, Fruehauf H, Sauter M, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterology and Motility. 2013;25(230):e163. [DOI] [PubMed] [Google Scholar]
- 11.Sharma M, Muthyala A, Feuerhak K, Narayanan SP, Bailey KR, Bharucha AE. Improving the Utility of High Resolution Manometry for the Diagnosis of Defecatory Disorders in Women with Chronic Constipation. Neurogastroenterol and Motility. 2020. Jul 01:e13910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bharucha AE, Fletcher JG, Camilleri M, Edge J, Carlson P, Zinsmeister AR. Effects of clonidine in women with fecal incontinence. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2014;12(5):843–851 e842; quiz e844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chakraborty S, Feuerhak K, Muthyala A, Harmsen WS, Bailey KR, Bharucha AE. Effects of Alfuzosin, an Alpha-1 Alphadrenergic Antagonist on Anal Pressures and Bowel Habits, in Women With and Without Defecatory Disorders. Clinical Gastroenterology & Hepatology. 2018;18:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muthyala A, Feuerhak KJ, Harmsen WS, Chakraborty S, Bailey KR, Bharucha AE. Effects of psychosensory stimulation on anal pressures: Effects of alfuzosin. Neurogastroenterol Motil. 2019;31(7):e13618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oblizajek NR, Gandhi S, Sharma M, et al. Anorectal pressures measured with high-resolution manometry in healthy people—Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterology and Motility : the official journal of the European Gastrointestinal Motility Society. 2019:e13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bharucha AE, Locke GR, Seide B, Zinsmeister AR. A New Questionnaire for Constipation and Fecal Incontinence. Alimentary Pharmacology & Therapeutics. 2004;20:355–364. [DOI] [PubMed] [Google Scholar]
- 17.Noelting J, Zinsmeister AR, Bharucha AE. Validating endpoints for therapeutic trials in fecal incontinence. Neurogastroenterology and Motility. 2016;28(8):1148–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ratuapli S, Bharucha AE, Harvey D, Zinsmeister AR. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil. 2013;25(12):e813–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prichard DO, Lee T, Parthasarathy G, Fletcher JG, Zinsmeister AR, Bharucha AE. High-resolution Anorectal Manometry for Identifying Defecatory Disorders and Rectal Structural Abnormalities in Women. Clinical Gastroenterology & Hepatology. 2017;15(3):412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mazor Y, Prott G, Jones M, Kellow J, Ejova A, Malcolm A. Anorectal physiology in health: A randomized trial to determine the optimum catheter for the balloon expulsion test. Neurogastroenterol Motil. 2019;31(4):e13552. [DOI] [PubMed] [Google Scholar]
- 21.Carrasco JL, Jover L. Estimating the generalized concordance correlation coefficient through variance components. Biometrics. 2003;59(4):849–858. [DOI] [PubMed] [Google Scholar]
- 22.Ang D, Vollebregt P, Carrington EV, Knowles CH, Scott SM. Redundancy in the International Anorectal Physiology Working Group Manometry Protocol: A Diagnostic Accuracy Study in Fecal Incontinence. Digestive Diseases & Sciences. 2021;03:03. [DOI] [PubMed] [Google Scholar]
- 23.Mazor Y, Jones M, Malcolm A. Repeated measurements in anorectal manometry. Neurogastroenterology & Motility. 2021;33(10):e14209. [DOI] [PubMed] [Google Scholar]
- 24.Townsend DC, Carrington EV, Grossi U, et al. Pathophysiology of fecal incontinence differs between men and women: a case-matched study in 200 patients. Neurogastroenterology & Motility. 2016;28(10):1580–1588. [DOI] [PubMed] [Google Scholar]
- 25.Zifan A, Ledgerwood-Lee M, Mittal RK. A Predictive Model to Identify Patients With Fecal Incontinence Based on High-Definition Anorectal Manometry. Clinical Gastroenterology & Hepatology. 2016;14(12):1788–1796.e1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carrington EV, Knowles CH, Grossi U, Scott SM. High-resolution Anorectal Manometry Measures Are More Accurate Than Conventional Measures in Detecting Anal Hypocontractility in Women With Fecal Incontinence. Clinical Gastroenterology & Hepatology. 2019;17(3):477–485.e479. [DOI] [PubMed] [Google Scholar]
- 27.Mazor Y, Jones M, Andrews A, Kellow JE, Malcolm A. Novel insights into fecal incontinence in men. American journal of physiology Gastrointestinal and liver physiology. 2017;312(1):G46–G51. [DOI] [PubMed] [Google Scholar]
- 28.Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterology & Motility. 2006;18(7):507–519. [DOI] [PubMed] [Google Scholar]
- 29.Cattle KR, Telford K, Kiff ES. Changes in fatigability of the striated anal canal after childbirth. Colorectal Disease. 2010;12(9):880–884. [DOI] [PubMed] [Google Scholar]
- 30.Telford KJ, Ali ASM, Lymer K, Hosker GL, Kiff ES, Hill J. Fatigability of the external anal sphincter in anal incontinence. Diseases of the Colon & Rectum. 2004;47(5):746–752; discussion 752. [DOI] [PubMed] [Google Scholar]
- 31.Marcello PW, Barrett RC, Coller JA, et al. Fatigue rate index as a new measurement of external sphincter function. Diseases of the Colon & Rectum. 1998;41(3):336–343. [DOI] [PubMed] [Google Scholar]
- 32.Wickramasinghe DP, Jayarajah U, Samarasekera DN. Duration taken for the anal sphincter pressures to stabilize prior to anorectal manometry. BMC Research Notes. 2018;11(1):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterology & Motility. 2020;32(1):e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noelting J, Ratuapli SK, Bharucha AE, Harvey D, Ravi K, Zinsmeister AR. Normal Values For High-Resolution Anorectal Manometry In Healthy Women: Effects Of Age And Significance Of Rectoanal Gradient. American Journal of Gastroenterology. 2012;107(10):1530–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.